Abstract
OBJECTIVE
Diabetes guidelines recommend aggressive screening for type 2 diabetes in Asian patients because they are considered to have a higher risk of developing diabetes and potentially worse prognosis. We determined incidence of diabetes and risk of death or macrovascular complications by sex among major Asian subgroups, South Asian and Chinese, and white patients with newly diagnosed diabetes.
RESEARCH DESIGN AND METHODS
Using population-based administrative data from British Columbia and Alberta, Canada (1997–1998 to 2006–2007), we identified patients with newly diagnosed diabetes aged ≥35 years and followed them for up to 10 years for death, acute myocardial infarction, stroke, or hospitalization for heart failure. Ethnicity was determined using validated surname algorithms.
RESULTS
There were 15,066 South Asian, 17,754 Chinese, and 244,017 white patients with newly diagnosed diabetes. Chinese women and men had the lowest incidence of diabetes relative to that of white or South Asian patients, who had the highest incidence. Mortality in those with newly diagnosed diabetes was lower in South Asian (hazard ratio 0.69 [95% CI 0.62–0.76], P < 0.001) and Chinese patients (0.69 [0.63–0.74], P < 0.001) then in white patients. Risk of acute myocardial infarction, stroke, or heart failure was similar or lower in the ethnic groups relative to that of white patients and varied by sex.
CONCLUSIONS
The incidence of diagnosed diabetes varies significantly among ethnic groups. Mortality was substantially lower in South Asian and Chinese patients with newly diagnosed diabetes than in white patients.
Over the past 20 years, we have seen an explosive increase in the number of cases of diabetes worldwide. The number of individuals with diabetes is expected to more than double by the year 2025. This will have a tremendous public health impact given the high rates of acute myocardial infarction [AMI], heart failure, stroke, and death that follow diabetes.
Along with advancing age and increases in obesity prevalence, one putative factor thought to be contributing to this global epidemic is an escalation in the population of nonwhite groups at higher risk for diabetes. The largest increases in diabetes worldwide are occurring in developing countries. The prevalence of diabetes in urban areas of India is as high as 18% (1) and a recent study shows a threefold increase in diabetes prevalence in certain areas of China (2). South Asian and Chinese groups may have a greater susceptibility to developing diabetes due to a predisposition to insulin resistance in the presence of environmental factors including diet and physical inactivity. Differences in health care systems, limited access to health services, and social deprivation can further compound the risk of developing diabetes and its complications.
Our current understanding of the incidence and prognosis of diabetes in South Asian and Chinese men and women is limited. There is a paucity of ethnicity- and sex-stratified longitudinal population-based studies. Incidence has only been estimated from prevalence data in cross-sectional studies under various health care systems. General practitioner clinic and general population surveys in Western countries uniformly observe a higher prevalence of diabetes in South Asian respondents compared with that in the general population (3,4). Results among Chinese migrants are inconsistent, with prevalence rates up to 14% (5). Further, it is unclear whether these groups also have a greater susceptibility to developing complications of diabetes. We conducted a large, population-based study in two Canadian provinces to determine the incidence of diabetes and the risk of death and macrovascular complications including AMI, heart failure, and stroke among South Asian, Chinese, and white women and men up to 10 years after a new diagnosis of diabetes.
RESEARCH DESIGN AND METHODS
Data sources
We used administrative data from two Canadian provinces (British Columbia 1993–2006 and Alberta 1994–2007) that comprise 44% of all Chinese and 34% of all South Asian people in Canada (6). Physician claims files contain information for each hospital and outpatient encounter for each patient. Hospital discharge abstracts include all inpatient services for all hospitals within these provinces and contain primary and secondary discharge diagnosis codes of the ICD-9 and ICD-10, with up to 25 diagnosis fields per individual admission. Physician claims and hospital discharge data are updated daily and include all patients with provincial health insurance. Under a universal health care system, virtually all residents of these provinces are covered by health insurance ensuring completeness of data. The provincial population registry contains surname, birth date, sex, and postal code on residents of the province. Population counts from provincial registries correspond to census population estimates (7), but, unlike census data, provide actual counts in inter-census years. All deaths are reported to the Vital Statistics database, and date of death was obtained by linking to Vital Statistics via a unique personal health number.
