Abstract
In a feasibility study using a prototype, lateral-flow test for human papillomavirus type 16, 18, and/or 45 (HPV16/18/45) E6 oncoproteins, 51 of 75 (68%; 95% confidence interval [95% CI] of 56 to 78%) of HPV16/18/45 DNA-positive specimens from women with a diagnosis of CIN3+ (cervical intraepithelial neoplasia grade 3+ or cervical cancer) tested positive for HPV16/18/45 E6 oncoprotein. None of 16 (95% CI of 0 to 37%) HPV16/18/45 DNA-positive cervical specimens from women with a negative or CIN1 diagnosis tested positive for HPV16/18/45 E6 oncoprotein.
Human papillomavirus (HPV) DNA detection has been proven to be a viable and potentially more effective alternative to Pap testing in both developed countries (3) and developing countries (7), where more than 80% of the almost half million annual cases of cervical cancer occur (5). A new generation of HPV DNA tests that are lower cost, faster, and easier to use are currently being developed (6). Although HPV DNA tests are very sensitive for the diagnosis of cervical precancer and early cancers, their specificity is limited, as they detect both the many benign HPV infections and the less frequent infections linked to clinically important disease.
Because elevated expression of E6 and E7 (mRNA and protein) is required for epithelial cell transformation to occur, detecting the E6/E7 proteins represents an attractive, disease-specific viral biomarker. To examine whether detection of E6 oncoprotein was feasible from cervical specimens and was more specific clinically than detection of HPV DNA, we conducted a pilot study on a convenience sample of cervical swab specimens using a prototype, lateral-flow test for HPV type 16, 18, and/or 45 (HPV16/18/45) E6 oncoproteins (AV Avantage HPV E6 test; Arbor Vita Corporation, Fremont, CA).
(i) Specimens.
A set of cervical swab specimens linked to histological outcomes were collected using a Dacron swab and stored without buffer or specimen transport medium at less than −60°C. The specimen set was assembled as a convenience sample from a variety of sources. The first group of specimens consisted of 16 specimens (negative histology) from Planned Parenthood (PPMM, San Jose, CA). The second group consisted of 55 specimens: 1 specimen from a woman with cervical intraepithelial neoplasia grade 1 (CIN1), 14 specimens from women with CIN3, 29 specimens from women with CIN3 or cervical cancer (CIN3+) (The exact diagnosis, CIN3 or cervical cancer, was not provided), and 11 specimens from women with cervical cancer. These specimens were acquired via BioImagene (Cupertino, CA), who obtained the specimens from a clinical trial being conducted in India. The third group of specimens consisted of 89 specimens (8 specimens with negative histology, 28 specimens from women with CIN1, 43 specimens from women with CIN3, and 10 specimens from women with cervical cancers were accumulated by the Program for Appropriate Technology in Health (PATH) as part of ongoing studies of low-cost HPV testing in China (6) and India. Thus, the final set of cervical swab specimens were collected from 24 women with community diagnosis of negative histology, 29 women with CIN1, 57 women with CIN3, 29 women with CIN3+, and 21 women with cervical cancer. There were 53 women with CIN1 or less severe histology (≤CIN1) and 97 women with CIN3+. Sample collection by BioImagene and by PPMM occurred according to the protocols customary in the respective health facilities. For specimens obtained via PATH, a standardized, expert approved collection protocol was applied. Samples were collected from the endocervical opening and the ectocervix by inserting the swab just inside the cervical os so that the tip reaches a depth of approximately 0.5 cm and rotate the swab 3 turns in a counterclockwise fashion and then gently wipe the surface of the ectocervix. Specimens obtained by BioImagene were collected within 3 weeks of a CIN3+ diagnosis. Specimens obtained by PATH were taken at the time of colposcopic evaluation without knowledge of the diagnosis. Use of the specimens was approved by internal review boards (IRB) and deemed exempt from IRB review by the NCI.
All specimens were shipped on dry ice, except for the 29 CIN3+ specimens from BioImagene, which had a cold chain break during shipment. Specimens from PPMM were stored for up to 1 week at −20°C and then transferred to −80°C for long-term storage. All other specimens were stored at −80°C for long-term storage. Specimens were thawed for approximately 10 min at ambient temperature before being tested.
(ii) HPV oncoprotein testing.
The E6 strip test is based on detection of HPV-E6 oncoprotein in cervical swab samples. The current prototype detects E6 oncoprotein of HPV type 16, type 18, and/or type 45 on three distinct test lines.
