Abstract
The interplay of psychotic and affective symptoms is a crucial challenge in understanding the pathogenesis of psychosis. In this study, we analyzed the interplay between two subclinical psychosis symptoms dimensions, and one depression symptoms dimension, using longitudinal data from Zurich. The Zurich study started in 1979 with a representative sample of 591 participants who were aged 20/21. Follow-up interviews were conducted at age 23, 28, 30, 35, and 41. The psychiatric symptoms were assessed with a semi-structured interview and the SCL 90-R. In this study, we analyzed three SCL-90-R subscales: the depression symptoms dimension and two distinct symptoms dimensions of subclinical psychosis, one representing a schizophrenia nuclear symptom dimension, the other representing a schizotypal symptoms dimension. Modeling was done with hybrid latent growth models, thereby including simultaneous and cross-lagged effects. The interplay between the two subclinical psychosis symptoms dimensions and the depression symptoms dimension includes several intertwined pathways. The schizotypal symptoms dimension has strong direct effects on the schizophrenia nuclear symptoms dimension, but also on the depression symptoms dimension. The latter has for its part an effect on the schizophrenia nuclear symptoms dimension. The main driving force within the dynamic interplay between depression and psychosis symptoms is a schizotypal symptoms dimension, which represents social and interpersonal deficiencies, ideas of reference, suspiciousness, paranoid ideation, and odd behavior. It does not only directly influence subclinical nuclear schizophrenia symptoms but also the symptoms of depression.
Keywords: Subclinical psychosis, Schizotypy, Schizotypal personality disorder, Depression, Community study, Epidemiological cohort
Introduction
The interplay between psychotic and affective symptoms is a crucial challenge in understanding the pathogenesis of psychosis. In most instances, the prodromal stages of schizophrenia involve concomitant depressive symptoms [16–18, 22, 23, 46]. Depression also frequently occurs during schizophrenic episodes [38]. The stages of depression and schizophrenia often appear to coalesce [2, 26]. These interactions have left much room for speculation. In this study, we analyzed the interplay between psychosis symptoms and depression symptoms using longitudinal data from the Zurich cohort study which covered a 20-year period.
Background
The current concept of schizophrenia is based on Kraepelin's categorical model of severe mental illnesses [24]. The Kraepelinian dichotomy between schizophrenia and affective disorders has received much empirical support and has formed the respective diagnostic concepts of DSM or ICD. However, this strict diagnostic dichotomy has been doubted by some scholars. Bleuler [7] in particular observed the occurrence of depressive symptoms in schizophrenia to such an extent that he came to regard depression as a genuine part of the illness process. Häfner et al. [16] hypothesized that both the depressive and the psychotic syndrome are preformed reaction patterns of the brain, though with a different threshold.
To provide more clarity on the interplay between psychosis and depression symptoms in the pathogenesis of psychosis, we should firstly investigate the initial levels of this interplay, i.e., when the disorder has not yet reached a clinical level, and secondly analyze the development of this interplay which is ideally done with longitudinal, prospective data.
Investigating subclinical symptoms
For a long time, research on somatic diseases such as cancer or cardiovascular diseases has encompassed initial stages, preclinical processes, and subclinical symptoms. There is no doubt how important it is to understand the initial levels of a pathogenetic process, for example in order to prevent a certain illness. In contrast, it is a longstanding professional understanding that psychotic symptoms are an expression of severe mental illness. Thus, the current discussion concerning functional psychosis in general, and schizophrenia, in particular, is impeded by the fact that most evidence almost exclusively comes from clinical, most severely ill populations. The related findings may be biased for several reasons:
the likelihood of utilizing mental health services increases with the severity of a disorder; patients with a less severe illness course usually are not included in the respective assessments
most patients involved have already received specific medication thus distorting the natural course of a disease entity
an increasing severity enhances the likelihood of various comorbid disorders [31] in general, and substance use in particular, thus also increasing the chances of confounded and biased findings
the subclinical onset of the illness is almost inevitably assessed retrospectively.
We can assess subclinical symptoms in siblings or close relatives of persons with a clinical expression of a respective illness, but these symptoms should be ideally assessed in community samples. In particular, recent work has suggested that psychosis may be much more frequently expressed at subclinical levels in community samples than has been commonly believed [20, 34, 39, 42].
Signifying subclinical syndromes
The subclinical or subthreshold phenotype of psychosis is often referred to by a diversity of terms as (attenuated) psychotic experiences or beliefs, psychotic (like) experiences, psychosis proneness, at-risk mental states, schizotypy, or schizotaxia [6, 19, 33, 41, 45].
Other authors also have identified those nuclear symptoms on a subclinical level. For example Yung et al. [45], who named those nuclear symptoms “bizarre experiences”, derived from a factor analysis of the “Community Assessment of Psychotic Experiences” (CAPE). Yung and others regularly regard those subclinical psychotic symptoms as transitory to, or prodromes of, frank psychosis. Persons who develop a full-blown psychosis display the same symptoms as in the transitory state albeit to a much greater intensity.
The case is slightly different as regards “schizotypal personality disorder”. Schizotypal personality disorder is regarded as a chronic constellation and represents in many regards a clinical endpoint. The APA [1] sees those persons at no higher risk as the general population for later development of schizophrenia. Others have highlighted the usefulness of studying this disorder in promoting insight into the prodromal state of schizophrenia [36]. Raine [33] views the schizotypal personality disorder as an attenuated form of schizophrenia that represents a premorbid or prodromal stage of this major disorder. He hypothesizes two forms of schizotypal personality disorders: one represents a relatively stable, neurodevelopmental disorder with significant brain and neurocognitive impairments that predispose to schizophrenia, while another form is hypothesized with a more pronounced psychosocial etiology and more symptom fluctuation, but no risk for later schizophrenia.
