Abstract
Background
Diagnostic validity of oppositional defiant and conduct disorders (ODD and CD) for preschoolers has been questioned based on concerns regarding the ability to differentiate normative, transient disruptive behavior from clinical symptoms. Data on concurrent validity has accumulated, but predictive validity is limited. Predictive validity is critical to refuting the hypothesis that diagnosing ODD and CD in young children leads to pathologizing normal behavior. ODD and CD have emerged as gateway disorders to many forms of adult psychopathology. Establishing how early we can identify symptoms and disorders that herald poor prognosis is one of the most important goals for research on etiology and prevention.
Methods
Subjects were 3–5 year old consecutive referrals to a child psychiatry clinic (n=123) and demographically matched children from a pediatric clinic (n=100). A diagnostic interview was used to assess DSM-IV ODD and CD in a prospective follow-up design from preschool to school age. Stability of ODD and CD diagnoses and level of impairment were tested as a function of preschool diagnosis.
Results
Over 80% of preschoolers diagnosed with ODD and approximately 60% of preschoolers diagnosed with CD met criteria for the same disorder during follow-up. Impairment over time varied significantly as a function of stability of diagnosis across three years.
Conclusions
These results provide the first evidence of the predictive validity of DSM-IV ODD and CD in clinically referred preschool children. The findings challenge the assumption that symptoms of disruptive behavior disorders that occur during the preschool period tend to be transient.
Keywords: preschool, oppositional defiant disorder, conduct disorder, impairment, predictive validity
Research on preschool psychopathology has evolved from two distinct trends: a clinical need to serve increasing numbers of young children presenting to mental health clinics (Ringel & Sturm, 1998), and emerging data indicating that the underpinnings of many disorders lie in deficits in behavioral and emotional functioning that are present early in life (Keenan & Shaw, 2003). The developmental appropriateness of DSM-IV nosology (APA, 1994), however, especially for oppositional defiant disorder (ODD) and conduct disorder (CD) for preschool children has been called into question (McClellan & Speltz, 2003; Thomas & Guskin, 2001). In response to these concerns, a research agenda was articulated calling for empirically based answers to the concerns about applying such diagnoses to preschoolers (Keenan & Wakschlag, 2002).
Since then, evidence has accumulated for reliability and concurrent validity of DSM-IV ODD and CD in preschool children. Strong one-week test-retest and inter-rater reliability of ODD and CD symptoms, and concurrent validity via associations with parent- and teacher-rated impairment were reported in samples of referred an d non referred 3–5 year olds (Keenan, Wakschlag, Danis, Hill, Humphries et al., 2007). ODD diagnosed using DSM-IV criteria has demonstrated good discriminant, divergent, and convergent validity in 2–5 year old children (Birmaher, Ehmann, Axelson, Goldstein, Monk et al., 2009).
Evidence for the predictive validity of preschool ODD and CD has been limited, but is critical for refuting the claim that such disorders pathologize normative behavior during this developmental period (McClellan & Speltz, 2003; Thomas & Guskin, 2001). Establishing predictive validity is also critical for identifying primary points in development for prevention and studies of etiology. ODD and CD during adolescence have been shown to predict many common forms of adult psychopathology (Kim-Cohen, Arsenault, Caspi, Tomas, Taylor et al., 2005). If ODD and CD symptoms and disorders as manifest in pre-school age children are empirically linked to those observed in older youth, then the point of deviation to focus on is early in childhood. Predictive validity of preschool diagnoses on a similar magnitude to that found for older children would be evidence of such an empirical link.
There is a long history of research in non-clinical samples supporting the hypothesis that caregiver ratings of behavioral and emotional problems that emerge early in life can be stable and predictive of later impairment in community samples (Campbell, Ewing, Breaux, & Szumowski, 1986; Cummings, lanotti, & Zahn-Waxler, 1989; Earls & Jung, 1987; Stevenson, Richman & Graham, 1985). The translation of this knowledge to clinical disorders and clinical populations, however, has progressed only minimally. In a few studies, predictive validity of disruptive behavior and attention deficit disorders has been established, but data on stability for each diagnostic category is typically not provided (Harvey, Youngwirth, Thakar, Errazuriz, 2009; Lavigne, Arend, Rosenbaum, Binns, Chrisoffel & Gibbons, 1998; Pierce, Ewing & Campbell, 1999). The E-Risk Study, a representative birth cohort followed longitudinally, is the only known study in which the validity of CD from preschool to school age was tested (Kim-Cohen, Arsenault, Caspi et al., 2005). Five-year-olds who were diagnosed with CD were at significantly greater risk for a CD diagnosis when followed up at age 7 (odds ratio = 20.6). Approximately half of the preschoolers diagnosed with CD had no CD symptoms at age 7, although evidence of social and academic impairment for those diagnosed as preschoolers continued to be present through the age of 10 years (Kim-Cohen, Arsenault, Newcombe, Adams, Bolton et al., 2005). An advantage of the E-risk study is that it used a representative birth cohort to test predictive validity. A disadvantage is that such a large study precluded the use of a diagnostic interview, which may have resulted in somewhat less reliable assessments of CD symptoms.
In the present study, we provide one of the first tests of the specificity of prediction of DSM-IV ODD and CD diagnosed in preschoolers (ages 3–5 years) using clinic-referred and non-referred samples that include both sexes and are largely comprised of African American children. A reliable, developmentally informed diagnostic interview was used to generate DSM-IV symptoms of ODD and CD. In addition to providing data on stability of diagnosis, we test whether stability is moderated by sex or race, examine symptom and diagnostic outcomes for children over 36 months, and test level of impairment as a function of stability of diagnosis. We focus on the utility of DSM-IV ODD and CD for children living under conditions of economic stress because they are at higher risk for developing disruptive behavior disorders, although specific mechanisms by which economic stress confers risk is not well known (Dohrenwend, Levav, Shrout, Schwarts, Naveh et al., 1992).