Briefly, the Dacron swab collection tip is placed in 0.933 ml of extraction buffer for 30 min with constant mixing. Then, 87 μl of proprietary buffer was added, and the mixture was incubated with mixing for another 30 min. The extracted, lysed specimen was clarified by centrifugation in a microcentrifuge at 13,000 × g for 10 min.
An aliquot of the specimen lysate (0.12 ml) was combined with a detector monoclonal antibody (MAb) cocktail consisting of two anti-E6 MAbs, one that binds to HPV16 E6 and another that binds to HPV18 E6 and HPV45 E6. Upon placement of the HPV E6 strip test into the vial containing the specimen lysate and alkaline phosphatase (AP)-conjugated detector MAbs, this mixture (referred to as test solution) migrated up the nitrocellulose membrane of the E6 strip test, driven by capillary forces. Capture of the E6 oncoprotein-detector MAb complex occurred using monoclonal anti-E6 oncoprotein antibodies (capture MAbs) immobilized onto the nitrocellulose membrane of the E6 strip test as three distinct “test lines.” Each test line consists of one capture MAb specific for HPV16 E6, HPV18 E6, or HPV45 E6. Conjugation of the detector MAbs with AP allowed for visualization of immobilized detector MAb via a colorimetric reaction with AP substrate, resulting in a red-purple deposit. A fourth line, located above the three test lines consisted of goat anti-mouse Ig antibody and served as an internal control for proper test solution flow and for proper function of the detection system. Test solution migration via the lateral-flow strip occurred over approximately 56 min. Next, the lateral-flow strip was placed into a small volume (0.05 ml) of wash solution for two 6-min wash steps. Finally, the lateral-flow strip was submerged into a vial with AP substrate solution, and the colorimetric reaction was developed for 15 min. After development and removal of the lateral-flow strip from the AP substrate vial, test outcome was obtained via visual inspection.
Aliquots of specimen lysates were also tested for 37 HPV genotypes as previously described (2). HPV types 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, and 68 were defined as the carcinogenic HPV genotypes (1).
Test results.
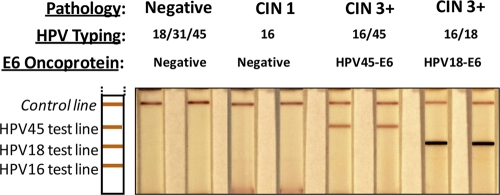
Table 1 shows the results of HPV16/18/45 E6 oncoprotein detection among cervical specimens that tested positive for HPV16, HPV18, and/or HPV45 DNA. Fifty-one of 75 (68%; 95% confidence interval [95% CI], 56 to 78%) of HPV16/18/45 DNA-positive specimens from women with a CIN3+ diagnosis tested positive for HPV16/18/45 E6 oncoprotein. None of the 16 (95% CI of 0 to 37%) HPV16/18/45 DNA-positive cervical specimens from women with a negative or CIN1 diagnosis tested positive for HPV16/18/45 E6 oncoprotein. Figure 1 shows examples of E6 oncoprotein-negative and -positive specimens run on the E6 strip test.
TABLE 1.
Results for HPV16, -18, and -45 E6 oncoprotein detection among specimens positive for HPV16/18/45 DNAa
| Histological diagnosis or scoreb | No. of specimens with the following test resultc: |
No. of specimens positive for HPV16/18/45d |
% HPV E6-positive/DNA-positive specimens (95% CI)e | ||||||
|---|---|---|---|---|---|---|---|---|---|
| HPV16 |
HPV18 |
HPV45 |
DNA | E6 | |||||
| DNA | E6 | DNA | E6 | DNA | E6 | ||||
| Negative | 6 | 0 | 1 | 0 | 2 | 0 | 8 | 0 | 0 (0-37) |
| CIN1 | 8 | 0 | 0 | 0 | 0 | 0 | 8 | 0 | 0 (0-37) |
| CIN3 | 29 | 15 | 5 | 3 | 0 | 2f | 34 | 20 | 59 (41-75) |
| CIN3+g | 24 | 12 | 5 | 4 | 3 | 1 | 25 | 17 | 68 (46-85) |
| Cancer | 15 | 13 | 1 | 1 | 0 | 1f | 16 | 14 | 62-98 |
| ≤CIN1 | 14 | 0 | 1 | 0 | 2 | 0 | 16 | 0 | 0 (0-37) |
| CIN3+ | 68 | 40 | 11 | 8 | 3 | 4 | 75 | 51 | 68 (56-78) |
| Total | 82 | 40 | 12 | 8 | 5 | 4 | 91 | 51 | 56 (45-66) |
The results of HPV16, -18, and -45 E6 oncoprotein detection are stratified by the severity of histologic diagnosis.