All in all, it seems clear that comparable to other mental disorders, the expression of psychotic symptoms in a population is continuous and is characterized by differing levels of severity and persistence. Thus, psychotic symptoms can be studied prospectively, and indeed, long before the disorder becomes clinically relevant.
Aims of the study
Assessing the interplay between symptoms of psychosis and depression requires longitudinal data. To date, there have been only few adequate data sources such as the Zurich study, a prospective cohort study over a 20-year period [3, 28]. The data of the Zurich study include subclinical psychotic symptoms, which previously were assigned to two psychosis symptoms dimensions (the schizophrenia nuclear symptoms dimension and the schizotypal symptoms dimension) [34].
In this study, we used the Zurich study data in order to examine the interrelations between these psychosis symptom dimensions and depression symptoms. According to previous research, our prime hypothesis was that depression symptoms are either a predictor, or a precursor, of psychotic symptoms.
Methods
Sample
The Zurich study is a prospective longitudinal cohort study. The Zurich study sample was selected on the basis of a two-phase procedure as described by Dunn et al. [13], which is common in epidemiological research. It is characterized by a screening part and an interview part, whereby the latter is carried out with a subsample of the initially screened subjects, typically stratified along selected criteria and cutoffs. In statistical analysis, the stratified data often need to be weighted for receiving correct point estimates such as prevalence rates.
The screening procedure in the Zurich study took place in 1978 with a sample of 4547 subjects (2201 men; 2346 women) born in 1958 and 1959 representative of the canton of Zurich in Switzerland. At that time, the male participants were 19 years old (at mandatory conscription) and the female participants were 20 years old (complete electoral register). In Switzerland, each male citizen has to present himself for military conscription. With permission from the authorities and independently of the military procedure, we could screen randomly half of the conscripts. The refusal rate was 0.3%. Women were identified at the age of 20 by the complete electoral register; half of the women chosen randomly received mailed questionnaires and 75% of them responded. A lower educational level was overrepresented among non-responding women; in order to correct for that the female interview sample was matched by educational level to the male sample. All subjects received the Symptom Checklist 90-R (SCL-90-R) [10], a comprehensive self-report questionnaire of 90 questions, which covers a broad range of psychiatric symptoms and a demographic questionnaire.
With regard to the second phase, a stratification procedure was applied in order to enrich the interview sample with cases at risk for the development of psychiatric syndromes. The stratification was based on a cutoff value of the SCL90-R global severity index (GSI) score. Two-thirds of the interview sample comprised high scorers (defined by the 85th percentile or above on the SCL90-R GSI scores), and one-third of the interview sample were randomly selected from the rest of the initial sample (GSI scores below the 85th percentile). A total of 591 subjects (292 men, 299 women) were selected for interview.
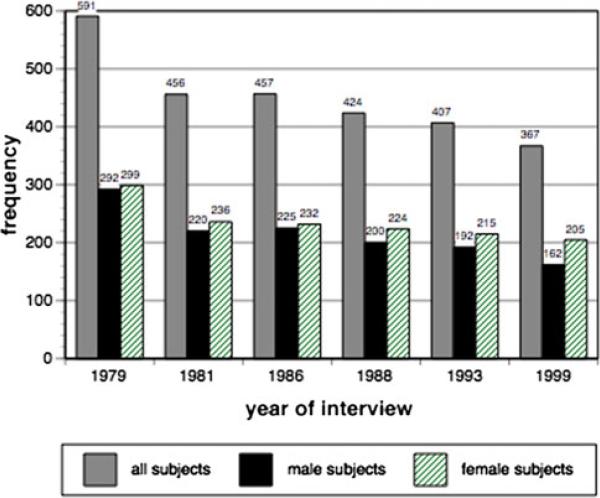
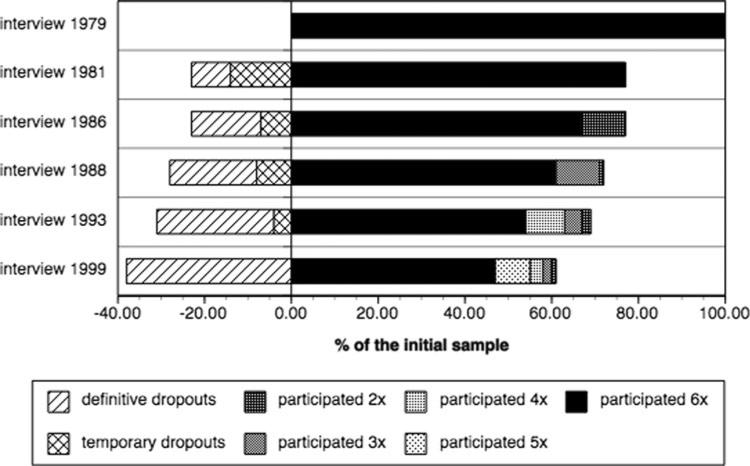
Face-to-face interviews were conducted with the interview sample at ages 21, 23, 28, 30, 35, and 41 years. Over 20 years, 62% of the original sample continued to participate in the study, and the following proportions participated in specific numbers of interviews: 47% in all six interviews; 63% in five interviews; 74% in four interviews; 82% in three interviews; and 91% in at least two interviews. On average, about 10% of the participants dropped out in each interview wave (Fig. 1).Those who dropped out did not differ significantly from those who stayed in follow-up interviews regarding psychiatrically relevant demographic characteristics [14]. The analyses reported below are based on 372 “stayers”—participants who completed five or all six interviews (Fig. 2).
Fig. 1.
