Abstract
Objective
Experts recommend that clinicians tailor their interactions according to each patient's preferred decision style. Because participation is associated with improved clinical outcomes, factors which modify preferred role should be addressed before determining the level at which patients wish to participate. The objective of this study was to determine if certainty related to initiating treatment is related to preferred role in decision making.
Methods
We conducted face-to-face interviews with 142 patients eligible for treatment of hepatitis C. Preferred role in decision making was measured using the Control Preferences Scale and certainty was measured with 11-point numeric rating scale.
Results
Subjects who were uncertain whether they wanted to start treatment were more likely to prefer Role 2: “to make the final selection of my treatment after seriously considering my doctor's opinion” over Role 1 “to make the final selection about which treatment I will receive” compared to those who were certain [Adjusted OR (95% CI) = 4.9 (1.7-14.5)]. Subjects who were uncertain were also more likely to prefer sharing responsibility for decision making over Role 1 compared to those who were certain [Adjusted OR (95% CI) = 3.7 (1.3-10.4)].
Conclusions
Certainty is associated with preferred decision styles. Physicians should ascertain their patients’ levels of uncertainty and adjust their input accordingly.
Practice Implication
Physicians should ascertain their patients’ levels of uncertainty and adjust their input accordingly.
Keywords: Decision Making, Patient Participation
1. Introduction
Several studies have demonstrated that patients’ preferred role in decision making varies with some patients preferring to take on an active role in making decisions related to their healthcare and others preferring to remain more passive (1). Consequently, experts recommend that clinicians determine each patient's preferred decision style and tailor their interactions accordingly (1-3).
Ideally, because participation is associated with improved satisfaction and clinical outcomes (e.g. hemoglobin A1c levels, disease activity in lupus, and severity of depression) (4-8), factors which modify patients’ preferred role should be addressed before physicians determine the level at which their patients wish to participate. Studies examining predictors of patients’ preferred role have largely focused on fixed variables (1). Mansell et al (3) found that patients’ perceived seriousness of the decision was associated with an increased desire to participate. Several studies have found that sicker patients prefer more passive roles (2, 9, 10). While older age is associated with preference for a more passive role, other demographic factors, including gender, education and race do not consistently predict patients’ role preferences (1, 2, 11-13).
A recent qualitative study suggested that role preference is variable and is related to how strongly patients feel about specific treatment options or diagnostic procedures (14). These results suggest that patient's preferred role in decision making may be related to their choice predisposition, or level of certainty regarding their desire to initiate or avoid therapy. Based on these findings, we sought to determine if patients’ level of certainty, a potentially modifiable factor, is related to their preferred role in decision making as measured by the Control Preferences Scale (15).
2. Methods
Subjects were interviewed as part of larger study examining patient preferences for treatment of hepatitis C (HCV). The decision to initiate therapy for HCV is difficult because, although HCV is effective at reducing progression to cirrhosis and the development of complications related to cirrhosis, many patients do not derive any benefit from treatment because of the variability in the progression of the disease (16). Moreover, the medications used can cause potentially serious adverse effects. We recruited consecutive patients eligible for treatment of HCV from outpatient liver clinics. Eligibility criteria included chronic HCV, no prior treatment for HCV, known genotype, and liver biopsy within the preceding two years or clinical evidence of cirrhosis. Eligible patients either signed informed consent at their biopsy visit, or when they arrived for their study visit, which was held on the same day as their follow-up appointment with their hepatologist. Subjects who did not have a scheduled liver biopsy were invited to participate by clinic staff, and consented by the research nurse on the day of their study visit. The protocol was approved by our institution's Human Investigations Committee.
2.1 Data Collection
Data were collected on the day subjects were scheduled to talk to their physician about treatment for HCV. Because the degree of liver damage is associated with the probability of benefiting from therapy, patients were informed of their liver biopsy results before completing the survey. As part of the survey patients marked their degree of certainty about treatment on an 11-point numeric rating scale (17):
Right now, how do you feel about possibly starting treatment for hepatitis C?