CIN1, cervical intraepithelial neoplasia grade 1; CIN3, cervical intraepithelial neoplasia grade 3; CIN3+, CIN3 or cancer.
The numbers of specimens with test results (negative test result or various CIN grades or cancer) for HPV16, HPV18, and HPV45 by DNA or E6 oncoprotein detection are shown.
The number of specimens positive for HPV16, -18, or -45 (HPV16/18/45) by DNA or E6 oncoprotein detection are shown.
The percentage of HPV E6-positive specimens among DNA-positive specimens and binomial 95% confidence interval (95% CI) are shown.
HPV16 DNA positive.
Reported as CIN3+ (did not differentiate whether the diagnosis was CIN3 or cervical cancer). Three cases were HPV18 E6 positive but were HPV18 DNA negative and HPV16 DNA positive.
FIG. 1.
Examples of E6 oncoprotein negative and positive results for specimens that tested positive for HPV16/18/45 DNA. Duplicate strips run from the same specimen are shown. The histopathology and the HPV DNA testing results are shown above the duplicate strips.
Among the 51 cases that tested positive for both HPV16/18/45 DNA and E6 oncoprotein, 4 tested DNA positive for more than one targeted HPV genotype, none of which were E6 positive for multiple targeted HPV genotypes. One tested E6 oncoprotein positive for HPV16 and HPV18 and was only DNA positive for HPV16. Classifying the results hierarchically based on cancer risk, 45 of 51 (88%) of the E6 and DNA positive tests were positive for the same HPV genotype (40 HPV16 and 5 HPV18); of the 6 discordant results, all tested HPV16 DNA positive, three tested positive for HPV18 E6 oncoprotein, and three tested positive for HPV45 E6 oncoprotein.
Table 2 shows the results of HPV16/18/45 E6 oncoprotein detection among cervical specimens that tested negative for HPV16, -18, and -45 DNA. Two of the 37 specimens (5.4%) from women with a negative or CIN1 diagnosis showed a weak positive test line for HPV16 E6 oncoprotein and negative for HPV DNA. Both these specimens belonged to the same collection performed more than 5 years ago. Therefore, it is possible that the long specimen storage time before use in the test contributed to these false positives. None of the 32 specimens from women with a CIN3+ diagnosis tested positive for HPV16 E6 oncoprotein.
TABLE 2.
Results for HPV16, -18, and -45 E6 oncoprotein detection among specimens negative for HPV16/18/45 DNAa
| Histological diagnosis or score | No. of specimens (%) negative for HPV16/18/45 |
% HPV E6-positive specimens/DNA-positive specimens | |
|---|---|---|---|
| DNA | E6 | ||
| Negative | 16 | 0 (0) | 0 |
| CIN1 | 21 | 2b (10) | 50 |
| CIN3 | 23 | 0 (0) | 0 |
| CIN3+c | 4 | 0 (0) | 0 |
| Cancer | 5 | 0 (0) | 0 |
| ≤CIN1 | 37 | 2 (5) | 17 |
| CIN3+ | 32 | 0 (0) | 0 |
The results of HPV16, -18, and -45 E6 oncoprotein detection are stratified by the severity of histological diagnosis.
Two specimens were HPV DNA negative and HPV16 E6 positive.
Reported as CIN3+ (did not differentiate whether the diagnosis was CIN3 or cervical cancer).
Conclusions.
We demonstrated that E6 detection from cervical swab specimens is both feasible and potentially more specific for CIN3+ than HPV DNA detection for the same HPV genotypes. The AV Avantage HPV E6 test prototype proved to be very specific for E6 oncoprotein of the targeted HPV genotypes. In about one third of all HPV16/18/45 DNA-positive CIN3 histology specimens, the test did not detect E6 oncoprotein. Only about one third of CIN3 cases progress to cervical cancer (4) over 30 years; notably, these CIN3 cases were found in older women and were presumably larger and more likely to progress on average than CIN3 found in routine screening (8). It is therefore possible but has not been demonstrated that these E6 oncoprotein-negative CIN3 cases may have never or not immediately progressed to cancer, if left untreated. It is also possible that some CIN3 was misclassified given the modest agreement for histological diagnosis of cervical biopsy specimens with different individuals rating the specimens (10). Additional carcinogenic HPV genotypes will be added to future versions of this test to provide better sensitivity for all CIN3+, not just those caused by HPV16, -18, and -45, which cause approximately 75% of all cervical cancer (9). The test can be run with minimal laboratory equipment, which may permit its deployment in low-resource settings, where it might be appropriate for direct triage to treatment. Further evaluations, especially in populations with a high HPV prevalence, such as human immunodeficiency virus-infected populations, are warranted.