The Zurich study: sample size over six interview waves
Fig. 2.
The Zurich study: percentage of participants and dropouts over six interview waves
Study instruments
The detailed interviews in the Zurich study were conducted with the SPIKE (Structured Psychopathological Interview and Rating of the Social Consequences of Psychological Disturbances for Epidemiology)—a semi-structured psychopathological interview developed for epidemiological studies which has been used in all waves since 1979 [3]. The successive SPIKE versions have allowed us to make diagnoses according to DSM III, IIIR, and IV with the exception that diagnoses of psychotic disorders could not be confirmed as the necessary criteria were not included [4]. SPIKE also recorded data concerning treatment, medication, service use, and impairment in work, social, and leisure activities.
However, in this study we used only data from the SCL90-R, which is one of the additional instruments applied in all interviews. In the SCL90-R, subjects respond on a five-point Likert scale of distress ranging from “not at all” (1) at one pole, to “a little bit” (2), “moderately” (3), “quite a bit” (4), and “extremely” (5), at the other. The time period covered by the SCL90-R in the Zurich study was 4 weeks. The 90 items of the SCL90-R are grouped along nine subscales (in the technical parts of the text the dimensions are labeled as subscales), reflecting a broad symptom status in a spectrum of individuals ranging from well controls, to somatic and psychiatric patients. The two SCL-subscales relevant for psychosis (“paranoid ideation” and “psychoticism”) were used for analysis. According to the SCL90-R manual [10], the six-item subscale “paranoid ideation” is characterized by projective thoughts, hostility, suspiciousness, grandiosity, centrality, fear of loss of autonomy, and delusions. The subscale “psychoticism” (10 items) includes items indicative of a withdrawn, isolated, schizoid lifestyle, as well as items representing symptoms of psychosis and schizophrenia such as hallucinations and thought broadcasting. The SCL-90-R depression symptoms subscale includes 13 items representing depressive moods, feelings of sadness, loneliness, suicidal thoughts, reduced (sexual) interest, weakness, weariness, hopelessness, low self-esteem, and finally, loss of energy.
The SCL90-R has shown good internal consistency and test–retest reliability [11, 12, 15, 35]. However, the factor structure of the instrument has shown inconsistent results. Commonly, less than nine factors are identified [35], and the psychoticism subscale has been shown to yield the least consistent results [32]. Such inconsistencies have been reported since the very first stages of development of SCL90-R [11].
These inconsistencies led us to challenge the paranoia and psychoticism subscales of the SCL-90-R and to develop two new subscales owing to preliminary factor analyses [34]. The first newly identified schizotypal symptoms subscale matches the original paranoid ideation subscale, additionally including the items “feeling lonely even when with people”, and “never feeling close to another person”. The second newly identified schizophrenia nuclear symptoms subscale includes the items thought insertion, thought broadcasting, thought control, and hearing voices from the original psychoticism subscale (Table 1).
Table 1.
Items of new subscales (schizophrenia nuclear symptoms subscale and schizotypal symptoms subscale) replacing the paranoia and psychoticism subscales of the SCL-90-R
| SCL-90-R item | Original SCL-90-R subscalea |
|---|---|
| Schizophrenia nuclear symptoms subscale | |
| 7: Someone else can control your thoughts | PS |
| 16: Hearing voices other people do not hear | PS |
| 35: Other being aware of your thoughts | PS |
| 62: Having thoughts that are not your own | PS |
| Schizotypal symptoms subscale | |
| 8: Others are to blame for your troubles | PN |
| 18: Feeling most people cannot be trusted | PN |
| 43: Feeling you are watched by others | PN |
| 68: Having ideas, others do not share | PN |
| 76: Others not giving you proper credit | PN |
| 77: Feeling lonely even when with people | PS |
| 83: Feeling people take advantage of you | PN |
| 88: Never feeling close to another person | PS |
PS psychoticism, PN paranoia
Excluded items (all pertaining to the original psychoticism subscale): 84 Thoughts about sex that bother you a lot, 85 Idea you should be punished for sins, 87 Idea something is wrong with body, 90 Idea something is wrong with your mind
Statistical modeling
We used latent growth models (LGMs) [9, 25, 37] to analyze simultaneously the two distinct psychosis subscales and the depression symptoms subscale. Thus, the analyses are based on 3*6 data points.
The LGM framework in longitudinal data analysis allows for modeling in parallel all three longitudinal variables representing the subscales. In addition, we included synchronous and time-lagged regression effects between the longitudinal variables. The respective path analysis submodels were expected to disentangle in particular the reciprocal effects between the two psychosis subscales on the one hand, and the depression symptoms subscale, on the other. Thus, the two model parts—the latent growth model and the path analysis submodels—created a hybrid model, which came close to the more general autoregressive latent trajectories model proposed by Bollen and Curran [8, 9].
The modeling procedure, which included several steps as usual in structural equation modeling, is described in the Appendix (see electronic supplementary material). The model fit was assessed using the following fit indices (values in the parentheses follow the suggestions by Yu [44]): chi-square (P < 0.01), TLI (>0.95), CFI (>0.96), SRMR (<0.07), RMSEA (<0.06). In addition, we looked at the AIC and the BIC. The analyses were carried out with the Mplus 4.21 software [30]. The missing values were replaced by the missing value procedure implemented in Mplus, which assumes missing at random (MAR) data.
