Abstract
Objective
The validity of using adult physiologic criteria to triage injured children in the out-of-hospital setting remains unproven. Among children meeting adult field physiologic criteria, we assessed the availability of physiologic information, the incidence of death or prolonged hospitalization, and whether age-specific criteria would improve the specificity of the physiologic triage step.
Methods
We analyzed a prospective, out-of-hospital cohort of injured children aged ≤14 years collected from December 2005 through February 2007 by 237 emergency medical services (EMS) agencies transporting to 207 acute care hospitals (trauma and nontrauma centers) in 11 sites across the United States and Canada. Inclusion criteria were standard adult physiologic values: systolic blood pressure (SBP) ≤90 mmHg, respiratory rate <10 or >29 breaths/min, Glasgow Coma Scale (GCS) score ≤12, and field intubation attempt. Seven physiologic variables (including age-specific values) and three demographic and mechanism variables were included in the analysis. “High-risk” children included those who died (field or in-hospital) or were hospitalized >2 days. The decision tree was derived and validated using binary recursive partitioning.
Results
Nine hundred fifty-five children were included in the analysis, of whom 62 (6.5%) died and 117 (12.3%) were hospitalized >2 days. Missing values were common, ranging from 6% (respiratory rate) to 53% (pulse oximetry), and were associated with younger age and high-risk outcome. The final decision rule included four variables (assisted ventilation, GCS score <11, pulse oximetry <95%, and SBP >96 mmHg), which demonstrated improved specificity (71.7% [95% confidence interval (CI) 66.7–76.6%]) at the expense of missing high-risk children (sensitivity 76.5% [95% CI 66.4–86.6%]).
Conclusions
The incidence of high-risk injured children meeting adult physiologic criteria is relatively low and the findings from this sample do not support using age-specific values to better identify such children. However, the amount and pattern of missing data may compromise the value and practical use of field physiologic information in pediatric triage.
Keywords: trauma, physiologic, emergency medical services, out-of-hospital, triage, children
INTRODUCTION
Rapid field identification of children with serious injury is vitally important in ensuring appropriate downstream hospital care and health outcomes. Previous studies have demonstrated that children with serious injuries have improved survival when cared for at hospitals capable of providing high-quality pediatric trauma care.1−5 However, a minority of hospitals in the United States have this capacity.6 Because many injured children will have medical care initiated through the 9-1-1 response system, primary triage decisions by emergency medical services (EMS) personnel play a major role in determining subsequent hospital care. Ideally, the capabilities of receiving hospitals are matched to the anticipated needs of injured children. This process is challenged by the limited information obtained during a short time period in a frequently chaotic environment at the scene.
Objective, field-based trauma triage criteria may provide a standardized means of differentiating children with potentially serious injuries from those with minor injuries, although such criteria must be derived and validated in a pediatric population. Most U.S. trauma systems currently use triage guidelines modeled from the American College of Surgeons Committee on Trauma (ACSCOT) field decision scheme, which was developed primarily from adult trauma research.7 The first “step” in the ACSCOT decision scheme uses physiologic values that are widely believed to identify the highest-risk trauma patients,8−13 though their utility in identifying children with serious injury remains unclear. Because adult triage practices are inexact, extrapolating such results to a pediatric population creates additional uncertainty in their ability to identify children in need of trauma center care.
Some trauma and EMS systems have integrated pediatric-specific field triage criteria (e.g., age-specific systolic blood pressure [SBP] values). However, there are studies showing no difference in the predictive value between adult and pediatric-specific physiologic criteria14−16 and others demonstrating outcome differences using age-specific values.17,18 In addition to predictive value, previous research has suggested that certain vital signs (i.e., blood pressure) are frequently missing in the field assessment of young children and that paramedic confidence and skills in acquiring vital signs vary dramatically by patient age.19 Defining the availability, role, and predictive value of field physiologic information for identifying seriously injured children may facilitate improved primary pediatric triage practices and the effective regional distribution of injured children to appropriate hospitals in a trauma system.
In this study, we evaluated injured children meeting standard adult field physiologic criteria in 11 North American sites to 1) provide an unbiased estimate of the incidence of mortality and prolonged hospital stay; 2) assess the availability of field physiologic information by age group and outcome; and 3) evaluate whether more restrictive or age-specific physiologic criteria would improve the specificity of the physiologic triage step without missing high-risk children.
METHODS
Study Design
We analyzed an out-of-hospital, consecutive-patient, prospective cohort registry of injured children aged ≤14 years in whom resuscitation was attempted and field-based physiologic abnormality was documented. This is a companion pediatric study to a similar project focusing on field physiology in adults.20
Setting
These data were collected as part of the Resuscitation Outcomes Consortium (ROC) epidemiologic out-of-hospital trauma registry (the “ROC Epistry–Trauma”), described in detail elsewhere.21 Population-based data were collected from December 1, 2005, through February 28, 2007, by 237 EMS agencies transporting to 207 acute care hospitals (both trauma centers and non–trauma centers) in 11 sites across the United States and Canada. The 11 participating sites included eight U.S. locations (Birmingham, AL; Dallas, TX; Iowa City, IA; Milwaukee, WI; Pittsburgh, PA; Portland, OR; San Diego, CA; and King County, WA) and three Canadian locations (Ottawa, Toronto, and Vancouver), which vary in size, location, geographic diversity, and EMS system structure.22 One hundred fifty-three institutional review boards/research ethics boards (127 hospital-based and 26 EMS agency-based) in both the United States and Canada reviewed and approved the ROC Epistry–Trauma project and waived the requirement for informed consent.
Selection of Participants
The study cohort consisted of consecutive injured children (age ≤14 years) for whom the emergency 9-1-1 response system was activated within predefined geographic regions of each ROC site. Inclusion criteria were EMS provider evaluation and the presence of standard, field-based adult physiologic criteria7 at any point during out-of-hospital evaluation. The physiologic criteria included SBP ≤90 mmHg, respiratory rate <10 or >29 breaths/min, Glasgow Coma Scale (GCS) score ≤12, or attempted field intubation. These inclusion criteria were based on ACSCOT physiologic trauma triage guidelines7 with previously demonstrated high specificity for serious injury and trauma resources among adults8−13 and represent the physiologic criteria applied to injured children in most U.S. trauma systems. “Injury” was broadly defined as any blunt, penetrating, or burn mechanism for which the EMS provider(s) believed trauma to be the primary clinical insult. We selected age ≤14 years to define “pediatric” for several reasons: This age range is used to define children in many trauma systems; the companion study to this project used a definition of ≥15 years for “adults”; by 14 years, the relationship between physiologic response to injury and outcome is very similar to that in adults23; and older adolescents frequently have different factors affecting injury risk (e.g., driving motor vehicles, increased risk-taking behavior, and alcohol and drug use). Injured children meeting the above criteria were included in the study regardless of subsequent events (e.g., death in the field after resuscitation), the receiving hospital to which they were transported (e.g., trauma center versus non–trauma center), or whether they were subsequently transferred to another acute care hospital. Children judged by EMS responders to be dead on EMS arrival with no resuscitation attempted were excluded from this analysis.
Methods of Measurement
Out-of-hospital variables routinely collected by EMS providers were included in the analysis. These variables included seven physiologic measures: SBP (mmHg), respiratory rate (breaths/min), GCS score, pulse rate (beats/min), pulse oximetry (percentage oxyhemoglobin saturation), shock index (pulse rate/SBP), and ventilatory support (either by bag–valve–mask ventilation or advanced airway management [intubation, supraglottic airway, or cricothyrotomy]) at any point during the field evaluation. Because the use of field intubation in children has been questioned24 and is variable among EMS agencies and regions, assisted ventilation procedures (advanced airway and bag–valve–mask) were combined for all analyses.
Initial physiologic values were used in the primary analysis to minimize the potential for bias when analyzing subsequent values (e.g., sicker children or those with longer transport times may be more likely to have repeat vital signs), to avoid the difficulty in interpreting vital signs performed after EMS interventions (e.g., intravenous fluid, use of sedatives and/or paralytics, or intubation), and because triage decisions generally need to be made early in the course of field evaluation. However, to evaluate the potential for misclassifying patients based on the use of initial values (i.e., children who had subsequent physiologic deterioration following the initial assessment), we also assessed the “worst” field physiologic values across the duration of out-of-hospital care.
Two strategies were used to account for potential age-specific relationships among physiologic measures. First, age (years) was included in all analyses to allow for effect modification (interaction) between physiologic measures and age. Second, age-specific values for hypotension and abnormal respiratory rates were also included in the analysis, based on standard reference texts and pediatric resuscitation courses.25−27 Age-specific values for GCS score were not used because previous research has demonstrated no change in GCS performance by age.18,28 For age-specific values, age groups were divided as follows: 0–1 years (infant), 2–3 years (toddler), 4–5 years (preschool), 6–10 years (grade school, nonadolescent), and 11–14 years (adolescent).23,26 Additional variables included gender, mechanism of injury (motor vehicle, cyclist, pedestrian, stabbing, firearm, machinery, fall, or other), and injury type (blunt, penetrating, or burn). These measures were considered in combination with the physiologic measures to determine whether such variables could further improve predictive value.
