Abstract
Reduction of low-density lipoprotein-cholesterol through statin therapy has only modestly decreased coronary heart disease (CHD)-associated mortality in developed countries, which has prompted the search for alternative therapeutic strategies for CHD. Major efforts are now focused on therapies that augment high-density lipoprotein (HDL)-mediated reverse cholesterol transport (RCT), and ultimately increase the fecal disposal of cholesterol. The process of RCT has long been thought to simply involve HDL-mediated delivery of peripheral cholesterol to the liver for biliary excretion out of the body. However, recent studies have revealed a novel pathway for RCT that does not rely on biliary secretion. This non-biliary pathway rather involves the direct excretion of cholesterol by the proximal small intestine. Compared to RCT therapies that augment biliary sterol loss, modulation of non-biliary fecal sterol loss through the intestine is a much more attractive therapeutic strategy, given that excessive biliary cholesterol secretion can promote gallstone formation. However, we are at an early stage in understanding the molecular mechanisms regulating the non-biliary pathway for RCT, and much additional work is required in order to effectively target this pathway for CHD prevention. The purpose of this review is to discuss our current understanding of biliary and non-biliary contributions to RCT with particular emphasis on the possibility of targeting the intestine as an inducible cholesterol secretory organ.
Keywords: Cholesterol, Intestine, Bile, Lipoprotein, Reverse cholesterol transport
INTRODUCTION
Atherosclerosis is the disease process underlying the clinical complications of coronary heart disease (CHD), an epidemic that has taken more lives in the United States over the past century than the next four causes combined[1]. Atherosclerotic cardiovascular disease (ASCVD) was long thought to be a problem of developed Western societies, but it is now understood that this cholesterol-driven disease pervades throughout most of the world[2,3]. The most accurate predictor of ASCVD incidence is the plasma concentration of low-density lipoprotein cholesterol (LDLc). Hence, lowering LDLc has been the primary therapeutic goal for decades, and statins have been the main drug used to accomplish this. However, even with the substantial LDLc lowering achieved with statin treatment, these drugs have been able to reduce CHD-associated mortality and morbidity by only approximately 30%[4]. Major pharmaceutical interest has thus shifted towards developing high-density lipoprotein cholesterol (HDLc)-elevating agents, since HDLc was shown to be an even stronger predictor than LDLc for CHD in the Framingham Heart Study[5]. There have been many mechanisms proposed as to how HDLc influences the development of CHD[6-8], but the most widely accepted is the idea that HDL directly facilitates the process of reverse cholesterol transport (RCT).
REVERSE CHOLESTEROL TRANSPORT: THE CLASSIC “BILIARY” MODEL REQUIRES RECONSIDERATION
Nearly forty years ago, Glomset et al[9,10] presented the seminal framework of HDL-driven RCT. This model for RCT was described as a process by which extrahepatic (peripheral) cholesterol is returned to the liver for excretion into bile for subsequent loss through the feces[9,10]. It is reasonable to assume that the process of RCT has primarily evolved to protect multiple peripheral tissues from the excess accumulation of unesterified cholesterol, which is known to be cytotoxic[11,12]. Importantly, in the context of ASCVD, RCT is thought to involve HDL-mediated efflux of cholesterol from the arterial wall, specifically from cholesterol-laden macrophages[13-15]. In the classic “biliary” view of RCT[9,10], HDL-mediated delivery of peripheral cholesterol to the liver directly results in biliary secretion[13-15]. Given this model, plasma HDLc levels should accurately predict both biliary sterol secretion and fecal sterol loss. However, there are now several examples where plasma HDLc levels do not predict the levels of cholesterol in bile or feces[16-18]. For example, in mice lacking ATP-binding cassette protein A1 (ABCA1) or apolipoprotein-AI, plasma HDLc is essentially at undetectable levels[16-18]. However, in the face of near complete absence of HDLc, biliary and fecal cholesterol levels are normal in these mice[16-18]. These studies quite convincingly demonstrate that plasma HDLc levels do not determine the amount of cholesterol ultimately excreted into the feces. These findings bring into question whether therapeutic strategies that simply raise HDLc will indeed promote fecal disposal of cholesterol. Ultimately, to effectively target RCT, a drug should show efficacy in promoting the fecal disposal of cholesterol, not simply raising HDLc.
