Abstract
This study was conducted in Nangabo sub-county of Wakiso district. The purpose was to document the common Traditional Medicine (TM) practices; assess the local people's preferences for TM versus western medicine (WM) and lastly to determine the awareness about the importance of TM by local people. Data were collected using semi-structured administered face-to-face with respondents. A total of 120 interviewed. Six focused group discussions (FGDs) were held to validate the questionnaire responses. Data were analyzed descriptively using Statistical Package for Social Sciences (SPSS). The findings indicated that most (43%) respondents derive their livelihoods from traditional medicine practices. Three forms of TM were reported-herbalism (67%), spiritual counseling (23%) and bone setting (10%). Although the majority (81%) of respondents were quite aware of the importance of TM in the sustenance of health care system, majority (55%) of them shunned TM in preference to WM, largely because of the belief that TM is evil-founded and devilish in nature. Only 45% of the respondents preferred TM to WM. The main reasons given for visiting TM practioners rather than western medical practitioners were that TM is sometimes more effective than WM and that in many instances it has very minimal side effects on the human body. There is, however, a need for Ugandan government to legitimize the practice of TM since it contributes a lot to health care needs in areas where western medicine is insufficiently provided. In addition, there is a need for further research into the efficacy and safety of traditional medicines if it is to be adequately integrated into western medicine.
Keywords: Traditional medicine, health care, herbalism, spiritual counseling, bone setting, Uganda
Introduction
Traditional Medicine (TM) can be defined as health practices, approaches, knowledge and beliefs including plant, animal and mineral-based medicines, spiritual therapies, manual techniques and exercises applied singularly or in combination to diagnose, treat and prevent illnesses or maintain well-being (WHO, 2003). It is very important for primary health care (PHC) delivery and its use is widespread in developing countries of Africa, Asia and Latin America. In Africa, up to 80% of the population uses TM for Primary Health Care (PHC) (WHO, 2002). In developed countries, adaptations of TM are termed as “Complementary” or “Alternative” Medicine (CAM). In Uganda, TM usage for day-to-day health care needs is reported to be close to 90% and that women and children form the bulk of the people reliant on herbal medicine (Kamatenesi-Mugisha and Oryem-Origa (2005). The relative ratio of traditional medicine practitioners and western university-trained doctors in relation to the whole population in Uganda is revealing as is true for many parts of the African continent. There is at least one traditional healer in Uganda for nearly 290 people compared to one Western-trained medical practitioner for every 10,000 people in the urban areas and 50,000 people in the rural areas respectively (Weisheit and Male, 2003).
TM its popularity to its accessibility, affordability and its firm embedment within the faith systems of the people (WHO, 2002). In the case of Uganda, western-trained medical personnel are either limited or not really accepted by the community, and traditional healers are easily consulted, living in the same community (Bannerman et al., 1993). The country imports most of its drugs from abroad and often experiences serious shortages. That points to the demand for TMPs for medicinal plants and the fact that the majority of the people, rural and urban alike, depend largely on herbal medicines for treating a variety of diseases (Esegu, 2002). This reliance is mainly due to the high cost of conventional medicine and inaccessibility of modern health care facilities in most areas.
Owing to TM's importance for the provision of primary health care, there is need for it to be developed, promoted and integrated into national health care systems (WHO, 1978). The government of Uganda has so far taken important steps to recognition of TM and a draft bill for a law to recognize, coordinate and regulate the practice of TM the country is under preparation (Ministry of Health, 2000). The role of TM in PHC, especially at a time when resources to access modern medical facilities are scarce, cannot be underestimated. In this study, therefore, we documented the common Traditional medicine (TM) practices; assessed the local people's preferences for TM versus western medicine (WM) and lastly to determined the local peoples' awareness about the importance of TM in Nangabo sub-county of Wakiso district, central Uganda.
The study area and Methods
The study area
The study was conducted in Nangabo sub-county located in Wakiso district of central Uganda. Nangabo lies between of latitude 0° 24′ N and longitude 32° 27′ E (UDIH, 2005). It is approximately 21.45 km2 in area and is divided into nine parishes of Bulamu, Gayaza, Kabubbu, Katadde, Kiteezi, Masooli, Nangabo, Wampeewo and Wattuba. The sub-county has a population of 58,426 people comprising 28,629 males and 29797 females (UBOS, 2003). The population is heterogeneous (UDHS, 2000/2001), the majority are Baganda, a Bantu-speaking group, though most inhabitants understand or speak Luganda, a Bantu language dialect. The area receives an annual precipitation of about of 1513mm, which is evenly distributed over the year. Mean annual temperatures are 17°C minimum and 21.9°C maximum respectively (UNCST, 2001). Livelihoods are mainly derived from subsistence agriculture comprising of arable farming and animal rearing. The study concentrated in the parishes of Gayaza, Nangabo and Kiteezi because they have a high population of traditional medicine practitioners (TMPs) in the sub-county.
