Abstract
Study objective
The first hour after the onset of out-of-hospital traumatic injury is referred to as the “golden hour,” yet the relationship between time and outcome remains unclear. We evaluate the association between emergency medical services (EMS) intervals and mortality among trauma patients with field-based physiologic abnormality.
Methods
This was a secondary analysis of an out-of-hospital, prospective cohort registry of adult (aged ≥15 years) trauma patients transported by 146 EMS agencies to 51 Level I and II trauma hospitals in 10 sites across North America from December 1, 2005, through March 31, 2007. Inclusion criteria were systolic blood pressure less than or equal to 90 mm Hg, respiratory rate less than 10 or greater than 29 breaths/min, Glasgow Coma Scale score less than or equal to 12, or advanced airway intervention. The outcome was inhospital mortality. We evaluated EMS intervals (activation, response, on-scene, transport, and total time) with logistic regression and 2-step instrumental variable models, adjusted for field-based confounders.
Results
There were 3,656 trauma patients available for analysis, of whom 806 (22.0%) died. In multivariable analyses, there was no significant association between time and mortality for any EMS interval: activation (odds ratio [OR] 1.00; 95% confidence interval [CI] 0.95 to 1.05), response (OR 1.00; 95% CI 9.97 to 1.04), on-scene (OR 1.00; 95% CI 0.99 to 1.01), transport (OR 1.00; 95% CI 0.98 to 1.01), or total EMS time (OR 1.00; 95% CI 0.99 to 1.01). Subgroup and instrumental variable analyses did not qualitatively change these findings.
Conclusion
In this North American sample, there was no association between EMS intervals and mortality among injured patients with physiologic abnormality in the field.
INTRODUCTION
Background
The first 60 minutes after traumatic injury has been termed the “golden hour.”1 The concept that definitive trauma care must be initiated within this 60-minute window has been promulgated, taught, and practiced for more than 3 decades; the belief that injury outcomes improve with a reduction in time to definitive care is a basic premise of trauma systems and emergency medical services (EMS) systems. However, there is little evidence to directly support this relationship.1 Two studies from Quebec suggested that increased total out-of-hospital (ie, EMS) time was associated with increased mortality among seriously injured trauma patients,2,3 yet this finding has not been replicated in other settings.4-10 Additional studies suggesting a link between out-of-hospital time and outcome have been tempered by indirect comparisons,11 small samples of highly selected surgical patients,12-14 rural trauma patients with long EMS response times,15 and mixed samples that included patients with nontraumatic cardiac arrest.16,17
Importance
To date, patients with out-of-hospital cardiac arrest remain the only field-based patient population with a consistent association between time (response interval) and survival.18,19 Despite the paucity of outcome evidence supporting rapid out-of-hospital times for the broader population of patients activating the 911 system, EMS agencies in North America are generally held to strict standards about intervals, particularly the response interval. Meeting such expectations requires comprehensive emergency vehicle and personnel coverage throughout a community and travel at high speeds in risky traffic situations (eg, intersections) that occasionally result in crashes causing injury and death to emergency vehicle occupants and others.20-22 Demonstrating the benefit of such time standards in noncardiac arrest patients is important in justifying the resources and risks inherent in meeting such goals in EMS systems. Previous studies assessing the time-outcome association in trauma have been limited by heterogeneous patient groups, single EMS agencies, small sample sizes, and the exclusion of patients who died in the field.
Goals of This Investigation
In this study, we tested the association between EMS intervals and mortality among trauma patients known to be at high risk of adverse outcomes (those with field-based physiologic abnormality) in 146 diverse EMS agencies across 10 North American sites. Patients who died in the field were also examined as a subset of this population.
MATERIALS AND METHODS
Study Design
This was a secondary analysis of an out-of-hospital, consecutive-patient, prospective cohort registry of injured persons with field-based physiologic abnormality.
