Abstract
Background
Accidental drug overdose is a major cause of mortality among drug users. Fears of police arrest may deter witnesses of drug overdose from calling for medical help and may be a determinant of drug overdose mortality. To our knowledge, no studies have empirically assessed the relation between levels of policing and drug overdose mortality. We hypothesized that levels of police activity, congruent with fears of police arrest, are positively associated with drug overdose mortality.
Methods
We assembled cross-sectional time-series data for 74 New York City (NYC) police precincts over the period 1990–1999 using data collected from the Office of the Chief Medical Examiner of NYC, the NYC Police Department, and the US Census Bureau. Misdemeanor arrest rate—reflecting police activity—was our primary independent variable of interest, and overdose rate our primary dependent variable of interest.
Results
The mean overdose rate per 100,000 among police precincts in NYC between 1990 and 1999 was 10.8 (standard deviation = 10.0). In a Bayesian hierarchical model that included random spatial and temporal effects and a space-time interaction, the misdemeanor arrest rate per 1,000 was associated with higher overdose mortality (posterior median = 0.003, 95% Credible Interval = 0.001, 0.005) after adjustment for overall drug use in the precinct and demographic characteristics.
Conclusions
Levels of police activity in a precinct are associated with accidental drug overdose mortality. Future research should examine aspects of police-community interactions that contribute to higher overdose mortality.
Keywords: drug use, overdose, cocaine, opiates, spatial, policing
1. Introduction
Drug overdose is common among drug users and is associated with considerable mortality. Approximately 60–70% of drug users experience an overdose during their lifetime (Sergeev et al., 2003; Warner-Smith et al., 2002). Drug users have mortality rates 6.9–22.0 times greater than rates among the general population (Frischer et al., 1997; Hulse et al., 1999; Joe and Simpson, 1987), and much of this excess mortality is attributable to drug overdose. In New York City (NYC), drug overdose is a significant problem; in 2007 death due to drug use and accidental overdose was the third leading cause of death among residents aged 15–34, and the fourth leading cause of death among residents aged 35–54 (NYC Bureau of Vital Statistics, 2008). In several jurisdictions within NYC the death rates from drug overdose have exceeded death rates due to homicide (NYC Department of Mental Health and Hygiene, 2005).
Drug overdoses are frequently witnessed by members of drug use networks (Darke and Hall, 2003; Segeev et al., 2003; Tracy et al., 2005), creating the opportunity for those present to mitigate drug overdose mortality by intervening on behalf of overdose victims. For example, because drug overdose is frequently associated with respiratory or cardiac failure (Paredes et al., 2004), calling for emergency medical help may improve survival from drug overdose by facilitating the response of paramedics to overdose events. It has been shown that heroin overdose victims who received emergency medical care while still exhibiting pulse and blood pressure had survival rates greater than 90% (Sporer et al., 1996).
Despite the potential for witnesses to intervene on behalf of overdose victims in this manner, evidence indicates that a substantial proportion of those who witness an overdose either delay or do not call for medical assistance (Darke et al., 2000; Strang et al., 2000; Tobin et al., 2005; Tracy et al., 2005). For example, a study of heroin, crack, and cocaine users in NYC showed that only 68% of respondents reported that they or someone else called for medical help for the overdose victim at the last heroin-related overdose they witnessed (Tracy et al., 2005). Additionally, a study of current and former drug users in Baltimore showed that only 23% of respondents called for an ambulance during the most recent overdose they witnessed (Tobin et al., 2005). Extant research suggests that fears of police involvement or of criminal prosecution are the primary reasons why persons who witness overdose may be reluctant to call for help. For example, in a sample of drug users in NYC, fear of police arrest was the most commonly cited reason for not calling or delaying before calling for help (Tracy et al., 2005). This finding has been corroborated in other studies of drug users (Baca and Grant, 2007; Davidson et al., 2003; McGregor et al., 1998; Pollini et al., 2006; Tobin et al., 2005). These results suggest that fear of police arrest may be an important determinant of drug overdose mortality; however, we are unaware of any studies that have assessed this directly.
Prior research has established a relationship between policing strategy and other drug use-related behaviors in urban communities. More aggressive policing will result in more incarcerations, and research has repeatedly established that incarceration is associated with risk of drug overdose (Binswanger et al., 2007; Bird and Hutchinson, 2003; Krinsky et al., 2009; Seaman et al., 1998; Verger et al 2003). In qualitative interviews of injection drug users, respondents reported being less likely to engage in safe injection practices when there was a policy of aggressive policing of drug crimes in a community (Aitken et al., 2002; Cooper et al., 2005a; Maher and Dixon, 1999). An analysis of number of participants at syringe exchange programs similarly indicated a decrease in the use of this service during a period of increased police intervention (Davis et al., 2005). Structured interviews of injection drug users in Vancouver before and after a period of aggressive policing of minor crimes found that the “crackdown” did not reduce drug use frequency, drug price, or treatment entry (Wood et al., 2004), and 70% of those who had drugs confiscated by the police during this period reported immediately obtaining more drugs (Werb et al., 2008). In contrast, however, periods of increased policing in NYC did not result in an increase in injection-related infections, which would be expected if there was an increase in unsafe and rushed drug injections (Cooper et al., 2005b).
The degree to which police are likely to arrest individuals for drug possession violations (at the scene of an overdose and otherwise) is influenced by local law enforcement policy. A major influence on law enforcement policy in recent decades has been the theory of “broken windows” policing (Cerda et al., 2009; Hinkle and Weisburd, 2008; Kawachi and Berkman, 2000; Sampson, 1996; Shaw and McKay, 1942; Wilson and Kelling, 1982). This theory posits that disorder and minor crimes result in fearfulness on the part of the local community, which decreases the cohesiveness of a society and, in turn, the stock of social capital available to facilitate collective action and informal control over acceptable behaviors. Under this theory, the aggressive enforcement of minor violations prevents more serious crimes, which has been supported by evidence that greater policing of misdemeanors is associated with reductions in homicide mortality (Cerda et al., 2009; Messner et al., 2007; Rosenfeld et al., 2007).