Methods
Participants
Data on the participants, preschool assessment, and the reliability and validity of the diagnostic instrument used in the present study have been published previously (Keenan et al., 2007). For clarity and ease of interpretation of the data presented in this study, we briefly review those results.
Two hundred twenty-three 3- to 5-year-old children, residing with their biological mothers, were enrolled in the study. Approximately half of the children (n=123) were comprised of consecutive referrals to a child psychiatry outpatient clinic because of aggression, defiance, and/or problems controlling temper. The other half (n=100) was recruited through the general pediatric clinic and was screened to establish that the caregiver was not seeking an evaluation for disruptive behavior problems. Family income was set at a cut-off of 250% of the U.S. poverty level by family size.
Of the 152 consecutive clinic referrals 130 (85.5%) agreed to participate, 8 (5.3%) refused to participate, 7 (4.6%) were unable to be scheduled for a visit, 5 (3.3%) sought services elsewhere, and 2 (1.3%) never completed the recruitment process. Seven children who were recruited into the study were later excluded from the analytic sample because of serious medical problems that had onsets prior to their referral (i.e., brain tumor, genetic syndrome, and seizure disorder).
Caregivers of non-referred children responded to fliers in the waiting rooms of the pediatric clinics at the University of Chicago. Of the 109 families who responded and were eligible for the study, 100 (91.7%) agreed to participate, 1 (0.9%) refused, and 8 (7.3%) were unable to be scheduled.
Eighty-two percent of all participating children were African American, and 52.5% were male. The age distribution was as follows: 79 (35.4%) three-year olds, 75 (33.6%) four-year olds, and 69 (30.9%) five-year olds. Matching on demographics during recruitment resulted in no significant differences between non-referred and referred children on demographic variables. The University of Chicago Institutional Review Board approved all study procedures. Written informed consent was obtained after providing a complete description of the study to the subjects.
Children were followed annually for a period of three years, up through school age. Retention was high at each wave: 92.4% at wave 1 (ages 4–6), 93.3% at wave 2 (ages 5–7), and 91.5% at wave 3 (ages 6–8). There were no significant differences between those participants who were and were not seen in each wave in terms of race, sex, referral status, or ODD and CD diagnosis at baseline. The biological mother was the informant in nearly all cases over the course of the study. In the final wave, only 3 (1.4%) of the 204 subjects retained had informants other than the biological mother.
ODD and CD symptoms and diagnoses
Bachelor’s level research assistants, who were blind to the referral status of the child, administered the Kiddie-Disruptive Behavior Disorder Schedule (K-DBDS; Keenan et al., 2007) to caregivers. Different research assistants administered the preschool and school age assessments. The K-DBDS was developed to assess disruptive behavior disorders in young children using developmentally appropriate operational definitions of symptoms. DSM-IV ODD symptoms were unchanged from how they are described in DSM-IV. Of the 15 DSM-IV CD symptoms, four were not assessed because of the lack of face validity: (1) breaking into a house, car, or building; (2) running away from home overnight; (3) often staying out late; and (4) truancy. The wording was modified for six symptoms. For example, “Has stolen items of nontrivial value without confronting a victim” was modified to read, “Has stolen from a store or purse on more than one occasion.” “Has used a weapon that can cause serious physical harm to others” was modified to read, “Has used an object (such as a stick, rock, or knife) to hurt or to try to hurt someone.” A complete description of modifications and examples of symptom manifestation has been published (Keenan et al., 2007).
The one-week test-re-test reliability of the K-DBDS was conducted in an independent sample of 31 referred and non-referred preschoolers. Test-retest reliability for total number of ODD and CD symptoms was high (ICC > .75). Inter-rater reliability for the total number of ODD and CD symptoms was high (ICC > .95), as was the inter-rater reliability for diagnoses (kappa > .90). Reliability was not affected by age or sex of the child. Validity of preschool diagnoses was demonstrated via associations with impairment, such as parental ratings of global impairment, and differentiation between referred and non-referred children (Keenan et al., 2007). The Principal Investigator (KK), a licensed clinical psychologist, reviewed the K-DBD and impairment ratings with the research team for each subject.
Impairment
Caregivers completed the non-clinician version of the Children’s-Global Assessment Scale (C-GAS; Setterberg, Bird, Gould, Shaffer, & Fisher, 1992), which has been validated for use with parents (Bird, Andrews, Schwab-Stone, Goodman, Dulcan, et al., 1996). Scores on the C-GAS range from 1 to 100 with each decile containing a description of whether and how much the child’s behavior negatively impacts functioning, with lower scores reflecting greater levels of impairment.
Results
Rates of ODD and CD at baseline
Among the 223 preschoolers, 89 met DSM-IV criteria for ODD (91.0% of who were from the clinically referred group). Seventy-six preschoolers met DSM-IV criteria for CD, (89.5% of who were from the clinically referred group). There were no significant sex differences in the rate of ODD or CD. Of the 103 children who met criteria for ODD and/or CD, 62 (60.2%) met criteria for both disorders, 27 (26.2%) met criteria for ODD, but not CD, and 14 (13.6%) met criteria for CD but not ODD. Half of the 14 preschoolers who met criteria for CD but did not meet criteria for ODD had 3 symptoms of ODD at baseline, approximately a third (35.7%) had 2 symptoms, and the remaining two cases had one and no symptoms of ODD at baseline, respectively.
Among those diagnosed with ODD, the most commonly endorsed symptoms were defiance (100.0%), losing temper (94.4%), annoying others on purpose (84.3%), and blaming others for her own mistakes (78.7%). Among those children diagnosed with CD at baseline, the most commonly endorsed symptoms were using an object to harm someone (85.5%), physical aggression towards others (84.2%), lying to con (72.4%), destroying property (50.0%), and stealing (44.7%).