Data Collection and Processing
The data collection, processing, and quality assurance for ROC Epistry–Trauma have been described in detail elsewhere.21 In brief, all variables were collected by on-site EMS providers and were not influenced by information provided after in-hospital evaluation. Investigative teams at each ROC site identified eligible out-of-hospital trauma patients from participating EMS agencies at the site and entered data from each agency into standardized data forms (web-based data entry or batch upload). EMS data were then matched to hospital outcomes, de-identified, and submitted to a central data coordinating center. ROC site quality assurance processes included initial training and continuing education of EMS providers for data collection, data element range and consistency checks during data entry, and annual site visits to review randomly selected study records, data capture processes, and site-specific mechanisms for quality assurance.
Outcome Measure
The primary outcome was mortality (whether out-of-hospital or in-hospital) or hospital length of stay (LOS) greater than two days. Children with the primary outcome are referred to as “high-risk” in this paper. W0068ile a portion of early deaths following resuscitation efforts may have represented cases in which further care was futile or in which injuries were nonsurvivable regardless of aggressive care, we opted to include such children in the analysis to minimize the potential for selection bias. A portion of such fatalities may have also been preventable with early aggressive trauma care, interventional therapies, or timely surgery. Hospital LOS was included in the composite outcome as a surrogate marker for serious injuries and the need for specialized trauma care (i.e., surgical intervention, blood transfusion, intensive care unit stay, or prolonged ventilation) among survivors. Detailed hospital-based outcomes are not available in the ROC Epistry–Trauma because data from hospital chart abstraction were limited by resource constraints. The LOS threshold (>2 days) was used to exclude children who were admitted for “observation” with limited or no interventions and therefore unlikely to have required immediate trauma center care (i.e., those with minor injuries). Hospital LOS, including the >2-day cutpoint used for this study, has been validated as a surrogate measure of injury severity and resource use among pediatric survivors in heterogeneous injury populations cared for in more than 380 hospitals.29
Data Analysis
We used descriptive statistics to compare groups with and without the primary outcome, as well as the proportion of missing values by age group. We then used binary recursive partitioning to derive and validate a decision rule using the out-of-hospital factors described above. Recursive partitioning is an analytic method well suited for identifying complex, higher-level interactions among variables, selecting appropriate cutpoints in continuous predictors, and generating highly sensitive decision rules.30,31 Every variable is considered as a possible predictor at each decision node (branch) in the tree, regardless of whether or not it has been used previously. The decision tree is built through an iterative process where branches in the tree are grown to further split (partition) the data into subgroups based on predicted outcome. The selection of splits lower in the tree is necessarily conditioned on the previous splits. The final tree is “pruned” to balance the need for simplicity with predictive value. Misclassification costs were selected with a goal of producing a highly sensitive (i.e., 90% or greater) decision rule, while also having moderate specificity (50% or greater) and being practical for field application. Because children meeting the Epistry inclusion criteria already fulfilled triage criteria for transport to a trauma center, we sought to preserve the sensitivity while increasing the specificity and, therefore, the predictive value of these criteria. Sixty percent of the sample was randomly selected to derive the rule, with the remaining 40% of children used for rule validation.
The primary analysis was restricted to the seven physiologic measures and age to remain consistent with the “physiologic” step 1 of the standard field decision scheme. Age-specific values for hypotension and abnormal respiratory rates were also included. Three additional variables (gender, injury mechanism, and injury type) were included in a supplemental analysis to assess whether such factors would improve performance of the resulting decision rule.
We used several strategies to minimize bias and account for missing values in the analysis. During data collection, site and agency case enrollment was evaluated monthly. Sites or agencies that had substantially higher or lower case capture (relative to their average) for a given month, as measured using a Poisson distribution with a 5% cutoff, were sent inquiries in an attempt to understand whether such fluctuations were secondary to natural variation versus biased case capture. These assessments were used to improve identification of eligible children and to select a time period for the sample when case capture appeared uniformly present. Because missing values for physiologic measures appeared to vary by age, we used two methods to handle missing values in the analysis: single imputation (imputing missing values using age-specific norms26) and coding missing values using a separate predictor term to assess whether “missingness” itself serves as a predictor of outcome. We did not use multiple imputation to handle missing values because of the difficulty in combining decision trees across multiply imputed data sets. The dates for enrollment and the resulting sample size were based on the inception of the ROC Epistry–Trauma database (December 1, 2005) through the most recent date demonstrating complete case capture and a high level of outcome completion (February 28, 2007).
All analyses performed for this article used R v2.4.0 and the rpart library v3.1-32 (Free Software Foundation Inc., Boston, MA).
RESULTS
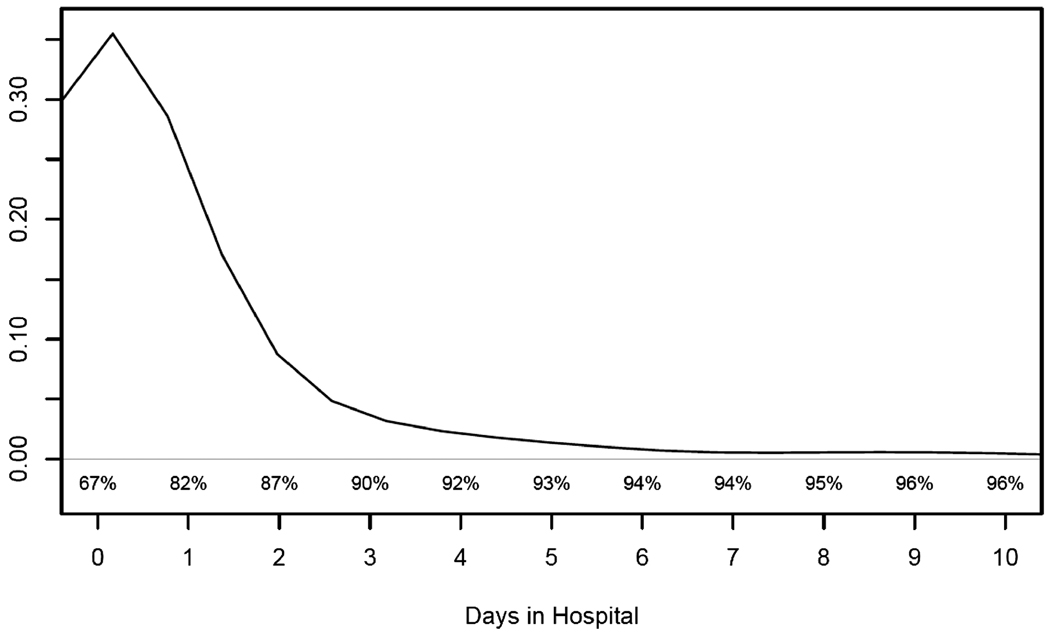
There were 1,096 out-of-hospital pediatric trauma patients meeting the physiologic inclusion criteria and having EMS field resuscitation over the 15-month period. After excluding 141 (12.9%) patients with missing outcome information, 955 children were retained for the analysis. Sixty-two (6.5%) children died following EMS resuscitative efforts, of whom seven (11.3% of deaths) children died in the field without transport and 55 died following transport to a hospital. One hundred seventeen (12.3%) children survived and were hospitalized more than two days, while 601 (62.9%) were discharged alive on the same day of evaluation. The distribution of hospital stay among survivors is illustrated in Figure 1. In total, 179 (18.7%) children died or required more than two days in the hospital.
FIGURE 1.
Length-of-stay distribution among survivors (n = 893).
Descriptive characteristics of the cohort are provided in Table 1. Differences were evident between high- and low-risk children for depressed GCS score, ventilatory assistance, SBP ≤90 mmHg, and abnormal respiratory rate. Similar trends were seen among children with only a single physiologic criterion for entry into the sample. Injured children with isolated abnormal respiratory rates or “hypotension” (by adult values) were frequently discharged alive from the hospital within two days (i.e., low risk).
TABLE 1.
