Lupus-prone mice develop a chronic inflammatory response to cutaneous injury that depends on the production of type I interferon, TLR7, and TLR9.
Abstract
Recognition of endogenous DNA and RNA by cells expressing TLR7 and TLR9 is an important contributor to the pathogenesis of systemic lupus erythematosus and has been suggested to contribute to cutaneous lupus and to a group of related inflammatory skin diseases termed interface dermatitis. We have developed a mouse model of TLR7- and TLR9-dependent skin inflammation using tape stripping. In normal mice, this resulted in a rapid but transient inflammatory cell infiltration accompanied by induction of type I IFN production by plasmacytoid dendritic cells (PDCs) and release of extracellular traps and proinflammatory cytokines by neutrophils. These responses were strongly reduced in MyD88-deficient mice and in mice treated with a bifunctional inhibitor of TLR7 and TLR9. In contrast, in lupus-prone (NZBxNZW)F1 mice, tape stripping induced the development of chronic lesions characterized by a persistent type I IFN gene signature and many clinical and histological features of cutaneous lupus. Depletion of PDCs before injury prevented the development of skin lesions, whereas treatment with a bifunctional TLR7/9 inhibitor before tape stripping or after the initial lesion was established led to a significant reduction of the disease. These data suggest that inhibitors of TLR7 and TLR9 signaling have potential therapeutic application for the treatment of interface dermatitis.
The triggering of TLR7 and TLR9 in plasmacytoid DC (PDC) precursors and B cells by self–nucleic acids is key in the pathogenesis of systemic lupus erythematosus (SLE). This leads to the production of type I IFNs from PDCs that can be detected by the up-regulation of IFN-regulated genes in the blood of patients (IFN signature) and anti-DNA and anti-RNP antibodies from B cells that form immunocomplexes (ICs) with DNA or RNA from dying cells (for reviews see Marshak-Rothstein, 2006; Barrat and Coffman, 2008). IFN-α and PDCs have been proposed to contribute to the pathogenesis of other autoimmune diseases characterized by IFN-α signature as well. Indeed, type I IFN–producing PDCs accumulate in the pancreas, muscle, and salivary glands of people affected by diabetes mellitus, dermatomyositis, and Sjögren’s syndrome, respectively, strongly suggesting that dysregulated PDC activation could be a more general feature of autoimmune disease (for reviews see Ueno et al., 2007; Barrat and Coffman, 2008; Guiducci et al., 2009).
PDCs and type I IFN appear to play a similar role in several cutaneous autoimmune diseases, including lichen planus, dermatomyositis, lichen sclerosis, cutaneous graft versus host disease and the cutaneous forms of lupus (cutaneous lupus erythematosus [CLE]; for review see Wenzel and Tüting, 2008). The common pathological feature of these diseases is interface dermatitis, a specific inflammatory pattern characterized by (a) vacuolar changes (liquefaction) of the basal layers of the epidermis, (b) the presence of apoptotic keratinocytes, (c) the accumulation of cytotoxic CD8 T cells and neutrophils in the upper dermis, and (d) prominent IFN-α signature in the skin. The close association between IFN-α–producing PDCs and granzyme B–positive T cells together with accumulation of nucleic acid–containing ICs at the junction of dermis and epidermis (for review see McCauliffe, 1996) suggests that the chronic presence of PDCs producing IFN-α may play a central role in disease development (Blomberg et al., 2001; Farkas et al., 2001; for review see Wenzel and Tüting, 2008).
Despite this evidence implicating PDCs in autoimmune skin inflammation in humans (for review see Wenzel and Tüting, 2008), studies of the mode of activation of PDCs and their contribution to pathogenesis have been hampered by the absence of an animal model reflecting the central features of such diseases. In this study, we report development of a mouse model in which cutaneous injury by tape stripping leads to rapid infiltration and activation of PDCs and neutrophils. Although tape stripping causes a transient, self-limiting response in normal mice, the same treatment in a strain of lupus-prone mice produces a chronic lesion with many similarities to CLE. Our data thus suggest that when chronically activated, PDCs are a key player in inducing skin damage through sustained production of IFN-regulated genes as well as proinflammatory cytokines. Furthermore, we demonstrate that novel specific inhibitors of TLR7 and TLR9 can prevent skin damage when used in therapeutic settings.
RESULTS
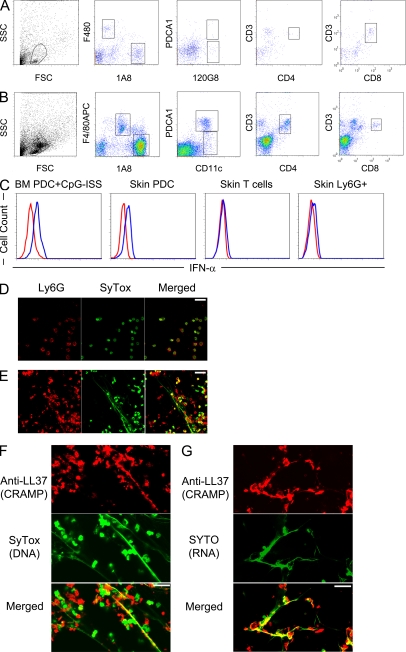
Activated PDCs and neutrophils infiltrate skin rapidly after tape stripping
As a method to induce mild cutaneous injury and inflammation, we used tape stripping, a method previously used to provoke disease in mouse models of psoriasis and atopic dermatitis (Inoue et al., 2005; Sano et al., 2005; Jin et al., 2009). Tape stripping has also been used as a noninvasive method for detecting and diagnosing lupus, as lupus patients overreact to this mild cutaneous injury compared with healthy individuals. However, the nature of the inflammatory response to tape stripping has not been well characterized at the cellular or molecular level. At 24 h after tape stripping, we observed a pronounced increase of inflammatory cells in the skin (Fig. 1 B) compared with untreated skin (Fig. 1 A), including a cell population expressing the PDC markers CD11c+ and PDCA1+ (Fig.1 B) as well as 120G8+ and Ly-6C (not depicted). The PDCs are functionally active as they produce IFN-α, measured by intracellular staining in cells isolated from the skin (Fig. 1 C). Flow cytometric analysis also revealed a massive influx of neutrophils (Ly-6G+ cells) and a lesser increase in macrophages (F4/80+ cells) along with CD4+ and CD8+ T cells (Fig. 1 B).
Figure 1.
Skin injury provokes leukocyte infiltration and activation, including production of IFN-α by PDCs and secretion of NETs by neutrophils. (A and B) Cellular infiltrate in the skin of 129 mice was characterized before (A) and 24 h after inflammation via tape stripping (B) by flow cytometry. PDCs were identified as CD11C+PDCA1+120G8+, conventional DCs as CD11c+PDCA1−120G8−, neutrophils as Ly-6G+(1A8) F480−, skin macrophages as F480+ Ly-6G low, and T cells as CD4+CD3+ and CD8+CD3+. Representative FACS plots of at least 10 mice processed from three independent experiments are shown. (C) 129 mice were tape stripped, and 24 h later, PDC infiltrating cells were assessed for IFN-α production by flow cytometry analysis. Neutrophils (Ly-6G+) and T cells (CD3+) were used as a negative control. Cultured BM-derived PDCs stimulated for 3 h with CpG-ISS were used as a positive control. A representative of three independent experiments (10 mice per experiments) with similar results is shown. (D and E) The ability of neutrophils to form NETs when isolated from BM (as source of inactivated neutrophils; D) or the skin of mice 24 h after tape stripping (E) was determined by immunostaining using Ly-6G to detect neutrophils and the SYTOX dye to stain DNA. (F and G) The presence of LL37-containing DNA (F) or RNA (G) NET fiber was detected by immunostaining using specific dyes. (D) Data from two independent experiments are shown. (E–G) Representative data from five fields from the skin of 10 mice from two independent experiments are shown. Bars, 20 µm.
Activated neutrophils produce neutrophil extracellular traps (NETs), which are essential to kill bacteria in vivo (Brinkmann et al., 2004; Fuchs et al., 2007; for review see Wartha and Henriques-Normark, 2008). Neutrophils infiltrating tape-stripped skin are activated, producing abundant NETs with long chromatin fibers (Fig. 1 E), whereas no NET formation was observed in unstimulated BM neutrophils that we used as controls (Fig. 1 D). In skin neutrophils, the long fibers of the NETs contained both DNA and RNA and were associated with LL37/CRAMP (Fig. 1, F and G), a cationic antimicrobial peptide secreted by activated neutrophils (Kessenbrock et al., 2009; for review see Wartha and Henriques-Normark, 2008).