Another problem with the classic model of RCT is that the levels of cholesterol secreted into bile do not accurately predict fecal disposal of cholesterol[19-24]. In support of this concept, it has been demonstrated in several mouse models where hepatobiliary cholesterol secretion is substantially diminished that fecal sterol loss is normal[19-23]. The first demonstration of this was seen in mice lacking the canalicular phospholipid transporter, multidrug resistance 2 (Mdr2)[19]. Mice lacking Mdr2 have the inability to secrete phospholipids into bile, and secondary to biliary phospholipid insufficiency these mice also have diminished biliary cholesterol secretion[19]. Quite strikingly, even with > 80% reduced levels of biliary cholesterol, Mdr2 null mice have normal or even increased fecal cholesterol loss compared to wild type mice[19,20]. Furthermore, activation of the liver X receptor (LXR) in Mdr2 null mice results in large increases in fecal sterol output, without increasing biliary cholesterol output, supporting the presence of an LXR-inducible non-biliary pathway for fecal sterol loss in these mice[20]. Our group has found strikingly similar results in another mouse model lacking the ability to secrete cholesterol into bile[21,22]. In order to characterize the role of Niemann-Pick C1-Like 1 (NPC1L1) in hepatobiliary sterol secretion, we previously generated mice transgenically overexpressing NPC1L1 in hepatocytes[21]. Interestingly, NPC1L1 overexpression in the liver results in a > 90% reduction in biliary cholesterol levels, yet mass fecal neutral sterol loss and macrophage RCT is normal in these mice[21,22]. In addition, LXR activation in NPC1L1-LiverTg mice results in large increases in macrophage RCT and mass fecal neutral sterol loss[22], further supporting the existence of a non-biliary pathway in this model. In order to more definitively test whether bile is required for macrophage RCT, we set out to create a surgical model where there would be no biliary emptying into the small intestine, without obstructing bile flow. In order to do this we surgically diverted bile flow away from the small intestine and measured macrophage RCT. Importantly, mice surgically lacking biliary contributions to the intestine have normal LXR-inducible macrophage RCT[22]. Collectively, these studies in mice demonstrate that mass fecal sterol loss and macrophage RCT can proceed in the complete absence of biliary sterol secretion, challenging the obligate role of bile in RCT. Although the classic “biliary” model has been instrumental in providing a framework for our current understanding of RCT, we now understand that fecal sterol loss does not absolutely require circulating HDL[16-18] or biliary sterol secretion[19-22]. Paradigm shifting data such as these[16-23] strongly suggest that an alternative model for RCT is now appropriate. Based on our current understanding, fecal sterols originate from at least two distinct excretory routes: (1) the classic hepatobiliary sterol secretion route; and (2) the non-biliary liver to plasma lipoprotein to small intestine to feces route (Figure 1). Importantly, the major mechanisms regulating cholesterol secretion into bile have been recently defined[19,21,24-27], but almost no information exists regarding mediators of non-biliary cholesterol secretion by the intestine.
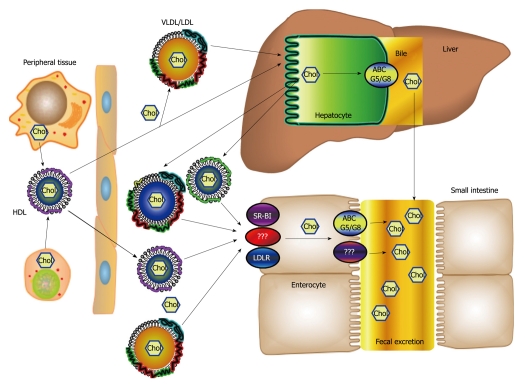
Figure 1.
Biliary and non-biliary fecal cholesterol excretion. In this proposed model, cholesterol is effluxed from peripheral cells onto high-density lipoprotein (HDL) and then delivered to the liver or small intestine via HDL or very low density lipoprotein (VLDL)/low-density lipoprotein (LDL) following cholesterol ester transfer protein-mediated transfer. The cholesterol internalized or de novo synthesized by the liver is secreted into bile through the action of ABCG5/G8 and subsequently excreted in the feces. Alternatively, the liver secretes the cholesterol in apoB-containing lipoproteins or HDL containing apoAI or apoE, which are specifically targeted to the small intestine. After being internalized by scavenger receptor, class B, type I (SR-BI), LDL receptor (LDLR), or another lipoprotein receptor system, the cholesterol is trafficked across the enterocytes to the brush border membrane and effluxed into the intestinal lumen by ABCG5/G8 or a currently unidentified cholesterol transporter.
REVERSE CHOLESTEROL TRANSPORT: EARLY SUPPORT FOR AN ALTERNATIVE “NON-BILIARY” MODEL
Long before Glomset et al[9,10] proposed the “biliary” model for RCT, the existence of a “non-biliary” pathway for RCT was proposed by Sperry et al[28]. In 1927, Sperry’s experiments demonstrated that in dogs that had undergone chronic biliary fistula surgery, fecal neutral sterol loss was paradoxically increased, compared to control bile intact dogs. Sperry’s findings were largely ignored given that it was already well accepted in the 1920s that bile was the only source of fecal lipids. Nearly a half-century later, Pertsemlidis et al[29] confirmed the results of Sperry et al[28], by demonstrating surgical biliary diversion resulted in complete loss of fecal acidic sterol output, yet fecal neutral sterol output actually increased approximately 7-fold. These studies, along with elegant work done by Dietschy et al[30,31], have demonstrated that bile is absolutely required for the enterohepatic circulation of acidic sterols, but this is not the case for neutral sterols. Similar results have been seen in bile diverted rats[32] and familial hypercholesterolemic humans[33]. Actually, as early as 1959, it was suggested that non-dietary fecal cholesterol loss in humans consists of two distinct fractions: (1) the traditional fraction coming from hepatobiliary secretion; and (2) an elusive fraction directly secreted by the intestine[34]. Unfortunately, a major drawback of these early biliary diversion or obstruction models is the interruption of enterohepatic circulation of bile acids and other non-lipid components that are found in bile. Under bile-diverted conditions, the absence of bile salt delivery to the intestinal lumen compromises intestinal cholesterol absorption, and endogenous cholesterol synthesis is strongly upregulated locally in the intestine[30]. Given these limitations, these early studies have been largely ignored, and the theory that fecal neutral sterol loss derives only from a biliary origin has become dogma. However, we have recently demonstrated that biliary cholesterol secretion is not required for macrophage RCT in mice using both surgical and genetic models of biliary insufficiency[22]. Collectively, findings in animal models of bile diversion have clearly demonstrated the presence of a non-biliary component of RCT, yet the mechanisms underlying such a process are poorly understood.
