Abstract
Background
Low health literacy has been identified as an independent predictor of poor asthma control. The Institute of Medicine considers the role of information technology (IT) as critical in providing “safe, effective, patient centered, timely, efficient, and equitable” care with the potential to reduce health disparities in underserved populations. The aim of this study was to design and evaluate an interactive computer-based questionnaire to assess asthma symptoms in children of parents with limited health literacy and/or limited English proficiency.
Methods
Volunteer caregivers attending a mobile asthma clinic were randomly assigned to complete the electronic or the paper-and-pencil version of an asthma screening questionnaire (ASQ) in their language of choice (English or Spanish). In the electronic version, a tablet computer was used to present the ASQ questions as video clips and to collect information through the touchscreen. Participants also completed a demographic questionnaire, a brief health literacy questionnaire, and a system usability and satisfaction questionnaire. Reliability of the paper and electronic self-assessments was evaluated by comparing each participant’s answers to information they provided during a nurse-guided structured interview (gold standard).
Results
A total of 48 parents participated in the study, 26 completed the electronic ASQ and 21 the paper-and-pencil form. Thirty-five percent of the children had well-controlled asthma (n = 17). Most participants were Spanish speaking (67%) Hispanic (n = 44) mothers (n = 43) with a median age of 32 years. More than half had ≤8 years of education (n = 25) and earned <$20,000 per year (n = 27). The median health literacy score was 32 (range 0 36). The correlation between health literacy scores and years of education was significant (p = .47, p < .01). Concordance between the electronic ASQ and the nurse interview was significantly higher than concordance between the paper ASQ and the nurse interview (68% versus 54%; p < .01). All parents who completed the electronic questionnaire reported being satisfied; 96% felt comfortable using it, and found it simple to use.
Conclusions
By facilitating the assessment of asthma symptoms at manageable cost, interactive information technology tools may help reduce barriers to access due to inadequate levels of English proficiency and health literacy.
Keywords: asthma, children, computer-based assessment, English proficiency, health literacy, parents, self-report
Introduction
Asthma is the most common chronic disease of childhood, with more than 6 million children affected (1,2). During the last three decades, the prevalence and morbidity of asthma have increased in the United States. Extensive research has shown that adverse asthma outcomes are a product of complex interactions of environmental, economic, and social factors, particularly among disadvantaged populations (3, 4). In addition, it has been suggested that many of the asthma disparities observed between patient groups are a product of these complex interactions (5–7). Among other factors, low health literacy has been identified as an independent predictor of poor asthma control (8,9). To fully address health disparities, investigators suggest that in addition to the management of asthma symptoms, other factors such as differences in education and literacy, income, and access to health services should be addressed (5–7).
Results from the National Adult Literacy Survey suggest that approximately 44 million Americans are functionally illiterate in the English language, and another 50 million have marginal literacy skills (10). This means that almost half of the adult population experiences some difficulty reading, speaking, writing, and using basic arithmetic in everyday life situations. Health literacy, the series of skills necessary to deal effectively with the health care system, seems to be considerably poorer than general literacy, in part because of unfamiliarity of many patients with the context and vocabulary specific to the health care system (4). Low health literacy may impact health care costs by leading to ineffective health care, which in turn results in poorer outcomes and higher hospitalization rates (10). Among other factors, low health literacy has been identified as a predictor of poor asthma control mediated by lack of adequate asthma knowledge and inadequate self-care (8). Although the majority of adults with poor literacy are Caucasian, 45% of Americans with limited health literacy are members of racial and ethnic minority groups (9–12). Further, barriers to health care, poorer health outcomes, and less overall satisfaction with the health care system have been consistently reported for Latino patients with limited English proficiency (LEP; 13–20). For example, concerns regarding their ability to communicate prevent many LEP patients from seeking care when sick (21), thus placing them at increased risk.
The Institute of Medicine’s Committee on Quality of Health Care recently identified the role of information technology (IT) as critical in creating a health system capable of providing care that is “safe, effective, patient centered, timely, efficient, and equitable,” as well as one that has the potential of reducing health disparities in underserved populations (22, 23). As an example, consider that for patients with low literacy skills who require substantially more assistance from health care providers to achieve the same level of care attained by high literacy patients, information technology can provide personalized assistance and instruction at a relatively low cost. Many patients with LEP require the services of professional interpreters not always available to health care agencies. Such increased level of support entails higher costs for health providers and acts as a major barrier to health care for patients (24, 25). Information technology can be effectively used to provide the extra level of support these patients need. For example, projects such as Baby CareLink, the Columbia University Informatics for Diabetes Education and Telemedicine (IDEATel) Project, and others (26–33) have demonstrated the feasibility and acceptability of e-health interventions for information and communication with populations typically considered underserved.