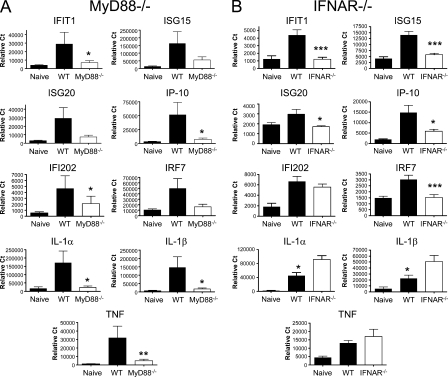
Signaling through TLR7 and TLR9 leads to rapid induction of IFN-regulated and proinflammatory genes at the site of cutaneous injury
Accompanying the cellular infiltration, epidermal injury resulted in strong induction of many prominent inflammatory genes in messenger RNA (mRNA) isolated from both skin biopsies and infiltrating leukocytes (Fig. 2 and Fig. S1). The induction of these genes required MyD88, as shown by the lack of gene induction in MyD88-deficient mice (Fig. 2 A and Fig. S1 A). To define the regulation of these genes, we repeated the experiment using IFNAR−/− mice that were lacking one chain of the type I IFN receptor. In these IFN-α/β–unresponsive mice, IFIT1, ISG15, IRF7, and ISG20, all IFN-regulated genes, were not induced (Fig. 2 B and Fig. S1 B) in either compartment, and IP-10 was reduced in the skin (Fig. 2 B) but not in the infiltrating cells (Fig. S1 B). Another IFN-regulated gene, IFI202, was induced in IFNAR−/− mice, which is consistent with previous studies showing an IFN-independent signaling pathway for this gene in mice (for reviews see Asefa et al., 2004; Choubey and Panchanathan, 2008). In contrast, the lack of IFN-α/β signaling did not reduce the induction of TNF, IL-1α, or IL-1β (Fig. 2 B and Fig. S1 B). Instead, expression of these inflammatory genes was somewhat increased in the IFNAR−/− in mRNA from total skin (Fig. 2 B) but not in infiltrating cells (Fig. S1 B), possibly reflecting the previously reported reciprocal regulation of the type I IFN and TNF pathways (for review see Banchereau et al., 2004). The clear requirement for MyD88 in the induction of all three proinflammatory genes demonstrates an important role for signaling through members of IL-1 receptor or Toll-like receptor (TLR) families.
Figure 2.
The MyD88 signaling pathway is necessary for the up-regulation of both type I IFN–regulated and proinflammatory genes. (A) MyD88−/− (white bars) and age-matched WT C57BL/6 mice (black bars) were either left untreated (naive) or tape stripped to provoke inflammation. 24 h later, skin biopsies were isolated, and the levels of proinflammatory genes were evaluated by TaqMan. (B) IFNAR−/− mice (white bars) and age-matched WT 129 mice (black bars) were either left untreated (naive) or tape stripped to provoke inflammation. 24 h later, skin biopsies were isolated, and the levels of proinflammatory genes were evaluated by TaqMan. Naive (untreated) groups are shown for C57BL/6 and 129 mice only. Cumulative data from at least two independent experiments (n = 15–20) are shown (mean ± SEM; *, P ≤ 0.05; **, P ≤ 0.01; ***, P ≤ 0.001).
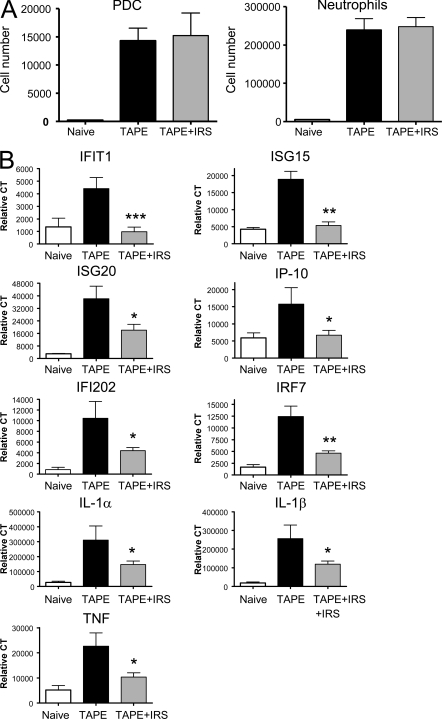
To test whether the two nucleic acid–specific TLRs, TLR7 and TLR9, were involved in the induction of these inflammatory genes signatures, we treated tape-stripped mice with IRS 954, a bifunctional oligonucleotide antagonist which blocks activation by TLR7 or TLR9 agonists in vitro (Barrat et al., 2005) and in vivo (Barrat et al., 2007). Treatment with IRS 954 significantly reduced the expression of both IFN-α–regulated genes and proinflammatory genes, in some cases reducing expression to the levels found in untreated mouse skin (Fig. 3 B and Fig. S3). Thus, signaling through TLR7 and/or TLR9 is central to the principal gene expression changes induced by tape stripping. In contrast, IRS 954 treatment had no measurable effect on the infiltration of cells, including PDCs and neutrophils (Fig. 3 B and Fig. S2), into the site of injury. This shows clearly that cell migration and cytokine secretion, although they appear coordinately regulated, are induced by different stimuli arising from tissue injury. We then further tested the role of each of these two receptors in the inflammatory response by measuring the response to tape stripping in the individual receptor-deficient animals. We observed partial reduction of the levels of gene expression in the skin after injury in either TLR7 (Fig. S4 A)- or TLR9 (Fig. S4 B)-deficient mice. However, none of the genes were exclusively dependent on only one of these two receptors. As expected, the addition of the bifunctional TLR7/9 inhibitor IRS 954 completed the inhibition in the TLR9-deficient animals (Fig. S4 B).
Figure 3.
Stimulation of TLR7 and TLR9 is required for the induction of skin inflammation but not for the cellular infiltration after skin injury. 129 mice were left untreated (naive; white bars), tape stripped (TAPE; black bars), or tape stripped immediately after treatment (s.c.) with 100 µg of the dual TLR7 and TLR9 inhibitor IRS 954. (A) 24 h later, skin-infiltrating cells were isolated, and PDCs and neutrophils were identified as in Fig. 1 A. Histograms show total cell number obtained from 2 × 2–cm skin biopsies (n = 10 mice) from two independent experiments (mean ± SEM). (B) Gene expression levels were evaluated by TaqMan. Cumulative data from at least two independent experiments (n = 10–15 mice) are shown (mean ± SEM; *, P ≤ 0.05; **, P ≤ 0.01; ***, P ≤ 0.001).
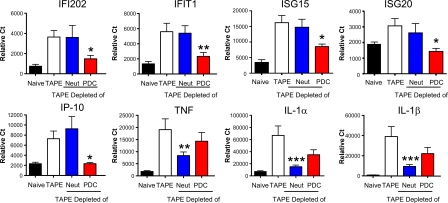
PDCs and neutrophils are responsible for different patterns of cytokine induction in response to tape stripping
To determine the relative contribution of each of these two prominent cell types in this model of skin inflammation, we specifically depleted each cell type before tape stripping. Depletion of PDCs with the 120G8 monoclonal antibody led to strong reduction of the type I IFN–regulated genes (IFI202, IFIT, ISG15, ISG20, and IP-10) in infiltrating cells (Fig. S5) and skin biopsies (Fig. 4), whereas these genes were relatively unaffected by depletion of neutrophils (Fig. 4 and Fig. S5). In contrast, neutrophil depletion resulted in a 70–90% reduction in TNF, IL-1α, and IL-1β mRNA, whereas depletion of PDCs led to a more modest 20–50% reduction in the expression of these genes. Concurrent depletion of both cell types, as expected, resulted in large reductions in the expression of both groups of genes (unpublished data). Collectively, these results suggest that in this acute skin injury model, PDCs and neutrophils are major components of the TLR7-, TLR9-, and MyD88-dependent inflammation but promote two separate inflammatory responses, one regulated by the type I IFNs produced by PDCs and one that involves neutrophil-dependent proinflammatory cytokines.
Figure 4.
