Abstract
BACKGROUND
Heart-type fatty acid binding protein (hFABP) functions as a myocardial fatty acid transporter and is released into the circulation early after myocardial injury. We hypothesized that hFABP is superior to conventional cardiac biomarkers for predicting early perioperative myocardial injury after coronary artery bypass graft (CABG) surgery.
METHODS
A prospective cohort study of 1298 patients undergoing primary CABG with cardiopulmonary bypass (CPB) was performed at 2 institutions. Four plasma myocardial injury biomarkers (hFABP; cardiac troponin I [cTnI]; creatine kinase, MB [CK-MB] fraction; and myoglobin) were measured at 7 perioperative time points. The association among perioperative cardiac biomarkers and ventricular dysfunction, hospital length of stay (HLOS), and up to 5-year postoperative mortality (median 3.3 years) was assessed using Cox proportional hazard models. We defined in-hospital ventricular dysfunction as a new requirement for 2 or more inotropes, or new placement of an intraaortic balloon pump, or ventricular assist device either during the intraoperative period after the patient separated from CPB or postoperatively in the intensive care unit.
RESULTS
The positive and negative predictive values of mortality for hFABP are 13% (95% confidence interval [CI], 9%–19%) and 95% (95% CI, 94%–96%), respectively, which is higher than for cTnI and CK-MB. After adjusting for clinical predictors, both postoperative day (POD) 1 and peak hFABP levels were independent predictors of ventricular dysfunction (P < 0.0001), HLOS (P < 0.05), and 5-year mortality (P < 0.0001) after CABG surgery. Furthermore, POD1 and peak hFABP levels were significantly superior to other evaluated biomarkers for predicting mortality. In a repeated-measures analysis, hFABP outperformed all other models of fit for HLOS. Patients with POD2 hFABP levels higher than post-CPB hFABP levels had an increased mortality compared with those patients whose POD2 hFABP levels decreased from their post-CPB level (hazard ratio, 10.9; 95% CI, 5.0–23.7; P = 7.2 × 10−10). Mortality in the 120 patients (10%) with a later hFABP peak was 18.3%, compared with 4.7% in those who did not peak later. Alternatively, for cTnI or CK-MB, no difference in mortality was detected.
CONCLUSION
Compared with traditional markers of myocardial injury after CABG surgery, hFABP peaks earlier and is a superior independent predictor of postoperative mortality and ventricular dysfunction.
Perioperative myocardial infarction (MI) occurs in 7% to 15% of cardiac surgical patients and is associated with an increased hospital length of stay (HLOS) and hospital cost and reduced short- and long-term survival.1,2 However, the diagnosis of perioperative myocardial injury can be challenging because cardiac-specific biomarkers can increase even after uncomplicated cardiac surgery to levels considered diagnostic of MI in ambulatory populations.3
Heart-type fatty acid binding protein (hFABP) is a small, 14.5-kDa cytosolic protein present in the myocardium and is a key cytosolic transporter of fatty acids.4 hFABP is comparable in size to myoglobin (18 kDa) but smaller than cardiac troponin I (cTnI) (25 kDa) and creatine kinase, MB (CK-MB) (87 kDa). Its release from injured myocardium was first described in 1998.5 Primarily, hFABP isoforms are found not only in the heart but also in much smaller concentrations in skeletal muscle, brain, and kidney.6–8 Despite similar sizes and release patterns, hFABP is more specific than myoglobin as a biomarker of myocardial injury because of its relatively higher concentration in the heart. Consequently, as a result of its relatively small size and its primary location in cytosol rather than myofibrils, hFABP is released earlier and in larger amounts into the circulation when membrane integrity is compromised because of myocardial injury.9 hFABP is released during myocardial ischemia even in the absence of irreversible myocardial necrosis, and is a sensitive marker of MI in the ambulatory setting.10,11
Previous studies in nonsurgical patients have associated increased hFABP with an increased risk of subsequent death and major cardiac events.12–14 However, its prognostic utility in the cardiac surgical population has not been established. We hypothesized that hFABP is an earlier marker of perioperative myocardial injury than cTnI, CK-MB fraction, and myoglobin and is an independent predictor of in-hospital ventricular dysfunction, extended HLOS, and all-cause mortality after isolated first-time coronary artery bypass graft (CABG) surgery with cardiopulmonary bypass (CPB). Furthermore, because hFABP is rapidly cleared from plasma, we sought to examine the predictive value of the time course of cardiac biomarker release on mortality and HLOS.
METHODS
Study Design
A prospective, longitudinal study of 1441 nonconsecutive patients undergoing primary CABG surgery with CPB between August 2001 and May 2006 at Brigham and Women’s Hospital, Boston, MA, and Texas Heart Institute, Houston, TX, was conducted (CABG Genomics Program; http://clinicaltrials.gov/show/NCT00281164). Our study complies with the Declaration of Helsinki, and after IRB approval, written informed consent was obtained from each patient. No funding agency had any input on study design, analysis, or data interpretation.
Exclusions
Patients were excluded from enrollment based on prospective criteria in the CABG Genomics Program including age <20 years, a preoperative hematocrit <25%, or if they had received leukocyte-rich blood products within 30 days before surgery. Patients were also excluded from subsequent analysis if they had prior heart surgery (n = 9), concurrent valve surgery (n = 57), off-pump surgery (n = 33), emergent surgery (n = 4), died in the operating room (n = 2), or had missing biomarker data (n = 43). A total of 1298 patients met eligibility criteria and were included in the analysis (Table 1). Seventy-four percent of patients were enrolled at institution 1.
Table 1.