In this study we tested a computerized multimedia application designed to present the parents of children with asthma with questions in the form of language-appropriate video clips, and to record their responses through a touchscreen, The goal was to minimize the parents’ need for reading and writing skills in providing accurate information about their children’s asthma symptoms. We hypothesized that using the interactive multimedia system would facilitate the screening processes by (1) reducing the amount of staff-time that would otherwise be required to collect accurate information; (2) reducing patients’ stress associated to reading and writing tasks during the medical visits; and (3) by generally improving patient satisfaction. The aims of this study were to evaluate the efficacy of an interactive computer-based multimedia system to assess asthma control and health care utilization in school children, and to assess the electronic system’s usability by a population characterized by low-literacy and low English proficiency.
Methods
We conducted a controlled study in which volunteer care-givers attending a mobile asthma clinic were randomly assigned the electronic or paper version of the Asthma Screening Questionnaire (ASQ). All participants were asked which language (English or Spanish) they preferred to use during the session. Then, the consenting process as well as questionnaires and all further interactions were conducted in their language of choice. The study protocol was approved independently by the institutional review boards of Arizona State University and the Phoenix Children’s Hospital. In compensation, all participants completing the assessments received a $25 gift certificate.
Sample and Setting
The Phoenix Children’s Hospital Breathmobile is a self-contained fully equipped mobile asthma clinic modeled after a Breathmobile program in Southern California (34). The clinic provides service to 19 public elementary schools in South Phoenix at their respective campuses with a team of asthma care specialists composed by the medical director (P.R.), a pediatric nurse practitioner (J.H.), a registered nurse, a respiratory therapist, and an operations coordinator. Children are identified and referred to the program by the school nurses, who also help coordinate appointments. The students at the targeted schools are mostly low-income, African American or Latino, and likely to be uninsured. The clinic staff sees approximately 70 patients per week during the school year. The service is free of charge and requires no physician referral. Once diagnosed, each child receives an asthma plan that includes education for asthma self-management, follow-up appointments, evaluations (lung function test), and 24-hour phone consultation as needed. The operations coordinator facilitates appointments and referrals, and processes requests for medication assistance programs for uninsured and indigent patients.
Procedure
During the first phase of the study we produced the video clips of all ASQ questions in both English and Spanish, implemented the electronic versions of the questionnaire, and the data collection forms. During the second phase, we conducted a pre-pilot test of the system to fine-tune the computer program, video clips, forms, and assessment procedures. During the pre-pilot, six consented participants completed the electronic version of the ASQ-e in their language of choice, provided demographic information, completed the Test of Functional Health Literacy in Adults (STOFHLA, short form), and completed a system usability and satisfaction questionnaire. Then, a registered nurse of the asthma clinic conducted a structured interview in which the questions contained in the ASQ were presented. As a result of the pre-pilot run, two minor changes (described below) were made to the program. Then, on the third phase, 41 more parent volunteers were consented and randomly assigned to receive either the electronic or the paper-and-pencil version of the ASQ. The information obtained through the structured interview served as the “gold standard” against which the information obtained by the electronic and paper forms of the ASQ was compared.
TOFHLA Short Form
The STOFHLA, a 7-minute test, with 36 reading comprehension items in two passages, is one of the most widely used health literacy assessments (35, 36), with a reliability coefficient of .97 and correlation with the Rapid Estimate of Adult Literacy in Medicine of .81 (37). It contains two passages: instructions for an upper gastrointestinal (GI) X-ray procedure, and the “Rights and Responsibilities” from a Medicaid application (35). The passages contain information about an upper gastrointestinal tract X-ray procedure, and the “Rights and Responsibilities” section from a Medicaid application, and have Gunning-Fox readability indices of fourth and tenth grade, respectively (35). The STOFHLA was developed and validated to provide a measure of functional health literacy to be used by health care providers and researchers. (35) Validation studies of the English and Spanish STOFHLA have found similar performance with strong positive associations with education and inverse associations with age (38, 39). Each selection is scored a “1” for correct or a “0” for incorrect and scores are summed over items to create a total score. Scores range from 0 to 36 with functional literacy cut-off points of 0–16 for inadequate, 17–22 for marginal, and 23–36 for adequate functional literacy (37).