The activation of both PDCs and neutrophils is critical for the burst of inflammatory genes after tape-stripping injury. 129 mice were either left untreated or tape stripped. PDCs and/or neutrophils were depleted before tape stripping using specific antibodies (250 µg given i.p. at day −2, day 0, and 8 h before tape stripping). Anti-120G8 antibody was used for depletion of PDCs and anti-GR1–Ly-6G antibody for depletion of neutrophils (Neut). Over 95% cellular depletion was achieved in both blood stream and skin infiltrate. 24 h after tape stripping, gene expression levels were measured in skin biopsies. Naive groups are shown for untreated mice only. Cumulative data from three independent experiments (n = 14 mice) are shown (mean ± SEM; *, P ≤ 0.05; **, P ≤ 0.01; ***, P ≤ 0.001).
Lupus-prone (NZBxNZW)F1 mice develop chronic skin lesions resembling human CLE after tape stripping
Patients with SLE or CLE are often much more sensitive to mild cutaneous irritation and injury, suggesting that injury initiates a process that is exacerbated and sustained by autoimmune processes. Hybrid (NZBxNZW)F1 mice spontaneously develop high levels of circulating anti-DNA and RNA autoantibodies (for review see Furukawa and Yoshimasu, 2005), leading to IC formation and lupus nephritis resembling that observed in SLE patients. Although these mice rarely show spontaneous development of skin lesions, there is an accumulation of ICs at the epidermis–dermis junction, similar to those observed in human CLE (for reviews see McCauliffe, 1996; Furukawa and Yoshimasu, 2005). As ICs containing endogenous RNA or DNA are potent ligands for TLR7 and TLR9, respectively (Barrat et al., 2005; Means et al., 2005), we postulated that (NZBxNZW)F1 mice could exhibit a prolonged or exacerbated response to tape stripping.
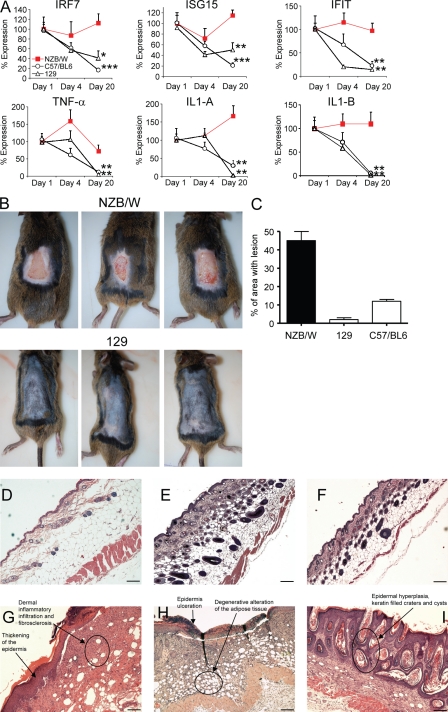
The initial response to tape stripping in (NZBxNZW)F1 mice was very similar to that in normal mice, with involved skin showing a consistent increase in the number of PDCs and neutrophils (Fig. S6, A–C). The abundant cellular infiltrate was accompanied by increased expression of IFN-regulated and proinflammatory genes. A single injection of IRS 954 before tape stripping efficiently inhibited this gene induction, which is consistent with a role of TLR7 and TLR9 in driving the acute response in this strain as well (Fig. S6 D). However, in contrast to the transient course of inflammation in normal mice, the inflammatory response in (NZBxNZW)F1 mice was sustained for many days; mRNA for both IFN-regulated genes and proinflammatory cytokines remained significantly elevated up to 3 wk after tape stripping (Fig. 5 A). This suggests that either these mice fail to properly resolve the inflammation or conditions exist to perpetuate the inflammatory signals once initiated by the injury of tape stripping. 3 wk after tape stripping, skin lesions of (NZBxNZW)F1 mice extended over 50% of tape stripped area, whereas in normal mice, lesions were healed (Fig. 5, B and C). At very early time points, 1 and 4 d after tape stripping, (NZBxNZW)F1 mice had severe multifocal thinning of the epidermis with epidermal necrosis and diffuse dermoepidermal leukocytic infiltrates composed largely of neutrophils and macrophages (unpublished data). By about 3 wk after the initial tape stripping, (NZBxNZW)F1 mice showed prominent epidermal hyperplasia with hyperkeratosis, keratin-filled craters or cysts, dermal fibrosclerosis, and degenerative changes of the s.c. fat tissue (Fig. 5, G–I and Fig. S7). In man, epidermal changes and vacuolar degeneration of the dermoepidermal junction are characteristic of all the forms of CLE, whereas other features of this model such as the presence of keratin-filled cysts and the degeneration of s.c. fat are more prominent in discoid CLE and verrucous discoid CLE (for review see Baltaci and Fritsch, 2009). Cutaneous lesions in (NZBxNZW)F1 mice showed persistent leukocytes infiltration, composed mainly of neutrophils, macrophages, and T cells, involving the epidermis, dermis, and adnexa as well as the s.c. fat (Fig. 5, G–I and Fig. S7). In the nonautoimmune mouse strains, 129 and C57BL/6, although a transient inflammation was observed involving the dermis (early time points 1 and 4 d; not depicted), it resolved spontaneously without producing sclerotic lesions, and at the same time points, infiltrating leukocytes were scarce and similar in number to untreated control skin (Fig. 5, E and F). A systematic review of the histopathological changes, based on the semiquantitative evaluation of multiple disease parameters including epidermis thickness, degree of ulceration, degree of intraepithelial, and dermal and panniculus inflammation, is shown in Table I. Overall disease score in lesions was significantly higher in (NZBxNZW)F1 mice compared with normal mice.
Figure 5.
Lupus-prone (NZBxNZW)F1 mice develop a severe and chronic skin disease resembling human CLE after tape stripping. (A) Lupus-prone mice (NZBxNZW)F1 and age-matched 129 and C57BL/6 mice were tape stripped, skin biopsies were collected 24 h, 4 d, and 20 d later, and gene expression was evaluated. The levels of expression at 24 h were set as 100 and compared with levels obtained at 4 d and 20 d after tape stripping. Cumulative data from three independent experiments are shown (n = 10; mean ± SEM; *, P ≤ 0.05; **, P ≤ 0.01; ***, P ≤ 0.001). (B) Macroscopic lesions in (NZBxNZW)F1 at 15–23 d after tape stripping as compared with normal 129 mice. (C) Quantification of area with open lesions 15–23 d after tape stripping in (NZBxNZW)F1, 129, and C57BL/6 mice. Cumulative data from at least two independent experiments (n = 15; mean ± SEM) are shown. (D–I) Representative sections of skin from untouched (NZBxNZW)F1 mice (D) or from the skin of 129 (E), C57BL/6 (F), or (NZBxNZW)F1 mice (G–I) 15–23 d after tape stripping. (D–I) Representative sections from >20 mice are shown. Bars, 200 µm.
Table I.
Pathologic evaluation of skin lesions after tape stripping
| Treatment groups | Epidermis thickness | Ulceration | Intraepithelial inflammation | Dermal inflammation | Panniculum inflammation | Total disease score |
| (NZBxNZW)F1 mice | 2.9 ± 1.7 | 1.6 ± 0.2 | 1.0 ± 0.16 | 2.3 ± 0.14 | 1.7 ± 0.12 | 8.4 ± 0.6 |
| C57BL/6 mice | 0.4 ± 0.3a | 0.4 ± 0.4b | 0.4 ± 0.4b | 0.8 ± 0.2a | 1.4 ± 0.3b | 3.4 ± 0.8a |
| 129 mice | 1.0 ± 0.2a | 0.0 ± 0.0a | 0.0 ± 0.0a | 1.6 ± 0.2a | 1.2 ± 0.2a | 3.1 ± 0.4a |
| (NZBxNZW)F1 + IRS 954 (pre-injury) | 0.7 ± 0.2a | 0.0 ± 0.0a | 0.2 ± 0.2b | 1.3±0.2a | 0.8 ± 0.1a | 3.2 ± 0.5a |
| (NZBxNZW)F1 + IRS 954 (therapeutic) | 1.0 ± 0.2a | 0.2 ± 0.1a | 0.2 ± 0.2a | 1.2 ± 0.1a | 1.0 ± 0.0a | 3.5 ± 0.4a |
| (NZBxNZW)F1 depleted of PDCs | 1.4 ± 0.3b | 0.1 ± 0.1a | 0.1 ± 0.1b | 1.4 ± 0.2a | 1.0 ± 0.2a | 4.0 ± 0.5a |
15–23 d after tape stripping, each of the histological features was scored singularly and graded 1 to 3 as indicated in Materials and methods; the overall disease score was calculated by combining the scores for each parameter. Data are from three to four different independent experiments (n = 12–30; mean ± SEM).
