Abstract
BACKGROUND:
Heart disease and stroke are leading causes of death in North America. Nevertheless, in 2003, the Heart and Stroke Foundation of Canada reported that nearly two-thirds of Canadians have misconceptions regarding heart disease and stroke, echoing the results of similar American studies. Good knowledge of these conditions is imperative for cardiac patients who are at greater risk than the general population and should, therefore, be better educated. The present study evaluated the awareness of heart disease and stroke among cardiac patients to assess the efficacy of current education efforts.
METHODS:
Two hundred fifty-one cardiac inpatients and outpatients at St Michael’s Hospital (Toronto, Ontario) were surveyed in July and August 2004. An unaided questionnaire assessed respondents’ knowledge of cardiovascular risk factors, symptoms of heart attack and stroke, and actions in the event of cardiovascular emergency. Demographic data and relevant medical history were also obtained.
RESULTS:
Cardiac patients demonstrated relatively adequate knowledge of heart attack warning symptoms. These patients also demonstrated adequate awareness of proper actions during cardiovascular emergencies. However, respondents were not aware of the most important risk factors for cardiovascular disease. Knowledge of stroke symptoms was also extremely poor. Socioeconomic status, and personal history of heart attack and stroke were positively correlated with good knowledge.
CONCLUSIONS:
Future patient education efforts should address the awareness of the important cardiovascular risk factors and knowledge of cardiovascular warning symptoms (especially for stroke), as well as inform patients of appropriate actions during a cardiovascular emergency. Emphasis should be placed on primary and secondary prevention, and interventions should be directed toward low-income cardiac patients.
Keywords: Heart attack, Myocardial infarction, Prevention, Public health education, Stroke
Abstract
HISTORIQUE :
Les maladies cardiaques et les accidents vasculaires cérébraux (AVC) sont des causes importantes de décès en Amérique du Nord. Néanmoins, en 2003, la Fondation des maladies du cœur du Canada a annoncé que près des deux tiers des Canadiens avaient des idées fausses au sujet des maladies cardiaques et des AVC, reflétant les résultats d’études américaines similaires. Il est impératif pour les patients cardiaques de bien connaître ces maladies, car ils sont plus vulnérables que la population générale et devraient donc être mieux informés. La présente étude a permis d’évaluer la sensibilisation aux maladies cardiaques et aux AVC chez les patients cardiaques, afin de déterminer l’efficacité des efforts d’éducation en cours.
MÉTHODOLOGIE :
Deux cent cinquante et un patients cardiaques hospitalisés et en consultations externes du St Michael’s Hospital (de Toronto, en Ontario) ont participé à un sondage en juillet et août 2004. Un questionnaire que les répondants remplissaient seuls a permis d’évaluer leurs connaissances des facteurs de risque cardiovasculaires, des symptômes de crise cardiaque et d’AVC et des mesures à prendre en cas d’urgence cardiaque. Les données démographiques et les antécédents médicaux pertinents étaient également sondés.
RÉSULTATS :
Les patients cardiaques avaient des connaissances relativement pertinentes sur les symptômes annonciateurs de crise cardiaque. Ils savaient également quelles mesures prendre pendant une urgence cardiaque. Cependant, ils ne connaissaient pas les principaux facteurs de risque de maladie cardiovasculaire et connaissaient très peu les symptômes d’AVC. Le statut socioéconomique et les antécédents personnels de crise cardiaque et d’AVC étaient corrélés positivement aux bonnes connaissances.
CONCLUSIONS :
Les futurs efforts d’éducation des patients devraient porter sur les principaux facteurs de risque cardiovasculaire et les symptômes annonciateurs de troubles cardiaques (surtout l’AVC) et les informer des mesures à prendre en cas d’urgence cardiaque. Il faudrait s’attarder sur la prévention primaire et secondaire et orienter les interventions vers les patients cardiaques à faible revenu.
The 2003 Heart and Stroke Foundation’s Annual Report Card on Canadians’ health (1) stated that up to 60% of Canadians were “seriously misinformed” with respect to their knowledge of the risk factors and warning symptoms of heart disease and stroke. According to the Health Belief Model, such health knowledge is important for behaviour modification and encourages prompt, proper emergency action (2) leading to effective treatment. Thrombolytic therapy has been shown to reduce morbidity and mortality when administered as soon as possible following the onset of a heart attack (3). In addition, early treatment with intravenous tissue plasminogen activator has been shown to improve patient outcomes when administered within 3 h of the onset of stroke (4).