“Broken windows” policing and other policing strategies that involve aggressive enforcement of misdemeanors, however, may have a more complicated relationship with mortality from accidental drug overdose than homicide. In a study of an intervention involving increased enforcement of minor violations (particularly for drug activity and prostitution), residents in areas that received the intervention reported greater levels of fear compared to residents in the control condition (Hinkle and Weisburd, 2008). Because drug possession is a misdemeanor offense in many regions of the US, including NYC, more aggressive enforcement of misdemeanors may have a particularly strong impact on fear of the police for individuals who witness a drug overdose. Specifically, in neighborhoods with a higher concentration of misdemeanor arrests, individuals who witness an overdose while using drugs may be less likely to call 911 because they fear being arrested on a misdemeanor charge for drug possession.
One way to analyze the effect of the fear of police arrest on overdose mortality is the use of ecological data, such as aggregated mortality records and neighborhood indicators. An ecological approach has been increasingly used to understand drug use in recent years (Ensminger et al., 1997; Freisthler et al., 2005; LaScala, et al., 2005; Mosher, 2001; Saxe et al., 2001), including analysis of spatial dynamics (Chandra and Swoboda, 2008; DiMaggio et al., 2008; Freisthler et al., 2005; Hannon and Cuddy, 2006). An ecological approach of using aggregate population-level data has also been used in prior studies to examine police enforcement of drug-related crimes (Mosher, 2001; Weisburd and Mazerolle, 2000). Prior research has also established a relationship between neighborhood characteristics, such as socioeconomic distribution (DiMaggio et al., 2008; Galea et al., 2003) and deterioration of the built environment (Hembree et al., 2005; Nandi et al., 2006), and overdose mortality.
This study examined whether levels of misdemeanor arrests were associated with drug overdose mortality in NYC. Specifically, we hypothesized that levels of misdemeanor arrests are congruent with levels of fear of police arrest and are positively associated with drug overdose mortality in NYC police precincts, independent of overall neighborhood drug use, levels of socioeconomic status, and other covariates. Because this relationship may differ by substance if misdemeanors related to particular substances are enforced more stringently, we further analyzed the association of misdemeanor arrest rate with cocaine and heroin overdose mortality separately.
2. Methods
Data for this study were collected from a number of sources, including the Office of the Chief Medical Examiner (OCME) of New York City, the NYC Police Department (NYPD), the NYC Human Resources Administration, and the United States Census Bureau.
2.1 Measures
2.1.1 Time varying data: drug overdose mortality rate, level of drug use, and police activity
Mortality data were collected from the OCME. The OCME is responsible for assessing all deaths of persons believed to have died in an unnatural manner in NYC. Therefore, all accidental deaths, including drug overdose deaths and non-overdose deaths (e.g., asphyxiation, drowning, firearm deaths, vehicular accidents, and other accidental deaths not due to human intent), in NYC would have been reviewed by the OCME and included in this sample. The OCME investigators use the decedent’s medical history, the circumstances and environment of the fatality (e.g., was the decedent found in a “shooting gallery”), autopsy findings, and laboratory data to attribute cause of death to each case reviewed. All accidental drug overdose deaths and non-overdose accidental deaths in NYC from 1990–1999 were identified through a standardized manual review and abstraction of medical files at the OCME.
NYC is divided into 76 police precincts. Precincts 33 and 34, covering the Washington Heights and Inwood areas, were treated as one precinct because they were split only in 1994. The Central Park precinct (Precinct 22) was excluded a priori since no one resides in this precinct and thus there is no population denominator available for rate estimation. We geocoded all accidental drug overdose deaths and all non-overdose accidental deaths to the remaining 74 police precincts by the address of the injury and used these data to determine the number of drug overdose deaths and the level of drug use per precinct per year, respectively. Expected counts of overdose deaths in each precinct in each year were calculated by multiplying the average overdose rate in NYC for the whole time period (1990–1999) by the total population estimate for the precinct in that year; population estimates were obtained from the US Census for 1990 and 2000 (Bureau of the Census, 1990) and a linear interpolation was conducted for the intervening years (1991–1999). Deaths that were attributed to both cocaine and opiates were excluded from the cocaine- and opiate-specific overdose rates in order to assess more distinctly the predictors of these two types of drug overdose. For each precinct and year, we used the proportion of accidental non-overdose decedents with positive toxicology for any illegal drug other than marijuana, for cocaine, and for opiates to represent the level of use of any drug, cocaine, and opiates, respectively (Cerda et al., 2009; Galea et al., 2003; Messner et al., 2007). Decedents without a valid address of injury were excluded from these analyses.
We used the number of misdemeanor arrests in a police precinct as a measure of police activity. The NYPD routinely collects data on all police arrests for various causes by precinct. Data were collected from the NYPD on all misdemeanor arrests by precinct from 1990–1999 to represent “broken windows”-oriented enforcement policy and related policing strategies, consistent with prior research (Cerda et al., 2009; Corman and Mocan, 2002; Harcourt and Ludwig, 2005; Kelling and Sousa, 2001). Annual rates were calculated by dividing the number of misdemeanor arrests per precinct per year by the total population of that precinct in that year (Bureau of the Census, 1990) and were expressed per 100,000 population.