ASQ-e
This project used TouchHear!, a computer program developed by the research team (E.R.) to create and interactively present questionnaires such as the Asthma Screening Questionnaire. The program, written in Microsoft Visual Basic 6.0, presents one question at a time, and users can freely move back and forth between questions and make corrections as needed. Questions are presented in the form of video clips, which participants can replay as needed. The video clips featured a native female English or Spanish speaker, depending on the participant’s language of choice. A tablet computer (Toshiba Satellite model R15-S822) filled with noise canceling headphones (Sony model MDR-NC500D) and a stylus was used, and responses to all questions (multiple choice) were entered by touching the screen with the stylus. The computer was handed over to the participants in tablet mode, which hides the keyboard and mouse pad, and facilitates handling. The collected data are stored in two Microsoft Access tables, one containing subject and session information (entered by the experimenter) and one used to record responses to the questionnaire.
Usability
We used a modified version of the IBM Post Study System Usability Questionnaire (40). The questionnaire consisted of 12 statements (e.g., It was simple to use the computer; I was able to complete the tasks quickly using the computer; I felt comfortable using the computer; I felt hurried/rushed using the computer; Whenever I made a mistake using the computer, I could recover easily and quickly). The instructions provided with the computer were clear) with a 7-point Likert scale anchored at the end points, with the terms strongly agree for 1 and strongly disagree for 7.
Data Management and Analyses
Because the program underwent only minor changes during the pre-pilot assessment, data from all subjects were combined for the final analysis. All statistical analyses were performed using SPSS 16.0 (SPSS, Chicago IL). Descriptive statistics were computed for all data. Primary analyses included (1) concordance (reliability) and (2) usability and satisfaction ratings. Group comparisons were conducted using t tests for unpaired samples. Concordance scores were calculated by comparing the responses obtained during the interview (gold standard) with those obtained on the ASQ self-administered for the control group, or the computerized video form for the experimental group:
Concordance = number of agreements /(number of agreements + disagreements) ×100
A multiple regression analysis was conducted to identify other variables that could account for or predict the concordance score among demographic, literacy, and asthma management skills variables, in addition to the experimental group assignment. Thus, parent age, family income, number of children, preferred language, STOFHLA score or years of education, years managing symptoms, and group assignment were entered into the analysis.
Results
Study Sample
A total of 48 parents participated in evaluating the system, 26 completed the ASQ-e and 21 the original paper-and-pencil form. One parent discontinued her participation early due to an unrelated emergency and was not included in the analyses. Most participants were mothers (n = 43) of Hispanic ethnicity (n = 44), with a median age of 32 years (range 22–64). Thirty-two (66.7%) spoke only Spanish at home. More than half of the participants had 8 years of formal education or less (n = 25) and had a family income of less than $20,000 per year (n = 27). A large number of families shared a home with others, reporting a median of five people per household (range 2–10). The median number of children per family was three (range 1–4), ranging in age between 1 and 19 years (median 10 years).
Asthma Control
Asthma control was assessed following the National Heart, Lung, and Blood Institute (NHLBI) classification. For reference, the NHLBI classification (41) of asthma control is reproduced in Table 1. Children participating in the study had a physician diagnosis of asthma and most parents reported having managed their children’s symptoms for at least 1 year (n = 38). Thirty-three families had a single child with asthma (range 1–4). As shown in Table 2, 35% of the children had well-controlled asthma (n = 17); the most frequent impairment reported by parents was limitation of daily activities and/or participation in sports (not controlled, n = 31, 64.58%).
TABLE 1.
Classification of asthma control per NHLBI asthma guidelines (41) and ASQ.
| Components of control | Well controlled | Not well | Poorly controlled |
|---|---|---|---|
| Daytime symptoms | ≤2 day/week | >2 day/week | Daily |
| Nighttime symptoms | <l–2 times/month | 3 times/week | ≥4 times/week |
| Limit activities/sports | Never | Some 1–2 times/month |
Extreme ≥3 times/month |
| ED visits | None | 1–2 times/year | ≥3 times/year |
TABLE 2.