Stability of ODD and CD across three years
Using diagnosis at baseline as the denominator, 72.0%, 66.3%, and 51.7% of the children diagnosed with DSM-IV ODD at baseline met criteria at the 12-, 24-, and 36-month follow-up, respectively, and 82.1% met criteria in at least one of the three follow-up assessments. Of the children who met criteria for CD at baseline, 48.6%, 33.3%, and 26.0% met criteria for CD at the 12-, 24-, and 36-month follow-up, respectively, and 61.1% met criteria in at least 1 of the three follow-up assessments.
As shown in Figure 1, very few children diagnosed at baseline were symptom free during the follow-up. In addition to the 82.1% of children meeting criteria for ODD during follow-up, another 8.3% had years in which 3 of the 4 symptoms required for meeting criteria were present, and only 1 (1.2%) child remained free of ODD symptoms during the 36-month follow-up (Figure 1). Among those diagnosed with CD and assessed at follow-up (N = 72), in addition to the 61.1% who met criteria for CD, 20.8% had years in which 2 of the 3 symptoms required for CD were present, and only 6 (8.3%) of those diagnosed at baseline were symptom free throughout the 36-month follow-up (Figure 1).
Figure 1.
Outcome of preschoolers meeting criteria for DSM-IV ODD and CD at ages 3–5 years
There were 30 new cases of ODD during the follow-up. Close to half (46.7%) of those children had 3 symptoms of ODD at baseline, 10 (33.3%) had 2 symptoms and 6 (20.0%) had no symptoms of ODD at baseline. However, of the six children with no ODD symptoms at baseline who developed ODD during the follow-up, all but one were reported to have symptoms of CD. Eleven new cases of CD were observed during the follow-up; all but one of the new onset cases had symptoms of CD at baseline.
Predictive validity of preschool diagnosis
The likelihood of meeting criteria for ODD at a subsequent assessment was tested using logistic regression with ODD diagnosis at baseline, race, and sex entered simultaneously. Race had no significant effect, and so was dropped from the models presented here. The odds (95% CI) of meeting criteria for ODD given a diagnosis at baseline were 16.3 (8.1 – 33.1), 16.4 (7.8 – 34.7), and 10.8 (5.2 – 22.3) for the 12, 24, and 36-month follow-ups, respectively. The odds of meeting criteria at least once during the 36-month follow-up were 18.1 (8.5 – 38.5) (Table 1). Sex was a significant predictor of ODD at the 24- and 36-month follow-up assessments; 20 of the 30 the new onset cases were boys. The interaction between sex and preschool ODD on subsequent ODD was tested but was not significant.
Table 1.
Predictive validity of preschool ODD across 3 years
| B | S.E. | Wald | Sig. | OR | 95% CI | ||
|---|---|---|---|---|---|---|---|
| ODD at 12 month follow-up | |||||||
| ODD diagnosis at baseline | 2.79 | 0.36 | 60.02 | .000 | 16.3 | 8.1–33.1 | |
| sex | −0.14 | 0.36 | 0.14 | .709 | 0.87 | 0.4–1.8 | |
| ODD at 24 month follow-up | |||||||
| ODD diagnosis at baseline | 2.80 | 0.38 | 53.53 | .000 | 16.4 | 7.8–34.7 | |
| sex | −1.01 | 0.38 | 6.97 | .008 | 0.4 | 0.2–0.8 | |
| ODD at 36 month follow-up | |||||||
| ODD diagnosis at baseline | 2.37 | 0.37 | 40.94 | .000 | 10.8 | 5.2–22.3 | |
| sex | −1.04 | 0.36 | 8.29 | .004 | 0.4 | 0.2–0.7 | |
|
ODD at any point during 36 month follow-up |
|||||||
| ODD diagnosis at baseline | 2.89 | 0.39 | 55.97 | .000 | 18.1 | 8.5–38.5 | |
| sex | −.53 | .36 | 2.16 | .142 | 0.6 | 0.3–1.2 | |
The odds of meeting criteria for CD given a diagnosis at baseline were 20.4 (8.0 – 52.5), 22.6 (6.4 – 79.0), and 7.3 (2.7 – 19.7) for the 12, 24, and 36-month follow-ups, respectively. The odds of meeting criteria at least once during the 36-month follow-up were 15.6 (7.1 – 34.0) (Table 2). Sex was a significant predictor of CD at the 36-month follow-up assessments, with more boys than girls meeting criteria. Of the 11 new cases of CD, 8 (72.7%) were boys. The interaction between sex and baseline CD on subsequent CD was tested but was not significant.
Table 2.
Predictive validity of preschool CD across 3 years
| B | S.E. | Wald | Sig. | OR | 95% CI | ||
|---|---|---|---|---|---|---|---|
| CD at 12 month follow-up | |||||||
| CD diagnosis at baseline | 3.20 | 0.48 | 39.3 | .000 | 20.4 | 8.0–52.5 | |
| sex | 0.18 | 0.41 | 0.2 | .673 | 1.2 | 0.5–2.7 | |
| CD at 24 month follow-up | |||||||
| CD diagnosis at baseline | 3.12 | 0.64 | 23.7 | .000 | 22.6 | 6.4–79.0 | |
| sex | −.927 | 0.49 | 3.6 | 0.60 | 0.4 | 0.2–1.0 | |
| CD at 36 month follow-up | |||||||
| CD diagnosis at baseline | 1.99 | 0.50 | 15.6 | .000 | 7.3 | 2.7–19.7 | |
| sex | −1.40 | 0.54 | 6.7 | .010 | 0.3 | 0.1–0.7 | |
|
CD at any point during 36 month follow-up |
|||||||
| CD diagnosis at baseline | 2.74 | 0.40 | 47.46 | .000 | 15.6 | 7.1–34.0 | |
| sex | −0.15 | −.39 | 0.15 | 0.70 | 0.9 | 0.4–1.8 | |
Reciprocal Influence of ODD and CD on stability
As stated earlier, co-occurrence of ODD and CD was common at baseline. Approximately half (53.8%) of the 223 children did not meet criteria for either disorder, 14 (6.3%) met criteria for CD but not ODD, 27 (12.1%) met criteria for ODD but not CD, and 62 (27.8%) met criteria for both disorders. We tested whether ODD, CD, and the co-occurrence of the two accounted for unique variance in meeting criteria in at least 1 of the three follow-up assessments. In predicting later ODD, a diagnosis of ODD at baseline (OR = 10.1, 95% CI = 3.9 – 30.8, p < .001), and a diagnosis of CD at baseline (OR = 3.6, 95% CI = 1.2 – 11.5, p < .05), but not their co-occurrence (OR = 0.5, 95% CI = 0.1 – 2.6, p > .10) were unique predictors. A later diagnosis of CD during the three-year follow-up period was predicted by a diagnosis of CD at baseline (OR = 5.3, 95% CI = 1.3 – 21.1, p < .05), but not a by diagnosis of ODD at baseline (OR = 3.1, 95% CI = 0.8 – 11.7, p > .10), nor by their co-occurrence (OR = 1.8, 95% CI = 0.3 – 11.5, p > .10).