2.1.2 Time fixed demographic and socioeconomic variables
Prior research has indicated that NYC precincts that experienced interventions of heightened police activity during the 1990s had residents that were on average younger and more impoverished and had a lower proportion of residents who were White than other precincts (Cooper et al., 2005b). Consequently, time fixed data on demographic and socioeconomic characteristics were collected from the 1990 US Census at the census tract level and aggregated to the police precinct level (Bureau of the Census, 1990) to be used as covariates in adjusted analyses. With respect to demographic variables, we calculated the percent of persons per precinct who were male, under age 35, and Black. We measured five socioeconomic variables, including the percent of persons per precinct who were unemployed, had less than a high school education, earned less money annually than 200% of the federal poverty level, and received public assistance, as well as the percent of households per precinct with a self-reported female head of household. Four of the socioeconomic variables (i.e. percent of persons with less than a high school education, percent of persons earning less than 200% of the poverty level, percent of persons receiving public assistance, and percent of households headed by a female) were highly collinear, with correlation coefficients ranging between 0.82 and 0.91. Consequently, we used principal components analysis to create a composite socioeconomic status score for each precinct. The composite was scored in the direction of disadvantage, with more socioeconomically disadvantaged precincts scoring higher (range 23.4–189.0). Percent of person unemployed had weaker correlations with the other socioeconomic indicators (correlation coefficients between 0.70 and 0.83) and prior research on policing and mortality has examined unemployment separately (Messner et al., 2007). Consequently, we included percent of persons unemployed as a separate variable from the socioeconomic status composite score in modeling.
2.2 Analytic approach
The unit of analysis was police precincts (n = 74). We determined the posterior estimates of spatio-temporal Poisson models using Bayesian hierarchical methods (Clayton and Kaldor, 1987; Lawson, 2009; Richardson et al., 2006; Wakefield et al., 2000; Waller and Gotway, 2004). All models were specified as follows:
where Oit denotes the observed overdose count in police precinct i at time t, Eit is the expected overdose count in precinct i at time t, α represents the baseline log relative risk of overdose across NYC, Xarrestsit is the misdemeanor arrest rate in precinct i at time t, Xdruguse.it is the percent of accidental deaths with a positive illegal drug toxicology screen in precinct i at time t,X is a set of baseline covariates, λi is the random spatially-structured effect, ξt is the random time effect, and νit is a random term allowing for space-time interaction (i.e. that spatial patterns of overdose may change over time) (Xia and Carlin, 1998).
In the Bayesian approach, all random effects are considered unknown, but prior knowledge of the structure of an effect is used to select a prior distribution for analysis (Richardson et al., 2006). We used spatial and time random effects to account for the correlation of risk for fatal overdose in nearby areas and contiguous years; these random effects were modeled with priors that have a conditionally autoregressive (CAR) distribution, with weights for first-order adjacent neighbors set at 1 (“neighbors” defined as precincts sharing a border in the case of the spatial random effect, and as immediately prior (t−1) and subsequent (t+1) years in the case of the time random effect). The space-time interaction random effect had a normally distributed prior. All priors have hyperpriors, which are distributions for the precision parameters of the spatial, temporal, and space-time interaction priors. The hyperpriors had a gamma distribution (Richardson et al., 2006; Wakefield et al., 2000). This type of model was chosen after a comparison of model fit between different types of model specifications for time and spatial clustering, based on the Deviance Information Criterion (DIC), indicated that this model provided the best fit to the data. All models were estimated with Winbugs with two parallel Markov chain Monte Carlo chains for a total of 25,000 iterations, the first 15,000 of which were discarded as a “burn-in” period. We then used the estimates from every tenth iteration (resulting in a total of 2,000 samples from the two chains for each model) to create a posterior distribution, from which the medians and 95% credible intervals were taken.
3. Results
Figure 1 depicts the overdose rate by police precinct for New York City from 1990 to 1999. The Moran’s I statistic was 0.37 for all overdoses, 0.35 for cocaine overdoses, and 0.35 for opiate overdoses (all p < 0.01). This indicates statistically significant spatial clustering (i.e., adjacent precincts have similar overdose rates).
Figure 1.
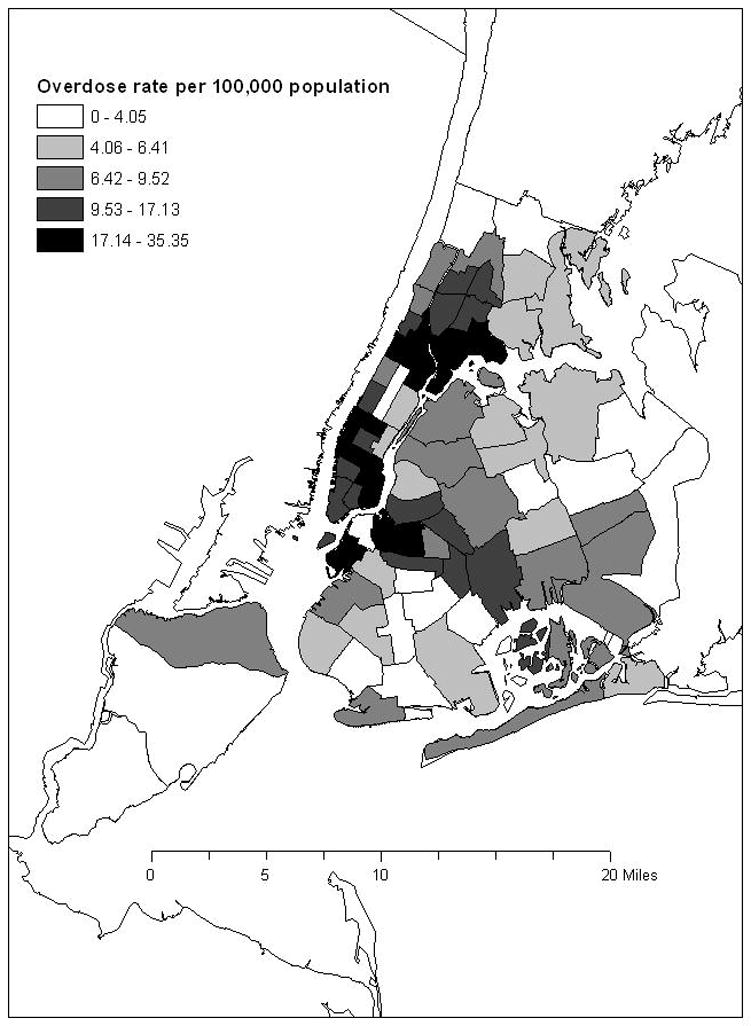
Map of overdose rate (per 100,000 population per year) by police precinct, New York City, 1990–1999.