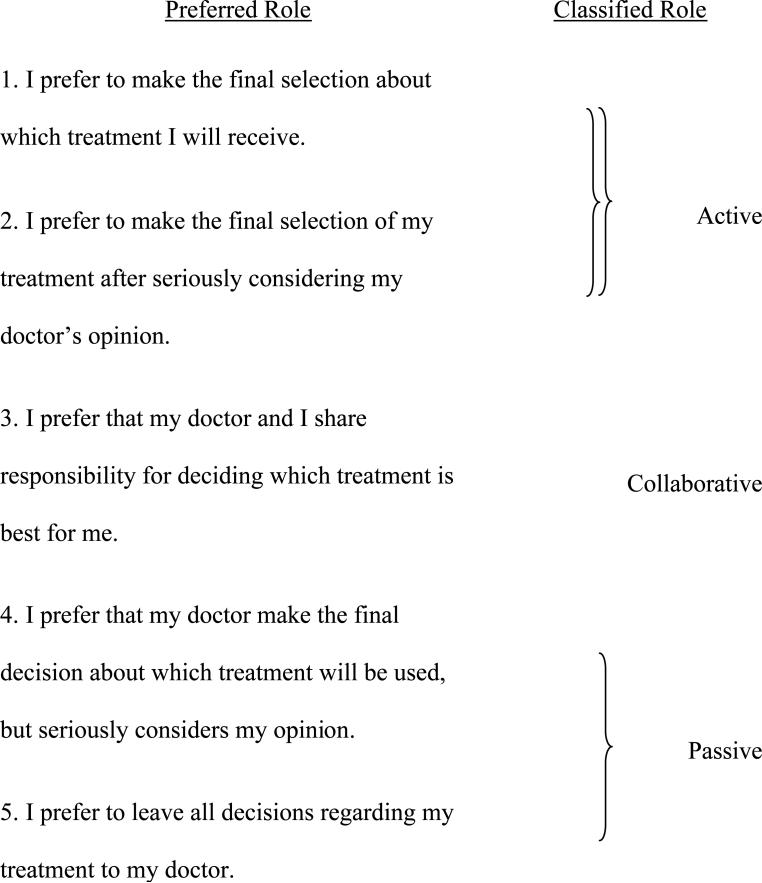
This item has a test-retest Pearson correlation coefficient greater than 0.90 (17). Participants choosing 0-1 or 9-10 were classified as certain and the remaining were classified as uncertain. Preferred role in decision making was measured by the widely used Control Preferences Scale which classifies patients as preferring an active, collaborative or passive role in decision making (see Appendix) (15). Patients choosing #1 or #2 are classified as preferring an active role, those choosing #3 a collaborative role, and #4 or #5 a passive role in medical decision-making (15).
2.2 Analyses
We examined the association between certainty and preferred role in decision making (referred to as Roles 1 through 5 throughout the manuscript) using the chi-square test and subsequently performed subgroup analyses to further define this relationship. Self-reported race, maximum level of education obtained (classified as high school graduate or less versus at least some college education), gender, age, genotype, overall self-reported health status (classified as excellent or very good versus good, fair, or poor) disease severity (classified as moderate to severe hepatic fibrosis versus mild or no fibrosis on liver biopsy), and trust in physician (measured using the 11-item Trust in Physician's Scale) (18) were examined as possible covariates. Logistic regression was used to adjust for covariates found to be associated (p ≤ 0.1) with preferred role in decision making in bivariate analysis. Sample size calculations were not performed, as these were exploratory analyses.
3. Results
Of 212 eligible subjects, 178 agreed to participate of which 21 patients cancelled or did not come to their physician's appointment, five did not have the time to complete the task, and eight could not participate because of a scheduling error. One hundred forty two subjects with HCV were interviewed. The mean (± SD) age of the sample was 51 ± 8, 85% were male, 59% Caucasian, 45% had some college education, 31% reporting having fair or poor overall health status, 83% were genotype 1, and 58% had moderate or severe liver disease.
The proportion of subjects preferring each role is described in Table 1. Given the small numbers of subjects classified as preferring Roles 4 and 5, the remaining analyses were restricted to patients preferring Roles 1, 2 and 3 (N= 123). Fifty-seven (46%) subjects were certain about whether or not they wanted to be treated. Level of certainty was significantly associated with preferred role in decision making, p= 0.007 (Table 2). Self-reported race, education and gender, age, health status, genotype, and trust in physician were not associated with preferred role (all p > 0.2); however, the severity of liver disease was (p= 0.006).
Table 1.
