Abstract
Background:
Early deterioration is common in intracerebral hemorrhage (ICH). Treatment at tertiary care centers has been associated with lower ICH mortality. Guidelines recommend aggressive care for 24 hours irrespective of the initial outlook. We examined the frequency of and factors associated with transfer to tertiary centers in ICH patients who initially presented at non-tertiary emergency departments (ED). We also compared observed to expected mortality in transferred and non-transferred patients using published short-term mortality predictors for ICH.
Methods:
Adult patients who resided in a 5-county region and presented to non-tertiary EDs with nontraumatic ICH in 2005 were identified. ICH Score and ICH Grading Scale (ICH-GS) were determined. Of 16 local hospitals, 2 were designated tertiary care centers. Logistic regression was used to assess factors associated with transfer.
Results:
Of 205 ICH patients who presented to non-tertiary EDs, 80 (39.0%) were transferred to a tertiary center. In multivariate regression, better baseline function (modified Rankin scale 0-2 vs. 3-5) (OR=0.42, 95%CI 0.21-0.85, p=0.016) and black race (OR=2.28, 95%CI 1.01-5.12, p=0.046) were associated with transfer. A trend toward higher 30-day mortality was observed in non-transferred patients (32.5% vs. 45.6%, p=0.06). The ICH-GS overestimated mortality for all patients, while the ICH Score adequately predicted mortality.
Conclusions:
We found no significant difference in mortality between transferred and non-transferred patients, but the trend toward higher mortality in non-transferred patients suggests that further evaluation of ED disposition decisions for ICH patients is warranted. Expected ICH mortality may be overestimated by published tools.
Keywords: emergency medicine, intracerebral hemorrhage, stroke, tertiary care center
Introduction
Spontaneous intracerebral hemorrhage (ICH) is a devastating form of stroke with no proven treatment. ICH occurs in an estimated 67,000 persons annually in the United States and has a 30-day mortality of up to 50%.1, 2 Scales that may be readily performed in the emergency department (ED) have been developed to predict short-term ICH mortality. Hemphill et al. proposed the ICH Score, which allocates points using the presenting Glasgow Coma Score (GCS), patient age, ICH volume, ICH location, and the presence of intraventricular hemorrhage (IVH); a higher score is more predictive of 30-day mortality.3 Using similar factors but different point allocations, Ruiz-Sandoval et al. proposed the ICH Grading Scale (ICH-GS) and found it to be more accurate than the ICH Score in predicting 30-day mortality and functional outcomes.4 Of the factors found to predict short-term ICH mortality, ICH volume is the strongest predictor. ICH volume may be easily calculated in the ED using the ABC/2 method.5
The ICH Score and ICH-GS do not account for withdrawal of care and its contribution to ICH mortality. Thus, there may be a self-fulfilling prophecy in determining very early in a patient's course whether further aggressive care might be futile.6 On the other hand, a previous report found that patients who had care withdrawn had no significant influence on the performance of the ICH Score to predict short-term ICH mortality.7 Nonetheless, ICH patients who receive aggressive specialized care at tertiary care centers have increased odds of survival compared with patients who receive non-specialized care. In an analysis of 1,038 ICH patients, care provided in a setting other than a neuroscience intensive care unit (NSICU) was associated with an increase in hospital mortality (OR 3.4, 95% CI 1.65-7.60).8
The proportion of ICH patients who are transferred from non-tertiary EDs to tertiary care centers for aggressive care is unknown. We hypothesized that ICH patients frequently are not transferred to tertiary care centers from non-tertiary EDs and that this may contribute to overall ICH mortality. In a population-based study, we sought to determine how frequently ICH patients are transferred from non-tertiary EDs to tertiary care centers, we examined factors associated with transfer to tertiary care centers, and we compared observed to expected short-term mortality in transferred and non-transferred ED ICH patients.
