Abstract
Despite California's 1994 statewide smoking ban, exposure to secondhand smoke (SHS) continues in California's Indian casinos. Few data are available on exposure to airborne fine particles (PM2.5) in casinos, especially on a statewide basis. We sought to measure PM2.5 concentrations in Indian casinos widely distributed across California, exploring differences due to casino size, separation of smoking and non-smoking areas, and area smoker density. A selection of 36 out of the 58 Indian casinos throughout California were each visited for 1–3 h on weekend or holiday evenings, using two or more concealed monitors to measure PM2.5 concentrations every 10 s. For each casino, the physical dimensions and the number of patrons and smokers were estimated. As a preliminary assessment of representativeness, we also measured eight casinos in Reno, NV. The average PM2.5 concentration for the smoking slot machine areas (63 μg/m3) was nine times as high as outdoors (7 μg/m3), whereas casino non-smoking restaurants (29 μg/m3) were four times as high. Levels in non-smoking slot machine areas varied: complete physical separation reduced concentrations almost to outdoor levels, but two other separation types had mean levels that were 13 and 29 μg/m3, respectively, higher than outdoors. Elevated PM2.5 concentrations in casinos can be attributed primarily to SHS. Average PM2.5 concentrations during 0.5–1 h visits to smoking areas exceeded 35 μg/m3 for 90% of the casino visits.
Keywords: secondhand smoke, particulate matter, PM2.5, casino, indoor air pollution, smoking activity
Introduction
Exposure to secondhand smoke (SHS) has been implicated as a risk factor for cardiovascular diseases, pulmonary malfunction, lung cancer, and mortality (Brennan et al., 2004; Nazaroff and Singer, 2004; CDC, 2005; California EPA, 2006; Surgeon General, 2006). Barnoya and Glantz (2005) found brief exposures (minutes to hours) to SHS were associated with adverse cardiovascular effects nearly as large (80–90%) as those experienced by chronic active smokers.
SHS is a major indoor source of airborne fine particles (PM2.5), which have been associated with a range of acute and chronic diseases (Pope et al., 2001, 2009; U.S. EPA, 2006). Currently, 164 countries have adopted comprehensive or partial smoke-free legislation (Koh et al., 2007; WHO, 2009). As of April 2009, 15 states in the United States, plus Washington DC, have enacted smoke-free laws in all workplaces, including bars and restaurants (ANRF, 2009).
California was the first state to enact a statewide ban on smoking in indoor workplaces. In 1994, California passed its Smoke-free Indoor Workplace Act, which prohibits smoking in enclosed places of employment (except tobacconists), including bars (1998) and restaurants. Some California towns and cities have subsequently passed stricter laws banning smoking outdoors near public buildings, in outdoor restaurant patios, and even in some apartment buildings. In 2007, California adopted a statewide law banning smoking in cars if children are present. However, due to the sovereign nation status of Indian tribes, exposure to SHS continues in nearly all California Indian casinos.
Indoor SHS in casinos imposes significant health risks on casino employees as well as on non-smoking patrons. Moreover, employees working on tribal reservations are not covered by California's worker safety laws (Dunstan, 1998). Earlier studies have found post-work shift or post-visit increases in the nicotine metabolite, cotinine, in casino employees and patrons (Trout et al., 1998; Wakefield et al., 2005; Abrams et al., 2006; Larsson et al., 2008; CDC, 2009; Repace, 2009). Two studies found increases in a tobacco-specific carcinogen in non-smoking casino patrons and dealers, respectively (Anderson et al., 2003; CDC, 2009). Other studies (Kado et al., 1991; Trout et al., 1998; Hammond, 1999) have examined airborne nicotine concentrations in casinos, and Larsson et al. (2008) reported that exposures for 87% of workers exceeded a nicotine threshold (0.5 μg/m3) associated with health risks. A survey of London casino workers (Pilkington et al., 2007) reported respiratory and sensory irritation symptoms associated with SHS exposure.
Exposures to SHS in hospitality locations and workplaces have been measured across the world (Siegel and Skeer, 2003; Hyland et al., 2008; López et al., 2008). However, the few published studies measuring fine particle concentrations inside casinos have considered relatively few casinos (Repace, 2004, 2009).
To the best of our knowledge, this study is the first to survey PM2.5 exposures in casinos on a statewide basis. Using a standardized protocol, we discreetly measured PM2.5 inside a selection of 36 casinos spread throughout California (including smoking areas, non-smoking areas, and restaurants), as well as outdoors. We also evaluated the effectiveness of different methods of separating the non-smoking from the smoking areas. Finally, as an initial exploration of whether the PM2.5 levels measured in California might also reflect casinos in other locations, we surveyed eight casinos in Reno, NV.
Methods
Research Location and Sample Selection
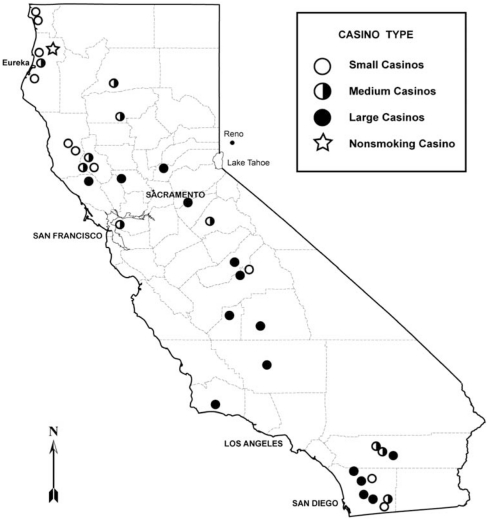
We surveyed 36 out of the 58 California Indian casinos (12 January to 25 December 2008), spanning locations across California (Figure 1). The locations, physical area, and the number of slot machines were tabulated for all 58 casinos from California Indian casino official websites. Each casino was classified based on the reported number of slot machines, as follows: small (<500), medium (500–1400), or large (>1400 slot machines). We sampled 10–15 casinos in each size range during nine trips covering different parts of the state. On each trip, we visited as many casinos as possible over a 3–8-day period. In addition, we visited what is, to the best of our knowledge, the only smoke-free Indian casino in California. We also surveyed, for comparison, eight casinos in Reno, NV, using the same sampling protocol.