Study population
All residents of these provinces with a physician diagnosis of diabetes were included. Individuals with diabetes were defined as those with an ICD-9 or ICD-10 code for diabetes (ICD-9-CM: 250.x; ICD-10: E109, E119, E139, E149, E101, E111, E131, E141, E105, E115, E135, and E145) for at least one hospital discharge abstract or two physician claims within 2 years. Patients aged <35 years were excluded to reduce the misclassification of type 2 diabetes as type 1 diabetes. Patients with gestational diabetes mellitus, identified with coding for an obstetrical event within 5 months of diabetes diagnosis were also excluded. This coding algorithm was extensively validated against physician diagnosis of diabetes across sex, age-groups, and rural/urban residents and among those with and without comorbid conditions with a sensitivity of 92.3%, specificity of 96.9%, and a positive predictive value (PPV) of 77% (8,9).
Categorizing ethnic group
Self-reported ethnicity is not documented in administrative data in Canada. We used validated surname analysis to categorize patients as South Asian (from Pakistan, India, or Bangladesh) or Chinese (from China, Taiwan, or Hong Kong) using surnames recorded in provincial registries. Compared with self-report, the sensitivity for the Quan surname algorithm for Chinese ethnicity was 78%, specificity was 99.7%, and PPV was 81% (10). For the Nam Pehchan algorithm for South Asian ethnicity, the sensitivity was 90–94%, specificity was 99.4%, and PPV was 63–96% (11–13). All remaining patients are referred to as “white” because this group is largely (93.2%) composed of white, nonvisible minority individuals (6).
Procedures
To determine incident cases, we identified all patients in whom diabetes was diagnosed at each fiscal year. Patients with incident cases had a minimum of 3 previous years without any coding for diabetes in hospital or physicians claims files to minimize misclassifying prevalent cases as incident (98.9% of patients in each ethnic group still had nondiabetes physician visits in this time period). Thus, incident cases are determined for 1997–2003. To avoid falsely attributing the absence of diabetes diagnosis to newly arrived immigrants, we only included those patients with health insurance registration for at least 3 years before their diabetes diagnosis.
To control for severity of illness at the time of diagnosis of diabetes, we measured clinical variables from the Charlson Comorbidity Index validated to predict mortality in patients with type 2 diabetes (14). Socioeconomic status (SES) was assessed using area level median income based on the patient's postal code. SES data were missing for 11,665 patients (2.5% Chinese, 2.9% South Asian, and 4.4% white). A missing value was assigned to these patients and retained in all models.
Outcomes
Time to death after diabetes diagnosis was the primary outcome. Secondary outcomes included hospitalization for AMI, acute stroke, or heart failure and were determined using validated coding algorithms in hospital discharge abstracts: AMI (ICD-9 410; ICD-10 I21), PPV 0.95 (15); stroke (ICD-9 430, 431, 434, and 436; ICD-10 I60-I62, I63.3-I63.5, I63.8, I63.9, and I64), PPV 0.85–0.98 (16); and heart failure (ICD-9 428.x; ICD-10 I5O), PPV 0.84 (17). Time to event was assessed up to 31 March 2006 for British Columbia and to 31 March 2007 for Alberta with up to 10 years follow-up (median 4.0 years). Patients were censored if they moved out of the province or reached the end of the observation period.
Statistical analysis
We determined age-specific (reported for the most recent fiscal year, 2003–2004) and age-standardized incidence of diagnosed diabetes for each ethnic and sex group. Yearly incidence of diagnosed diabetes (per 1,000 population) was calculated using new cases of diabetes for each group as the numerator with the corresponding population count as the denominator for the most recent 5-year time period (1999–2003). Annual population counts for each ethnic and sex group were determined by applying the surname algorithms to the annual provincial registry population counts, minimizing denominator bias. We used direct age standardization for each group with the total provincial population in the same fiscal year as the reference group. Poisson regression analysis was used to compare incidence rates between ethnic and sex groups and linear regression was used to determine change in incidence over time.
Categorical variables were compared using the χ2 test. Cox proportional hazards models were constructed and stratified by sex, with adjustment for province, SES quintile, age in 5-year categories, previous history of AMI, heart failure, cerebrovascular disease, peripheral arterial disease, renal impairment, cancer, dementia, chronic pulmonary disease, hypertension, rheumatic disease, peptic ulcer disease, liver disease, hemiplegia, metastatic carcinoma, and AIDS/HIV. We also conducted sensitivity analyses using the British Columbia cohort by additionally adjusting for insulin, metformin, statin, or ACE inhibitor prescribing within 5 years of diagnosis using a province-wide prescription drug database (PharmaNet) only available in British Columbia.