Setting
These data were collected as part of the Resuscitation Outcomes Consortium epidemiologic out-of-hospital trauma registry (the Resuscitation Outcomes Consortium Epistry-Trauma).23 The primary sample for this study was collected from December 1, 2005, through March 31, 2007. Eligible patients were identified from 146 EMS agencies (ground and air medical) transporting to 51 Level I and II trauma hospitals in 10 sites across the United States and Canada (Birmingham, AL; Dallas, TX; Iowa; Milwaukee, WI; Pittsburgh, PA; Portland, OR; King County, WA; Ottawa, ON; Toronto, ON; and Vancouver, BC). The sites vary in size, location, and EMS system structure and provide care to injured persons from diverse urban, suburban, rural, and frontier regions.24 One hundred fifty-three institutional review boards/research ethics boards (127 hospital-based and 26 EMS agency-based) in both the United States and Canada reviewed and approved the Resuscitation Outcomes Consortium Epistry-Trauma project and waived the requirement for informed consent.
Selection of Participants
The primary study cohort consisted of consecutive injured adults (aged ≥15 years) requiring activation of the emergency 911 system within predefined geographic regions at each Resuscitation Outcomes Consortium site. For the primary sample, patients must have been evaluated by an EMS provider, had signs of physiologic abnormality at any point during out-of-hospital evaluation, and required EMS transport to a hospital. The definition for out-of-hospital physiologic abnormality was based on the American College of Surgeons Committee on Trauma Field Triage Decision Scheme “Step 1” criteria25 that have been demonstrated to have high specificity for identifying patients with serious injury and need for specialized trauma resources.26-34 Injured patients with one or more of the following criteria were included: systolic blood pressure (SBP) less than or equal to 90 mm Hg, Glasgow Coma Scale (GCS) score less than or equal to 12, respiratory rate less than 10 or greater than 29 breaths/min, or advanced airway intervention (tracheal intubation, supraglottic airway, or cricothyrotomy). “Injury” was broadly defined as any blunt, penetrating, or burn mechanism for which the EMS provider(s) believed trauma to be the primary clinical insult.
The primary analysis included patients transported directly to trauma centers to minimize the effect of hospital type (trauma versus nontrauma hospitals) on outcome.35 Injured persons who were not transported by EMS (ie, died in the field with or without resuscitative measures, refused transport, or were not otherwise transported by EMS) were excluded from the primary analysis because certain out-of-hospital intervals (on-scene, transport, total out-of-hospital) could not be calculated. Children (aged <15 years) were excluded because of different responses to injury, different “normal” physiologic ranges compared with those of adults, and age-based variability in EMS procedure use (eg, tracheal intubation). Although these patients groups were excluded from the primary analysis, information on such patients was collected during the same period and included in sensitivity analyses to better understand how the broader inclusion of such injury patients may affect study results.
Patients enrolled in a concurrent clinical trial with embargoed outcomes (Hypertonic Resuscitation Following Traumatic Injury, ClinicalTrials.gov identifiers NCT00316017 and NCT00316004) were also excluded from the Trauma Epistry database.
Data Collection and Processing
The process used for data collection in Resuscitation Outcomes Consortium Epistry-Trauma has been described in detail elsewhere.23 In brief, each Resuscitation Outcomes Consortium site identified eligible out-of-hospital trauma patients from participating EMS agencies. Standardized data were collected from each agency, processed locally, entered into standardized data forms, matched to hospital outcomes, deidentified, and submitted to a central data coordinating center (Seattle, WA). Quality assurance processes included EMS provider data collection training, data element range and consistency checks, and annual site visits to review randomly selected study records, data capture processes, and local data quality efforts. Sites and agencies that had substantially higher or lower monthly case capture (relative to their average), as determined with a Poisson distribution with a 5% cutoff, were sent inquiries to reduce biased sampling. The dates for enrollment and resulting sample size were based on the initial inception of the Resuscitation Outcomes Consortium Epistry-Trauma database (December 1, 2005) through the most recent date demonstrating complete case capture and a high level of outcome completion (March 31, 2007).