The univariate characteristics of the 74 police precincts averaged over the period from 1990–1999 are presented in Table 1. Overall, 6,655 of the 8,467 (78.6%) accidental drug overdose deaths occurring in NYC from 1990–1999 were successfully geocoded to the police precinct level and included in these analyses. Men were less likely than females to be excluded from analysis (p < 0.05), and whites were less likely to be excluded because of missing address data than other races (p < 0.05). The mean misdemeanor arrest rate per precinct was 46.0 (standard deviation [SD] = 49.1) per 1,000 residents. The mean rate of accidental drug overdose mortality per precinct was 10.8 (SD = 10.0) deaths per 100,000 residents for all drugs, 2.7 (SD = 3.1) deaths per 100,000 residents for cocaine (without opiates), and 3.2 (SD = 3.4) deaths per 100,000 residents for opiates (without cocaine). The average percent of accidental non-drug overdose decedents per precinct with positive toxicology, our measure of the level of drug use in a particular precinct, was 17% (SD = 13.7) for any illegal drug, 8.0% (SD = 10.6) for cocaine, and 8.9% (SD = 9.3) for opiates. On average, 47.0% (SD = 2.3) of persons per precinct were male, 52.1% (SD = 7.5) were under age 35, 4.5% (SD = 1.2) were unemployed, and 27.5% (SD=27.2) were Black.
Table 1.
Descriptive statistics for NYC police precincts, 1990–1999 (n=74).
| 1990–1999 | ||||
|---|---|---|---|---|
| Mean | SD | Minimum | Maximum | |
| Overdose rate (per 100,000 residents per year)a | 10.8 | 10.0 | 0.0 | 82.3 |
| Cocaine overdose rate (per 100,000 residents per year)a,b | 2.7 | 3.1 | 0.0 | 22.1 |
| Opiate overdose rate (per 100,000 residents per year)a,b | 3.2 | 3.4 | 0.0 | 25.1 |
| Exposure variables | ||||
| Misdemeanor arrest rate (per 1,000 residents per year)a | 46.0 | 49.1 | 1.4 | 313.7 |
| Percent of accident deaths with any illegal drug detecteda,c | 17.0 | 13.7 | 0.0 | 100.0 |
| Percent of accident deaths with cocaine detecteda,c | 8.0 | 10.6 | 0.0 | 100.0 |
| Percent of accident deaths with opiates detecteda,c | 8.9 | 9.3 | 0.0 | 57.1 |
| Control variables | ||||
| Percent maled | 47.0 | 2.3 | 43.3 | 56.3 |
| Percent under age 35 | 52.1 | 7.5 | 38.6 | 68.6 |
| Percent unemployedd | 4.5 | 1.2 | 2.6 | 7.2 |
| Percent blackd | 27.5 | 27.2 | 0.4 | 92.1 |
| SES composited,e | 91.1 | 41.8 | 23.4 | 185.0 |
Data available each year, 1990–1999
Excludes overdose deaths attributed to both cocaine and opiates
Non-overdose accidental deaths only
Data available for 1990 only
SES composite index includes the following socioeconomic variables aggregated to the police precinct level: % less than high school education, % less than 200% poverty, % female-headed households, % receiving public assistance
Table 2 shows the adjusted relations between the precinct-level covariates of interest and accidental drug overdose mortality based on posterior parameter estimates for spatio-temporal Poisson models for all drugs, cocaine, and opiates. Police activity, measured by the misdemeanor arrest rate, was positively associated with drug overdose mortality for all drugs, cocaine, and opiates (all p < 0.05). A one-unit increase in misdemeanor arrests per 1,000 population is associated with a 0.3% higher overdose rate (e0.003 = 1.003). An increase of one standard deviation (49.1) in misdemeanor arrests per 1,000 population is associated with a 16% higher overdose rate (e0.003*49.1 = 1.16). The percent of the residents of a precinct who were black was positively associated with cocaine overdose mortality, but not opiate overdose or total overdose mortality. Precincts with a higher composite socioeconomic score, indicating more disadvantage, had higher accidental drug overdose mortality for all drug overdoses and opiate overdoses (p < 0.05), but not cocaine. The level of drug use in a precinct was not associated with accidental drug overdose mortality in adjusted models.
Table 2.
Posterior parameter estimates for spatio-temporal Poisson models predicting total overdoses, cocaine-only overdoses, and opiates-only overdoses, for NYC police precincts, 1990–1999 (n=74).
| All Overdoses | Cocaine Overdoses | Opiates Overdoses | ||||
|---|---|---|---|---|---|---|
| Posterior Median | 95% Credible Interval | Posterior Median | 95% Credible Interval | Posterior Median | 95% Credible Interval | |
| Exposure variables | ||||||
| Misdemeanor arrest rate (per 1,000) | 0.003 | 0.001, 0.005 | 0.004 | 0.002, 0.01 | 0.003 | 0.001, 0.01 |
| Percent accident decedents with any illegal drug detected | 0.003 | −0.0004, 0.006 | −0.002 | −0.01, 0.004 | 0.0005 | −0.01, 0.01 |
| Control variablesa | ||||||
| Percent male | −0.05 | −0.18, 0.08 | −0.06 | −0.19, 0.07 | −0.05 | −0.19, 0.10 |
| Percent under age 35 | 0.06 | −0.16, 0.28 | 0.20 | −0.03, 0.42 | 0.12 | −0.13, 0.36 |
| Percent unemployed | −0.03 | −0.27, 0.23 | −0.07 | −0.34, 0.19 | −0.18 | −0.46, 0.10 |
| Percent black | 0.01 | −0.18, 0.19 | 0.29 | 0.12, 0.47 | −0.08 | −0.27, 0.11 |
| SES composite | 0.32 | 0.06, 0.56 | 0.16 | −0.12, 0.43 | 0.35 | 0.05, 0.64 |
| Precision parameters | ||||||
| Space CAR effect | 2.09 | 1.33, 3.33 | 2.60 | 1.50, 4.90 | 2.09 | 1.22, 3.68 |
| Time CAR effect | 25.90 | 7.95, 66.04 | 19.09 | 5.49, 62.16 | 23.26 | 7.42, 70.40 |
| Space-time interaction | 8.69 | 6.85, 11.11 | 9.19 | 5.61, 19.84 | 7.02 | 4.84, 11.00 |
| Intercept | −0.26 | −0.37, −0.16 | −0.30 | −0.43, −0.17 | −0.28 | −0.42, −0.14 |
The control variables have been standardized to have mean 0 and standard deviation 1, so that the coefficient represents the effect of a 1 standard-deviation increase.