Methods
Participatory Rural Appraisal (PRA) techniques including focus group discussions (FGDs), informal and formal interviews using semi-structured questionnaires were used to collect the data. Purposive sampling was used to select knowledgeable informants (herbalists, spiritualists, bone setters and traditional birth attendants) that were directly involved in traditional medicine use and promotion. Participants were identified by the first authors assisted by civic leaders from different villages in the three parishes surveyed. On-site clients were selected using quota-sampling technique while stratified random sampling was used to select resident respondents for individual interviews. A total of 12 villages in 3 parishes (4 villages in each parish) were selected and questionnaires administered to 10 resident respondents in each village. In addition, two (2) focused group discussions (FGDs) were held with TMPs in each of the three parishes. FGDs were conducted in Luganda while in-depth interviews were conducted in either English or Luganda. Data were analyzed descriptively using Statistical Packages for Social Sciences (SPSS).
Results
Socio-economic characteristics of the respondents
Most (33%) of the respondents were aged 45 years (Table 1). Fifty one percent of the respondents were males and 45% had attained tertiary education. Only 10% of respondents did not attend any form of formal education. Most (43%) of the respondents derived livelihoods from traditional medicine practices.
Table 1.
Demographic and socio- economic characteristics of respondents in Nangabo sub-county, Wakiso district, central Uganda (N=120)
| Variable | (%) response |
| Sex | |
| Male | 51 |
| Female | 49 |
| Age | |
| 16–25 | 24 |
| 26–35 | 29 |
| 36–45 | 14 |
| >45 | 33 |
| Level of education attained | |
| No formal education | 10 |
| Primary | 13 |
| Secondary | 32 |
| Tertiary | 45 |
| Main income source | |
| Subsistence farming | 20 |
| Business | 20 |
| TM practices | 43 |
| Civil service | 17 |
Types of traditional medicine practices
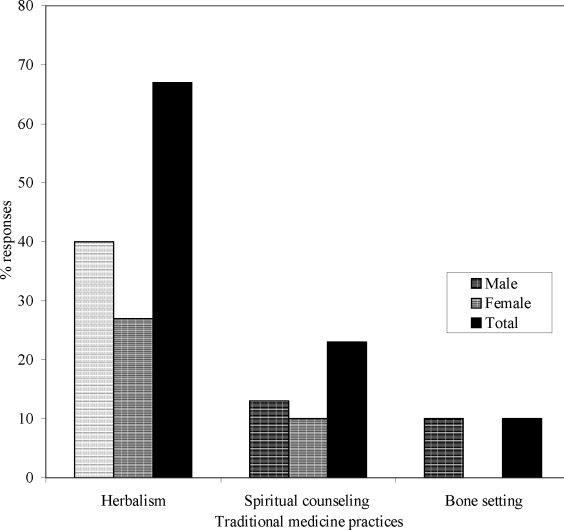
Herbalism (67%) was the major TM practice reported by the people interviewed (Figure 1). Herbalists use traditional therapies to identify and treat various ailments such as malaria, headache, measles, importance, dermatitis and mental sicknesses. Other types of TM practices in Nangabo sub-county included spiritual counseling (23%) and bone setting (10%). In all cases of TM practices, men responded more than women. Bone setting as one form of TM practices was reported only by men.
Figure 1.
Types of traditional medicine practices in Nangabo sub-county, Wakiso district, Central Uganda
Preferences for TM versus western medicine (WM)
Generally, respondents preferred western medicine to TM (Table 2). Only 45% of the respondents preferred TM. The rest (55%) wanted western medicine. The literacy level of the patients seems to be a key factor determining the choice of treatment. Respondents who had attained primary and secondary education preferered TM to WM. Those who were more educated (attained tertiary level of education) more often preferred WM to TM.
Table 2.
Cross tabulation of education level and local preferences for traditional medicine (TM) versus western medicine in Nangabo sub-county, Central Uganda (WM) (N=120)
| Education level | Preferred type of medicine (%) | Total % | |
| WM | TM | ||
| No formal education | 8 | 2 | 10 |
| Primary | 3 | 10 | 13 |
| Secondary | 12 | 20 | 32 |
| Tertiary | 32 | 13 | 45 |
| Total | 55 | 45 | 100 |
The main reasons given for visiting traditional medicine practioners (TMPs) rather than western trained doctors were numerous (Table 3). TM was largely (51%) considered by many respondents as having very minimal side effects on the human body as opposed to many drugs used in western medical practices. Majority (41%) of the respondents also reported that TM have a propensity to reduce the prevalence levels of ailments much faster in some circumstances than most of the prescriptions used in western-style medicine. Equally important, is the belief that most (32%) respondent that TM sometimes cure the ailment more faster than the WM. Other people (24%) simply have faith in TM as a good substitute to WM.