Methods of Measurement
EMS intervals were calculated from dispatch records and all available out-of-hospital patient care reports. For patients with multiple sources of time records (eg, dispatch, 2 or more patient care reports from different EMS agencies), discrepancies were resolved between data sources to produce the most accurate representation of true times. Intervals were based on standard EMS definitions, including activation interval (time 911 call received at dispatch to alarm activation at EMS first response agency), response interval (time from alarm activation to arrival of first responding vehicle on scene), on-scene interval (time arrival of first EMS responding vehicle on scene until leaving the scene), and transport interval (time leaving the scene to vehicle arrival at the receiving hospital).36 We defined the total EMS interval as time from 911 call received to arrival at the receiving hospital. This definition was used to approximate the interval from time of injury to time of definitive care and represents a slightly longer duration than the “total out-of-hospital interval” defined by Spaite et al.36 Time at patient’s side and time of care transfer in the hospital were not consistently captured by all sites and were therefore not available in this study. We considered all intervals as continuous covariates but also evaluated categorical versions of total EMS time (≤60 versus >60 minutes) and response interval (<4, 4 to 8, and >8) according to previously defined response intervals for cardiac arrest.18,19
Fourteen additional out-of-hospital variables were considered in the analysis. Physiologic information included the initial (ie, preintervention) field values (SBP [mm Hg], GCS score, respiratory rate [breaths/min], shock index [pulse rate/SBP]) and use advanced airway procedures (tracheal intubation and “rescue” airways [supraglottic airway or cricothyrotomy]). SBP (<90, 150 to 179, and ≥180 mm Hg; reference 90 to 149 mm Hg) and respiratory rate (<10 and >29 breaths/min; reference 10 to 29 breaths/min) were categorized to allow for nonlinear associations with outcome. The “worst” physiologic values (eg, lowest GCS score) were also assessed to account for the portion of patients with repeated vital sign measurements that demonstrated physiologic decompensation after initial field assessment. Additional variables included age (years), sex, mechanism of injury (motor vehicle, motorcycle, pedal cyclist, pedestrian, other transport, fall, struck by/against, stabbing, firearm, machinery, burn, natural/environment, other), type of injury (blunt versus penetrating), trauma hospital level (I versus II), use of intravenous or intraosseous fluids, hemorrhage control (ie, compression), mode of transport (ground ambulance versus helicopter), EMS service level of first responding vehicle (advanced versus basic life support), and site. The primary outcome was inhospital mortality (whether in the emergency department [ED] or after hospital admission).
We also collected and geocoded census tract location of the injury event (ESRI ArcMap v. 9.1, Redlands, CA) and then identified the center of these locations by weighting on census block (United States) or dissemination areas (Canada). The straight-line distance from the weighted center of each census tract (the “centroid”) to the receiving hospital was then calculated for each patient and used as an instrument in 2-step instrumental variable analyses (described below). We validated this distance measure against the “true” distance calculated from latitude/longitude coordinates for a subset of patients at 2 sites (n=498).
Primary Data Analysis
We used descriptive statistics to compare groups by quartile of total EMS time. We then used 2 types of multivariable regression models to test the association between EMS intervals and mortality. Multivariable logistic regression models were used for all analyses, and 2-step instrumental variable models were used for analyses in which distance fulfilled criteria as an “instrument.” Instrumental variable analysis is an analytic strategy used in observational research to account for both measured and unmeasured confounders, allowing improved estimation of causal effect, provided an appropriate instrument is available and certain assumptions are met.37-39 The instrumental variable analysis was proposed in our study as a potential analytic solution to the dilemma of unmeasured confounding (eg, injury severity, patient acuity) and because we believed EMS intervals were strongly influenced by paramedic perception of serious injury and acuity (ie, shorter times for sicker patients with inherently worse prognosis). Measures of distance have been used as instruments in previous trauma studies.40,41 Additional details about the instrumental variable analysis are included in Appendix E1 (available online at http://www.annemergmed.com).
Study site was included in all models as a fixed-effects term to account for the potential clustering of cases within sites.42 We used an indicator of missingness to handle covariates with missing data because more sophisticated methods of handling missing values (eg, multiple imputation) present problems for combining results across 2-step instrumental variable models. The final models were generated according to a priori understanding of known confounders. Potential interactions between intervals and clinical covariates were tested, and the presence of effect modification was noted if such terms demonstrated statistical significance at P<.05. Model fit was assessed with the Hosmer-Lemeshow goodness of fit test and examination of diagnostic plots for change in coefficients (Δ-β) when individual episodes were excluded from the analysis.