Asthma control per nurse interview (n = 48).
| Components of control impairment /risk (missing) |
Well controlled (%) |
Not well controlled (%) |
Poorly controlled (%) |
|---|---|---|---|
| Daytime symptoms (n = 2) | 40 (86.96) | 3 (6.52) | 3 (6.52) |
| Nighttime symptoms (n = 2) | 36 (78.26) | 4 (8.70) | 6 (13.04) |
| Limit daily activities (n = 2) | 22 (47.83) | 13 (28.26) | 11 (23.91) |
| Limit sports (n = 2) | 19 (41.30) | 13 (28.26) | 14 (30.43) |
| Risk: ED visits (n = 6) | 29 (69.04) | 7 (16.66) | 6 (14.28) |
| Overall* | 17 (35.42) | 13 (27.08) | 18 (37.50) |
A patient’s level of control is based on the most severe impairment category reported (41).
STOFHLA Score
Forty-seven parents completed the STOFHLA resulting in a median score of 32 (range 0–36). Most parents were classified as having adequate literacy skills (n = 34,72%). All but one of those who completed the questionnaire in English (who was scored as possessing marginal literacy) were classified as having adequate health literacy skills (n = 9). On the other hand, of the parents who chose Spanish (n = 37), 25 (68%) were classified as having adequate health literacy skills, 8 (22%) were classified as having marginal skills, and 4 parents were classified as having inadequate skills. Although health literacy scores were slightly lower in the ASQ-e group, the difference did not reach statistical significance (27.46 versus 29.0; p = .57). As expected, the correlation between individual STOFHLA scores and years of education was significant (Spearman rho = .47, p < .01).
Concordance
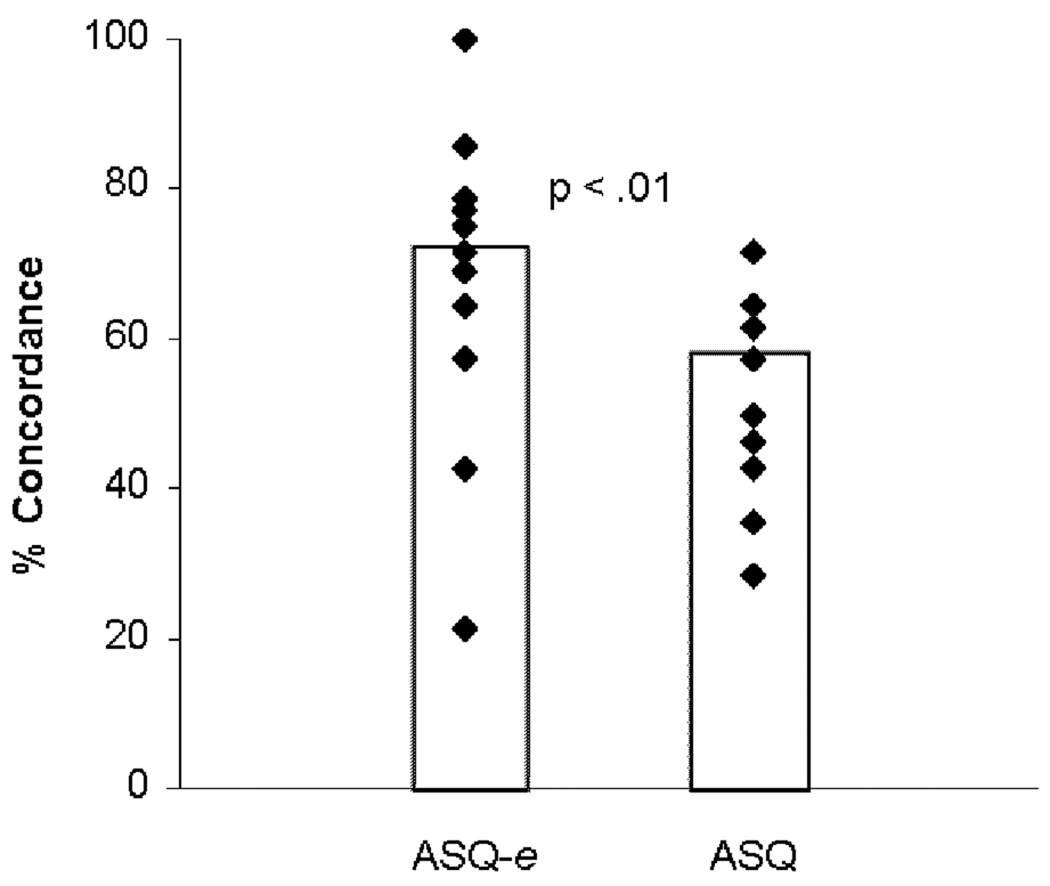
As shown in Figure 1, concordance between the electronic ASQ-e and the structured interview was significantly higher (68% versus 54%; p < .01) than that between the interview and the paper-and-pencil form.