Characteristics of Injured Children Meeting the American College of Surgeons Committee on Trauma Step 1 Field Triage Decision Scheme Physiologic Criteria*
| Total (N = 955) | Alive and LOS ≤2 Days (n = 776) | Death or LOS >2 Days (n = 179) | |
|---|---|---|---|
| Out-of-hospital physiologic characteristics | |||
| Site A | 2 (0.2%) | 2 (0.3%) | 0 (0.0%) |
| Site B | 11 (1.2%) | 2 (0.3%) | 9 (5.0%) |
| Site C | 109 (11.4%) | 83 (10.7%) | 26 (14.5%) |
| Site D | 254 (26.6%) | 234 (30.1%) | 20 (11.2%) |
| Site E | 32 (3.4%) | 15 (1.9%) | 17 (9.5%) |
| Site F | 52 (5.5%) | 37 (4.8%) | 15 (8.4%) |
| Site G | 74 (7.8%) | 62 (8.0%) | 12 (6.7%) |
| Site H | 226 (23.7%) | 202 (26.0%) | 24 (13.4%) |
| Site I | 86 (9.0%) | 72 (9.3%) | 14 (7.8%) |
| Site J | 12 (1.3%) | 3 (0.4%) | 9 (5.0%) |
| Site K | 97 (10.2%) | 64 (8.3%) | 33 (18.4%) |
| GCS score ≤12 | 180 (18.9%) | 98 (12.6%) | 82 (45.8%) |
| SBP ≤90 mmHg | 400 (41.9%) | 357 (46.0%) | 43 (24.0%) |
| Respiratory rate <10 or >29 breaths/min | 443 (46.4%) | 364 (46.9%) | 79 (44.1%) |
| Advanced airway† | 68 (7.1%) | 13 (1.7%) | 55 (30.7%) |
| Advanced airway† or bag–mask | 108 (11.3%) | 25 (3.2%) | 83 (46.4%) |
| Single physiologic criteria: | 761 (79.7%) | 662 (85.3%) | 99 (55.3%) |
| GCS score ≤12 | 82 (8.6%) | 55 (7.1%) | 27 (15.1%) |
| SBP ≤90 mmHg | 319 (33.4%) | 303 (39.0%) | 16 (8.9%) |
| Respiratory rate <10 or >29 breaths/min | 334 (35.0%) | 301 (38.8%) | 33 (18.4%) |
| Advanced airway† | 26 (2.7%) | 3 (0.4%) | 23 (12.8%) |
| Additional physiologic information | |||
| Mean Pulse rate (beats/min) | 112 (28.7) | 114 (25.5) | 99.6 (38.9) |
| Mean Shock index (pulse/SBP) | 1.14 (0.32) | 1.16 (0.31) | 1.01 (0.35) |
| Mean Pulse oximetry (%) | 97.7 (7.36) | 98.3 (5.52) | 95.3 (12.0) |
| Additional out-of-hospital characteristics | |||
| Mean Age (years) | 5.23 (4.57) | 4.87 (4.39) | 6.78 (5.01) |
| Gender—male | 582 (60.9%) | 459 (59.1%) | 123 (68.7%) |
| Mechanism of injury | |||
| Motor vehicle | 140 (14.7%) | 109 (14.1%) | 31 (17.3%) |
| Cyclist or pedestrian | 117 (12.3%) | 66 (8.5%) | 51 (28.5%) |
| Stabbing or firearm | 36 (3.8%) | 17 (2.2%) | 19 (10.6%) |
| Fall | 428 (44.8%) | 394 (50.8%) | 34 (19.0%) |
| Other | 221 (23.1%) | 180 (23.2%) | 41 (22.9%) |
| Penetrating injury type | 48 (5.0%) | 28 (3.6%) | 20 (11.2%) |
| Burns | 54 (5.7%) | 36 (4.6%) | 18 (10.1%) |
| Hospital trauma level | |||
| Level I | 446 (46.7%) | 315 (40.6%) | 131 (73.2%) |
| Level II | 36 (3.8%) | 21 (2.7%) | 15 (8.4%) |
| Level III | 216 (22.6%) | 202 (26.0%) | 14 (7.8%) |
| Level IV | 47 (4.9%) | 47 (6.1%) | 0 (0%) |
| Not accredited, other, or unknown | 210 (22.0%) | 191 (24.6%) | 19 (10.6%) |
Values presented represent the mean (standard deviation) or proportions of continuous and categorical covariates, respectively. Values are based on column totals.
Advanced airway use included any of the following: intubation (oral or nasopharyngeal), supraglottic airway (e.g., Combitube), or cricothyrotomy.
GCS = Glasgow Coma Scale score; LOS = length of stay; SBP = systolic blood pressure.
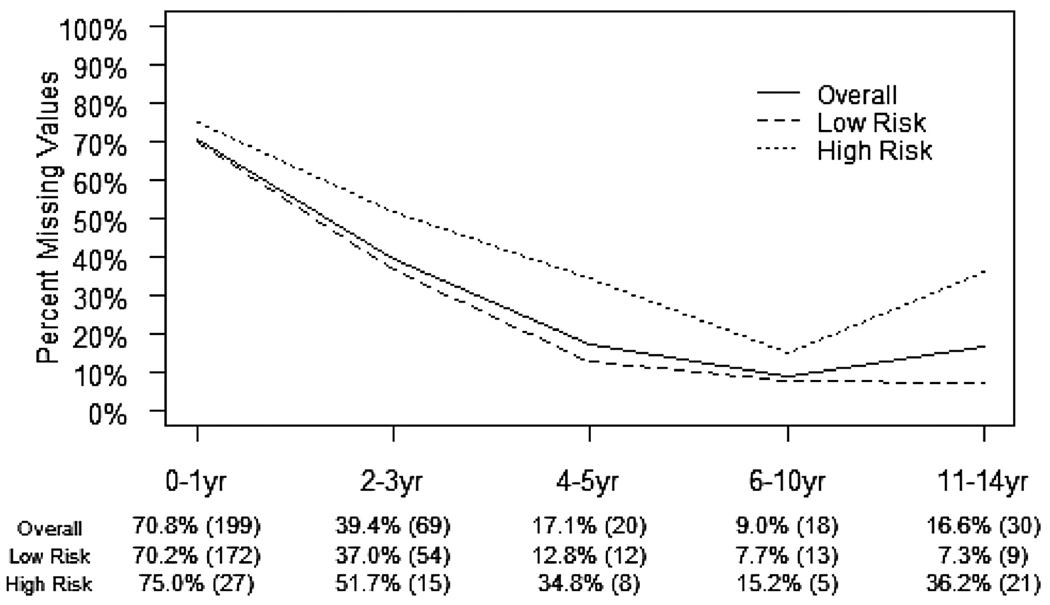
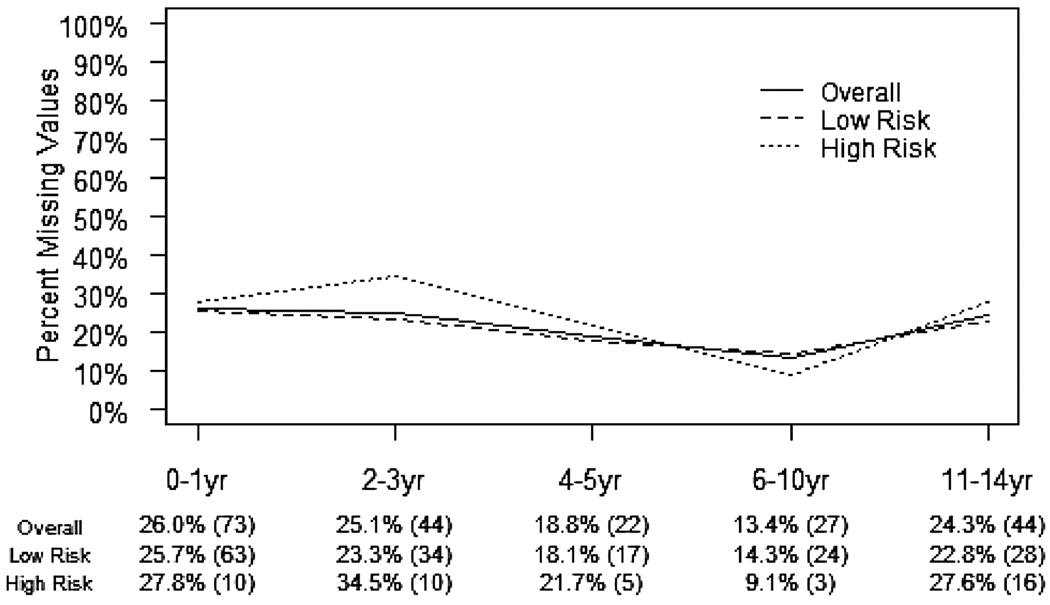
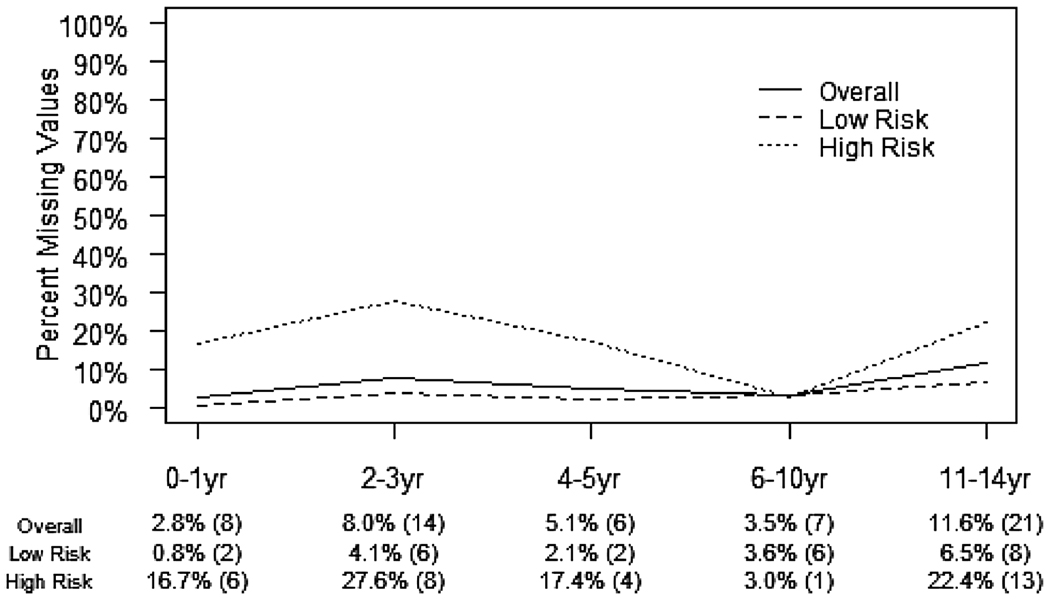
The proportions of children with missing values for the three core physiologic measures (SBP, respiratory rate, and GCS score) were 35.2%, 5.9%, and 22.0%, respectively. Pulse oximetry was the most commonly missing physiologic measure (52.8%). The proportion of missing values for physiologic markers differed by age group and outcome (Figs. 2–4). Missing values for SBP were highest among the youngest children and decreased as age increased. High-risk children had more missing values for SBP across all age groups. Missing values for field respiratory rates did not differ by age group, yet high-risk children tended to have more missing values. Overall, GCS score also had a substantial portion of missing data, although there was no consistent association with age group or outcome.