Figure 1.
Map of California showing the locations and size categories of the 36 Indian casinos sampled.
Monitoring Protocol
Most casinos were sampled on weekend or holiday evenings, when occupancy was high. On each casino visit, two or more investigators carried concealed real-time (i.e. continuous) aerosol monitors (AM510 SidePak laser photometer; TSI, Shoreview, MN, USA) with a short intake (Tygon tubing) protruding from a handbag or pocket, with data logged every 10 s. The monitors were equipped with a 2.5-μm size-selective impactor.
The sampling locations at each casino included (1) outdoors (10-min periods before-and-after indoor sampling), (2) smoking slot machine areas (one 30-min period for small casinos, two 30-min periods for medium or large casinos), (3) non-smoking slot machine areas (30 min), and (4) restaurants (∼1 h). When sampling in smoking slot machine or non-smoking slot machine locations, the investigators followed separate routes without returning to the same area. While outdoors or at restaurants, the investigators walked or sat side-by-side. The protocol included an additional collocation period (∼10 min) in a non-smoking slot machine area or restaurant in which two or more monitors were placed side-by-side to compare readings. A typical sampling event started at 1800–2000 hours and lasted for 1–4 h, depending on the size and complexity of the casino.
Quality Assurance of Aerosol Monitors
The SidePak monitors determine the mass concentration from the intensity of scattered laser light. The monitor has a lower detection limit of 1 μg/m3 and an upper detection limit of 20,000 μg/m3 (TSI, 2008). The light scattering properties of particles vary with the size and composition of particles. Thus, it is essential to calibrate for the type of particles being sampled.
Before and after the field survey, we compared 12 SidePak monitors with gravimetric PM2.5 measurements. Fresh SHS was introduced into a 3 m3 chamber by a volunteer smoker, with four samples collected spanning a concentration range typical of indoor SHS levels (40–400 μg/m3). The relative humidity was 40% and 47%, respectively, for the before-and-after experiments.
For each SHS level, we collected pairs of gravimetric PM2.5 samples onto PTFE membrane filters (47 mm diameter, 2-μm pore size, Pall Corp., Ann Arbor, MI, USA) downstream of a cyclone separator, using critical orifices to maintain a stable flow rate through each filter. Flow rates were measured before and after by a primary flow (bubble) calibrator (Gilian Instrument Corp., West Caldwell, NJ, USA).
Gravimetric filters were equilibrated for over 24 h at controlled relative humidity (∼60%) and temperature (70°F) and then weighed before-and-after sampling using a Mettler M3 Microbalance (Mettler-Toledo, Columbus, OH, USA).
The slope from a linear regression of the gravimetric PM2.5 versus each SidePak determined the multiplication factor (custom calibration factor) for rescaling the SidePak's data. For individual monitors, custom calibration factors ranged from 0.24 to 0.31, with an average of 0.29 (SD=0.02) before and 0.28 (SD=0.02) after the field survey. R2 values were all above 0.995; intercepts were close to zero. The average absolute deviation of calibration factors between before-and-after experiments was 4% (range, 0–8% SD=3%). The average monitor precision was 3% (range, 1–12% SD=3%). Our calibration factors, which were nearly identical to values found by Lee et al. (2008) for SHS with SidePak monitors, were applied to all casino measurements (relative humidity was always under 47%). We scaled the measurements for each individual monitor by multiplying by the average of the before-and-after calibration factors.
Counting Protocol and Casino Dimensions
For each casino sampled, one investigator — the counter — measured the casino dimensions, and counted slot machines, players, and active smokers, while one or more other investigators measured PM2.5 concentrations carrying concealed SidePak monitors. For smaller casinos, the counter counted every slot machine, player, and active smoker on the casino gaming floor by walking through smoking and non-smoking slot machine areas, for 30 min each. In casinos where counting the entire slot area was not feasible within 30 min, the counter counted in randomly selected rows of slot machines throughout a large portion of the gaming area.
The occupancy (%) of a casino gaming area was calculated as:
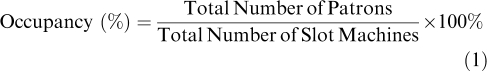 |
The active smoking prevalence (%) within the casino smoking area was defined as:
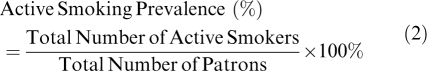 |
We measured the horizontal dimensions of each casino by calibrated foot pacing. Each active smoker was counted only once. The area smoker density (active smokers/100 m2) was calculated as:
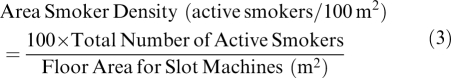 |
Data Analysis
We applied descriptive statistics, linear regression analysis, analysis of variance (ANOVA), paired t-test, and the Shapiro–Wilks test for normality. SigmaPlot software, Version 11.0 (Systat Software, San Jose, CA, USA), and the R statistical package, Version 2.5.1 (R Development Core Team, 2008) were used to perform the analyses.
Results
California Casino Sample Characteristics
The 58 casinos in California comprised 22 small, 15 medium, and 21 large ones. Our sample consisted of 11 small (including 1 smoke-free location), 10 medium, and 15 large casinos (Figure 1). The number of slot machines ranged from ∼200 to over 3000, and gaming floor areas ranged from ∼280 m2 to over 65,000 m2. All but four of the casinos had slot machines on a single floor. The temperature and relative humidity inside each casino, measured by a digital Hygro-Thermometer (Sunleaves, Bloomington, IN, USA), was 70–80°F and 16–46%, respectively.