Community-based, open-ended telephone survey studies in the United States and Australia (5–9) have reported that awareness of all heart attack and stroke symptoms is low among the general public. Individuals categorized as being at higher risk for coronary artery disease have also been shown to exhibit poor knowledge of its risk factors (10,11). However, little is known about heart disease patients’ knowledge of the risk factors and symptoms for heart disease and stroke. These patients are expected to be more familiar with these topics because they are at greater risk of suffering from heart attacks and strokes than the general population, and should also be better educated in this regard (5).
We conducted a cross-sectional study of patients admitted to cardiology floors or attending outpatient cardiology clinics at an inner-city tertiary care hospital in Toronto, Ontario. The objective of the study was to determine the level of cardiovascular knowledge in this group of patients. The cardiovascular knowledge assessed included level of awareness of cardiac risk factors, warning symptoms and appropriate emergency actions in case of a heart attack or stroke. This information will help gauge the adequacy of our current education efforts and aid in the development of health promotion initiatives targeted to this high-risk population. It will also identify specific knowledge gaps and misconceptions regarding heart disease and stroke among cardiac patients.
METHODS
A 30-item questionnaire was administered to inpatients admitted to the cardiology units (coronary care unit and cardiology ward) and outpatients attending cardiology clinics at St Michael’s Hospital in Toronto. The questionnaire was adopted from Chow et al (12), who evaluated cardiovascular health knowledge among Chinese Canadians. Individuals employed in health-related fields, their relatives and those younger than 18 years of age were excluded from participation in the study. Inpatients who were recovering from cardiac operations were also excluded. In total, 251 patients agreed to participate in the study. The response rate was 93%; 20 patients declined to participate.
A trained research assistant (RG) administered the questionnaire to each participant after obtaining signed consent forms. The questionnaire was unaided (ie, responses were not prompted). During the interviews, patients were first asked to list the risk factors of heart disease and stroke. They were then asked to name the warning symptoms for these two conditions. The ‘correct’ warning symptoms for heart attack and stroke were obtained from the website and brochures of the Heart and Stroke Foundation of Canada (13) and the American Heart Association (14). The cardiovascular risk factors included sex, family history, age, diet, hypertension, stress, diabetes, alcohol abuse, cholesterol, overweight or obesity, smoking, and inactivity or lack of exercise. Warning symptoms of heart attack included chest pain, arm pain, sweating, trouble breathing, nausea and loss of consciousness. Warning symptoms of stroke included weakness in one-half of the body, numbness in one-half of the body, speech difficulties, visual disturbances, severe headache, loss of consciousness and dizziness.
Following the criteria used by Weltermann et al (15), subjects were classified as having good knowledge of risk factors, heart attack warning symptoms or stroke warning symptoms if they were able to identify at least two correct answers in each category. In addition, subjects were defined as having excellent knowledge if they were able to identify at least four correct responses. Participants were also asked to state what action they would take in the event of a heart attack or stroke. Patient demographic variables of interest included age, sex, level of education, household income and relevant medical history (for heart disease and stroke).
SPSS (Mac OS version 11, SPSS Inc, USA) was used for statistical analysis. Descriptive data were presented as frequency and percentage. χ2 and multiple logistic regression analysis were used to identify predictors of the ability to identify risk factors, heart attack or stroke warning symptoms. Statistical significance was set at P<0.05.
The study was approved by the Research Ethics Board of St Michael’s Hospital.
RESULTS
Characterization of survey subjects
Between July 2 and August 23, 2004, 251 patients from St Michael’s Hospital were interviewed. Forty-eight per cent of the respondents were inpatients from the cardiology ward and coronary care unit, while 52% were outpatients attending cardiology clinics. The subjects’ median age was 66 years, and 63% were men. Seventy-four study participants had a history of heart disease and 12 had a history of stroke (Table 1).
TABLE 1.