FIGURE 2.
The proportion of missing values for out-of-hospital systolic blood pressure among injured children, by age group and outcome (N = 955).High-risk = mortality (field or in-hospital) or length of hospital stay >2 days; low-risk = survival with 0–2-day length of stay.
FIGURE 4.
The proportion of missing values for out-of-hospital Glasgow Coma Scale (GCS) score among injured children, by age group and outcome (N = 955). High-risk = mortality (field or in-hospital) or length of hospital stay >2 days; low-risk = survival with 0–2-day length of stay.
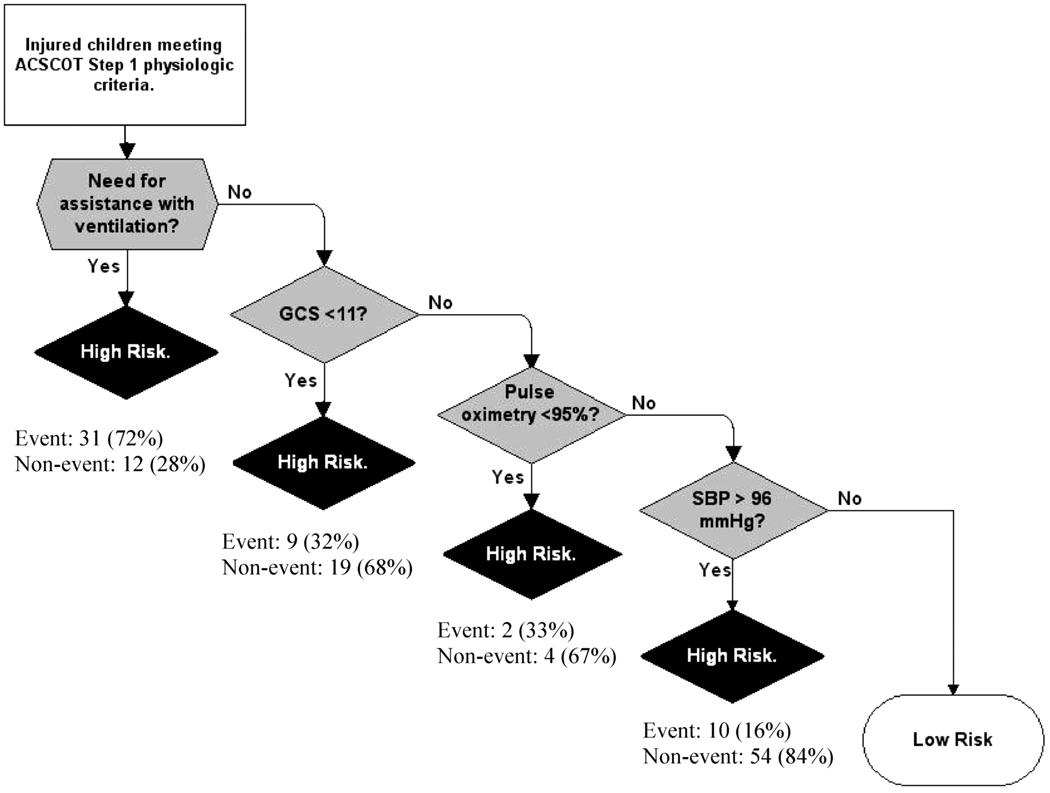
Using the seven physiologic measures and age, the primary decision tree included assisted ventilation (bag–valve–mask or intubation), GCS score <11, pulse oximetry <95%, and SBP >96 mmHg (Fig. 5). Rule validation demonstrated sensitivity 76.5% (95% confidence interval [CI] 66.4–86.6%) and specificity 71.7% (95% CI 66.7–76.6%) (Table 2). Neither age nor age-specific values for hypotension or respiratory rates were selected for the final physiologic decision tree. In addition, the presence of missing physiologic values was not predictive of outcome in the decision tree. In a supplemental analysis that included the three additional demographic and mechanism factors, the resulting decision tree included assisted ventilation, mechanism of injury (stabbing, firearm, cyclist, or pedestrian vs. auto), and SBP >111 mm Hg (figure not shown). Validation results for the supplemental decision tree had a sensitivity of 70.6% (95% CI 59.8–81.4) and a specificity of 78.3% (95% CI 73.8–82.9) (Table 3). When the “worst” physiologic values were examined (rather than solely using initial physiologic values), the predicted risk group changed in only six (1.6%) patients for the first tree and four (1.0%) for the second tree.
FIGURE 5.
Physiologic decision rule to identify high-risk injured children (mortality or length of hospital stay >2 days) meeting American College of Surgeons Committee on Trauma (ACSCOT) step 1 criteria (validation set, n = 382). Event = mortality (either field-based after resuscitative efforts or in-hospital) or hospital length of stay greater than 2 days. Non-event = survival with hospital length of stay 0–2 days. Predictor variables considered in developing this decision tree included systolic blood pressure (SBP) (mmHg), respiratory rate (breaths/min), Glasgow Coma Scale (GCS) score, pulse rate (beats/min), pulse oximetry (percentage oxyhemoglobin saturation), shock index (pulse rate/SBP), ventilatory support (bag–valve–mask or advanced airway), and age.
TABLE 2.
Summary Accuracy Measures for the Out-of-Hospital Pediatric Clinical Decision Tree (Physiologic Measures Only) Using the Validation Sample (n = 382)
| Estimate | 95% Confidence Interval | |
|---|---|---|
| Sensitivity | 76.5% | (66.4–86.6) |
| Specificity | 71.7% | (66.7–76.6) |
| Positive predictive value | 36.9% | (28.9–44.8) |
| Negative predictive value | 93.4% | (90.2–96.5) |
| Positive likelihood ratio | 2.70 | (2.11–3.29) |
| Negative likelihood ratio | 0.33 | (0.19–0.47) |
TABLE 3.
Summary Accuracy Measures for the Out-of-Hospital Pediatric Clinical Decision Tree (Physiologic Measures, Plus Mechanism, Injury Type, and Gender) Using the Validation Sample (n = 382)
| Estimate | 95% Confidence Interval | |
|---|---|---|
| Sensitivity | 70.6% | (59.8–81.4) |
| Specificity | 78.3% | (73.8–82.9) |
| Positive predictive value | 41.4% | (32.4–50.3) |
| Negative predictive value | 92.5% | (89.3–95.7) |
| Positive likelihood ratio | 3.26 | (2.41–4.11) |
| Negative likelihood ratio | 0.38 | (0.24–0.52) |
DISCUSSION
In this study, we demonstrate the incidence of mortality and prolonged hospitalization among injured children meeting standard ACSCOT physiologic criteria to be markedly lower than that of adults (19% vs. 58%20) when sampled from the same sites, the same EMS agencies, and during the same time period. Based on these results, more than 80% of children meeting such criteria for transport “to the highest level of care within the trauma system”7 will survive and be discharged within two days after presentation, many on the same day of evaluation. Integrating age-specific values of physiologic derangement or further restricting these measures did little to improve the predictive yield of the physiologic triage step, though missing information and the need for a simple rule were primary limitations in the analysis. Missing data were very common, particularly among young and high-risk children, suggesting significant practical limitations in the field use of physiologic measures to triage children. These findings are important both for field triage and when considering the selection of children for future field-based interventions or therapies.
Systolic blood pressure is one of the three core physiologic measures in the ACSCOT step 1 criteria and continues to be the major determinant of “hypotension” and “shock” in injured adults. There have been mixed results regarding the utility of hypotension in injured children. Some studies suggest that SBP is not a useful field marker of injury in children,18,32 while others demonstrate hypotension to be important in predicting outcome.17,33 In addition to the question of predictive value, the amount and systematic pattern of missing values for blood pressure call into question the practical use of field SBP in children. Gausche and colleagues demonstrated similarly high rates of absent SBP values in EMS charts for young children.19 The inclusion of age-specific values for SBP did not appear to improve the specificity for identifying high-risk children, though missing values limited the validity of this assessment. In the final decision tree, SBP was included at a lower “branch,” making the application of this measure specific to a very select subset of injured children. The blood pressure decision node also had an unexpected direction of effect (i.e., higher blood pressure associated with worse outcome). While it is possible that higher blood pressure may be deleterious in certain injured children (e.g., traumatic brain injury), it is also possible that other factors (e.g., the pattern of missing values or other logistical aspects of obtaining accurate SBP readings in children) affected the results of the final decision tree.
The use of field respiratory rate to identify seriously injured children has also had mixed results. Some studies suggest that respiratory rate is a poor predictor of outcome,14,32,34 while others indicate this measure to be useful in trauma triage.18,33 Neither respiratory rate nor age-specific values were included in the final decision tree, though almost 20% of high-risk children had abnormal respiratory rate as a sole criterion for entry into the sample. While the overall frequency of missing values for respiratory rate was low, the higher rate of missing values among high-risk children raises concerns about systematic bias in the availability of this vital sign.