RELATIVE CONTRIBUTION OF THE NON-BILIARY PATHWAY TO RCT
In addition to the classic RCT pathway involving cholesterol secretion into the bile, there is mounting evidence that a non-biliary pathway quantitatively contributes to fecal cholesterol excretion. The non-biliary RCT pathway appears to involve the targeting of plasma cholesterol to the small intestine and the subsequent cellular secretion of the cholesterol into the lumen of this organ. Christened transintestinal cholesterol efflux (TICE) by Kuipers, Groen and their colleagues, the relative contribution of the non-biliary pathway to fecal cholesterol loss has not been fully defined. In normal chow-fed C57BL/6J mice, TICE accounts for 33% of total fecal neutral sterol loss[35], and roughly 20% of total fecal sterol loss in FVB mice[20]. However, it is important to point out that non-biliary fecal cholesterol loss is quite sensitive to pharmacological manipulation. To this end, LXR activation can dramatically augment non-biliary macrophage RCT[22], and increases mass fecal neutral sterol loss[20,22,35]. In fact, LXR activation in C57BL/6J increases the contribution of TICE to fecal cholesterol loss from 33% in vehicle treated mice to 63% in LXR agonist-treated mice[35]. Furthermore, activation of the peroxisome proliferator activated receptor δ (PPAR-δ) also promotes non-biliary neutral fecal sterol loss in mice[36]. Importantly, now in three independent genetically modified mouse models (ABCG5/G8-/-, Mdr2-/-, and NPC1L1-LiverTg) that have severely diminished biliary cholesterol secretion, fecal neutral sterol loss is only modestly decreased[24] or not altered at all[20,22]. This clearly indicates that the non-biliary pathway must be able to adequately compensate for biliary insufficiency to maintain normal fecal cholesterol loss in rodents. Collectively, these data support the idea that fecal neutral sterol loss is a mixture of dietary, biliary, and intestinally-derived cholesterol, and the origins of the latter source likely originates from the plasma compartment[20,23,35]. Given the plasma source of intestinally derived fecal neutral sterols, and the central role of the liver in lipoprotein metabolism, it is tempting to speculate that the liver may serve as a potential site of organization for non-biliary fecal cholesterol loss.
ORIGINS OF NEUTRAL STEROLS FOR TRANSINTESTINAL CHOLESTEROL EFFLUX
In the classic view of RCT, the liver plays a central role in moving peripheral cholesterol out of the body[13-15]. In parallel, we believe that the liver also plays a central role in the non-biliary pathway by re-packaging peripheral cholesterol into liver-derived lipoproteins that are targeted for subsequent intestinal uptake[23]. In support of this concept, most of the mouse models where non-biliary fecal cholesterol loss has been described[20-23] represent conditions where free cholesterol could potentially accumulate in the liver due to defects in normal hepatic elimination pathways. It remains possible that under conditions where hepatic free cholesterol burden becomes too excessive for disposal through biliary secretion (i.e. Mdr2-/- mice[20], ACAT2 ASO treatment[22], or NPC1L1-Liver-Tg mice[22,23]), an alternative non-biliary plasma lipoprotein-based route for fecal cholesterol disposal is utilized. In previous work, we were able to show that the liver can secrete lipoprotein particles that preferentially deliver cholesterol to the proximal small intestine for fecal excretion[22]. However, whether these liver-derived lipoproteins represent nascent very low density lipoprotein (VLDL) particles, nascent HDL particles, or some novel lipoprotein remains to be addressed.
POSSIBLE COMPONENTS IN THE TRANSINTESTINAL CHOLESTEROL EFFLUX PATHWAY
Based upon their ability to transport mass amounts of cholesterol in the blood and deliver the cholesterol to specific cells within tissues and organs, lipoproteins are almost certainly involved in the TICE pathway. However, it is unclear which lipoprotein class or classes is involved and how the lipoprotein is targeted to the small intestine. Because of its role in the removal of excess cholesterol from peripheral tissues, HDL is a logical choice for the lipoprotein responsible for cholesterol trafficking to the small intestine. However, ABCA1 null mice, which have very low levels of HDL in plasma, have normal or increased fecal cholesterol excretion under basal conditions[16,18,37]. Furthermore, treatment with an LXR agonist, which stimulates TICE, causes fecal cholesterol excretion to increase to the same extent in both wild type and ABCA1 null mice[38]. Thus, at least in mice, HDL does not appear to be necessary for non-biliary RCT.