All analyses were conducted with SAS (version 9.1.3) and graphs were plotted using R. This study was approved by the local ethics institutional review boards.
RESULTS
There were 555,206 patients who met the coding definition for diabetes. After exclusion of 18,037 patients aged <35 years, 17,602 with gestational diabetes, 199,592 patients without a minimum 3-year period of observation without a diabetes diagnosis, and 43,138 patients without insurance registration within 3 years before diabetes diagnosis, 276,837 remaining patients were identified as having incident cases of diagnosed diabetes (15,066 [5.4%] South Asian, 17,754 [6.4%] Chinese, and 244,017 [88.1%] white patients).
South Asian patients were 4.6 years younger on average than Chinese and white patients at diagnosis of diabetes (Table 1). White patients were more likely to have cardiovascular disease and cancer relative to the ethnic groups.
Table 1.
Baseline characteristics among diabetic patients aged ≥35 years
| Characteristics | Chinese | South Asian | White | P value |
|---|---|---|---|---|
| n | 17,754 | 15,066 | 244,017 | |
| Age at diagnosis | ||||
| Age (years) | 59.7 ± 12.8 | 56.5 ± 12.3 | 61.3 ± 13.1 | <0.001 |
| 35–49 years | 4,390 (24.7) | 4,753 (31.6) | 50,082 (20.5) | <0.001 |
| 50–64 years | 6,680 (37.6) | 6,307 (41.9) | 94,788 (38.8) | |
| 65–79 years | 5,507 (31.0) | 3,424 (22.7) | 76,717 (31.4) | |
| ≥80 years | 1,177 (6.6) | 582 (3.9) | 22,430 (9.2) | |
| Female sex | 8,458 (47.6) | 6,672 (44.3) | 110,142 (45.1) | <0.001 |
| Province: British Columbia | 14,084 (79.3) | 9,529 (63.3) | 143,630 (58.9) | <0.001 |
| Socioeconomic quintile | ||||
| First quintile (low) | 4,370 (24.6) | 3,208 (21.3) | 56,915 (23.3) | <0.001 |
| Second quintile | 3,908 (22.0) | 3,498 (23.2) | 49,138 (20.1) | |
| Third quintile | 2,990 (16.8) | 3,051 (20.3) | 46,377 (19.0) | |
| Fourth quintile | 2,814 (15.9) | 2,730 (18.1) | 42,607 (17.5) | |
| Fifth quintile (high) | 3,223 (18.2) | 2,147 (14.3) | 38,196 (15.7) | |
| Unknown | 449 (2.5) | 432 (2.9) | 10,784 (4.4) | |
| Comorbid conditions | ||||
| Hypertension | 7,308 (41.2) | 5,612 (37.3) | 99,578 (40.8) | <0.001 |
| Myocardial infarction | 266 (1.5) | 473 (3.1) | 10,152 (4.2) | <0.001 |
| Congestive heart failure | 444 (2.5) | 498 (3.3) | 14,578 (6.0) | <0.001 |
| Peripheral vascular disease | 245 (1.4) | 155 (1.0) | 6,234 (2.6) | <0.001 |
| Cerebrovascular disease | 447 (2.5) | 358 (2.4) | 9,318 (3.8) | <0.001 |
| Dementia | 121 (0.7) | 106 (0.7) | 4,103 (1.7) | <0.001 |
| Chronic pulmonary disease | 1,394 (7.9) | 1,794 (11.9) | 31,032 (12.7) | <0.001 |
| Renal disease | 324 (1.8) | 194 (1.3) | 5,090 (2.1) | <0.001 |
| Cancer | 593 (3.3) | 372 (2.5) | 14,127 (5.8) | <0.001 |
| Oral hypoglycemic agent* | 4,619 (32.8) | 3,731 (39.1) | 52,590 (36.6) | <0.001 |
| Insulin* | 149 (1.1) | 130 (1.36) | 4,092 (2.85) | <0.001 |
Data are means ± SD or n (%).