Table 3.
Reasons for preference of traditional medicine in Nangabo sub-county, Central Uganda (WM) (N=120)
| Reason for preference of TM | % response | ||
| Males | Females | Total | |
| TM in most cases has minimal side effects than WM | 27 | 22 | 51 |
| TM reduce prevalence levels | 10 | 31 | 41 |
| TM sometimes cures faster then WM | 13 | 19 | 32 |
| TM is a good substitute to WM | 14 | 10 | 24 |
| TM has complementary function | 2 | 14 | 16 |
| TMPs are easier to access than WMD | 6 | 5 | 11 |
| TM is sometimes useful for certain unique health | 6 | 4 | 10 |
| problems | |||
| TM is crucial option as a First Aid especially in cases | 8 | 1 | 9 |
| where health clinics are away from home | |||
| TM is cheaper than WM | 3 | 3 | 6 |
TM-Traditional Medicine, WM- Western Medicine, TMP's-Traditional Medical Practioners WMD-Western Trained Doctors
Traditional medicine practices were also reported by some (11%) respondents to be more accessible than the western medicine practitioners. Other reasons cited by the respondents as to why the members of their community prefer TM included amongst other things-complementarity functions of most type of TM, the uniqueness of TM to certain health problems such as health dilemmas associated with witchcrafts. TM was preferred because of the central role it plays as a First Aid especially in cases where health clinics are away from homes and the fact that TM is generally cheaper form of medicine to afford by poor households as opposed to WM.
Awareness of the importance of traditional medicine amongst the local people
Generally, majority (81%) of the respondents were aware of the importance of TM. Elderly people (>45 years of age) were more informed about the importance of TM compared to other age categories (Table 4). The level of awareness of the importance of TM by respondents, though high, appears to contradict their health seeking behaviors, because, most of them reportedly prefer WM more than TM. This discrepancy could perhaps be cause of the efforts often made government in promoting WM.
Table 4.
Cross tabulation of respondents ages with the awareness of the importance of TM in Nangabo sub-county, Central Uganda (WM) (N=120)
| Age groups (years) | Importance of TM (% response) | ||
| Aware | Not aware | Total | |
| 18–25 | 23 | 1 | 24 |
| 26–35 | 18 | 11 | 29 |
| 36–45 | 10 | 4 | 14 |
| >45 | 30 | 3 | 33 |
| Total | 81 | 19 | 100 |
Discussion
The empirical results show that three major form of TM practices exits in Nangabo sub-county, some of which have been reported in earlier surveys (Mugumya, 1997; Barak et al., 2000). Like in this study, herbalism and spiritual counseling were reported to be key TM practices in central Uganda (Mugumya, 1997) and healers often use their knowledge, training and indiscernible powers from the spirit world to diagnose and treat various forms of illnesses (Barak et al., 2000). The findings of this study demonstrated that in certain circumstances, traditional medical practitioners (TMPs) have the advantage over the modern healthcare providers in that they spend more time with the patient and keep good track of them by maintaining a close personal relationship with them, a practice that is often uncommon with western trained medical practitioners. As a result, patients usually feel secure to disclose their experiences, including family matters, to the TMPs. This always enables the TMPs to guide their patients on how to deal with different ailments and at the same time on how to cope-up with the demands of life.
Given their counseling skills, most TMPs often persuade many patients or clients who claim for instance to be bewitched to take their counseling services. Most TM practices like herbalism were said to have limited side effects as compared to western pharmaceutical drugs. Side effects such as resistance to herbal therapies, body weakness and nerve damage, were said to be very uncommon with TM. This perhaps could be explained by the fact that most TMPs use herbs, which are often administered in their natural form with no added chemical preservatives or concentrates (THETA, 1998). Apart from curing opportunistic infections, the herbs probably play a preventive role by strengthening the body immunity to resist infections, restore vital body nutrients, provide energy, restore appetite and prevent body wasting.
As also reported by Namata (2000), the participants in this study noted some form of TM practices like herbalism is easier to administer than some form of WM. There is no need for patients to undergo painful treatments like injections in WM. In addition, a study by WHO (2000) reported that visiting a medical centre for injections can be irregular and expensive to some patients especially in a rural setting. In this study, it was reported that TM is relatively cheaper and easier to access compared to WM and that some times TM is unconsciously used especially by households that depends a lot on traditional/wild vegetables and fruits. In Nangabo sub-county, most of the herbal plants are readily available in people's gardens and the patients can easily prepare an herbal infusion on their own and use them without much supervision.