Methods
This report analyzes data from a group of patients with ICH identified as part of the Genetic and Environmental Risk Factors for Hemorrhagic Stroke (GERFHS) study. The methodology of the GERFHS study has been previously described.9 Briefly, a portion of this study attempted to identify all residents of the five-county Greater Cincinnati/Northern Kentucky (GCNK) area ≥ 18 years of age who were hospitalized with first-ever ICH between 1/01/05 and 12/31/05. Cases were identified by retrospective review of primary and secondary ICD-9 codes 430-438.9. Study nurses also maintained active surveillance (“hot pursuit”) at several hospitals that treat most ICH in the area by reviewing neurosurgery logs and patient rosters several times each week. Two of 16 area hospitals that treat adult patients were designated as tertiary care centers, as determined by the availability of 24-hour emergent attending and resident neurosurgery coverage in addition to the presence of a dedicated NSICU. A 17th hospital exists in the region, but it is devoted to the care of children and is not included in the analysis. All potential cases were abstracted by study nurses and confirmed by study physicians. Patients living outside the five counties, determined by zip code of residence, were excluded. Other exclusion criteria were previous ICH, traumatic ICH, hemorrhagic cerebral infarction, hemorrhage associated with brain tumor or encephalitis, and hemorrhage resulting from thrombolytic treatment of ischemic stroke. IRB approval was obtained at all participating hospitals.
Patient demographics, hospital of presentation (tertiary care center or non-tertiary facility), ICH location (infratentorial or supratentorial), ICH volume, presence of IVH and hydrocephalus, presenting GCS score, baseline (pre-ICH) modified Rankin scale (mRS) score, ED disposition (transfer to a tertiary care center or not), and 30-day mortality were obtained; mRS was determined by retrospective review. Mortality was assessed by querying GERFHS study records and the Social Security Death Index. Hemorrhage volumes were measured using the ABC/2 method.5 GCS, patient age, ICH volume, location, and IVH presence were used to determine the ICH Score and ICH-GS. To estimate whether withdrawal of care decisions in the ED may have impacted the decision not to transfer to a tertiary care center, we compared death within 3 days of symptom onset in transferred and non-transferred patients.
For comparisons between transferred and non-transferred patients, Student's t-test was used for age and volume, and the chi-square test was used for dichotomized mRS (0-2: good baseline function; 3-5: poor baseline function), gender, race, presence of IVH and hydrocephalus, and location. GCS, ICH Score, and ICH-GS were considered ordinal variables and were compared using the Kruskal-Wallis test. Mortality after ICH in the two groups was compared with a log rank test. To compare observed to expected mortality as predicted by the ICH Score and ICH-GS, logistic regression models were constructed with the mortality at 30 days as the dependent variable and the two groups of ICH patients as the independent variables, adjusting for the ICH Score and ICH-GS, as appropriate. Logistic regression was also used to determine factors associated with transfer to a tertiary care center.
Results
In 2005, 286 ICH cases occurred among GCNK residents. Six cases of pure IVH were excluded from the analysis because the ICH Score and ICH-GS could not be calculated due to lack of ICH volume. Excluded from the remaining 280 cases were 53 cases who presented to tertiary care EDs, 21 cases who were not seen in an ED (6 were hospitalized for a different condition at a tertiary care hospital, 11 were hospitalized for a different condition at a non-tertiary hospital, and 4 were directly admitted to non-tertiary hospitals), and 1 case whose GCS score was not available. Thus, 205 ICH patients who presented to non-tertiary EDs are included in the analysis; 80 (39.0%) were transferred to a tertiary care center from the non-tertiary ED.