Apolipoprotein E (apoE)-rich HDL (HDL-E) could also be involved in delivering cholesterol to the small intestine for fecal excretion. HDL-E is found in the plasma of wild type mice[21] but its concentration is significantly increased in two mouse models with upregulated TICE, NPC1L1-LiverTg and LXR agonist-treated wild type mice[21,39,40]. Compared to LDL and apoAI-rich HDL, HDL-E has an intermediate size and a higher ratio of free cholesterol to cholesteryl ester. The source of HDL-E is currently unknown, but it could be generated by hepatic ABCA1 effluxing cholesterol and phospholipid to lipid-poor apoE. Hepatic ABCA1 is increased in both NPC1L1-LiverTg and LXR-agonist treated mice and it has been shown that hepatic overexpression of ABCA1 in mice increases the plasma concentration of HDL-E[41]. Humans and other species with high levels of cholesterol ester transfer protein activity have low concentrations of plasma HDL-E[42]. Thus, the contribution of HDL-E to the TICE pathway would presumably be much greater in mice than humans.
Evidence from our group also suggests that liver-derived apoB-containing lipoproteins can deliver cholesterol for TICE[23]. In order to study the hepatic function of the cholesterol esterifying enzyme ACAT2, we treated mice with an antisense oligonucleotide (ASO) which targets ACAT2 mRNA for degradation. Mice treated with ACAT2 ASO vs control ASO had no change in biliary cholesterol secretion but had a 2-fold increase in fecal cholesterol excretion. The increased fecal cholesterol excretion was concluded to be the result of TICE since ACAT2 ASO-treated mice, unlike ACAT2 null mice, did not have a significant reduction in cholesterol absorption. To determine whether the liver was producing a lipoprotein that was targeted for clearance by the small intestine, isolated liver perfusion was conducted on mice that had been radiolabeled with [3H]cholesterol and treated with control or ACAT2 ASO. The radiolabeled perfusate, which carried almost 100% of the cholesterol on VLDL, was then injected into control and ACAT2 ASO treated mice. After 6 h, 2-3 fold more [3H]cholesterol from the ACAT2 ASO perfusate compared to the control ASO perfusate had accumulated in the lumen and wall of the proximal small intestine. One interpretation of this result was that the VLDL secreted from the ACAT2 ASO liver was preferentially targeted to the small intestine. It is also possible that following clearance of the perfusate VLDL by the liver, the [3H]cholesterol was packaged into another lipoprotein that delivered the cholesterol to the intestine. However, hepatic production of this lipoprotein would likely be driven by some factor secreted exclusively into the ACAT2 ASO perfusate since intestinal accumulation of [3H]cholesterol from ACAT2 ASO perfusate was similar in control and ACAT2 ASO-treated recipient mice.
Regardless of the lipoprotein class that delivers cholesterol to the small intestine, there must be receptors involved in the internalization or uptake of the lipoprotein cholesterol by the enterocytes. Scavenger receptor, class B, type I (SR-BI), which is expressed on the basolateral surface of enterocytes, is one receptor that could potentially play a role in TICE. SR-BI can bind VLDL, LDL, and HDL and subsequently mediates the selective uptake of the cholesteryl ester[43]. Intestinal expression of SR-BI also increases with LXR agonist treatment of mice[20,38]. However, when measured using an intestinal perfusion system, TICE was found to be significantly increased in SR-BI null mice[44]. Studies involving mice with intestine specific overexpression or deletion of SR-BI may aid in determining whether SR-BI plays a part in TICE.
If apoE-rich HDL or apoB-containing lipoproteins are involved in the TICE pathway then a member of the LDL receptor family may mediate the uptake of these particles by the enterocytes. The LDL receptor is expressed in the small intestine; however its expression at the protein level is downregulated in mice treated with LXR agonist[45]. Moreover, TICE appears to be stimulated in LDL receptor null mice treated with ACAT2 ASO compared to control ASO[23]. This data indicates that the LDL receptor is not necessary for TICE but does not exclude the possibility that other members of the LDL receptor family may compensate when the LDL receptor is absent.
Following delivery of lipoprotein cholesterol to the enterocytes, the ATP-binding cassette (ABC) transporters G5 and G8 appear to participate in pumping the cholesterol into the lumen of the small intestine. Expressed in the liver and small intestine[46], ABCG5/G8 functions as an obligate heterodimer and facilitates cholesterol excretion from the body by effluxing cholesterol from the apical surface of hepatocytes and enterocytes into bile and intestinal contents, respectively[24,25,46,47]. By employing stable isotope tracers, it was determined that the contribution of TICE to fecal cholesterol excretion decreased from 25% in wild type mice to 15% in ABCG5 null mice[35]. In addition, LXR agonist treatment of ABCG5/G8 null mice, unlike wild type mice, did not increase mass fecal neutral sterol loss[48] and macrophage reverse cholesterol transport[49]. Although this data indicates that ABCG5/8 plays a role in TICE, there appears to be multiple or redundant pathways for effluxing cholesterol from enterocytes into the intestinal lumen since TICE continues to function, albeit at lower efficiency, in the absence of ABCG5/G8.
