Abstract
Background
The present study was designed to examine the influence of suicidality on relapse in alcohol-dependent patients. Specifically, a lifetime suicide attempt at baseline was used to predict relapse in the year after treatment. Also, the unique contribution of impulsive suicide attempts was examined.
Methods
A total of 154 patients with alcohol dependence, consecutively admitted to four addiction treatment facilities in Warsaw, Poland participated in the study. Of the 154 eligible patients, 118 (76.6%) completed a standardized follow-up assessment at 12 months.
Results
Previous suicide attempts were common in adults treated for alcohol dependence with 43% patients in the present sample reporting an attempt at some point during their lifetime. Additionally, more than 62% of those with a lifetime suicide attempt reported making an impulsive attempt. Lifetime suicide attempts were not associated with post-treatment relapse (chi-square=2.37, df=1, p=0.124). However, impulsive suicide attempts strongly predicted relapse (OR=2.81, 95%C.I. = 1.13–6.95, p=0.026) and time to relapse (OR=2.10, 95% C.I. = 1.18–3.74, p=0.012) even after adjusting for other measures of baseline psychopathology, depression, impulsivity, hopelessness and alcohol use severity.
Conclusions
This study is the first to document the relationship between pre-treatment impulsive suicide attempts and higher likelihood of post-treatment relapse in alcohol-dependent patents. Clinicians should routinely conduct an assessment for previous suicide attempts in patients with alcohol use disorders, and when impulsive suicidality is reported, they should recognize the increased risk for relapse and formulate their patients' treatment plans accordingly with the goals of reducing both alcoholic relapse and suicide rates.
Keywords: suicide, alcohol dependence, impulsivity, treatment, relapse
1. Introduction
Alcohol dependence is characterized by a prolonged course of alcohol-related problems and a persistent vulnerability to relapse (Dawson et al., 2007; Jin et al., 1998; Moos and Moos, 2006). The high risk of relapse remains following treatment, even though, on average, participation in alcohol treatment results in improvements in multiple domains of life (Emrick, 1974; Miller et al., 2001). For example, the Project Match Research Group found that between 65% and 81% of alcohol-dependent patients experienced a relapse over the 1-year follow-up period (Project MATCH, 1997). In order to better understand the process of relapse and improve outcomes for individuals with alcohol dependence, more work is needed to identify which patients are particularly susceptible to a relapse following alcohol treatment (Brady and Sonne, 1999; Brown et al., 1995; Witkiewitz and Marlatt, 2004).
Psychiatric comorbidity has received considerable attention as a potential predictor of poor treatment outcomes in alcohol-dependent individuals (Bradizza et al., 2006; Kranzler et al., 1996; Krushner et al., 2005). Several studies have found that affective, anxiety, and antisocial personality disorders are associated with a high risk of relapse to heavy drinking (Driessen et al., 2001; Galen et al., 2000; Greenfield et al., 1998; Kranzler et al., 1996; Strowig, 2000; Verheul et al., 1998; Willinger et al., 2002). In addition to psychiatric diagnoses, severity of psychopathology also has been found to be more pronounced among patients who had relapsed to alcohol and/or drug use compared with abstainers (Curran et al., 2000; Hasin et al., 2002; McLellan et al., 1983; Snow and Anderson, 2000).
However, not all prior research has described a consistent relationship between comorbid psychopathology and poor alcohol treatment outcomes (Miller et al., 1997; Sellman and Joyce, 1996). In fact, some prior research has found that alcohol-dependent patients with comorbid major depression had longer periods of post-treatment abstinence and a lower risk of relapse than patients without depression, especially women (Kranzler et al., 1996; Rounsaville et al., 1987). One possible explanation for these inconsistent results is the considerable heterogeneity that exists within psychiatric diagnoses. An alternative approach to examining the relationship between psychopathology and relapse is to focus on a specific symptom (or set of symptoms) that likely reflects a narrower group of patients with elevated psychopathology.
One such aspect of psychopathology which has received comparatively little attention as a predictor of relapse in alcohol dependence is suicidality. Suicide attempts may be linked to relapse because research in alcohol and/or drug users indicates that they can reflect high levels of both impulsivity and depression (Aharonovich et al., 2002; Dougherty et al., 2004; Koller et al., 2002; Swann et al., 2005), which are important predictors of relapse (e.g., Fox et al., 2008; Greenfield et al., 1998; Miller, 1991). Thus, examining past suicidal behavior in alcohol-dependent patients could be one way to focus on a group of patients with more severe psychopathology who are also at a higher risk for relapse. Additionally, asking about past suicide attempts may be more clinically straightforward compared to assessing for diagnostic type and severity of psychiatric disorders in alcohol-dependent patients.
Previous research documents the high prevalence of lifetime suicide attempts in patients with alcohol dependence. According to some estimates, more than 40% of all patients seeking treatment for alcohol dependence report a suicide attempt at some point in their lifetime (Anderson et al., 1995; Koller et al., 2002; Roy, 2003). Additionally, impulsive suicide attempts are common in those with an alcohol use disorder (Ikeda et al., 2001) and may be especially important in understanding suicidal behaviors and the process of relapse in individuals with alcohol dependence (Conner, 2004). However, research has yet to establish the impact of suicide attempts on risk for relapse in alcohol-dependent patients.
Limited research has focused on recent suicide attempts in mixed samples of drug and alcohol users and has generally found little difference in the post-treatment drinking behaviors of those with and without a recent attempt (Harrison and Asche, 1999; Ilgen et al., 2005; Ilgen et al., 2004). The failure to find a difference may result from not further classifying recent attempts into subcategories such as impulsive vs. non-impulsive. Moreover, this research on recent attempts likely misses the larger group of individuals with suicide attempts at some prior point in their lifetimes. Schuckit (1986), for example, found that lifetime suicide attempts in a sample of 450 alcohol-dependent men predicted increased alcohol-related problems at 1-year follow-up. Thus, more research is needed to better understand how lifetime suicide attempts relate to post-treatment alcohol use.
The present study was designed to examine the impact of suicidality on relapse in alcohol-dependent patients. Specifically, a lifetime suicide attempt at baseline was used to predict time to relapse in the year after treatment in a sample of patients treated for alcohol dependence in Warsaw, Poland. In addition to examining lifetime suicide attempts as a predictor of relapse, the unique contribution of impulsive suicide attempts was also examined.
2. Methods
2.1. Participants
A total of 300 patients with alcohol dependence, consecutively admitted to four addiction treatment facilities (2 outpatient and 2 residential) in Warsaw, Poland, were approached and invited to participate in the study. One hundred and five of these patients (35%) refused (i.e., did not provide consent) to participate, and 41 (13.7%) left the program prior to completion of the baseline assessment, leaving a final intake sample of 154 patients.