Results
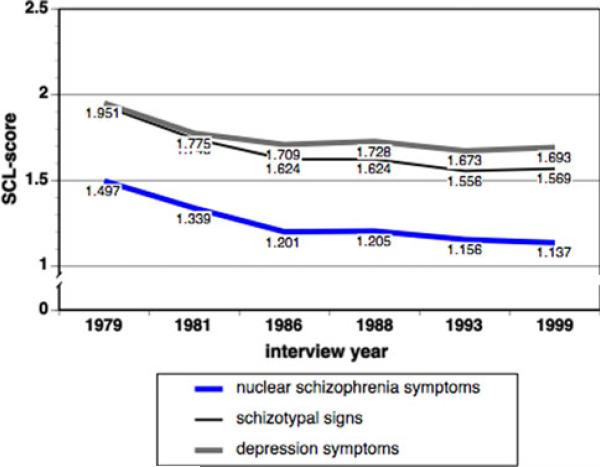
The overall trajectories of the schizophrenia nuclear symptoms subscale, the schizotypal symptoms subscale, and the depression subscale of the SCL-90-R over 20 years are shown in Fig. 3. The curves start at age of 20/21 in 1979 and end at age 40/41 in 1999. In all three trajectories, there is an immediate decline of the scores. The mean and standard deviation are shown in Fig. 3.
Fig. 3.
Course of the schizophrenia nuclear symptoms subscale, the schizotypal symptoms subscale and the depression subscale of the SCL-90-R in the Zurich Study, 1979–1999, i.e., ages 20/21 through 40/41. Note: The standard deviations are 0.54, 0.48, 0.34, 0.36, 0.33, 0.29 (schizophrenia nuclear symptoms subscale); 0.69, 0.63, 0.58, 0.55, 0.56, 0.57 (schizotypal symptoms subscale); 0.71, 0.65, 0.65, 0.62, 0.65, 0.64 (depression subscale)
The correlations in each interview between the schizophrenia nuclear symptoms subscale, the schizotypal symptoms subscale, and the depression subscale of the SCL-90-R provide a preliminary impression of their interrelations. They are shown in Table 2. All correlations are consistently high. However, the correlations between the schizotypal symptoms and the depression symptoms subscale are distinctly higher than any correlation including schizophrenia nuclear symptoms. The results of separate analyses for men and women were perfectly congruent (results not shown).
Table 2.
Correlations between the schizophrenia nuclear symptoms subscale, the schizotypal symptoms subscale, and the depression subscale of the SCL-90-R, by interview
| Interview | Nuclear/depression | Schizotypal/depression | Nuclear/schizotypal |
|---|---|---|---|
| 1979 | 0.50 | 0.77 | 0.53 |
| 1981 | 0.53 | 0.77 | 0.59 |
| 1986 | 0.48 | 0.77 | 0.50 |
| 1988 | 0.49 | 0.76 | 0.49 |
| 1993 | 0.45 | 0.75 | 0.50 |
| 1999 | 0.42 | 0.76 | 0.47 |
All correlations: P < 0.001
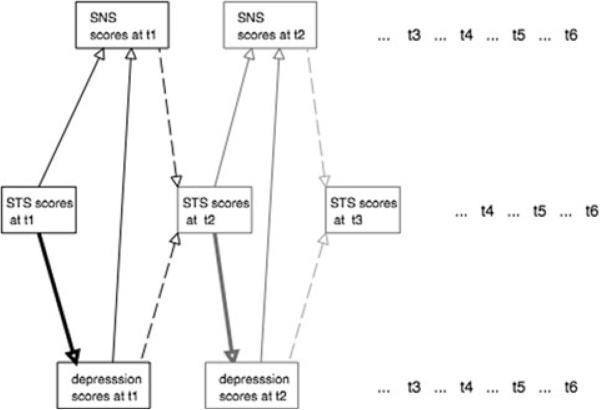
The Appendix informs about the results from the subsequent modeling steps in longitudinal data analysis. In a first intermediate step, we determined a basic trivariate growth model with all three subscales. This model comprised standardized covariances between the latent variables (representing the initial status and rate of change of each subscale), and secondly, standardized covariances between the simultaneous variable scores of each subscale (see model 1 in the Table A1 from the Appendix of the supplementary material). Subsequently, we replaced the standardized covariances one by one by directed paths. Model 4 (see Table A1 in the Appendix of the supplementary material) had distinctly the best fit when one out of three possible directed paths between the simultaneous variable scores was introduced. In this model, depression scores predict the SNS scores (but not vice versa). Based on this model, we exchanged also the other standardized covariances between the simultaneous variable scores with directed paths. The best model was model 8 (see Table A1 from the Appendix of the supplementary material) including the following unidirectional effects:
moderate effect of the depression subscale on the schizophrenia nuclear symptoms subscale
moderate effect of the schizotypal symptoms subscale on the schizophrenia nuclear symptoms subscale
strong effect of the schizotypal symptoms subscale on the depression subscale.
The fit of model 8 is comparable to the fit of model 4; however, model 8 contains distinctly more substantial information due to the directed paths.
In a final step, we introduced tentatively additional cross-lagged effects (for example, depression scores at time t + 1 regressed on schizotypal symptoms subscale (schizophrenia nuclear symptoms) scores at time t). The cross-lagged effects on the schizotypal symptoms subscale—either deriving from the schizophrenia nuclear symptoms subscale, or the depression subscale—improved the model fit moderately. This final model is shown in Fig. 4, the corresponding estimates are reported in Table 3. The fit indices were chi-square = 159.6 (df 116), CFI = 0.989, TLI = 0.985, AIC = 5663.7, BIC = 5949.8, RMSEA = 0.032, SRMR = 0.051.
Fig. 4.
Effects in the path model part of the hybrid latent growth model (see Table 3)
Table 3.