METHODOLOGIES FOR MEASURING TRANSINTESTINAL CHOLESTEROL EFFLUX
Several different methodologies have been used to measure TICE or non-biliary excretion in mice. Taking into consideration dietary intake, biliary secretion, fractional absorption, and fecal excretion of cholesterol, it was calculated that under basal conditions in wild type mice, TICE contributed 20%-50% of the cholesterol in feces[20,50]. Using similar measurements, approximately 40% of fecal cholesterol excretion was attributed to TICE in wild type mice treated with LXR agonist[20]. By determining the kinetics of stable isotopically labeled cholesterol that was delivered orally and intravenously plus assessing the fate of de novo synthesized cholesterol that was isotopically labeled, it was determined that 33% and 63% of fecal cholesterol excretion in mice treated with vehicle or LXR agonist was the result of TICE[35].
Cholesterol secretion into the lumen of the small intestine was also observed when the intestine of wild type mice was perfused with bile acid; phospholipid micelles[36,44,50]. The rate of cholesterol secretion was found to be highest in the proximal third of the small intestine[50], and was dependent upon the concentration of the phospholipid in the micelles[44]. Since [14C]cholesterol that was intravenously injected was found in the perfusate, a portion of the cholesterol secreted into the lumen was derived from the plasma. Moreover, the plasma cholesterol secreted in the lumen must have trafficked through and mixed with the cholesterol pool of the enterocytes since the specific activity of the cholesterol in the perfusate was similar to that of the mucosa but was 10-fold less than that of the serum[50]. Although these studies showed that bile salt:phospholipid micelles could mediate the efflux of cholesterol from the small intestine, the question remains whether TICE would occur if the micelles consisted of physiological concentrations of not only bile salt and phospholipid but also cholesterol.
DOES TICE PLAY A MAJOR ROLE IN HUMAN FECAL CHOLESTEROL EXCRETION?
Since most of the studies of the TICE pathway have been conducted in mice, the question remains whether TICE contributes significantly to fecal cholesterol excretion in humans. Using an intestinal perfusion system, it was estimated that approximately 44% of total fecal cholesterol output originated from non-biliary sources in humans[51]. Yet, it cannot be determined from this data whether TICE was the source of the non-biliary sterol. The current methodologies used to measure TICE in murine models are invasive and therefore could not be implemented in humans. However, the procedures used to measure TICE in mice could be applied to non-human primates, whose lipoprotein and cholesterol metabolism closely resembles that of man. If in non-human primates TICE can be shown to play a significant part in fecal cholesterol excretion and to be amenable to pharmaceutical manipulation then future studies in humans could be warranted. Although our understanding of non-biliary fecal sterol excretion is still in its infancy, continued research surrounding this pathway has strong potential to lead to novel therapies for the prevention and/or treatment of ASCVD.
Footnotes
Supported by Pathway to Independence Grants (5R00HL088528 to Temel RE and 1K99-HL096166 to Brown JM) from the National Heart, Lung, and Blood Institute
Peer reviewer: Valentina Medici, MD, Assistant Professor, Division of Gastroenterology and Hepatology, Department of Internal Medicine, University of California Davis, 4150 V Street, Suite 3500, Sacramento, CA 95817, United States
S- Editor Cheng JX L- Editor O’Neill M E- Editor Ma WH
References
- 1.Lloyd-Jones D, Adams RJ, Brown TM, Carnethon M, Dai S, De Simone G, Ferguson TB, Ford E, Furie K, Gillespie C, et al. Executive summary: heart disease and stroke statistics--2010 update: a report from the American Heart Association. Circulation. 2010;121:948–954. doi: 10.1161/CIRCULATIONAHA.109.192666. [DOI] [PubMed] [Google Scholar]
- 2.Ramaraj R, Alpert JS. Indian poverty and cardiovascular disease. Am J Cardiol. 2008;102:102–106. doi: 10.1016/j.amjcard.2008.02.104. [DOI] [PubMed] [Google Scholar]
- 3.Cheng TO. Price of modernization of China. Circulation. 2001;103:E131–E133. doi: 10.1161/01.cir.103.25.e131. [DOI] [PubMed] [Google Scholar]