Impairment as a function of ODD and CD diagnostic stability
Mutually exclusive diagnostic stability groups were created to test differences in average impairment ratings over time using caregiver report on the C-GAS. Children were categorized as having no diagnosis, or a diagnosis that was chronic (i.e. meeting diagnostic criteria in at least 2 of the 3 follow up assessments), in full remission (i.e., no diagnosis at any of the three follow-ups), in partial remission (i.e., meeting criteria in only 1 of the three follow-ups), or as having a new onset (i.e. children meeting criteria after the baseline assessment). The total n for these analyses was 186: the number with complete follow-up data.
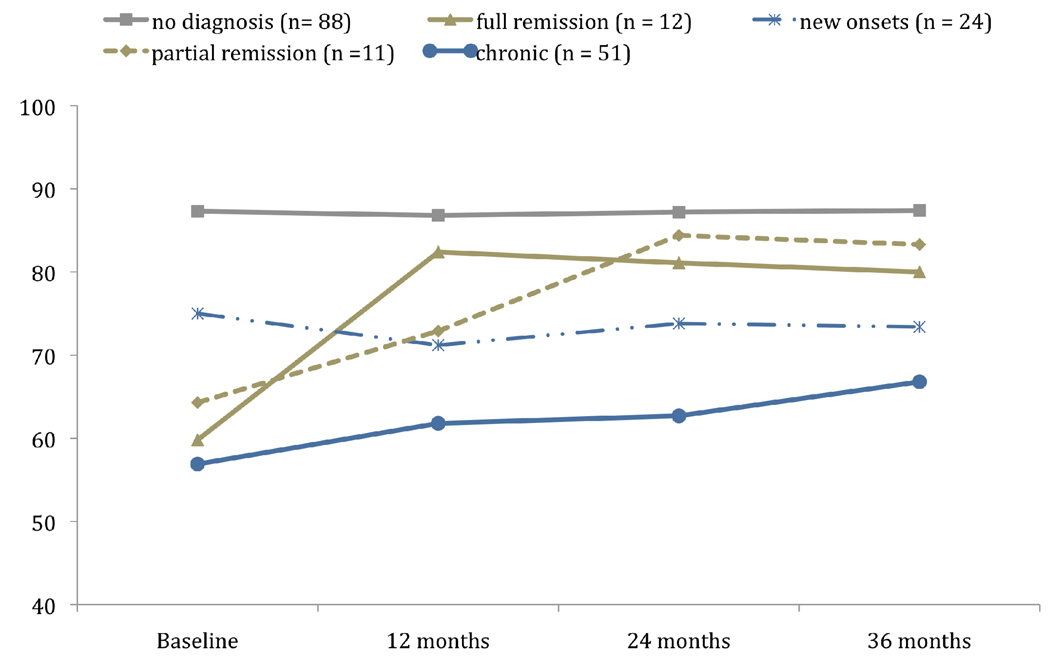
As shown in Figure 2, a significant interaction of time and diagnostic stability of ODD on impairment levels was observed (F [4,181) = 13.31, p < .001, eta = .37). We conducted post-hoc comparisons using a Bonferroni correction to test whether each diagnostic stability group differed from the no diagnosis group and from each other on impairment ratings over time. These post-hoc tests revealed significant differences between the no diagnosis group and each of the four other groups, between the partial and full remission groups and the chronic group, and between the new onset group and the chronic group (Figure 2).
Figure 2.
Average rating of functional impairment over time as a function of ODD diagnostic status
Significant effect of time by diagnostic status on impairment (F [4,181) = 13.31, p < .001, eta = .37).
ODD diagnostic groups also were compared on baseline impairment ratings. This analysis yielded a significant difference overall (F [4, 181) = 39.20, p < .001, eta = .68), with post-hoc comparisons revealing significant differences between the no diagnosis and all other groups, but no significant differences among children with chronic, recurring, or remitting ODD.