P < 0.001 as compared with the (NZBxNZW)F1 group.
P < 0.05 as compared with the (NZBxNZW)F1 group.
PDCs and signaling through TLR7 and TLR9 are required for the initiation and maintenance of cutaneous lesions in (NZBxNZW)F1 mice
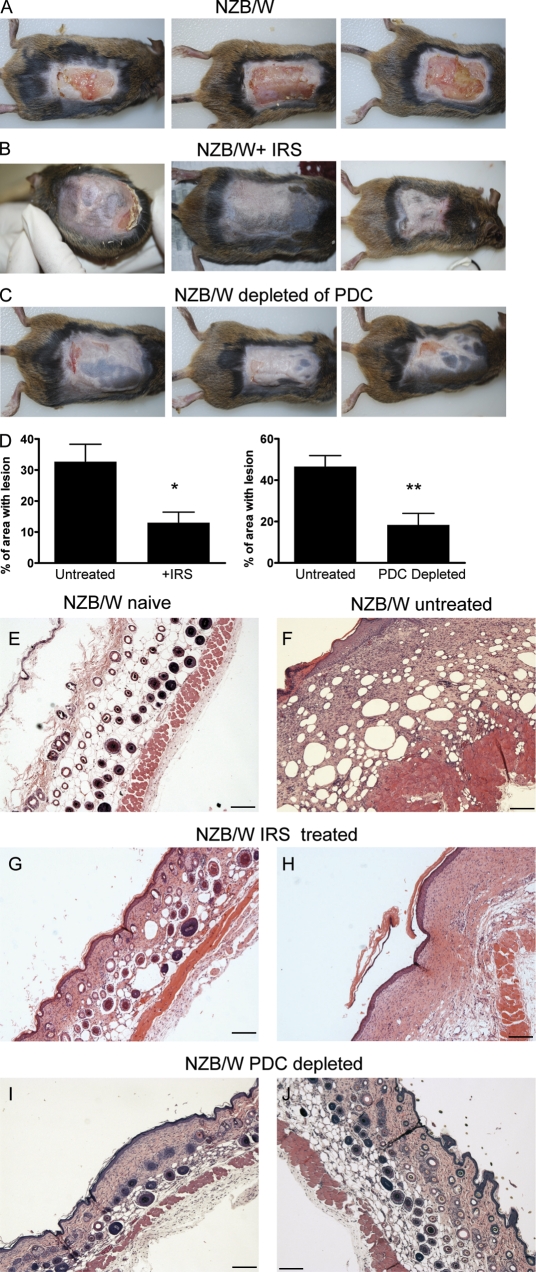
To demonstrate that PDCs and recognition of nucleic acids by TLR7 and TLR9 are central to the tape-stripping response in (NZBxNZW)F1 mice, animals were treated with IRS 954 before skin injury and for the duration of the experiment, according to the schedule in Fig. S8. In contrast to untreated mice (Fig. 6, A, D, and F), IRS 954–treated mice healed completely or had small lesions (<15% of the stripped area; Fig. 6, B and D). Skin from IRS 954–treated mice showed a very mild hyperplasia of the epithelium with slight hyperkeratosis and absence of ulceration. The inflammatory infiltrate and fibrotic reaction of the dermis appeared greatly reduced if compared with untreated animals, and no cellular infiltration was present in the epidermis (Fig. 6, G and H). Depletion of PDCs starting before tape stripping (Fig. S8) produced a very similar inhibition of the response to tape stripping. PDC-depleted mice had a normal appearance (Fig. 6, C and D) with normal to slight hyperplasic epithelium, negligible alterations of the dermis, epidermis, and adnexa, and minimal presence of inflammatory infiltration of the dermis (Fig. 6, I and J). Histological disease score confirmed these results and showed a significant difference between untreated mice and mice treated with IRS 954 or depleted of PDCs (Table I). These results suggest that PDCs are key cells in the response to cutaneous injury through their ability to sense DNA and RNA through the two nucleic acid–specific TLRs expressed by PDCs.
Figure 6.
PDCs and TLR7 and TLR9 signaling are required for cutaneous disease formation in lupus-prone mice. (A–C) Macroscopical skin lesions 15–23 d after tape stripping in (NZBxNZW)F1 mice (A), (NZBxNZW)F1 treated with weekly injection of IRS 954 (B), and (NZBxNZW)F1 mice in which PDCs were depleted during the course of the experiment (C; see Fig. S8). (D) Quantification of area with open lesions 15–23 d after tape stripping in mice as in A–C. Cumulative data from at least two independent experiments (n = 12; mean ± SEM; *, P ≤ 0.05; **, P ≤ 0.01) are shown. (E–J) Representative sections of skin from untouched (NZBxNZW)F1 mice (naive; E) or from skin isolated 15–23 d after tape stripping from (NZBxNZW)F1 mice left untreated (F) or treated with IRS 954 (G and H) or depleted of PDCs (I and J). Representative sections from ∼15 mice are shown. Bars, 200 µm.
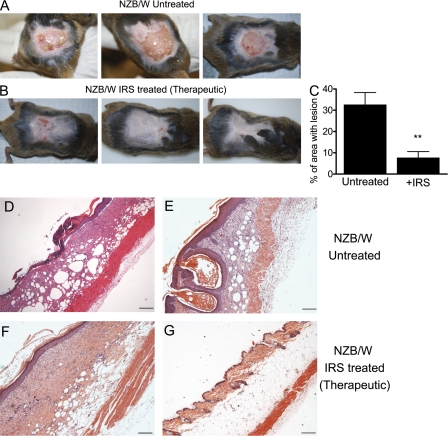
To evaluate whether TLR7 and TLR9 signaling continues to be required for the prolonged response in (NZBxNZW)F1 mice or is primarily involved in the initiation of the response, we delayed the first IRS 954 treatment until 4 d after the tape stripping, at a time when the lesions were fully developed. Strikingly, the cutaneous lesions of mice treated with IRS 954 beginning at day 4 were almost completely healed by day 15–23 with only 10% of the surface still covered by open lesions (Fig. 7, B and C). In contrast, untreated animals had substantial unhealed lesions (Fig. 7, A and C–E) at these time points. Skin specimens from IRS 954–treated mice presented moderate alterations with very modest dermal inflammatory infiltration and fibrosclerosis and negligible involvement of the adipose tissue (Fig. 7, F and G; and Table I). In summary, these findings demonstrate that the chronic activation of TLR7 and/or TLR9 in PDCs is required both to initiate and maintain the inflammation in the skin of (NZBxNZW)F1 mice. It also suggests that blocking this process with a specific TLR7/9 inhibitor such as IRS 954 is effective in a therapeutic setting, acting to resolve ongoing skin inflammation.
Figure 7.
Therapeutic treatment of lupus-prone mice with chronic skin inflammation using IRS 954 significantly ameliorates CLE-like phenotype. (A and B) Gross appearance of skin lesions isolated 15–23 d after tape stripping from (NZBxNZW)F1 mice left untreated or (NZBxNZW)F1 mice treated from day 4–20 with IRS 954 in a therapeutic setting (scheme of treatment in Fig. S8). (C) Quantification of area with open lesions 15–23 d after tape stripping in mice as in A and B. Cumulative data from two independent experiments (n = 12; mean ± SEM; **, P ≤ 0.01) are shown. (D–G) Representative sections of skin from (NZBxNZW)F1 mice either left untreated (D and E) or treated from day 4 with IRS 954 (F and G). Data show representative sections of ∼12 mice. Bars, 200 µm.
DISCUSSION
CLE belongs to a group of diseases named interface dermatitis (for review see Wenzel and Tüting, 2008) that shares a pattern of epidermal changes characterized by large areas of liquefaction at the derma–epidermal junction. The specific causes of these diseases are unknown, although the infiltration of IFN-α–producing PDCs in the area of vacuolization has been suggested to play a role in either initiating the disease and/or maintaining its chronicity (Farkas et al., 2001; for reviews see Wenzel and Tüting, 2007, 2008). The pathogenic effect of IFN-α in the skin could be explained in part by the induction of IFN-regulated cytokines such as IP-10, which induce the infiltration of pathogenic CXCR3+ T cells (for review see Wenzel and Tüting, 2008). In addition, IFN-α has been shown to boost cytotoxic activity of T cells and to activate neutrophils to produce reactive oxygen intermediates, which mediate end-organ damage (Martinelli et al., 2004). Neutrophils that accumulate abundantly in the early phase of CLE lesions (for review see Lipsker and Saurat, 2008) also express both TLR7 and TLR9. Ligation of Fc-γ receptors by ICs activates these cells to produce proinflammatory cytokines, reactive oxygen intermediates, and proteases (Coxon et al., 2001; Hayashi et al., 2003; Tsuboi et al., 2008), thus playing an important role in the liquefaction process typical of CLE (Hayashi et al., 2003; for reviews see Lipsker and Saurat, 2008; Baltaci and Fritsch, 2009). Both type I IFNs and proinflammatory cytokines such as TNF, IL-1α, and IL-1β are abundantly expressed in CLE and can promote the migration of inflammatory cells to the skin (Popovic et al., 2005; for review see Werth, 2007).
