Abstract
OBJECTIVES
Obesity and morbid obesity have been shown to increase wound infections and occasionally mortality after many surgical procedures. Little is known about the relative impact of body mass index on these outcomes after open (OAR) and endovascular abdominal aortic aneurysm repair (EVAR).
METHODS
The 2005–2007 National Surgical Quality Improvement Program (NSQIP), a multi-institutional risk-adjusted database, was retrospectively queried to compare perioperative mortality (in-hospital or 30-day) and postoperative wound infections after OAR and EVAR. Patient demographics, comorbidities, and operative details were analyzed. Body mass index (BMI) was calculated from height and weight variables and definitions of obesity and morbid obesity were defined as BMI > 30kg/m2 and BMI > 40kg/m2 respectively. Student's T-test, Wilcoxon Rank Sum, Chi-square, and multivariate logistic regression were used to compare outcomes.
RESULTS
There were 2,097 OAR and 3,358 EVAR. Compared to EVAR, OAR patients were younger, more likely to be female (26% vs. 17%, P < .001), and less obese (27% vs. 32%, P < .001). Mortality was 3.7% vs. 1.2% after OAR vs. EVAR respectively (RR 3.1, P < .001) and overall morbidity was 28% vs. 12% (RR 2.3, P < .001). Morbidly obese patients had a higher mortality for both OAR (7.3%) and EVAR (2.4%) than obese patients (3.9% OAR; 1.5% EVAR) or non-obese patients (3.7% OAR; 1.1% EVAR). Obese patients had a higher rate of wound infection vs. non-obese after open repair (6.3% vs. 2.4%, P < .001) and EVAR (3.3% vs. 1.5%, P < .001). Morbid obesity predicted mortality after OAR but not EVAR and obesity was an independent predictor of wound infection after OAR and EVAR.
CONCLUSIONS
Morbid obesity confers a worse outcome for mortality after AAA repair. Obesity is also a risk factor for infectious complications after OAR and EVAR. Obese patients and particularly morbidly obese patients should be treated with EVAR when anatomically feasible.
Introduction
As the obesity epidemic in the United States continues to grow, the effect that this may have upon medical outcomes must be considered.1 It has been associated with increased prevalence of morbidity and infectious complications following cardiac and general surgical operations, however, the impact of obesity or body mass index upon perioperative mortality is less definitive.2–5 A few studies have shown a significant increase in mortality in obese patients, but many large studies have failed to find significant relationships.2–5 In fact, being underweight but not overweight has been associated with increased mortality in some studies.5
The impact of body mass index upon vascular procedures is even less well known.6–10 In lower extremity bypass, obesity has been associated with greater wound complications but not mortality.6–7 With the increasing use of endovascular techniques, there is a question of how obesity impacts morbidity and mortality with both open vascular and endovascular procedures. Endovascular aortic aneurysm repair (EVAR), as compared to its open surgical counterpart, avoids a large retroperitoneal or transperitoneal incision. The groin incisions required to expose the femoral arteries for EVAR are even being replaced by totally percutaneous techniques in many patients.11,12 Wound complications may be reduced with this trend toward smaller incisions, but even percutaneous access has been found to have higher complication rates in morbid obesity.11 Additionally, obesity, may result in increased wound infections regardless of repair method.
Most large databases do not include adequate information to evaluate obesity as a predictor for morbidity or mortality. The American College of Surgeons National Surgical Quality Improvement Program (NSQIP), however, contains height and weight variables as well as detailed 30 day outcomes including wound infections and a number of other postoperative complications which make it ideally suited for this purpose.13 We used the NSQIP database to assess the impact of body mass index on perioperative mortality and morbidity with specific attention to surgical site infections after open abdominal aortic aneurysm repair and EVAR.
Methods
Database
We reviewed the data within the NSQIP database from 2005–2007. This database is a national, prospective, risk-adjusted database including data from over 200 participating community and academic medical centers throughout the United States.12 Commensurate with each center's overall case volume, all or a randomly selected proportion of procedures are prospectively selected for analysis. Trained clinical nurses review prosepectively recorded data and patient information. A comprehensive list of preoperative comorbidies are collected, along with operative and perioperative variables and the primary surgeons specialty. 30-day postoperative outcomes are collected including hospital course, re-hospitalization and reoperation data, postoperative clinic visits, and/or follow-up phone contact.
Data Analysis
The NSQIP database was queried using SAS statistical software (Version 9.1, SAS Institute Inc., Cary, NC) for elective open and endovascular abdominal aortic aneurysm repairs as identified by Current Procedural Terminology, 4th edition (CPT-4) procedural coding combined with International Classification of Diseases, 9th edition (ICD-9) diagnosis coding. Ruptured aneurysms, thoracic and thoracoabdominal aneurysms, and aortic dissections were excluded. Patients unresponsive on initial hospital arrival or those requiring mechanical ventilation within 48 hours prior to surgery were excluded for the purposes of this study as they may have represented incorrectly identified ruptured aneurysms..Patients undergoing open conversion following attempted EVAR were excluded from analysis as well.