In contrast, respiratory failure requiring ventilatory assistance was a strong predictor of high-risk children. Previous studies have demonstrated intubation among injured children to be associated with high rates of serious injury, use of trauma resources, and adverse outcomes.18,34−36 However, ventilatory assistance is not explicitly listed in the ACSCOT decision scheme.7 Even GCS score, typically considered an important factor in identifying seriously injured children,18,32−34,37 was included below ventilatory assistance in the final decision tree. The presence of respiratory distress requiring field ventilatory support appears to provide more predictive value than the simple numeric respiratory rate and should be considered for inclusion in future triage decision schemes for children.
Examination of the presence and pattern of missing values was integral to this analysis. We demonstrate that the presence of missing data was quite common in this sample and there appeared to be a systematic (i.e., nonrandom) mechanism by which certain physiologic measures were missing. It is possible that the techniques we used to handle missing data introduced bias and affected the selection of cutpoints (e.g., SBP) in the final decision trees; however, more rigorous methods of handling missing values (e.g., multiple imputation) are difficult to combine with binary recursive partitioning trees. Despite the analytic challenges with missing values in this sample, the recognition that core physiologic information is frequently absent is problematic because current triage guidelines assume such information is uniformly present among injured children. Possible explanations for these findings include low EMS provider confidence and/or experience in obtaining such information (especially from young children), lack of age-specific equipment (e.g., blood pressure cuffs), or lack of time in the face of other patient care priorities. These data were collected from mature EMS systems in the setting of a research consortium, which likely translates into higher-quality and more complete data than may be present in less-developed systems. That is, the proportion of missing values we present may underestimate the prevalence of the problem in other EMS systems. While one might assume that more training, appropriate equipment, or other interventions may increase the ability to obtain field physiologic information from children, these assumptions might not be true. Our findings suggest that pediatric triage rules placing heavy emphasis on physiologic information may have substantial practical limitations and therefore shift reliance to other parts of the field triage algorithm.
We were unable to apply more restrictive physiologic cutpoints for children (with or without age-specific criteria) without missing high-risk patients. The basis for these observations is not entirely clear. Perhaps injured children are less likely to exhibit physiologic derangement early after injury (e.g., better compensation) or they may simply manifest these clinical findings less consistently. The presence of higher rates and systematic patterns of missing physiologic values among children may further compromise the use of physiologic values as a triage tool. It is possible that the current stepwise schematic for field trauma triage may not fit the injured pediatric population as well as it does adults. It is also important to recognize that injured children account for a much lower trauma volume relative to adults, and therefore overtriage (i.e., triaging patients with minor injuries to trauma centers) presents a smaller burden than for adults. As our results suggest that more restrictive physiologic criteria will miss seriously injured children, attempting to cut overtriage rates among the pediatric injury population may not be fruitful.
Limitations
There were limitations in this study. The inclusion criteria for the ROC Epistry–Trauma database were based on standard ACSCOT step 1 adult physiologic criteria in use by most U.S. trauma systems. Consequently, children with “normal” field physiologic measures were excluded, regardless of whether they ultimately had serious injury. For this reason, we were unable to assess whether the use of broader ranges of physiologic parameters (e.g., GCS score >12 or respiratory rates between 10 and 28 breaths/min) would better identify high-risk children. It is unclear how our decision tree or further assessment of more restrictive physiologic criteria may perform in a broader population of injured children. In addition, the assessment of missing values was based on a cohort of children for whom at least one physiologic abnormality had to be documented for inclusion in the sample. This requirement may have led to an underestimation of the true proportion of missing data among the more heterogeneous group of injured children cared for by EMS providers.
There were also analytic limitations in the study. The growth of final decision trees was restricted by the need for a relatively simple algorithm that could be implemented in the field. It is likely that removing this restriction could have generated trees with improved accuracy measures. In addition, decision trees generated using recursive partitioning can become unstable (particularly the lower branches) based on subtle changes in the data, including missing values. Although the presence of missing values was not associated with the identification of high-risk children in the decision trees, the volume of missing data could have affected certain branches in the tree (e.g., SBP).
We were unable to directly assess other commonly used injury outcomes (e.g., injury severity and resource use) because the ROC Epistry–Trauma database does not capture such measures. Duration of hospital stay provided a surrogate measure for survivors with serious injury and/or requiring specialized resources, though we recognize that hospital stay is only a proxy for such outcomes. Simplifying the outcome to only mortality would have ignored this important population of injured children.
CONCLUSIONS
We demonstrate that injured children meeting standard adult-based field physiologic criteria have a much lower rate of mortality and prolonged hospitalization than adults. In addition, there were high rates and systematic patterns of missing data for core physiologic measures, which may affect the practical use and predictive value of such information. Our findings do not support the field use of more restrictive or age-specific physiologic values to identify high-risk children, though these findings are tempered by the degree and pattern of missing data.
FIGURE 3.
The proportion of missing values for out-of-hospital respiratory rate among injured children, by age group and outcome (N = 955). High-risk = mortality (field or in-hospital) or length of hospital stay >2 days; low-risk = survival with 0–2-day length of stay.
Acknowledgments
We acknowledge and thank the many contributing EMS agencies, EMS providers, study coordinators, staff, and investigators (see Appendix 1) for their willingness to participate in and support this project, and for their continued dedication to improving the EMS care and outcomes for their patients.
The Resuscitation Outcome Consortium (ROC) was supported by a series of cooperative agreements to 10 regional clinical centers and one data Coordinating Center (5U01 HL077863, HL077881, HL077871 HL077872, HL077866, HL077908, HL077867, HL077885, HL077877, HL077873) from the National Heart, Lung and Blood Institute in partnership with the National Institute of Neurological Disorders and Stroke, U.S. Army Medical Research &Material Command, The Canadian Institutes of Health Research (CIHR)–Institute of Circulatory and Respiratory Health, Defence Research and Development Canada, the Heart and Stroke Foundation of Canada, and the American Heart Association.
Appendix
Research Outcomes Consortium (ROC) Epistry Contributors
Please go to the ROC website at www.uwctc.org and click on ROC for additional acknowledgments.
Alabama Resuscitation Center, University of Alabama at Birmingham, Birmingham, AL: Jeffrey D. Kerby, MD, PhD, Principal Investigator
Core Investigators: Todd B. Brown, MD, MSPH, Thomas Terndrup, MD
Coordinators: Shannon W. Stephens, EMT-P, Carolyn R. Williams, BSN, BSME
EMS Investigators/Collaborators: Joe E. Acker, EMT-P, MPH, Michael L. Minor, EMT-P
Hospital Investigators/Collaborators: Paul A. MacLennan, PhD, Patrick R. Pritchard, MD, Sandra Caldwell, MA, Katherine R. Lai, BS