Demographics of study subjects
| Characteristic | n (%) |
|---|---|
| Age >65 years | 126 (50.2) |
| Sex (male) | 159 (63.3) |
| Inpatients | 120 (47.8) |
| Level of education ≥ college | 129 (51.4) |
| Household income ≥$50,000 | 91 (36.3)* |
| History of heart disease | 74 (29.5) |
| History of stroke | 12 (4.8) |
76 patients refused to answer
Risk factor awareness
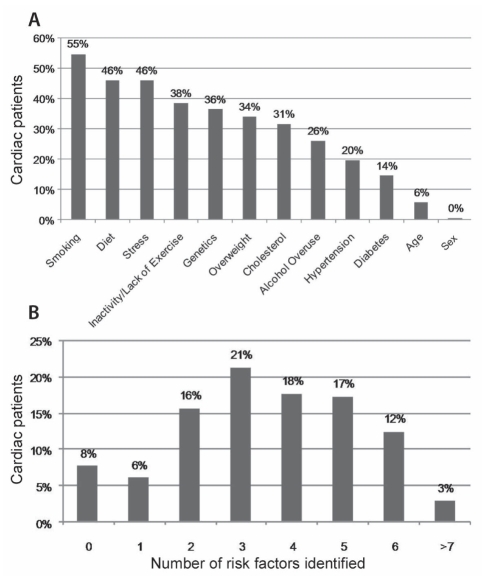
Respondents were first asked to independently identify risk factors for heart disease and stroke. Smoking, diet, stress, inactivity or lack of exercise, and genetics were the five most commonly stated cardiovascular risk factors. Only smoking was identified by more than 50% of the patients. Alcohol abuse, hypertension, diabetes, age and sex were the five least commonly stated risk factors (Figure 1A). Eighty-seven per cent of subjects were able to name at least two risk factors and, therefore, had good knowledge according to criteria set by Weltermann et al (15). A total of 50% named at least four risk factors and had excellent knowledge. Eight per cent of the participants were unable to identify any risk factors (Figure 1B). A household income of $50,000 or more (P=0.017) and the absence of stroke history (P=0.006) were significant predictors of good risk factor knowledge (Table 2).
Figure 1).
A Cardiovascular risk factors for heart disease and stroke as identified by cardiac patients. B Number of cardiovascular risk factors for heart disease and stroke identified by cardiac patients
TABLE 2.
Multivariate analysis of good cardiovascular risk factor knowledge
| Independent variable | Adjusted | ||||
|---|---|---|---|---|---|
| Estimate | SE | OR | 95% CI | P | |
| Stroke history | –1.659 | 0.607 | 0.190 | 0.058–0.625 | 0.006 |
| Income ≥$50,000 | 1.354 | 0.570 | 3.874 | 1.268–11.839 | 0.017 |
Heart attack symptom knowledge
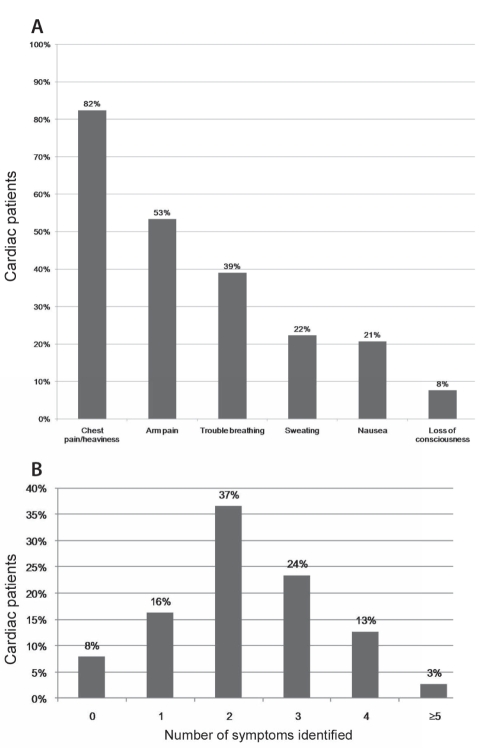
The cardiac patients’ knowledge of heart attack symptoms was then assessed in an open-ended fashion. More than one-half of the respondents were able to name chest pain and arm pain as heart attack symptoms. Only 39% stated shortness of breath, while fewer than 25% identified sweating, nausea or loss of consciousness as warning symptoms of heart attack (Figure 2A). Seventy-seven per cent had good knowledge of heart attack symptoms, while only 16% were able to list at least four and 8% were unable to name any (Figure 2B). A household income of $50,000 or more (P=0.005) and a history of heart disease (P<0.001) were significant predictors of good knowledge of heart attack symptoms (Table 3).
