Abstract
We genotyped Streptococcus pneumoniae serotype 6C (Sp6C) isolates collected from Jewish and Bedouin children in southern Israel during the decade before vaccination. Sp6C constituted 8.2% of the presumed Sp6A isolates. All of the Sp6C clonal clusters were associated with serogroup 6, mainly Sp6A. Different clonal distributions were found in the two subpopulations.
Streptococcus pneumoniae serotype 6C (Sp6C) has recently been identified using monoclonal antibodies (8, 13). This serotype was previously typed as Sp6A by the quellung reaction. Genetic studies have found that the capsule gene locus of Sp6C is very similar to that of Sp6A, except for wciN; wciN6A encodes a galactosyltransferase, whereas wciN6C encodes a glucosyltransferase (12). Since the two genes are completely divergent in nucleotide sequence, they can be differentiated by a specific PCR assay (1, 12). Studies in the United States (9, 11) documented a stepwise annual increase in the incidence of invasive disease caused by Sp6C following the implementation of the 7-valent pneumococcal conjugate vaccine (PCV7). Another study in the United States (7) demonstrated an increased incidence of both invasive and noninvasive Sp6C strains, almost half carrying multidrug resistance. In this study (7), most of the genotypes, identified by base composition analysis of internal fragments of the multilocus sequence typing (MLST) loci, were closely related to Sp6A and Sp6B strains, indicating likely capsular switching from serotypes 6A and 6B. Some of these genotypes were rarely associated with other serotypes; e.g., ST690 and ST1390 represent strains of serotype 19A too. Gertz et al. have also documented an increase in the prevalence of invasive, non-penicillin-susceptible Sp6C in the United States in the post-PCV7 era (6). Carriage data from children in Portugal (10) also showed an increased prevalence of Sp6C with diverse genetic background and with increasing antibiotic resistance rates, including multidrug resistance.
PCV7 was introduced into the national immunization program in Israel in July 2009. Surveillance of newly emerging serotypes is important for the design of new vaccines. The aims of this study were to identify Sp6C from previously characterized Sp6A in southern Israel during the decade (1999 to 2008) before PCV7 implementation and to describe the circulation of Sp6C clones among two distinct ethnic subpopulations of children <5 years old.
The study population consisted of Jewish children with a lifestyle resembling that of developed populations and Moslem Bedouin children with a lifestyle resembling that of developing populations (15). The Soroka University Medical Center is the only general hospital providing full health services to the entire population of southern Israel (590,000 persons; The Israel Central Bureau of Statistics, 2008).
S. pneumoniae isolates were cultured from four isolation sites: blood/cerebrospinal fluid (CSF), middle ear fluid (MEF), conjunctiva, and nasopharyngeal (NP) cultures (17). Identification, antimicrobial susceptibility testing, and serotyping were performed as previously described (15). Of 1,396 presumed Sp6A isolates, 1,299 (93.1%) were available for Sp6C typing by PCR (12). Sp6C constituted 8.2% (106/1,299) of the presumed Sp6A isolates: 2/27 (7.4%) from blood/CSF, 8/262 (3.1%) from MEF, 5/84 (6.0%) from conjunctiva, and 91/926 (9.8%) from NP cultures. Sp6C constituted 9.8% (54/552) of the presumed Sp6A isolates from Jewish children and 7.0% (52/747) of those from Bedouin children (P = 0.066). Most of the isolates (100/106, 94.3%) were susceptible to all of the antibiotics tested. Only 6/106 (5.7%) were penicillin nonsusceptible, and of these, only 1 was multidrug resistant.