Participating EMS Agencies: Alabama LifeSaver, Bessemer Fire and Rescue, Birmingham Fire and Rescue, Center Point Fire District, Chelsea Fire and Rescue, American Medical Response, Homewood Fire Department, Pelham Fire Department, Rocky Ridge Fire Department, Regional Paramedic Services, Trussville Fire Department, Vestavia Hills Fire and Rescue
Dallas Center for Resuscitation Research, University of Texas Southwestern Medical Center, Dallas, TX: Ahamed H. Idris, MD, Principal Investigator
Core Investigators: Fernando Benitez, MD, Raymond Fowler, MD, Dorothy Lemecha, MD, Joseph Minei, MD, Paul Pepe, MD, Michael Ramsay, MD, Robert Simonson, MD, Jane Wigginton, MD
Coordinators: Dixie Climer, RN, Melinda Moffat, RN, Kate Newman, RN, Pamela Owens, Andrea Bennett, BS
EMS Investigators/Collaborators: Richard Black, EMT-P, Debra Cason, RN, Billy Craft, EMT-P, Lucy Detamble, RN, Ryan Dykes, EMT-P, Tony Harvey, EMT-P, Suzanne Hewitt, RN, Marshal Isaacs, MD, Joe Kay, EMT-P, Tami Kayea, EMT-P, Richard LaChance, EMT-P, Thomas Lehman, Paul Mayer, MD, Jeffrey Metzger, MD, Danny Miller, EMT-P, Kenneth Navarro, EMT-P, Steven Parker, EMT-P, Karen Pickard, RN, Warren Porter, EMT-P, T. J. Starling, EMT-P, Tommy Tine, EMT-P, Chris Vinson, EMT-P
Hospital Investigators/Collaborators: David Abebefe, MD, Steven Arze, MD, Sean Black, MD, Matthew Bush, MD, Michael Forman, MD, Jeffery Goodloe, MD, Ralph Kelly, DO, Gregory Lachar, MD, Alicia Mangram, MD, Marc Morales, MD, Edward Thornton, MD, Robert Wiebe, MD
Participating EMS Agencies: Carrollton Fire Department, Dallas Fire and Rescue, DeSoto Fire Department, Duncanville Fire Department, Farmers Branch Fire Department, Garland Fire Department, Highland Park Department of Public Safety, Irving Fire Department, Lancaster Fire Department, Mesquite Fire Department, Plano Fire Department, University Park Fire Department
University of Iowa Carver College of Medicine–Iowa Resuscitation Network, University of Iowa, Iowa City, IA: Richard Kerber, MD, Principal Investigator
Core Investigators: Steve Hata, MD, Dianne Atkins, MD
Coordinators: Melanie Kenney, RN, MA, CPNP, Catherine Rost, Alexander Drum, EMT-P, Michael Hartley, EMT-P
Participating EMS Agencies: Area Ambulance Service, Davenport Hospital Ambulance Corporation, Covenant Health System–Covenant Ambulance, Covenant Health System–Mercy Oelwein, Covenant Health System–Sartori, City of Dubuque Fire Department, Dallas County Emergency Medical Services, West Des Moines Emergency Medical Services, Des Moines Fire Department EMS, Henry County Health Center Emergency Medical Services, Johnson County Ambulance, Siouxland Paramedics, Inc., Waterloo Fire Rescue
Milwaukee Resuscitation Research Center, Medical College of Wisconsin, Milwaukee, WI: Tom P. Aufderheide, MD, Principal Investigator
Core Investigators: Ronald G. Pirrallo, MD, MHSA, Karen J. Brasel, MD, MPH, Andrea L. Winthrop, MD, John P. Klein, PhD
Coordinators: David J. Kitscha, BS, MS, Barbara J. Burja, BA, EMT, Chris von Briesen, BA, CCRC, Christopher W. Sparks, EMT, Sara Kaebisch, BS
EMS Investigators/Collaborators: John Chianelli, MS, Rosemarie Forster, MSOLQ, RHIA, EMT-P, Michael Milbrath, EMT-P, Lauryl Pukansky, BS, RHIA, Kenneth Sternig, MS-EHS, BSN, EMT-P, Eugene Chin, RN, EMT-P, Nancy Frieberg, RN, EMT-P, Kim Krueger, RN, EMT-P, Del Szewczuga, RN, EMT-P, Thomas Duerr, Rebecca Funk, BS, RHIA, EMT-B, Gail Jacobsen, BS, Janis Spitzer, Richard Demien, James Martins, John Cohn, Russell R. Spahn, MA, EMT-P, Mike Jankowski, BA, EMT-P, Timothy James, William E. Wentlandt Jr., MBA, EFO, David Berousek, Brian M. Satula, BA, NREMT, Jay B. Behling, BS, EMT-B, Dean K. Redman, BA, EFO, Steven Hook, BS, CFOD, Andrew Neargarder, Jim Singer, RN
Hospital Investigators/Collaborators: Thomas Reminga, MD, Dennis Shepherd, MD, Peter Holzhauer, MD, Jonathan Rubin, MD, Craig Skold, MD, Orlando Alvarez, MD, Heidi Harkins, MD, Edward Barthell, MD, William Haselow, MD, Albert Yee, MD, John Whitcomb, MD, Eduardo E. Castro, MD, Steven Motarjeme, MD
Participating EMS Agencies: Cudahy Fire Department, Flight for Life, Franklin Fire Department, Greendale Fire Department, Greenfield Fire Department, Hales Corners Fire Department, Milwaukee County Airport Fire Department, Milwaukee Fire Department, North Shore Fire Department, Oak Creek Fire Department, South Milwaukee Fire Department, St. Francis Fire Department, Wauwatosa Fire Department, West Allis Fire Department
Ottawa/OPALS/British Columbia RCC, Ottawa Health Research Institute, University of Ottawa, Ottawa, Ontario and St. Paul’s Hospital, University of British Columbia, British Columbia, Canada: Ian Stiell, MD, Principal Investigator
Core Investigators: Jim Christenson, MD, Morad Hameed, MD, Jean Denis Yelle, MD, Martin Osmond, MD, Christian Vaillancourt, MD, David Evans, MD, Riyad Abu-Laban, MD
Coordinators: Cathy Clement, RN, Tammy Beaudoin, CCHRA, Barb Boychuk, RN, Sarah Pennington, RN, Helen Connolly, RN, Patrick Lefaivre, PCP, Jane Banek, CCHRA, Angela Marcantonio, Rina Marcantonio, CCHRA, Christine Leclair, RN, Julie Cummins, RN
EMS Investigators/Collaborators: Matthew Stempien, MD, Jonathan Dreyer, MD, Douglas Munkley, MD, Justin Maloney, MD, Paul Colella, MD, Andrew Affleck, MD, David Waldbillig, MD, Paul Bradford, MD, Martin Lees, MD, Vincent Arcieri, MD, Ann Wilson, BSc, ACP, Kenneth Boyle, EMCA, RRT, CMA, Lorraine Luinstra-Toohey, BScN, MHA, John Trickett, BScN, Nicole Sykes, BScN, RN, Elaine Graham, ACP, Kieran Ballah, EMCA, Cathy Hedges, A-EMCA, ACP, Paul Mathers, A-EMCA, Dug Andrusiek, MSc, Dan Bishop, ACP, Ron Straight, ACP, Brian Twaites, ACP, Stuart Donn, PhD
Participating EMS Agencies: A.A. and M. Volunteer Ambulance Service, Burlington Fire and Rescue, Cambridge Fire Department, Cornwall Fire and Rescue, Cornwall SDG Emergency Medical Services, Essex–Windsor Emergency Medical Services, Essex–Windsor Fire and Rescue, Frontenac Paramedic Service, Halton Emergency Medical Services, Harrow Ambulance Service Ltd., Kawartha Lakes Emergency Medical Services, Kawartha Lakes Fire and Rescue, Kingston Fire and Rescue, Kitchener Fire Department, Lambton County Emergency Medical Services, Lasalle Fire Department, London Fire Department, Niagara Emergency Medical Services, Niagara Falls Fire and Rescue, Northumberland Emergency Medical Service, Oakville Fire Department, Ottawa Fire and Rescue, Ottawa Paramedic Service, Peterborough Emergency Medical System, Peterborough Fire Department, Prescott-Russell Emergency Medical Services, Sarnia Fire Services, St. Catharine’s Fire and Rescue, Sudbury Emergency Medical Services, Sudbury Fire and Rescue, SunParlour Emergency Services Inc., Superior North Emergency Medical Services, Tecumseh Fire Department, Thames Emergency Medical Services, Thunder Bay Fire and Rescue, Waterloo Fire and Rescue, Waterloo Regional Emergency Medical Services, Welland Fire and Rescue, Windsor Fire and Rescue, British Columbia Ambulance Service, Abbotsford Fire Department, Aggassiz Valley Fire Department, Burnaby Fire Department, Campbell River Fire Department, Central Saanich Fire Department, City of North Vancouver Fire Department, Coquitlam Fire Department, Delta Fire Department, Esquimalt Fire Department, Kamloops Fire Department, Kelowna Fire Department, Lake Country V Fire Department, Langford Fire Department, Langley City Fire Department, Langley Township Fire Department, Maple Ridge Fire Department, Mission Fire Department, Nanaimo Fire Department, New Westminster Fire Department, North Vancouver District Fire Department, Oak Bay Fire Department, Peachland Valley Fire Department, Pitt Meadows Fire Department, Port Coquitlam Fire Rescue, Port Moody Fire Department, Prince George Fire Department, Prince Rupert Fire Department, Qualicum Beach Fire Department, Richmond Fire Department, Saanich Fire Department, Sooke V Fire Department, Squamish Fire Department, Surrey Fire Department, Trail Fire Department, Vancouver Fire Department, Victoria Fire Department, West Vancouver Fire Department, Whistler Fire Department, White Rock Fire Department
Pittsburgh Resuscitation Network, the University of Pittsburgh, Pittsburgh, PA: Clifton Callaway, MD, PhD, Principal Investigator
Core Investigators: Samuel Tisherman, MD, Jon Rittenberger, MD, David Hostler, PhD
Coordinators: Joseph Condle, Mitch Kampmeyer, Timothy Markham, Maureen Morgan