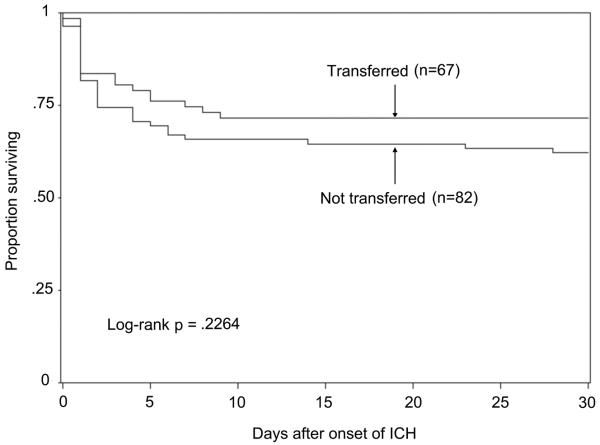
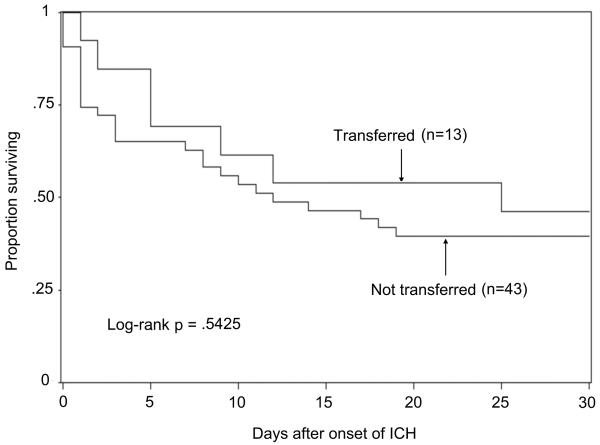
Transferred patients were 6 years younger on average, had a trend toward lower 30-day mortality, were more likely to be black, and had better baseline functional status as assessed by mRS (Table). In multivariate analysis, age, GCS, ICH location and hemorrhage volume were not associated with transfer to a tertiary care center, while better baseline mRS (OR=0.42, 95%CI 0.21-0.85, p=0.016) and black race (OR=2.28, 95%CI 1.01-5.12, p=0.046) remained associated with transfer to a tertiary care center. To examine whether the trend toward lower mortality in transferred patients was a function of better baseline mRS in those patients, we compared 30-day mortality in transferred and non-transferred patients, stratifying by mRS (Figure 1). No significant difference was found among patients with a baseline mRS of 0-2 (Figure 1a, p=0.23) or among patients with baseline mRS 3-5 (Figure 1b, p=0.54). However, when all transferred patients were compared with all non-transferred patients, the difference in mortality approached significance (Figure 2, p=0.06). Early mortality (within 3 days of onset) was significantly lower in transferred patients (17.2% vs. 32.0%, p=0.02) (Figure 2).
Table.
Comparison of Transferred and Non-transferred ICH Patients Presenting to Non-tertiary EDs in the Greater Cincinnati Region in 2005
| Transferred | Non-transferred | p value | |
|---|---|---|---|
| N | 80 | 125 | |
| Age, mean (SD) | 66.3(15.6) | 72.4(15.3) | 0.006 |
| Black Race (%) | 18(22.5) | 12(9.6) | 0.01 |
| Female Gender (%) | 42(52.5) | 71(56.8) | 0.55 |
| Baseline mRS 0-2, N (%) | 67(83.8) | 82(65.6) | 0.0044 |
| Baseline GCS, median (range) |
14(3-15) | 13(3-15) | 0.33 |
| ICH volume, mean(CI) | 15.6(10.9-22.3) | 13.3(9.7-18.3) | 0.53 |
| Infratentorial location, N (%) |
15(18.8) | 17(13.6) | 0.067 |
| IVH (Y or N) | 35(43.8) | 50(40.3) | 0.63 |
| Hydrocephalus (Y or N) | 24(30.0) | 43(34.4) | 0.51 |
| ICH Score, median (range) | 2(0-5) | 2(0-5) | 0.76 |
| ICH-GS, median (range) | 8.5(5-13) | 8.0(5-13) | 0.68 |
| 30-day mortality, N (%) | 26(32.5) | 57(45.6) | 0.06 |
Figure 1.
Thirty Day Survival Curves in Transferred and Non-transferred ICH Patients, by mRS
1a – mRS 0-2
1b – mRS 3-5
Figure 2.