4. Discussion
Using NYC mortality data from 1990–1999, we found that police activity in a precinct was associated with accidental drug overdose mortality. Specifically, Bayesian hierarchical modeling showed that accidental fatal drug overdose, as well as cocaine-specific and opiate-specific fatal overdose, was significantly higher in police precincts with higher misdemeanor arrest rates, independent of potential confounding by gender, age, race, unemployment, socioeconomic status, and the level of drug use. We infer that greater police activity in a neighborhood is associated with higher rates of drug overdose mortality, possibly due to greater reluctance of persons who witness overdose to call for help. Although increased levels of misdemeanor policing may decrease the rate of drug overdose mortality in a precinct both directly, by reducing levels of drug use, and indirectly, by strengthening the community capacity to maintain informal control over drug use and associated risk behaviors, it may also engender an environment in which drug users are increasingly fearful of police arrest for minor infractions. Fears of arrest may promote behaviors, such as not calling for medical help when witnessing an overdose, which delay medical responses to overdose events and increase the rate of drug overdose mortality in a precinct.
We found that accidental drug overdose mortality for all drugs, cocaine, and opiates was significantly higher in police precincts with greater levels of police activity. The present findings suggest that greater drug overdose mortality may be a negative consequence of greater levels of police activity that may somewhat offset the benefits associated with aggressive enforcement of misdemeanor violations, such as reduced homicide mortality (Cerda et al., 2009; Messner et al., 2007; Rosenfeld et al., 2007). We note that these findings are particularly important when considering that in NYC, where this study was conducted, there have been more deaths due to accidental drug overdose than there have been due to homicide every year since 1996. Therefore, if police activity is indeed a contributor to higher overdose mortality rates, this consequence of greater policing is not trivial, but rather one that may have substantial implications for population health.
There are several possible explanations for the present findings. Based on extant research about the circumstances surrounding drug overdose (Tracy et al., 2005; Tobin et al., 2005), we suggest that the primary mechanism linking greater police activity and overdose death is fear of police arrest among persons who witness overdose. It has been amply demonstrated that the vast majority of overdoses are witnessed and that timely calls to emergency medical services may substantially reduce overdose mortality (Powis et al., 1999). However, extant research shows that fear of police arrest is the primary reason why persons who witness an overdose may be reluctant to call for help (Baca and Grant, 2007; Pollini et al., 2006; Tobin et al., 2005; Tracy et al., 2005). Delaying the response of emergency medical services to an overdose event may contribute to the rate of overdose mortality in a precinct by increasing the probability of death conditional on drug overdose. A secondary mechanism explaining the observed relation may be that increased police presence, and hence increased fear of police arrest, may increase the rate of drug overdose mortality in a precinct by promoting drug use in more secluded areas (Dovey et al., 2001) where overdose victims are less likely to receive medical attention (Tracy et al., 2005). A third possible mechanism is that precincts characterized by increased police activity and fears of police involvement may have increased rates of drug overdose mortality because drug users in these precincts are subjected to psychosocial stressors that increase the likelihood of drug overdose (Sinha, 2001) and death from drug overdose. Additionally, a forth possible mechanism is that areas with more arrests have more incarcerations, and the period after release from incarceration is a known risk period for both fatal and non-fatal overdose (Bird and Hutchinson, 2003; Kerr et al., 2007; Krinsky et al., 2009). Lastly, we cannot rule out the possibility of unmeasured confounding. Further work is needed to elucidate the specific pathways linking misdemeanor arrest rates to the likelihood of drug overdose death.
There are several limitations to this study. First, with respect to study design, it is important to note that this analysis was ecological and inference should not be made about the risk of individual overdose events. Second, our measure of police activity was based on the number of misdemeanor arrests in a precinct. Although this measure is consistent with prior research (Corman and Mocan, 2002; Harcourt and Ludwig, 2005; Lekking and Sousa, 2001; Cerda et al., 2009) and has been considered a reasonable measure of misdemeanor policing activity in a given area, it may not fully capture the level of policing perceived by drug users in a particular precinct. In addition, this measure does not address fear of policing per se. Although we observe an association between greater police activity and drug overdose mortality, we can only posit the possible mechanisms that explain the observed association. We have also focused on how misdemeanor arrests, which include drug possession violations, might influence fear of police arrest for overdose witnesses and consequently delay their getting help for the overdose victim. Consequently, other aspects of policing, such as felony arrest rates and size of the police force, are beyond the scope of this study. Furthermore, we used the proportion of non-overdose accident decedents in whom illegal drugs were detected as a proxy measure for levels of drug use in each police precinct. While this is an accepted practice for measuring drug use on a community level (Cerda et al., 2009; Galea et al., 2003; Messner et al., 2007), it is not a direct measure of use and an inexact measure of the drug use of the larger community. Consequently, caution should be exercised in interpretation of the present findings because residual confounding, specifically due to incomplete measure of the prevalence of frequency of drug use within precincts, may be present.
