Breast cancer is the commonest form of cancer in women worldwide; there were an estimated 1.4 million cases worldwide in 2008 [1] and there is no part of the world where breast cancer is now a rare form of cancer [2]. In all major regions of the world, breast cancer is the commonest, or second commonest, cancer in women [3].
Focus on breast cancer up until now has almost entirely been on the situation in high-income, westernized, industrialised countries. However, there is a world out there outwith North America and Western Europe where cancer is a major and growing problem facing public health. With the growth and ageing of the world's population, notable increases in life expectancy in people of lower-income levels in many countries and the increased tendency to adopt a westernised lifestyle, cancer is a rapidly growing global problem [4] and not one that the majority of the world is ready to cope with.
Of course, in the above statements, 'cancer' could be replaced by 'vascular disease' or 'chronic obstructive pulmonary disease' or 'diabetes' or any number of chronic conditions associated with ageing populations adopting a westernised lifestyle.
Today, there is no population around the world with a truly low risk of breast cancer and no woman in the world at a truly low risk of developing the disease. The global burden of breast cancer doubled between 1975 and 2000. It seems certain to double again between now and 2030 and the great majority of this burden will fall on low-income and lower middle-income countries, where the resources to deal with the current situation, never mind future increases, are absent to a great degree.
Breast cancer in Africa
The widespread belief that breast and other cancers are rare in low-income regions such as Africa is a myth. Akarolo-Anthony and colleagues [5] note that the probability that a woman who lives to age 65 in Kampala (Uganda) would develop a cancer is only 20% lower than that of her European contemporary. What differs markedly is the probability that the African woman will live to be 65 years of age compared to women in developed countries. The concepts of risk and burden should be clearly differentiated and it should be noted that as life expectancy in Africa increases, so too will the cancer burden.
Akarolo-Anthony and colleagues [5] also note the increasing breast cancer rates occurring in Africa. Many factors could be associated with this increase but it appears attributable to a mixture of earlier age at menarche, women having fewer children and having their first child at a later age, a reduction in the total time spent breast feeding, increased body mass index and a reduction in physical activity. Prospects for prevention through lifestyle alterations appear limited to increasing breast feeding, weight control and increasing levels of physical activity. There are proven chemoprevention approaches [6] but these have not been widely adopted even in high-resource countries.
In these lower-income settings, the case fatality rate is poor in comparison to high-resource countries. Women with breast cancer either present with large, advanced tumours or do not present until the disease is at an incurable stage. Of course, women still die from breast cancer in such countries without ever coming into contact with medical services. The stigma associated with breast cancer in many countries is a major impediment to progress in controlling the disease and it should be a priority to reduce this stigma and eventually eliminate it entirely. Such stigma existed until recent decades even in countries such as the United States, but much work has been done to gradually overcome this phenomenon (see [7] for a clear description of this in the United States in the 1960s).
In lower-resource settings, treatment facilities, professional expertise and modern therapeutic technologies frequently do not exist. Howell [8] has summarised some of the difficulties associated with introducing optimal treatment for breast cancer, as defined by standards in high-income countries, in the developing world, high-lighted by the absence or low frequency of radiotherapy and systemic therapy services. In Africa, for example, a survey demonstrated that radiotherapy services were available in only 17 of 44 countries surveyed [9]. The Breast Health Global Initiative guidelines for the introduction of radiation therapy suggest the cheaper and simpler cobalt machines compared with linear accelerators or shorter schedules [10]. Not only are cobalt machines cheaper, but they are practical given the absence of reliable electricity supplies in many lower resource settings.
Modern, curative treatments and treatment facilities are not generally available, and pain control, palliative, supportive and terminal care are notoriously absent. There are 29 countries identified in Africa where the importation of opioid drugs is prohibited, and in many others the dosage administered varies 100-fold [11]. Merriman [12] describes the situation on the ground in Africa and presents a viable model for improving this situation in an effective and inexpensive manner.
Breast cancer in India
In India, there are remarkable differences between the incidence rates of breast cancer in metropolitan, urban and rural areas. Using age-standardised incidence rates for the years 2006 to 2008, the recent provisional report of the National Cancer Incidence Programme (NCRP, unpublished data) provides reliable information on cancer incidence in many parts of India. In the greater metropolitan areas of Mumbai and Chennai, the breast cancer incidence rates are 33 and 32.1 per 100,000, respectively; in the urban areas of Pune and Bhopal, the incidence rates are lower at 24.4 and 25.5 per 100,000, respectively; and in the rural areas of Barshi and Barshi Town the rates are lower still at 7.7 and 15.0 per 100,000, respectively.