Several important strata and subgroups were identified a priori for the analysis. These groups included mode of transport (ground ambulance versus air medical), level of first responding EMS vehicle on scene (advanced life support versus basic life support), injury type (blunt versus penetrating), traumatic brain injury (GCS score ≤8), shock (SBP ≤70 mm Hg or SBP 71 to 90 mm Hg, with pulse rate >108 beats/min43), advanced airway intervention, and country (United States versus Canada). Two additional subgroups (aged ≥65 years and Revised Trauma Score ≤2) were evaluated in post hoc analyses.
Regression analyses were performed using SPlus (version 6.2; Seattle, WA), and 2-step instrumental variable analyses were done with Stata (version 9.1; StataCorp, College Station, TX).
Sensitivity Analyses
To further explore the potential for correlated data to alter our results, we analyzed 2 additional cluster-adjusted analyses: a hierarchical linear probability model that allowed for non-nested multilevel clustering (up to 2 EMS agencies and hospital) and a random-effects model with sites as clusters. To better understand the relationship between time and outcome, sensitivity analyses also included injured adults transported by participating EMS agencies to all types of hospitals (trauma centers and nontrauma centers), children (aged <15 years), and patients who died in the field (activation and response intervals only).
RESULTS
Characteristics of Study Subjects
Of the 7,555 patients meeting Epistry inclusion criteria and transported to a hospital, there were 4,276 adult trauma patients transported by 146 EMS agencies to 51 Level I or II trauma centers during the 16-month period (Figure 1). After exclusion of patients with missing survival status (n=152), coenrollment in a concurrent clinical trial with embargoed outcomes (n=130), and missing or erroneous out-of-hospital times, locations, or other incomplete data (n=338), 3,656 adults with complete information were retained for the primary analysis (Figure 1). Eight hundred six (22.0%) patients died after EMS transport to a hospital, including 504 (62.5% of deaths) on the same day as EMS evaluation. Among hospitalized patients, median length of stay was 2 days (interquartile range [IQR] 0 to 8), though this was substantially different between survivors (median 3 days) and patients who died (median 0 days). When excluded patients (adults transported to major trauma centers; n=620) were compared with the study sample (n=3,656) for important demographic, physiologic, and mechanism measures, the excluded population was younger (median age 34 years; IQR 24 to 49 years), with slightly lower GCS scores (median 8; IQR 3 to 13), lower rate of penetrating injury (16.8%), and a higher rate of air medical transport (36.2%).
Figure 1.
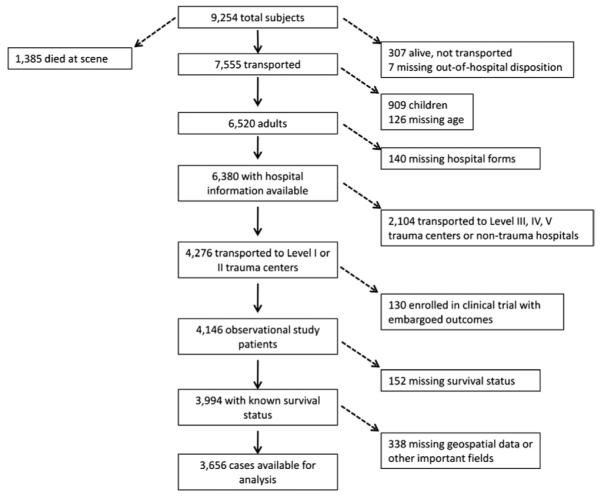
Flow diagram of patients included in the primary analysis.
There was substantial variation between sites and countries in all intervals (Table 1). Across the 10 sites, the median (IQR) intervals were activation 0.98 minutes (0.27 to 1.62 minutes), response 4.28 minutes (3.00 to 6.30 minutes), on-scene 19.0 minutes (13.4 to 26.0 minutes), transport 10.0 minutes (6.37 to 15.30 minutes), and total EMS time 36.3 minutes (28.4 to 47.0 minutes). Distribution of total EMS time is illustrated in Figure 2. Descriptive characteristics of the cohort, by quartiles of total time, are listed in Table 2. Depressed GCS score and hypotension (SBP ≤90 mm Hg) appeared more common among patients with the shortest EMS times, though other physiologic measures were similar across quartiles. The proportion of tracheal intubations attempted, median age, women, air medical transport, blunt injury, and unadjusted survival all increased with increasing total EMS times.