Of the 154 eligible patients, 118 (76.6%) completed a standardized follow-up assessment approximately 11 months (SD: 2.8; referred to as the 1-year follow-up) following baseline and constitute the sample of interest for this study. Further description of the sample is provided in Table 1. Followed patients (n=118) were more likely than non-followed patients (n=36) to be married or in a stable relationship (87% vs.71%, p=0.04), have more years of education (13.5 vs. 12.0 years; p=0.04), and be employed (86.3% vs. 71.6%; p=0.04). They also drank less alcohol during the last 3 months prior to the baseline assessment (mean: 183.2 [SD: 115.6] vs. 278.7 [179.5] g daily; p=0.013) than those without follow-up data. The two groups, however, did not differ in terms of age, gender, financial situation, social support, other substance use and substance use disorders, past substance use disorder treatment, parental history of substance abuse, legal status, psychiatric severity, impulsivity, or history of suicide attempts, and current suicidal ideation.
Table 1.
Baseline Sociodemographic and Clinical Characteristics of the Study Sample
| Characteristics | Participants N=154 |
|---|---|
| Age (years); mean ± SD | 43.65 ± 9.64 |
| Gender (males); N (%) | 117 (76.0) |
| Education (years); mean ± SD | 12.27 ± 3.66 |
| Married; N (%) | 73 (47.4) |
| Drinking days in past 3 months; mean ± SD | 24.71 ± 26.72 |
| Number of standard drinks per day; mean ± SD | 20.87 ± 14.12 |
| Severity of psychopathology (GSI; T-score); mean ± SD | 49.95 ± 11.87 |
| Severity of depression (BDI-II); mean ± SD | 19.71 ± 11.54 |
| Hopelessness (BHS); mean ± SD | 5.88 ± 5.07 |
| Impulsiveness (BIS-11); mean ± SD | 71.66 ± 10.42 |
| Prior suicide attempt; N (%) | 66 (42.9) |
| Impulsive suicide attempt; N (%) | 41 (26.6) |
| Recent suicide ideas; N (%) | 26 (16.9) |
| Family history of suicide; N (%) | 23 (14.9) |
SD = standard deviation; GSI = General Severity Index derived from Brief Symptom Inventory; BDI-II = Beck Depression Inventory version 2; BHS = Beck Hopelessness Scale; BIS-11 = Barratt Impulsiveness Scale
2.2. Procedures
This study was designed to be a prospective, naturalistic examination of the impact of baseline suicidality and impulsivity on 1-year post-treatment drinking outcomes. Only patients with a diagnosis of alcohol dependence were eligible to participate. Alcohol and substance use disorder diagnoses were made according to the DSM-IV criteria by the consensus of an addiction-specialized multidisciplinary team including a psychiatrist and an addiction therapist.
Patients completed standardized assessments as part of the research protocol. Patients were informed that they would answer questionnaires about their health, substance use, and other aspects of their lives to evaluate the effectiveness of the treatment program. After data collection and cleaning were completed, linkages between personal identifiers and the dataset were destroyed. Both the Medical Institutional Review Board at the University of Michigan and the Bioethics Committee at the Medical University of Warsaw approved the research protocol and use of research data for analyses and publication.
Patients were recruited from outpatient and residential alcohol treatment programs at four treatment centers in Warsaw, Poland. Programs were abstinence-based and combined group and individual therapy as well as elements of 12-step facilitation and relapse prevention. Intensive outpatient treatment consisted of group and individual therapy 3 days a week for 3 hours per day. After 8–12 weeks of full programming, patients attended another 40 weeks of lower intensity outpatient continuing care treatment. Residential treatment programs lasted for 8 weeks and included intensive daily group therapy and individual therapy offered 3 hours a week.
Of the 154 patients, 34 (22.1 %) attended outpatient and 120 (77.9%) attended residential treatment programs. The two treatment groups differed in education level (mean 14.1, SD: 2.7 years for outpatients vs. mean 11.7, SD: 3.8 years for residential patients, p=0.001) and employment status (70.6% vs. 22.5%, respectively; p<0.001). The groups did not significantly differ from one another in any other baseline characteristics. The total amount of psychotherapy (group and individual) during follow-up was comparable in patients from different settings: outpatients in the studied population received more formal treatment (hours of therapy) than did inpatients, but the difference was not statistically significant (122 vs. 81 hours; U=944, p=0.135). For the purposes of this study the two treatment groups were combined (n=154) due to similar amount of treatment received, no significant association between the amount of treatment administered and relapse rate or time to relapse, and a small sample size of outpatients.
2.3. Measures
A comprehensive process was used to ensure that the measures in this study were properly translated into Polish. In instances when Polish-language versions were unavailable, the original authors or the distributing companies that own copyright for the relevant instruments were contacted and their agreement sought. The methodology used for the translations was the simultaneous forward/single back-translation method (Cella et al., 1996; Guillemin et al., 1993; Hunt, 1988). Essentially, each instrument was translated simultaneously by two independent native Polish speaking professionals. These individuals then reached an agreement for the final version of forward translation. The forward version was then back translated by a native English speaking professional, and the reconciled forward and the back-translation were then submitted to a bilingual/bicultural expert in linguistics and compared to the original with close collaboration of the original author/company. Finally, the best final forward translation was subjected to pilot testing with a population of Polish target patients to ensure semantic and content equivalence.
Questions related to suicidality were drawn from the Mini International Neuropsychiatric Interview (MINI) (Sheehan et al., 1998). The MINI is a short, structured interview for both DSM-IV and ICD-10 psychiatric diagnoses. The MINI has reasonable validity and reliability in psychiatric patients (Sheehan et al., 1998). Participants were asked a set of questions from the MINI related to attempted suicide. Based on their responses, participants were categorized as either having made a suicide attempt in their lifetime or not. In those with a past suicide attempt, interviewers asked patients how long they had spent planning their most recent suicide attempt. Those attempts with less than 30 minutes of planning prior to the suicide attempt were categorized as “impulsive suicide attempts.” This approach was based on a similar method used previously by other research groups (Conner et al., 2006; Simon et al., 2001).
The University of Arkansas Substance Abuse Outcomes Module (SAOM) is a self-administered questionnaire that collects information about demographics, family history, substance use, work functioning, legal problems, and social support (Smith et al., 1996). Questions included the quantity and frequency of drinking in the past 1 month. Smith et al. (1996) reported excellent test-retest reliability for these questions (ICC=0.87) and concurrent validity with the Time-Line Follow-Back Interview (r=0.74). The SAOM also includes a 17-item severity of dependence scale (Smith et al., 1996).