The situation of breast cancer in India is, in a certain sense, fairly typical of the situation in many countries of Asia and other regions where dramatic economic and social change is taking place. Breast cancer is the second most common cancer among women in India and accounts for 7% of global burden of breast cancer and one-fifth of all cancers among women in India. Over 90,000 new cancer cases are estimated to occur this year and over 50,000 women are estimated to die of it annually in India [1]. It is the number one cancer among women in urban areas of India. The incidence of breast cancer is approximately three times higher in urban areas compared to rural areas.
The age-standardised incidence rates of breast cancer in India are still much lower than in high-resource countries (Figure 1). Given the myriad factors affecting the incidence of breast cancer, including the aging and growth of the Indian population and the increasing trends in breast cancer incidence, NS Murthy of the Indian Medical Research Council has estimated that the breast cancer burden in India will grow from 80,000 in 2005, through 122,000 new cases in 2011, and attain a level of 141,000 cases by 2016 (R Badwe, personal communication).
Figure 1.
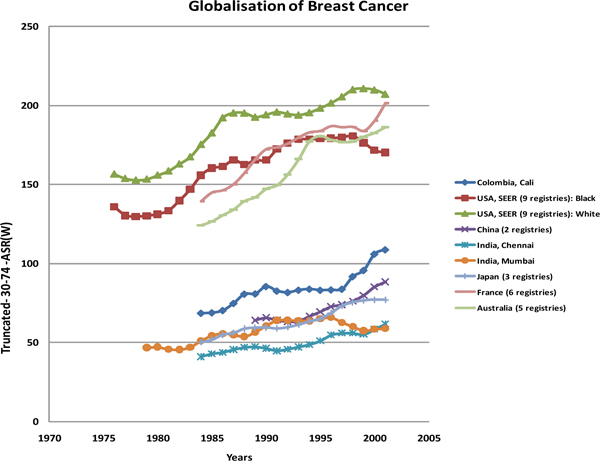
Globalissation of breast cancer. Average, annual age-standardised truncated (age 30 to 74 years) breast cancer incidence rates (1975 onwards) in Mumbai and Chennai (India), China (Hong Kong and Shanghai), Colombia (Cali), Japan (Miyagi, Osaka, Yamagata), France (Bas Rhin, Calvados, Doubs, Isere, Somme, Tarn), Australia (New South Wales, South Australia, Victoria, Tasmania, Western Australia) and of whites and blacks in the United States Surveillance, Epidemiology and End Results (SEER) Program (Atlanta, Connecticut, Detroit, Hawaii, Iowa, New Mexico, San Francisco-Oakland, Seattle-Puget Sound, Utah).
India, typical of many countries undergoing rapid economic evolution, and a special case in many respects because of the large size of its population, requires investment in prevention, diagnosis and treatment. These include the widespread availability of reliable hormone receptor assessment, the availability of affordable drugs (for example, tamoxifen at US$1 per month and anthra-cyclines at US$25 per cycle), cost-effective early detection models and programmes, low-cost intervention to improve outcome in spite late presentation, and effective population prevention interventions, including increasing breast feeding, reducing overweight and obesity and increasing physical activity.
Conclusions: do it rather than talk about it
One of the major barriers to progress in low-income and lower middle-income countries was the failure to mention cancer and other chronic diseases in the Millennium Development Goals [4]. Signed and approved by most of the heads of state or government at the United Nations, these ten points were designed to help the 1 billion poorest people on the planet. Governments and health departments strive to accomplish these goals and one consequence is the lower priority currently afforded to chronic disease in some of the world's poorest countries.
The growing epidemic of breast cancer in lower resource settings presents a major challenge to global public health, especially given the failure to cope with the current situation. This epidemic is here and now confronting the cancer control community and will assuredly become worse.
What can be done about this? The first and crucial step must be to turn this question from the passive to the active voice. What can we do about this? Not your neighbour, not your cancer organisation or the cancer organisation in another country, nor some international association. Responsibility cannot be shifted onto the shoulders of others. The cancer control community needs to take more responsibility. Too often too diffuse to be effective, this community needs to gain focus and acquire strong leadership. The time for committees, meetings, reports and declarations is over and the need for real and effective action is a call that must not be ignored.