*Medication prescribed within 1 year of diagnosis in British Columbia patients only.
Diabetes incidence
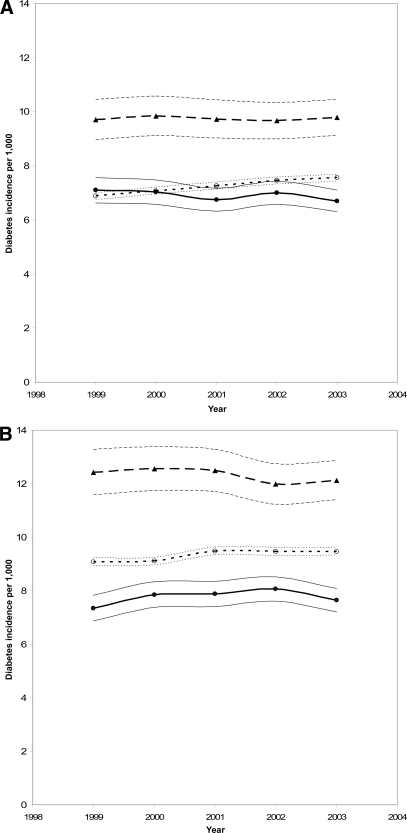
From Table 2, incidence of diagnosed diabetes was higher among men relative to women for all ethnic groups. Overall, South Asian patients had the highest age-adjusted incidence of diabetes, whereas Chinese patients had the lowest (Fig. 1). In the age-specific incidence, South Asian patients had the highest incidence of diabetes in all young to middle-aged categories. However, after the age of 65, the incidence of diabetes was highest among white patients. Diabetes incidence for white patients and Chinese men increased during the observation period but remained stable for South Asian patients and Chinese women (Fig. 1).
Table 2.
Age-specific incidence of diagnosed diabetes by ethnicity and sex (per 1,000 population) in fiscal year 2003–2004
| Age | Chinese |
South Asian |
White |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| New cases | Pop* | Incidence (95% CI) | P value | New cases | Pop* | Incidence (95% CI) | P value | New cases | Pop | Incidence (95% CI) | |
| Women | |||||||||||
| 35–44 years | 128 | 61,099 | 2.1 (1.7–2.5) | 0.006 | 129 | 27,846 | 4.6 (3.8–5.4) | <0.001 | 1,367 | 506,420 | 2.7 (2.6–2.8) |
| 45–54 years | 292 | 50,900 | 5.7 (5.1–6.4) | 0.99 | 205 | 22,069 | 9.3 (8.0–10.6) | <0.001 | 2,757 | 480,861 | 5.7 (5.5–6.0) |
| 55–64 years | 214 | 23,479 | 9.1 (7.9–10.3) | 0.04 | 257 | 16,795 | 15.3 (13.5–17.2) | <0.001 | 3,424 | 323,964 | 10.6 (10.2–10.9) |
| >65 years | 464 | 40,374 | 11.5 (10.5–12.5) | 0.004 | 240 | 19,257 | 12.5 (10.9–14.0) | 0.4 | 5,787 | 438,246 | 13.2 (12.9–13.5) |
| Men | |||||||||||
| 35–44 years | 154 | 53,886 | 2.9 (2.4–3.3) | 0.1 | 257 | 30,600 | 8.4 (7.4–9.4) | <0.001 | 1,622 | 502,421 | 3.2 (3.1–3.4) |
| 45–54 years | 339 | 50,521 | 6.7 (6.0–7.4) | 0.02 | 277 | 22,760 | 12.2 (10.8–13.6) | <0.001 | 3,704 | 482,218 | 7.7 (7.4–7.9) |
| 55–64 years | 290 | 23,681 | 12.3 (10.9–13.7) | 0.02 | 288 | 16,709 | 17.2 (15.3–19.2) | <0.001 | 4,572 | 324,698 | 14.1 (13.7–14.5) |
| >65 years | 411 | 35,126 | 11.7 (10.6–12.8) | <0.001 | 228 | 17,768 | 12.8 (11.2–14.5) | <0.001 | 5,940 | 354,004 | 16.8 (16.4–17.2) |
*2003–2004 population.
Figure 1.