Psychiatric severity was assessed using the Brief Symptom Inventory (BSI) (Derogatis and Melisaratos, 1983), a self-administered instrument that quantifies symptom distress in the past 7 days. Its General Severity Index (GSI) was calculated as a T-score, which was keyed to healthy non-patient participants with separate norms for men and women. In prior research, the GSI of the BSI has demonstrated good reliability (Derogatis and Melisaratos, 1983).
The measure of impulsivity for this study was the Barratt Impulsiveness Scale (BIS-11) (Barratt, 1959; Patton et al., 1995). This is a 30-item self-report questionnaire that has been validated to assess impulsiveness in various populations including substance-dependent individuals as well as violent suicide attempters (Allen et al., 1998; Patton et al., 1995).
The Beck Hopelessness Scale (BHS) (Beck et al., 1974) was used to measure the extent of negative attitudes about the future (pessimism) as perceived by patients. The scale has been used as an indirect indicator of suicide risk in depressed individuals who have made suicide attempts and for detection of hopelessness in adult populations. The BHS is a fully structured instrument that is self-administered by the participant. Previous work has established the strong reliability and validity of this measure (Beck and Steer, 1993; Keller and Wolfersdorf, 1993).
Depression was measured using the Beck Depression Inventory (BDI) (Beck et al., 1961). The BDI has 21 items and the total score ranges from 0 to 63, reflecting the intensity of symptoms. There is considerable literature on the BDI, and its reliability and validity in mental health contexts are well established.
At the one year follow-up assessment, the Alcohol Time-Line Follow-Back Interview (TLFB) (Sobell et al., 1979; Sobell et al., 1988) was used to evaluate the frequency of alcohol use during the entire follow-up period. The TLFB data allowed us to derive two primary outcomes: (1) post-treatment relapse defined as any drinking in the follow-up period (no/yes) and (2) time to relapse to any drinking.
2.4. Data analyses
The analyses focused on identifying the association between lifetime suicide attempts and impulsive suicide attempts and post-treatment relapse. We began by examining the bivariate relationship between lifetime suicide attempt, impulsive suicide attempt, and the indicator of relapse within the follow-up interval using chi square analyses. Additionally, we compared the mean time to relapse between those with an impulsive suicide attempt and those without. Then, we conducted multivariate analyses to examine the impact of impulsive suicide attempts on risk of relapse after accounting for all other potentially important baseline factors. We conducted two separate multivariate analyses: one multiple logistic regression predicting relapse and a Cox Proportional Hazards analysis to predict time to relapse.
3. Results
3.1. Baseline suicidality and relapse
Among the 154 patients entering alcohol treatment, 66 patients (42.9%) reported at least one suicide attempt in the past. Among all suicide attempters, 62.1% (or 41 individuals) reported that their last suicide attempt was impulsive. Among those patients who reported past suicide attempts, the most frequent methods of attempt were: 1) taking medication (n=27, 40.9%); 2) hanging (n=16, 24.2%); 3) cutting (n= 9, 13.6%); 4) jumping from a high place (n=9, 13.6%); 5) poisoning with gas or other toxic substances (n=3, 4.5%); 6) using a gun (n=2, 3.0%). At the one-year follow-up assessment, relapse to alcohol use occurred in 59 (50%) of 118 patients. Time to relapse averaged 226 (SD=129) days.
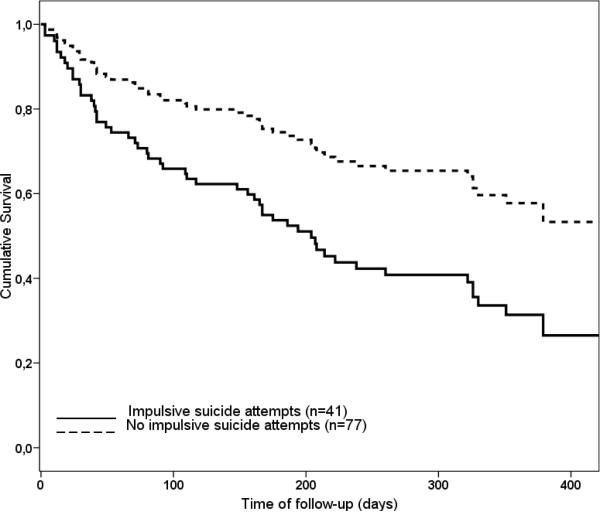
Lifetime suicide attempts were not significantly associated with post-treatment relapse (chi-square=2.37, df =1, p=0.124). However, impulsive suicide attempts were significantly associated with an increased probability of relapse (chi-square=6.05, df =1, p=0.014). Specifically, 65.5% of those with an impulsive suicide attempt at baseline relapsed during the follow-up interval compared to 39.3% of those without an impulsive attempt. Thus, the report of a prior impulsive attempt was associated with an increased odds of relapse of 3.02 (95% C.I. =1.25–7.26; p=0.014). Patients with prior impulsive suicide attempts also relapsed to alcohol use earlier than patients without a history of impulsive attempts (mean 168 [SD=134] days vs. 245 [122] days; t=−2.85, df =117, p=0.005) (Fig. 1).
Fig. 1.
Survival time to first relapse. Relapse = any drinking in the follow-up. Survival analysis: Kaplan-Meier log rank statistics = 7.9, df = 1, p = 0.005.
There were 8 patients who attempted suicide during the follow-up period. Relapse rates among patients who attempted suicide during the study period were higher but not significantly higher than those who did not attempt suicide (62.5% vs. 44.5%; p=0.268). There were no significant associations between method of suicide attempt or family history of suicide and relapse rates and times to relapse.
3.2. Multivariate analyses of impulsive suicide attempt and relapse
We conducted a logistic regression analysis examining the association between impulsive suicide attempts and relapse after adjusting for other potentially important baseline characteristics (baseline demographics, severity of psychopathology, severity of depression, impulsivity, hopelessness, and severity of pre-treatment alcohol use). In this analysis (see Table 2), even after controlling for these variables, impulsive suicide attempts were significantly related to a higher likelihood of post-treatment relapse (OR=2.81, 95% C.I. = 1.13–6.95, p=0.026). Next, we conducted a similar survival analysis controlling for the same set of baseline characteristics and predicting time to relapse (Table 3). In this analysis, impulsive suicide attempts were associated with a shorter time to relapse (Beta=0.740, OR=2.10, 95% C.I. = 1.18–3.74, p=0.012).
Table 2.