Studies of the pathogenic mechanisms of CLE and development of new therapies for CLE have been hampered by the absence of animal models of interface dermatitis that replicate key features and pathways of the human disease (for review see Wenzel and Tüting, 2008). In this study, we report that skin injury caused by tape striping in normal mice is followed by an acute inflammatory response accompanied by conspicuous infiltration of innate immune cells, including PDCs and neutrophils, paralleled with induction of type I IFN–regulated genes and proinflammatory cytokines. This increased expression of cytokine genes is completely abrogated in MyD88-deficient mice and in mice treated with a specific inhibitor of TLR7 and TLR9, indicating a central role for stimulation by RNA and/or DNA. Among the leukocytes that infiltrate the lesional skin, both PDCs and neutrophils express TLR7 and TLR9 receptors (Kadowaki et al., 2001; Edwards et al., 2003; Hayashi et al., 2003). The magnitude and composition of the cellular infiltrate are not significantly altered by TLR7 and TLR9 inhibition, suggesting that these pathways are not required for extravasation and homing. Using specific depleting antibodies, we demonstrate that PDCs, not neutrophils, are the source of type I IFN response, whereas proinflammatory cytokines IL-1α, IL-1β, and TNF are profoundly inhibited by neutrophil depletion. The reduction in cytokine gene expression in skin depleted of PDCs or neutrophils is similar in RNA samples extracted from infiltrating leukocytes or from whole skin biopsies, suggesting that keratinocytes or endothelial cells are not major contributors to this gene expression pattern. The finding that both IRS 954 and neutrophil depletion inhibit proinflammatory cytokines to a similar extent suggests that neutrophils do respond directly through one or both of these receptors. Alternatively, the inhibition of TLR7 and TLR9 may prevent induction of a factor made by another cell type (not PDCs) that activates neutrophils. The absence of TLR9 exacerbated disease in MRL/lpr lupus-prone mice, suggesting that TLR9 itself has a protective role in developing autoimmune inflammatory disorders (Christensen et al., 2006; Nickerson et al., 2010). However, we did not observe any exacerbation of skin inflammation in the TLR9-deficient animals.
The most likely ligands for TLR7 and TLR9 in injured skin are endogenous nucleic acids released from keratinocytes and other cell types dying as a consequence of mechanical injury or neutrophil cytotoxicity. Another potential source would be DNA specifically extruded from neutrophils in the form of NETs. This is not likely the major source of the initial TLR stimulation, as neutrophil depletion before injury does not significantly reduce the activation of PDCs (Fig. 4 and Fig. S5); however, this may be a relevant source in the chronic activation observed in autoimmune mice. Tissue injury in a largely sterile environment has been shown to stimulate a similar nucleic acid–dependent inflammatory response. Indeed, DNA release from necrotic hepatocytes stimulates cytokine production by neutrophils in a TLR9-dependent manner, and this has been suggested to be a primary mechanism of liver damage after some forms of hepatic injury (Imaeda et al., 2009; Bamboat et al., 2010).
In 129 or C57BL/6 mice, the burst of mRNA encoding inflammatory cytokines is transient, and gene expression levels return to pretreatment levels within 10 d of tape stripping. This is paralleled by reduction in cellular infiltration and progressive wound healing (unpublished data). Thus, this model represents an acute activation of pathways that are activated chronically in lupus, CLE, and related diseases. In contrast, tape stripping of lupus-prone (NZBxNZW)F1 mice produces a lesion quite similar to that in nonautoimmune strains, but instead of healing spontaneously, it evolves into lesions that resemble the human CLE situation both clinically and histologically. The inflammation is mediated by TLR7 and TLR9 as the treatment of (NZBxNZW)F1 mice with the specific TLR7/9 inhibitor IRS 954 is able to prevent disease onset as shown by gross appearance of the skin, histological examination, and the normalization of the gene signatures. TLR7 and TLR9 activation is required not only for the induction of the inflammatory response but also for continuation of the chronic response seen in lupus-prone mice. This is shown clearly by the fact that IRS 954 treatment initiated after the development of the initial cellular infiltrate and cutaneous lesions leads to accelerated healing. This finding identifies TLR7 and TLR9 as important potential targets for therapy in CLE and related cutaneous autoimmune diseases.
Although the initial source of TLR ligands may be similar in normal and autoimmune mice, an important difference may be the continued presence of ligands for TLR7 and TLR9 in (NZBxNZW)F1 mice, specifically the ICs that accumulate at the dermis–epidermis junction (for reviews see McCauliffe, 1996; Furukawa and Yoshimasu, 2005) and the presence of circulating anti-DNA and RNA autoantibodies in these mice (for review see Furukawa and Yoshimasu, 2005). A similar phenomenon might take place in human CLE, where anti-DNA and RNA ICs in circulation and deposited in skin tissue have been extensively described (for reviews see McCauliffe, 1996; Wenzel and Tüting, 2008). Another source of DNA and RNA for this continued stimulation might be the neutrophils themselves. Skin neutrophils are highly activated after tape stripping and produce abundant NET fibers containing DNA and RNA molecules. NET-producing neutrophils were found in normal mice only at early time points, before the inflammatory response is resolved. However, in (NZBxNZW)F1 mice, significant infiltration of NET-producing neutrophils is detectable at later time points in well-established lesions (unpublished data), suggesting that they may constitute a source of endogenous nucleic acid leading to chronic TLR signaling. Interestingly, we found that the antimicrobial peptide LL37/CRAMP was associated with the fibers of the NETs from skin neutrophils. LL37/CRAMP is a cationic antimicrobial peptide highly inducible in keratinocytes and has been shown to convert endogenous DNA and RNA into a potent TLR9 or TLR7 agonists by promoting aggregation and enhanced uptake by PDCs in vitro (Lande et al., 2007; Ganguly et al., 2009). In addition to self-DNA/RNA, it is possible that microbial nucleic acids can participate in this process either directly by activating the TLRs or indirectly by promoting the release of NETs by neutrophils. This is particularly relevant to the chronic model in which the skin is exposed for a long period of time.
The development of cutaneous lesions after injury in lupus-prone mice is similar to the Koebner phenomenon observed in patients with CLE and other autoimmune disease of the skin after skin trauma (for review see Ueki, 2005). The development of the lesions in (NZBxNZW)F1 is characterized by a persistent IFN signature and a high level of proinflammatory mediators such as IL-1α, IL-1β, and TNF similarly to the situation in human CLE (Werth et al., 2002; Clancy et al., 2004; Popovic et al., 2005; for review see Werth, 2007). The absence of spontaneous macroscopic lesions in lupus-prone mice is expected as most mouse model skin diseases require mild wounding (Spergel et al., 1999; Sano et al., 2005; Matsunaga et al., 2007).
In conclusion, we provide evidence that an abnormal response to endogenous ligands leading to chronic activation of both TLR7 and TLR9 may constitute a fundamental trigger of autoimmunity in the skin. The difference in outcome in lupus-prone versus normal mice after mild injury in the skin thus reflects the nature of the response, acute versus chronic, by PDCs and neutrophils to nucleic acids in the skin. Our data suggest that an abnormal/chronic response to TLR7 and TLR9 ligands can establish a self-perpetuating inflammatory loop driving diseases such as cutaneous lupus or other diseases with interface dermatitis. We also demonstrate that using novel oligonucleotide-based inhibitors of TLR7 and TLR9 could prove to be valuable therapeutics for skin autoimmune diseases.
MATERIALS AND METHODS
Reagents.