Currently, a clearer picture of the global issues of cancer is emerging and clear priority targets can be identified. Individually, we must get involved, and collectively, we can make a difference.
There is an urgent need to enact effective cancer control policies in many parts of the world and the urgency is emphasised by the rapid changes taking place in cancer risk and cancer burden, particularly in lower and middle income countries. Breast cancer, being such a common form of the disease, is a good model for what can be done and what should be done. Two examples illustrate key elements of what is needed. The Breast Health Global Initiative [13] seeks to improve diagnosis, treatment and outcome through a highly successful, hands-on programme of scientific and clinical activities. The Susan G Komen Global Alliance, building on the great success of Susan G Komen for the Cure, is spearheading a coalition whose aim is to take active steps to reduce the breast cancer burden, and that of other cancers, among women living in poor regions of the world. The Alliance serves as a platform for innovative partnerships to provide screening and treatment to low-resource, under-served global populations and also as an organizing platform to bring together various organizations to design, fund and implement health programs that include screening and/or treatment for breast and cervical cancer.
Benjamin Disraeli and William Gladstone were two legendary British politicians and political rivals in the late 1800 s. In Parliament, Disraeli was requested to differentiate a tragedy and a calamity. He responded that if Mr Gladstone was to fall in the Thames, then that could be described as a tragedy. If someone was to pull him out, then that would be a calamity.
The impact of the current and future global cancer burden can be described as a tragedy. If we fail to do anything about this evolving epidemic, then that would be a calamity.
Competing interests
The author declares that he has no competing interests.
Acknowledgements
Details of the situation in India are a result of the work of Professor Rajendra Badwe and this is duly acknowledged.
This article has been published as part of Breast Cancer Research Volume 12 Supplement 4, 2010: Controversies in Breast Cancer 2010. The full contents of the supplement are available online at http://breast-cancer-research.com/supplements/12/S4
References
- Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010. in press . [DOI] [PubMed]
- Curado MP, Edwards BK, Shin HR, Storm HH, Heanue M, Ferlay J, Boyle P. Cancer Incidence in Five Continents. Vol. 9. Lyon, France: IARC Press; 2007. [IARC Scientific Publications, no. 160] [Google Scholar]
- Boyle P, Levin B. World Cancer Report 2008. Lyon, France: IARC Press; 2008. [Google Scholar]
- Boyle P. The globalisation of cancer. Lancet. 2006;368:629–630. doi: 10.1016/S0140-6736(06)69225-8. [DOI] [PubMed] [Google Scholar]
- Akarolo-Anthony SN, Ogundiran TO, Adebamowo CA. Emerging breast cancer epidemic: evidence from Africa. Breast Cancer Research. 2010;12(Suppl 4):S8. doi: 10.1186/bcr2737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuzick J. Breast cancer prevention in the developing world. Breast Cancer Research. 2010;12(Suppl 4):S9. doi: 10.1186/bcr2738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brinker NG. Promise Me. New York, NY: Broadway Books; 2010. [Google Scholar]
- Howell A. The emerging breast cancer epidemic: early diagnosis and treatment. Breast Cancer Research. 2010;12(Suppl 4):S10. doi: 10.1186/bcr2739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barton MB, Frommer M, Shafiq J. Role of radiotherapy in cancer control in low-income and middle-income countries. Lancet Oncol. 2006;7:584–595. doi: 10.1016/S1470-2045(06)70759-8. [DOI] [PubMed] [Google Scholar]
- Eniu A, Carlson RW, El Saghir NS, Bines J, Bese NS, Vorobiof D, Masettie R, Anderson BO. Guideline implementation for breast healthcare in low and middle income countries: treatment resource allocation. Cancer. 2008;113:2269–2281. doi: 10.1002/cncr.23843. [DOI] [PubMed] [Google Scholar]
- International Narcotics Control Board. Narcotic Drugs: Estimated World Requirements for 2004. Statistics for 2002. New York: United Nations; 2004. [Google Scholar]
- Merriman A. Emerging breast cancer epidemic: impact on palliative care. Breast Cancer Research. 2010;12(Suppl 4):S11. doi: 10.1186/bcr2740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson BO, Yip C-H, Smith RA, Shyyan R, Sener SF, Eniu A, Carlson RW, Azavedo E, Harford J. Guideline implementation for breast healthcare in low-income and middle-income countries. Cancer. 2008;113(Suppl):2221–2243. doi: 10.1002/cncr.23844. [DOI] [PubMed] [Google Scholar]