A: Age-adjusted incidence of diagnosed diabetes by ethnicity in women aged ≥35 years (1999–2003). B: Age-adjusted incidence of diagnosed diabetes by ethnicity in men aged ≥35 years. ▴, South Asian; ○, white; ●, Chinese.
Mortality and macrovascular complications
Total mortality was substantially lower in South Asian and Chinese men and women than in white men and women (Table 3). Even after adjustment for baseline characteristics, mortality remained substantially lower in South Asian and Chinese patients. Additional adjustment for use of insulin, metformin, ACE inhibitors, or statin therapy in the sensitivity analysis did not materially affect these results. These differences were seen across different age subgroups, within each province, and among those with and without comorbid conditions.
Table 3.
Age-standardized and -adjusted outcomes by ethnicity in diabetic women and men aged ≥35 years
| Outcome | Age standardized events/1,000 patient years |
Hazard ratio (95% CI),*P value |
|||
|---|---|---|---|---|---|
| Chinese | South Asian | White | Chinese vs. white | South Asian vs. white | |
| Women | |||||
| n | 8,458 | 6,672 | 110,142 | ||
| Mortality | 18.6 | 20.7 | 30.9 | 0.69 (0.63–0.74) P < 0.001 | 0.69 (0.62–0.76) P < 0.001 |
| Stroke | 4.1 | 5.3 | 4.7 | 0.91 (0.76–1.08) P = 0.26 | 1.06 (0.88–1.29) P = 0.54 |
| AMI | 1.5 | 5.4 | 4.5 | 0.34 (0.26–0.46) P < 0.001 | 1.19 (0.99–1.44) P = 0.06 |
| Heart failure | 2.3 | 6.0 | 6.3 | 0.42 (0.34–0.54) P < 0.01 | 0.95 (0.79–1.15) P = 0.6 |
| Men | |||||
| n | 9,296 | 8,394 | 133,875 | ||
| Mortality | 17.8 | 20.5 | 32.6 | 0.61 (0.60–0.66) P < 0.001 | 0.68 (0.63–0.74) P < 0.001 |
| Stroke | 4.2 | 4.3 | 5.1 | 0.81 (0.69–0.96) P = 0.01 | 0.82 (0.68–0.99) P = 0.04 |
| AMI | 2.8 | 7.9 | 7.9 | 0.37 (0.31–0.45) P < 0.001 | 1.05 (0.92–1.19) P = 0.49 |
| Heart failure | 2.0 | 4.4 | 6.4 | 0.38 (0.30–0.48) P < 0.01 | 0.71 (0.56–0.92) P < 0.01 |
*Hazard ratios are adjusted for age, SES, province, and comorbid conditions including previous history of AMI, heart failure, cerebrovascular disease, peripheral arterial disease, renal impairment, cancer, dementia, chronic pulmonary disease, hypertension, connective tissue disease-rheumatic disease, peptic ulcer disease, mild liver disease, paraplegia and hemiplegia, moderate or severe liver disease, metastatic carcinoma, and AIDS/HIV.
Macrovascular complications among ethnic groups varied by sex. South Asian and white women had a similar risk of developing macrovascular complications. However, Chinese women had a substantially lower risk of AMI and heart failure. South Asian and Chinese men had a lower risk of stroke and heart failure relative to that of white men. Chinese men had the lowest risk for AMI whereas South Asian and white men had a similar risk of AMI.
CONCLUSIONS
South Asian patients had the highest incidence of diagnosed diabetes, whereas Chinese patients had the lowest incidence. Mortality was also lower for South Asian and Chinese patients compared with that for white patients with newly diagnosed diabetes, for both men and women. However, macrovascular complications varied by ethnicity and sex.
There is a disproportionately high rate of new cases of diabetes among young to middle-aged, South Asian patients. Our findings affirm estimates from numerous prevalence studies (3,4). The age- and sex-specific incidence pattern of diabetes among white patients is also consistent with general population incidence rates (8). The observed lower incidence of diabetes in Chinese patients contrasts with that in a small study reporting a similar incidence between Chinese and other patients in the U.S.; however, age-adjusted incidence was not determined (18).