Preoperative demographic and comorbidity variables were recorded for each patient. Weight classification was assigned based upon BMI and the NIH definitions of underweight (BMI ≤18.6 kg/m2), normal weight (18.7–25 kg/m2), overweight (25.1–30 kg/m2), obese class I (30.1–35 kg/m2), obese class II (35.1–40 kg/m2), and obese class III (>40 kg/m2). Obesity overall includes obese class I through III and the subset of obese class III was often considered separately and referred to as morbid obesity. Renal disease was defined as hemodialysis dependence or a preoperative serum creatinine >1.8mg/dl. Angina and congestive heart failure comorbidity definitions required active symptoms within 30 days pre-admission. Intraoperative outcome variables included blood transfusion volume (units), operative time (hours), and intraoperative complications (cardiac arrest, myocardial infarction, or unplanned intubation). Thirty day postoperative events included mortality, surgical site infection (superficial, deep, or organ space infection), wound dehiscence, graft failure, subsequent major operation, and 13 other NSQIP-defined complications. Graft failure was defined by NSQIP as “mechanical graft failure requiring return to the operating room, interventional radiology, or balloon angioplasty.” Hospital length of stay was also measured.
Statistical Analysis
Statistical analysis was performed using STATA statistical software (College Station, TX: StataCorp LP). Statistical significance was defined as P <.05. Demographics, comorbidities, and perioperative events and outcomes were compared between OAR and EVAR cohorts. Categorical variables were analyzed using Chi-square or Fischer's Exact tests and continuous variables were compared using Student's T-test for parametric data or Wilcoxon Rank Sum test for nonparametric data. Preoperative predictors of wound infection, overall morbidity, and mortality were analyzed by univariate and multivariate logistic regression with backwards selection. For postoperative events, a univariate analysis of mortality was performed.
Results
There were a total of 2,097 OARs (38.4%) and 3,358 EVARs (61.6%) performed within the time period. The proportion of EVAR increased from 2005 (57.6%) to 2007 (64.2%). Ninety-seven percent of procedures, both EVAR and OAR, were performed by vascular surgeons.
Demographics and Comorbidities
Patient variables are detailed in Table I. EVAR patients were older and included significantly more octogenarians. EVAR patients were more frequently male. Race was equivalent. Of comorbidities, patients undergoing EVAR had higher rates of congestive heart failure, diabetes mellitus, obesity class I and II, and chronic steroid use. Open repair patients had higher rates of hypertension, rest pain or gangrene, current smoking, and significant alcohol use.
Table I.
Baseline Characteristics of Patients Undergoing Endovascular or Open Repair of Abdominal Aortic Aneurysms in 2005–2007.
| Open Repair (N=2,097) | Endovascular Repair (N=3,358) | P-value | |
|---|---|---|---|
| Age, mean +/- SD | 71.5 +/- 8.5 | 74.1 +/- 8.4 | <.001 |
| <60 years | 10.0% | 6.5% | <.001 |
| 61–70 years | 32.8% | 24.9% | <.001 |
| 71–80 years | 43.6% | 44.4% | .56 |