Figure 1.
Concordance between the “Gold standard ”nurse interview and the electronic ASQ-e was significantly higher than the concordance for the paper-and-pencil ASQ from (68% versus 54%) Closed diamonds represent individual scores and bars represent group means.
Multiple regression was used to identify participant characteristics that might predict the observed concordance scores. Group assignment, demographic characteristics (i.e., parent’s age, years of education, family income, and number of children), health literacy score, language of choice, and years of asthma management experience were entered in the analysis as potential predictors. As shown in Table 3, of all the potential predictors entered, only the experimental group (ASQ versus ASQ-e; p < .01), age of the caregiver (p < .05), and years of education (p < .05) contributed significantly to the observed concordance score (percentage of agreements between responses recorded with the assigned form and responses provided during the interview). Health literacy scores correlated positively with years of education, but only years of education contributed significantly to the regression model. The resulting regression model fits the data well (p = .03), accounting for 43% of the variance.
TABLE 3.
Regression model with concordance score as outcome variable.
| Unstandardized coefficients |
Standardized coefficients |
||||
|---|---|---|---|---|---|
| Model | B | SE | Beta | t | Significance |
| Age | .702 | .337 | .364 | 2.084 | .048 |
| Years of education |
3.334 | 1.423 | .466 | 2.344 | .027 |
| Language | −10.239 | 7.007 | −.273 | −1.461 | .156 |
| Family income |
−1.963 | 4.051 | −.089 | −.485 | .632 |
| Number of children |
−1.132 | 2.325 | −.081 | −.487 | .631 |
| Years managing symptoms |
.976 | 2.542 | .064 | .384 | .704 |
| Group | −13.826 | 4.886 | −.446 | −2.830 | .009 |
Usability
Of the 24 parents who completed the ASQ-e, 95.8% found it simple to use, felt comfortable responding to questions, and found the screens and instructions clear and easy to understand. In addition, all of the participants reported liking the system, feeling comfortable using it, being willing to use it again, and being satisfied using both the computer and the program. Of the 11 people who made errors while attempting to complete the ASQ-e, only 1 reported not having been able to correct it. Twenty-five percent felt rushed using the system (n = 6) and 12% found it frustrating (n = 3).
Discussion
This study showed that there was better agreement between the answers provided with the electronic form of the questionnaire than the paper and pencil form when compared with those provided during the structured interview conducted by a nurse. Additionally, age and education level of the caregiver were found to contribute positively to the observed levels of concordance.
As expected, comparison of mean health literacy scores between the groups showed no significant differences. In addition, although there was a significant and expected correlation between literacy scores and self-reported years of education, only the latter contributed significantly to the observed levels of concordance. It is not entirely clear how being older acted to enhance concordance between the scores. It is possible, however, that older individuals might have more experience reporting health-related information, and more experience observing their children’s behavior and symptoms, and reporting to health care providers.
Satisfaction with the electronic system was overall extremely high and users rated the system’s usability as very good. Direct observation of the participants confirmed that there were few operational problems while completing the assessment, and that participants appeared not to be intimidated by the device; an issue we were most concerned about. This pilot study, however, identified some areas that need improvement. For example, on the assessment screen of the ASQ-e, it was some-times necessary to remind participants to touch the “Next” button to advance to the following question. Although too much prompting during execution of a computer program can be confusing and annoying, for this population it seems necessary to include a reminder to move to the next screen once a choice is made if 3 to 4 seconds go by before they touch on the “Next” button. Also, during pre-pilot assessment of the Spanish version, it became apparent that participants were confusing the capital letter “O” with a zero; so, we changed it to a lower case “o”, which completely resolved the matter. In the current version of the ASQ-e participants can freely move back and forth between the questions, a feature that generally facilitated correcting errors; however, this feature makes it possible to advance to the next question without having responded to the current one. Although this occurred on very few occasions during the study, the problem is entirely preventable. The computer program should be modified to limit browsing and editing to questions that have been previously answered.