Diabetes guidelines generally recommend initial screening for diabetes at age 45 years, although a younger threshold is recommended for patients of Asian descent. The optimal age at which to start early surveillance in South Asians is unclear. It is also not known whether early surveillance would benefit other Asian groups (e.g., Chinese). This study identified an alarmingly high incidence of diabetes in South Asian patients, particularly in men aged 35–44 years, indicating that screening as early as 35 years may be warranted. Our findings also suggest that Chinese patients do not necessarily share this early proclivity for developing diabetes.
Despite a greater predilection for developing diabetes, we found a paradoxically lower mortality among South Asians than among white patients. Chinese patients also had a significantly lower mortality. Although South Asian patients were considerably younger and both South Asian and Chinese patients possessed fewer comorbid conditions at the onset of diabetes, the mortality benefit persisted after adjustment for these differences. Our findings are consistent with results from several smaller studies of diabetic patients (19,20), and general population mortality rates also indicate lower all-cause mortality for South Asian and Chinese patients compared with white patients living in North America (21). Our results, however, contrast with those for the Southall Diabetes Survey cohort, which reported a nonsignificant trend toward increased mortality in South Asian patients compared with their white counterparts using prevalent rather than incident cases (22). However, mortality rates for all groups were substantially higher compared with general population mortality rates for Chinese, South Asian, and white patients living in North America (21). This observation suggests that the presence of diabetes confers a greater risk of death regardless of ethnicity.
The reasons for the ethnic and sex differences in mortality and macrovascular complications of diabetes are unclear, and we can speculate on possible mechanisms. South Asian and Chinese patients, particularly men, may have their diabetes diagnosed earlier along the course of disease and may receive more aggressive care. However, even after we adjusted for metformin, statin, and ACE inhibitor prescribing, the mortality benefit in South Asian and Chinese patients persisted. Alternatively, some ethnic patients may not have accessed medical care and were therefore not included in the study population. These individuals with undiagnosed diabetes may be more likely to experience early mortality. However, a national survey in Canada found that visible minority and white patients reported a similarly high frequency of physician visits (23). Chinese and South Asian patients have lower rates of smoking and BMI, potentially contributing to their survival advantage. However, these differences are unlikely to account for all the benefit. In a U.S. study, despite adjustment for these differences, a lower risk of AMI, stroke, and heart failure was identified in Asian patients with newly diagnosed diabetes (24); however, South Asian and Chinese subgroups were not analyzed separately. In our analysis, white patients had higher rates of cardiovascular complications and therefore may have higher rates of cardiovascular death. Consistent with a general population study, white patients may also have higher rates of noncardiovascular death, including deaths due to cancer (21), collectively contributing to their higher all-cause mortality. Ethnic differences in macrovascular complications were largely attenuated in women. This observation may reflect fewer differences in diabetes management among women of different ethnic backgrounds. A study of 9,833 diabetic patients identified similar service delivery and intermediate outcomes including A1C levels and systolic blood pressure among Scottish and South Asian women (25). The lower rates of cardiovascular complications in the ethnic groups may reflect possible differences in chronic disease management including increased adherence to medication and strong family supports. Some of these influences such as family support and care-giving may also differ by sex within cultural groups.
The strengths of this study include the use of population-based data for a large, ethnically diverse area using coding algorithms extensively validated against physician diagnosis in the same geographic region. However, there are several limitations. First, we used surname algorithms alone to categorize ethnicity rather than self-report. Although the specificities of these algorithms were high, there is potential for some misclassification of ethnic categories that would underestimate differences among ethnic categories. Second, we could not differentiate type 1 and type 2 diabetes, although from our sensitivity analysis in British Columbia, <3% of patients received insulin within 1 year of diabetes diagnosis. Third, we were only able to identify physician-diagnosed diabetes, underestimating the true incidence of diabetes. Fourth, observational studies are susceptible to bias from residual confounding including confounding by age. There may be residual confounding by age. We were unable to control for differences in smoking, BMI, visceral fat, and diabetes control. We did not have information on year of immigration, but because the majority of immigration to Canada by these ethnic groups has occurred in the past 25 years (6), this population would largely be composed of first-generation immigrants. Finally, we used broad ethnic categories, and there is likely some heterogeneity among smaller subgroups within each ethnic category.