Logistic Regression Analysis Results for Predictors of Relapse
| Predictor variable | Odds Ratio | 95% CI | p |
|---|---|---|---|
| Prior impulsive suicide attempt | 2.81 | 1.13–6.95 | 0.026 |
| Age | 0.99 | 0.95–1.04 | 0.683 |
| Gender | 1.39 | 0.29–1.85 | 0.521 |
| Marital status | 0.92 | 0.41–2.09 | 0.921 |
| Baseline psychiatric severity (GSI) | 0.98 | 0.94–1.04 | 0.575 |
| Hopelessness score (BHS) | 1.07 | 0.95–1.19 | 0.275 |
| Severity of Depression (BDI-II) | 1.01 | 0.95–1.06 | 0.891 |
| Impulsiveness (BIS) | 1.01 | 0.95–1.06 | 0.897 |
| Drinking days (past 3 months) | 1.01 | 0.99–1.03 | 0.091 |
GSI = General Severtiy Index derived from Brief Symptom Inventory; BDI-II = Beck Depression Inventory version 2; BHS = Beck Hopelessness Scale; BIS-11 = Barratt Impulsiveness Scale
Table 3.
Cox Proportional Hazard Regression Analysis Results for Predictors of Time to Relapse
| Predictor variable | Beta | OR | 95% CI | p |
|---|---|---|---|---|
| Prior impulsive suicide attempt | 0.740 | 2.10 | 1.18–3.74 | 0.012 |
| Age | −0.015 | 0.99 | 0.95–1.02 | 0.392 |
| Gender | 0.209 | 1.23 | 0.62–2.44 | 0.548 |
| Marital status | 0.085 | 1.09 | 0.60–1.96 | 0.777 |
| Baseline psychiatric severity (GSI) | −0.008 | 0.99 | 0.96–1.03 | 0.656 |
| Hopelessness score (BHS) | 0.035 | 1.04 | 0.96–1.11 | 0.339 |
| Severity of Depression (BDI-II) | 0.009 | 1.01 | 0.97–1.05 | 0.617 |
| Impulsiveness (BIS) | 0.008 | 1.01 | 0.97–1.04 | 0.676 |
| Drinking days (past 3 months) | 0.007 | 1.01 | 0.99–1.02 | 0.185 |
GSI = General Severtiy Index derived from Brief Symptom Inventory; BDI-II = Beck Depression Inventory version 2; BHS = Beck Hopelessness Scale; BIS-11 = Barratt Impulsiveness Scale
3.3. Supplementary Analyses
Because prior research indicates that individuals who are lost to follow-up are generally more likely to have relapsed than individuals with follow-up data (Bottlender and Soyka, 2005; Mann et al., 2004; Mann et al., 2005), we re-ran the primary multivariate regression analyses with all missing data counted as relapsed. Thus, this analysis now included 154 cases, 64 of whom were classified as non-relapsed and 90 of whom were now classified as relapsed. In these analyses, the effect of impulsive suicide attempt on the likelihood of relapse remained significant (OR=2.34, 95%C.I. = 1.01–5.43, p=0.049) as well as the effect on the time to relapse (Beta=0.627, OR=1.87, 95% C.I. = 1.10–3.19, p=0.021). An additional set of analyses examined whether initial treatment setting accounted for the association between baseline impulsive suicide attempt and relapse. The results of these analyses indicate that controlling for treatment setting (residential vs. outpatient) in the logistic regression and Cox regression models did not change the relationship between impulsive suicide attempts and treatment outcomes.
4. Discussion
Previous suicide attempts are common in adults treated for alcohol dependence in Poland, with as many as 43% of patients in the present sample reporting an attempt at some point during their lifetime. Additionally, more than 62% of patients who reported a prior suicide attempt indicated that they had spent less than 30 minutes in planning their most recent attempt. A history of impulsive suicide attempts strongly predicted time to relapse in the year after treatment. Also, even after controlling for other related risk factors such as baseline severity of alcohol use, depression, and impulsivity, a history of an impulsive suicide attempt was the strongest single predictor of earlier time to relapse in the present sample.
These findings are consistent with the previously described association between problematic alcohol use and suicidality (Kessler et al., 1999). The rates of a suicide attempt in the present sample are also broadly consistent with other samples of patients seen for treatment of drug dependence (Johnsson and Fridell, 1997). Clearly, many patients who present to treatment for alcohol problems have previously engaged in suicidal behaviors and these individuals are at an elevated risk for future suicidal behaviors (Cornelius et al., 2004; Ilgen et al., 2007; Wines et al., 2004).
The rates of impulsive suicide attempts in patients seeking treatment for alcohol dependence are particularly striking. In a prior study, Simon and colleagues (2001) reported that 40% of all suicide attempts in their sample were impulsive. Others have highlighted the potential role of alcohol use as an important component of impulsive suicidal behaviors (Conner, 2004; Conner and Duberstein, 2004). The rate of impulsive suicide attempts among those with a lifetime suicide attempt in the present sample of 62% likely reflects the severity of alcohol dependence in this sample.
This study was one of only a few known prospective investigations of the role of pre-treatment suicidality as a predictor of post-treatment alcohol use. One prior study found that suicide attempts in a sample of 450 alcohol-dependent men predicted increased alcohol-related problems at 1-year follow-up (Schuckit, 1986). Three other studies of patients seeking substance use disorder treatment found that recent attempts were generally not associated with poorer post-treatment substance use outcomes; in fact, some patients treated in residential settings reported better outcomes than other patients without recent suicide attempts at baseline (Harrison and Asche, 1999; Ilgen et al., 2005; Ilgen et al., 2004). In the present study, a lifetime history of a prior suicidal attempt was not associated with relapse after treatment. However, the present findings indicate that a subset of patients with prior attempts, those who made impulsive attempts, were at an elevated risk for relapse. Thus, the discrepancy in findings in terms of the relationship between suicide attempts and relapse may be influenced by the proportion of impulsive suicide attempters included in each study.
In this sample, impulsive suicide attempts predicted relapse even after adjusting for other measures of impulsivity and baseline severity. As noted earlier, Conner and colleagues have highlighted the strong overlap between alcohol use, impulsivity, and suicide risk (Conner, 2004; Conner and Duberstein, 2004). Much of this research is understandably focused on understanding and modeling risk for suicidality. However, the present findings indicate that considerations of impulsive suicide attempts are also important in understanding risk for relapse. In all likelihood, those with prior impulsive suicide attempts have state-like characteristics that place them at increased risk for both future suicidal behavior and substance use. In fact, a cyclical pattern may exist in which a high probability for relapse in those with prior impulsive attempts places them at an even greater risk for future suicide attempts and suicide mortality. More work is needed to better understand the key distal and proximal risk factors that are potentially involved in this process.