Table 1.
EMS intervals among trauma patients with physiologic abnormality, by site (n=3,656)
| Site | Activation Interval* | Response Interval* |
On-Scene Interval |
Transport Interval |
Total EMS Interval |
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| Median | IQR | Median | IQR | Median | IQR | Median | IQR | Median | IQR | |
| Birmingham, AL | 0.00 | 0.00-0.50 | 5.00 | 4.00-7.00 | 14.0 | 11.0-18.0 | 9.76 | 6.00-15.0 | 30.0 | 24.0-41.0 |
| Dallas, TX | 0.98 | 0.63-1.40 | 3.82 | 2.58-5.53 | 15.7 | 10.9-21.4 | 8.58 | 5.24-13.2 | 31.5 | 25.0-39.6 |
| Iowa | 0.86 | 0.02-1.53 | 4.00 | 3.00-5.55 | 15.4 | 11.9-20.0 | 7.98 | 4.93-10.2 | 28.1 | 23.3-37.2 |
| Milwaukee, WI | 0.00 | 0.00-1.00 | 3.00 | 3.00-4.00 | 22.0 | 16.0-27.0 | 12.0 | 9.00-15.0 | 38.0 | 32.0-45.0 |
| Ottawa | 0.60 | 0.37-1.00 | 5.44 | 3.88-8.19 | 21.2 | 15.9-27.5 | 9.67 | 6.45-16.0 | 39.3 | 31.2-49.1 |
| Pittsburgh, PA | 1.13 | 0.65-2.00 | 5.60 | 3.62-9.10 | 13.9 | 8.41-25.5 | 10.0 | 6.73-13.5 | 33.4 | 24.2-53.1 |
| Portland, OR | 0.18 | 0.10-0.72 | 4.28 | 3.10-5.94 | 16.8 | 12.4-23.0 | 13.5 | 9.60-18.1 | 36.3 | 29.6-45.9 |
| Seattle/King County, WA | 1.08 | 0.60-1.68 | 3.94 | 3.05-5.18 | 24.1 | 18.6-30.5 | 10.3 | 6.52-17.9 | 42.1 | 32.8-53.1 |
| Toronto | 1.62 | 1.00-2.38 | 4.78 | 3.52-7.45 | 19.1 | 14.4-25.0 | 9.45 | 5.00-15.1 | 37.0 | 29.6-48.1 |
| Vancouver | 1.70 | 1.12-2.68 | 4.99 | 3.16-8.18 | 20.3 | 14.8-29.3 | 10.1 | 6.24-15.5 | 39.0 | 31.1-54.5 |
| United States | 0.82 | 0.08-1.32 | 4.00 | 3.00-5.87 | 18.2 | 13.0-25.5 | 10.2 | 6.66-15.2 | 35.7 | 27.8-45.7 |
| Canada | 1.28 | 0.67-2.15 | 5.00 | 3.53-8.00 | 20.2 | 14.9-27.0 | 9.75 | 5.85-15.4 | 38.1 | 30.5-49.9 |
| Overall | 0.98 | 0.27-1.62 | 4.28 | 3.00-6.30 | 19.0 | 13.4-26.0 | 10.0 | 6.37-15.3 | 36.3 | 28.4-47.0 |
Calculation of activation and response intervals include patients who died in the field and had nonmissing values for times (n=914).
Figure 2.
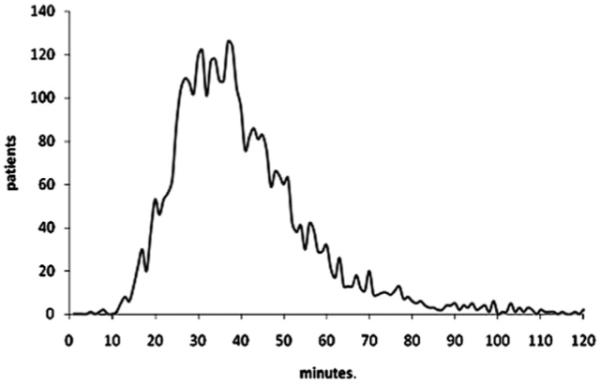
Distribution of the total EMS times for 10 sites across North America (n=3656).