Thirty Day Survival Curves in All Transferred and Non-transferred ICH Patients
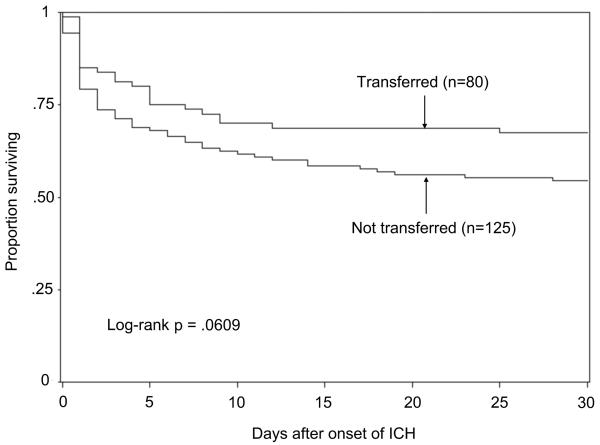
ICH Scores and ICH-GS were similar in transferred and non-transferred patients. The observed 30-day mortality for all transferred patients was 32.5%, which was similar to the expected mortality of 29.2% by the ICH Score (p=0.35). For non-transferred patients, the observed 30-day mortality was 45.6%, again similar to the expected mortality of 47.6% by ICH Score (p=0.13). Figure 3 illustrates the observed and expected 30-day mortality in transferred and non-transferred patients, distributed by ICH Score.
Figure 3.
Observed vs. Expected 30-Day Mortality by ICH Score
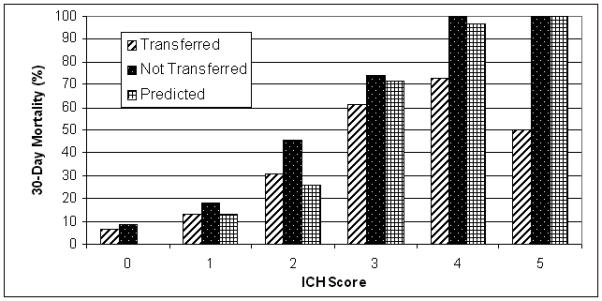
Using the ICH-GS, the observed 30-day mortality for all transferred patients of 32.5% was significantly lower than the expected mortality of 43.1% (p<0.001). The observed 30-day mortality of 45.6% for all non-transferred patients was lower than the expected mortality of 68.6% using the ICH-GS (p=0.002). Figure 4 illustrates the observed and expected 30-day mortality in transferred and non-transferred patients, distributed by ICH-GS.
Figure 4.
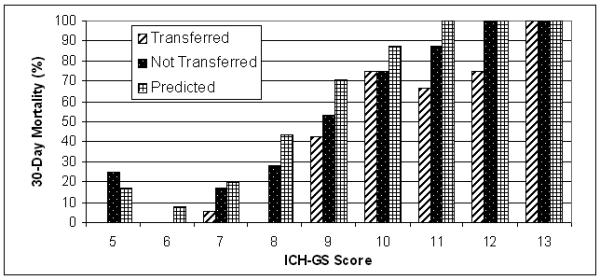
Observed vs. Expected 30-Day Mortality by ICH-GS
Discussion
We found that 93% (259/280) of ICH cases in our community in 2005 were first assessed in an ED, 79% (205/259) of these cases presented to a non-tertiary ED, and fewer than half (39%) of those patients were subsequently transferred to a tertiary center for continued care. Baseline function and black race were significantly associated with transfer to a tertiary center in multivariate modeling. The proportion of ICH patients who initially present to non-tertiary EDs, the proportion transferred to tertiary care centers, and factors associated with transfer have not been previously studied. The lower likelihood of transfer with poorer baseline function may be due to patient/family preference. Poorer function may also make it less likely for physicians to transfer patients for more aggressive care. While we are unable to definitively determine why black race was associated with a higher likelihood of transfer, it is possible that blacks in our community were more likely to seek higher level care.
We did not find a significant difference in 30-day mortality between transferred and non-transferred patients, although there was a trend toward higher mortality in non-transferred patients. Since poorer baseline function was associated with transfer, we compared mortality in transferred and non-transferred patients after stratifying by mRS. Mortality was lower in transferred patients with and without serious disability (Figure 1). This suggests the trend toward lower mortality in transferred compared with non-transferred patients was independent of baseline function. Well-recognized predictors of ICH mortality include age, GCS, ICH volume, IVH, hydrocephalus, and ICH location.1 Previous reports have suggested that care at tertiary centers and the availability of specialized neurocritical care may be associated with improved ICH survival.8, 10 This may account for the trend toward lower mortality in our transferred patients. The lack of a significant mortality benefit from transferring ICH patients to a tertiary center in our study may be due to sample size limitations and the similarities in ICH volume, location, IVH and hydrocephalus in transferred versus non-transferred patients (Table). Further, unaccounted confounders or a real lack of difference may also account for our findings.