Demographic and Operative Characteristics of Enrolled Patients
| Characteristics | Total cohort | hFABP POD 2 < post-CPB | hFABP POD 2 > post-CPB |
|---|---|---|---|
| Number of subjects (%) | 1298 | 1090 (90) | 120 (10) |
| Gender (% male) | 82 | 83 | 73* |
| Age (y) | 63 (57–72) | 63 (57–71) | 68 (60–76)† |
| Caucasian race (%) | 84 | 84 | 86 |
| Institution 1 (%) | 74 | 74 | 79 |
| Medical history | |||
| Preoperative LVEF (%) | 55 (45–60) | 55 (45–60) | 55 (45–60) |
| Insulin or noninsulin dependent diabetes (%) | 29 | 29 | 35 |
| Past or present smoker (%) | 70 | 70 | 64 |
| Pulmonary disease (%) | 4.6 | 4.5 | 4.2 |
| Preoperative creatinine (mg/dL) | 1 (0.9–1.2) | 1 (0.9–1.2) | 1.2 (1.0–1.4)† |
| Preoperative hematocrit (%) | 40.4 (37.2–43.6) | 40.5 (37.4–43.7) | 39.4 (36.1–43.1)* |
| Hypertension (%) | 75 | 74 | 83* |
| Hypercholesterolemia (%) | 74 | 75 | 72 |
| Previous myocardial infarction (%) | 44 | 43 | 52 |
| Preoperative medications | |||
| ACE inhibitor (%) | 46 | 46 | 45 |
| β-Blocker (%) | 77 | 78 | 71 |
| Ca++ antagonist (%) | 14 | 13 | 18 |
| Aspirin (%) | 76 | 78 | 66* |
| HMG-CoA reductase inhibitor (%) | 77 | 77 | 74 |
| Surgery | |||
| No. of CABG (%) | |||
| 1 | 2 | 2 | 3 |
| 2 | 13 | 13 | 16 |
| 3 | 45 | 45 | 43 |
| ≥4 | 40 | 40 | 38 |
| CPB duration (min) | 94 (66–118) | 93 (66–117) | 100 (68–125) |
| Aortic cross-clamp duration (min) | 70 (46–90) | 69 (46–89) | 72 (49–95) |
| Biomarkers—preoperative | |||
| CKMB, μg/L (median; IQR) | 0.6 (0.2–1.3) | 0.6 (0.2–1.3) | 0.7 (0.3–1.7)* |
| hFABP, μg/L (median; IQR) | 4.9 (3.5–7.2) | 4.7 (3.5–6.8) | 7.1 (5.2–10.0)† |
| Myoglobin, μg/L (median; IQR) | 61 (46–85) | 59 (45–83) | 79 (61–108)† |
| cTnI, μg/L (median; IQR) | 0 (0–0.04) | 0 (0–0.04) | 0 (0–0.05) |
| Postoperative data | |||
| HLOS (d) | 7 (6–9) | 7 (6–9) | 9 (7–13)† |
| Mortality N (%) up to 5 y | 79 (6) | 51 (4.7) | 22 (18.3)† |
| Ventricular dysfunction (%) | 12 | 11 | 20* |
Each variable is also listed for those patients whose hFABP level peaked at the post-cardiopulmonary bypass (CPB) time point or on postoperative day (POD) 2. Data are shown as percentage for dichotomous variables and median (25th, 75th percentiles for interquartile range [IQR]) for continuous variables. Columns 2 and 3 designate patients who have a decrease in hFABP level between POD2 and immediately post-CPB and those with an elevated hFABP on POD2 compared with immediately after CPB. Biomarker data on 88 additional patients was missing between POD 2 and post CPB.
P values are Kruskal-Wallis 1-way analysis of variance by ranks for continuous data and χ2 distribution or Fisher exact for nominal and ordinal data.
LVEF = left ventricular ejection fraction; ACE = angiotensin converting enzyme; HMG = 3-hydroxy-3-methyl-glutaryl-CoA reductase; CABG = coronary artery bypass graft; CKMB = creatinine kinase MB fraction; hFABP = heart-type fatty acid binding protein; cTnI = cardiac troponin I; CPB = cardiopulmonary bypass; HLOS = hospital length of stay.
P < 0.05,
P < 0.0001 (for hFABP POD 2 > versus < post-CPB).
Operative Techniques
No specific attempts were made to standardize the anesthetic and surgical management. Extracorporeal circulation was performed with normothermic, nonpulsatile flow and a membrane oxygenator. Cold crystalloid cardioplegia (St. Thomas’ Hospital solution) or cold blood cardioplegia was used to induce and maintain cardioplegic arrest according to the surgeon’s preference. Inotropic support was initiated at the discretion of the surgeon and anesthesiologist, and routine or prophylactic inotropes were not initiated.
Demographics
The medical records of consenting patients undergoing isolated, primary CABG surgery were reviewed by dedicated trained research staff. Demographics, medical and surgical history, medications, results of preoperative coronary angiography, and other predictors of adverse outcomes were recorded using a defined protocol in a purpose-built case report form. Mortality was followed up through queries of the Social Security Death Index for up to 5 years after surgery (mean follow-up, 3.3 ± 1.4 years; median, 3.3 years).
Blood Samples
Blood samples were obtained from all patients at 7 perioperative time points: before induction of general anesthesia, after weaning from CPB, and on the mornings of postoperative days (PODs) 1 to 5. Citrated plasma was stored in vapor-phase liquid nitrogen at −130°C until analysis. cTnI, CK-MB, and myoglobin were analyzed with a sandwich immunoassay on a Triage® platform using monoclonal and polyclonal antibodies (Biosite, San Diego, CA). hFABP was analyzed with a 2-step direct sandwich enzyme-linked immunosorbent assay using 2 distinct mouse antihuman hFABP monoclonal antibodies (Biosite). The percentages of the root mean square coefficient of variation, which represents normalized measure of dispersion of a probability distribution, were 14%, 9%, 13%, and 13% over the reportable range for CK-MB, hFABP, myoglobin, and hFABP assays, respectively.
Clinical practitioners caring for the patients were blinded to these results. Thus, patient care and treatment for myocardial injury or MI were not proscribed by this study.
Clinical End Points
The primary clinical end point for this analysis was all-cause mortality up to 5 years after surgery. Secondary end points included extended HLOS and ventricular dysfunction. HLOS was measured in days, which included the date of surgery and date of discharge. Extended HLOS was defined as >12 PODs (90th percentile). Patients who died before discharge or within 30 days of surgery were censored; those who stayed >30 days were counted as having a truncated HLOS of 30 days. In-hospital ventricular dysfunction was defined as a new requirement for 2 or more inotropes, new placement of an intraaortic balloon pump, or ventricular assist device either during the intraoperative period after the patient separated from CPB or postoperatively in the intensive care unit. Inotrope support was defined as continuous infusion of amrinone, milrinone, dobutamine, dopamine (>5 μg · kg−1 · min−1), epinephrine, isoproterenol, norepinephrine, or vasopressin.
Statistical Methods
Statistical analyses were performed using SAS version 9.1.3 and JMP 8.0 (SAS Institute, Cary, NC). Data are presented as median with interquartile range (IQR: 25%–75%) unless otherwise stated. Continuous variables were compared using analysis of variance and the Wilcoxon-Mann-Whitney rank sum test. Categorical variables were compared with the Fisher exact test. Cumulative survival and HLOS was estimated by Kaplan-Meier analysis; the comparison of survival curves was performed with the non-parametric log-rank test. A P value <0.05 was considered significant.
To compare the clinical value of each biomarker and to establish a time point with the highest predictive value, we used 3 methods to examine the relationship between cardiac biomarkers and clinical outcomes.