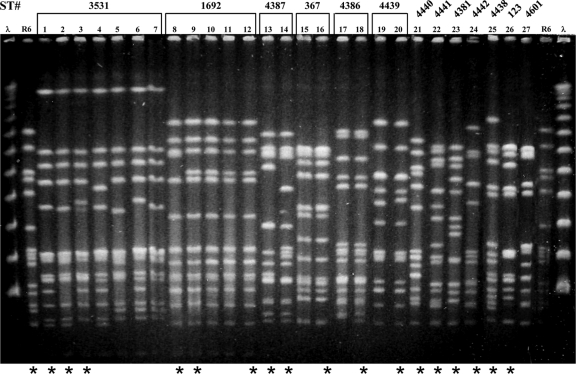
Pulsed-field gel electrophoresis (PFGE) (16) (Fig. 1) revealed the presence of two major and four minor clusters, which constituted 76.4% (81/106) and 17.0% (18/106) of the Sp6C strains, respectively. Seven isolates exhibited unique PFGE patterns. Representative strains from each PFGE cluster and all of the strains with unique PFGE patterns (a total of 18 isolates) were further characterized by MLST (5; www.mlst.net [queried on 07/21/2010]) (Table 1), which yielded four known and nine novel sequence types (STs). eBURST analysis (http://spneumoniae.mlst.net/eburst) based on the minimal similarity of five of seven identical loci (double-locus variant [DLV]) revealed that all of the clones (except the singletons, i.e., ST4438, ST4439, ST4440, ST4441, and ST4386 and ST4387, which are single-locus variants [SLVs] of each other) belonged to clonal clusters that were formerly associated with Sp6A and/or Sp6B; e.g., major clone ST3531 is a DLV of STs primarily recorded among Sp6B and is a triple-locus variant of ST176, which is very common among Sp6B strains.
FIG. 1.
PFGE patterns of chromosomal SmaI digests of Sp6C isolated from children in southern Israel from 1999 to 2008. Strains marked by asterisks were characterized by MLST (Table 1). Lanes 1 to 7, ST3531; lanes 8 to 12, ST1692; lanes 13 and 14, ST4387; lanes 15 and 16, ST367; lanes 17 and 18, ST4386; lanes 19 and 20, ST4439; lane 21, ST4440; lane 22, ST4441; lane 23, ST4381; lane 24, ST4442; lane 25, ST4438; lane 26, ST123; lane 27, ST4601. λ, lambda ladder; R6, S. pneumoniae reference strain used as a molecular weight marker.
TABLE 1.
Molecular characteristics of Sp6C isolates from Jewish and Bedouin children in southern Israel from 1999 to 2008: distribution by isolation site
| ST | Total no. of isolatesa | No. (%)b from: |
No. from: |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| NP |
MEF |
Conjunctiva |
Blood |
||||||||
| Jc | Bd | J | B | J | B | J | B | J | B | ||
| ST3531 | 52 | 8 (14.8) | 44 (84.6) | 7 | 37 | 1 | 4 | 0 | 3 | 0 | 0 |
| ST1692 | 29 | 28 (51.9) | 1 (1.9) | 27 | 1 | 1 | 0 | 0 | 0 | 0 | 0 |
| ST4387 | 5 | 5 (9.3) | 0 | 5 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| ST4386 | 5 | 5 (9.3) | 0 | 4 | 0 | 0 | 0 | 1 | 0 | 0 | 0 |
| ST367 | 6 | 2 (3.7) | 4 (7.7) | 2 | 4 | 0 | 0 | 0 | 0 | 0 | 0 |
| ST4439 | 2 | 2 (3.7) | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| ST4438 | 1 | 1 (1.9) | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| ST123 | 1 | 1 (1.9) | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| ST4601 | 1 | 1 (1.9) | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 |
| ST4440 | 1 | 0 | 1 (1.9) | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 |
| ST4441 | 1 | 0 | 1 (1.9) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 |
| ST4442 | 1 | 0 | 1 (1.9) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 |
| ST4381 | 1 | 1 (1.9) | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 |
| Total | 106 | 54 | 52 | 49 | 42 | 4 | 4 | 1 | 4 | 0 | 2 |
Number of isolates based on PFGE data and MLST of representative isolates of each PFGE cluster (a total of 18).
Percentage of each clone in the total number of Sp6C isolates from each ethnic group.
J, Jewish children.
B, Bedouin children.
Comparison of clonal distributions between Jewish and Bedouin children, using the χ2 method, was based on NP isolates only (91/106, 85.8%) due to the small number (15/106, 14.2%) of Sp6C isolates from other sources. A P value of <0.05 was considered significant.