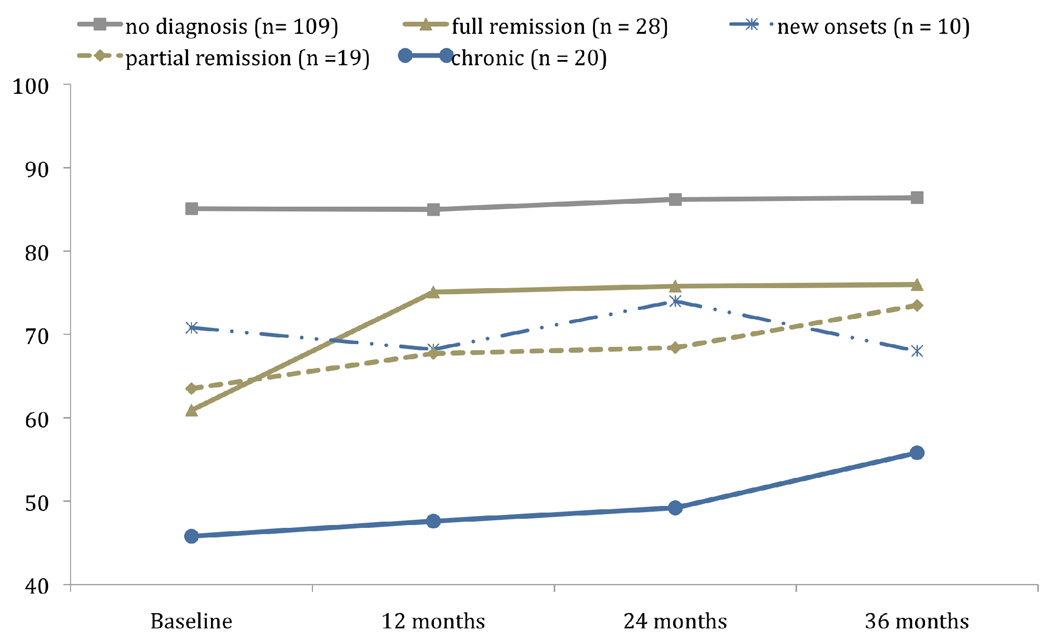
A significant interaction of time and diagnostic stability was observed for CD as well (F [4, 181) = 6.47, p < .001, eta = .35). Pot-hoc comparisons using a Bonferroni correction revealed the same pattern as that generated for ODD: significant differences between C-GAS ratings over time were found between the no diagnosis group and each of the other four groups, the partial and full remission groups compared to chronic group, and the new onset group compared to the chronic group (Figure 3). A test of baseline impairment ratings showed a similar pattern to ODD (F [4, 181) = 44.63, p < .001, eta = .70), revealing significant differences between the no diagnosis and all other groups. In addition, the level of impairment at baseline for preschoolers who would go on to follow a chronic course of CD was significantly greater than those whose course would be characterized as partial or full remission during the follow-up period.
Figure 3.
Average rating of functional impairment over time as a function of CD diagnostic status
Significant effect of time by diagnostic status on impairment (F [4,181) = 6.47, p < .001, eta = .35).
Sex and race effects on the chronicity of and remission from ODD and CD
Finally, we examined whether sex or race was associated with chronicity and remission of disorder. For these analyses we used the above mutually exclusive groups, but excluded the no diagnosis and new onset cases, because we were primarily interested in the effects of race and sex on chronicity, and because we knew already from the predictive validity analyses that boys were over-represented among the new onset cases.
Race had no effect on chronicity of ODD (χ2 (df = 2) = 1.11, p > .10) or CD (χ2 (df = 2) = 0.41, p > .10). There was a significant effect of sex on the chronicity of CD (χ2 (df = 2) = 7.80, p < .05), but not on the chronicity of ODD (χ2 (2) = 1.64, p > .10). Among the 29 girls with CD, 11 (37.9%) demonstrated full remission, 13 (44.8%) demonstrated partial remission, and 5 (17.2%) had chronic CD. Among the 38 boys, 17 (44.7%) demonstrated full remission, 6 (15.8%) demonstrated partial remission, and 15 (39.5%) had chronic CD. Thus, girls were less likely to manifest chronic CD than were boys.
Discussion
There are two statements in the DSM-IV (APA, 1994) regarding ODD and CD in preschoolers. The first is that CD may occur as early as age 5–6 years but usually does not occur until late childhood or early adolescence. The second is that caution should be used in diagnosing ODD in preschoolers because transient oppositional behavior is very common during the preschool period. In the absence of a large representative, prospective study beginning in early childhood using DSM-IV based diagnostic interviews, the typical age of onset of CD or ODD is still not known. What is known from the results of the present study, and from previously published reports on reliability and concurrent validity, is that CD does occur as early as the preschool period and that the vast majority of preschoolers who present for mental health services and meet criteria for ODD are not demonstrating transient oppositional behavior. These are results that could be useful in the revision to the DSM that is currently underway, and that address issues that have been highlighted as critical to the research agenda on disruptive behavior disorders (Moffitt, Arsenault, Jaffee, Kim-Cohen, Koenen et al., 2008).
In the present study, approximately 80% of preschoolers who met criteria for ODD and 60% of preschoolers who met criteria for CD continued to meet criteria in at least one assessment during a 36-month follow-up period. These levels of stability are higher than those reported for community samples of school age children, but similar to those reported for clinical samples of school age children. For example, in the Great Smoky Mountain Study, about a third of school-age children diagnosed with ODD and a third of those diagnosed with CD by combined youth and parent report met criteria for the same disorder in at least 1 of 3 subsequent assessments (Rowe, Maughan, Costello & Angold, 2005). In a population-based sample, 40% of girls and 46% of boys with a disruptive behavior diagnosis (i.e., ODD, CD or DBD-NOS) had a similar diagnosis three years later (Messer, Goodman, Rose, Meltzer & Maughan, 2006).
In contrast, Lahey et al (1995) reported that the stability of CD in a sample of clinically referred school age boys, for whom three informants were used, ranged from 50%–60% in any one subsequent year, and up to 80% when multiple years were assessed, indicating that multiple waves of assessment generate a more reliable measure of CD because symptoms fluctuate over time. Twenty years ago, Cantwell and Baker (1989) stated that DSM-III ODD showed the poorest recovery rate of all the behavioral psychiatric disorders. Surprisingly, there have been few studies since then in which the stability of ODD has been tested in either clinical or non-clinical samples.
Beyond describing stability, the predictive validity, as measured by the odds of a future diagnosis given a diagnosis at ages 3–5 was very strong for both disorders. This was especially the case at the 12- and 24-month follow-ups. The data in the present study suggest that ODD may demonstrate a more stable pattern than CD, and this makes sense given the differences in nosology. ODD comprises symptoms of defiance and negative emotionality. All ODD symptoms are required to be present “often.” Thus, one would expect that a child’s frequent difficulty managing negative emotion would stay relatively constant. In contrast, CD symptoms are comprised of discrete behaviors, some of which are required to occur often (e.g., lying to con and bullying), but many of which are lower base rate behaviors.