The path model part of the hybrid latent growth model: standardized coefficients over 6 interviews in the Zurich study; “on” represents regression relationships (e.g., schizophrenia nuclear symptoms regressed on depression)
| Effects in the model | Interviews |
|||||
|---|---|---|---|---|---|---|
| At t1 1979 | At t2 1981 | At t3 1986 | At t4 1988 | At t5 1993 | At t6 1999 | |
| SNS on STS | 0.39** | 0.42*** | 0.25*** | 0.23*** | 0.28*** | 0.32*** |
| SNS on DEP | 0.30** | 0.18* | 0.22*** | 0.23*** | 0.21*** | 0.15* |
| DEP on STS | 0.73*** | 0.70*** | 0.69*** | 0.68*** | 0.69*** | 0.72*** |
| STS on lag(SNS) | 0.04 | 0.13* | 0.09* | 0.01 | 0.11* | |
| STS on lag(DEP) | 0.06 | 0.12* | 0.15** | 0.18** | 0.07 | |
SNS Schizophrenia nuclear symptoms subscale, STS Schizotypal symptoms subscale, DEP Depression subscale; all subscales were derived from the SCL-90-R
P < 0.05
P < 0.01
P < 0.001
To summarize, the main driving force within the dynamics between symptoms of psychosis and depression is the schizotypal symptoms subscale, which represents social and interpersonal deficiencies, ideas of reference, suspiciousness, paranoid ideation, and finally, odd behavior. It exercises a strong effect on the depression symptoms, and a moderate effect on the schizophrenia nuclear symptoms subscale. Depression has partly a mediator function in this dynamics.
Discussion
This study examined the dynamics of two distinct psychosis symptoms dimensions as previously derived by means of factor analyses from the SCL 90-R [34], and one depression symptoms dimension represented by items as provided by the SCL 90-R manual in a population-based cohort. Two syndromes represented the psychosis symptoms, the first, which we called the nuclear schizophrenia symptoms dimension, and the second, which was called the schizotypal symptoms dimension. The schizophrenia nuclear symptoms (thought insertion, thought broadcasting, thought control, and hearing voices) correspond to the Schneiderian first rank symptoms. The second dimension addresses social and interpersonal deficiencies (“feeling lonely even when with people”), with reduced capacity for close relationships (“never feeling close to another person”), as well as ideas of reference (“feeling watched by others”), odd beliefs (“having ideas that others do not share”), suspiciousness (“other people cannot be trusted”), or paranoid ideation (“others are to blame for your troubles”, “persons are taking advantage of you”). As such, this dimension is reminiscent of the criteria required for the diagnosis of a “schizotypal personality disorder”. The symptoms of our second dimension schizotypal symptoms also correspond to the positive and negative schizotypal factors, which were identified by Vollema & Hoijtink [43] in a three-factor model of schizotypy. Finally, the depression dimension was calculated according to the SCL-90-R manual [10]. It includes 13 common symptoms representing depressive mood, feelings of sadness, loneliness, suicidal thoughts, reduced (sexual) interest, weakness, weariness, hopelessness, low self-esteem, and loss of energy.
At first glance, the correlations of all three symptom dimensions are consistently high over time, but even more elevated are the correlations between the schizotypal symptoms, and the depression symptoms. The directions of the relations and their temporal order emerged in hybrid latent growth models.
The latent growth models allowed us to examine the longitudinal data from all three symptom dimensions “in parallel”. Our models indicated that as regards schizotypal symptoms, neither the depression symptoms nor the nuclear symptoms are the main driving force within the complex triangular relations. The schizotypal symptoms do not only directly impact on the nuclear symptoms but clearly also on depression symptoms. There is also a reverse impact, i.e., from the nuclear schizophrenia symptom dimension, and from the depression symptom dimension, on the schizotypal symptoms, but considerably weaker in strength. Finally, there is also a moderate impact of the depression syndrome on the nuclear schizophrenia syndrome. The crucial role of the schizotypal symptoms challenges our understanding of how subclinical psychosis and depression symptoms both emerge and interact. Thus, depression is not simply a precursor of subclinical psychosis but is mainly a mediator of schizotypal symptoms, which precede these subclinical nuclear symptoms.
Disentangling the hybrid latent growth model
The “latent growth” part of the hybrid model accounted for the longitudinal effects in the data. All three syndromes showed a decline over time, which is due to the regression to the mean, i.e., a statistical phenomenon. But the decline might also express the natural course of these symptom dimensions as in particular in schizophrenia, there is a similar decline with the highest rates in young adulthood. The other part of the hybrid model, which involves path analysis, comprised simultaneous and lagged paths. These effects were selected after comparison of alternative models at each step of the analysis.
It is noteworthy that the path analytic model tells us that the impact of the schizotypal symptoms on schizophrenia nuclear symptoms includes two pathways, a direct one and an indirect one via depressive symptoms. The direct (and in our study, weaker) pathway from schizotypal symptoms to schizophrenia nuclear symptoms reflects the same pathway as from schizotypy to schizophrenia. On a subclinical level, the pathway identified in this study supports the hypothesis of Raine [33] that there might be a form of schizotypy with a more pronounced psychosocial etiology, and more symptom fluctuation. Our dimension “schizotypal symptoms” is highly variable in the symptom course over time and shows a strong link to childhood adversity as a risk factor [34].
The link with depression symptoms
The other challenge emerging from this study concerns the link with depression. Numerous studies have documented the association between depression and psychotic symptoms. Our model suggests that the major part of the associations with schizophrenia nuclear symptoms is introduced by shared variance due to the impact of the schizotypal symptoms. There is only a minor direct effect of the depression symptom dimension on the nuclear symptoms. Thus, some hypotheses and theories in this direction possibly need to be re-examined. For example, our results do not strongly support the empirical findings and further hypotheses of Häfner and colleagues [17, 27] that due to a low threshold, depressive symptoms are widespread in the population and independent of frank psychosis with a significant higher threshold. Our findings propose suggest strongly that schizotypal symptoms preferably convey depression symptoms, which for their part can convey schizophrenia nuclear symptoms. A congruent view was proposed by Kirkpatrick and colleagues [21, 29]. They found that suspiciousness, which is an acknowledged symptom of schizotypy, is a risk factor for major depression in schizophrenia.