Occupancy and active smoking prevalence were obtained for 35 casino visits, and area smoker density for 31 visits (Table 1). The occupancy on weekend and holiday evenings averaged 48% (range, 12–87%); the active smoking prevalence averaged 11% (range, 5–25%); and the area smoker density averaged 2.3 active smokers/100 m2 (range, 0.5–5.3 active smokers/100 m2). The mean occupancy in large casinos (60%) was significantly higher (one-way ANOVA, P<0.05) than in medium (43%) and small casinos (34%). However, the mean active smoking prevalence was significantly higher in small casinos (16%, versus 10% for large and medium casinos; P<0.05). Differences in the mean area smoker density by casino size were not statistically significant.
Table 1. Summary statistics for the 36 California casinos in the statewide survey.
| Casino IDa | Average concentrations (μg/m3) | Occupancy (%) | Active smoking prevalence (%) | Area smoker density (active smokers/100 m2) | |||
|---|---|---|---|---|---|---|---|
| Smoking | Outdoor | Non-smoking | Restaurant | ||||
| LA | 42.7 | 1.6 | 15.6 | 23.1 | 87.1 | 4.9 | 1.41 |
| LB | 39.9 | 19.0 | 24.2 | 19.0 | 54.4 | 6.3 | 1.38 |
| LC | 86.7 | 9.6 | 7.9 | 60.5 | 39.9 | 9.9 | 1.78 |
| LD | 35.9 | 6.9 | 16.3 | 36.4 | 43.5 | 5.0 | 1.00 |
| LEb | 40.8 | 9.5 | 25.5 | 18.8 | 52.8 | 7.5 | — |
| LE2c | 88.8 | 29.7 | 44.5 | 20.7 | 70.7 | 6.3 | 2.15 |
| LF | 49.3 | 16.3 | 4.4 | 35.6 | 48.7 | 6.2 | 1.79 |
| LG | 47.4 | 1.3 | — | 1.2 | 24.1 | 18.7 | 1.70 |
| LHb | 42.0 | 8.5 | 3.9 | 34.4 | 47.1 | 8.9 | — |
| LH2c | 45.8 | 2.3 | 12.3 | 41.1 | 67.5 | 9.6 | 2.56 |
| LI | 57.4 | 2.2 | 1.0 | 4.0 | 78.6 | 8.3 | 3.16 |
| LJ | 74.0 | 4.2 | 9.8 | 5.1 | 69.0 | 14.1 | 4.54 |
| LK | 109.6 | 5.3 | — | — | 63.5 | 14.1 | 4.18 |
| LM | 72.1 | 4.4 | 6.5 | — | 62.5 | 17.5 | 5.09 |
| LN | 62.4 | 1.3 | 57.2 | 34.6 | 87.2 | 7.7 | 3.15 |
| LO | 77.0 | 7.4 | 75.6 | 56.9 | — | — | — |
| LP | 75.8 | 1.3 | 24.6 | — | — | — | — |
| MA | 73.4 | 3.3 | — | 64.1 | 37.0 | 18.9 | — |
| MBb | 30.2 | 4.4 | 5.0 | 8.0 | 17.6 | 11.4 | — |
| MB2c | 21.2 | 3.4 | 6.6 | — | 24.1 | 10.3 | 0.98 |
| MC | 45.7 | 12.2 | 16.5 | 19.4 | 39.6 | 9.1 | 1.39 |
| MD | 60.5 | 2.9 | 32.6 | 43.7 | 19.6 | 10.8 | 1.27 |
| ME | 66.0 | 4.5 | — | — | 29.1 | 5.0 | 0.48 |
| MF | 68.2 | 7.9 | 81.2 | — | 73.0 | 10.0 | 1.84 |
| MG | 94.1 | 2.4 | 32.1 | — | 77.8 | 8.6 | 3.16 |
| MH | 83.8 | 5.4 | 8.4 | — | 52.8 | 8.8 | 1.51 |
| MH2c | 75.5 | 7.6 | 14.1 | — | 50.5 | 7.9 | 1.29 |
| MI | 44.0 | 6.7 | 16.5 | — | — | — | — |
| MJ | 52.7 | 6.7 | 11.2 | 22.5 | 51.8 | 7.4 | 1.07 |
| SA | 48.2 | 5.8 | — | — | 5.7 | 10.0 | 0.46 |
| SB | 29.2 | 5.1 | 23.1 | — | 23.7 | 25.4 | 3.96 |
| SC | 76.6 | 13.6 | — | — | 41.8 | 14.4 | 3.82 |
| SD | 63.7 | 3.5 | — | — | 62.2 | 15.7 | 5.25 |
| SE | 70.8 | 7.4 | 25.2 | 20.4 | 33.1 | 19.8 | 2.91 |
| SF | 64.5 | 3.2 | — | — | 43.5 | 9.9 | 1.68 |
| SG | 42.1 | 7.3 | — | — | 20.1 | 21.4 | 1.83 |
| SH | 105.0 | 4.4 | — | — | 61.0 | 13.1 | 4.86 |
| SI | 18.5 | 0.8 | — | — | 16.9 | 10.2 | 0.93 |
| SJ | 183.4 | 14.1 | — | — | — | — | — |
| NS | — | 4.9 | 4.8 | — | 26.0 | — | — |
| Meand | 63.2 | 6.7 | 22.3 | 28.5 | 47.9 | 11.2 | 2.34 |
| SDd | 29.4 | 5.7 | 20.7 | 18.4 | 21.5 | 5.1 | 1.41 |
IDs starting with “L”, “M”, and “S” indicate large, medium, and small casinos, respectively. “NS” is the only non-smoking casino.
Sampling and counting took place only in a portion of the casino, of an undetermined area.
Second visits for four casinos.
Calculated only for smoking casinos.
PM2.5 Concentrations in Smoking Areas
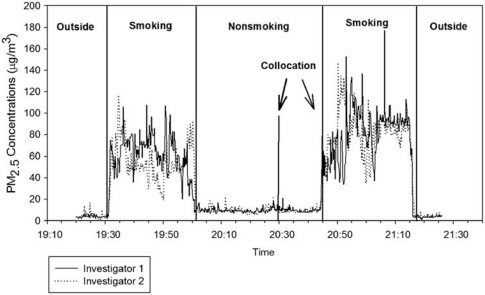
Figure 2 shows an example of the PM2.5 concentrations as a function of time measured in a casino. As the two investigators moved independently through the smoking areas, momentary differences in concentrations were substantial; however, the average values for each location were quite similar.