| >80 years | 13.6% | 24.2% | <.001 |
| Female | 26.2% | 17.2% | <.001 |
| Black or Other Race (vs. White) | 7.0% | 7.4% | .55 |
| Admission from | |||
| Home | 96.5% | 98.3% | <.001 |
| Acute Care | 3.5% | 1.7% | <.001 |
| Comorbidities | |||
| Obese | 27.1% | 31.7% | <.001 |
| Weight Classifications by BMI | |||
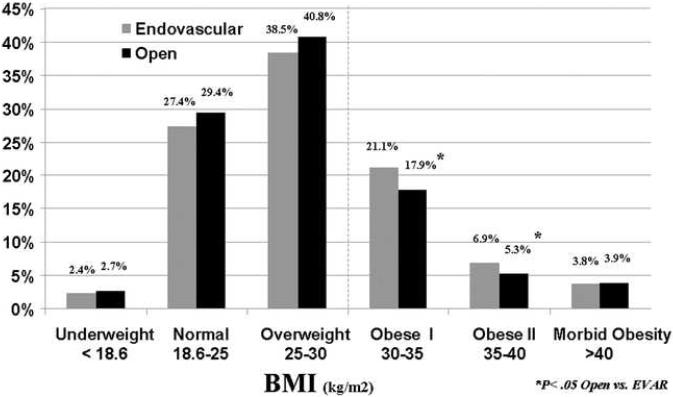
| Underweight: < 18.6kg/m2 | 2.7% | 2.4% | .51 |
| Normal Weight: 18.6–25kg/m2 | 29.4% | 27.4% | .11 |
| Overweight: 25–30kg/m2 | 40.8% | 38.5% | .09 |
| Obese I:30–35kg/m2 | 17.9% | 21.1% | <.01 |
| Obese II: 35–40kg/m2 | 5.3% | 6.9% | <.05 |
| Morbid Obesity: ≥ 40kg/m2 | 3.9% | 3.8% | .84 |
| Renal Disease | 9.3% | 8.6% | .36 |
| Dialysis Dependent End Stage Renal Disease | 0.6% | 1.0% | .12 |
| Chronic Renal Insufficiency (Creatinine>1.8mg/dl) | 9.3% | 8.5% | .33 |
| Cardiac Disease | 39.0% | 40.9% | .17 |
| Previous Cardiac Surgery | 24.9% | 25.4% | .66 |
| Previous Percutaneous Cardiac Intervention | 19.5% | 20.2% | .53 |
| Prior Myocardial Infarction (Within 6 Months) | 1.7% | 1.2% | .21 |
| Angina (Within 30 Days) | 2.2% | 2.2% | .98 |
| Congestive Heart Failure (Within 30 Days) | 0.8% | 1.4% | <.05 |
| Prior Surgery for PVD (PTA/Stent, BPG, or Amputation) | 5.6% | 5.6% | .92 |
| PVD with Rest Pain or Tissue Loss | 1.8% | 0.9% | <.01 |
| Cerebrovascular Disease | 14.9% | 14.6% | .78 |
| Hypertension | 83.3% | 78.5% | <.001 |
| Diabetes Mellitus (Oral Medication or Insulin) | 11.5% | 14.4% | <.01 |
| Insulin Controlled | 1.9% | 2.6% | .12 |
| Oral Medication Controlled | 9.6% | 11.8% | <.01 |
| Chronic Obstructive Pulmonary Disease | 18.4% | 19.0% | .58 |
| Chronic Steroid Use | 3.1% | 4.1% | <.05 |
| Weight Loss (>10% Within 6 Months) | 2.3% | 2.0% | .46 |
| Poor Functional Status Prior to Surgery | 4.8% | 4.3% | .42 |
| Current Smoker (Within 1 Year) | 41.5% | 28.7% | <.001 |
| Alcohol (> 2 Drinks per Day Within past 2 Weeks) | 5.4% | 4.2% | <.05 |
| Pre-operative Transfusion >4 Units | 0.05% | 0.03% | .74 |
| Pre-operative wound | 1.2% | 1.2% | .96 |
| Pre-operative Acute Renal Failure | 0.2% | 0.2% | .87 |
| Sepsis | 2.2% | 1.6% | .12 |
BMI Body Mass Index
PVD Peripheral Vascular Disease
PTA Percutaneous Transluminal Angioplasty
BPG Bypass Graft
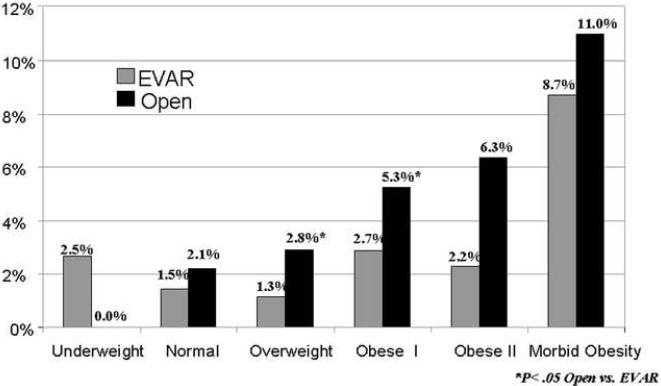
When the distribution of BMI was compared by repair method as shown in Figure 1, obese class I and obese class II patients were more likely to have EVAR performed than OAR. In comparison, open repair was utilized more frequently in underweight, normal weight, overweight, and morbidly obese patients although the differences lacked statistical significance. There were no differences in pre-operative incidences of wound infection or sepsis. (Table I)
Figure 1.
Weight Class Categorization of Patients Undergoing Endovascular or Open Repair of Abdominal Aortic Aneurysms in 2005–2007.
Intraoperative Variables
General anesthesia was nearly always used for OAR (98%) while it was used in only 77% of EVAR cases (P < .001). Median operative times (3.6 hours vs. 2.5 hours, P < .001) and blood transfusion requirements (2 units vs. 0 units, P < .001) were higher for OAR compared to EVAR. Intraoperative complications were rare in both repairs (0.5% versus 0.3%, P = .40).