The study has three notable limitations. One drawback of the study is the small sample size. In addition, because participation in the study was voluntary, it is possible that the results might have been affected by self-selection and social desirability bias effects. Finally, as with all self-reports, responding to the ASQ is susceptible to recall inaccuracies.
The electronic Asthma Screening Questionnaire yielded better concordance with the interview than the paper form, and was very acceptable to participants characterized by low levels of health literacy and/or low proficiency in the English language. These results are encouraging, and suggest that through the use of informational technology it may be possible to reduce some barriers to access, and limits in treatment efficacy that are due to inadequate levels of English literacy and health literacy. By limiting the cost involved in providing personal attention from health care providers and interpreters, IT-based systems may offer viable solutions to some well documented inequalities in health care. We believe that systems such as the one evaluated here can be further developed to integrate tailored asthma management assistance and freely available education in different settings, including physicians offices, clinics and emergency departments, as well as at home over the Internet.
Acknowledgments
This work was supported by Arizona State University (ASU) New College Research and Creative Activities Grant Program, and was conducted at the ASU–West Campus and the Phoenix Children’s Hospital Breath-mobile clinic. Support for Dr. Vargas was also provided by the National Institutes of Health/National Center on Minority Health and Health Disparities (P20 MD002316; solicited RFA MD-06-003 Establishing Exploratory NCMHD Centers of Excellence; http://grants.nih.gov/ grants/guide/rfa-files/RFA-MD-06-003.html)
We thank the parents who participated in the study and the Breathmobile staff: Gena Wilson, CPNP; Audrey Schoonmaker, RN; Sherry Hunkler, RRT; and Ramona Rodriguez for their invaluable help in the conduct of the study. We want to acknowledge the contribution of Peggy Radford, MD, and Judith Harris, CPNP, to the conception of this study, data analysis, and the final editing of the manuscript. We also acknowledge Elias Robles, PhD, and Perla A. Vargas, PhD, participation in the study design and implementation, data collection and analysis, and preparation of the manuscript. We thank Rebecca Wilson for her participation in producing the video clips.
Footnotes
Declaration of Interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- 1.National Heart, Lung, and Blood Institute. Morbidity and Mortality: 2002 Chart Book on Cardiovascular, Lung, and Blood Diseases. Washington, DC: US DHHS; 2002. [Google Scholar]
- 2.Centers for Disease Control. Measuring childhood asthma prevalence before and after the 1997 redesign of the National Health Interview Survey–United States. MMWR Morb Mort Wkly Rep. 2000;49:908–911. [PubMed] [Google Scholar]
- 3.Kirsch IS, Jungblut A, Jenkins L, Kolstat A. Adult Literacy in America: A First Look at the Result of the National Adult Literacy Survey. Washington, DC: National Center for Education Statistics, US Department of Education; 1993. [Google Scholar]
- 4.Chang C, Cella DF. Item reading difficulty and its impact on quality of life measurement. Qual Life. 1999;8:599. [Google Scholar]
- 5.Clement LT, Jones CA, Cole J. Health disparities in the United States: childhood asthma. Am J Med Sci. 2008;335:260–265. doi: 10.1097/maj.0b013e318169031c. [DOI] [PubMed] [Google Scholar]
- 6.Canino G, McQuaid EL, Rand CS. Addressing asthma health disparities: a multilevel challenge. J Allergy Clin Immunol. 2009;123:1209–1217. doi: 10.1016/j.jaci.2009.02.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Paasche-Orlow MK, Riekert KA, Bilderback A, Chanmugam A, Hill P, Rand CS, Krishnan J. Tailored education may reduce health literacy disparities in asthma self-management. Am J Respir Crit Care Med. 2005;172:980–986. doi: 10.1164/rccm.200409-1291OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Williams MV, Baker DW, Honig EG, Lee TM, Nowlan A. Inadequate literacy is a barrier to asthma knowledge and self-care. Chest. 1998;114:1008–1015. doi: 10.1378/chest.114.4.1008. [DOI] [PubMed] [Google Scholar]