Other possible factors may explain why individuals with impulsive suicide attempts are particularly vulnerable to relapse. Those who make impulsive suicide attempts, as compared to those who engage in more planning prior to an attempt, could be manifesting a more extreme form of behavioral impulsivity that applies both to suicidal acts and use of alcohol. In this study, higher levels of impulsivity as measured by BIS-11 were not associated with higher relapse rates or shorter times to relapse. Others have reported that severe suicide attempts are associated with behavioral measures of impulsivity but not self-report measures of impulsive traits (Swann et al., 2005). We suspect that “impulsivity” as indicated by having made an impulsive suicide attempt could be a stronger measure of high-risk impulsivity than the more general measures of impulsive traits that are typically utilized (such as the Barratt Impulsiveness Scale). Additionally, prior research has shown an association between suicide attempts, impulsivity, alcohol dependence and a deficiency in serotonin neurotransmission (Evenden, 1999; Gorwood, 2001; Joiner et al., 2002; Mann et al., 2001). It is possible that impulsive suicide attempts may reflect a level of serotonergic hypofunctioning that could be particularly important for understanding relapse in alcohol-dependent individuals. The nature and associated characteristics of impulsive suicide attempts in alcohol-dependent individuals requires further study.
The present findings should be considered with caution for several reasons. This study is based on a sample of four clinics in Warsaw, Poland, and the extent to which these findings generalize to the rest of Poland or to samples from other countries is unknown. Due to concerns about lack of power and the broad similarities in patient attributes and treatment outcomes of patients from outpatient and residential settings, we combined the data from all clinics into a single dataset. Additionally, a series of supplementary analyses indicated that treatment setting did not significantly influence the primary findings in this study. Combining the two samples allowed for better representation of the population of alcohol-dependent patients in Poland. Future work could examine the extent to which specific aspects of the treatment context moderate the effect of impulsive suicide attempts on risk of relapse. Similarly, due to low numbers of women, we did not conduct the analyses separately in men and women. However, the primary analyses indicate that the effects of interest remain after including gender as a covariate in the models.
The rates of use of other illicit substances in this sample (although likely representative of Polish alcohol-dependent patients) are clearly lower than those seen in other countries like the United States. Additionally, only 51% of those individuals who were initially approached to participate in the study actually consented and completed the baseline assessments. Thus, our sample is not fully representative of all patients seeking alcohol treatment in these four clinics. It is possible that refusals may have been more common in those with greater severity of psychopathology. Unfortunately, refusal to participate in the study (n=105; 35%) occurred prior to the consent process so no further information was available about these individuals. Thus, we also do not have any information about severity of substance use or psychopathology in these individuals. Anecdotally, based on our informal interactions with those who did participate, many refused because of potential concerns about confidentiality. This rate of refusal may be partially influenced by cultural factors (i.e., general concerns in Polish society about disclosing personal information, and some distrust among the adult population about being followed over time by a government-related institution, i.e., Medical University of Warsaw). However, we did control for level of psychopathology as a covariate in our primary analyses and including this variable did not diminish the strength of the relationship between impulsive suicide attempts and relapse. Moreover, the rate of follow-up of recruited patients was relatively high (77%), increasing our confidence that the present findings accurately reflect the make-up of the baseline sample.
The primary findings were based on a small subset of questions from the MINI. Additionally, the assessment of impulsive suicide attempt was based on a single question that was added as a supplement to the suicide-related section of the MINI. Although the instrument has been found to have sound psychometric properties in other samples, more finely grained examinations of the validity of single items from the MINI (and the supplemental item on impulsive suicide attempts) do not exist. Thus, we do not know to what extent the report of prior suicidality (and impulsive suicidality) corresponded to actual suicidal behaviors. However, most prior work on suicidality in treatment-seeking substance-dependent patients has also utilized single-item measures to assess for past attempts (e.g., Ilgen et al., 2007). In general, research on suicidality in patients with substance use disorders would benefit from the use of more comprehensive measures of suicidality.
Similarly, the primary outcome measure, time to relapse, was based on data collected during a single 1-year assessment period. Although previous research has demonstrated that timeline follow-back methods can provide accurate data (Sobell et al., 1986), these approaches are still vulnerable to the influence of recall bias. The use of multiple assessments of post-treatment drinking, biochemical corroboration, or corroboration from a significant other would likely increase the sensitivity and validity of these measures.
The design of the present study did not allow for the comprehensive assessment of potential mediators of the relationship between prior suicidality and relapse in alcohol-dependent patients. Thus, the exact mechanisms that explain this relationship are not known. Also, this design did not allow for the examination of the extent to which engagement in specific aspects of treatment might influence the relationship between prior suicidality and subsequent relapse. Future research with multiple assessment points prior to the time of relapse could identify the proximal changes that could explain how impulsive suicide attempts lead to relapse and highlight the ways that treatment providers could intervene in this process.
Despite these limitations, this study is the first of which we are aware to document the relationship between pre-treatment impulsive suicide attempts and post-treatment relapse in alcohol-dependent patents. Clearly, impulsive suicidal behaviors are common in alcohol-dependent patients and these patients are at an elevated risk for relapse. Although a good deal of emphasis has been understandably placed on improving the management of suicide risk in patients with prior suicidal behaviors (Institute of Medicine, 2002), the present findings highlight the fact that these patients are also at risk for relapse in addition to future suicidal behaviors. Thus, clinicians should routinely conduct concomitant assessments of suicidality, including the nature of previous attempts, in those receiving evaluation and treatment for alcohol use disorders. When a history of impulsive suicidality is obtained, clinicians should recognize the increased risk for relapse and formulate their patients' treatment plans accordingly. For example, aggressively treating comorbid psychiatric disorders, involving supportive significant others, using pharmacotherapy (e.g., naltrexone or acamprosate), motivating patients for relapse prevention, and monitoring with frequent treatment contacts during early recovery may all be indicated. A combination of such approaches may accomplish the goals of reducing both alcohol relapse and suicide rates.
Acknowledgements
This work was supported by the Fogarty International Center/NIDA International Substance Abuse Research Program grant D43-TW05818, the Fogarty International Center/NIAAA International Collaborative Alcohol and Injury Research Training Program grant 5 D43 TW007569, and the Polish Ministry of Science and Higher Education grant No 2P05D 004 29. We would like to thank the medical staff and patients at “Kolska”, “Pruszkow”, “Petra” and “Solec” Addiction Treatment Centers in Warsaw, Poland for their support of this research.