Figure 2.
A time-series plot illustrating the sampling protocol performed by two investigators visiting three locations in a casino.
The mean PM2.5 concentration over 0.5–1 h in the smoking sections ranged from 18 to 183 μg/m3 and averaged 63 μg/m3, with 50% of the visits exceeding 50 μg/m3; 20% exceeding 80 μg/m3; and 5% exceeding 100 μg/m3. The average PM2.5 concentrations in smoking areas among the three casino sizes were not significantly different.
Results from duplicate visits to four casinos (LE, LH, MB, and MH, Table 1) showed variations in indoor PM2.5 concentrations between visits. These may be attributable, for example, to changes in smoking activity and/or occupancy immediately before the sampling events, which would change the initial background PM2.5 level. Three of the four first visits involved sampling and counting in just a portion of the casino; thus spatial heterogeneity could also be a factor.
Shorter-term exposures ranged much higher. For example, the maximum 1-min PM2.5 concentrations in casino smoking areas ranged from 44 to 291 μg/m3, with an average of the maxima of 116 μg/m3 (SD=55 μg/m3). The maximum 1-min concentrations were 12–223 μg/m3 higher than the 0.5–1 h mean concentrations for the 39 visits in casino smoking areas (Supplementary Table S1).
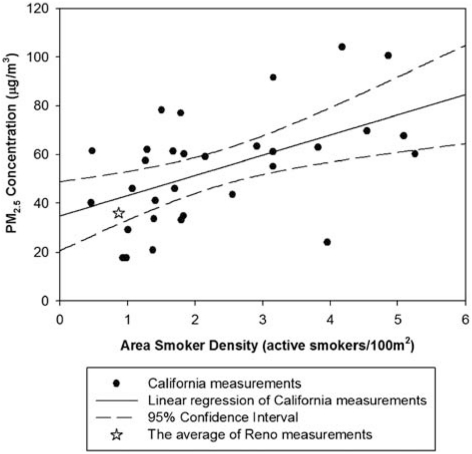
The relationship between average incremental concentrations (concentration greater than the outdoors) in smoking areas and the area smoker densities is shown in Figure 3. Significant scatter in the data was expected due to differences in building characteristics that were not measured, such as the ventilation rate and ceiling heights. The linear regression results indicated area smoker density was positively associated with incremental smoking PM2.5 concentrations in California casinos with r=0.52. This result implied that 27% of the variation in the incremental PM2.5 concentrations could be explained by the area smoker density (R2=0.27; n=31).
Figure 3.
Linear regression analysis of incremental PM2.5 concentrations (concentrations above the outdoor levels) in the smoking areas of California casinos versus area smoking densities (n=31). Regression equation: PM2.5 concentration=8.3 × (area smoker density)+34.7 (R2=0.27; r=0.52). The star symbol represents the average incremental PM2.5 concentration for the average smoker density observed in seven Reno smoking casinos.
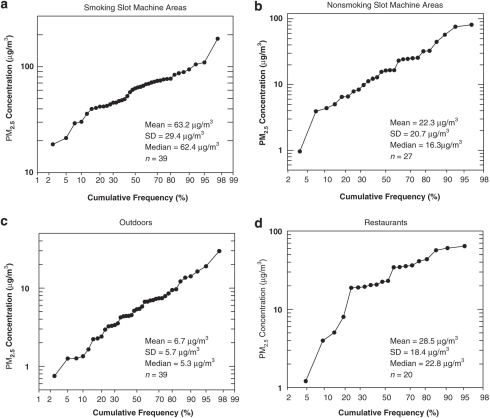
Figure 4 shows frequency distributions of the average PM2.5 measurements from the casinos at four locations: (1) smoking slot machine areas, (2) non-smoking slot machine areas, (3) outdoors, and (4) restaurants. The relative straightness of the frequency distributions in locations (1), (2), and (3) indicated a tendency toward a lognormal distribution. With the exception of one outlier, indoor smoking concentrations could be treated as normally distributed, but outdoor data did not fit a normal distribution (Shapiro–Wilks test; P<0.001). The distribution of the relatively small sample of restaurant data (n=20) appeared neither normal nor lognormal.
Figure 4.
Frequency distribution plots for PM2.5 concentrations in the (a) smoking areas, (b) non-smoking areas, (c) outdoors, and (d) restaurants of the 39 visits to 35 smoking Indian casinos in California.
Comparison of Smoking Versus Non-smoking Areas
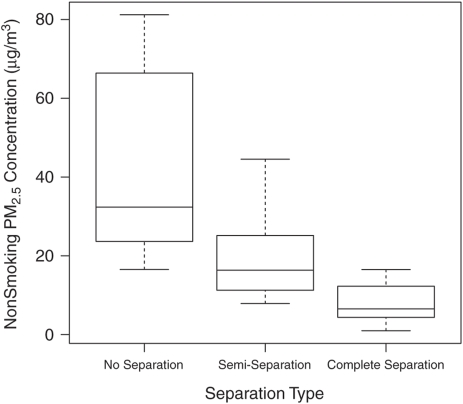
In 23 of the 35 smoking casinos, there were signs marking slot machine areas prohibiting smoking. The average PM2.5 concentration in the non-smoking areas was 22 μg/m3 (range, 1–81 μg/m3). We compared three methods of separation from the smoking areas: (1) no physical separation — the non-smoking section was not in a separate room; (2) semi-separation — a separate non-smoking room but no closing doors; and (3) complete physical separation — a separate room with closing doors. The average PM2.5 levels shown in Figure 5 for non-smoking areas with no separation (43 μg/m3, n=8) and with semi-separation (20 μg/m3, n=9) were significantly higher than in areas with complete separation (7.9 μg/m3, n=10) (one-way ANOVA, P<0.05).