- 4.Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106:3143–3421. [PubMed] [Google Scholar]
- 5.Gordon T, Castelli WP, Hjortland MC, Kannel WB, Dawber TR. High density lipoprotein as a protective factor against coronary heart disease. The Framingham Study. Am J Med. 1977;62:707–714. doi: 10.1016/0002-9343(77)90874-9. [DOI] [PubMed] [Google Scholar]
- 6.Assmann G, Schulte H, von Eckardstein A, Huang Y. High-density lipoprotein cholesterol as a predictor of coronary heart disease risk. The PROCAM experience and pathophysiological implications for reverse cholesterol transport. Atherosclerosis. 1996;124 Suppl:S11–S20. doi: 10.1016/0021-9150(96)05852-2. [DOI] [PubMed] [Google Scholar]
- 7.Gordon DJ, Probstfield JL, Garrison RJ, Neaton JD, Castelli WP, Knoke JD, Jacobs DR Jr, Bangdiwala S, Tyroler HA. High-density lipoprotein cholesterol and cardiovascular disease. Four prospective American studies. Circulation. 1989;79:8–15. doi: 10.1161/01.cir.79.1.8. [DOI] [PubMed] [Google Scholar]
- 8.Barter PJ, Nicholls S, Rye KA, Anantharamaiah GM, Navab M, Fogelman AM. Antiinflammatory properties of HDL. Circ Res. 2004;95:764–772. doi: 10.1161/01.RES.0000146094.59640.13. [DOI] [PubMed] [Google Scholar]
- 9.Glomset JA. The plasma lecithins:cholesterol acyltransferase reaction. J Lipid Res. 1968;9:155–167. [PubMed] [Google Scholar]
- 10.Glomset JA, Norum KR. The metabolic role of lecithin: cholesterol acyltransferase: perspectives form pathology. Adv Lipid Res. 1973;11:1–65. [PubMed] [Google Scholar]
- 11.Maxfield FR, Tabas I. Role of cholesterol and lipid organization in disease. Nature. 2005;438:612–621. doi: 10.1038/nature04399. [DOI] [PubMed] [Google Scholar]
- 12.Tabas I. Consequences of cellular cholesterol accumulation: basic concepts and physiological implications. J Clin Invest. 2002;110:905–911. doi: 10.1172/JCI16452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lewis GF, Rader DJ. New insights into the regulation of HDL metabolism and reverse cholesterol transport. Circ Res. 2005;96:1221–1232. doi: 10.1161/01.RES.0000170946.56981.5c. [DOI] [PubMed] [Google Scholar]
- 14.Wang X, Rader DJ. Molecular regulation of macrophage reverse cholesterol transport. Curr Opin Cardiol. 2007;22:368–372. doi: 10.1097/HCO.0b013e3281ec5113. [DOI] [PubMed] [Google Scholar]
- 15.Lewis GF. Determinants of plasma HDL concentrations and reverse cholesterol transport. Curr Opin Cardiol. 2006;21:345–352. doi: 10.1097/01.hco.0000231405.76930.a0. [DOI] [PubMed] [Google Scholar]
- 16.Groen AK, Bloks VW, Bandsma RH, Ottenhoff R, Chimini G, Kuipers F. Hepatobiliary cholesterol transport is not impaired in Abca1-null mice lacking HDL. J Clin Invest. 2001;108:843–850. doi: 10.1172/JCI12473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jolley CD, Woollett LA, Turley SD, Dietschy JM. Centripetal cholesterol flux to the liver is dictated by events in the peripheral organs and not by the plasma high density lipoprotein or apolipoprotein A-I concentration. J Lipid Res. 1998;39:2143–2149. [PubMed] [Google Scholar]
- 18.Xie C, Turley SD, Dietschy JM. ABCA1 plays no role in the centripetal movement of cholesterol from peripheral tissues to the liver and intestine in the mouse. J Lipid Res. 2009;50:1316–1329. doi: 10.1194/jlr.M900024-JLR200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Voshol PJ, Havinga R, Wolters H, Ottenhoff R, Princen HM, Oude Elferink RP, Groen AK, Kuipers F. Reduced plasma cholesterol and increased fecal sterol loss in multidrug resistance gene 2 P-glycoprotein-deficient mice. Gastroenterology. 1998;114:1024–1034. doi: 10.1016/s0016-5085(98)70323-3. [DOI] [PubMed] [Google Scholar]
- 20.Kruit JK, Plösch T, Havinga R, Boverhof R, Groot PH, Groen AK, Kuipers F. Increased fecal neutral sterol loss upon liver X receptor activation is independent of biliary sterol secretion in mice. Gastroenterology. 2005;128:147–156. doi: 10.1053/j.gastro.2004.10.006. [DOI] [PubMed] [Google Scholar]