In summary, diabetes incidence and outcomes are heavily influenced by ethnicity and sex. South Asian patients have a significantly higher incidence of physician-diagnosed diabetes that is concentrated at young and middle ages, whereas Chinese patients do not. These results may have implications for screening and timing of culturally sensitive interventions to reduce this epidemic. We also observed a paradoxical finding that despite a high incidence of diabetes, mortality was lower in South Asian patients than in the general diabetic population and macrovascular complication occurrence further varied by sex. Mortality was similarly low in Chinese patients. Further studies are needed to confirm this paradoxical finding and elucidate underlying mechanisms for differences in diabetes risk and outcomes by ethnicity and sex.
Acknowledgments
This study was funded by the Canadian Institutes of Health Research (CIHR). N.A.K. is a CIHR New Investigator, a GENESIS (Sex and Sex Determinants of Cardiovascular Disease, funded by CIHR and Heart and Stroke Foundation Canada) scholar, and a St. Paul's Hospital Physician Scholar. H.Q. is a CIHR New Investigator and a senior population health investigator at the Alberta Heritage Foundation for Medical Research. S.A. holds the Michael G. DeGroote Heart and Stroke Foundation of Ontario Chair in Population Health and the Eli Lilly May Cohen Chair in Women's Health Research at McMaster University. L.P. holds a career investigator award from the Fonds de la recherche en santé du Québec and the William Dawson Chair of Medicine at McGill University.
The study sponsor had no role whatsoever in study design; in the collection, analyses, and interpretation of data; in the writing of the report; and in the decision to submit the paper for publication.
No potential conflicts of interest relevant to this article were reported.
N.A.K. and H.Q. developed the study design, contributed to data collection, conducted data analysis, contributed to data interpretation, and wrote the manuscript. H.W. conducted data analysis, contributed to data interpretation, and wrote the manuscript. S.A. and N.R.C.C. developed the study design, contributed to data interpretation, and wrote the manuscript. Y.J. contributed to data collection, contributed to data interpretation, and wrote the manuscript. L.P. contributed to data interpretation and wrote the manuscript.
Footnotes
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
References
- 1.Ramachandran A, Snehalatha C, Latha E, Vijay V, Viswanathan M: Rising prevalence of NIDDM in an urban population in India. Diabetologia 1997;40:232–237 [DOI] [PubMed] [Google Scholar]
- 2.Pan XR, Yang WY, Li GW, Liu J: Prevalence of diabetes and its risk factors in China, 1994. National Diabetes Prevention and Control Cooperative Group. Diabetes Care 1997;20:1664–1669 [DOI] [PubMed] [Google Scholar]
- 3.McKeigue PM, Shah B, Marmot MG: Relation of central obesity and insulin resistance with high diabetes prevalence and cardiovascular risk in South Asians. Lancet 1991;337:382–386 [DOI] [PubMed] [Google Scholar]
- 4.Simmons D, Williams DR, Powell MJ: Prevalence of diabetes in a predominantly Asian community: preliminary findings of the Coventry diabetes study. BMJ 1989;298:18–21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kramer H, Han C, Post W, Goff D, Diez-Roux A, Cooper R, Jinagouda S, Shea S: Racial/ethnic differences in hypertension and hypertension treatment and control in the Multi-Ethnic Study of Atherosclerosis (MESA). Am J Hypertens 2004;17:963–970 [DOI] [PubMed] [Google Scholar]
- 6.Statistics Canada [article online], 2006. Available from http://www.statcan.gc.ca Accessed 26 July 2010
- 7.Alberta Health and Wellness Comparison of Alberta population counts between the AHCIP Registry and the 2006 Census [article online], 2006. Available from http://www.health.alberta.ca/documents/Population-2006-Comparison-2009.pdf Accessed 26 July 2010
- 8.Lipscombe LL, Hux JE: Trends in diabetes prevalence, incidence, and mortality in Ontario, Canada 1995–2005: a population-based study. Lancet 2007;369:750–756 [DOI] [PubMed] [Google Scholar]