Figure 5.
Box plots comparing average PM2.5 levels in casino non-smoking gaming areas stratified by three separation methods. Boxes represent the interquartile range (25th–75th percentiles, median indicated by horizontal line), and whiskers extend to the 5th and 95th percentiles.
On average, the PM2.5 concentration in casino gaming areas with smokers was 36 μg/m3 higher than in non-smoking gaming areas. In non-smoking areas with no separation, the average PM2.5 concentration was not significantly lower than the adjacent smoking areas. In contrast, PM2.5 concentrations in semi-separated or completely separated non-smoking areas were significantly lower than in the nearby smoking areas (paired t-test, P<0.01).
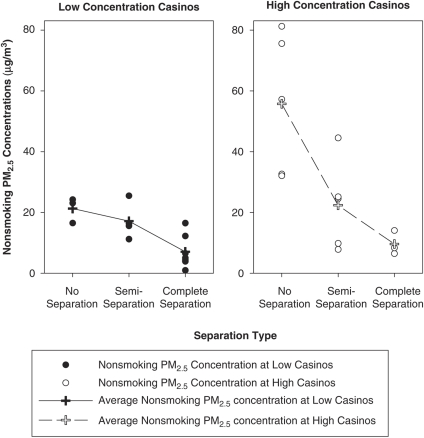
For those casinos that have both smoking and non-smoking slot machine areas (n=27), we examined how strongly the smoking areas affected the nearby non-smoking areas. We chose 60 μg/m3, a value close to the median (57.4 μg/m3) to subdivide these casinos into two groups of approximately equal size: the low concentration casinos (n=14) had average PM2.5 levels below 60 μg/m3 in the smoking areas, and the high concentration casinos (n=13) were above 60 μg/m3 in the smoking areas (Figure 6). For all three non-smoking separation types, low concentration casinos had the lower average PM2.5 levels. The difference in the average non-smoking PM2.5 level between low concentration casinos and high concentration casinos was greatest for areas with no separation, and smallest for areas with complete physical separation. Thus, PM2.5 levels in smoking areas had a greater impact on adjacent non-smoking areas if no physical barriers existed between the two sections.
Figure 6.
Interaction effects of PM2.5 levels in casino smoking areas and three methods of separating the non-smoking areas on PM2.5 levels in casino non-smoking gaming areas. Average PM2.5 concentrations in smoking slot machine areas for low concentration casinos were below 60 μg/m3 and for high concentration casinos were above 60 μg/m3.
PM2.5 Concentrations for Outdoors, Restaurants, Other Locations
The PM2.5 concentrations measured outdoors averaged 7 μg/m3; with one exception (during a nearby forest fire), all outdoor locations were below 19 μg/m3 (Table 1). On average, the PM2.5 concentration in indoor smoking areas was 56 μg/m3 higher than outdoors. Compared with outdoor measurements, the average PM2.5 concentration in non-smoking areas was 36 μg/m3 higher for no separation, 12 μg/m3 higher for semi-separation (both statistically significant, P<0.01), and 1 μg/m3 higher for complete separation (not statistically significant).
The mean PM2.5 level of 29 μg/m3 in the non-smoking restaurants (n=20), where children were often present, was 22 μg/m3 above the average outdoor concentration, and 7 μg/m3 higher than the non-smoking gaming areas.
In three of the smoking casinos, the mean PM2.5 concentrations in non-smoking poker rooms were 64, 22, and 14 μg/m3. Other non-smoking locations measured included a casino delicatessen (11 μg/m3), bowling alley (31 μg/m3), and bingo room (10 μg/m3).
A Smoke-Free Casino
There was one small casino in California that banned smoking indoors (see star symbol on map in Figure 1). The average PM2.5 level inside this casino was 5.4 μg/m3, comparable to the mean outdoor concentration (5.5 μg/m3). The indoor PM2.5 level in this smoke-free casino was less than 1/10th the average in the smoking areas of the 35 other casinos, and 1/4th the average in the non-smoking areas of the casinos that allowed smoking.
PM2.5 Concentrations in Reno Casinos
To initially explore, using the same sampling and monitoring protocol, whether the relationship seen in the California casinos between incremental PM2.5 concentrations and area smoker density might hold for other locations, we also measured eight non-Indian casinos in Reno, including one smoke-free casino (Supplementary Tables S2 and S3).
For the seven Reno smoking casinos, the average PM2.5 level in the smoking areas during weekend evenings was 37 μg/m3, 30 times as high as outdoors (1.2 μg/m3). The restaurants averaged 17 μg/m3 (n=5). The mean PM2.5 levels for designated non-smoking areas were 10 and 7 μg/m3 for two areas with semi-separation, lower than in one other area with no physical separation (22 μg/m3). Casino occupancy averaged 38% (range, 31–49%), active smoking prevalence averaged 10% (range, 7–12%), and area smoker density averaged 0.9 active smokers/100 m2 (range, 0.4–1.3 active smokers/100 m2). Temperature and relative humidity inside these casinos were 70–75°F and 20–30%, respectively.
The average PM2.5 concentration inside the one non-smoking Reno casino was 0.6 μg/m3, compared with an average outdoor concentration of 1.2 μg/m3; the occupancy was 20%.
We compared the PM2.5 concentrations in the smoking areas of Reno casinos to California casinos, accounting for smoker density (Figure 3). The average incremental smoking concentration of Reno casinos (shown as a star) falls within the 95% confidence interval about the mean for the California casinos. Thus, when the effects of outdoor concentrations and smoker density are included, the average PM2.5 concentration measured in smoking areas of these Reno casinos is consistent with the relationship for the means of California casinos.