Footnotes
Conflict of interest All authors declare that they have no conflicts of interest.
References
- Aharonovich E, Liu X, Nunes E, Hasin DS. Suicide attempts in substance abusers: effects of major depression in relation to substance use disorders. Am. J. Psychiatry. 2002;159:1600–1602. doi: 10.1176/appi.ajp.159.9.1600. [DOI] [PubMed] [Google Scholar]
- Allen TJ, Moeller FG, Rhoades HM, Cherek DR. Impulsivity and history of drug dependence. Drug Alcohol Depend. 1998;50:137–145. doi: 10.1016/s0376-8716(98)00023-4. [DOI] [PubMed] [Google Scholar]
- Anderson BA, Howard MO, Walker RD, Suchinsky RT. Characteristics of substance-abusing veterans attempting suicide: a national study. Psychol. Rep. 1995;77:1231–1242. doi: 10.2466/pr0.1995.77.3f.1231. [DOI] [PubMed] [Google Scholar]
- Barratt ES. Anxiety and impulsiveness related to psychomotor efficiency. Percept. Motor Skills. 1959;9:191–198. [Google Scholar]
- Beck AT, Steer RA. Beck Hopelessness Scale Manual. Harcourt Brace; San Antonio, TX: 1993. [Google Scholar]
- Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch. Gen. Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- Beck AT, Weissman A, Lester D, Trexler L. The measurement of pessimism: the hopelessness scale. J. Consult. Clin. Psychol. 1974;42:861–865. doi: 10.1037/h0037562. [DOI] [PubMed] [Google Scholar]
- Bottlender M, Soyka M. Outpatient alcoholism treatment: predictors of outcome after 3 years. Drug Alcohol Depend. 2005;80:83–89. doi: 10.1016/j.drugalcdep.2005.03.011. [DOI] [PubMed] [Google Scholar]
- Bradizza CM, Stasiewicz PR, Paas ND. Relapse to alcohol and drug use among individuals diagnosed with co-occurring mental health and substance use disorders: a review. Clin. Psychol. Rev. 2006;26:162–78. doi: 10.1016/j.cpr.2005.11.005. [DOI] [PubMed] [Google Scholar]
- Brady KT, Sonne SC. The role of stress in alcohol use, alcoholism treatment, and relapse. Alcohol Res. Health. 1999;23:263–271. [PMC free article] [PubMed] [Google Scholar]
- Brown SA, Vik PW, Patterson TL, Grant I, Schuckit MA. Stress, vulnerability and adult alcohol relapse. J. Stud. Alcohol. 1995;56:538–545. doi: 10.15288/jsa.1995.56.538. [DOI] [PubMed] [Google Scholar]
- Cella DF, Lloyd SR, Wright BD. Cross-Cultural Instrument Equating: Current Research and Future Directions. In: Spilker B, editor. Quality of Life and Pharmacoeconomics in Clinical Trials. Second Edition Lippincott-Raven; Philadelphia, PA: 1996. pp. 707–714. [Google Scholar]
- Conner KR. A call for research on planned vs. unplanned suicidal behavior. Suicide Life Threat. Behav. 2004;34:89–98. doi: 10.1521/suli.34.2.89.32780. [DOI] [PubMed] [Google Scholar]
- Conner KR, Duberstein PR. Predisposing and precipitating factors for suicide among alcoholics: empirical review and conceptual integration. Alcohol. Clin. Exp. Res. 2004;28:6S–17S. doi: 10.1097/01.alc.0000127410.84505.2a. [DOI] [PubMed] [Google Scholar]
- Conner KR, Hesselbrock VM, Schuckit MA, Hirsch JK, Knox KL, Meldrum S, Bucholz KK, Kramer J, Kuperman S, Preuss U, Soyka M. Precontemplated and impulsive suicide attempts among individuals with alcohol dependence. J. Stud. Alcohol. 2006;67:95–101. doi: 10.15288/jsa.2006.67.95. [DOI] [PubMed] [Google Scholar]
- Cornelius JR, Clark DB, Salloum IM, Bukstein OG, Kelly TM. Interventions in suicidal alcoholics. Alcohol. Clin. Exp. Res. 2004;28:89S–96S. doi: 10.1097/01.alc.0000127418.93914.ac. [DOI] [PubMed] [Google Scholar]
- Curran GM, Flynn HA, Kirchner J, Booth BM. Depression after alcohol treatment as a risk factor for relapse among male veterans. J. Subst. Abuse Treat. 2000;19:259–65. doi: 10.1016/s0740-5472(00)00107-0. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Goldstein RB, Grant BF. Rates and correlates of relapse among individuals in remission from DSM-IV alcohol dependence: A 3-year follow-up. Alcohol. Clin. Exp. Res. 2007;31:2036–2045. doi: 10.1111/j.1530-0277.2007.00536.x. [DOI] [PubMed] [Google Scholar]
- Derogatis LR, Melisaratos N. The Brief Symptom Inventory: an introductory report. Psychol. Med. 1983;13:595–605. [PubMed] [Google Scholar]
- Dougherty DM, Mathias CW, Marsh DM, Papageorgiou TD, Swann AC, Moeller FG. Laboratory measured behavioral impulsivity relates to suicide attempt history. Suicide Life Threat. Behav. 2004;34:374–385. doi: 10.1521/suli.34.4.374.53738. [DOI] [PubMed] [Google Scholar]
- Driessen M, Meier S, Hill A, Wetterling T, Lange W, Junghanns K. The course of anxiety, depression and drinking behaviours after completed detoxification in alcoholics with and without comorbid anxiety and depressive disorders. Alcohol Alcohol. 2001;36:249–55. doi: 10.1093/alcalc/36.3.249. [DOI] [PubMed] [Google Scholar]
- Emrick CD. A review of psychologically oriented treatment of alcoholism. I. The use and interrelationships of outcome criteria and drinking behavior following treatment. Q. J. Stud. Alcohol. 1974;35:523–549. [PubMed] [Google Scholar]
- Evenden J. Impulsivity: a discussion of clinical and experimental findings. J. Psychopharmacol. 1999;13:180–192. doi: 10.1177/026988119901300211. [DOI] [PubMed] [Google Scholar]
- Fox HC, Hong KA, Sinha R. Difficulties in emotion regulation and impulse control in recently abstinent alcoholics compared with social drinkers. Addict. Behav. 2008;33:388–394. doi: 10.1016/j.addbeh.2007.10.002. [DOI] [PubMed] [Google Scholar]