- 9.Chen G, Khan N, Walker R, Quan H: Validating ICD coding algorithms for diabetes mellitus from administrative data. Diabetes Res Clinical Pract 2010;89:189–195 [DOI] [PubMed] [Google Scholar]
- 10.Quan H, Wang F, Schopflocher D, Norris C, Galbraith PD, Faris P, Graham MM, Knudtson ML, Ghali WA: Development and validation of a surname list to define Chinese ethnicity. Med Care 2006;44:328–333 [DOI] [PubMed] [Google Scholar]
- 11.Nam Pehchan News Computer Services, Bradford Council (Dept 13). Bradford, U.K., Britannia House, Summer 1998 [Google Scholar]
- 12.Cummins C, Winter H, Cheng KK, Maric R, Silcocks P, Varghese C: An assessment of the Nam Pehchan computer program for the identification of names of South Asian ethnic origin. J Public Health Med 1999;21:401–406 [DOI] [PubMed] [Google Scholar]
- 13.Harding S, Dews H, Simpson SL: The potential to identify South Asians using a computerised algorithm to classify names. Popul Trends 1999;97:46–49 [PubMed] [Google Scholar]
- 14.Monami M, Lambertucci L, Lamanna C, Lotti E, Marsili A, Masotti G, Marchionni N, Mannucci E: Are comorbidity indices useful in predicting all-cause mortality in type 2 diabetic patients? Comparison between Charlson index and disease count. Aging Clin Exp Res 2007;19:492–496 [DOI] [PubMed] [Google Scholar]
- 15.Varas-Lorenzo C, Castellsague J, Stang MR, Tomas L, Aguado J, Perez-Gutthann S: Positive predictive value of ICD-9 codes 410 and 411 in the identification of cases of acute coronary syndromes in the Saskatchewan Hospital automated database. Pharmacoepidemiol Drug Saf 2008;17:842–852 [DOI] [PubMed] [Google Scholar]
- 16.Kokotailo RA, Hill MD: Coding of stroke and stroke risk factors using International Classification of Diseases, revisions 9 and 10. Stroke 2005;36:1776–1781 [DOI] [PubMed] [Google Scholar]
- 17.Goff DC, Jr, Pandey DK, Chan FA, Ortiz C, Nichaman MZ: Congestive heart failure in the United States: is there more than meets the I(CD code)? The Corpus Christi Heart Project. Arch Intern Med 2000;160:197–202 [DOI] [PubMed] [Google Scholar]
- 18.Nettleton JA, Steffen LM, Ni H, Liu K, Jacobs DR, Jr: Dietary patterns and risk of incident type 2 diabetes in the Multi-Ethnic Study of Atherosclerosis (MESA). Diabetes Care 2008;31:1777–1782 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chandie Shaw PK, Baboe F, van Es LA, van der Vijver JC, van de Ree MA, de Jonge N, Rabelink TJ: South-Asian type 2 diabetic patients have higher incidence and faster progression of renal disease compared with Dutch-European diabetic patients. Diabetes Care 2006;29:1383–1385 [DOI] [PubMed] [Google Scholar]
- 20.McBean AM, Li S, Gilbertson DT, Collins AJ: Differences in diabetes prevalence, incidence, and mortality among the elderly of four racial/ethnic groups: whites, blacks, Hispanics, and Asians. Diabetes Care 2004;27:2317–2324 [DOI] [PubMed] [Google Scholar]
- 21.Sheth T, Nair C, Nargundkar M, Anand S, Yusuf S: Cardiovascular and cancer mortality among Canadians of European, south Asian and Chinese origin from 1979 to 1993: an analysis of 1.2 million deaths. CMAJ 1999;161:132–138 [PMC free article] [PubMed] [Google Scholar]
- 22.Mather HM, Chaturvedi N, Fuller JH: Mortality and morbidity from diabetes in South Asians and Europeans: 11 year follow-up of the Southall Diabetes Survey, London, UK. Diabet Med 1998;15:53–59 [DOI] [PubMed] [Google Scholar]
- 23.Quan H, Fong A, De Coster C, Wang J, Musto R, Noseworthy TW, Ghali WA: Variation in health services utilization among ethnic populations. CMAJ 2006;174:787–791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Karter AJ, Ferrara A, Liu JY, Moffet HH, Ackerson LM, Selby JV: Ethnic disparities in diabetic complications in an insured population. JAMA 2002;287:2519–2527 [DOI] [PubMed] [Google Scholar]
- 25.Fischbacher CM, Bhopal R, Steiner M, Morris AD, Chalmers J: Is there equity of service delivery and intermediate outcomes in South Asians with type 2 diabetes? Analysis of DARTS database and summary of UK publications. J Public Health (Oxf) 2009;31:239–249 [DOI] [PubMed] [Google Scholar]