Discussion
The active smoking prevalence averaged 11% for California casinos and 10% for Reno casinos, higher than the average of 8.5% in a Delaware casino (Repace, 2004), and 7% at casinos in Las Vegas, Reno, and Lake Tahoe (Pritsos et al., 2008) and in Pennsylvania (Repace, 2009). Repace (2009) estimates the “adult smoking prevalence” as three times the active smoking prevalence, making the adult smoking prevalence in California smoking casinos much higher than the state's adult smoking prevalence of 13% (CDPH, 2008).
We found a positive correlation between area smoker density and incremental PM2.5 concentration. However, the area smoker density alone is not sufficient to predict incremental PM2.5 concentrations. Measurements of other building characteristics, such as the ventilation rates and ceiling heights, are necessary to better interpret indoor PM2.5 levels. For example, Repace (2009) has used the indoor and outdoor CO2 difference, along with occupancy counts, to assess ventilation rates in casinos, and the results suggest that the PM2.5 concentration is inversely proportional to the ventilation rate per occupant. In an unpublished analysis, Repace and coworkers found that the R2 value of the regression between incremental PM2.5 concentrations and the ratio of smoker density to ventilation rate per occupant was close to 0.8 (n=7). Measuring CO2 concentrations and including ventilation estimates in regression analysis is expected to improve our ability to explain variation in PM2.5 levels.
The only short-term U.S. EPA National Air Quality Standard for PM2.5 is a 24-h standard for ambient (outdoor) levels, set at 35 μg/m3. We found that 90% of the average 0.5–1 h PM2.5 concentrations measured on weekend and holiday evenings in the smoking areas of California casinos exceeded 35 μg/m3. If we consider the highest 1 h average PM2.5 concentration of 183 μg/m3 measured in a casino smoking area, a person (such as an employee) spending 8 h in the casino with zero exposure for the remaining 16 h would experience a 24-h exposure of 61 μg/m3, well above the U.S. EPA standard.
The range of mean PM2.5 concentrations for the California casino smoking areas was similar to the range for three Las Vegas (CDC, 2009), one Delaware (Repace, 2004), and three Pennsylvania casinos (Repace, 2009). Variations among study sites were expected due to differences in smoker densities, ventilation, and building characteristics. Variations in PM2.5 for duplicate visits to a given study site also were expected, and were observed for four casinos. In addition to variables such as smoker activity, occupancy, and spatial heterogeneity, differences in the initial indoor concentrations (e.g. due to higher or lower smoking activity before the start of sampling) could also contribute. Ott et al. (1996) also found substantial variability in respirable particle concentrations for 26 visits to a sports tavern that allowed smoking.
The fine particle levels we observed in casino smoking areas were also comparable to levels previously observed in other public places. For example, the study measuring PM3.5 on 26 visits to a sports tavern before the California smoking ban yielded concentrations of 25–180 μg/m3 with an incremental mean concentration of 57 μg/m3 (Ott et al., 1996), almost identical to the incremental mean concentration of 56 μg/m3 for our Indian casinos. In Italy, before a smoking ban, average PM2.5 concentrations included 47 μg/m3 in 14 bars, 111 μg/m3 in 12 restaurants, and 150 μg/m3 in 8 video game parlors (Valente et al., 2007). A German study reported median PM2.5 levels of 178 μg/m3 for 11 restaurants, and 192 μg/m3 for 7 pubs (Bolte et al., 2008). In smoking areas of two coffee shops in Taiwan, median PM2.5 concentrations were 106 and 80 μg/m3 (Lung et al., 2004). In UK bars and pubs with mechanical ventilation, the median PM2.5 concentration was 57 μg/m3 when smoking was allowed (Carrington et al., 2003). In Texas, before a smoking ban, the average PM2.5 level was 151 μg/m3 in 17 bars (Waring and Siegel, 2007).
Our findings indicate that non-smoking areas with no physical barriers provided little protection from exposures to SHS; this has also been reported for other public locations (Cains et al., 2004; Lung et al., 2004). Designating separate rooms as non-smoking areas, especially with closed doors, was somewhat effective in reducing PM2.5 levels. However, for 23 of 27 visits, the mean PM2.5 levels in indoor non-smoking areas were higher than outdoors. Similarly, Cains et al. (2004) reported that separated non-smoking rooms in Australian social and gaming clubs reduced PM10 concentrations more than non-smoking areas contiguous with the smoking areas. Other previous studies (Carrington et al., 2003; Cenko et al., 2004) have concluded that a separated ventilation system was not effective, and that exposure to SHS in non-smoking areas may still represent an appreciable health risk.
Determining exposure is essential for assessing health effects. There has been increasing interest in health effects associated with very short-term (i.e. a few minutes) exposure to SHS (Barnoya and Glantz, 2005). In 2001, Pope et al. found that a 2-h exposure to SHS with an average PM3 level of 78 μg/m3 was associated with decrements in heart rate variability and increased cardiac vulnerability. In our study, 7 out of 39 casino visits of 0.5–1 h had mean PM2.5 concentrations higher than 78 μg/m3. A comprehensive review (Pope and Dockery, 2006) found evidence that a 20 μg/m3 increase in long-term average outdoor PM2.5 concentration is associated with a 20% increase in cardiopulmonary mortality. If the toxicity of PM2.5 from SHS is similar to outdoor PM2.5, then frequent exposure to the average elevation of 56 μg/m3 observed in smoking areas of California casinos is likely to be associated with significant increases in adverse health effects.
Conclusions
PM2.5 concentrations in the smoking areas of 35 smoking Indian casinos in California averaged 63 μg/m3, 3 times as high as in the non-smoking areas (22 μg/m3), 2 times as high as in casino restaurants (29 μg/m3), and >10 times as high as in the smoke-free casino (5.4 μg/m3). These results, taken together, strongly indicate that SHS is the predominant cause of elevated PM2.5 concentrations in the casinos sampled. In addition, we found:
Average concentrations in indoor smoking areas, non-smoking areas, and restaurants were, respectively, 56, 15 and 22 μg/m3 above outdoor levels.
In contrast, the two non-smoking casinos measured (one in Reno and one in California) had indoor concentrations that were as low as outdoors.