Phosphorothioate oligodeoxynucleotides were prepared as previously described (Duramad et al., 2003). The prototype for inhibitor of TLR7 and TLR9 used was IRS 954, 5′-TGCTCCTGGAGGGGTTGT-3′ (Barrat et al., 2005). Control oligonucleotide was 5′-TCCTGCAGGTTAAGT-3′. Mouse IFN-α ELISA sets were purchased from PBL Biomedical Laboratories.
Animals and in vivo treatments.
C57BL/6 and 129 mice were purchased from Charles River. We purchased (NZBxNZW)F1 female mice from The Jackson Laboratory and used them at 18–22 wk of age. MyD88/KO and TLR9/KO mouse colonies were maintained at Simonsen Laboratories and were used with age-matched C57BL/6 WT controls at 8–12 wk of age. Animal experiments were conducted at MuriGenics. All animal experiments were approved by the institutional animal care and use committee of MuriGenics, in conformity with the Guide for the Care and Use of Laboratory Animals (National Research Council).We performed tape stripping after shaving the dorsal area (3 × 3 cm) using 10 strokes with duct tape. IRS 954 was administered just before tape stripping s.c. at a distant site. Alternatively, in (NZBxNZW)F1 mice, IRS 954 was administered long term, as depicted in Fig. S8. In certain experiments, PDCs and neutrophils were depleted with 250 µg IRS 954 given i.p. at day −2, day 0, and 8 h before tape stripping. We used anti-120G8 (Imgenex) for depletion of PDCs (Asselin-Paturel et al., 2003) and anti–GR1-Ly-6G (clone 1A8; BioLegend) for depletion of neutrophils (Daley et al., 2008). Over 95% cellular depletion was achieved in both blood stream and skin infiltrate. In experiments in which PDCs were depleted, long-term 120G8-depleting antibody was administered as depicted in Fig. S8. Experiments in (NZBxNZW)F1 mice were terminated between 15 and 23 d after initial tape stripping, depending on the progression of the lesions in the untreated groups in each experiment. The percentage of area with open lesions in (NZBxNZW)F1 and normal mice was evaluated with NIS-elements software (Nikon).
Histological analysis of skin inflammation and tissue pathology.
The biopsy specimens were fixed in formalin and embedded in paraffin. Sections were stained with hematoxylin and eosin. Multiple skin sections of 12–30 mice per group were evaluated in a blinded fashion. The following histological features were assessed and graded from 1 to 3: (a) epidermis thickness, (b) degree of ulceration, (c) intraepithelial inflammation, (d) dermal inflammation, and (e) panniculus inflammation. Histological grading was assigned as follows: 0, normal skin architecture, few dermal leukocytes, and regular adnexa; 1, mild inflammation, slight epidermal hyperplasia, and signs of dermal fibroblast proliferation; 2, moderate inflammation, noticeable epidermal hyperplasia (two- to fourfold increase in epithelial thickness) with hyperkeratosis, significant leukocyte/neutrophil-granulocyte dermal infiltrate with few macrophages, moderate fibrosclerosis of the dermis, reduction in the number of adnexa, and slight degenerative changes of the hypodermic adipose tissue; and 3, severe inflammation, marked epidermal hyperplasia (more than fourfold increase in epithelial thickness) with hyperkeratosis, formation of keratin-filled craters and cysts, diffuse discontinuity of the epidermal layer (ulceration), extensive dermal infiltrate with abundant neutrophils and macrophages, pronounced dermal fibrosclerosis, vanishing of adnexa, and evident degenerative changes of the hypodermic adipose tissue. The different parameters were scored separately and summed to obtain a total disease score (Table I). Statistical significance among groups was calculated with a Mann-Whitney U test.
Skin sample processing and flow cytometry.
For analysis of cellular infiltrate, mice were killed 24 h later, and epidermis and dermis were mechanically separated, followed by enzymatic digestion with 0.28 U/ml Liberase 3 (Roche) for 20 min at 37°C, passed trough a 70-µm filter washed in RPMI without serum, and counted. The cellular infiltrate was subsequently used for preparation of RNA for TaqMan assay and/or stained for flow cytometric analyses. We performed flow cytometric analyses using fluorochrome-conjugated monoclonal antibodies to mouse CD3, CD8, CD4, B220, CD11c (BD), GR1–Ly-6G (1A8 clone), F4/80 (BioLegend), PDCA1 (Miltenyi Biotech), and 120G8 (Imgenex). Specific gating to characterize skin infiltrate was performed as follows: PDCs were CD11c+, PDCA1+; 120G8+, Ly-6C+, myeloid DCs were CD11c+ PDCA1− 120G8− Ly-6C−, T cells were CD3+ CD4+; CD3+CD8+, neutrophils were GR1–Ly-6G high F4/80−, and macrophages were GR1–Ly-6G low F480+. In the experiments in which IFN-α production by PDCs was evaluated by FACS analysis, skin was processed as described for the analysis of the cellular infiltrate but in the presence of 5 µg/ml brefeldin A. Cellular infiltrate was seeded in noncoated plastic plates at a concentration of 106/ml in RPMI medium (supplemented with 10% FCS) with the addition of 5 µg/ml brefeldin A for 2 h. Afterward, cells were stained for surface markers with anti-CD11c plus anti-PDCA1–conjugated antibodies to identify PDCs. Cells were then fixed in 2% paraformaldehyde and permeabilized for 10 min in 0.5% saponin and 1% BSA in PBS and then stained in the same buffer with 5 µg/ml anti–IFN-α–conjugated antibody (PBL Biomedical Laboratories). As a positive control, BM-derived PDCs were stimulated for 4 h with CpG-C ISS; 5 µg/ml brefeldin A was added in the last 2 h of stimulation. In some of the experiments, the ability of skin-infiltrating neutrophils to produce NETs was assayed as previously described (Brinkmann et al., 2004; Fuchs et al., 2007; Kessenbrock et al., 2009; for review see Wartha and Henriques-Normark, 2008). In brief, skin-infiltrating cells were seeded on coated glass (0.001% polylysine; Sigma-Aldrich) at a concentration of 106/ml for 10 min at 37°C in RPMI and 2% FCS. Afterward, cells were stained with anti–Ly-6G–conjugated antibody for 10 min on ice and immediately fixed in 2% paraformaldehyde and counterstained for DNA with SYTOX green (1:5000; Invitrogen; Fuchs et al., 2007). In some experiments, after fixation, neutrophils were further stained with 5 µg/ml anti-LL37/CRAMP antibody (Innovagen) and then counterstained for DNA with SYTOX green (1:5000) or with a specific RNA dye SYTO RNA Select (1:5000; Invitrogen).
Real-time quantitative PCR (TaqMan) analysis.
PCR reactions were performed as described previously (Barrat et al., 2005). In brief, RNA was extracted from skin-infiltrating cells as described for the analysis of the cellular infiltrate (see previous section) using an RNA micro kit (QIAGEN) and from skin tissues with a fibrous tissue RNA extraction kit (QIAGEN) according to the manufacturer’s instructions. RNA and cDNA were generated with SuperScript First-Strand Synthesis System (Invitrogen). RCT threshold cycle (CT) values for each gene were normalized to the housekeeping gene ubiquitin using the formula gene expression = 1.8(Avg CT Ubi − CT Gene) × 100,000, where Ubi is the mean CT of triplicate housekeeping gene runs, Gene is the mean CT of duplicate runs of the gene of interest, and 100,000 is arbitrarily chosen as a factor to bring all values above 1. Primers sequences used were as follows: IFI202R, 5′-CTAGGATGCCACTGCTGTTG-3′; IFI202F, 5′-CAAGCCTCTCCTGGACCTAA-3′; IRF7R, 5′-TCCAAGCTCCCGGCTAAGT-3′; IRF7F, 5′-ACAGGGCGTTTTATCTTGCG-3′; ISG15R, 5′-CCCCTTTCGTTCCTCACCAG-3′; ISG15F, 5′-ACGGTCTTACCCTTTCCAGTC-3′; ISG20R, 5′-CCACCAGCTTGCCTTTCAGAA-3′; ISG20F, 5′-GTCACGCCTCAGCACATGGT-3′; NMIR, 5′-AATGCCTTCTAATCCGGTCA-3′; NMIF, 5′-AGTGGAAAGCGTGGATTATGA-3′; IFIT1R, 5′-TCTGGATTTAACCGGACAGC-3′; IFIT1F, 5′-AGGCTGGAGTGTGCTGAGAT-3′; IL-1AR, 5′-CCGACAGCACGAGGCTTT-3′; IL-1AF, 5′-TGGTGTGTGACGTTCCCATT-3′; TNF-AR, 5′-GGTCTGGGCCATAGAACTGATG-3′; TNF-AF, 5′-GCCACCACGCTCTTCTGTCT-3′; IL-1BR, 5′-AAACCGTTTTTCCATCTTCTTCTTT-3′; IL-1BF, 5′-GACGGCACACCCACCCT-3′; IP-10F, 5′-GACGGTCCGCTGCAACTG-3′; and IP-10R, 5′-GCTTCCCTATGGCCCTCATT-3′.