Thus, not only the mechanisms endorsing psychosis symptoms need a closer look, but also the depression symptoms themselves are deserving of closer scrutiny. Our models confirmed that the effect of the schizotypal symptoms on depression is much more relevant than it is on the reciprocal effect. Schizotypal symptoms even appear to be a major force influencing depression. The strong impact of schizotypal symptoms on depression might be also interpreted as a depressive reaction to the experience of being excluded and lonely, as many persons suffering from schizotypal symptoms describe it.
To summarize, schizotypy, depression, and schizophrenia nuclear symptoms—the latter ones being assumed to build the core of schizophrenia—interact on a subclinical level, paving the pathway to clinical psychosis. The model presented in this study improves our understanding of the dynamics in the development of psychosis on a subthreshold level. Many well-known findings may be integrated in this model, thus leading to new perspectives.
Limitations
Despite its strengths, our study also has its limitations. This study entailed only a part of the syndromes representing psychosis, namely positive (nuclear) symptoms. Negative symptoms, such as disorganization, and putative other dimensions of psychosis are not covered by the SCL-90-R or other data in the Zurich study. There is no corresponding psychosis section in the SPIKE questionnaire, which might serve to control or supplement the information derived from the SCL-90-R. The SCL-90-R also underestimates the prevalence of symptoms, which is commonly described by a 12-month period. The symptoms assessed by the SCL-90-R in the Zurich study only cover the last 4 weeks. From a methodological point of view, one should be aware that the time periods between the interviews of the Zurich study are up to 5 years. Thus, our analysis could assess only partially the dynamics between the syndromes. Shorter time periods between the interviews doubtless would provide stronger lagged effects. And finally the models represent a dimension-guided approach to the data. Thus, the results would be valid for the most frequent or most typical patterns. Nevertheless, there are many cases not compatible with the typical patterns: for instance, persons with high levels on only one of the dimensions, or persons with a reversed development, i.e., for example who developed nuclear symptoms first, and only later, schizotypal symptoms. Cluster analysis within a subgroup-guided approach [5, 40] remains to be conducted as a next step in order to describe not only the most typical patterns but also subgroups with less frequent patterns.
Supplementary Material
Acknowledgments
The study was supported by the Swiss National Science Foundation (grant # 32-50881.97).
Footnotes
Electronic supplementary material The online version of this article (doi:10.1007/s00406-010-0123-0) contains supplementary material, which is available to authorized users.
Contributor Information
Wulf Rössler, Department of General and Social Psychiatry, Psychiatric University Hospital, University of Zurich, Militärstrasse 8, 8021 Zurich, Switzerland roessler@dgsp.uzh.ch; Collegium Helveticum, University of Zurich and Swiss Federal Institute of Technology, Zurich, Switzerland.
Jules Angst, Department of General and Social Psychiatry, Psychiatric University Hospital, University of Zurich, Militärstrasse 8, 8021 Zurich, Switzerland.
Alex Gamma, Department of General and Social Psychiatry, Psychiatric University Hospital, University of Zurich, Militärstrasse 8, 8021 Zurich, Switzerland.
Helene Haker, Department of General and Social Psychiatry, Psychiatric University Hospital, University of Zurich, Militärstrasse 8, 8021 Zurich, Switzerland.
Niklaus Stulz, Department of General and Social Psychiatry, Psychiatric University Hospital, University of Zurich, Militärstrasse 8, 8021 Zurich, Switzerland.
Kathleen R. Merikangas, Department of Health and Human Services, National Institute of Mental Health, National Institutes of Health, Bethesda, MD, USA
Vladeta Ajdacic-Gross, Department of General and Social Psychiatry, Psychiatric University Hospital, University of Zurich, Militärstrasse 8, 8021 Zurich, Switzerland.