For 90% of the casino visits, mean concentrations in smoking areas averaged over 0.5–1 h exceeded 35 μg/m3.
Separated non-smoking rooms with closing doors had lower PM2.5 concentrations than rooms with open doors or non-smoking areas with no physical separation.
The indoor PM2.5 mean concentration of 7 Reno non-Indian casinos was consistent with mean concentrations in the smoking areas of 35 California Indian casinos when adjusted for outdoor levels and area smoker density.
The results of this study represent PM2.5 concentrations measured in single visits on weekend and holiday evenings in slot machine areas and restaurants of California Indian casinos. As our results illuminate the potential health risks for people spending time inside smoking casinos, they are valuable to casino workers, unions, owners, the general public, and government agencies, who make decisions on smoking bans. Exposure to the average elevation of 56 μg/m3 observed in smoking areas of California casinos is likely to be associated with significant increases in adverse health effects. In addition to characterizing PM2.5 concentrations at other times and locations, future studies should more intensively examine casino worker exposures, the impact of building characteristics, and particle levels before-and-after smoking bans.
Acknowledgments
We acknowledge the Flight Attendant Medical Research Institute for supporting this research, and Le verne McClure, John Moye and Thivanka Muthumalage for sampling some casinos. This paper represents the views of the authors and not necessarily those of the sponsor. Mention of commercial products does not constitute endorsement or recommendation.
Mr. Repace is an international secondhand smoke consultant to governmental and private entities, and has served as an expert witness in litigation between workers injured by secondhand smoke and casinos, as well as the tobacco industry. The other authors declare no conflict of interest.
Supplementary Material
References
- Abrams S., Mahoney M., Hyland A., Cummings M., Davis W., Song L. Early evidence on the effectiveness of clean indoor air legislation in New York State. Am J Public Health. 2006;96:296–298. doi: 10.2105/AJPH.2004.055012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson K., Kliris J., Murphy L., Carmella S., Han S., Link C., et al. Metabolites of a tobacco-specific lung carcinogen in nonsmoking casino patrons. Cancer Epidem Biomar. 2003;12:1544–1546. [PubMed] [Google Scholar]
- ANRF (American Nonsmokers' Rights Foundation) Smoke-free lists, maps and dataAvailable at http://www.no-smoke.org accessed 11 May 2009, 2009
- Barnoya J., Glantz S. Cardiovascular effects of secondhand smoke nearly as large as smoking. Circulation. 2005;111:2684–2698. doi: 10.1161/CIRCULATIONAHA.104.492215. [DOI] [PubMed] [Google Scholar]
- Bolte G., Heitmann D., Kiranoglu M., Schierl R., Diemer J., Koerner W., Fromme H. Exposure to environmental tobacco smoke in German restaurants, pubs, and discotheques. J Expo Sci Environ Epidemiol. 2008;18:262–271. doi: 10.1038/sj.jes.7500590. [DOI] [PubMed] [Google Scholar]
- Brennan P., Buffler P.A., Reynolds P., Wu A.H., Wichmann H.E., Agudo A., et al. Secondhand smoke exposure in adulthood and risk of lung cancer among never smokers: a pooled analysis of two large studies. Int J Cancer. 2004;109:125–131. doi: 10.1002/ijc.11682. [DOI] [PubMed] [Google Scholar]
- Cains T., Cannata S., Poulos R., Ferson M.J., Stewart B.W. Designated “no smoking” areas provide from partial to no protection from environmental tobacco smoke. Tob Control. 2004;13:17–22. doi: 10.1136/tc.2003.005488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- California EPA (Environmental Protection Agency) Proposed identification of environmental tobacco smoke as a toxic air contaminantAvailable at http://www.arb.ca.gov/regact/ets2006/ets2006.htm accessed 8 December 2008, 2006
- Carrington J., Watson A., Gee I. The effects of smoking status and ventilation on environmental tobacco smoke concentrations in public areas of UK pubs and bars. Atmos Environ. 2003;37:3255–3266. [Google Scholar]
- CDC Environmental and biological assessment of environmental tobacco smoke exposure among casino dealers. Health Hazard Evaluation ReportAvailable at http://www.cdc.gov/niosh/hhe/ accessed 9 June 2009, 2009
- CDC (Center for Disease Control and Prevention) Annual smoking-attributable mortality, years of potential life lost, and productivity losses—U.S., 1997–2001. MMWR. 2005;54:625–628. [PubMed] [Google Scholar]
- CDPH (California Department of Public Health Services) California adult smoking prevalenceAvailable at http://www.cdph.ca.gov accessed 28 May 2009, 2008
- Cenko C., Pisaniello D., Esterman A. A study of environmental tobacco smoke in south Australian pubs, clubs and cafes. Int J Environ Heal R. 2004;14:3–11. doi: 10.1080/09603120310001633903. [DOI] [PubMed] [Google Scholar]
- Dunstan R.Indian casinos in California. California State LibraryAvailable at http://www.library.ca.gov/crb/98/15/98015.pdf accessed 25 August 2009, 1998
- Hammond S.K. Exposure of U.S. workers to environmental tobacco smoke. Environ Health Perspect. 1999;107 (Suppl 2:329–340. doi: 10.1289/ehp.99107s2329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hyland A., Travers M.J., Dresler C., Higbee C., Cummings K.M. A 32-country comparison of tobacco smoke derived particle levels in indoor public places. Tob Control. 2008;17:159–165. doi: 10.1136/tc.2007.020479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kado N.Y., Mccurdy S.A., Tesluk S.J., Hammond S.K., Hsieh D., Jones J., et al. Measuring personal exposure to airborne mutagens and nicotine in environmental tobacco smoke. Mutat Res. 1991;261:75–82. doi: 10.1016/0165-1218(91)90100-z. [DOI] [PubMed] [Google Scholar]