Mortality and Morbidity
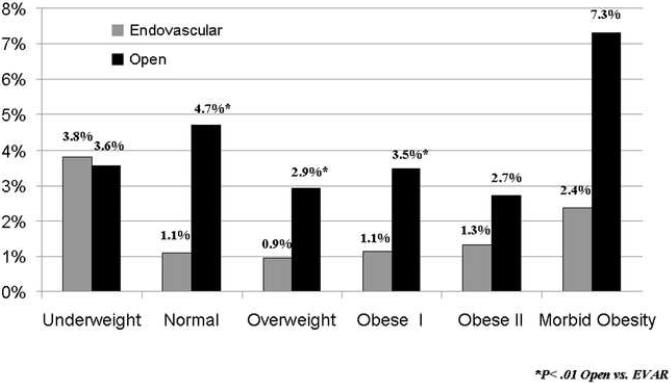
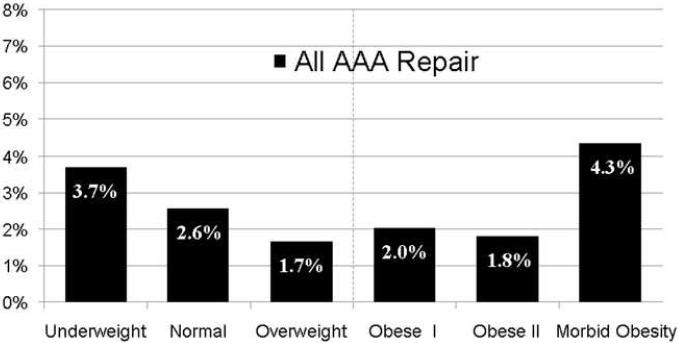
Mortality was 3.7% after OAR and 1.2% after EVAR (P < .001). Overall AAA mortality for both repair types combined showed a U-shaped distribution (Figure 2A). There was a higher mortality at the extremes of weight, underweight (3.7%) and morbidly obese patients (4.3%), compared to the remaining weight classifications which had a combined mortality of 2.1% (P < .01 amd P < .01). Comparing OAR and EVAR individually by weight class, mortality after OAR was nearly twice as high in morbidly obese patients (7.3%) compared to other OAR weight categories (P = .08) and nearly three times as high as similarly obese EVAR patients (P = .09) although not statistically significant (Figure 2B). For underweight OAR patients, the effect of BMI <18 was not as apparent with mortality comparable to the OAR group as a whole (3.6% vs 3.7%, P = .95). The highest mortality for EVAR was seen in the underweight population (3.8%, >3 times the overall EVAR risk, P < .05) whilethe morbidly obese group also had a trend of higher mortality (2.4%, 2 times the overall EVAR risk, P = .20). For all weight classifications other than underweight, mortality after EVAR was less than half of the mortality after OAR (Figure 2a). For underweight EVAR patients this EVAR mortality benefit was negated with similar mortality rates to OAR (3.6% OAR vs. EVAR 3.8%, P = 0.95).
Figure 2.
Mortality by BMI Classification for Patients Undergoing Endovascular or Open Repair of Abdominal Aortic Aneurysms in 2005–2007. A) All AAA Repair. B) EVAR vs. Open Repair.
Overall morbidity was 28% after OAR and 12% after EVAR (P < .001) with subsequent major operation, pneumonia, reintubation, and septic shock being the most frequent complications. Subsequent major operations within 30 days were performed in 8% of OAR cases and 5% of EVAR cases (P < .001). Graft failure with need for reintervention was seen in 1% of patients with a mean time to graft failure of 5.2 days after OAR versus 8.5 days after EVAR (P < .05). EVAR morbidity across weight classifications showed slightly higher rates at the extremes of weight strata (P < .05 overall) with the most significant difference in underweight patients (21.5% vs. 11.9%, P < .01). OAR morbidity was highest in the underweight category (43%, P < .05) and similar amongst the remaining BMI classes (Figure 3). Comparing obese to non-obese patients, morbidity was similar (19% vs 18%, P = .48).
Figure 3.
Morbidity by BMI Classification for Patients Undergoing Endovascular or Open Repair of Abdominal Aortic Aneurysms in 2005–2007.