Notwithstanding these limitations, our findings suggest that the level of misdemeanor police activity in a precinct may be an important determinant of drug overdose mortality. This finding, taken together with evidence that fear of police arrest is the primary reason why those who witness overdose do not call for help (Tracy et al., 2005) suggests that “broken windows” policing may be associated with greater overdose mortality. It is important to note that this unintended consequence of greater policing is not, in and of itself, an intractable feature of policing activity. The solution is not to reduce policing, but to offset increases in fear due to high enforcement of misdemeanor infractions with complimentary policing practices. Some jurisdictions have implemented efforts that aim to reassure persons who call for help on witnessing an overdose that they will not be prosecuted (Drug Policy Alliance, 2006). Similarly, policies that prevent police officers from responding to overdose events may reduce fears of arrest and increase the likelihood that witnesses of drug overdoses call for medical help. A broad approach (not specific to concerns about overdose events) is problem-oriented policing, which has been demonstrated to decrease crime and disorder while building positive relationships with the residents of the area being policed (Weisburd and Eck, 2004).
The present study highlights the complex consequences of efforts such as increased policing in urban neighborhoods. A comprehensive assessment of the full range of these consequences, coupled with targeted efforts to mitigate the potential negative effects of such efforts, is warranted.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Aitken C, Moore D, Higgs D, Kelsall J, Kerger M. The impact of a police crackdown on a street drug scene: evidence from the street. Int J Drug Policy. 2002;13:189–198. [Google Scholar]
- Baca CT, Grant KJ. What heroin users tell us about overdose. J Addict Dis. 2007;26:63–68. doi: 10.1300/J069v26n04_08. [DOI] [PubMed] [Google Scholar]
- Binswanger IA, Stern MF, Deyo RA, Heagerty PJ, Cheadle A, Elmore JG, Koepsell TD. Release from prison--a high risk of death for former inmates. N Engl J Med. 2007;356:157–165. doi: 10.1056/NEJMsa064115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bird SM, Hutchinson SJ. Male drugs-related deaths in the fortnight after release from prison: Scotland, 1996–99. Addiction. 2003;98:185–190. doi: 10.1046/j.1360-0443.2003.00264.x. [DOI] [PubMed] [Google Scholar]
- Bureau of the Census. Census summary tape, file 3A (STF 3A) 1990. [Google Scholar]
- Bureau of Vital Statistics. Summary of Vital Statistics 2007. the City of New York: New York City Department of Health and Mental Hygiene; 2008. [online]. 2008. [Cited 2009 April 22]. Available from URL: http://www.nyc.gov/html/doh/downloads/pdf/vs/2007sum.pdf. [Google Scholar]
- Centers for Disease Control and Prevention (CDC) Unintentional and undetermined poisoning deaths -- 11 states, 1990–2001. MMWR Morb Mortal Wkly Rep. 2004;53:233–238. [PubMed] [Google Scholar]
- Cerda M, Tracy M, Messner SF, Vlahov D, Tardiff K, Galea S. Misdemeanor policing, physical disorder, and gun-related homicide: a spatial analytic test of “broken-windows” theory. Epidemiology. 2009;20:533–541. doi: 10.1097/EDE.0b013e3181a48a99. [DOI] [PubMed] [Google Scholar]
- Chandra S, Swoboda A. Are spatial variables important? The case of markets for multiple drugs in British Bengal. In: Thomas YF, Richardson D, Cheung I, editors. Geography and Drug Addiction. Springer; New York: 2008. pp. 221–242. [Google Scholar]
- Clayton D, Kaldor J. Empirical bayes estimates of age-standardized relative risks for use in disease mapping. Biometrics. 1987;43:671–681. [PubMed] [Google Scholar]
- Cooper H, Moore L, Gruskin S, Krieger N. The impact of a police drug crackdown on drug injectors’ ability to practice harm reduction: a qualitative study. Soc Sci Med. 2005a;61:673–684. doi: 10.1016/j.socscimed.2004.12.030. [DOI] [PubMed] [Google Scholar]
- Cooper HLF, Wypij D, Krieger N. Police drug crackdowns and hospitalisation rates for illicit-injection-related infections in New York City. Int J Drug Policy. 2005b;16:150–160. [Google Scholar]
- Corman H, Mocan N. Carrots, Sticks and Broken Windows. NBER Working Paper 9061. 2002 http://www.nber.org/paper/w9061.
- Darke S, Hall W. Heroin overdose: research and evidence-based intervention. J Urban Health. 2003;80:189–200. doi: 10.1093/jurban/jtg022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darke S, Ross J, Zador D, Sunjic S. Heroin-related deaths in New South Wales, Australia, 1992–1996. Drug Alcohol Depend. 2000;60:141–150. doi: 10.1016/s0376-8716(99)00147-7. [DOI] [PubMed] [Google Scholar]
- Davidson PJ, McLean RL, Kral AH, Gleghorn AA, Edlin BR, Moss AR. Fatal heroin-related overdose in San Francisco, 1997–2000: a case for targeted intervention. J Urban Health. 2003;80:261–273. doi: 10.1093/jurban/jtg029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis CS, Burris S, Kraut-Becher J, Lynch KG, Metzger D. Effects of an intensive street-level police intervention on syringe exchange program use in Philadelphia, PA. Am J Public Health. 2005;95:233–236. doi: 10.2105/AJPH.2003.033563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiMaggio C, Bucciarelli A, Tardiff K, Vlahov D, Galea S. Spatial analytic approaches to explaining the trends and patterns of drug overdose deaths. In: Thomas YF, Richardson D, Cheung I, editors. Geography and Drug Addiction. Springer; New York: 2008. pp. 447–464. [Google Scholar]
- Dovey K, Fitzgerald J, Choi Y. Safety becomes danger: dilemmas of drug-use in public space. Health Place. 2001;7:319–331. doi: 10.1016/s1353-8292(01)00024-7. [DOI] [PubMed] [Google Scholar]
- Drug Policy Alliance. As Death Toll from Fentanyl-laced Heroin Continues to Rise, Senator Richard Durbin Introduces Federal Legislation to Save Lives. 2006 [Cited 2009 October 5]. Available at: http://www.drugpolicy.org/news/pressroom/pressrelease/pr062206.cfm.