Figure 2).
A Percentage of cardiac patients who identified a heart attack warning symptom. B Number of heart disease symptoms identified by cardiac patients
TABLE 3.
Multivariate analysis of good heart attack symptom knowledge
| Independent variable | Adjusted | ||||
|---|---|---|---|---|---|
| Estimate | SE | OR | 95% CI | P | |
| CVD history | 1.595 | 0.455 | 4.928 | 2.020–12.025 | <0.001 |
| Income ≥$50,000 | 1.182 | 0.417 | 3.261 | 1.440–7.385 | 0.005 |
CVD Cardiovascular disease
Stroke symptom knowledge
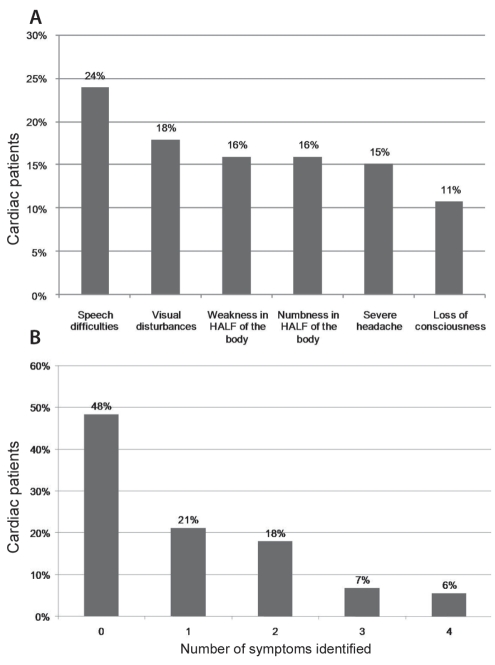
Patients were also asked to spontaneously identify stroke symptoms. Fewer than 25% were able to identify any one symptom (Figure 3A). Almost one-half (48%) of the patients were unable to name any stroke symptoms and only 31% had good knowledge. Only 6% had excellent knowledge (Figure 3B). Having more than a college education (P=0.038), a household income $50,000 or more (P=0.014) and a history of stroke (P=0.043) were significant predictors of good stroke symptom knowledge (Table 4).
Figure 3).
A Percentage of cardiac patients who identified stroke warning symptoms. B Number of stroke symptoms identified by cardiac patients
TABLE 4.
Multivariate analysis of good stroke symptom knowledge
| Independent variable | Adjusted | ||||
|---|---|---|---|---|---|
| Estimate | SE | OR | 95% CI | P | |
| Education ≥ college | 0.757 | 0.364 | 2.131 | 1.044–4.350 | 0.038 |
| Stroke history | 1.033 | 0.511 | 2.809 | 1.032–7.647 | 0.043 |
| Income ≥$50,000 | 0.893 | 0.362 | 2.443 | 1.202–4.969 | 0.014 |
Knowledge of action in case of cardiovascular emergency
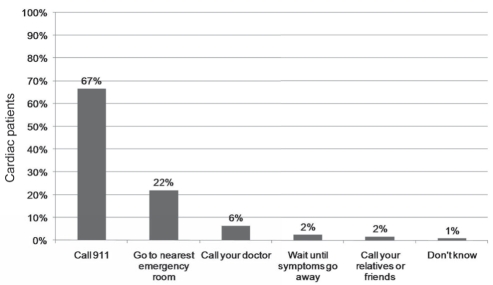
Finally, respondents were asked what action they would take in the event of a cardiovascular emergency such as a heart attack or stroke. Eighty-nine per cent of the patients surveyed stated that they would either call 911 or go to the nearest emergency room. These were characterized as good emergency actions. Ten per cent said they would call their family doctor or relatives and friends, or wait for symptoms to subside (Figure 4). There were no significant predictors of appropriate emergency action.
Figure 4).