Table 2.
Characteristics of injured persons with field physiologic abnormality, by quartile of total EMS time*
| Characteristics | Lowest (First) Quartile EMS Time (n=917) |
Second Quartile EMS Time (n=913) |
Third Quartile EMS Time (n=927) |
Highest (Fourth Quartile EMS Time (n=899) |
|---|---|---|---|---|
| Initial physiologic measures | ||||
| GCS score ≤12 (%) | 652 (71.1) | 602 (65.9) | 615 (66.3) | 535 (59.5) |
| Median GCS score (IQR) | 9 (3-14) | 10 (4-15) | 10 (3-15) | 11 (4-15) |
| SBP ≤90 mm Hg (%) | 418 (45.6) | 353 (38.7) | 361 (38.9) | 351 (39.0) |
| Median SBP (IQR) | 100 (70.5-134) | 110 (83-136) | 110 (81.5-140) | 110 (80-140) |
| RR <10 or >29 breaths/min (%) | 162 (17.7) | 167 (18.3) | 146 (15.7) | 167 (18.6) |
| Median low RR (IQR) | 18 (16-24) | 20 (16-24) | 20 (16-24) | 20 (16-24) |
| Pulse (beats/min) | ||||
| Median low pulse (IQR) | 94 (75-110) | 94 (80-110) | 92 (77.5-110) | 92 (76-110) |
| Median shock index, pulse/SBP (IQR) | 0.75 (0.55-1.00) | 0.78 (0.62-1.00) | 0.77 (0.60-1.00) | 0.78 (0.57-1.05 |
| Tracheal intubation attempt (%) | 194 (21.1) | 200 (21.9) | 237 (25.6) | 314 (34.9) |
| Rescue airway (%) | 22 (2.4) | 14 (1.5) | 14 (1.5) | 15 (1.7) |
| Median pulse oximetry (IQR) | 98 (94-99) | 97 (94-99) | 98 (95-100) | 98 (94-99) |
| Demographics | ||||
| Median age, y (IQR) | 34 (24-49) | 37 (25-50) | 38 (25-53) | 39 (25-54) |
| Male (%) | 697 (76.0) | 682 (74.7) | 669 (72.2) | 621 (69.1) |
| Type of injury (%) | ||||
| Blunt | 593 (64.7) | 667 (73.1) | 712 (76.8) | 744 (82.8) |
| Penetrating | 298 (32.5) | 228 (25.0) | 175 (18.9) | 106 (11.8) |
| Burn | 9 (1.0) | 10 (1.1) | 13 (1.4) | 12 (1.3) |
| Other | 7 (0.8) | 6 (0.7) | 16 (1.7) | 12 (1.3) |
| Unknown | 9 (1.0) | 2 (0.2) | 11 (1.2) | 23 (2.6) |
| Injury mechanism (%) | ||||
| Motor vehicle occupant | 163 (17.8) | 201 (22.0) | 209 (22.5) | 322 (35.8) |
| Motorcyclist | 38 (4.1) | 41 (4.5) | 29 (3.1) | 42 (4.6) |
| Pedal cyclist | 23 (2.5) | 29 (3.2) | 17 (1.8) | 16 (1.7) |
| Pedestrian | 126 (13.7) | 86 (9.4) | 75 (8.1) | 43 (4.8) |
| Other transport | 3 (0.3) | 6 (0.7) | 10 (1.1) | 20 (2.2) |
| Fall | 160 (17.4) | 212 (23.2) | 267 (28.8) | 231 (25.7) |
| Stuck by/against or crushed | 65 (7.1) | 80 (8.8) | 91 (9.8) | 82 (9.1) |
| Cut/pierce stab | 102 (11.1) | 78 (8.5) | 72 (7.8) | 38 (4.2) |
| Fire/burn | 10 (1.1) | 12 (1.3) | 10 (1.1) | 10 (1.1) |
| Machinery | 5 (0.5) | 2 (0.2) | 4 (0.4) | 5 (0.6) |
| Firearm gunshot | 183 (20.0) | 139 (15.2) | 98 (10.6) | 57 (6.3) |
| Natural/environment | 1 (0.1) | 0 | 0 | 0 |
| Other | 17 (1.9) | 23 (2.5) | 29 (3.1) | 23 (2.6) |
| Unknown | 19 (2.1) | 4 (0.4) | 16 (1.7) | 9 (1.0) |
| Scene information | ||||
| Time of day | ||||
| Morning (%) | 100 (10.9) | 112 (12.3) | 143 (15.4) | 144 (16.0) |