Acknowledgments
P. E. Castle was supported (in part) by the Intramural Research Program of the NIH, National Cancer Institute. The AV Avantage HPV E6 test prototype development was a collaboration between Arbor Vita Corporation and PATH and was funded by NIH SBIR grants 2R43CA103383-01, 5R44CA121155-03, and 5R43 AI068160-02 and by a PATH grant through the START project, funded by the Bill & Melinda Gates Foundation.
Footnotes
Published ahead of print on 6 October 2010.
REFERENCES
- 1.Bouvard, V., R. Baan, K. Straif, Y. Grosse, B. Secretan, F. El Ghissassi, L. Benbrahim-Tallaa, N. Guha, C. Freeman, L. Galichet, and V. Cogliano on behalf of the WHO International Agency for Research on Cancer Monograph Working Group. 2009. A review of human carcinogens-Part B: biological agents. Lancet Oncol. 10:321-322. [DOI] [PubMed] [Google Scholar]
- 2.Castle, P. E., P. E. Gravitt, D. Solomon, C. M. Wheeler, and M. Schiffman. 2008. Comparison of linear array and line blot assay for detection of human papillomavirus and diagnosis of cervical precancer and cancer in the atypical squamous cell of undetermined significance and low-grade squamous intraepithelial lesion triage study. J. Clin. Microbiol. 46:109-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cuzick, J., C. Clavel, K. U. Petry, C. J. Meijer, H. Hoyer, S. Ratnam, A. Szarewski, P. Birembaut, S. Kulasingam, P. Sasieni, and T. Iftner. 2006. Overview of the European and North American studies on HPV testing in primary cervical cancer screening. Int. J. Cancer 119:1095-1101. [DOI] [PubMed] [Google Scholar]
- 4.McCredie, M. R., K. J. Sharples, C. Paul, J. Baranyai, G. Medley, R. W. Jones, and D. C. Skegg. 2008. Natural history of cervical neoplasia and risk of invasive cancer in women with cervical intraepithelial neoplasia 3: a retrospective cohort study. Lancet Oncol. 9:425-434. [DOI] [PubMed] [Google Scholar]
- 5.Parkin, D. M. 2006. The global health burden of infection-associated cancers in the year 2002. Int. J. Cancer 118:3030-3044. [DOI] [PubMed] [Google Scholar]
- 6.Qiao, Y. L., J. W. Sellors, P. S. Eder, Y. P. Bao, J. M. Lim, F. H. Zhao, B. Weigl, W. H. Zhang, R. B. Peck, L. Li, F. Chen, Q. J. Pan, and A. T. Lorincz. 2008. A new HPV-DNA test for cervical-cancer screening in developing regions: a cross-sectional study of clinical accuracy in rural China. Lancet Oncol. 9:929-936. [DOI] [PubMed] [Google Scholar]
- 7.Sankaranarayanan, R., B. M. Nene, S. S. Shastri, K. Jayant, R. Muwonge, A. M. Budukh, S. Hingmire, S. G. Malvi, R. Thorat, A. Kothari, R. Chinoy, R. Kelkar, S. Kane, S. Desai, V. R. Keskar, R. Rajeshwarkar, N. Panse, and K. A. Dinshaw. 2009. HPV screening for cervical cancer in rural India. N. Engl. J. Med. 360:1385-1394. [DOI] [PubMed] [Google Scholar]
- 8.Schiffman, M., and A. C. Rodriguez. 2008. Heterogeneity in CIN3 diagnosis. Lancet Oncol. 9:404-406. [DOI] [PubMed] [Google Scholar]
- 9.Smith, J. S., L. Lindsay, B. Hoots, J. Keys, S. Franceschi, R. Winer, and G. M. Clifford. 2007. Human papillomavirus type distribution in invasive cervical cancer and high-grade cervical lesions: a meta-analysis update. Int. J. Cancer 121:621-632. [DOI] [PubMed] [Google Scholar]
- 10.Stoler, M. H., and M. Schiffman. 2001. Interobserver reproducibility of cervical cytologic and histologic interpretations: realistic estimates from the ASCUS-LSIL Triage Study. JAMA 285:1500-1505. [DOI] [PubMed] [Google Scholar]