The most dominant clone, ST3531, constituted 14.3% (7/49) of the isolates from Jews versus 88.1% (37/42) of those from Bedouins (P < 0.001), while the second most prevalent clone, ST1692, constituted 55.1% (27/49) of the isolates from Jews versus 2.4% (1/42) of those from Bedouins (P < 0.001). All of the penicillin-nonsusceptible isolates (two intermediate, three resistant, and one multidrug resistant) were included in this ST and were isolated from the NPs of Jewish children in 2008 (the last year of the study). Two additional groups, ST4387 (five isolates) and ST4386 (four isolates), were also recovered from Jewish children only.
Noteworthy is the fact that the two invasive isolates had unique STs, ST4441 and ST4442, which were not found among mucosal strains. However, ST4442 is an SLV of ST367 found within six of the NP isolates described here.
Our study shows that Sp6C has been circulating in Israel for more than a decade. As shown by others (1, 4, 10), this serotype is frequently found in the NPs of healthy children and is also causing mucosal and invasive diseases. Only 6% of the Sp6C isolates in our study were penicillin nonsusceptible. The resistant strains emerged in the last year of the study; further analysis is needed to assess their prevalence in the future.
Characterization of the strains by PFGE and MLST revealed the presence of 13 genotypes, 9 of which were first described in this study. One cannot rule out the possibility that more STs were present than detected, given that not all of the isolates were evaluated by MLST. All of the Sp6C STs detected in this study (except the singletons) are associated with serogroup 6, mainly Sp6A, which makes it very likely that horizontal transfer of the wciN6C genetic element has repeatedly involved serogroup 6 recipients.
The clonal distributions between the two study populations, Jewish and Bedouin children, were different due to the rarity of contact between them. Different clonal distributions among the two study populations were already shown by us for serotypes 19A and 6A (3, 15).
PCV7 does not confer protection against Sp6C (11), and therefore, its introduction is expected to lead to the expansion of non-vaccine-type strains, including Sp6C. Since the Sp6C clones found in this study have been around for more than a decade among Israeli children, their prevalence is expected to increase after the introduction of PCV7. Recently, Park et al. (14) have shown that an experimental PCV2 containing capsular types 6A and 23F induced opsonic responses to Sp6A, Sp6B, and Sp6C. Hence, the new 13-valent PCV containing serotype 6A, which was recently licensed in the United States (2), may provide sufficient protection also against serotype 6C (8). Further surveillance is needed to assess the importance of this serotype and to consider its inclusion in future PCVs.
Acknowledgments
We thank Rachel Benisty for her useful remarks and Ronit Trefler for technical assistance.
This work was partially supported by a grant from Wyeth (0887X1-4463) to N.P. and an NIH grant (AI-31473) to M.H.N.
Footnotes
Published ahead of print on 13 October 2010.
REFERENCES
- 1.Carvalho, M. D., F. C. Pimenta, R. E. Gertz, Jr., H. H. Joshi, A. A. Trujillo, L. E. Keys, J. Findley, I. S. Moura, I. H. Park, S. K. Hollingshead, T. Pilishvili, C. G. Whitney, M. H. Nahm, and B. W. Beall for the Active Bacterial Core Surveillance Team. 2009. PCR-based quantitation and clonal diversity of the current prevalent invasive serogroup 6 pneumococcal serotype, 6C, in the United States in 1999 and 2006 to 2007. J. Clin. Microbiol. 47:554-559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. 2010. Licensure of a 13-valent pneumococcal conjugate vaccine (PCV13) and recommendations for use among children—Advisory Committee on Immunization Practices (ACIP), 2010. Morbid. Mortal. Wkly. Rep. 59:258-261. [PubMed] [Google Scholar]
- 3.Dagan, R., N. Givon-Lavi, E. Leibovitz, D. Greenberg, and N. Porat. 2009. Introduction and proliferation of multidrug-resistant Streptococcus pneumoniae serotype 19A clones that cause acute otitis media in an unvaccinated population. J. Infect. Dis. 199:776-785. [DOI] [PubMed] [Google Scholar]