The vast majority of predictive validity was accounted for by the presence of the disorder itself, with little additional variance accounted for by sex and none accounted for by race, although it is important to note that only about 20% of the sample was not African American. The reciprocal effects of ODD and CD on their respective predictive validity was modest, with CD accounting for some of the predictive validity to later ODD, but no effect of ODD on the prediction of CD. These data call into question the hierarchical organization of the two disorders. ODD is conceptualized as a stepping-stone to CD, and it is recommended in the DSM-IV that ODD not be diagnosed if CD is present. These results provide evidence that CD and ODD do not interact in determining predictive validity of either disorder. Moreover, the patterns of stability suggest that ODD may be more persistent than CD. Thus, the nesting of ODD within CD may obscure important differences in prognosis.
Ratings of impaired functioning over time provided further validation of ODD and CD. For both disorders, significantly greater levels of impairment (as evidenced by lower scores) from baseline to follow-up at school age were found as a function of stability of diagnosis. For preschoolers with chronic ODD, impairment levels at baseline did not differ from those whose ODD would partially or fully remit. In contrast, preschoolers with chronic CD had significantly lower scores on our global measure of adaptive functioning at baseline from those whose CD would partially or fully remit. Thus, impairment ratings can further differentiate preschool CD in terms of prognosis. It should be noted, however, that a 36-month follow-up period into school age might not be sufficient for capturing the waxing and waning course of CD. In addition, a valid assessment of CD during the school-age period will likely require self-report.
There were a few notable sex differences. Boys were more likely than girls to develop ODD and CD at school age, and preschool boys with CD were more likely to follow a chronic course than were girls. These sex differences are consistent with developmental models of the diverging course of psychopathology from early childhood that incorporate sex differences in other competencies, such as language development and empathic concern (e.g., Keenan & Shaw, 1997). Such competencies may affect the course of early ODD and CD. An important next step is to test sex differences in homo- and heterotypic continuity of preschool ODD and CD. Based on studies of older children (Costello, Mustillo, Erkanli, Keeler & Angold, 2003), preschool girls may be more likely than boys to show prediction from preschool ODD and CD to a variety of other forms of psychopathology, including depression.
Several limitations to the present study are noted. First, data were derived from a single informant. Although primary caregivers are typically the sole informant in a clinical setting, and ODD is one of the few disorders in which symptoms may be manifest in the home setting only, validating maternal report for preschoolers is an important next step. Second, our participants were selected based on living within 250% of the poverty level for the U.S. The stability of preschool DBDs for children living in other income environments may be different. In addition to the non-representativeness of the sample in terms of economic living environment, insufficient numbers of cases among the non-referred children meant that we were unable to adequately test whether predictive validity is significantly different for non-clinical cases. The results from the E-risk (Kim-Cohen et al., 2005) study suggest that the predictive validity of DSM disruptive behavior disorders in non-referred children is, in fact, adequate. Given that the vast majority of children with mental health disorders are not referred for services (Costello, Copeland, Cowell & Keeler, 2007; Lavigne, Lebailly, Hopkins, Gouze & Binns, 2009), further work to establish the utility of DSM-IV disruptive behavior nosology for preschool children with disruptive behavior who are non-referred is indicated.
Third, because of the rate of overlap of the two disorders we were unable to test the predictive validity of CD in the absence of ODD. If the more common presentation in the clinic setting is one in which CD occurs without ODD, then the results of the present study are limited with respect to the stability of CD. If, however, CD typically co-occurs with ODD in clinically referred preschoolers, then the data are generalizable. It is known that among clinically referred samples of older children the level of co-occurring ODD in children with CD is high and consistent with the level reported in the present study; between 80% and 95% of clinically referred youth who meet criteria for CD also meet criteria for ODD (Lahey et al., 1992). Thus, it is likely that the same pattern would be observed in other sample of clinically referred preschoolers. Because symptoms of CD in preschool children are typically not assessed, however, we are unable to compare the overlap between ODD and CD in the present sample to other comparably aged samples.
Fourth, the co-occurrence with other DSM-IV disorders was not assessed. The participants were selected for referral for ODD and CD symptoms. It is possible, however, that the presence of symptoms of other disorders such as depression, anxiety and ADHD, influenced the stability. The goal of the present paper was to establish predictive validity of ODD and CD. A larger and more diverse sample, with respect to reason for clinical referral, is needed to adequately examine the contribution of comorbidities to predictive validity of ODD and CD in preschoolers.
The implications of these results for prevention are significant. As models of developmental psychopathology incorporate the interface between genetic vulnerability and environmental stressors, the focus of inquiry with regard to developmental timing is critical. If findings such as these in the present study are replicated, then screening for the vulnerabilities for mental disorders and identifying the putative environmental stressors that interact with such vulnerabilities will need to take place the first years of life. The present study adds to the existing knowledge base on characterizing the emergence of psychopathology early in life including depression (Luby, Si, Belden, Tandon & Spitznagel, 2009; Luby, Belden, Sullivan, Hayden, McCadney & Spiznagel, 2009) and ADHD (Lahey, Pelham, Loney, Kipp, Ehrhardt et al., 2004; Lee, Lahey, Owens, & Hinshaw, 2008), and places ODD and CD among these disorders in terms of the presence of core deficits early in life, the predictive validity of the diagnostic constructs, and the enduring impairment associated with early diagnosis.
Key Points
DSM-IV ODD and CD diagnosed in clinically referred preschoolers demonstrate predictive validity.
Preschool CD contributes to prediction of ODD, but preschool ODD did not account for variance in later CD.
Parent-rated impairment was associated with chronicity of diagnosis, especially for CD
Boys were more likely than girls to develop ODD and CD at school age, and preschool boys with CD were more likely to follow a chronic course than were girls
Acknowledgements
This project was supported by NIMH grants R01 MH62437 and R01 MH68455
Abbreviations
- DSM-IV
Diagnostic and Statistical Manual-4th Edition
- ODD
oppositional defiant disorder
- CD
conduct disorder
Contributor Information
Kate Keenan, Department of Psychiatry and Behavioral Neuroscience, University of Chicago.