References
- 1.American Psychiatric Association . Diagnostic and statistical manual of mental disorders. American Psychiatric Association; Washington, DC: 1994. edn. [Google Scholar]
- 2.Angst J, Cassano G. The mood spectrum: improving the diagnosis of bipolar disorder. Bipolar Disord. 2005;7(Suppl 4):4–12. doi: 10.1111/j.1399-5618.2005.00210.x. [DOI] [PubMed] [Google Scholar]
- 3.Angst J, Dobler-Mikola A, Binder J. The Zurich study—a prospective epidemiological study of depressive, neurotic and psychosomatic syndromes. I. Problem, methodology. Eur Arch Psychiatry Neurol Sci. 1984;234:13–20. doi: 10.1007/BF00432878. [DOI] [PubMed] [Google Scholar]
- 4.Angst J, Gamma A, Neuenschwander M, Ajdacic-Gross V, Eich D, Rossler W, Merikangas KR. Prevalence of mental disorders in the Zurich cohort study: a twenty year prospective study. Epidemiol Psichiatr Soc. 2005;14:68–76. doi: 10.1017/s1121189x00006278. [DOI] [PubMed] [Google Scholar]
- 5.Bak M, Krabbendam L, Janssen I, de Graaf R, Vollebergh W, van Os J. Early trauma may increase the risk for psychotic experiences by impacting on emotional response and perception of control. Acta Psychiatr Scand. 2005;112:360–366. doi: 10.1111/j.1600-0447.2005.00646.x. [DOI] [PubMed] [Google Scholar]
- 6.Bedwell JS, Donnelly RS. Schizotypal personality disorder or prodromal symptoms of schizophrenia? Schizophr Res. 2005;80:263–269. doi: 10.1016/j.schres.2005.07.023. [DOI] [PubMed] [Google Scholar]
- 7.Bleuler E. Dementia praecox oder die Gruppe der Schizophrenien. Denticke; Leipzig: 1911. [DOI] [PubMed] [Google Scholar]
- 8.Bollen KA, Curran PJ. Autoregressive latent trajectory (ALT) models: a synthesis of two traditions. Sociol Methods Res. 2004;32:336–383. [Google Scholar]
- 9.Bollen KA, Curran PJ. A structural equation perspective. Wiley; Hoboken: 2006. Latent curve models. [Google Scholar]
- 10.Derogatis LR. SCL-90. Administration, scoring and procedures manual-1 for the R (revised) version and other instruments of the psychopathology rating scale series. Chigaco: 1977. [Google Scholar]
- 11.Derogatis LR, Cleary PA. Confirmation of the dimensional structure of the SCL-90: a study in construct validity. J Clin Psychol. 1977;33:981–989. [Google Scholar]
- 12.Derogatis LR, Melisaratos N. The brief symptom inventory: an introductory report. Psychol Med. 1983;13:595–605. [PubMed] [Google Scholar]
- 13.Dunn G, Pickles A, Tansella M, Vazquez-Barquero JL. Two-phase epidemiological surveys in psychiatric research. Br J Psychiatry. 1999;174:95–100. doi: 10.1192/bjp.174.2.95. [DOI] [PubMed] [Google Scholar]
- 14.Eich D, Ajdacic-Gross V, Condrau M, Huber H, Gamma A, Angst J, Rossler W. The Zurich study: participation patterns and symptom checklist 90-R scores in six interviews, 1979–1999. Acta Psychiatr Scand. 2003;108(Suppl 418):11–14. doi: 10.1034/j.1600-0447.108.s418.3.x. [DOI] [PubMed] [Google Scholar]
- 15.Hafkenscheid A. Psychometric evaluation of the symptom checklist (SCL-90) in psychiatric patients. Pers Individ Dif. 1993;14:751–756. [Google Scholar]
- 16.Hafner H, Ander Heiden W, Maurer K. Evidence for separate diseases? Stages of one disease or different combinations of symptom dimensions? Eur Arch Psychiatry Clin Neurosci. 2008;258(Suppl 2):85–96. doi: 10.1007/s00406-008-2011-4. [DOI] [PubMed] [Google Scholar]
- 17.Hafner H, Maurer K, Trendler G, an der Heiden W, Schmidt M, Konnecke R. Schizophrenia and depression: challenging the paradigm of two separate diseases–a controlled study of schizophrenia, depression and healthy controls. Schizophr Res. 2005;77:11–24. doi: 10.1016/j.schres.2005.01.004. [DOI] [PubMed] [Google Scholar]
- 18.Hanssen M, Bak M, Bijl R, Vollebergh W, van Os J. The incidence and outcome of subclinical psychotic experiences in the general population. Br J Clin Psychol. 2005;44:181–191. doi: 10.1348/014466505X29611. [DOI] [PubMed] [Google Scholar]
- 19.Horan WP, Blanchard JJ, Clark LA, Green MF. Affective traits in schizophrenia and schizotypy. Schizophr Bull. 2008;34:856–874. doi: 10.1093/schbul/sbn083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Johns LC, Cannon M, Singleton N, Murray RM, Farrell M, Brugha T, Bebbington P, Jenkins R, Meltzer H. Prevalence and correlates of self-reported psychotic symptoms in the British population. Br J Psychiatry. 2004;185:298–305. doi: 10.1192/bjp.185.4.298. [DOI] [PubMed] [Google Scholar]
- 21.Kirkpatrick B, Amador XF, Yale SA, Bustillo JR, Buchanan RW, Tohen M. The deficit syndrome in the DSM-IV field trial. Part II. Depressive episodes and persecutory belief. Schizophr Res. 1996;20:79–90. doi: 10.1016/0920-9964(95)00101-8. [DOI] [PubMed] [Google Scholar]
- 22.Krabbendam L, Myin-Germeys I, Hanssen M, de Graaf R, Vollebergh W, Bak M, van Os J. Development of depressed mood predicts onset of psychotic disorder in individuals who report hallucinatory experiences. Br J Clin Psychol. 2005;44:113–125. doi: 10.1348/014466504X19767. [DOI] [PubMed] [Google Scholar]
- 23.Krabbendam L, van Os J. Affective processes in the onset and persistence of psychosis. Eur Arch Psychiatry Clin Neurosci. 2005;255:185–189. doi: 10.1007/s00406-005-0586-6. [DOI] [PubMed] [Google Scholar]