- Galen LW, Brower KJ, Gillespie BW, Zucker RA. Sociopathy, gender, and treatment outcome among outpatient substance abusers. Drug Alcohol Depend. 2000;61:23–33. doi: 10.1016/s0376-8716(00)00125-3. [DOI] [PubMed] [Google Scholar]
- Gorwood P. Biological markers for suicidal behavior in alcohol dependence. Eur. Psychiatry. 2001;16:410–417. doi: 10.1016/s0924-9338(01)00599-5. [DOI] [PubMed] [Google Scholar]
- Greenfield SF, Weiss RD, Muenz LR, Vagge LM, Kelly JF, Bello LR, Michael J. The effect of depression on return to drinking: a prospective study. Arch. Gen. Psychiatry. 1998;55:259–65. doi: 10.1001/archpsyc.55.3.259. [DOI] [PubMed] [Google Scholar]
- Guillemin F, Bombardier C, Beaton D. Cross-cultural adaptation of health-related quality of life measures: literature review and proposed guidelines. J. Clin. Epidemiol. 1993;46:1417–1432. doi: 10.1016/0895-4356(93)90142-n. [DOI] [PubMed] [Google Scholar]
- Harrison PA, Asche SE. Comparison of substance abuse treatment outcomes for inpatients and outpatients. J. Subst. Abuse Treat. 1999;17:207–220. doi: 10.1016/s0740-5472(99)00004-5. [DOI] [PubMed] [Google Scholar]
- Hasin D, Liu X, Nunes E, McCloud S, Samet S, Endicott J. Effects of major depression on remission and relapse of substance dependence. Arch. Gen. Psychiatry. 2002;59:375–80. doi: 10.1001/archpsyc.59.4.375. [DOI] [PubMed] [Google Scholar]
- Hunt SM. A methodology for the translation of health measures. Galen Research and Consultancy, Manchester. 1988:1–8. [Google Scholar]
- Ikeda RM, Kresnow MJ, Mercy JA, Powell KE, Simon TR, Potter LB, Durant TM, Swahn MH. Medical conditions and nearly lethal suicide attempts. Suicide Life Threat. Behav. 2001;32:60–67. doi: 10.1521/suli.32.1.5.60.24207. [DOI] [PubMed] [Google Scholar]
- Ilgen MA, Harris AH, Moos RH, Tiet QQ. Predictors of a suicide attempt one year after entry into substance use disorder treatment. Alcohol. Clin. Exp. Res. 2007;31:635–642. doi: 10.1111/j.1530-0277.2007.00348.x. [DOI] [PubMed] [Google Scholar]
- Ilgen MA, Tiet Q, Finney JW, Harris AH. Recent suicide attempt and the effectiveness of inpatient and outpatient substance use disorder treatment. Alcohol. Clin. Exp. Res. 2005;29:1664–1671. doi: 10.1097/01.alc.0000179411.88057.3a. [DOI] [PubMed] [Google Scholar]
- Ilgen MA, Tiet Q, Moos R. Outcomes of substance use disorder treatment in suicidal and nonsuicidal male patients. J. Stud. Alcohol. 2004;65:643–650. doi: 10.15288/jsa.2004.65.643. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine . Reducing Suicide: A National Imperative. National Academies Press; Washington, DC: 2002. [PubMed] [Google Scholar]
- Jin H, Rourke SB, Patterson TL, Taylor MJ, Grant I. Predictors of relapse in long-term abstinent alcoholics. J. Stud. Alcohol. 1998;56:640–646. doi: 10.15288/jsa.1998.59.640. [DOI] [PubMed] [Google Scholar]
- Johnsson E, Fridell M. Suicide attempts in a cohort of drug abusers: a 5-year follow-up study. Acta Psychiatr. Scand. 1997;96:362–366. doi: 10.1111/j.1600-0447.1997.tb09930.x. [DOI] [PubMed] [Google Scholar]
- Joiner TE, Jr., Johnson F, Soderstrom K. Association between serotonin transporter gene polymorphism and family history of attempted and completed suicide. Suicide Life Threat. Behav. 2002;32:329–332. doi: 10.1521/suli.32.3.329.22167. [DOI] [PubMed] [Google Scholar]
- Keller F, Wolfersdorf M. Hopelessness and the tendency to commit suicide in the course of depressive disorders. Crisis. 1993;14:173–177. [PubMed] [Google Scholar]
- Kessler RC, Borges G, Walters EE. Prevalence of and risk factors for lifetime suicide attempts in the National Comorbidity Survey. Arch. Gen. Psychiatry. 1999;56:617–626. doi: 10.1001/archpsyc.56.7.617. [DOI] [PubMed] [Google Scholar]
- Koller G, Preuss UW, Bottlender M, Wenzel K, Soyka M. Impulsivity and aggression as predictors of suicide attempts in alcoholics. Eur. Arch. Psychiatry Clin. Neurosci. 2002;252:155–160. doi: 10.1007/s00406-002-0362-9. [DOI] [PubMed] [Google Scholar]
- Kranzler HR, Del Boca FK, Rounsaville BJ. Comorbid psychiatric diagnosis predicts three-year outcomes in alcoholics: a posttreatment natural history study. J. Stud. Alcohol. 1996;57:619–26. doi: 10.15288/jsa.1996.57.619. [DOI] [PubMed] [Google Scholar]
- Krushner MG, Abrams K, Thuras P, Hanson KL, Brekke M, Sletten S. Follow-up study of anxiety disorder and alcohol dependence in comorbid alcoholism treatment patients. Alcohol. Clin. Exp. Res. 2005;29:1432–1443. doi: 10.1097/01.alc.0000175072.17623.f8. [DOI] [PubMed] [Google Scholar]
- Mann JJ, Brent DA, Arango V. The neurobiology and genetics of suicide and attempted suicide: a focus on the serotonergic system. Neuropsychopharmacology. 2001;24:467–77. doi: 10.1016/S0893-133X(00)00228-1. [DOI] [PubMed] [Google Scholar]
- Mann K, Hintz T, Jung M. Does psychiatric comorbidity in alcohol-dependent patients affect treatment outcome? Eur. Arch. Psychiatry Clin. Neurosci. 2004;254:172–181. doi: 10.1007/s00406-004-0465-6. [DOI] [PubMed] [Google Scholar]
- Mann K, Schafer DR, Langle G, Ackermann K, Croissant B. The long-term course of alcoholism, 5, 10 and 16 years after treatment. Addiction. 2005;100:797–805. doi: 10.1111/j.1360-0443.2005.01065.x. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Luborsky L, Woody GE, O'Brien CP, Druley KA. Predicting response to alcohol and drug abuse treatments. Role of psychiatric severity. Arch. Gen. Psychiatry. 1983;40:620–5. doi: 10.1001/archpsyc.1983.04390010030004. [DOI] [PubMed] [Google Scholar]