EMS Investigators/Collaborators: Paul Sabol, Gina Sicchitano, Scott Sherry, Anthony Shrader, Greg Stull, Manuel Torres, MS, William Groft, Robert McCaughan, Rodney Rohrer, John Cole, MD, David Fuchs, MD, Francis Guyette, MD, MS, William Jenkins, MD, Ronald Roth, MD, Heather Walker, MD
Hospital Investigators/Collaborators: Alain Corcos, MD, Ankur Doshi, MD, Adrian Ong, MD, Andrew Peitzman, MD
Participating EMS Agencies: Washington Ambulance and Chair, Pittsburgh Bureau of Emergency Medical Services, Pittsburgh Bureau of Fire, Mutual Aid Ambulance Service, STAT Medevac
Portland Resuscitation Outcomes Consortium, Oregon Health & Science University, Portland, OR: Jerris R. Hedges, MD, MS, Principal Investigator
Core Investigators: Craig D. Newgard, MD, MPH, Mohamud R. Daya, MD, MS, Robert A. Lowe, MD, MPH
Coordinators: Denise Griffiths, BS, John Brett, EMT-P, Dana Zive, MPH, Abdolaziz Yekrang, MPA, MA, Yoko Nakamura, MD, Brooke Frakes, BS, Aaron Monnig, EMT-P
EMS Investigators/Collaborators: Jonathan Jui, MD, MPH, Terri A. Schmidt, MD, MS, Ritu Sahni, MD, Craig R. Warden, MD, MPH, Marc D. Muhr, EMT-P2, John A. Stouffer, EMT-P, Kyle Gorman, MBA, EMT-P, Pontine Rosteck, EMT-P, Karl Koenig, EMT-P, Jan Lee, EMT-P, Roxy Barnes, EMT-P, Heather Tucker, EMT-P, Brad Allen, EMT-P, T. J. Bishop, EMT-P, Adam Glaser, EMT-P
Hospital Investigators/Collaborators: Martin A. Schreiber, MD, Jim Anderson, MD, Ameen I. Ramzy, MD, K. Dean Gubler, DO, Lynn K. Wittwer, MD, Samantha Underwood, MS, Brooke Barone, BS, Denise Haun-Taylor, RN, Elizabeth Bryant, RN, Joanne Miller, ARNP
Participating EMS Agencies: American Medical Response—Clackamas, Clark, and Multnomah Counties, Camas Fire Department, Clackamas County Fire District #1, Clark County Fire District #6, Lake Oswego Fire Department, LifeFlight, MetroWest Ambulance, North Country Ambulance, Tualatin Valley Fire and Rescue, Vancouver Fire Department, Portland Fire and Rescue, Portland International Airport Fire Department, Gresham Fire and Emergency Services
UCSD–San Diego Resuscitation Research Center, University of California at San Diego, San Diego, CA: Daniel Davis, MD, Principal Investigator
Core Investigators: David Hoyt, MD, Raul Coimbra, MD, PhD, Gary Vilke, MD
Coordinators: Donna Kelly, RN, Lana McCallum-Brown, RN
EMS Investigators/Collaborators: Bruce Haynes, MD, Brad Schwartz, MD
Hospital Investigators/Collaborators: Michael Sise, MD, Frank Kennedy, MD, Fred Simon, MD, Gail Tominaga, MD, John Steele, MD
Participating EMS Agencies: Alpine Fire Protection District, American Medical Response, Barona Fire Department, Bonita/Sunnyside Fire Protection, Borrego Springs Fire Protection District, Carlsbad Fire Department, Chula Vista Fire Department, Coronado Fire Department, CSA-17 ALS Transporting Agency, Deer Springs, Del Mar Fire Department, East County Fire Protection District, El Cajon Fire Department, Elfin Forest CSA 107, Encinitas Fire Protection District, Escondido Fire Department, Federal Fire Department San Diego, Imperial Beach Fire Department, Julian-Cuyamaca Fire Department, La Mesa Fire Department, Lakeside Fire Protection District, Lemon Grove Fire Department, Mercy Air, Miramar Fire Department, National City Fire Department, North County Fire, Oceanside Fire Department, Pala Fire Department, Poway Fire Department, Ramona Fire Department, Rancho Santa Fe Fire Protection District, San Diego Rural Fire Protection District, San Marcos Fire Department, San Miguel Fire Protection District, Santee Fire Department, Solana Beach Fire Department, Sycuan Fire Department, Valley Center/Mercy Ambulance, Viejas Fire Department, Vista Fire Department
Seattle–King County Center for Resuscitation Research at the University of Washington, University of Washington, Seattle, WA: Peter J. Kudenchuk, MD, Principal Investigator
Core Investigators: Tom D. Rea, MD, Eileen Bulger, MD, Mickey S. Eisenberg, MD, Michael Copass, MD
Coordinators: Michele Olsufka, RN, Sally Ragsdale, ARNP, Debi Solberg, RN, MN, Susan Damon, RN, Randi Phelps, Jeanne O’Brien, RN, MN
EMS Investigators/Collaborators: Earl Sodeman, Marty LaFave, James Boehl, Dave Jones, Gary Somers, Deborah Ayrs, Adrian Whorton, Sam Warren, Jim Fogarty, Jonathan Larsen, Mike Helbock
Participating EMS Agencies: Bellevue Fire Department, Redmond Fire Department, Seattle Fire Department, Shoreline Fire Department, King Co Medic 1, Vashon Island Medic One, Bothell Fire Department, Burien Fire Department, Kirkland Fire Department, Renton Fire Department, Snoqualmie Fire Department, Duvall Fire Department, Eastside Fire and Rescue, Enumclaw Fire Department, Fall City Fire Department, Skyway Fire Department, Kent Fire Department, Maple Valley Fire and Life Safety, Mercer Island Fire Department, King County Fire District #44, North Highline Fire Department, Northshore/Kenmore Fire Department, Port of Seattle Fire Department, King County Fire District #47, King County Fire District #40, SeaTac Fire Department, Skykomish Fire Department, Snoqualmie Pass, South King Co Medic 1, South King Fire and Rescue, Tukwila Fire Department, Valley Regional Fire Authority, Vashon Island Fire and Rescue, Woodinville Fire Department
Toronto Regional Resuscitation Research Out of Hospital Network (Toronto Regional RESCUeNET), University of Toronto, Toronto, Ontario, Canada: Arthur Slutsky, MD, Principal Investigator
Core Investigators: Laurie Morrison, MD, MSc, Paul Dorian, MD
Coordinators: Craig Beers, Blair Bigham, Dina Braga, Grace Burgess, Bruce Cameron, Suzanne Chung, Pete De Maio, Steve Driscoll, Lynne Fell, Jamie Frank, Mark McLennan, Lesley Ann Molyneaux, Welson Ryan, Angela Schotsman, Jacob Simonini, Lynda Turcotte, Flo Veel, Amy Wassenaar, Cathy Zahn
EMS Investigators/Collaborators: Dana Bradshaw, Rob Burgess, Bruce Cameron, Sandra Chad, Sheldon Cheskes, Allan Craig, Steve Dewar, Tim Dodd, Rob Duquette, Marty Epp, Michael Feldman, Verena Jones, Russell MacDonald, Larry MacKay, Steve McNenley, Judy Moore, Philip Moran, Michael Murray, Michael Nemeth, Russ Olnyk, Tyrone Perreira, Richard Renaud, Karen Roche, Jennifer Shield, Doug Silver, Jacob Stevens, Rick Verbeek, Tim Waite, Ken Webb, Michelle Welsford
Hospital Investigators/Collaborators: Rosemarie Farrell, Jamie Hutchison
Participating EMS Agencies: Ajax Fire and Emergency Services, Barrie Fire and Emergency Service, Beausoleil First Nation Emergency Medical Services, Bradford West Gwillimbury Fire and Emergency Services, Brampton Fire and Emergency Services, Brock Township Fire Department, Caledon Fire and Emergency Services, City of Hamilton Emergency Services–EMS, City of Hamilton Emergency Services–Fire, City of Orillia Fire Department, Clarington Emergency and Fire Services, County of Simcoe Paramedic Services, Durham Regional Emergency Medical Services, Innisfil Fire and Rescue Service, Mississauga Fire and Emergency Services, Mnjikaning Fire Rescue Service, Muskoka Ambulance Service, Muskoka Ambulance Communication Center, New Tecumseth Fire Department, OrngeTransport Medicine, Oro Medonte Fire and Emergency Services, Oshawa Fire Services, Pickering Fire Services, The Ramara Township Fire and Rescue Service, Peel Regional Paramedic Services, Toronto EMS, Toronto Fire Services, Township of Essa Fire Department, Township of Georgian Bay Fire Department, Township of Scugog Fire Department, Township of Uxbridge Fire Department, Wasaga Beach Fire Department, Whitby Fire and Emergency Services, Durham Regional Basehospital, Sunnybrook Osler Center for Prehospital Care, Hamilton Health Sciences Paramedic Base Hospital Program, Simcoe Muskoka Basehospital
Steering Committee Chair, Myron Weisfeldt, MD, Johns Hopkins University School of Medicine, Baltimore, MD, Co-Chair-Cardiac, Joseph P. Ornato, MD, Virginia Commonwealth University Health System, Richmond, VA, Co-Chair-Trauma, David B. Hoyt, MD, University of California at San Diego, San Diego, CA, replacing Col. John B. Holcomb, MD, Commander, U.S. Army ISR
National Heart, Lung and Blood Institute, Bethesda, MD: Tracey Hoke, MD, George Sopko, MD, MPH, David Lathrop, PhD, Alice Mascette, MD, Patrice Desvigne Nickens, MD
Clinical Trial Center, University of Washington, Seattle, WA: Al Hallstrom, PhD, Graham Nichol, MD, MPH, Scott Emerson, MD, PhD, Judy Powell, BSN, Gena Sears, BSN, Berit Bardarson, RN, Lois Van Ottingham, BSN, Anna Leonen, MS, Robert B. Ledingham, MS, Chris Finley, Richard Moore, BS, Ben Bergsten-Buret
Footnotes
The Research Outcomes Consortium (ROC) contributors are listed in Appendix 1.
Presented as an abstract at the Society for Academic Emergency Medicine annual meeting, New Orleans, Louisiana, May 2009.