Immediate action in case of cardiac emergency identified by cardiac patients
DISCUSSION
Cardiac patients are at substantially higher risk for heart disease and stroke than the general population. In fact, the risk of stroke is increased 44-fold following myocardial infarction, compared with individuals who have not experienced a heart attack (16). It is, therefore, imperative that cardiac patients be well informed of cardiovascular risk factors and warning symptoms, as well as the appropriate action in case of a cardiovascular emergency. Many of the patients surveyed at the hospital were visiting cardiologists because they had a history of heart disease or stroke, or were at high risk of developing cardiovascular disease. They were, therefore, expected to be better informed regarding these conditions compared with the general public. These patients’ knowledge of heart disease and stroke was ascertained using an unaided questionnaire to assess contemporary education efforts and identify particularly misinformed subgroups. Inpatients and outpatients were analyzed together because they did not differ substantially in terms of demographics or degree of cardiovascular disease knowledge. The results of the present study showed that among cardiac patients, knowledge of cardiovascular risk factors and appropriate emergency action was relatively adequate, but knowledge deficits with respect to cardiovascular warning symptoms, especially those of stroke, need to be remedied.
We decided to use an unaided questionnaire to avoid prompting respondents, which would have led to greater estimated levels of knowledge (17,18). When patients’ wrong or incomplete responses were corrected following the surveys, many claimed they were actually aware of the right answers. While this suggests that our data may underestimate respondents’ knowledge, we believe that unaided answers provide an accurate representation of patients’ knowledge and awareness during cardiovascular emergencies. Individuals able to state symptoms without prompting may have a better understanding of heart disease and stroke, making them better prepared for such medical emergencies (19).
Eighty-seven per cent of the surveyed subjects were able to name at least two risk factors and, therefore, had good knowledge according to criteria set by Weltermann et al (15) (Figure 1B). This compares favourably with the number of people able to identify two or more risk factors (25% to 62%) in open-ended telephone surveys of the general population’s knowledge of heart disease and stroke (7–9). An annual household income of $50,000 or more and a personal history of stroke were predictors of good risk factor knowledge. Community-based telephone studies (9,10) also found socioeconomic status to be positively correlated with risk factor knowledge.
Although a large percentage of patients had good risk factor knowledge, the risk factors considered to be of greater importance by the medical community (age, sex, diabetes, hypertension and alcohol abuse) were identified least frequently (Figure 1A). Only 20% of our subjects identified hypertension, which is the most important risk factor for stroke (20). This was consistent with findings from a study on the Canadian public’s awareness of cardiovascular disease risk factors (10). Interestingly, higher proportions of the general public in the United States (32% to 51%) (6–8) and Australia (32%) (9) were able to identify hypertension, although this may be attributable to the fact that these data were from studies focused on stroke. Nevertheless, considering the intimate relationship between heart attack and stroke, future education efforts need to emphasize the significance of hypertension along with the other important cardiovascular risk factors that were under-reported.
Heart attack symptom knowledge was appropriate, which was expected considering the patient population being studied (Figure 2B). Good knowledge was significantly correlated with a history of heart attack and a household income of $50,000 or more, which is consistent with results from the community-based telephone study by Goff et al (5). However, nearly 90% of individuals surveyed in that study were able to identify chest paint as a heart attack symptom (5), compared with 82% in the present study. This suggests that current efforts to educate cardiac patients should be better because this subgroup is expected, and needs, to be more knowledgeable about heart disease warning symptoms than the general public. Further improvements in symptom knowledge will ultimately lead to further improvements in patient outcome.
Cardiac patients’ knowledge of stroke symptoms was extremely poor. Only 31% of respondents had good stroke symptom knowledge (Figure 3B). Similarly, close to 30% of respondents exhibited good knowledge in other community-based, open-ended telephone surveys (7–9). Postsecondary education, a history of stroke and a household income of $50,000 or more were significant predictors of good knowledge of stroke symptoms. These characteristics have also been reported to be correlates of good stroke symptom knowledge in studies on the general population (7,9). Recognition of stroke symptoms can be challenging due to their heterogeneous nature (21). Nevertheless, given the 44-fold increased risk of stroke following myocardial infarction (16), it is crucial for cardiac patients to be well educated about stroke symptoms. Furthermore, as was the case with heart attack symptoms, early recognition of stroke warning symptoms leads to proper emergency action and reduced mortality (4,22).