We also found that the ICH Score adequately predicted 30-day mortality while the ICH-GS significantly overestimated short-term mortality in all patients in our cohort. This finding is consistent with a recent report that found an overestimation of mortality with the ICH-GS but not the ICH Score in 125 patients with ICH.11 Other published reports have validated the ICH Score as an accurate predictor of short-term ICH mortality,7, 12-14 while the ICH-GS is yet to be independently validated. On the other hand, Ruiz-Sandoval et al. found the ICH Score to be less accurate than the ICH-GS in predicting functional outcome in survivors of ICH.4 Thus, caution must be taken in utilizing these prediction tools in clinical decision making for the individual ICH patient in the ED.
A limitation of our study is the inability to assess the impact of withdrawal of care and/or patient or family preference on the decision to transfer ICH patients to tertiary centers. As depicted in Figure 2, early mortality was greater in non-transferred patients. Although withdrawal of care within 24 hours of symptom onset is contrary to current guidelines,1 patient/family decision regarding transfer for a higher level of care may prompt care limitation given a poor initial outlook. The fact that baseline function was significantly associated with transfer may reflect this, although there are limitations to our retrospective ascertainment of baseline function. We were also unable to evaluate functional outcomes in our cohort. While short-term mortality may be reduced by care at tertiary centers, no proven interventions are available to improve functional outcomes in ICH. Thus, it is unlikely that tertiary care center management in itself would improve outcomes among survivors. Nonetheless, future studies are planned to evaluate functional outcomes in ICH patients who receive care in tertiary and non-tertiary settings.
No clear delineation of tertiary versus non-tertiary hospitals exists. The centers we designated as tertiary centers received approximately 90% of ED ICH referrals in our region in 2005, serve as the primary referral centers for neurosurgical emergencies, and did not transfer acute ICH patients to other hospitals in the region. In the absence of other criteria, we believe these criteria constitute a reasonable definition of tertiary centers. A final limitation is that ED disposition of ICH patients in our community may not reflect practice patterns elsewhere, thereby limiting the generalizability of our findings. As mentioned above, we are unaware of other reports that discuss where most ICH patients initially present or the subsequent disposition of those patients from the ED. Practice patterns may vary locally and across the country. The 16 hospitals in our region belong to a variety of health systems and are served by at least six separate and independent practice groups of emergency physicians.
In summary, we found a non-significant trend toward higher mortality in non-transferred ICH patients, suggesting that further evaluation of ED disposition decisions for ICH patients is warranted. Expected ICH mortality may be overestimated by published tools for predicting ICH outcomes. Thus, caution must be taken in using these tools in clinical decision making. Future investigations are planned to determine the association of withdrawal of care decisions with ED disposition of ICH patients, to assess functional outcomes in patients who receive care in tertiary versus non-tertiary centers, and to clarify how race and baseline function may influence transfer decisions.