References
- 1.Cooper A, Barlow B, DiScala C, String D, Ray K, Mottley L. Efficacy of pediatric trauma care: results of a population-based study. J Pediatr Surg. 1993;28:299–303. doi: 10.1016/0022-3468(93)90221-6. [DOI] [PubMed] [Google Scholar]
- 2.Hulka F, Mullins RJ, Mann NC, et al. Influence of a statewide trauma system on pediatric hospitalization and outcome. J Trauma. 1997;42:514–519. doi: 10.1097/00005373-199703000-00020. [DOI] [PubMed] [Google Scholar]
- 3.Johnson DL, Krishnamurthy S. Send severely head-injured children to a pediatric trauma center. Pediatr Neurosurg. 1996;25:309–314. doi: 10.1159/000121145. [DOI] [PubMed] [Google Scholar]
- 4.Hall JR, Reyes HM, Meller JL, Loeff DS, Dembek R. The outcome for children with blunt trauma is best at a pediatric trauma center. J Pediatr Surg. 1996;31:72–77. doi: 10.1016/s0022-3468(96)90322-x. [DOI] [PubMed] [Google Scholar]
- 5.Pracht EE, Tepas JJ, Langland-Orban B, Simpson L, Pieper P, Flint LM. Do pediatric patients with trauma in Florida have reduced mortality rates when treated in designated trauma centers? J Pediatr Surg. 2008;43:212–221. doi: 10.1016/j.jpedsurg.2007.09.047. [DOI] [PubMed] [Google Scholar]
- 6.Future of Emergency Care Series: Emergency Care for Children, Growing Pains. Washington, DC: National Academy Press; 2006. Committee on the Future of Emergency Care in the United States Health System, Board on Health Care Services. Institute of Medicine of the National Academies. [Google Scholar]
- 7.Resources for Optimal Care of the Injured Patient. Chicago, IL: American College of Surgeons; 2006. Committee on Trauma. [Google Scholar]
- 8.Esposito TJ, Offner PJ, Jurkovich GJ, Griffith J, Maier RV. Do prehospital trauma center triage criteria identify major trauma victims? Arch Surg. 1995;130:171–176. doi: 10.1001/archsurg.1995.01430020061010. [DOI] [PubMed] [Google Scholar]
- 9.Kane G, Engelhardt R, Celentano J, et al. Empirical development and evaluation of prehospital trauma triage instruments. J Trauma. 1985;25:482–489. doi: 10.1097/00005373-198506000-00002. [DOI] [PubMed] [Google Scholar]
- 10.Henry MC, Hollander JE, Alicandro JM, Cassara G, O’Malley S, Thode HC., Jr Incremental benefit of individual American College of Surgeons trauma triage criteria. Acad Emerg Med. 1996;3:992–1000. doi: 10.1111/j.1553-2712.1996.tb03340.x. [DOI] [PubMed] [Google Scholar]
- 11.Henry MC, Alicandro JM, Hollander JE, Moldashel JG, Cassara G, Thode HC., Jr Evaluation of American College of Surgeons trauma triage criteria in a suburban and rural setting. Am J Emerg Med. 1996;14:124–129. doi: 10.1016/S0735-6757(96)90117-5. [DOI] [PubMed] [Google Scholar]
- 12.Hannan EL, Farrell LS, Cooper A, Henry M, Simon B, Simon R. Physiologic trauma triage criteria in adult trauma patients: are they effective in saving lives by transporting patients to trauma centers? J Am Coll Surg. 2005;200:584–592. doi: 10.1016/j.jamcollsurg.2004.12.016. [DOI] [PubMed] [Google Scholar]
- 13.Norwood SH, McAuley CE, Berne JD, Vallina VL, Creath RG, McLarty J. A prehospital Glasgow Coma Scale score ≤14 accurately predicts the need for full trauma team activation and patient hospitalization after motor vehicle collisions. J Trauma. 2002;53:503–507. doi: 10.1097/00005373-200209000-00018. [DOI] [PubMed] [Google Scholar]
- 14.Eichelberger MR, Gotschall CS, Sacco WJ, Bowman LM, Mangubat EA, Lowenstein AD. A comparison of the trauma score, the revised trauma score, and the pediatric trauma score. Ann Emerg Med. 1989;18:1053–1058. doi: 10.1016/s0196-0644(89)80930-8. [DOI] [PubMed] [Google Scholar]
- 15.Kaufmann CR, Maier RV, Rivara FP, Carrico CJ. Evaluation of the pediatric trauma score. JAMA. 1990;263:69–72. [PubMed] [Google Scholar]
- 16.Nayduch DA, Moylan J, Rutledge R, et al. Comparison of the ability of adult and pediatric trauma scores to predict pediatric outcome following major trauma. J Trauma. 1991;31:452–458. doi: 10.1097/00005373-199104000-00003. [DOI] [PubMed] [Google Scholar]
- 17.Coates BM, Vavilala MS, Mack CD, et al. Influence of definition and location of hypotension on outcome following severe pediatric traumatic brain injury. Crit Care Med. 2005;33:2645–2650. doi: 10.1097/01.ccm.0000186417.19199.9b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Newgard CD, Cudnik M, Warden CR, Hedges JR. The predictive value and appropriate ranges of prehospital physiological parameters for high-risk injured children. Pediatr Emerg Care. 2007;23:450–456. doi: 10.1097/01.pec.0000280508.90665.df. [DOI] [PubMed] [Google Scholar]
- 19.Gausche M, Henderson DP, Seidel JS. Vital signs as part of the prehospital assessment of the pediatric patient: a survey of paramedics. Ann Emerg Med. 1990;19:173–178. doi: 10.1016/s0196-0644(05)81804-9. [DOI] [PubMed] [Google Scholar]
- 20.Newgard CD, Rudser K, Hedges JR, et al. A critical assessment of the out-of-hospital trauma triage guidelines for physiologic abnormality. J Trauma. doi: 10.1097/TA.0b013e3181ae20c9. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Newgard CD, Sears GK, Rea TD, et al. The Resuscitation Outcomes Consortium Epistry–Trauma: Design, Development, and Implementation of a North American Epidemiologic Out-of-hospital Trauma Registry. Resuscitation. 2008;78:170–178. doi: 10.1016/j.resuscitation.2008.01.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Davis DP, Garberson LA, Andrusiekc D, et al. A descriptive analysis of emergency medical service systems participating in the Resuscitation Outcomes Consortium (ROC) network. Prehosp Emerg Care. 2007;11:369–382. doi: 10.1080/10903120701537147. [DOI] [PubMed] [Google Scholar]
- 23.Newgard CD, Cudnik M, Warden CR, Hedges JR. The predictive value and appropriate ranges of prehospital physiologic parameters for high-risk injured children. Pediatr Emerg Care. 2007;23:450–456. doi: 10.1097/01.pec.0000280508.90665.df. [DOI] [PubMed] [Google Scholar]
- 24.Gausche M, Lewis RJ, Stratton SJ, et al. Effect of out-of-hospital pediatric endotracheal intubation on survival and neurological outcome: a controlled clinical trial. JAMA. 2000;283:783–790. doi: 10.1001/jama.283.6.783. [DOI] [PubMed] [Google Scholar]
- 25.Emergency Cardiovascular Care Committee. 2005 AHA Guidelines for Cardiovascular Resuscitation and Emergency Cardiovascular Care: Pediatric Advanced Life Support. Circulation. 2005;112 suppl 112:IV-188–IV-195. [Google Scholar]
- 26.Gausche-Hill M, Fuchs S, Yamamoto L, editors. Advanced Pediatric Life Support, The Pediatric Emergency Medicine Resource. ed. 4. Sudbury, MA: Jones and Bartlett; 2006. [Google Scholar]
- 27.ATLS for Trauma Student Course Manual. 6th ed. Chicago, IL: American College of Surgeons; 1997. Committee on Trauma. [Google Scholar]
- 28.Holmes JF, Palchak MJ, MacFarlane T, Kupperman N. Performance of the pediatric Glasgow Coma Scale in children with blunt head trauma. Acad Emerg Med. 2005;12:814–819. doi: 10.1197/j.aem.2005.04.019. [DOI] [PubMed] [Google Scholar]
- 29.Newgard CD, Fleischman R, Choo E, et al. Validation of length of hospital stay as a surrogate measure for injury severity and resource use among injury survivors [abstract] Acad Emerg Med. 2009;16 supplement 1:s238. doi: 10.1111/j.1553-2712.2009.00647.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Breiman L, Freidman JH, Olshen RA, Stone CJ. Classification and Regression Trees. New York: Chapman & Hall; 1984. [Google Scholar]
- 31.Stiell IG, Wells GA. Methodologic standard for the development of clinical decision rules in emergency medicine. Ann Emerg Med. 1999;33:437–447. doi: 10.1016/s0196-0644(99)70309-4. [DOI] [PubMed] [Google Scholar]
- 32.Phillips S, Rond PC, Kelly SM, Swartz PD. The need for pediatric-specific triage criteria: results from the Florida trauma triage study. Pediatr Emerg Care. 1996;12:394–398. doi: 10.1097/00006565-199612000-00002. [DOI] [PubMed] [Google Scholar]
- 33.Engum SA, Mitchell MK, Scherer LR, et al. Prehospital triage in the injured pediatric patient. J Pediatr Surg. 2000;35(1):82–87. doi: 10.1016/s0022-3468(00)80019-6. [DOI] [PubMed] [Google Scholar]
- 34.Burd RS, Jang TS, Nair SS. Predicting hospital mortality among injured children using a national trauma database. J Trauma. 2006;60:792–801. doi: 10.1097/01.ta.0000214589.02515.dd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.DiRusso SM, Sullivan T, Risucci D, Nealon P, Slim M. Intubation of pediatric trauma patients in the field: predictor of negative outcome despite risk stratification. J Trauma. 2005;59:84–91. doi: 10.1097/01.ta.0000171462.28379.f3. [DOI] [PubMed] [Google Scholar]
- 36.Edil BH, Tuggle DW, Jones S, et al. Pediatric major resuscitation—respiratory compromise as a criterion for mandatory surgeon presence. J Pediatr Surg. 2005;40:926–928. doi: 10.1016/j.jpedsurg.2005.03.006. [DOI] [PubMed] [Google Scholar]
- 37.Newgard CD, Hui J, Griffin A, Wuerstle M, Pratt F, Lewis RJ. Prospective validation of an out-of-hospital decision rule to identify seriously injured children involved in motor vehicle crashes. Acad Emerg Med. 2005;12:679–687. doi: 10.1197/j.aem.2005.03.526. [DOI] [PubMed] [Google Scholar]