Not surprisingly, history of heart disease and stroke were predictors of good heart attack and stroke symptom knowledge, respectively. Therefore, targeted community-based interventions that aim to facilitate primary and secondary prevention of these diseases would be appropriate. A household income of $50,000 or more was consistently associated with good cardiovascular disease knowledge. This can be attributed to the fact that a higher income enables individuals to be better informed about health information and better able to put this knowledge into practice as a consequence of having access to more social and economic resources (23). The opposite is true for individuals with low socioeconomic status who should, therefore, be a focus of future education efforts. Interestingly, income was a much stronger predictor of good knowledge than higher education, which was only associated with good stroke symptom knowledge. This is consistent with the notion that education reflects access to resources earlier on in people’s lives, while income is more reflective of present conditions and opportunities (10).
As mentioned, recognition of heart attack and stroke warning symptoms is an important prerequisite for prompt and effective care. This also requires taking proper emergency action (calling 911 or going to the nearest hospital). Among the patients surveyed, there were no significant predictors of proper action. Eighty-nine per cent of respondents said they would take such emergency actions (Figure 4). A similarly high proportion (89.9%) of the general population respondents examined by Sug Yoon et al (9) said they would take proper emergency action in the event of a stroke. Therefore, while our finding among cardiac patients is encouraging, their comparability with the general population despite being at higher risk indicates room for improvement.
While the present study assessed the major barriers to seeking prompt and proper care during cardiovascular emergencies, issues such as denial and fear of embarrassment during false alarms, and misconceptions about heart disease and stroke merit consideration. Therefore, in addition to emphasizing proper emergency actions, future education efforts should also teach patients what not to do in the event of a heart attack or stroke.
CONCLUSION
Given cardiac patients’ knowledge, or lack thereof, regarding heart disease and stroke, future education strategies should emphasize the most important cardiovascular risk factors, especially hypertension; further improve heart attack symptom knowledge; and substantially improve stroke symptom knowledge, in light of the intimate relationship between heart disease and stroke. Considering the importance of prompt treatment in improving patient outcomes, we must continue to advise patients with regard to appropriate action during emergencies. Finally, the most important implication of the present study is the need to focus on primary and secondary prevention, and crucially, target low-income cardiac patients.
Footnotes
DISCLOSURE: This study was presented in part as an oral abstract presentation at the Canadian Cardiovascular Congress, 2005.
REFERENCES
- 1.Seven Deadly Myths Threatening Canadians’ Heart Health, says Heart and Stroke Foundation’s Annual Report Card. Feb 23, 2003. < http://www.heartandstroke.ns.ca/site/c.inKMIPNlEiG/b.3668395/k.46AC/2003_Report_Card__Seven_Deadly_Myths_Threatening_Canadians_Heart_Health.htm> (Accessed on April 2, 2009).
- 2.Maiman LA, Becker MH, Kirscht JP, Haefner DP, Drachman RH. Scales for measuring health belief model dimensions: A test of predictive value, internal consistency, and relationships among beliefs. Health Educ Monogr. 1977;5:215–30. doi: 10.1177/109019817700500303. [DOI] [PubMed] [Google Scholar]
- 3.Stenestrand U, Lindback J, Wallentin L. Long-term outcome of primary percutaneous coronary intervention vs prehospital and in-hospital thrombolysis for patients with ST-elevation myocardial infarction. JAMA. 2006;296:1749–56. doi: 10.1001/jama.296.14.1749. [DOI] [PubMed] [Google Scholar]