Peak measurement of each biomarker, defined as the highest level observed between the post-CPB to POD 5 measurements.
POD 1 time point of each biomarker.
Later versus earlier peak of each biomarker. We examined patients whose peak biomarker level occurred after the usual peak at the post-CPB (hFABP) or POD 1 (CK-MB, myoglobin, and cTnI) time points, respectively. Specifically, for hFABP, an increase from the post-CPB time point to POD 2 was examined, whereas for CK-MB, myoglobin, and cTnI, an increase from POD 1 to POD 3 was examined.
Covariates with a 2-tailed nominal P < 0.15 in univariate analyses and clinically relevant covariates were entered into stepwise multivariable logistic regression models for each outcome. Age, gender, race, and institution were forced into the model. To estimate the independent prognostic utility of hFABP on 5-year all-cause mortality and extended HLOS, a Cox proportional hazard model with time-dependent repeated measurements was constructed to estimate the hazard ratios (HRs) and 95% confidence intervals (CIs) associated with elevated levels of the 4 biomarkers, while adjusting for demographics and clinical covariates (Table 2). A logistic regression model was constructed in similar fashion for postoperative ventricular dysfunction (Table 2). To account for differences in confounding related to the outcome, separate models for the 3 outcomes of mortality, ventricular dysfunction, and HLOS were created; mortality and HLOS were analyzed with a Cox proportional hazard model, whereas ventricular dysfunction was analyzed with a logistic regression model. All POD 1 and peak biomarker values were adjusted for their respective preoperative values. We added a continuous variable to account for the time of day surgery began.
Table 2.
Multivariable Models of 5-y Mortality, Hospital Length of Stay (HLOS), and Ventricular Dysfunction
| Model variables | Mortality |
Hospital length of stay |
Ventricular dysfunction |
|||
|---|---|---|---|---|---|---|
| HR (95% CI) | P | HR (95% CI) | P | OR (95% CI) | P | |
| Age (years in deciles) | 1.62 (1.25–2.09) | 0.0002 | 1.12 (1.06–1.19) | <0.0001 | 1.13 (0.93–1.38) | 0.189 |
| Gender (female) | 0.48 (0.24–0.96) | 0.0376 | 1.29 (1.09–1.51) | 0.0023 | 0.60 (0.33–1.03) | 0.0747 |
| Institution 1 | 0.77 (0.39–1.49) | 0.4475 | 0.62 (0.53–0.72) | <0.0001 | 0.53 (0.32–0.90) | 0.0189 |
| Caucasian race | 1.62 (0.68–3.83) | 0.2695 | 1.21 (1.02–1.43) | 0.0225 | 1.49 (0.84–2.73) | 0.1802 |
| Preoperative LVEF (%) | 0.97 (0.95–0.99) | 0.0014 | 0.99 (0.99–1) | 0.0716 | 0.94 (0.92–0.95) | <0.0001 |
| Hematocrit | 0.92 (0.88–0.97) | 0.0053 | 0.99 (0.97–1.00) | 0.2363 | 0.94 (0.90–0.98) | 0.0085 |
| CPB duration | 0.99 (0.98–1) | 0.0601 | 1.00 (1.00–1.00) | 0.0065 | 1.00 (1.00–1.01) | 0.0003 |
| Time of day surgery began | 1.02 (0.94–1.10) | 0.636 | 0.98 (0.96–1.00) | 0.0622 | 0.94 (0.79–1.02) | 0.1094 |
| Highest postoperative creatinine | 5.20 (3.22–8.40) | <0.0001 | 1.38 (1.14–1.73) | 0.0017 | ||
| Preoperative digoxin | 2.37 (1.07–5.26) | 0.0331 | ||||
| Hypertension | 0.63 (0.39–1.04) | 0.0746 | ||||
| HMG-CoA reductase inhibitor | 0.58 (0.36–0.94) | 0.0271 | ||||
| BMI | 1.00 (0.99–1.01) | 0.1056 | ||||
| Postoperative new AF | 1.83 (1.60–2.09) | <0.0001 | ||||
| Postoperative inotrope | 1.46 (1.33–1.59) | <0.0001 | ||||
| Preoperative ACEI | 1.67 (1.13–2.49) | 0.0101 | ||||
| MI within 2 wk | 1.82 (1.18–2.77) | 0.0057 | ||||
| Preoperative diuretic | 1.45 (0.94–2.21) | 0.0835 | ||||
| Biomarkers added individually to above clinical models | ||||||
| hFABP | ||||||
| Post CPB | 1.00 (0.99–1.01) | 0.5244 | 1.00 (1.00–1.00) | 0.4083 | 1.00 (1.00–1.01) | 0.2298 |
| POD1 | 1.01 (1.01–1.02) | <0.0001 | 1.00 (1.00–1.00) | 0.0004 | 1.01 (1.01–1.01) | <0.0001 |
| Peak | 1.01 (1.01–1.01) | <0.0001 | 1.00 (1.00–1.00) | 0.0309 | 1.01 (1.01–1.01) | <0.0001 |
| cTnI | ||||||
| POD1 | 1.03 (1.01–1.04) | 0.0077 | 0.99 (0.98–1.00) | 0.0039 | 1.03 (1.01–1.05) | 0.0072 |
| Peak | 1.03 (1.01–1.05) | 0.0062 | 0.99 (0.98–1.00) | 0.0047 | 1.03 (1.01–1.05) | 0.0024 |
| Myoglobin | ||||||
| POD1 | 1.00 (1.00–1.00) | 0.0544 | 1.00 (1.00–1.00) | 0.0002 | 1.00 (1.00–1.00) | 0.2133 |
| Peak | 1.00 (1.00–1.00) | 0.019 | 1.00 (1.00–1.00) | <0.0001 | 1.00 (1.00–1.00) | 0.0341 |
| CKMB | ||||||
| POD1 | 1.01 (1.00–1.01) | 0.06 | 1.00 (1.00–1.00) | 0.0044 | 1.00 (1.00–1.01) | 0.2179 |
| Peak | 1.01 (1.00–1.01) | 0.0614 | 1.00 (1.00–1.00) | 0.0008 | 1.00 (1.00–1.01) | 0.3627 |
All demographic and clinical variables (excluding biomarkers) shown in model columns are included in the analyses. Mortality and HLOS were modeled as Cox proportional hazard models, ventricular dysfunction as a nominal logistic regression model. Biomarkers were added individually and independently and adjusted for their respective preoperative values. Hospital length of stay is a continuous outcome measured in days.
P values are expressed using Wald test.