- 24.Kraepelin E. Psychiatrie: Ein Lehrbuch für Studierende undÄrzte. Verlag J. A. Barth; Leipzig: 1896. [Google Scholar]
- 25.MacCallum RC, Kim C, Malarkey WB, Kiecolt-Glaser JK. Studying multivariate change using multilevel models and latent curve models. Multivariate Behav Res. 1997;32:215–253. doi: 10.1207/s15327906mbr3203_1. [DOI] [PubMed] [Google Scholar]
- 26.Marneros A, Deister A, Rohde A, Junemann H, Fimmers R. Long-term course of schizoaffective disorders. Part I: Definitions, methods, frequency of episodes and cycles. Eur Arch Psychiatry Neurol Sci. 1988;237:264–275. doi: 10.1007/BF00450545. [DOI] [PubMed] [Google Scholar]
- 27.Maurer K, Trendler G, Schmidt M, An der Heiden W, Konnecke R, Hafner H. Schizophrenia and depression. Nervenarzt. 2006;77:809–822. doi: 10.1007/s00115-005-1920-y. [DOI] [PubMed] [Google Scholar]
- 28.Merikangas KR, Zhang H, Avenevoli S, Acharyya S, Neuenschwander M, Angst J. Longitudinal trajectories of depression and anxiety in a prospective community study: the Zurich cohort study. Arch Gen Psychiatry. 2003;60:993–1000. doi: 10.1001/archpsyc.60.9.993. [DOI] [PubMed] [Google Scholar]
- 29.Messias E, Kirkpatrick B, Ram R, Tien AY. Suspiciousness as a specific risk factor for major depressive episodes in schizophrenia. Schizophr Res. 2001;47:159–165. doi: 10.1016/s0920-9964(00)00030-x. [DOI] [PubMed] [Google Scholar]
- 30.Muthén LK, Muthén BO. Mplus user's guide. 4th edn. Muthén & Muthén; Los Angeles, CA: 1998–2006. [Google Scholar]
- 31.Myin-Germeys I, Spauwen J, Jacobs N, Lieb R, Wittchen HU, van Os J. The aetiological continuum of psychosis. In: Gattaz WF, Häfner H, editors. Search for the causes of schizophrenia. Vol. 5. Steinkopff; Darmstadt: 2004. pp. 342–366. [Google Scholar]
- 32.Olsen LR, Mortensen EL, Bech P. The SCL-90 and SCL-90R versions validated by item response models in a Danish community sample. Acta Psychiatr Scand. 2004;110:225–229. doi: 10.1111/j.1600-0447.2004.00399.x. [DOI] [PubMed] [Google Scholar]
- 33.Raine A. Schizotypal personality: neuro developmental and psychosocial trajectories. Annu Rev Clin Psychol. 2006;2:291–326. doi: 10.1146/annurev.clinpsy.2.022305.095318. [DOI] [PubMed] [Google Scholar]
- 34.Rössler W, Riecher-Rössler A, Angst J, Murray R, Gamma A, Eich D, van Os J, Ajdacic-Gross V. Psychotic experiences in the general population: a twenty-year prospective community study. Schizophr Res. 2007;92:1–14. doi: 10.1016/j.schres.2007.01.002. [DOI] [PubMed] [Google Scholar]
- 35.Schmitz N, Hartkamp N, Franke GH. Assessing clinically significant change: application to the SCL-90-R. Psychol Rep. 2000;86:263–274. doi: 10.2466/pr0.2000.86.1.263. [DOI] [PubMed] [Google Scholar]
- 36.Seeber K, Cadenhead KS. How does studying schizotypal personality disorder inform us about the prodrome of schizophrenia? Curr Psychiatry Rep. 2005;7:41–50. doi: 10.1007/s11920-005-0024-5. [DOI] [PubMed] [Google Scholar]
- 37.Singer JD, Willett JB. Applied longitudinal data analysis. Oxford University Press; New York: 2003. [Google Scholar]
- 38.Siris SG, Bench C. In: Depression and schizophrenia. Schizophrenia. 2nd edn. Hirsch SR, Weinberger DR, editors. Blackwell Publishing; Oxford: 2003. pp. 142–167. [Google Scholar]
- 39.Spauwen J, Krabbendam L, Lieb R, Wittchen HU, van Os J. Sex differences in psychosis: normal or pathological? Schizophr Res. 2003;62:45–49. doi: 10.1016/s0920-9964(03)00063-x. [DOI] [PubMed] [Google Scholar]
- 40.Suhr JA, Spitznagel MB. Factor versus cluster models of schizotypal traits. I: a comparison of unselected and highly schizotypal samples. Schizophr Res. 2001;52:231–239. doi: 10.1016/s0920-9964(00)00170-5. [DOI] [PubMed] [Google Scholar]
- 41.Tsuang MT, Stone WS, Tarbox SI, Faraone SV. An integration of schizophrenia with schizotypy: identification of schizotaxia and implications for research on treatment and prevention. Schizophr Res. 2002;54:169–175. doi: 10.1016/s0920-9964(01)00364-4. [DOI] [PubMed] [Google Scholar]
- 42.van Os J, Hanssen M, Bijl RV, Ravelli A. Strauss (1969) revisited: a psychosis continuum in the general population? Schizophr Res. 2000;45:11–20. doi: 10.1016/s0920-9964(99)00224-8. [DOI] [PubMed] [Google Scholar]
- 43.Vollema MG, Hoijtink H. The multidimensionality of self-report schizotypy in a psychiatric population: an analysis using multidimensional Rasch models. Schizophr Bull. 2000;26:565–575. doi: 10.1093/oxfordjournals.schbul.a033478. [DOI] [PubMed] [Google Scholar]
- 44.Yu CY. Evaluating cutoff criteria of model fit I indices for latent variable models with binary and continuous outcomes. University of California; Los Angeles: 2002. [Google Scholar]
- 45.Yung AR, Buckby JA, Cotton SM, Cosgrave EM, Killackey EJ, Stanford C, Godfrey K, McGorry PD. Psychotic-like experiences in nonpsychotic help-seekers: associations with distress, depression, and disability. Schizophr Bull. 2006;32:352–359. doi: 10.1093/schbul/sbj018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Yung AR, McGorry PD. The prodromal phase of first-episode psychosis: past and current conceptualizations. Schizophr Bull. 1996;22:353–370. doi: 10.1093/schbul/22.2.353. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.