- Koh H., Joossen L., Connolly G. Making smoking history worldwide. N Engl J Med. 2007;365:1496–1498. doi: 10.1056/NEJMp068279. [DOI] [PubMed] [Google Scholar]
- Larsson M., Boëthius G., Axelsson S., Montgomery S. Exposure to environmental tobacco smoke and health effects among hospitality workers in Sweden – before and after the implementation of a smoke-free law. Scand J Work Environ Health. 2008;34:267–277. doi: 10.5271/sjweh.1243. [DOI] [PubMed] [Google Scholar]
- Lee K., Hahn E., Okoli C., Repace J., Troutman A. Differential impacts of smoke-free laws on indoor air quality. J Environ Health. 2008;40:24–30. [PubMed] [Google Scholar]
- López M.J., Nebot M., Albertini M., Birkui P., Centrich F., Chudzikova M., et al. Secondhand smoke exposure in hospitality venues in Europe. Environ Health Perspect. 2008;116:1469–1472. doi: 10.1289/ehp.11374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lung S.C.C., Wu M.J., Lin C.C. Customers' exposure to PM2.5 and polycyclic aromatic hydrocarbons in smoking/nonsmoking sections of 24-h coffee shops in Taiwan. J Expo Anal Environ Epidemiol. 2004;14:529–535. doi: 10.1038/sj.jea.7500371. [DOI] [PubMed] [Google Scholar]
- Nazaroff W.W., Singer B.C. Inhalation of hazardous air pollutants from environmental tobacco smoke in US residences. J Expo Anal Environ Epidemiol. 2004;14:S71–S77. doi: 10.1038/sj.jea.7500361. [DOI] [PubMed] [Google Scholar]
- Ott W., Switzer P., Robinson J. Particle concentrations inside a tavern before and after prohibition of smoking: evaluating the performance of an indoor air quality model. J Air Waste Manage Assoc. 1996;46:1120–1134. doi: 10.1080/10473289.1996.10467548. [DOI] [PubMed] [Google Scholar]
- Pilkington P., Gray S., Gilmore A. Health impacts of exposure to second hand smoke (SHS) amongst a highly exposed workforce: survey of London casino workers. BMC Public Health. 2007;7:257–264. doi: 10.1186/1471-2458-7-257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pope C.A., Dockery D.W. Health effects of fine particulate air pollution: lines that connect. J Air Waste Manage Assoc. 2006;56:709–742. doi: 10.1080/10473289.2006.10464485. [DOI] [PubMed] [Google Scholar]
- Pope C.A., Eatough D.J., Gold D.R., Pang Y., Nielsen K.R., Nath P., et al. Acute exposure to environmental tobacco smoke and heart rate variability. Environ Health Perspect. 2001;109:711–716. doi: 10.1289/ehp.01109711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pope C.A., Ezzati M., Dockery D. Fine-particulate air pollution and life expectancy in the United States. N Engl J Med. 2009;360:376–386. doi: 10.1056/NEJMsa0805646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pritsos C.A., Pritsos K.L., Spears K.E. Smoking rates among gamblers at Nevada casinos mirror US smoking rate. Tob Control. 2008;17:82–85. doi: 10.1136/tc.2007.021196. [DOI] [PubMed] [Google Scholar]
- R Development Core Team . R: A Language and Environment for Statistical Computing. Version 2.5.1. Vienna, Austria; 2008. [Google Scholar]
- Repace J. Respirable particles and carcinogens in the air of Delaware hospitality venues before and after a smoking ban. J Occup Environ Med. 2004;46:887–905. doi: 10.1097/01.jom.0000141644.69355.52. [DOI] [PubMed] [Google Scholar]
- Repace J. Secondhand smoke in Pennsylvania casinos: a study of nonsmokers' exposure, dose, and risk. Am J Public Health. 2009;99:1478–1485. doi: 10.2105/AJPH.2008.146241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegel M., Skeer M. Exposure to secondhand smoke and excess lung cancer mortality risk among workers in the “5 B's”: bars, bowling alleys, billiard halls, betting establishments and bingo parlours. Tob Control. 2003;12:333–338. doi: 10.1136/tc.12.3.333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Surgeon General U.S. Department of Health and Human Services. The health consequences of involuntary exposure to tobacco smoke: a report of the Surgeon GeneralAvailable at http://www.surgeongeneral.gov/library accessed 9 May 2009, 2006 [PubMed]
- Trout D., Decker J., Mueller C., Bernett J., Pirkle J. Exposure of casino employees to environmental tobacco smoke. J Occup Environ Med. 1998;40:270–276. doi: 10.1097/00043764-199803000-00009. [DOI] [PubMed] [Google Scholar]
- TSI Model AM510 SidePak™ Personal Aerosol Monitor User Guide, 1980456, Revision F. Shoreview, MN: TSI IncorporatedAvailable at http://www.tsi.com/uploadedFiles/Product_Information/Literature/Manuals/SidePak_AIM510-1980456f.pdf accessed 24 November 2009, 2008
- U.S. EPA Particulate matter standardsAvailable at http://www.epa.gov accessed 9 May 2009, 2006
- Valente P., Forastiere F., Bacosi A., Cattani G., Di Carlo S., Ferri M., et al. Exposure to fine and ultrafine particles from secondhand smoke in public places before and after the smoking ban, Italy 2005. Tob Control. 2007;16:312–317. doi: 10.1136/tc.2006.019646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wakefield M., Cameron M., Inglis G., Lecher T., Durkin S. Secondhand smoke exposure and respiratory symptoms among casinos, club and office workers in Victoria, Australia. J Occup Environ Med. 2005;47:698–703. doi: 10.1097/01.jom.0000167285.33870.f9. [DOI] [PubMed] [Google Scholar]
- Waring M.S., Siegel J.A. An evaluation of the indoor air quality in bars before and after a smoking ban in Austin, Texas. J Expo Anal Environ Epidemiol. 2007;17:260–268. doi: 10.1038/sj.jes.7500513. [DOI] [PubMed] [Google Scholar]
- WHO (World Health Organization) Framework convention on tobacco controlAvailable at http://www.who.int/fctc/en/ accessed 27 May 2009, 2009
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.