Acknowledgments
Supported by NINDS (R-01-NS 36695)
References
- 1.Broderick J, Connolly S, Feldmann E, et al. Guidelines for the management of spontaneous intracerebral hemorrhage in adults: 2007 update: a guideline from the American Heart Association/American Stroke Association Stroke Council, High Blood Pressure Research Council, and the Quality of Care and Outcomes in Research Interdisciplinary Working Group. Circulation. 2007;116(16):e391–413. doi: 10.1161/CIRCULATIONAHA.107.183689. [DOI] [PubMed] [Google Scholar]
- 2.Lloyd-Jones D, Adams R, Carnethon M, et al. Heart Disease and Stroke Statistics--2009 Update. A Report From the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2008 doi: 10.1161/CIRCULATIONAHA.108.191261. [DOI] [PubMed] [Google Scholar]
- 3.Hemphill JC, 3rd, Bonovich DC, Besmertis L, Manley GT, Johnston SC. The ICH score: a simple, reliable grading scale for intracerebral hemorrhage. Stroke; a journal of cerebral circulation. 2001;32(4):891–7. doi: 10.1161/01.str.32.4.891. [DOI] [PubMed] [Google Scholar]
- 4.Ruiz-Sandoval JL, Chiquete E, Romero-Vargas S, Padilla-Martinez JJ, Gonzalez-Cornejo S. Grading scale for prediction of outcome in primary intracerebral hemorrhages. Stroke; a journal of cerebral circulation. 2007;38(5):1641–4. doi: 10.1161/STROKEAHA.106.478222. [DOI] [PubMed] [Google Scholar]
- 5.Kothari RU, Brott T, Broderick JP, et al. The ABCs of measuring intracerebral hemorrhage volumes. Stroke; a journal of cerebral circulation. 1996;27(8):1304–5. doi: 10.1161/01.str.27.8.1304. [DOI] [PubMed] [Google Scholar]
- 6.Becker KJ, Baxter AB, Cohen WA, et al. Withdrawal of support in intracerebral hemorrhage may lead to self-fulfilling prophecies. Neurology. 2001;56(6):766–72. doi: 10.1212/wnl.56.6.766. [DOI] [PubMed] [Google Scholar]
- 7.Matchett SC, Castaldo J, Wasser TE, Baker K, Mathiesen C, Rodgers J. Predicting mortality after intracerebral hemorrhage: comparison of scoring systems and influence of withdrawal of care. J Stroke Cerebrovasc Dis. 2006;15(4):144–50. doi: 10.1016/j.jstrokecerebrovasdis.2006.03.006. [DOI] [PubMed] [Google Scholar]
- 8.Diringer MN, Edwards DF. Admission to a neurologic/neurosurgical intensive care unit is associated with reduced mortality rate after intracerebral hemorrhage. Critical care medicine. 2001;29(3):635–40. doi: 10.1097/00003246-200103000-00031. [DOI] [PubMed] [Google Scholar]
- 9.Woo D, Sauerbeck LR, Kissela BM, et al. Genetic and environmental risk factors for intracerebral hemorrhage: preliminary results of a population-based study. Stroke; a journal of cerebral circulation. 2002;33(5):1190–5. doi: 10.1161/01.str.0000014774.88027.22. [DOI] [PubMed] [Google Scholar]
- 10.Suarez JI, Zaidat OO, Suri MF, et al. Length of stay and mortality in neurocritically ill patients: impact of a specialized neurocritical care team. Critical care medicine. 2004;32(11):2311–7. doi: 10.1097/01.ccm.0000146132.29042.4c. [DOI] [PubMed] [Google Scholar]
- 11.Naval NS, Mirski MA, Carhuapoma JR. Impact of statins on validation of ICH mortality prediction models. Neurological research. 2008 doi: 10.1179/174313208X353686. [DOI] [PubMed] [Google Scholar]
- 12.Godoy DA, Pinero G, Di Napoli M. Predicting mortality in spontaneous intracerebral hemorrhage: can modification to original score improve the prediction? Stroke; a journal of cerebral circulation. 2006;37(4):1038–44. doi: 10.1161/01.STR.0000206441.79646.49. [DOI] [PubMed] [Google Scholar]
- 13.Godoy DA, Boccio A. ICH score in a rural village in the Republic of Argentina. Stroke; a journal of cerebral circulation. 2003;34(9):e150–1. doi: 10.1161/01.STR.0000089493.23505.CA. author reply e-1. [DOI] [PubMed] [Google Scholar]
- 14.Cheung RT, Zou LY. Use of the original, modified, or new intracerebral hemorrhage score to predict mortality and morbidity after intracerebral hemorrhage. Stroke; a journal of cerebral circulation. 2003;34(7):1717–22. doi: 10.1161/01.STR.0000078657.22835.B9. [DOI] [PubMed] [Google Scholar]