- 9.DeWalt DA, Dilling MH, Rosenthal MS, Pignone MR. Low parental literacy is associated with worse asthma care measures in children. Ambul Pediatr. 2007;7:25–31. doi: 10.1016/j.ambp.2006.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Baker DW, Parker RM, Williams MV, Clark WS, Nurss J. The relationship of patient reading ability to self-reported health and use of health services. Am J Public Health. 1997;86:1027–1030. doi: 10.2105/ajph.87.6.1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Weiss BD, Reed RL, Kligman EW. Literacy skills and communication methods of low-income older persons. Patient Educ Couns. 1995;25:109–119. doi: 10.1016/0738-3991(95)00710-h. [DOI] [PubMed] [Google Scholar]
- 12.Kutner M, Greenberg E, Jin Y, Paulsen C. The Health Literacy of America’s Adults: Results from the 2003 National Assessment of Adult Literacy. Washington DC: U.S. Department of Education; 2006. [Google Scholar]
- 13.Derose KP, Baker DW. Limited English proficiency and Latinos’ use of physician services. Med Care Res Rev. 2000;57:76–91. doi: 10.1177/107755870005700105. [DOI] [PubMed] [Google Scholar]
- 14.Kirkman-Liff B, Mondragon D. Language of interview: relevance for research of Southwest Hispanics. Am J Public Health. 1991;81:1399–1404. doi: 10.2105/ajph.81.11.1399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schur CL, Albers LA. Language, sociodemographics, and healthcare use of Hispanic adults. J Health Care Poor Underserved. 1996;7:140–158. doi: 10.1353/hpu.2010.0024. [DOI] [PubMed] [Google Scholar]
- 16.Solis JM, Marks G, Garcia M, Shelton D. Acculturation, access to care, and use of preventive services by Hispanics: findings from HHANES 1982–84. Am J Public Health. 1990;80 (Suppl):11–19. doi: 10.2105/ajph.80.suppl.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hu DJ, Covell RM. Healthcare usage by Hispanic outpatients as function of primary language. Western J Med. 1986;144:490–493. [PMC free article] [PubMed] [Google Scholar]
- 18.Woloshin S, Schwartz LM, Katz SJ, Welch HG. Is language a barrier to the use of preventive services? J Gen Intern Med. 1997;12:472–477. doi: 10.1046/j.1525-1497.1997.00085.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Carrasquillo O, Orav EJ, Brennan TA, Burstin HR. Impact of language barriers on patient satisfaction in an emergency department. J Gen Intern Med. 1999;14:82–87. doi: 10.1046/j.1525-1497.1999.00293.x. [DOI] [PubMed] [Google Scholar]
- 20.Timmins CL. The impact of language barriers on the healthcare of Latinos in the United States: a review of the literature and guidelines for practice. J Midwifery Womens Health. 2002;47:80–96. doi: 10.1016/s1526-9523(02)00218-0. [DOI] [PubMed] [Google Scholar]
- 21.Wu S, Ridgely MS, Escarce JJ, Morales LS. Language access services for Latinos with limited English proficiency: lessons learned from Hablamos Juntos. J Gen Intern Med. 2007;22 Suppl 2:350–355. doi: 10.1007/s11606-007-0323-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Institute of Medicine. The Richard and Hinda Rosenthal Lectures 2005: Next Steps Toward Higher Quality Health Care. Washington, DC: The National Academies Press; 2006. [Google Scholar]
- 23.Andrulis DP, Brach C. Integrating literacy, culture, and language to improve health care quality for diverse populations. Am J Health Behav. 2007;31:S122–S133. doi: 10.5555/ajhb.2007.31.supp.S122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gold MR, Siegel JE, Russell LB, Weinstein MC. Cost-Effectiveness in Health and Medicine. New York: Oxford University Press; 1996. [Google Scholar]