Subjects’ Preferred Role in Decision Making
| Preferred Role | Number (%) |
|---|---|
| Total = 142 | |
| I prefer to make the final selection about which treatment I will receive. (Role 1) | 26 (18) |
| I prefer to make the final selection of my treatment after seriously considering my doctor's opinion. (Role 2) | 50 (35) |
| I prefer that my doctor and I share responsibility for deciding which treatment is best for me. (Role 3) | 47 (33) |
| I prefer that my doctor make the final decision about which treatment will be used, but seriously considers my opinion. (Role 4) | 9 (6) |
| I prefer to leave all decisions regarding my treatment to my doctor. (Role 5) | 10 (7) |
Table 2.
Association between Preferred Role in Decision Making and Certainty
| Preferred Role | Certain (N=57) | Uncertain (N=66) |
|---|---|---|
| I prefer to make the final selection about which treatment I will receive. (Role 1) | 33% | 11% |
| I prefer to make the final selection of my treatment after seriously considering my doctor's opinion. (Role 2) | 32% | 48% |
| I prefer that my doctor and I share responsibility for deciding which treatment is best for me. (Role 3) | 35% | 41% |
Subjects who were uncertain whether or not they wanted to receive treatment were more likely to prefer Role 2 over Role 1 compared to those who were certain (82% versus 49%, p=0.002). This association remained statistically significant after controlling for disease severity [Adjusted OR (95% CI) = 4.9 (1.7-14.5)]. Subjects who were uncertain whether or not they wanted to receive treatment were also more likely to prefer Role 3 over Role 1 compared to those who were certain [79% versus 51%, p =0.01; Adjusted OR (95% CI) = 3.7 (1.3-10.4)]. However, subjects who were uncertain whether or not they wanted to receive treatment were not more likely to prefer Role 2 over Role 3 compared to those who were certain (46% versus 53%, p =0.5).
4. Discussion and Conclusion
4.1 Discussion
Our results suggest that patients’ level of certainty is related to their desired role to participate in decision making. Subjects who are uncertain about their desire for treatment are more likely to prefer greater physician input whether it be in the form of a recommendation (as in Role 2) or collaboration (as in Role 3). In contrast, subjects who feel strongly about whether or not they want to be treated are more likely to prefer an autonomous role. The observation that subjects with more uncertainty are more likely to prefer Role 2 suggest that patients attach qualitatively different meanings to the statements used in Roles 1 and 2 and raise concerns related to the classification of the Control Preferences Scale (Appendix) which groups both together in a single category. It is possible that less certain patients prefer Role 2 because this is the only item that specifies obtaining a doctor's recommendation. This hypothesis requires confirmation in future studies.
The results of this study suggest that patients’ preferred roles in decision making reflect their need for additional information as opposed to their desire to participate in a process which is meant to lead to value concordant decisions. Thus, despite the important work performed by Deber et al (19) to distinguish the act of participating in decision making from problem solving, it appears that patients continue to have difficulty differentiating between these two tasks and to appreciate the value of their contribution to a shared decision making process.
Limitations of this study include the small number of patients classified per role. This precluded our ability to examine associations between choice predisposition and preference for Roles 4 and 5. In addition, preferred role in decision making is context dependent, and the results noted in this study may not apply to other clinical contexts.
4.2 Conclusion
In summary, certainty is associated with patients’ preferred decision styles. Patients who are uncertain desire roles which involve greater physician input, while those who are certain about which course they want to pursue are more likely to assume an autonomous role. In both cases, physicians should ensure that patients are adequately informed before ascertaining or confirming level of certainty and role preference.
4.3 Practice Implications
Physicians should ascertain their patients’ levels of uncertainty and adjust their input accordingly.
Acknowledgments
This study was funded by the VA Health Services Research Department Grant IIR 03-621-1 and the Yale Liver Center Pilot Project Grant DK P30 34989. Dr. Fraenkel is also supported by the K23 Award AR048826-01.