HR = hazard ratio; OR = odds ratio; CI = confidence interval; MI = myocardial infarction; BMI = body mass index; LVEF = left ventricular ejection fraction; AF = atrial fibrillation; HMG = 3-hydroxy-3-methyl-glutaryl-CoA reductase; ACE = angiotensin converting enzyme; CPB = cardiopulmonary bypass; Post = post-CPB; POD = postoperative day; hFABP = heart-type fatty acid binding protein; cTnI = cardiac troponin I; CKMB = creatinine kinase MB fraction.
To assess the predictive value of adding each biomarker individually to the clinical model of all-cause mortality and HLOS, we computed the c-index for the censored data. The c-index is a generalization of the area under the receiver operating characteristic curve that represents the probability of concordance between predicted and observed survival, with c = 0.5 for random prediction and c = 1.0 for a perfectly discriminating model. We then computed the U statistic to test whether the model with the addition of the biomarker was more concordant than the model without the biomarker. In addition, we used 3 global measures of model fit (the likelihood ratio test [−2LL], Akaike information criterion [AIC],16 and Bayesian information criterion [BIC]).17 F tests were used to compare generalized r2.
RESULTS
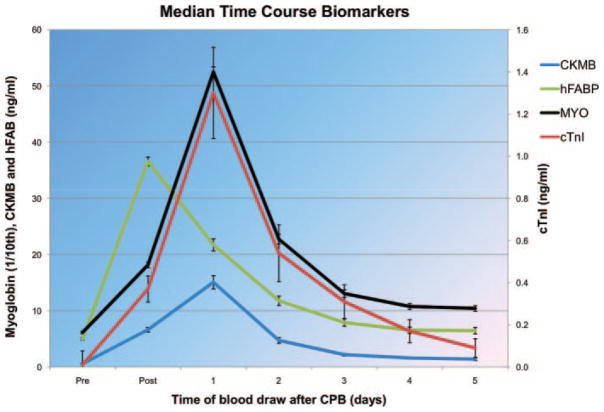
Baseline characteristics of the study population are shown in Table 1, and the time course of median biomarker levels are shown in Figure 1. Serum hFABP levels were higher after CABG, with 74% of patients peaking at the post-CPB time point (median [interquartile range], 36.3 ng/mL [26.2–49.7 ng/mL]). In contrast, cTnI, myoglobin, and CK-MB levels peaked on POD 1 in 89%, 84%, and 91% of patients, respectively. On POD 1, hFABP levels were correlated with CK-MB (r = 0.36, P < 0.001), myoglobin (r = 0.39, P < 0.001), and cTnI (r = 0.44, P < 0.001).
Figure 1.
Time course of median biomarker levels (±SE). Myoglobin levels shown as one-tenth of actual value. Pre = preoperatively; post = postprotamine dose; CK-MB = creatinine kinase, MB fraction; cTnI = cardiac troponin I; hFABP = heart-type fatty acid binding protein; MYO = myoglobin; CPB = cardiopulmonary bypass.
Mortality
Median duration of follow-up was 3.3 years (2.1–4.6 years). All-cause mortality up to 5 years of follow-up was 6% (n = 79) with a 30-day operative mortality of 0.6% (n = 8). POD 1 hFABP concentrations were 21.0 ng/mL (12.8–36.4 ng/mL) for survivors and 26.3 ng/mL (18.2–51.5 ng/mL) for patients who died within 5 years of surgery (P < 0.001). The positive and negative predictive values for mortality of hFABP are 13% (95% CI, 9%–19%) and 95% (95% CI, 94%–96%), respectively. After adjusting for clinical predictors of mortality, POD 1 and peak postoperative hFABP levels were independent predictors of nonsurvival after CABG surgery among the 4 evaluated cardiac biomarkers (Table 2). Addition of POD 1 hFABP and cTnI level to the Cox proportional hazards model was significantly associated with mortality, whereas the addition of myoglobin or CK-MB was not. The area under the curve for the censored Cox proportional hazard model for mortality was 0.730, 0.745, and 0.773 for the baseline model and for the models with the addition of cTnI and hFABP, respectively. In addition, POD 1 and peak hFABP levels had the best predictive values when assessed with 3 global measures of model fit (Table 3). By contrast, the post-CPB hFABP measurement had no predictive value (Table 3).
Table 3.
Global Measures of Model Fit for All-Cause Mortality and Hospital Length of Stay (HLOS)
| Postoperative Day 1 biomarker |
Peak biomarker |
Repeated measures |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Δ −2LL | Δ AIC | Δ BIC | Δ −2LL | Δ AIC | Δ BIC | Δ −2LL | Δ AIC | Δ BIC | |
| Mortality | |||||||||
| w/o biomarkers | 56.5 | 36.5 | 13.3 | 56.5 | 36.5 | 13.3 | 43.3 | 23.3 | 3.6 |
| hFABP | 72.3* | 50.3 | 24.8 | 70.0* | 48.0 | 22.5 | 68.1* | 46.1 | 24.4 |
| Myoglobin | 58.5 | 36.5 | 11.0 | 59.2 | 37.2 | 11.7 | 66.2* | 44.2 | 22.5 |
| CKMB | 57.9 | 35.9 | 10.4 | 57.5 | 35.5 | 10.0 | 45.5 | 23.5 | 1.8 |
| cTnI | 56.9 | 34.9 | 9.4 | 56.7 | 34.7 | 9.2 | 43.7 | 21.7 | 0.0 |
| Hospital length of stay | |||||||||
| w/o biomarkers | 384.1 | 362.1 | 306.0 | 384.1 | 362.1 | 306.0 | 295.0 | 273.0 | 219.8 |
| hFABP | 393.4* | 369.4 | 308.2 | 388.6* | 364.6 | 303.4 | 314.9* | 290.9 | 232.9 |
| Myoglobin | 394.1* | 370.1 | 308.9 | 396.8* | 372.8 | 311.5 | 312.5* | 288.5 | 230.5 |
| CKMB | 393.9* | 369.9 | 308.6 | 402.1* | 378.1 | 316.9 | 300.0* | 276.0 | 218.0 |
| cTnI | 389.5* | 365.5 | 304.3 | 390.4 | 366.4 | 305.1 | 295.9 | 271.9 | 213.9 |
The predictive value of adding each biomarker individually to the baseline clinical model of all-cause mortality and HLOS is shown. Higher values indicate better fit. AIC and BIC reward the model for covariates that contribute significantly and penalizes for each additional variable (larger numbers = better model fit).
−2LL = negative two log likelihood ratio; AIC = Akaike information criterion; BIC = Bayesian information criterion; hFABP = heart-type fatty acid binding protein; cTnI = cardiac troponin I; CKMB = creatinine kinase MB fraction.