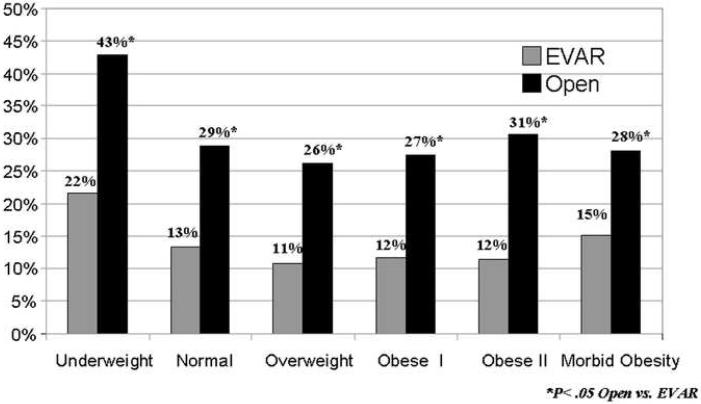
As a subset of morbidity, surgical site infections occurred in 4% of open cases and 2% of EVAR (P < .01). Obese (Class I, II, and morbidly obese) patients had an increased prevalence of surgical site infections for all AAA repair (4.4% vs. 1.9%, P < .001) as well as the subsets of OAR (6.3% VS 2.4%, P < .001) and EVAR (3.3% vs 1.5%, P < .001). There was an increasing prevalence of surgical site infections with increasing BMI in OAR patients (Figure 4). For all AAA repair, surgical site infections were associated with a longer median length of stay (7 versus 4 days, P < .001), a greater likelihood of subsequent major operation (32% versus 5%, P < .001), and a higher rate of graft failure (8% versus 1%, P < .001). Surgical site infections were also associated with an increased mortality in open repair (OR 3.4, 95%CI 1.6–7.4, P < .01). There were no patients with postoperative wound infections after EVAR that died. Wound infection was associated with early graft failure after both OAR (OR 12.9, 95%CI 4.8–34.5, P < .001) and EVAR (OR 7.3, 95%CI 2.8–19.2, P < .001) as well as with return to the OR within 30 days for OAR (OR 9.0, 95%CI 5.5–14.8, P < .001) and EVAR (OR 6.3, 95%CI 3.5–11.5, P < .001).
Figure 4.
Surgical Site Infections by BMI Classification for Patients Undergoing Endovascular or Open Repair of Abdominal Aortic Aneurysms in 2005–2007.
Predictors of Mortality
Multivariate predictors of OAR mortality were increasing age, chronic steroid use, peripheral vascular disease with prior surgery or intervention (PVD), cardiac disease, renal disease, and morbid obesity (compared to normal and mildly overweight patients) (Table IIa). In the male-only population, morbid obesity carried a similar risk with an odds ratio of 2.6 (P < .05). Significant predictors of EVAR mortality were cardiac disease, and female gender (Table IIb). Underweight BMI classification nearly reached significance after adjustment for other factors with an OR of 3.5 (P =.052). In the subset of males only, underweight patients as a similarly increased risk of mortality (OR 3.6, P < .05). Analyzing all AAA repairs combined, predictors of mortality were open repair (OR 3.7), increasing age(1.3), cardiac disease (2.0), chronic steroid use(2.9), PVD(2.3), renal disease(1.9), female gender (1.6), and morbid obesity (2.2) (P< .001).
Table II.
Multivariate Predictors of Mortality after Open and Endovascular AAA Repair NSQIP 2005–2007.
| A) Multivariate Predictors of Mortality after Open AAA Repair | |||
|---|---|---|---|
| OR | 95% CI | P Value | |
| Age (per decade) | 1.3 | 1.2–1.6 | <.001 |
| Chronic Steroid Use | 3.9 | 1.7–9.0 | <.01 |
| PVD with Prior Surgery | 3.0 | 1.5–6.2 | <.01 |
| Cardiac Disease | 2.0 | 1.2–3.2 | <.01 |
| Renal Disease | 2.0 | 1.1–3.7 | <.05 |
| Weight Class (vs. Normal/Overweight:BMI 18.6–30kg/m2) | |||
| Underweight BMI < 18.6kg/m2 | 0.9 | 0.2–3.8 | .85 |
| Obese I: BMI 30–35kg/m2 | 1.0 | 0.6–1.9 | .90 |
| Obese II: BMI 35–40kg/m2 | 1.0 | 0.3–3.0 | .88 |
| Morbid Obesity: BMI ≥ 40kg/m2 | 2.6 | 1.04–6.3 | <.05 |
| B) Multivariate Predictors of Mortality after Endovascular AAA Repair | |||
|---|---|---|---|
| OR | 95% CI | P Value | |
| Age (per decade) | 1.2 | .99–1.5 | .06 |
| Female Gender | 2.7 | 14–5.4 | <.01 |
| Cardiac Disease | 2.0 | 1.04–3.8 | <.05 |
| Weight Class (vs. Normal/Overweight:BMI 18.6–30kg/m2) | |||
| Underweight BMI < 18.6kg/m2 | 3.5 | .99–12.1 | .052 |
| Obese I: BMI 30–35kg/m2 | 1.3 | 0.6–3.0 | .52 |
| Obese II: BMI 35–40kg/m2 | 1.4 | 0.4–5.2 | .50 |
| Morbid Obesity: BMI ≥ 40kg/m2 | 2.5 | 0.7–8.5 | .13 |
PVD Peripheral Vascular Disease
BMI Body Mass Index
Predictors of Morbidity
Overall morbidity was predicted by open repair, increasing age, chronic steroid use, renal disease, PVD, female gender, cardiac disease, and underweight classification (Table III).