Debra Boeldt, Department of Psychiatry and Behavioral Neuroscience, University of Chicago.
Diane Chen, Department of Psychiatry and Behavioral Neuroscience, University of Chicago.
Claire Coyne, Department of Psychiatry and Behavioral Neuroscience, University of Chicago.
Radiah Donald, Department of Psychiatry and Behavioral Neuroscience, University of Chicago.
Jeanne Duax, Department of Psychiatry and Behavioral Neuroscience, University of Chicago.
Katherine Hart, Department of Psychiatry and Behavioral Neuroscience, University of Chicago.
Jennifer Perrott, Department of Psychiatry and Behavioral Neuroscience, University of Chicago.
Jennifer Strickland, Department of Psychiatry and Behavioral Neuroscience, University of Chicago.
Barbara Danis, Department of Psychiatry, University of Illinois at Chicago.
Carri Hill, Department of Psychiatry, University of Illinois at Chicago.
Shante Davis, Department of Psychiatry, University of Illinois at Chicago.
Smita Kampani, Department of Psychiatry, University of Illinois at Chicago.
Marisha Humphries, Department of Educational Psychology, University of Illinois at Chicago.
References
- American Psychiatric Association. Diagnostic and Statistical Manual - Fourth Edition. Washington DC: American Psychiatric Association Press; 1994. [Google Scholar]
- Bird HR, Andrews H, Schwab-Stone M, Goodman S, Dulcan M, Richters J, Rubio-Stipec M, Moore RE, Chiang P, Hoven C, Canino G, Fisher P, Gould MS. Global measures of impairment for epidemiologic and clinical use with children and adolescents. International Journal of Methods in Psychiatric Research. 1996;6:295–307. [Google Scholar]
- Birmaher B, Ehmann M, Axelson DA, Goldstein BI, Monk K, Kalas C, Kupfer D, Gill MK, Leibenluft E, Bridge J, Guyer A, Egger HL, Brent DA. Schedule for affective disorders and schizophrenia for school-age children (K-SADS-PL) for the assessment of preschool children: A preliminary psychometric study. Journal of Psychiatric Research. 2009;43:680–686. doi: 10.1016/j.jpsychires.2008.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cantwell DP, Baker L. Stability and natural history of DSM-III childhood diagnoses. Journal of the American Academy of Child and Adolescent Psychiatry. 1989;28:691–700. doi: 10.1097/00004583-198909000-00009. [DOI] [PubMed] [Google Scholar]
- Costello EJ, Copeland W, Cowell A, Keeler G. Service costs of caring for adolescents with mental illness in a rural community, 1993–2000. American Journal of Psychiatry. 2007;164:36–42. doi: 10.1176/appi.ajp.2007.164.9.A36. [DOI] [PubMed] [Google Scholar]
- Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A. Prevalence and development of psychiatric disorders in childhood and adolescence. Archives of General Psychiatry. 2003;60:837–844. doi: 10.1001/archpsyc.60.8.837. [DOI] [PubMed] [Google Scholar]
- Cummings EM, lannotti RJ, Zahn-Waxler C. Aggression between peers in early childhood: Individual continuity and developmental change. Child Development. 1989;60:887–895. doi: 10.1111/j.1467-8624.1989.tb03521.x. [DOI] [PubMed] [Google Scholar]
- Earls F, Jung KG. Temperament and home environment characteristics as causal factors in the early development of childhood psychopathology. Journal of the American Academy of Child and Adolescent Psychiatry. 1987;26:491–498. doi: 10.1097/00004583-198707000-00005. [DOI] [PubMed] [Google Scholar]
- Fischer M, Rolf JE, Hasazi JE, Cummings L. Follow-up of a preschool epidemiological sample; Cross-age continuities and predictions of later adjustment with internalizing and externalizing dimensions of behavior. Child Development. 1984;55:137–150. [PubMed] [Google Scholar]
- Dohrenwend BP, Levav I, Shrout PE, Schwartz S, Naveh G, Link BG, Skodol AE, Stuve A. Socioeconomic status and psychiatric disorders: The causation-selection issue. Science. 1992;255:946–952. doi: 10.1126/science.1546291. [DOI] [PubMed] [Google Scholar]
- Harvey EA, Youngwirth SD, Thakar DA, Errazuriz PA. Predicting attention-deficit/hyperactivity disorder and oppositional defiant disorder from preschool diagnostic assessments. Journal of Consulting and Clinical Psychology. 2009;77:349–354. doi: 10.1037/a0014638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keenan K, Shaw DS. Developmental and social influences on young girls' behavioral and emotional problems. Psychological Bulletin. 1997;121:97–113. doi: 10.1037/0033-2909.121.1.95. [DOI] [PubMed] [Google Scholar]
- Keenan K, Shaw DS. Starting at the beginning: Identifying etiological factors for antisocial behavior in the first years of life. In: Lahey BB, Moffitt TE, Caspi A, editors. The Causes of Conduct Disorder and Serious Delinquency. New York: Guilford Publications, Inc.; 2003. pp. 153–181. [Google Scholar]
- Keenan K, Wakschlag LS, Danis B, Hill C, Humphries M, Duax J, Donald R. Further evidence of the reliability and validity of DSM-IV ODD and CD in preschool children. Journal of the American Academy of Child and Adolescent Psychiatry. 2007;46:457–468. doi: 10.1097/CHI.0b013e31803062d3. [DOI] [PubMed] [Google Scholar]
- Keenan K, Wakschlag LS. Are ODD and CD symptoms normative behaviors in preschoolers? A comparison of referred and non-referred children. American Journal of Psychiatry. 2004;161:356–358. doi: 10.1176/appi.ajp.161.2.356. [DOI] [PubMed] [Google Scholar]