| Day (%) | 194 (21.1) | 219 (24.0) | 229 (24.7) | 244 (27.1) |
| Evening (%) | 302 (32.9) | 286 (31.3) | 269 (29.0) | 267 (29.7) |
| Night (%) | 321 (35.0) | 296 (32.4) | 286 (30.9) | 244 (27.1) |
| Weekend (%) | 324 (35.3) | 315 (34.5) | 336 (36.2) | 313 (34.8) |
| Air medical transport | 2 (0.2) | 7 (0.8) | 20 (2.2) | 133 (14.8) |
| Hospitals receiving patients | 40 | 43 | 47 | 44 |
| Outcomes | ||||
| Mortality (%) | 268 (29.2) | 189 (20.7) | 181 (19.5) | 168 (18.7) |
| Median hospital length of stay (days) | 1 (0-8) | 2 (0-8) | 2 (0-8) | 3 (0-11) |
RR, Respiratory rate.
Values were calculated according to available (ie, nonmissing) data. Rescue airways included supraglottic airway (eg, esophageal-tracheal twin-lumen airway device [Combitube; Kendall-Sheridan Catheter Corp, Argyle, NY]) or cricothyrotomy.
Main Results
In the multivariable logistic regression model, total EMS time was not associated with mortality (odds ratio [OR] for every minute of total time 1.00; 95% confidence interval [CI] 0.99 to 1.01) (Table 3). When the sample was assessed with 10-minute increments for total EMS time, there was no evidence of increased mortality with increasing field times (OR 0.90; 95% CI 0.80 to 1.02). Similar results were obtained when total times were grouped by quartile (OR 0.95; 95% CI 0.83 to 1.08). We were also unable to demonstrate independent associations between mortality and any other EMS interval for the overall sample (Table 4). When total EMS time was dichotomized to compare patients with greater than 60 minutes to those with less than or equal to 60 minutes, there was no association with mortality (OR 1.11; 95% CI 0.70 to 1.77). Categorization of total EMS time into quartiles did not suggest a threshold effect between time and mortality (quartile 1=reference; quartile 2=OR 0.69, 95% CI 0.47 to 1.00; quartile 3=OR 0.77, 95% CI 0.53 to 1.13; quartile 4=OR 0.81, 95% CI 0.54 to 1.21). For categorized response interval, there was no association with mortality for patients with a 4- to 8-minute interval (OR 0.95; 95% CI 0.71 to 1.25) or greater than 8-minute interval (OR 1.22; 95% CI 0.80 to 1.85) compared with patients with a response less than 4 minutes. Two-step instrumental variable analyses were used only in subgroup analyses (described below) because the correlation between distance and time was low (F test <10) for all intervals using the primary sample. These results did not qualitatively change when the “worst” physiologic values were used in place of initial values (data not shown). The primary model was well fit (Hosmer-Lemeshow goodness of fit statistic P=.80). There was no evidence of effect modification between any interval and clinical variables (all interactions P>.05).
Table 3.