Table III.
Multivariate Predictors of Overall Morbidity and Surgical Site Infections after Endovascular and Open AAA Repair NSQIP 2005–2007.
| A) Multivariate Predictors of Morbidity after Open and Endovascular AAA Repair | |||
|---|---|---|---|
| OR | 95% CI | P Value | |
| Age (per decade) | 1.1 | 1.1–1.2 | <.001 |
| Open Repair | 3.0 | 2.6–3.5 | <.001 |
| Chronic Steroid Use | 1.8 | 1.3–2.6 | <.001 |
| Renal Disease | 1.5 | 1.2–1.9 | <.001 |
| PVD with Prior Surgery | 1.6 | 1.2–2.1 | <.01 |
| Female Gender | 1.3 | 1.1–1.5 | <.01 |
| Cardiac Disease | 1.2 | 1.04–1.4 | <.05 |
| Weight Class (vs. Normal/Overweight:BMI 18.6–30kg/m2) | |||
| Underweight BMI < 18.6kg/m2 | 1.9 | 1.3–2.8 | <.01 |
| Obese I: BMI 30–35kg/m2 | 1.1 | 0.9–1.3 | .46 |
| Obese II: BMI 35–40kg/m2 | 1.2 | 0.9–1.6 | .30 |
| Morbid Obesity: BMI ≥ 40kg/m2 | 1.2 | 0.8–1.7 | .40 |
| B) Multivariate Predictors of Surgical Site Infection after Open and Endovascular AAA Repair | |||
|---|---|---|---|
| OR | 95% CI | P Value | |
| Age (per decade) | 1.0 | .9–1.1 | .47 |
| Open Repair | 1.7 | 1.2–2.4 | <.01 |
| Renal Disease | 1.9 | 1.2–3.0 | <.01 |
| Chronic Steroid Use | 2.0 | 1.01–3.9 | <.05 |
| Female Gender | 1.6 | 1.01–2.2 | <.05 |
| Weight Class (vs. Normal/Overweight:BMI 18.6–30kg/m2) | |||
| Underweight BMI < 18.6kg/m2 | 0.7 | 0.2–3.0 | .65 |
| Obese I: BMI 30–35kg/m2 | 2.1 | 1.4–3.2 | <.001 |
| Obese II: BMI 35–40kg/m2 | 2.0 | 1.1–3.8 | <.05 |
| Morbid Obesity: BMI ≥ 40kg/m2 | 5.2 | 3.1–8.8 | <.001 |
PVD Peripheral Vascular Disease
BMI Body Mass Index
Predictors of Wound Infection
Multivariate predictors of postoperative surgical site infection were open repair, chronic steroid use, female gender, and obesity (Class I, II, and morbid obesity) (Table III). Morbid obesity was associated with a greater than 5 fold increased risk of surgical site infection.
Discussion
Over 20% of the US population is considered obese and the rates are consistently increasing.1 Smaller studies of vascular procedures have not shown a significant relationship with obesity and mortality.6,8 Infectious complications however, have been more reliably linked to obesity.6,14 Stratification by BMI classification is also an important and novel feature of the current analysis for AAA repair outcomes.
This study demonstrates that perioperative mortality for AAA repair varies by weight classification with an overall U-shaped distribution where patients at weight extremes (underweight or morbidly obese) fare the worst. The differences gained statistical significance however must be interpreted with caution as there were few patients at the extremes of weight. Interestingly, for underweight patients there is a lack of mortality benefit with EVAR compared to OAR.
Mullen et al. found an increased risk of death within underweight patients after surgical oncology procedures. Other BMI classes were not at an increased risk.2 Our institution has previously shown that obesity was unrelated to mortality after lower extremity bypass procedures.6 More recently, however, we have shown using the NSQIP database, that a similar U-shaped distribution exists for mortality after lower extremity bypass when patients are characterized by BMI classification rather than as a dichotomous obesity variable.15 A European study looking at a decade of elective and emergent vascular procedures including AAA repair found that obesity was not associated with an increased risk of mortality.14 In our analysis, among open repair patients, morbidly obese patients were at a 2.6 fold higher risk of mortality. In contrast, for those undergoing EVAR, underweight patients had a 3.5 fold increased risk of mortality that was just shy of statistical significance. There was a trend for morbidly obese patients undergoing EVAR to also have an increased risk of mortality (OR 2.5, P = .13). For the combined measure of all AAA repair, morbid obesity remains a strong mortality predictor.