- 4.Tissue plasminogen activator for acute ischemic stroke The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. N Engl J Med. 1995;333:1581–7. doi: 10.1056/NEJM199512143332401. [DOI] [PubMed] [Google Scholar]
- 5.Goff DC, Jr, Sellers DE, McGovern PG, et al. Knowledge of heart attack symptoms in a population survey in the United States: The REACT Trial. Rapid Early Action for Coronary Treatment. Arch Intern Med. 1998;158:2329–38. doi: 10.1001/archinte.158.21.2329. [DOI] [PubMed] [Google Scholar]
- 6.Hux K, Rogers T, Mongar K. Common perceptions about strokes. J Community Health. 2000;25:47–65. doi: 10.1023/a:1005140918066. [DOI] [PubMed] [Google Scholar]
- 7.Reeves MJ, Hogan JG, Rafferty AP. Knowledge of stroke risk factors and warning signs among Michigan adults. Neurology. 2002;59:1547–52. doi: 10.1212/01.wnl.0000031796.52748.a5. [DOI] [PubMed] [Google Scholar]
- 8.Schneider AT, Pancioli AM, Khoury JC. Trends in community knowledge of the warning signs and risk factors for stroke. JAMA. 2003;289:343–6. doi: 10.1001/jama.289.3.343. [DOI] [PubMed] [Google Scholar]
- 9.Sug Yoon S, Heller RF, Levi C, Wiggers J, Fitzgerald PE. Knowledge of stroke risk factors, warning symptoms, and treatment among an Australian urban population. Stroke. 2001;32:1926–30. doi: 10.1161/01.str.32.8.1926. [DOI] [PubMed] [Google Scholar]
- 10.Potvin L, Richard L, Edwards AC. Knowledge of cardiovascular disease risk factors among the Canadian population: Relationships with indicators of socioeconomic status. CMAJ. 2000;162(9 Suppl):S5–11. [PMC free article] [PubMed] [Google Scholar]
- 11.Zerwic JJ, King KB, Wlasowicz GS. Perceptions of patients with cardiovascular disease about the causes of coronary artery disease. Heart Lung. 1997;26:92–8. doi: 10.1016/s0147-9563(97)90068-6. [DOI] [PubMed] [Google Scholar]
- 12.Chow CM, Chu JY, Tu JV, Moe GW. Lack of awareness of heart disease and stroke among Chinese Canadians: Results of a pilot study of the Chinese Canadian Cardiovascular Health Project. Can J Cardiol. 2008;24:623–8. doi: 10.1016/s0828-282x(08)70650-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Heart and Stroke Foundation of Canada < http://www.heartandstroke.ca/> (Accessed on April 2, 2009).
- 14.American Heart Association < http://www.americanheart.org/> (Accessed on April 2, 2009).
- 15.Weltermann BM, Homann J, Rogalewski A, Brach S, Voss S, Ringelstein EB. Stroke knowledge among stroke support group members. Stroke. 2000;31:1230–3. doi: 10.1161/01.str.31.6.1230. [DOI] [PubMed] [Google Scholar]
- 16.Witt BJ, Brown RD, Jr, Jacobsen SJ, Weston SA, Yawn BP, Roger VL. A community-based study of stroke incidence after myocardial infarction. Ann Intern Med. 2005;143:785–92. doi: 10.7326/0003-4819-143-11-200512060-00006. [DOI] [PubMed] [Google Scholar]
- 17.Haines CM, Ward GW. Recent trends in public knowledge, attitudes, and reported behaviour with respect to high blood pressure. Public Health Rep. 1981;96:514–22. [PMC free article] [PubMed] [Google Scholar]
- 18.Sudman S, Bradburn NM. Asking questions. San Francisco: Jossey-Bass; 1982. [Google Scholar]
- 19.Margellos-Anast H, Estarziau M, Kaufman G. Cardiovascular disease knowledge among culturally deaf patients in Chicago. Prev Med. 2006;42:235–9. doi: 10.1016/j.ypmed.2005.12.012. [DOI] [PubMed] [Google Scholar]
- 20.Feinberg WM. Primary and secondary stroke prevention. Curr Opin Neurol. 1996;9:46–52. doi: 10.1097/00019052-199602000-00010. [DOI] [PubMed] [Google Scholar]
- 21.Yoon SS, Byles J. Perceptions of stroke in the general public and patients with stroke: A qualitative study. BMJ. 2002;324:1065–8. doi: 10.1136/bmj.324.7345.1065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Evenson KR, Rosamond WD, Morris DL. Prehospital and in-hospital delays in acute stroke care. Neuroepidemiology. 2001;20:65–76. doi: 10.1159/000054763. [DOI] [PubMed] [Google Scholar]
- 23.Link B, Phelan J. Social conditions as fundamental causes of disease. J Health Soc Behav. 1995 Spec No:80-94. [PubMed] [Google Scholar]