- 25.Jacobs EA, Shepard DS, Suaya JA, Stone EL. Am J Public Health. Vol. 94. 2004. Overcoming language barriers in health care: costs and benefits of interpreter services; pp. 866–869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Somers HL, Caress AL, Evans DG, Johnson MJ, Lovel HJ, Mohamed Z. A computer-based aid for communication between patients with limited English and their clinicians, using symbols and digitised speech. Int J Med Inform. 2007;10:507–517. doi: 10.1016/j.ijmedinf.2007.10.007. [DOI] [PubMed] [Google Scholar]
- 27.Gustafson D, Hawkins R, Pingree S, McTavish F, Arora NK, Mendenhall J. Effect of computer support on younger women with breast cancer. J Gen Intern Med. 2001;16:435–445. doi: 10.1046/j.1525-1497.2001.016007435.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Newell S, Girgis A, Sanson-Fisher RW, et al. Are touch-screen computer surveys acceptable to medical oncology patients? J Psychosoc Oncol. 1997;15:37–46. [Google Scholar]
- 29.Wright EP, Smith AB, Velikova G, et al. Automated screening and recording of quality of life data: a comparison of data capture methods. Psychooncology. 1998;7:67. [Google Scholar]
- 30.Velikova G, Wright EP, Smith AB, Cull A, Gould A, Forman D, Perren T, Stead M, Brown J, Selby PJ. Automatic collection of quality-of-life data: a comparison of paper and computer touch-screen questionnaires. J Clin Oncol. 1999;17:998–1007. doi: 10.1200/JCO.1999.17.3.998. [DOI] [PubMed] [Google Scholar]
- 31.Starren J, Hripcsak G, Sengupta S, Msee A, Knudson PE, Weinstock RS, Shea S. Columbia University’s Informatics for Diabetes Education and Telemedicine (IDEATel) Project: technical implementation. J Am Med Inform Assoc. 2002;9:25–26. doi: 10.1136/jamia.2002.0090025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shea S, Starren J, Weinstock RS, Knudson PE, Teresi J, Holmes D, Palmas W, Field L, Goland R, Tuck C, et al. Columbia University’s Informatics for Diabetes Education and Telemedicine (IDEATel) Project: rationale and design. J Am Med Inform Assoc. 2002;9:49–62. doi: 10.1136/jamia.2002.0090049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Safran C. The collaborative edge: patient empowerment for vulnerable populations. Int J Med Inf. 2003;69:185–190. doi: 10.1016/s1386-5056(02)00130-2. [DOI] [PubMed] [Google Scholar]
- 34.Jones C, Clement L, Hanley-Lopez J, Morphew T, Choi Kwong KY, Lifson F, Opas L, Guterman JJ. The Breathmobile Program: structure, implementation, and evolution of a large-scale, urban, pediatric asthma disease management program. Dis Manage. 2005;8:205–222. doi: 10.1089/dis.2005.8.205. [DOI] [PubMed] [Google Scholar]
- 35.Baker DW, Williams MV, Parker RM, Gazmararian JA, Nurss J. Development of a brief test to measure functional health literacy. Patient Educ Couns. 1999;38:33–42. doi: 10.1016/s0738-3991(98)00116-5. [DOI] [PubMed] [Google Scholar]
- 36.Nielsen-Bohlman L, Kindig SA, editors. Committee on Health Literacy. Health Literacy: A Prescription to End Confusion. Washington, DC: The National Academies Press; 2004. pp. 31–58. Chapter 3. What is Health Literacy. [PubMed] [Google Scholar]
- 37.Nurss J, Parker RM, Williams MV, Baker DW. Directions for administration and scoring and technical data, Short Test of Functional Health Literacy in Adults (STOFHLA-English & STOFHLA-Spanish) Atlanta, GA: Center for the Study of Adult Literacy; Georgia State University; 1998. [Google Scholar]
- 38.Lee Y, Bender DE, Ruiz RE, Cho YI. Development of an easy-to-use Spanish Health Literacy test. Health Serv Res. 2006;41:1392–1412. doi: 10.1111/j.1475-6773.2006.00532.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Calkins-Aguirre A, Ebrahim N, Shea JA. Performance of the English and Spanish S-TOFHLA among publicly insured Medicaid and Medicare patients. Patient Educ Couns. 2005;56:332–339. doi: 10.1016/j.pec.2004.03.007. [DOI] [PubMed] [Google Scholar]
- 40.Lewis RJ. IBM Computer Usability Satisfaction Questionnaires: Psychometric Evaluation and Instructions for Use. Vol. 54. Boca Raton, FL: Human Factors Group, IBM Technical Report; 1993. p. 786. [Google Scholar]
- 41.National Heart, Lung, and Blood Institute, Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma. Bethesda, MD: National Institutes of Health, Bethesda, MD; 2007. Aug, NIH Publication 07–4051. [Google Scholar]