- 4.du Plessis, M., A. von Gottberg, S. A. Madhi, O. Hattingh, L. de Gouveia, and K. P. Klugman. 2008. Serotype 6C is associated with penicillin-susceptible meningeal infections in human immunodeficiency virus (HIV)-infected adults among invasive pneumococcal isolates previously identified as serotype 6A in South Africa. Int. J. Antimicrob. Agents 32(Suppl. 1):S66-S70. [DOI] [PubMed] [Google Scholar]
- 5.Enright, M. C., and B. G. Spratt. 1998. A multilocus sequence typing scheme for Streptococcus pneumoniae: identification of clones associated with serious invasive disease. Microbiology 144(Pt. 11):3049-3060. [DOI] [PubMed] [Google Scholar]
- 6.Gertz, R. E., Jr., Z. Li, F. B. Pimenta, D. Jackson, B. A. Juni, R. Lynfield, J. H. Jorgensen, Mda. G. Carvalho, and B. W. Beall. 2010. Increased penicillin nonsusceptibility of nonvaccine-serotype invasive pneumococci other than serotypes 19A and 6A in post-7-valent conjugate vaccine era. J. Infect. Dis. 201:770-775. [DOI] [PubMed] [Google Scholar]
- 7.Jacobs, M. R., S. Bajaksouzian, R. A. Bonomo, C. E. Good, A. R. Windau, A. M. Hujer, C. Massire, R. Melton, L. B. Blyn, D. J. Ecker, and R. Sampath. 2009. Occurrence, distribution, and origins of Streptococcus pneumoniae serotype 6C, a recently recognized serotype. J. Clin. Microbiol. 47:64-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lin, J., M. S. Kaltoft, A. P. Brandao, G. Echaniz-Aviles, M. C. Brandileone, S. K. Hollingshead, W. H. Benjamin, and M. H. Nahm. 2006. Validation of a multiplex pneumococcal serotyping assay with clinical samples. J. Clin. Microbiol. 44:383-388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nahm, M. H., J. Lin, J. A. Finkelstein, and S. I. Pelton. 2009. Increase in the prevalence of the newly discovered pneumococcal serotype 6C in the nasopharynx after introduction of pneumococcal conjugate vaccine. J. Infect. Dis. 199:320-325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nunes, S., C. Valente, R. Sa-Leao, and H. de Lencastre. 2009. Temporal trends and molecular epidemiology of recently described serotype 6C of Streptococcus pneumoniae. J. Clin. Microbiol. 47:472-474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Park, I. H., M. R. Moore, J. J. Treanor, S. I. Pelton, T. Pilishvili, B. Beall, M. A. Shelly, B. E. Mahon, and M. H. Nahm. 2008. Differential effects of pneumococcal vaccines against serotypes 6A and 6C. J. Infect. Dis. 198:1818-1822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Park, I. H., S. Park, S. K. Hollingshead, and M. H. Nahm. 2007. Genetic basis for the new pneumococcal serotype, 6C. Infect. Immun. 75:4482-4489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Park, I. H., D. G. Pritchard, R. Cartee, A. Brandao, M. C. Brandileone, and M. H. Nahm. 2007. Discovery of a new capsular serotype (6C) within serogroup 6 of Streptococcus pneumoniae. J. Clin. Microbiol. 45:1225-1233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Park, S., P. D. Fernsten, and M. H. Nahm. 2009. Functional cross-reactivity within Streptococcus pneumoniae serogroup 6 elicited by pneumococcal conjugate and polysaccharide vaccines, abstr. G1-1006. 49th Intersci. Conf. Antimicrob. Agents Chemother., San Francisco, CA.
- 15.Porat, N., U. Amit, N. Givon-Lavi, E. Leibovitz, and R. Dagan. 2010. Increasing importance of multidrug-resistant serotype 6A Streptococcus pneumoniae clones in acute otitis media in southern Israel. Pediatr. Infect. Dis. J. 29:126-130. [DOI] [PubMed] [Google Scholar]
- 16.Porat, N., G. Barkai, M. R. Jacobs, R. Trefler, and R. Dagan. 2004. Four antibiotic resistant S. pneumoniae clones unrelated to the pneumococcal conjugate vaccine serotypes, including 2 new serotypes, causing acute otitis media in southern Israel. J. Infect. Dis. 189:385-392. [DOI] [PubMed] [Google Scholar]
- 17.Shouval, D. S., D. Greenberg, N. Givon-Lavi, N. Porat, and R. Dagan. 2006. Site-specific disease potential of individual Streptococcus pneumoniae serotypes in pediatric invasive disease, acute otitis media and acute conjunctivitis. Pediatr. Infect. Dis. J. 25:602-607. [DOI] [PubMed] [Google Scholar]