Statistical analysis.
Data were analyzed using a two-tailed Student’s t test. All analyses were performed using Prism software (GraphPad Software, Inc.). Differences were considered significant at a P-value of <0.05.
Online supplemental material.
Fig. S1 shows that the up-regulation of type I IFN–regulated genes in skin-infiltrating cells in normal mice is IFNAR dependent. Fig. S2 shows that TLR7 and TLR9 inhibition does not affect the ability of leukocytes to infiltrate the injured skin. Fig. S3 shows that stimulation of TLR7 and TLR9 is necessary for the up-regulation of type I IFN–regulated genes and inflammatory genes as measured in RNA samples from skin biopsies. Fig. S4 shows that the up-regulation of type I IFN–regulated genes and inflammatory genes is dependent on both TLR7 and TLR9 receptors. Fig. S5 shows that the activation of both PDCs and neutrophils is critical for the burst of inflammatory genes after tape-stripping injury. Fig. S6 shows that in lupus-prone mice, (NZBxNZW)F1, tape stripping is followed by up-regulation of type I IFN–regulated genes and inflammatory genes in a TLR7- and TLR9-dependent way. Fig. S7 shows histopathological details in lesions of (NZBxNZW)F1 at high magnification. Fig. S8 depicts the treatment protocols in (NZBxNZW)F1 with the TLR7 and TLR9 inhibitor IRS 954 and in the PDC-depleting experiments. Online supplemental material is available at http://www.jem.org/cgi/content/full/jem.20101048/DC1.
Acknowledgments
We would like to thank our colleagues at Dynavax Technologies Corporation for their critical reading of the manuscript. We also thank Steve Noonan and Henry Lopez (MuriGenics) for invaluable assistance with animal work.
This work was in part funded by National Institutes of Health Small Business Innovation Research grant 5R43A182839-2 (to F.J. Barrat). M.P. Colombo’s work was supported by grants from the Associazione Italiana Ricerca sul Cancro, Italian Ministry of Health, and Fondazione Cariplo.
C. Guiducci, M. Gong, R.L. Coffman, and F.J. Barrat are full-time employees of Dynavax Technologies Corporation; otherwise, the authors have no conflicting financial interest.
Footnotes
Abbreviations used:
- CLE
- cutaneous lupus erythematosus
- IC
- immunocomplex
- mRNA
- messenger RNA
- NET
- neutrophil extracellular trap
- PDC
- plasmacytoid DC
- SLE
- systemic lupus erythematosus
- TLR
- Toll-like receptor
References
- Asefa B., Klarmann K.D., Copeland N.G., Gilbert D.J., Jenkins N.A., Keller J.R. 2004. The interferon-inducible p200 family of proteins: a perspective on their roles in cell cycle regulation and differentiation. Blood Cells Mol. Dis. 32:155–167 10.1016/j.bcmd.2003.10.002 [DOI] [PubMed] [Google Scholar]
- Asselin-Paturel C., Brizard G., Pin J.J., Brière F., Trinchieri G. 2003. Mouse strain differences in plasmacytoid dendritic cell frequency and function revealed by a novel monoclonal antibody. J. Immunol. 171:6466–6477 [DOI] [PubMed] [Google Scholar]
- Baltaci M., Fritsch P. 2009. Histologic features of cutaneous lupus erythematosus. Autoimmun. Rev. 8:467–473 10.1016/j.autrev.2008.12.014 [DOI] [PubMed] [Google Scholar]
- Bamboat Z.M., Balachandran V.P., Ocuin L.M., Obaid H., Plitas G., DeMatteo R.P. 2010. Toll-like receptor 9 inhibition confers protection from liver ischemia-reperfusion injury. Hepatology. 51:621–632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banchereau J., Pascual V., Palucka A.K. 2004. Autoimmunity through cytokine-induced dendritic cell activation. Immunity. 20:539–550 [DOI] [PubMed] [Google Scholar]
- Barrat F.J., Coffman R.L. 2008. Development of TLR inhibitors for the treatment of autoimmune diseases. Immunol. Rev. 223:271–283 [DOI] [PubMed] [Google Scholar]
- Barrat F.J., Meeker T., Gregorio J., Chan J.H., Uematsu S., Akira S., Chang B., Duramad O., Coffman R.L. 2005. Nucleic acids of mammalian origin can act as endogenous ligands for Toll-like receptors and may promote systemic lupus erythematosus. J. Exp. Med. 202:1131–1139 10.1084/jem.20050914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrat F.J., Meeker T., Chan J.H., Guiducci C., Coffman R.L. 2007. Treatment of lupus-prone mice with a dual inhibitor of TLR7 and TLR9 leads to reduction of autoantibody production and amelioration of disease symptoms. Eur. J. Immunol. 37:3582–3586 10.1002/eji.200737815 [DOI] [PubMed] [Google Scholar]
- Blomberg S., Eloranta M.L., Cederblad B., Nordlin K., Alm G.V., Rönnblom L. 2001. Presence of cutaneous interferon-alpha producing cells in patients with systemic lupus erythematosus. Lupus. 10:484–490 10.1191/096120301678416042 [DOI] [PubMed] [Google Scholar]
- Brinkmann V., Reichard U., Goosmann C., Fauler B., Uhlemann Y., Weiss D.S., Weinrauch Y., Zychlinsky A. 2004. Neutrophil extracellular traps kill bacteria. Science. 303:1532–1535 [DOI] [PubMed] [Google Scholar]
- Choubey D., Panchanathan R. 2008. Interferon-inducible Ifi200-family genes in systemic lupus erythematosus. Immunol. Lett. 119:32–41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christensen S.R., Shupe J., Nickerson K., Kashgarian M., Flavell R.A., Shlomchik M.J. 2006. Toll-like receptor 7 and TLR9 dictate autoantibody specificity and have opposing inflammatory and regulatory roles in a murine model of lupus. Immunity. 25:417–428 10.1016/j.immuni.2006.07.013 [DOI] [PubMed] [Google Scholar]
- Clancy R.M., Backer C.B., Yin X., Chang M.W., Cohen S.R., Lee L.A., Buyon J.P. 2004. Genetic association of cutaneous neonatal lupus with HLA class II and tumor necrosis factor alpha: implications for pathogenesis. Arthritis Rheum. 50:2598–2603 10.1002/art.20442 [DOI] [PubMed] [Google Scholar]
- Coxon A., Cullere X., Knight S., Sethi S., Wakelin M.W., Stavrakis G., Luscinskas F.W., Mayadas T.N. 2001. Fc gamma RIII mediates neutrophil recruitment to immune complexes. a mechanism for neutrophil accumulation in immune-mediated inflammation. Immunity. 14:693–704 10.1016/S1074-7613(01)00150-9 [DOI] [PubMed] [Google Scholar]
- Daley J.M., Thomay A.A., Connolly M.D., Reichner J.S., Albina J.E. 2008. Use of Ly6G-specific monoclonal antibody to deplete neutrophils in mice. J. Leukoc. Biol. 83:64–70 [DOI] [PubMed] [Google Scholar]
- Duramad O., Fearon K.L., Chan J.H., Kanzler H., Marshall J.D., Coffman R.L., Barrat F.J. 2003. IL-10 regulates plasmacytoid dendritic cell response to CpG-containing immunostimulatory sequences. Blood. 102:4487–4492 [DOI] [PubMed] [Google Scholar]
- Edwards A.D., Diebold S.S., Slack E.M., Tomizawa H., Hemmi H., Kaisho T., Akira S., Reis e Sousa C. 2003. Toll-like receptor expression in murine DC subsets: lack of TLR7 expression by CD8 alpha+ DC correlates with unresponsiveness to imidazoquinolines. Eur. J. Immunol. 33:827–833 10.1002/eji.200323797 [DOI] [PubMed] [Google Scholar]
- Farkas L., Beiske K., Lund-Johansen F., Brandtzaeg P., Jahnsen F.L. 2001. Plasmacytoid dendritic cells (natural interferon- alpha/beta-producing cells) accumulate in cutaneous lupus erythematosus lesions. Am. J. Pathol. 159:237–243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuchs T.A., Abed U., Goosmann C., Hurwitz R., Schulze I., Wahn V., Weinrauch Y., Brinkmann V., Zychlinsky A. 2007. Novel cell death program leads to neutrophil extracellular traps. J. Cell Biol. 176:231–241 10.1083/jcb.200606027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furukawa F., Yoshimasu T. 2005. Animal models of spontaneous and drug-induced cutaneous lupus erythematosus. Autoimmun. Rev. 4:345–350 [DOI] [PubMed] [Google Scholar]