- Miller L. Predicting relapse and recovery in alcoholism and addiction: Neuropsychology, personality, and cognitive style. J. Subst. Abuse Treat. 1991;8:277–291. doi: 10.1016/0740-5472(91)90051-b. [DOI] [PubMed] [Google Scholar]
- Miller NS, Hoffmann NG, Ninonuevo F, Astrachan BM. Lifetime diagnosis of major depression as a multivariate predictor of treatment outcome for inpatients with substance use disorders from abstinence-based programs. Ann. Clin. Psychiatry. 1997;9:127–137. doi: 10.1023/a:1026269706001. [DOI] [PubMed] [Google Scholar]
- Miller WR, Walters ST, Bennett ME. How effective is alcoholism treatment in the United States? J. Stud. Alcohol. 2001;62:211–220. doi: 10.15288/jsa.2001.62.211. [DOI] [PubMed] [Google Scholar]
- Moos RH, Moos BS. Rates and predictors of relapse after natural and treated remission from alcohol use disorders. Addiction. 2006;101:212–222. doi: 10.1111/j.1360-0443.2006.01310.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patton JH, Stanford MS, Barratt ES. Factor structure of the Barratt impulsiveness scale. J. Clin. Psychol. 1995;51:768–774. doi: 10.1002/1097-4679(199511)51:6<768::aid-jclp2270510607>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- Project MATCH Matching Alcoholism Treatments to Client Heterogeneity: Project MATCH posttreatment drinking outcomes. J. Stud. Alcohol. 1997;58:7–29. [PubMed] [Google Scholar]
- Rounsaville BJ, Dolinsky ZS, Babor TF, Meyer RE. Psychopathology as a predictor of treatment outcome in alcoholics. Arch. Gen. Psychiatry. 1987;44:505–513. doi: 10.1001/archpsyc.1987.01800180015002. [DOI] [PubMed] [Google Scholar]
- Roy A. Distanl risk factors for suicidal behavior in alcoholics: Replications and new findings. J. Affect. Disord. 2003;77:267–271. doi: 10.1016/s0165-0327(02)00173-8. [DOI] [PubMed] [Google Scholar]
- Schuckit MA. Primary men alcoholics with histories of suicide attempts. J. Stud. Alcohol. 1986;47:78–81. doi: 10.15288/jsa.1986.47.78. [DOI] [PubMed] [Google Scholar]
- Sellman JD, Joyce PR. Does depression predict relapse in the 6 months following treatment for men with alcohol dependence? Aust. N. Z. J. Psychiatry. 1996;30:573–578. doi: 10.3109/00048679609062652. [DOI] [PubMed] [Google Scholar]
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Hergueta T, Baker R, Dunbar GC. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J. Clin. Psychiatry. 1998;5920(Suppl):22–33. [PubMed] [Google Scholar]
- Simon OR, Swann AC, Powell KE, Potter LB, Kresnow MJ, O'Carroll PW. Characteristics of impulsive suicide attempts and attempters. Suicide Life Threat. Behav. 2001;32:49–59. doi: 10.1521/suli.32.1.5.49.24212. [DOI] [PubMed] [Google Scholar]
- Smith GE, Ross RL, Rost KM. Psychiatric outcomes module: substance abuse outcomes module (SAOM) In: Sederer LI, Dickey B, editors. Outcome assessment in clinical practice. Williams and Wilkins; Baltimore, MD: 1996. pp. 85–88. [Google Scholar]
- Snow D, Anderson C. Exploring the factors influencing relapse and recovery among drug and alcohol addicted women. J. Psychosoc. Nurs. Ment. Health Serv. 2000;38:8–19. doi: 10.3928/0279-3695-20000701-08. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Maisto SA, Sobell MB, Cooper AM. Reliability of alcohol abusers' self-reports of drinking behavior. Behav. Res. Ther. 1979;17:157–160. doi: 10.1016/0005-7967(79)90025-1. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB, Leo GI, Cancilla A. Reliability of a timeline method: assessing normal drinkers' reports of recent drinking and a comparative evaluation across several populations. Br. J. Addict. 1988;83:393–402. doi: 10.1111/j.1360-0443.1988.tb00485.x. [DOI] [PubMed] [Google Scholar]
- Sobell MB, Sobell LC, Klajner F, Pavan D, Basian E. The reliability of a timeline method for assessing normal drinker college students' recent drinking history: utility for alcohol research. Addict. Behav. 1986;11:149–161. doi: 10.1016/0306-4603(86)90040-7. [DOI] [PubMed] [Google Scholar]
- Strowig AB. Relapse determinants reported by men treated for alcohol addiction: the prominence of depressed mood. J. Subst. Abuse Treat. 2000;19:469–74. doi: 10.1016/s0740-5472(00)00122-7. [DOI] [PubMed] [Google Scholar]
- Swann AC, Dougherty DM, Pazzaglia PJ, Pham M, Steinberg JL, Moeller FG. Increased impulsivity associated with severity of suicide attempt history in patients with bipolar disorder. Am. J. Psychiatry. 2005;162:1680–1687. doi: 10.1176/appi.ajp.162.9.1680. [DOI] [PubMed] [Google Scholar]
- Verheul R, van den Brink W, Hartgers C. Personality disorders predict relapse in alcoholic patients. Addict. Behav. 1998;23:869–82. doi: 10.1016/s0306-4603(98)00065-3. [DOI] [PubMed] [Google Scholar]
- Willinger U, Lenzinger E, Hornik K, Fischer G, Schonbeck G, Aschauer HN, Meszaros K. Anxiety as a predictor of relapse in detoxified alcohol-dependent patients. Alcohol Alcohol. 2002;37:609–12. doi: 10.1093/alcalc/37.6.609. [DOI] [PubMed] [Google Scholar]
- Wines JD, Jr., Saitz R, Horton NJ, Lloyd-Travaglini C, Samet JH. Suicidal behavior, drug use and depressive symptoms after detoxification: a 2-year prospective study. Drug Alcohol Depend. 2004;76(Suppl):S21–29. doi: 10.1016/j.drugalcdep.2004.08.004. [DOI] [PubMed] [Google Scholar]
- Witkiewitz K, Marlatt GA. Relapse prevention for alcohol and drug problems: that was Zen, this is Tao. Am. Psychol. 2004;59:224–235. doi: 10.1037/0003-066X.59.4.224. [DOI] [PubMed] [Google Scholar]