P < 0.05 is significance of biomarkers compared with baseline clinical model for the negative two log likelihood ratio in a χ2 distribution with 1 degree of freedom.
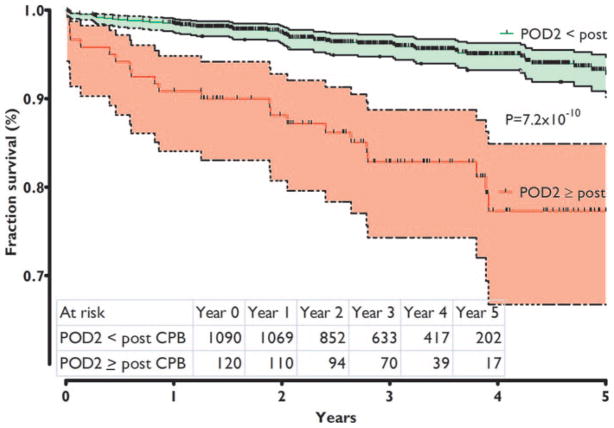
We examined patients whose biomarker levels peaked later than the post-CPB level for hFABP and later than POD 1 for cTnI, myoglobin, or CK-MB (Table 1). An hFABP level higher than the post-CPB level on any day was independently associated with increased mortality (P = 0.001) after adjusting for demographic and clinical covariates in a Cox proportional hazards model. Patients with POD 2 hFABP levels higher than post-CPB hFABP levels had an increased mortality compared with those patients whose POD 2 hFABP level decreased from their post-CPB level (HR, 10.9; 95% CI, 5.0–23.7; P < 0.0001; Fig. 2). Mortality in the 120 patients (10%) with a later hFABP peak was 18.3%, compared with 4.7% in those who did not. Alternatively, for cTnI or CK-MB, no elevation above the cohort-observed peak on POD 1 was significantly associated with mortality.
Figure 2.
Kaplan-Meier survival curve for time of peak heart-type fatty acid binding protein (hFABP) level. Difference in survival for patients with a decrease in hFABP level between POD2 and immediately after cardiopulmonary bypass (CPB) and those with an increased hFABP on POD2 compared with immediately after CPB (shaded area = 95% confidence interval). P value refers to the level of difference between curves. POD = postoperative day.
Hospital Length of Stay
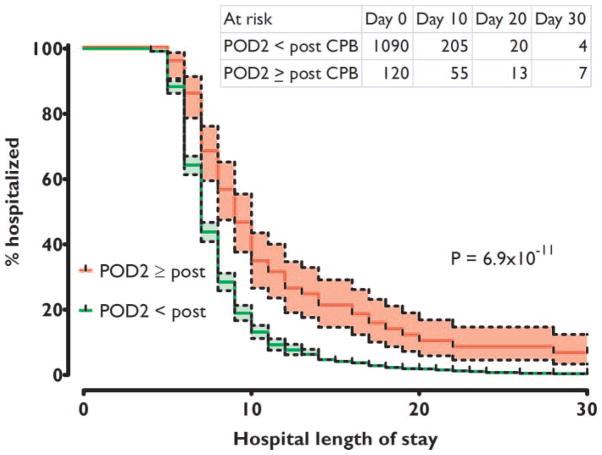
Median HLOS was 7 days (IQR, 6–9 days). POD 1 and peak levels of all 4 biomarkers were independent predictors of HLOS when added individually to the multivariate model (Table 2). hFABP outperformed the other biomarkers for model fit on POD 1 and in a repeated-measures analysis (Table 3). However, no significant difference between biomarkers for the peak level was found.
An hFABP level higher than the post-CPB level on any postoperative day was independently associated with increased HLOS (P = 0.0001) after adjusting for demographic and clinical covariates in a Cox proportional hazards model. Likewise, the median HLOS increased by 2 days, and the unadjusted risk of prolonged HLOS was twice as high for patients with a higher hFABP on POD 2 compared with the post-CPB level (HR, 1.98; 1.64–2.38; P = 6.9 × 10−11; Fig. 3). For cTnI or CK-MB, no increase above the cohort-observed peak on POD 1 was significant or improved model prediction for HLOS.
Figure 3.
Hospital length of stay discharge curve for time of peak heart-type fatty acid binding protein (hFABP) level. Difference in discharge from hospital for patients with a decrease in hFABP level between POD2 and immediately after cardiopulmonary bypass (CPB) and those with an increased hFABP on POD2 compared with immediately after CPB (shaded area = 95% confidence interval). P value refers to the level of difference between curves. For example, at a hospital length of stay of 10 days, 40% of patients with a high hFABP level on postoperative day (POD) 2 are still hospitalized versus 20% with a low hFABP level.
Ventricular Dysfunction
To further establish that association of hFABP with mortality and HLOS is likely related to clinically relevant myocardial injury, we assessed the association between POD 1 and peak postoperative hFABP and the development of in-hospital postoperative ventricular dysfunction (12% incidence). After adjusting for clinical predictors of ventricular dysfunction, peak postoperative hFABP and cTnI levels were independent predictors of postoperative ventricular dysfunction (Table 2). Both POD 1 hFABP and cTnI levels were independent predictors of ventricular dysfunction, whereas neither myoglobin nor CK-MB was an independent predictor. POD 1 hFABP was a significantly better predictor of ventricular dysfunction than cTnI.
Multimarker Models
The predictive value of the baseline multivariate clinical model of ventricular dysfunction, HLOS, or mortality was not significantly improved by concomitantly adding POD 1 or peak CK-MB, myoglobin, or cTnI to POD 1 and peak hFABP at their respective time points using AIC, BIC, and −2LL.
DISCUSSION
This study demonstrates that hFABP is superior to cTnI, CK-MB, and myoglobin for predicting all-cause mortality up to 5 years after CABG surgery. We further found that hFABP levels after CPB were independently associated with ventricular dysfunction and were comparable with cTnI, CK-MB, and myoglobin for predicting HLOS after CABG surgery with CPB. This novel observation in the cardiac surgical population confirms similar findings in the nonsurgical population.12,13 Furthermore, we now describe a unique increase in hFABP level after the usual peak that identifies patients at exceptionally increased risk for mortality and extended HLOS. This finding is not observed with conventional biomarkers of myocardial injury, perhaps because of their longer plasma half-life times.