Johnson et al. recently examined obesity related outcomes after open repair and EVAR from over two thousand patients undergoing open AAA repair and EVAR from the Veterans Affairs NSQIP 2004 and 2005. They found no difference in 30-day mortality between overweight and normal-weight patients. The authors were able to examine long-term outcomes and also found no significant differences among weight classifications for mortality at 2-years, however, found that the relative benefit of EVAR compared to open repair was increased in obese patients from a 47% relative risk reduction compared to 18% in non-obese patients. Their study group was predominately male patients (99%) and the underweight patients had to be excluded as only 0.3% had a BMI < 18.5.16 Given these differences, therefore, it is difficult to draw comparisons to our current study population. When we further examined our study population excluding females, the conclusions were similar however. Further studies examining the role of gender in AAA outcomes with obesity may be indicated based upon these two study findings however. Medical comorbidities that were predictors of mortality that were shown in this study are consistent with prior studies evaluating AAA repair.17–19
Overall morbidity after EVAR shows a U-shaped distribution among weight classes while after OAR the highest morbidity is in the underweight category and other weight classes range from 26% to 31%. Within general surgery operations Mullen et al. found an increased risk of morbidity for obese class I and II patients whereas underweight patients were not at increased risk.2 Within the current study, morbidity was most frequently return to the operating room, respiratory, or septic complications. The exact indications for reoperation however are not included within the database, so conclusions based on this information are limited. The NSQIP definition for return to the operating room includes only “major” surgical procedures within 30 days. This definition however may include a spectrum of procedure magnitude from bowel operation for colonic ischemia to endovascular reinterventions such as coil embolization for an endoleak.
Surgical site infections are relatively uncommon following EVAR, however they are associated with adverse outcomes for both OAR and EVAR. Obesity (obese I, II, and morbid obesity) is a risk factor for surgical site infection and recognition of this increased risk is important in the choice of repair method and perioperative management. Infections were associated with increased mortality, graft failure, subsequent major operation, and length of stay within OAR patients. After EVAR, infections were associated with increased graft failure, subsequent operations, and length of stay but not mortality. It is likely that graft failure and subsequent operation are responsible for the increased wound infection rate rather than the converse, however we cannot infer a causal relationship with this data. Other studies have found similar relationships between obesity and higher wound complication rates.2,6,14
The NSQIP database, while more robust than most administrative databases, still has a few notable limitations which remain and must be addressed. The database was designed as a tool for quality control assessment so individual institutions could compare their performance, in a risk adjusted manner, to national benchmarks. As participation has grown, the dataset has changed rapidly to include not only academic centers but community and rural hospitals as well. Information regarding the characteristics of the represented population within a given year is not readily available, therefore extrapolation of outcomes to the general Unites States population is difficult.
The database is also subject to reviewer error and data miscoding as well as having a lack of certain details important to AAA repair. We may not make conclusions regarding aneurysm size or suitability for EVARin addition to paravisceral extension. Additionally, we cannot identify symptomatic presentation other than ruptured AAAs. We have no information detailing what procedures were done for patients undergoing reoperations. Duration of ICU stay and discharge destination are unfortunately also not included in the dataset.
Conclusion
Body mass index must be considered as a risk factor when planning aneurysm repair. While underweight patients have the highest mortality risk with EVAR, morbidly obese patients have the highest mortality risk with OAR. There is no mortality benefit with EVAR compared to open surgery for underweight patients whereas morbidly obese patients may be better suited for endovascular repair. Additionally, given the lower mortality, EVAR is being underutilized in normal, overweight, and morbidly obese patients while it is being appropriately used more frequently than open repair in mild and moderately obese patients. Surgical site infections, higher in all obese patients, were found to be associated with increased rates of death, graft failure, and subsequent operation, making this an important relationship to consider as well.