Appendix
 |
References
- 1.Say R, Murtagh M, Thomson R. Patients’ preference for involvement in medical decision making: a narrative review. Patient Educ Counsel. 2006;60:102–14. doi: 10.1016/j.pec.2005.02.003. [DOI] [PubMed] [Google Scholar]
- 2.Levinson W, Kao A, Kuby A, Thisted RA. Not all patients want to participate in decision-making. J Gen Intern Med. 2005;20:531–35. doi: 10.1111/j.1525-1497.2005.04101.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mansell D, Poses RM, Kazis L, Duefield CA. Clinical factors that influence patients’ desire for participation in decisions about illness. Arch Intern Med. 2000;160:2991–6. doi: 10.1001/archinte.160.19.2991. [DOI] [PubMed] [Google Scholar]
- 4.Greenfield S, Kaplan SH, Ware JE, Jr., Yano EM, Frank HJ. Patients’ participation in medical care: effects on blood sugar control and quality of life in diabetes. J Gen Intern Med. 1988;3:448–57. doi: 10.1007/BF02595921. [DOI] [PubMed] [Google Scholar]
- 5.Kaplan SH, Greenfield S, Ware JE., Jr Assessing the effects of physician-patient interactions on the outcomes of chronic disease. Med Care. 1989;27:S110–27. doi: 10.1097/00005650-198903001-00010. [DOI] [PubMed] [Google Scholar]
- 6.van Dam HA, van der Horst F, van den Borne B, Ryckman R, Crebolder H. Provider-patient interaction in diabetes care: effects on patients’ self-care and outcomes. Patient Educ Counsel. 2003;51:17–28. doi: 10.1016/s0738-3991(02)00122-2. [DOI] [PubMed] [Google Scholar]
- 7.Ward MM, Sundaramurthy S, Lotstein D, Bush TM, Neuwelt CM, Street RJ. Participatory patient-physician communication and morbidity in patients with systemic lupus erythematosus. Arthritis Rheum. 2003;49:810–18. doi: 10.1002/art.11467. [DOI] [PubMed] [Google Scholar]
- 8.Clever SL, Ford DE, Rubenstein LV, et al. Primary care patients’ involvement in decision-making is associated with improvement in depression. Med Care. 2006;44:398–405. doi: 10.1097/01.mlr.0000208117.15531.da. [DOI] [PubMed] [Google Scholar]
- 9.Strull WM, Lo B, Charles G. Do patients want to participate in medical decision making? JAMA. 1984;252:2990–4. [PubMed] [Google Scholar]
- 10.Stiggelbout AM, Kiebert GM. Patient preferences for information and participation in clinical decision making: a role for the sick role. Can Med Assoc J. 1997;157:383–9. [PMC free article] [PubMed] [Google Scholar]
- 11.Funk LM. Who wants to be involved? Decision-making preferences among residents of long-term care facilities. Can J Aging. 2004;23:47–58. doi: 10.1353/cja.2004.0004. [DOI] [PubMed] [Google Scholar]
- 12.Gattellari M, Ward JE. Measuring men's preferences for involvement in medical care: getting the question right. J Eval Clin Pract. 2005;11:237–46. doi: 10.1111/j.1365-2753.2005.00530.x. [DOI] [PubMed] [Google Scholar]
- 13.Ende J, Kazis L, Ash A, M.A. M. Measuring patients’ desire for autonomy. J Gen Intern Med. 1989;4:23–30. doi: 10.1007/BF02596485. [DOI] [PubMed] [Google Scholar]
- 14.Fraenkel L, McGraw S. What are the essential elements to enable patient participation in medical decision making? J Gen Intern Med. 2007;22:614–9. doi: 10.1007/s11606-007-0149-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Degner LF, Sloan JA, Venkatesh P. The Control Preferences Scale. Can J Nurs Res. 1997;29:21–43. [PubMed] [Google Scholar]
- 16.Fried MW, Shiffman ML, Reddy KR, et al. Peginterferon alfa-2a plus ribavirin for chronic hepatitis C virus infection. N Engl J of Med. 2002;347:975–82. doi: 10.1056/NEJMoa020047. [DOI] [PubMed] [Google Scholar]
- 17.O'Connor AM, Tugwell P, Wells GA, et al. A decision aid for women considering hormone therapy after menopause: Decision support framework and evaluation. Patient Educ Counsel. 1998;33:267–79. doi: 10.1016/s0738-3991(98)00026-3. [DOI] [PubMed] [Google Scholar]
- 18.Thom DH, Ribisl KM, Stewart AL, et al. Further validation and reliability testing of the trust in physician scale. Med Care. 1999;37:510–17. doi: 10.1097/00005650-199905000-00010. [DOI] [PubMed] [Google Scholar]
- 19.Deber RB, Kraetschmer N, Irvine J. What role do patients wich to play in treatment decision making? Arch Intern Med. 1996;156:1414–20. [PubMed] [Google Scholar]