In the nonsurgical setting, hFABP is highly sensitive and specific for predicting the outcomes of acute MI and coronary syndromes, often exceeding the current clinical “gold standard” of diagnosis, cTnI.18 Furthermore, hFABP is not only useful as a marker of MI in conjunction with cTnI12 but also offers independent prognostic information in identifying patients at high risk of death and major cardiac events despite a normal cTnI level.13
In contrast to extensive evaluation in nonsurgical patients, only a few small studies involving cardiac surgical populations have examined the utility of hFABP in determining the extent of myocardial injury, and none have examined its association with long-term outcomes.19–21 Hasegawa et al.19 measured serial hFABP levels at 0, 1, 2, 3, and 6 hours after aortic unclamping in pediatric cardiac surgery. They and others demonstrated that the initial rapid increase and peak of hFABP approximately 1 hour after aortic unclamping was followed by a fast decrease to within 10% of baseline by 24 hours.19,20,22,23 This characteristic pattern in cardiac surgical patients develops earlier than in the nonsurgical population in whom detection is possible as early as 20 minutes after a myocardial ischemic event, but peak levels do not occur until 6 to 8 hours after myocardial injury.15 The possible mechanism of this early release in cardiac surgery patients includes sustained ischemic injury during CPB while the aorta is cross-clamped, followed by subsequent reperfusion injury leading to substantial release of hFABP after the aortic unclamping.
We found that the absolute value of hFABP is not only an independent predictor of myocardial injury severity defined as ventricular dysfunction, extended HLOS, and mortality, but that an increase of hFABP after the primary post-CPB peak is an even more important indicator of sustained or recurring myocardial injury associated with higher mortality rates and a propensity for extended HLOS. This unique delayed release pattern was not seen with the other examined biomarkers.
Why Do We Need Another Myocardial Injury Biomarker?
The importance of finding a biomarker with high specificity and sensitivity for myocardial injury after cardiac surgery is highlighted by the observation that even after uncomplicated cardiac surgery, there is a high frequency of indeterminate diagnostic electrocardiogram criteria24 and routine elevation of cardiac-specific biomarkers to levels considered diagnostic of MI in ambulatory populations.3 Consequently, the diagnosis of perioperative myocardial injury can be particularly challenging. Perioperative elevation of cardiac-specific biomarkers may not only be due to coronary artery disease–related myocardial injury but also associated with insults occurring during routine cardiac surgery including transient myocardial ischemia due to aortic cross-clamping or cardiotomy required for valve surgery.
The faster increase and more rapid clearance of hFABP, compared with traditional biomarkers of myocardial injury, make it a more sensitive marker for sustained or recurring myocardial injury. The slower release of CK-MB and cTnI generates an inability to discriminate between graft failure with massive tissue necrosis and ischemia reperfusion injury within 24 hours after CABG surgery.25 This suggests that the more rapid peak of hFABP may enable earlier reintervention to restore myocardial perfusion in those with ischemia or infarction. The faster increase and more rapid clearance of hFABP was first reported in a patient with recurrent MI10 and later confirmed in patients stratified by MI diagnosed by electrocardiogram criteria.26 hFABP is also reported to be more sensitive than cTnI in detecting continuing myocardial damage in chronic heart failure.27
A point-of-care test that uses hFABP has been developed for the diagnosis of MI in nonsurgical patients with purportedly superior sensitivity and specificity than cTnI.28–30 A point-of-care test for the perioperative setting has the potential to have an effect on time-efficient risk stratification and management after cardiac surgery. Earliest identification of patients with clinically relevant myocardial injury could enable clinicians to identify patients in need of further diagnostic or therapeutic procedures to reduce loss of myocardial mass or performance.
Study Limitations
The timing of perioperative blood sampling in this study was designed for examining genetic markers of adverse outcomes after CABG surgery and not specifically to evaluate the release kinetics of hFABP. In more recent studies of patients undergoing cardiac surgery, investigators have observed peak hFABP level approximately 1 to 2 hours after removal of the aortic cross-clamp.19,20 Therefore, post-CPB level of our study was likely measured before and underestimated the actual hFABP peak, thereby limiting its value for differentiating patients with varying adverse outcomes. For the majority of patients, the POD 1 hFABP level was much lower than the post-CPB measurement. Therefore, the highly predictive value of POD 1 is likely related to those patients who do not peak immediately in the first hours after CPB.
The diagnosis of perioperative ventricular dysfunction is hindered by the absence of a standardized definition in the cardiac surgical literature. It is not standard practice at either institution to use prophylactic inotropes to facilitate separation from CPB. Therefore, we elected to define ventricular dysfunction after CABG surgery as the need for 2 or more inotropes, new intraaortic balloon pump, or new ventricular assist device support. A definition based on practitioners’ therapies introduces potential bias associated with practitioner behaviors. Nevertheless, we have previously used this definition to show the association between ventricular dysfunction and increased morbidity and mortality after CABG surgery.31,32
Although this study used a large cohort of patients from 2 institutions, the role of assessing myocardial ischemia by measuring hFABP, and prospectively using measured levels for therapeutic intervention that may alter outcomes such as mortality and HLOS, has not been evaluated. Such prospective trials seem warranted by our observations of early diagnosis of myocardial injury by hFABP, when myocardial recovery may be optimized by early intervention.
Finally, our primary end point of all-cause mortality may not necessarily differentiate between cardiac-specific and non-cardiac causes of death. Nevertheless, prior studies have demonstrated that all-cause and cardiac mortality are equally robust, most likely because of the strong association between these two outcomes in cardiac surgical populations.33,34
CONCLUSION
hFABP is superior to cTnI, CK-MB, and myoglobin for predicting up to 5-year all-cause mortality and ventricular dysfunction and is comparable with these biomarkers of myocardial injury for predicting HLOS after CABG surgery with CPB, even after adjusting for relevant demographic and clinical predictors. In addition, with its rapid increase and decrease, hFABP may allow diagnosis of continuing or recurring myocardial injury after cardiac surgery and therefore may permit more timely initiation of specific treatment strategies.
Acknowledgments
Supported by a Bayer® Fellowship in Blood Conservation grant, Wyckoff, NJ (to JDM); Biosite Inc., San Diego, CA; a Society of Cardiovascular Anesthesiologists Research Starter grant, Richmond, VA (to JDM); a grant from National Institutes of Health, NHLBI HL-068774, Bethesda, MD (to SCB); a a Mercedes Concepcion Faculty Development Fellowship (JDM) and Scholar in Translational Anaesthesia Research grant (TEP) from the Department of Anesthesiology, Perioperative and Pain Medicine, Brigham and Women’s Hospital, Harvard Medical School, Boston, MA.
The authors acknowledge the outstanding contributory efforts of the CABG Genomics research staff: James Gosnell, RN; Kujtim Bodinaku, MD; Jai Madan, MD, MPH; Svetlana Gorbatov, MPH; James Chen, RN; and Isabella Candelaria. The authors also thank all study participants in the CABG.