Acknowledgments
We would like to acknowledge that this work was supported by the NIH T32 Harvard Longwood Research Training in Vascular Surgery grant HL007734.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Obesity trends among US adults. BRFSS, CDC; [Google Scholar]
- 2.Mullen JT, Davenport DL, Hutter MM, Hosokawa PW, Henderson WG, Khuri SF, et al. Impact of body mass index on perioperative outcomes in patients undergoing major intra-abdominal cancer surgery. Ann Surg Oncol. 2008;15:2164–72. doi: 10.1245/s10434-008-9990-2. [DOI] [PubMed] [Google Scholar]
- 3.Klasen J, Junger A, Hartmann B, Jost A, Benson M, Virabjan T, et al. Increased body mass index and peri-operative risk in patients undergoing non-cardiac surgery. Obes Surg. 2004;14:275–81. doi: 10.1381/096089204322857708. [DOI] [PubMed] [Google Scholar]
- 4.Dindo D, Muller MK, Weber M, Clavien PA. Obesity in general elective surgery. Lancet. 2003;361:2032–5. doi: 10.1016/S0140-6736(03)13640-9. [DOI] [PubMed] [Google Scholar]
- 5.Perrotta S, Nilsson F, Brandrup-Wognsen G, Jeppsson A. Body mass index and outcome after coronary artery bypass surgery. J Cardiovasc Surg (Torino) 2007;48:239–45. [PubMed] [Google Scholar]
- 6.Patel VI, Hamdan AD, Schermerhorn ML, Hile C, Dahlberg S, Campbell D, et al. Lower extremity arterial revascularization in obese patients. J Vasc Surg. 2007;46:738–42. doi: 10.1016/j.jvs.2007.05.044. [DOI] [PubMed] [Google Scholar]
- 7.Chang JK, Calligaro KD, Ryan S, Runyan D, Dougherty MJ, Stern JJ. Risk factors associated with infection of lower extremity revascularization: analysis of 365 procedures performed at a teaching hospital. Ann Vasc Surg. 2003;17:91–6. doi: 10.1007/s10016-001-0337-8. [DOI] [PubMed] [Google Scholar]
- 8.Nicholson ML, Dennis MJS, Makin GS, Hopkinson BR, Wenham PW. Obesity as a risk factor in major reconstructive vascular surgery. Eur J Vasc Surg. 1994;8:209–13. doi: 10.1016/s0950-821x(05)80462-1. [DOI] [PubMed] [Google Scholar]
- 9.O'Hare AM, Feinglass J, Sidawy AN, Bacchetti P, Rodriguez RA, Daley J, et al. Impact of renal insufficiency on short-term morbidity and mortality after lower extremity revascularization: Data from the Department of Veterans Affairs' National Surgical Quality Improvement Program. J Am Soc Nephrol. 2003;14:1287–95. doi: 10.1097/01.asn.0000061776.60146.02. [DOI] [PubMed] [Google Scholar]
- 10.Davenport DL, Xenos ES, Hosokawa P, Radford J, Henderson WG, Endean ED. The influence of body mass index obesity status on vascular surgery 30-day morbidity and mortality. J Vasc Surg. 2009;49:140–7. doi: 10.1016/j.jvs.2008.08.052. epub ahead of prin. [DOI] [PubMed] [Google Scholar]
- 11.Starnes BW, Andersen CA, Ronsivalle JA, Stockmaster NR, Mullenix PS, Statler JD. Totally percutaneous aortic aneurysm repair: experience and prudence. J Vasc Surg. 2006;43:270–6. doi: 10.1016/j.jvs.2005.11.004. [DOI] [PubMed] [Google Scholar]
- 12.Lee WA, Brown MP, Nelson PR, Huber TS. Total percutaneous access for endovascular aortic aneurysm repair (“Preclose” technique) J Vasc Surg. 2007;45:1095–101. doi: 10.1016/j.jvs.2007.01.050. [DOI] [PubMed] [Google Scholar]
- 13.American College of Surgeons National Quality Surgical Improvement Program http://www.acsnsqip.org/
- 14.Khandanpour N, Armon MP, Foxall R, Meyer FJ. The effects of increasing obesity on outcomes of vascular surgery. Ann Vasc Surg. 2009;23:310–6. doi: 10.1016/j.avsg.2008.05.012. [DOI] [PubMed] [Google Scholar]
- 15.Giles KA, Hamdan AD, Pomposelli FB, Wyers MC, Siracuse JJ, Schermerhorn ML. Body mass index: surgical site infections and mortality after lower extremity bypass from the National Surgical Quality Improvement Program 2005–2007. Ann Vasc Surg. 2010;24:48–6. doi: 10.1016/j.avsg.2009.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Johnson ON, Sidawy AN, Scanlon JM, Walcott R, Arora S, Macsata RA, et al. Impact of obesity on outcomes after open surgical and endovascular abdominal aortic aneurysm repair. J Am Coll Surg. 2010;210:166–77. doi: 10.1016/j.jamcollsurg.2009.10.011. [DOI] [PubMed] [Google Scholar]
- 17.Hua HT, Cambria RP, Chuang SK, Stoner MC, Kwolek CJ, Rowell KS, et al. Early outcomes of endovascular versus open abdominal aortic aneurysm repair in the National Surgical Quality Improvement Program-Private Sector (NSQIP-PS) J Vasc Surg. 2005;41:382–9. doi: 10.1016/j.jvs.2004.12.048. [DOI] [PubMed] [Google Scholar]
- 18.Giles KA, Schermerhorn ML, O'Malley AJ, Cotterill P, Jhaveri A, Pomposelli FB, Landon BE. Risk prediction for perioperative mortality of endovascular vs open abdominal aortic aneurysms using the Medicare population. J Vasc Surg. 2009;50:256–62. doi: 10.1016/j.jvs.2009.01.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Beck AW, Goodney PP, Nolan BW, Likosky DS, Eldrup-Jorgensen J, Cronenwett JL, et al. Predicting 1-year mortality after abdominal aortic aneurysm repair. J Vasc Surg. 2009;49:838–43. doi: 10.1016/j.jvs.2008.10.067. [DOI] [PubMed] [Google Scholar]