- 21.Temel RE, Tang W, Ma Y, Rudel LL, Willingham MC, Ioannou YA, Davies JP, Nilsson LM, Yu L. Hepatic Niemann-Pick C1-like 1 regulates biliary cholesterol concentration and is a target of ezetimibe. J Clin Invest. 2007;117:1968–1978. doi: 10.1172/JCI30060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Temel RE, Sawyer JK, Yu L, Lord C, Degirolamo C, McDaniel A, Marshall S, Wang N, Shah R, Rudel LL, et al. Biliary sterol secretion is not required for macrophage reverse cholesterol transport. Cell Metab. 2010;12:96–102. doi: 10.1016/j.cmet.2010.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Brown JM, Bell TA 3rd, Alger HM, Sawyer JK, Smith TL, Kelley K, Shah R, Wilson MD, Davis MA, Lee RG, et al. Targeted depletion of hepatic ACAT2-driven cholesterol esterification reveals a non-biliary route for fecal neutral sterol loss. J Biol Chem. 2008;283:10522–10534. doi: 10.1074/jbc.M707659200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yu L, Hammer RE, Li-Hawkins J, Von Bergmann K, Lutjohann D, Cohen JC, Hobbs HH. Disruption of Abcg5 and Abcg8 in mice reveals their crucial role in biliary cholesterol secretion. Proc Natl Acad Sci USA. 2002;99:16237–16242. doi: 10.1073/pnas.252582399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yu L, Li-Hawkins J, Hammer RE, Berge KE, Horton JD, Cohen JC, Hobbs HH. Overexpression of ABCG5 and ABCG8 promotes biliary cholesterol secretion and reduces fractional absorption of dietary cholesterol. J Clin Invest. 2002;110:671–680. doi: 10.1172/JCI16001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Groen A, Kunne C, Jongsma G, van den Oever K, Mok KS, Petruzzelli M, Vrins CL, Bull L, Paulusma CC, Oude Elferink RP. Abcg5/8 independent biliary cholesterol excretion in Atp8b1-deficient mice. Gastroenterology. 2008;134:2091–2100. doi: 10.1053/j.gastro.2008.02.097. [DOI] [PubMed] [Google Scholar]
- 27.Wiersma H, Gatti A, Nijstad N, Oude Elferink RP, Kuipers F, Tietge UJ. Scavenger receptor class B type I mediates biliary cholesterol secretion independent of ATP-binding cassette transporter g5/g8 in mice. Hepatology. 2009;50:1263–1272. doi: 10.1002/hep.23112. [DOI] [PubMed] [Google Scholar]
- 28.Sperry WM. Lipid excretion IV. A study of the relationship of the bile to the fecal lipids with special reference to certain problems of sterol metabolism. J Biol Chem. 1927;71:351–378. [Google Scholar]
- 29.Pertsemlidis D, Kirchman EH, Ahrens EH Jr. Regulation of cholesterol metabolism in the dog. I. Effects of complete bile diversion and of cholesterol feeding on absorption, synthesis, accumulation, and excretion rates measured during life. J Clin Invest. 1973;52:2353–2367. doi: 10.1172/JCI107424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dietschy JM. The role of bile salts in controlling the rate of intestinal cholesterogenesis. J Clin Invest. 1968;47:286–300. doi: 10.1172/JCI105725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dietschy JM, Siperstein MD. Cholesterol synthesis by the gastrointestinal tract: localization and mechanisms of control. J Clin Invest. 1965;44:1311–1327. doi: 10.1172/JCI105237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bandsma RH, Stellaard F, Vonk RJ, Nagel GT, Neese RA, Hellerstein MK, Kuipers F. Contribution of newly synthesized cholesterol to rat plasma and bile determined by mass isotopomer distribution analysis: bile-salt flux promotes secretion of newly synthesized cholesterol into bile. Biochem J. 1998;329(Pt 3):699–703. doi: 10.1042/bj3290699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Deckelbaum RJ, Lees RS, Small DM, Hedberg SE, Grundy SM. Failure of complete bile diversion and oral bile acid therapy in the treatment of homozygous familial hypercholesterolemia. N Engl J Med. 1977;296:465–470. doi: 10.1056/NEJM197703032960901. [DOI] [PubMed] [Google Scholar]
- 34.Cheng SH, Stanley MM. Secretion of cholesterol by intestinal mucosa in patients with complete common bile duct obstruction. Proc Soc Exp Biol Med. 1959;101:223–225. doi: 10.3181/00379727-101-24890. [DOI] [PubMed] [Google Scholar]
- 35.van der Veen JN, van Dijk TH, Vrins CL, van Meer H, Havinga R, Bijsterveld K, Tietge UJ, Groen AK, Kuipers F. Activation of the liver X receptor stimulates trans-intestinal excretion of plasma cholesterol. J Biol Chem. 2009;284:19211–19219. doi: 10.1074/jbc.M109.014860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Vrins CL, van der Velde AE, van den Oever K, Levels JH, Huet S, Oude Elferink RP, Kuipers F, Groen AK. Peroxisome proliferator-activated receptor delta activation leads to increased transintestinal cholesterol efflux. J Lipid Res. 2009;50:2046–2054. doi: 10.1194/jlr.M800579-JLR200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Temel RE, Lee RG, Kelley KL, Davis MA, Shah R, Sawyer JK, Wilson MD, Rudel LL. Intestinal cholesterol absorption is substantially reduced in mice deficient in both ABCA1 and ACAT2. J Lipid Res. 2005;46:2423–2431. doi: 10.1194/jlr.M500232-JLR200. [DOI] [PubMed] [Google Scholar]