Footnotes
AUTHOR CONTRIBUTIONS
JDM, TEP, and AAF helped design the study, conduct the study, analyze the data, and write the manuscript. K-YL helped design the study and analyze the data. CDC helped design the study and write the manuscript. SKS and SCB helped design the study, conduct the study, and analyze the data.
References
- 1.Croal BL, Hillis GS, Gibson PH, Fazal MT, El-Shafei H, Gibson G, Jeffrey RR, Buchan KG, West D, Cuthbertson BH. Relationship between postoperative cardiac troponin I levels and outcome of cardiac surgery. Circulation. 2006;114:1468–75. doi: 10.1161/CIRCULATIONAHA.105.602370. [DOI] [PubMed] [Google Scholar]
- 2.Chen JC, Kaul P, Levy JH, Haverich A, Menasche P, Smith PK, Carrier M, Verrier ED, Van de Werf F, Burge R, Finnegan P, Mark DB, Shernan SK. Myocardial infarction following coronary artery bypass graft surgery increases healthcare resource utilization. Crit Care Med. 2007;35:1296–301. doi: 10.1097/01.CCM.0000262403.08546.A2. [DOI] [PubMed] [Google Scholar]
- 3.Ramsay J, Shernan S, Fitch J, Finnegan P, Todaro T, Filloon T, Nussmeier NA. Increased creatine kinase MB level predicts postoperative mortality after cardiac surgery independent of new Q waves. J Thorac Cardiovasc Surg. 2005;129:300–6. doi: 10.1016/j.jtcvs.2004.06.005. [DOI] [PubMed] [Google Scholar]
- 4.Azzazy HM, Pelsers MM, Christenson RH. Unbound free fatty acids and heart-type fatty acid-binding protein: diagnostic assays and clinical applications. Clin Chem. 2006;52:19–29. doi: 10.1373/clinchem.2005.056143. [DOI] [PubMed] [Google Scholar]
- 5.Glatz JF, van der Vusse GJ, Simoons ML, Kragten JA, van Dieijen-Visser MP, Hermens WT. Fatty acid-binding protein and the early detection of acute myocardial infarction. Clin Chim Acta. 1998;272:87–92. doi: 10.1016/s0009-8981(97)00255-6. [DOI] [PubMed] [Google Scholar]
- 6.Kleine AH, Glatz JF, Van Nieuwenhoven FA, Van der Vusse GJ. Release of heart fatty acid-binding protein into plasma after acute myocardial infarction in man. Mol Cell Biochem. 1992;116:155–62. doi: 10.1007/BF01270583. [DOI] [PubMed] [Google Scholar]
- 7.Veerkamp JH, Peeters RA, Maatman RG. Structural and functional features of different types of cytoplasmic fatty acid-binding proteins. Biochim Biophys Acta. 1991;1081:1–24. doi: 10.1016/0005-2760(91)90244-c. [DOI] [PubMed] [Google Scholar]
- 8.Veerkamp JH, Paulussen RJ, Peeters RA, Maatman RG, van Moerkerk HT, van Kuppevelt TH. Detection, tissue distribution and (sub)cellular localization of fatty acid-binding protein types. Mol Cell Biochem. 1990;98:11–8. doi: 10.1007/BF00231362. [DOI] [PubMed] [Google Scholar]
- 9.O’Brien PJ. Cardiac troponin is the most effective translational safety biomarker for myocardial injury in cardiotoxicity. Toxicology. 2008;245:206–18. doi: 10.1016/j.tox.2007.12.006. [DOI] [PubMed] [Google Scholar]
- 10.Glatz JF, Kleine AH, van Nieuwenhoven FA, Hermens WT, van Dieijen-Visser MP, van der Vusse GJ. Fatty-acid-binding protein as a plasma marker for the estimation of myocardial infarct size in humans. Br Heart J. 1994;71:135–40. doi: 10.1136/hrt.71.2.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Meng X, Ming M, Wang E. Heart fatty acid binding protein as a marker for postmortem detection of early myocardial damage. Forensic Sci Int. 2006;160:11–6. doi: 10.1016/j.forsciint.2005.08.008. [DOI] [PubMed] [Google Scholar]
- 12.Kilcullen N, Viswanathan K, Das R, Morrell C, Farrin A, Barth JH, Hall AS. Heart-type fatty acid-binding protein predicts long-term mortality after acute coronary syndrome and identifies high-risk patients across the range of troponin values. J Am Coll Cardiol. 2007;50:2061–7. doi: 10.1016/j.jacc.2007.08.021. [DOI] [PubMed] [Google Scholar]
- 13.O’Donoghue M, de Lemos JA, Morrow DA, Murphy SA, Buros JL, Cannon CP, Sabatine MS. Prognostic utility of heart-type fatty acid binding protein in patients with acute coronary syndromes. Circulation. 2006;114:550–7. doi: 10.1161/CIRCULATIONAHA.106.641936. [DOI] [PubMed] [Google Scholar]
- 14.Ishii J, Ozaki Y, Lu J, Kitagawa F, Kuno T, Nakano T, Nakamura Y, Naruse H, Mori Y, Matsui S, Oshima H, Nomura M, Ezaki K, Hishida H. Prognostic value of serum concentration of heart-type fatty acid-binding protein relative to cardiac troponin T on admission in the early hours of acute coronary syndrome. Clin Chem. 2005;51:1397–404. doi: 10.1373/clinchem.2004.047662. [DOI] [PubMed] [Google Scholar]
- 15.Colli A, Josa M, Pomar JL, Mestres CA, Gherli T. Heart fatty acid binding protein in the diagnosis of myocardial infarction: where do we stand today? Cardiology. 2007;108:4–10. doi: 10.1159/000095594. [DOI] [PubMed] [Google Scholar]
- 16.Harrell FE, Jr, Lee KL, Mark DB. Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med. 1996;15:361–87. doi: 10.1002/(SICI)1097-0258(19960229)15:4<361::AID-SIM168>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]
- 17.Cook NR, Buring JE, Ridker PM. The effect of including C-reactive protein in cardiovascular risk prediction models for women. Ann Intern Med. 2006;145:21–9. doi: 10.7326/0003-4819-145-1-200607040-00128. [DOI] [PubMed] [Google Scholar]
- 18.Valle HA, Riesgo LG, Bel MS, Gonzalo FE, Sanchez MS, Oliva LI. Clinical assessment of heart-type fatty acid binding protein in early diagnosis of acute coronary syndrome. Eur J Emerg Med. 2008;15:140–4. doi: 10.1097/MEJ.0b013e3282efd47a. [DOI] [PubMed] [Google Scholar]