- Ganguly D., Chamilos G., Lande R., Gregorio J., Meller S., Facchinetti V., Homey B., Barrat F.J., Zal T., Gilliet M. 2009. Self-RNA–antimicrobial peptide complexes activate human dendritic cells through TLR7 and TLR8. J. Exp. Med. 206:1983–1994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guiducci C., Coffman R.L., Barrat F.J. 2009. Signalling pathways leading to IFN-alpha production in human plasmacytoid dendritic cell and the possible use of agonists or antagonists of TLR7 and TLR9 in clinical indications. J. Intern. Med. 265:43–57 10.1111/j.1365-2796.2008.02050.x [DOI] [PubMed] [Google Scholar]
- Hayashi F., Means T.K., Luster A.D. 2003. Toll-like receptors stimulate human neutrophil function. Blood. 102:2660–2669 10.1182/blood-2003-04-1078 [DOI] [PubMed] [Google Scholar]
- Imaeda A.B., Watanabe A., Sohail M.A., Mahmood S., Mohamadnejad M., Sutterwala F.S., Flavell R.A., Mehal W.Z. 2009. Acetaminophen-induced hepatotoxicity in mice is dependent on Tlr9 and the Nalp3 inflammasome. J. Clin. Invest. 119:305–314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inoue J., Yotsumoto S., Sakamoto T., Tsuchiya S., Aramaki Y. 2005. Changes in immune responses to antigen applied to tape-stripped skin with CpG-oligodeoxynucleotide in mice. J. Control. Release. 108:294–305 [DOI] [PubMed] [Google Scholar]
- Jin H., Oyoshi M.K., Le Y., Bianchi T., Koduru S., Mathias C.B., Kumar L., Le Bras S., Young D., Collins M., et al. 2009. IL-21R is essential for epicutaneous sensitization and allergic skin inflammation in humans and mice. J. Clin. Invest. 119:47–60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kadowaki N., Ho S., Antonenko S., Malefyt R.W., Kastelein R.A., Bazan F., Liu Y.J. 2001. Subsets of human dendritic cell precursors express different toll-like receptors and respond to different microbial antigens. J. Exp. Med. 194:863–869 10.1084/jem.194.6.863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessenbrock K., Krumbholz M., Schönermarck U., Back W., Gross W.L., Werb Z., Gröne H.J., Brinkmann V., Jenne D.E. 2009. Netting neutrophils in autoimmune small-vessel vasculitis. Nat. Med. 15:623–625 10.1038/nm.1959 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lande R., Gregorio J., Facchinetti V., Chatterjee B., Wang Y.H., Homey B., Cao W., Wang Y.H., Su B., Nestle F.O., et al. 2007. Plasmacytoid dendritic cells sense self-DNA coupled with antimicrobial peptide. Nature. 449:564–569 10.1038/nature06116 [DOI] [PubMed] [Google Scholar]
- Lipsker D., Saurat J.H. 2008. Neutrophilic cutaneous lupus erythematosus. At the edge between innate and acquired immunity? Dermatology. 216:283–286 [DOI] [PubMed] [Google Scholar]
- Marshak-Rothstein A. 2006. Toll-like receptors in systemic autoimmune disease. Nat. Rev. Immunol. 6:823–835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinelli S., Urosevic M., Daryadel A., Oberholzer P.A., Baumann C., Fey M.F., Dummer R., Simon H.U., Yousefi S. 2004. Induction of genes mediating interferon-dependent extracellular trap formation during neutrophil differentiation. J. Biol. Chem. 279:44123–44132 10.1074/jbc.M405883200 [DOI] [PubMed] [Google Scholar]
- Matsunaga Y., Ogura Y., Ehama R., Amano S., Nishiyama T., Tagami H. 2007. Establishment of a mouse skin model of the lichenification in human chronic eczematous dermatitis. Br. J. Dermatol. 156:884–891 10.1111/j.1365-2133.2007.07770.x [DOI] [PubMed] [Google Scholar]
- McCauliffe D.P. 1996. Antibody penetration into the cells of mice and men. J. Invest. Dermatol. 107:3–4 10.1111/1523-1747.ep12293642 [DOI] [PubMed] [Google Scholar]
- Means T.K., Latz E., Hayashi F., Murali M.R., Golenbock D.T., Luster A.D. 2005. Human lupus autoantibody-DNA complexes activate DCs through cooperation of CD32 and TLR9. J. Clin. Invest. 115:407–417 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nickerson K.M., Christensen S.R., Shupe J., Kashgarian M., Kim D., Elkon K., Shlomchik M.J. 2010. TLR9 regulates TLR7- and MyD88-dependent autoantibody production and disease in a murine model of lupus. J. Immunol. 184:1840–1848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Popovic K., Ek M., Espinosa A., Padyukov L., Harris H.E., Wahren-Herlenius M., Nyberg F. 2005. Increased expression of the novel proinflammatory cytokine high mobility group box chromosomal protein 1 in skin lesions of patients with lupus erythematosus. Arthritis Rheum. 52:3639–3645 10.1002/art.21398 [DOI] [PubMed] [Google Scholar]
- Sano S., Chan K.S., Carbajal S., Clifford J., Peavey M., Kiguchi K., Itami S., Nickoloff B.J., DiGiovanni J. 2005. Stat3 links activated keratinocytes and immunocytes required for development of psoriasis in a novel transgenic mouse model. Nat. Med. 11:43–49 10.1038/nm1162 [DOI] [PubMed] [Google Scholar]
- Spergel J.M., Mizoguchi E., Oettgen H., Bhan A.K., Geha R.S. 1999. Roles of TH1 and TH2 cytokines in a murine model of allergic dermatitis. J. Clin. Invest. 103:1103–1111 10.1172/JCI5669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsuboi N., Asano K., Lauterbach M., Mayadas T.N. 2008. Human neutrophil Fcgamma receptors initiate and play specialized nonredundant roles in antibody-mediated inflammatory diseases. Immunity. 28:833–846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ueki H. 2005. Koebner phenomenon in lupus erythematosus with special consideration of clinical findings. Autoimmun. Rev. 4:219–223 [DOI] [PubMed] [Google Scholar]
- Ueno H., Klechevsky E., Morita R., Aspord C., Cao T., Matsui T., Di Pucchio T., Connolly J., Fay J.W., Pascual V., et al. 2007. Dendritic cell subsets in health and disease. Immunol. Rev. 219:118–142 10.1111/j.1600-065X.2007.00551.x [DOI] [PubMed] [Google Scholar]
- Wartha F., Henriques-Normark B. 2008. ETosis: a novel cell death pathway. Sci. Signal. 1:pe25 10.1126/stke.121pe25 [DOI] [PubMed] [Google Scholar]
- Wenzel J., Tüting T. 2007. Identification of type I interferon-associated inflammation in the pathogenesis of cutaneous lupus erythematosus opens up options for novel therapeutic approaches. Exp. Dermatol. 16:454–463 10.1111/j.1600-0625.2007.00556.x [DOI] [PubMed] [Google Scholar]
- Wenzel J., Tüting T. 2008. An IFN-associated cytotoxic cellular immune response against viral, self-, or tumor antigens is a common pathogenetic feature in “interface dermatitis”. J. Invest. Dermatol. 128:2392–2402 [DOI] [PubMed] [Google Scholar]
- Werth V.P. 2007. Cutaneous lupus: insights into pathogenesis and disease classification. Bull. NYU Hosp. Jt. Dis. 65:200–204 [PubMed] [Google Scholar]
- Werth V.P., Callen J.P., Ang G., Sullivan K.E. 2002. Associations of tumor necrosis factor alpha and HLA polymorphisms with adult dermatomyositis: implications for a unique pathogenesis. J. Invest. Dermatol. 119:617–620 10.1046/j.1523-1747.2002.01869.x [DOI] [PubMed] [Google Scholar]