In spite of the good services provided by TMPs and the high level of awareness about the importance of TM, some respondents still did not like TM practices. The fact the majority of them preferred WM is consistent with what Namata (2000) reported “that the moment one mentions about TM practices, some members of the society especially religious leaders do not feel happy about it because they always regard it as evil and barbaric and therefore undermine its wider use”. Witchcraft is a common practice associated with traditional medicine for which western medicine claims advantage over it. As reported by Evans (1993), religious preaching is more often against TM practices and sometimes the issue of human sacrifices associated with TM practices overshadows its importance.
Nonetheless, TM will still continue to preliminary play a significant role in health care of many rural families. There is need to legitimize and monitor the practice of TM in Uganda so that useful practices can be further developed and promoted. More outreach activities on TM practices also need to be conducted if the general public is to fully appreciate the role of TM in preliminary health care system. In addition, there is a need for further research into the efficacy and safety of traditional medicines especially with regards to herbal medicine if it is to be adequately integrated into western medicine. There is a need to follow up this preliminary work with one more focusing more on of age and gender of the respondents other than sex.
References
- 1.Bannerman RH, Burton J, Chien Wen-Chieh. Traditional Medicine and Health Care Coverage. Geneva: World Health Organisation; 1993. [Google Scholar]
- 2.Barak A K, Eden E S, Faull M M. “Alter AIDS Complementary Medicine for a Healthier Community, Medicinal Plants Research Net work, India. 2000. [Google Scholar]
- 3.Esegu JFO. Research in Medicinal Plants in Uganda, Internal Presentation. Kampala, Uganda: Forest Recources Research Institute; 2002. [Google Scholar]
- 4.Evans P. African Studies v 53. Johannesburg: 1993. “Can We Get a Beast Without Hair?” Medicine Murder in Swaziland from 1970 to 1988. [Google Scholar]
- 5.Kamatenesi-Mugisha M, Oryem-Origa H. Traditional herbal remedies used in the management of sexual impotence and erectile dysfunction in western Uganda. Afr Hlth Sci. 2005;5(1):40–49. [PMC free article] [PubMed] [Google Scholar]
- 6.Ministry of Health, author. Health Sector Strategic Plan 2000 / 01–2004 / 05. Kampala: Ministry of Health; 2000. [Google Scholar]
- 7.Mugumya F. A study of Attitude and beliefs of people towards Hot Springs as a source of Traditional Healing in Humurwa Sub-county, BSc. Special Project Report. Kampala: Makerere University; 1997. p. 59. [Google Scholar]
- 8.Namata R, K. Understanding Indigenous Knowledge; Trainers Manual. Kampala: Uganda National Council of Science and Technology; 2000. p. 48. [Google Scholar]
- 9.THETA, author. Participatory Evaluation Report. Kampala: THETA; 1998. [Google Scholar]
- 10.UBOS, author. Uganda National Household Survey 2002–2003. Scocioeconomic survey. Entebbe: MFPED; 2003. p. 104. [Google Scholar]
- 11.UDHS, author. Uganda Bureau of Statistics and Macro International, Inc; 2001. Uganda Demographic and Health Survey (UDHS) report. Calverton, MD, USA: 2000/2001. [Google Scholar]
- 12.UDIH, author. Uganda Districts Information Handbook. Kampala: Fountain Publishers; 2005. [Google Scholar]
- 13.UNCST, author. IK resource development news letter. Kampala: 2001. Indigenous Knowledge Up date; p. 65. [Google Scholar]
- 14.Weisheit A, Male M. Traditional Medicine Practice in Contemporary Uganda. IK Notes. World Bank. 2003. http://www.worldbank.org/afr/ik/default.htm.
- 15.WHO, author. The Promotion and Development of Traditional Medicine. Technical Report Series 622. Geneva: 1978. [PubMed] [Google Scholar]
- 16.WHO, author. Promoting the Role of Traditional Medicine in Health Systems, A Strategy for the African Region. Harare: AFR/RC50/R3; 2000. [Google Scholar]
- 17.WHO, author. WHO Traditional Medicine Strategy 2002–05. Geneva: World Health Organization; 2002. WHO/ EDM / TRM / 2002.1. [Google Scholar]
- 18.WHO, author. Traditional Medicine. Geneva: WHO Media center; 2003. Fact sheet number. 134. [Google Scholar]