- 19.Hasegawa T, Yoshimura N, Oka S, Ootaki Y, Toyoda Y, Yamaguchi M. Evaluation of heart fatty acid-binding protein as a rapid indicator for assessment of myocardial damage in pediatric cardiac surgery. J Thorac Cardiovasc Surg. 2004;127:1697–702. doi: 10.1016/j.jtcvs.2004.02.006. [DOI] [PubMed] [Google Scholar]
- 20.Malik V, Kale SC, Chowdhury UK, Ramakrishnan L, Chauhan S, Kiran U. Myocardial injury in coronary artery bypass grafting: on-pump versus off-pump comparison by measuring heart-type fatty-acid-binding protein release. Tex Heart Inst J. 2006;33:321–7. [PMC free article] [PubMed] [Google Scholar]
- 21.Chowdhury UK, Malik V, Yadav R, Seth S, Ramakrishnan L, Kalaivani M, Reddy SM, Subramaniam GK, Govindappa R, Kakani M. Myocardial injury in coronary artery bypass grafting: on-pump versus off-pump comparison by measuring high-sensitivity C-reactive protein, cardiac troponin I, heart-type fatty acid-binding protein, creatine kinase-MB, and myoglobin release. J Thorac Cardiovasc Surg. 2008;135:1110–9. 1119, e1–10. doi: 10.1016/j.jtcvs.2007.12.029. [DOI] [PubMed] [Google Scholar]
- 22.Suzuki K, Sawa Y, Kadoba K, Takahashi T, Ichikawa H, Kagisaki K, Ohata T, Matsuda H. Early detection of cardiac damage with heart fatty acid-binding protein after cardiac operations. Ann Thorac Surg. 1998;65:54–8. doi: 10.1016/s0003-4975(97)01260-5. [DOI] [PubMed] [Google Scholar]
- 23.Hayashida N, Chihara S, Akasu K, Oda T, Tayama E, Kai E, Kawara T, Aoyagi S. Plasma and urinary levels of heart fatty acid-binding protein in patients undergoing cardiac surgery. Jpn Circ J. 2000;64:18–22. doi: 10.1253/jcj.64.18. [DOI] [PubMed] [Google Scholar]
- 24.Muehlschlegel JD, Perry TE, Liu K-Y, Nascimben L, Fox AA, Collard CD, Avery EG, Aranki SF, D’Ambra MN, Shernan SK, Body SC CABG Genomics Investigators. Troponin is superior to electrocardiogram and creatinine kinase MB for predicting clinically significant myocardial injury after coronary artery bypass grafting. Eur Heart J. 2009;30:1574–83. doi: 10.1093/eurheartj/ehp134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Thielmann M, Massoudy P, Schmermund A, Neuhauser M, Marggraf G, Kamler M, Herold U, Aleksic I, Mann K, Haude M, Heusch G, Erbel R, Jakob H. Diagnostic discrimination between graft-related and non-graft-related perioperative myocardial infarction with cardiac troponin I after coronary artery bypass surgery. Eur Heart J. 2005;26:2440–7. doi: 10.1093/eurheartj/ehi437. [DOI] [PubMed] [Google Scholar]
- 26.Petzold T, Feindt P, Sunderdiek U, Boeken U, Fischer Y, Gams E. Heart-type fatty acid binding protein (hFABP) in the diagnosis of myocardial damage in coronary artery bypass grafting. Eur J Cardiothorac Surg. 2001;19:859–64. doi: 10.1016/s1010-7940(01)00709-6. [DOI] [PubMed] [Google Scholar]
- 27.Niizeki T, Takeishi Y, Arimoto T, Takabatake N, Nozaki N, Hirono O, Watanabe T, Nitobe J, Harada M, Suzuki S, Koyama Y, Kitahara T, Sasaki T, Kubota I. Heart-type fatty acid-binding protein is more sensitive than troponin T to detect the ongoing myocardial damage in chronic heart failure patients. J Card Fail. 2007;13:120–7. doi: 10.1016/j.cardfail.2006.10.014. [DOI] [PubMed] [Google Scholar]
- 28.Alhashemi JA. Diagnostic accuracy of a bedside qualitative immunochromatographic test for acute myocardial infarction. Am J Emerg Med. 2006;24:149–55. doi: 10.1016/j.ajem.2005.08.002. [DOI] [PubMed] [Google Scholar]
- 29.Liao J, Chan CP, Cheung YC, Lu JH, Luo Y, Cautherley GW, Glatz JF, Renneberg R. Human heart-type fatty acid-binding protein for on-site diagnosis of early acute myocardial infarction. Int J Cardiol. 2009;133:420–3. doi: 10.1016/j.ijcard.2008.01.049. [DOI] [PubMed] [Google Scholar]
- 30.Mad P, Domanovits H, Fazelnia C, Stiassny K, Russmuller G, Cseh A, Sodeck G, Binder T, Christ G, Szekeres T, Laggner A, Herkner H. Human heart-type fatty-acid-binding protein as a point-of-care test in the early diagnosis of acute myocardial infarction. QJM. 2007;100:203–10. doi: 10.1093/qjmed/hcm007. [DOI] [PubMed] [Google Scholar]
- 31.Fox AA, Collard CD, Shernan SK, Seidman CE, Seidman JG, Liu KY, Muehlschlegel JD, Perry TE, Aranki SF, Lange C, Herman DS, Meitinger T, Lichtner P, Body SC. Natriuretic peptide system gene variants are associated with ventricular dysfunction after coronary artery bypass grafting. Anesthesiology. 2009;110:738–47. doi: 10.1097/aln.0b013e31819c7496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fox AA, Shernan SK, Collard CD, Liu KY, Aranki SF, DeSantis SM, Jarolim P, Body SC. Preoperative B-type natriuretic peptide is as independent predictor of ventricular dysfunction and mortality after primary coronary artery bypass grafting. J Thorac Cardiovasc Surg. 2008;136:452–61. doi: 10.1016/j.jtcvs.2007.12.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Daniels LB, Laughlin GA, Clopton P, Maisel AS, Barrett-Connor E. Minimally elevated cardiac troponin T and elevated N-terminal pro-B-type natriuretic peptide predict mortality in older adults: results from the Rancho Bernardo Study. J Am Coll Cardiol. 2008;52:450–9. doi: 10.1016/j.jacc.2008.04.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Swaminathan M, Morris RW, De Meyts DD, Podgoreanu MV, Jollis JG, Grocott HP, Milano CA, Newman MF, Mathew JP. Deterioration of regional wall motion immediately after coronary artery bypass graft surgery is associated with long-term major adverse cardiac events. Anesthesiology. 2007;107:739–45. doi: 10.1097/01.anes.0000287008.70453.81. [DOI] [PubMed] [Google Scholar]