- Ensminger ME, Anthony JC, McCord J. The inner city and drug use: initial findings from an epidemiological study. Drug Alcohol Depend. 1997;48:175–184. doi: 10.1016/s0376-8716(97)00124-5. [DOI] [PubMed] [Google Scholar]
- Freisthler B, Gruenewald PJ, Johnson FW, Treno AJ, LaScala EA. An exploratory study examining the spatial dynamics of illicit drug availability and rates of drug use. J Drug Educ. 2005;35:15–27. doi: 10.2190/25QY-PBC3-B1EB-JB5Y. [DOI] [PubMed] [Google Scholar]
- Frischer M, Goldberg D, Rahman M, Berney L. Mortality and survival among a cohort of drug injectors in Glasgow, 1982–1994. Addiction. 1997;92:419–427. [PubMed] [Google Scholar]
- Galea S, Ahern J, Vlahov D, Coffin PO, Fuller C, Leon AC, Tardiff K. Income distribution and risk of fatal drug overdose in New York City neighborhoods. Drug Alcohol Depend. 2003;70:139–148. doi: 10.1016/s0376-8716(02)00342-3. [DOI] [PubMed] [Google Scholar]
- Hannon L, Cuddy MM. Neighborhood ecology and drug dependence mortality: an analysis of New York City census tracts. Am J Drug Alcohol Abuse. 2006;32:453–463. doi: 10.1080/00952990600753966. [DOI] [PubMed] [Google Scholar]
- Harcourt BE, Ludwig J. University of Chicago Public Law and Legal Theory Working Paper No 93. 2005. Broken Windows: New Evidence from New York City & in a Five-City Social Experiment. [Google Scholar]
- Hembree C, Galea S, Ahern J, Tracy M, Markham Piper T, Miller J, Vlahov D, Tardiff KJ. The urban built environment and overdose mortality in New York City neighborhoods. Health Place. 2005;11:147–156. doi: 10.1016/j.healthplace.2004.02.005. [DOI] [PubMed] [Google Scholar]
- Hinkle JC, Weisburd D. The irony of broken windows policing: A micro-place study of the relationship between disorder, focused police crackdowns and fear of crime. J Crim Justice. 2008;36:503–512. [Google Scholar]
- Hulse GK, English DR, Milne E, Holman CD. The quantification of mortality resulting from the regular use of illicit opiates. Addiction. 1999;94:221–229. doi: 10.1046/j.1360-0443.1999.9422216.x. [DOI] [PubMed] [Google Scholar]
- Joe GW, Simpson DD. Mortality rates among opioid addicts in a longitudinal study. Am J Public Health. 1987;77:347–348. doi: 10.2105/ajph.77.3.347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawachi I, Berkman LF. Social cohesion, social capital, and health. In: Berkman LF, Kawachi I, editors. Social Epidemiology. Oxford University; New York: 2000. pp. 174–190. [Google Scholar]
- Kelling GL, Sousa WH. Do Police Matter? An Analysis of the Impact of New York City’s Police Reforms. Civic Report. 2001;22 [Google Scholar]
- Kerr T, Fairbairn N, Tyndall M, Marsh D, Li K, Montaner J, Wood E. Predictors of non-fatal overdose among a cohort of polysubstance-using injection drug users. Drug Alcohol Depend. 2007;87:39–45. doi: 10.1016/j.drugalcdep.2006.07.009. [DOI] [PubMed] [Google Scholar]
- Krinsky CS, Lathrop SL, Brown P, Nolte KB. Drugs, detention, and death: a study of the mortality of recently released prisoners. Am J Forensic Med Pathol. 2009;30:6–9. doi: 10.1097/PAF.0b013e3181873784. [DOI] [PubMed] [Google Scholar]
- LaScala EA, Freisthler B, Gruenewald PJ. Population ecologies of drug use, drinking and related problems. In: Stockwell T, Gruenewald PJ, Toumbourou J, Loxley W, editors. Preventing harmful substance use: The evidence base for policy and practice. John Wiley; New York: 2005. [Google Scholar]
- Lawson AB. Bayesian Disease Mapping: Heirarchical Modeling in Spatial Epidemiology. Chapman & Hall/CRC; Boca Raton, FL: 2009. [Google Scholar]
- Maher L, Dixon D. Policing and public health: law enforcement and harm minimization in a street-level drug market. Br J Criminol. 1999;39:488–512. [Google Scholar]
- McGregor C, Darke S, Ali R, Christie P. Experience of non-fatal overdose among heroin users in Adelaide, Australia: circumstances and risk perceptions. Addiction. 1998;93:701–711. doi: 10.1046/j.1360-0443.1998.9357016.x. [DOI] [PubMed] [Google Scholar]
- Messner SF, Galea S, Tardiff KJ, Tracy M, Bucciarelli A, Markham Piper T, Frye V, Vlahov D. Policing, drugs, and the homicide decline in New York City in the 1990s. Criminology. 2007;45:385–413. [Google Scholar]
- Mosher C. Predicting drug arrest rates: Conflict and social disorganization perpsectives. Crime Delinq. 2001;47:84–104. [Google Scholar]
- Nandi A, Galea S, Ahern J, Bucciarelli A, Vlahov D, Tardiff K. What explains the association between neighborhood-level income inequality and the risk of fatal overdose in New York City? Soc Sci Med. 2006;63:662–674. doi: 10.1016/j.socscimed.2006.02.001. [DOI] [PubMed] [Google Scholar]
- New York City Department of Mental Health and Hygeine. Summary of vital statistics 2004. the City of New York: Office of Vital Statistics; 2005. [Google Scholar]
- Paredes VL, Rea TD, Eisenberg MS, Cobb LA, Copass MK, Cagle A, Martin TG. Out-of-hospital care of critical drug overdoses involving cardiac arrest. Acad Emerg Med. 2004;11:71–74. doi: 10.1197/j.aem.2003.08.014. [DOI] [PubMed] [Google Scholar]