- Kim-Cohen J, Arsenault L, Caspi A, Tomas MP, Taylor A, Moffit TE. Validity of DSM-IV Conduct disorder in 4 1/2–5 year old children: A longitudinal epidemiological study. American Journal of Psychiatry. 2005;162:1108–1117. doi: 10.1176/appi.ajp.162.6.1108. [DOI] [PubMed] [Google Scholar]
- Kim-Cohen J, Arsenault L, Newcombe R, Adams F, Bolton H, Cant L, Delgado K, Freeman J, Golaszewski A, Kelesidi K, Matthews C, Mountain N, Oxley D, Watson S, Werts H, Caspi A, Moffitt TE. Five-year predictive validity of DSM-IV Conduct disorder research diagnosis in 4 ½-5-year-old children. European Child and Adolescent Psychiatry. 2009;18:284–291. doi: 10.1007/s00787-008-0729-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim-Cohen J, Caspi A, Moffitt TE, Harrington H, Milne BJ, Poulton R. Prior juvenile diagnoses in adults with mental disorder: Developmental follow-back of a prospective-longitudinal cohort. Archives of General Psychiatry. 2003;60:709–717. doi: 10.1001/archpsyc.60.7.709. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Loeber R, Hart E, Frick PJ, Applegate B, Zhang Q, Green SM, Russo MF. Four-year longitudinal study of conduct disorder in boys: Patterns and predictors of persistence. Journal of Abnormal Psychology. 1995;104:83–93. doi: 10.1037/0021-843X.104.1.83. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Pelham WE, Loney J, Kipp H, Ehrhardt A, Lee SS, Willcutt EG, Hartung CM, Chronis A, Massetti G. Three-year predictive validity of DSM-IV attention deficit hyperactivity disorder in children diagnosed at 4–6 years of age. American Journal of Psychiatry. 2004;161:2014–2020. doi: 10.1176/appi.ajp.161.11.2014. [DOI] [PubMed] [Google Scholar]
- Lavigne JV, Arend R, Rosenbaum D, Binns HJ, Christoffel KK, Gibbons R. Psychiatric disorders with onset in the preschool years: I. Stability of diagnoses. Journal of the American Academy of Child and Adolescent Psychiatry. 1998;37:1246–1254. doi: 10.1097/00004583-199812000-00007. [DOI] [PubMed] [Google Scholar]
- Lavigne JV, Lebailly SA, Hopkins J, Gouze KR, Binns HJ. The prevalence of ADHD, ODD, depression, and anxiety in a community sample of 4-year-olds. Journal of Clinical Child and Adolescent Psychology. 2009;38:315–328. doi: 10.1080/15374410902851382. [DOI] [PubMed] [Google Scholar]
- Lee SS, Lahey BB, Owens EB, Hinshaw SP. Few preschool boys and girls with ADHD are well-adjusted during adolescence. Journal of Abnormal Child Psychology. 2008;36:373–383. doi: 10.1007/s10802-007-9184-6. [DOI] [PubMed] [Google Scholar]
- Luby JL, Belden AC, Sullivan J, Hayen R, McCadney A, Spitznagel E. Shame and guilt in preschool depression: evidence for elevations in self-conscious emotions in depression as early as age 3. Journal of Child Psychology and Psychiatry. 2009;50:1156–1166. doi: 10.1111/j.1469-7610.2009.02077.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luby JL, Si X, Belden AC, Tandon M, Spitznagel E. Preschool depression: homotypic continuity and course over 24 months. Archives of General Psychiatry. 2009;66:897–905. doi: 10.1001/archgenpsychiatry.2009.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McClellan J, Speltz M. Psychiatric diagnosis in preschool children. Journal of the American Academy of Child and Adolescent Psychiatry. 2003;42:129. doi: 10.1097/00004583-200302000-00002. [DOI] [PubMed] [Google Scholar]
- Messer J, Goodman R, Rowe R, Meltzer H, Maughan B. Preadolescent conduct problems in girls and boys. Journal of the American Academy of Child and Adolescent Psychiatry. 2006;45:184–191. doi: 10.1097/01.chi.0000186403.13088.d8. [DOI] [PubMed] [Google Scholar]
- Moffitt TE, Arseneault L, Jaffee SR, Kim-Cohen J, Koenen KC, Odgers CL, Slutske WS, Viding E. Research review: DSM-V Conduct disorder: Research needs for an evidence base. Journal of Child Psychology and Psychiatry. 2008;49:3–33. doi: 10.1111/j.1469-7610.2007.01823.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierce EW, Ewing LJ, Campbell SB. Diagnostic status and symptomatic behavior of hard-to-manage preschool children in middle childhood and early adolescence. Journal of Clinical Child and Adolescent Psychology. 1999;28:44–57. doi: 10.1207/s15374424jccp2801_4. [DOI] [PubMed] [Google Scholar]
- Ringel JS, Sturm R. National estimates of mental health utilization and expenditures for children in 1998. Journal of Behavioral Health Services Research. 2001;28:319–333. doi: 10.1007/BF02287247. [DOI] [PubMed] [Google Scholar]
- Rowe R, Maughan B, Costello EJ, Angold A. Defining oppositional defiant disorder. Journal of Child Psychology and Psychiatry. 2005;46:1309–1316. doi: 10.1111/j.1469-7610.2005.01420.x. [DOI] [PubMed] [Google Scholar]
- Setterberg S, Bird H, Gould M, Saffer D, Fisher P. Parent and interviewer versions of the Children’s Global Assessment Scale. New York: Columbia University; 1992. [Google Scholar]
- Stevenson J, Richman N, Graham PJ. Behaviour problems and language abilities at three years and behavioural deviance at eight years. Journal of Child Psychology and Psychiatry. 1985;26:215–230. doi: 10.1111/j.1469-7610.1985.tb02261.x. [DOI] [PubMed] [Google Scholar]
- Thomas JM, Guskin KA. Disruptive behavior in young children: What does it mean? Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40:44–51. doi: 10.1097/00004583-200101000-00015. [DOI] [PubMed] [Google Scholar]