- 38.Plōsch T, Kok T, Bloks VW, Smit MJ, Havinga R, Chimini G, Groen AK, Kuipers F. Increased hepatobiliary and fecal cholesterol excretion upon activation of the liver X receptor is independent of ABCA1. J Biol Chem. 2002;277:33870–33877. doi: 10.1074/jbc.M206522200. [DOI] [PubMed] [Google Scholar]
- 39.Cao G, Beyer TP, Yang XP, Schmidt RJ, Zhang Y, Bensch WR, Kauffman RF, Gao H, Ryan TP, Liang Y, et al. Phospholipid transfer protein is regulated by liver X receptors in vivo. J Biol Chem. 2002;277:39561–39565. doi: 10.1074/jbc.M207187200. [DOI] [PubMed] [Google Scholar]
- 40.Jiang XC, Beyer TP, Li Z, Liu J, Quan W, Schmidt RJ, Zhang Y, Bensch WR, Eacho PI, Cao G. Enlargement of high density lipoprotein in mice via liver X receptor activation requires apolipoprotein E and is abolished by cholesteryl ester transfer protein expression. J Biol Chem. 2003;278:49072–49078. doi: 10.1074/jbc.M304274200. [DOI] [PubMed] [Google Scholar]
- 41.Vaisman BL, Lambert G, Amar M, Joyce C, Ito T, Shamburek RD, Cain WJ, Fruchart-Najib J, Neufeld ED, Remaley AT, et al. ABCA1 overexpression leads to hyperalphalipoproteinemia and increased biliary cholesterol excretion in transgenic mice. J Clin Invest. 2001;108:303–309. doi: 10.1172/JCI12517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tall AR. Plasma lipid transfer proteins. J Lipid Res. 1986;27:361–367. [PubMed] [Google Scholar]
- 43.Trigatti BL, Krieger M, Rigotti A. Influence of the HDL receptor SR-BI on lipoprotein metabolism and atherosclerosis. Arterioscler Thromb Vasc Biol. 2003;23:1732–1738. doi: 10.1161/01.ATV.0000091363.28501.84. [DOI] [PubMed] [Google Scholar]
- 44.van der Velde AE, Vrins CL, van den Oever K, Seemann I, Oude Elferink RP, van Eck M, Kuipers F, Groen AK. Regulation of direct transintestinal cholesterol excretion in mice. Am J Physiol Gastrointest Liver Physiol. 2008;295:G203–G208. doi: 10.1152/ajpgi.90231.2008. [DOI] [PubMed] [Google Scholar]
- 45.Zelcer N, Hong C, Boyadjian R, Tontonoz P. LXR regulates cholesterol uptake through Idol-dependent ubiquitination of the LDL receptor. Science. 2009;325:100–104. doi: 10.1126/science.1168974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Berge KE, Tian H, Graf GA, Yu L, Grishin NV, Schultz J, Kwiterovich P, Shan B, Barnes R, Hobbs HH. Accumulation of dietary cholesterol in sitosterolemia caused by mutations in adjacent ABC transporters. Science. 2000;290:1771–1775. doi: 10.1126/science.290.5497.1771. [DOI] [PubMed] [Google Scholar]
- 47.Graf GA, Yu L, Li WP, Gerard R, Tuma PL, Cohen JC, Hobbs HH. ABCG5 and ABCG8 are obligate heterodimers for protein trafficking and biliary cholesterol excretion. J Biol Chem. 2003;278:48275–48282. doi: 10.1074/jbc.M310223200. [DOI] [PubMed] [Google Scholar]
- 48.Yu L, York J, von Bergmann K, Lutjohann D, Cohen JC, Hobbs HH. Stimulation of cholesterol excretion by the liver X receptor agonist requires ATP-binding cassette transporters G5 and G8. J Biol Chem. 2003;278:15565–15570. doi: 10.1074/jbc.M301311200. [DOI] [PubMed] [Google Scholar]
- 49.Calpe-Berdiel L, Rotllan N, Fiévet C, Roig R, Blanco-Vaca F, Escolà-Gil JC. Liver X receptor-mediated activation of reverse cholesterol transport from macrophages to feces in vivo requires ABCG5/G8. J Lipid Res. 2008;49:1904–1911. doi: 10.1194/jlr.M700470-JLR200. [DOI] [PubMed] [Google Scholar]
- 50.van der Velde AE, Vrins CL, van den Oever K, Kunne C, Oude Elferink RP, Kuipers F, Groen AK. Direct intestinal cholesterol secretion contributes significantly to total fecal neutral sterol excretion in mice. Gastroenterology. 2007;133:967–975. doi: 10.1053/j.gastro.2007.06.019. [DOI] [PubMed] [Google Scholar]
- 51.Simmonds WJ, Hofmann AF, Theodor E. Absorption of cholesterol from a micellar solution: intestinal perfusion studies in man. J Clin Invest. 1967;46:874–890. doi: 10.1172/JCI105587. [DOI] [PMC free article] [PubMed] [Google Scholar]