- Pollini RA, McCall L, Mehta SH, Vlahov D, Strathdee SA. Non-fatal overdose and subsequent drug treatment among injection drug users. Drug Alcohol Depend. 2006;83:104–110. doi: 10.1016/j.drugalcdep.2005.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powis B, Strang J, Griffiths P, Taylor C, Williamson S, Fountain J, Gossop M. Self-reported overdose among injecting drug users in London: extent and nature of the problem. Addiction. 1999;94:471–478. doi: 10.1046/j.1360-0443.1999.9444712.x. [DOI] [PubMed] [Google Scholar]
- Richardson S, Abellan JJ, Best N. Bayesian spatio-temporal analysis of joint patterns of male and female lung cancer risks in Yorkshire (UK) Stat Methods Med Res. 2006;15:385–407. doi: 10.1191/0962280206sm458oa. [DOI] [PubMed] [Google Scholar]
- Rosenfeld R, Fornango R, Rengifo AF. The impact of order-maintenance policing on New York City homicide and robbery rates: 1988–2001. Criminology. 2007;45:355–384. [Google Scholar]
- Sampson RJ. The community. In: Wilson JQ, Petersilia J, editors. Crime. Institute for Contemporary Studies; San Francisco: 1996. [Google Scholar]
- Saxe L, Kadushin C, Beveridge A, Livert D, Tighe E, Rindskopf D, Ford J, Brodsky A. The visibility of illicit drugs: implications for community-based drug control strategies. Am J Public Health. 2001;91:1987–1994. doi: 10.2105/ajph.91.12.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seaman SR, Brettle RP, Gore SM. Mortality from overdose among injecting drug users recently released from prison: database linkage study. BMJ. 1998;316:426–428. doi: 10.1136/bmj.316.7129.426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sergeev B, Karpets A, Sarang A, Tikhonov M. Prevalence and circumstances of opiate overdose among injection drug users in the Russian Federation. J Urban Health. 2003;80:212–219. doi: 10.1093/jurban/jtg024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw CR, McKay HD. Juvenile delinquency and urban areas: A study of the rates of delinquents in relation to differential characteristics of local communities in American cities. University of Chicago Press; Chicago: 1942. [Google Scholar]
- Sinha R. How does stress increase risk of drug abuse and relapse? Psychopharmacology (Berl) 2001;158:343–359. doi: 10.1007/s002130100917. [DOI] [PubMed] [Google Scholar]
- Sporer KA, Firestone J, Isaacs SM. Out-of-hospital treatment of opioid overdoses in an urban setting. Acad Emerg Med. 1996;3:660–667. doi: 10.1111/j.1553-2712.1996.tb03487.x. [DOI] [PubMed] [Google Scholar]
- Strang J, Best D, Man L, Noble A, Gossop M. Peer-initiated overdose resuscitation: fellow drug users could be mobilised to implement resuscitation. Int J Drug Policy. 2000;11:437–445. doi: 10.1016/s0955-3959(00)00070-0. [DOI] [PubMed] [Google Scholar]
- Tobin KE, Davey MA, Latkin CA. Calling emergency medical services during drug overdose: an examination of individual, social and setting correlates. Addiction. 2005;100:397–404. doi: 10.1111/j.1360-0443.2005.00975.x. [DOI] [PubMed] [Google Scholar]
- Tracy M, Piper TM, Ompad D, Bucciarelli A, Coffin PO, Vlahov D, Galea S. Circumstances of witnessed drug overdose in New York City: implications for intervention. Drug Alcohol Depend. 2005;79:181–190. doi: 10.1016/j.drugalcdep.2005.01.010. [DOI] [PubMed] [Google Scholar]
- Verger P, Rotily M, Prudhomme J, Bird S. High mortality rates among inmates during the year following their discharge from a French prison. J Forensic Sci. 2003;48:614–616. [PubMed] [Google Scholar]
- Wakefield JC, Best NG, Waller L. Bayesian approaches to disease mapping. In: Elliott P, Wakefield JC, Best NG, Briggs DJ, editors. Spatial Epidemiology. Oxford University Press; New York: 2000. pp. 104–127. [Google Scholar]
- Waller L, Gotway C. Wiley Series in Probability and Statistics. Wiley Publishers; Hoboken, NJ: 2004. Applied Spatial Statistics for Public Health Data. [Google Scholar]
- Warner-Smith M, Darke S, Day C. Morbidity associated with non-fatal heroin overdose. Addiction. 2002;97:963–967. doi: 10.1046/j.1360-0443.2002.00132.x. [DOI] [PubMed] [Google Scholar]
- Weisburd D, Eck JE. What can police do to reduce crime, disorder, and fear? Ann Am Acad Pol Soc Sci. 2004;593:42–65. [Google Scholar]
- Weisburd D, Mazerolle LG. Crime and disorder in drug hot spots: Implications for theory and practice in policing. Police Quarterly. 2000;3:331–349. [Google Scholar]
- Werb D, Wood E, Small W, Strathdee S, Li K, Montaner J, Kerr T. Effects of police confiscation of illicit drugs and syringes among injection drug users in Vancouver. Int J Drug Policy. 2008;19:332–338. doi: 10.1016/j.drugpo.2007.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson JQ, Kelling GL. Broken windows: the police and neighborhood safety. Atlantic Monthly. 1982;249:29–38. [Google Scholar]
- Wood E, Spittal PM, Small W, Kerr T, Li K, Hogg RS, Tyndall MW, Montaner JS, Schechter MT. Displacement of Canada’s largest public illicit drug market in response to a police crackdown. CMAJ. 2004;170:1551–1556. doi: 10.1503/cmaj.1031928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xia H, Carlin B. Spatio-temporal models with errors in covariates: mapping Ohio lung care mortality. Stat Med. 1998;17:2025–2043. doi: 10.1002/(sici)1097-0258(19980930)17:18<2025::aid-sim865>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]