Multivariable logistic regression model evaluating the association between total EMS time and mortality (n=3,656)*
| Covariates | OR | 95% CI |
|---|---|---|
| Total EMS time (by minute) | 1.00 | (0.99-1.01) |
| Ln (age) | 4.63 | (3.34-6.42) |
| Sex | 0.87 | (0.65-1.16) |
| Air transport | 0.71 | (0.34-1.48) |
| GCS score obtained | 5.42 | (3.17-9.26) |
| Total GCS score (by increasing score) | 0.81 | (0.78-0.84) |
| SBP obtained | 0.10 | (0.04-0.23) |
| SBP <90 mm Hg | 1.62 | (1.10-2.38) |
| 180>SBP≥150 mm Hg | 1.06 | (0.71-1.58) |
| SBP ≥180 mm Hg | 1.57 | (0.93-2.65) |
| 150>SBP≥90 mm Hg | Reference | |
| Respiratory rate obtained | 0.39 | (0.21-0.75) |
| Respiratory rate <10 breaths/min | 3.87 | (2.45-6.12) |
| Respiratory rate >29 breaths/min | 1.42 | (0.93-2.19) |
| 29≥RR≥10 | Reference | |
| Shock index ≥1.0 | 1.32 | (0.93-1.88) |
| Shock index <1.0 | Reference | |
| Firearm or stabbing | 1.06 | (0.57-1.96) |
| Burn | 2.02 | (1.37-2.99) |
| Struck by/against crushed or fall | 0.79 | (0.22-2.82) |
| Other injury mechanism | 0.93 | (0.67-1.28) |
| Motor vehicle related | Reference | |
| Intravenous or intraosseous line placed | 1.03 | (0.69-1.56) |
| Hemorrhage control | 0.72 | (0.50-1.03) |
| Tracheal intubation attempt | 3.76 | (2.65-5.34) |
| Rescue airway | 2.60 | (1.10-6.15) |
| Hospital level | 1.13 | (0.72-1.77) |
Site was included in the model as a fixed-effects term to account for clustering.
Table 4.
Adjusted ORs for mortality, using EMS intervals (in minutes) among injury subgroups*
| Subgroup/Strata | n | Total EMS Interval | Activation Interval |
Response Interval |
On-Scene Interval |
Transport Interval |
|---|---|---|---|---|---|---|
| Ground | 3,498 | 1.00 (0.99-1.01) | 1.00 (0.95-1.05) | 1.00 (0.96-1.04) | 1.00 (0.98-1.01) | 1.00 (0.99-1.01) |
| Air | 158 | 0.97 (0.91-1.02) | 0.67 (0.25-1.79) | 1.00 (0.87-1.16) | 1.03 (0.97-1.09) | 0.93 (0.86-1.02) |
| Blunt | 2,716 | 1.00 (0.99-1.005) | 1.00 (0.95-1.05) | 1.01 (0.97-1.06) | 0.99 (0.98-1.01) | 0.99 (0.98-1.01) |
| Penetrating | 807 | 1.01 (0.99-1.04) | 1.01 (0.73-1.39) | 1.03 (0.94-1.13) | 1.02 (0.99-1.05) | 1.01 (0.96-1.06) |
| TBI (GCS score ≤8) | 1,145 | 0.99 (0.98-1.003) | 0.92 (0.82-1.03) | 0.98 (0.93-1.04) | 0.99 (0.98-1.01) | 0.99 (0.97-1.01) |
| Shock (SBP ≤70, or SBP 71-90 with pulse rate ≥108 beats/min) |
1,483 | 0.99 (0.98-1.01) | 0.86 (0.68-1.10) | 1.02 (0.95-1.09) | 1.00 (0.98-1.03) | 0.97 (0.94-1.001) |
| Advanced airway management | 945 | 0.99 (0.98-1.01) | 1.05 (0.95-1.16) | 0.97 (0.89-1.05) | 1.00 (0.98-1.02) | 0.98 (0.96-1.01) |
| Revised Trauma Score ≤2 | 79 | 1.01 (0.94-1.09) | 1.79 (0.49-6.50) | 1.32 (0.51-3.44) | 1.00 (0.93-1.08) | 1.09 (0.87-1.36) |
| BLS first arriving | 1,803 | 1.01 (0.99-1.02) | 1.03 (0.97-1.10) | 0.99 (0.94-1.05) | 1.01 (0.99-1.03) | 1.00 (0.997-1.003) |
| ALS first arriving | 1,853 | 0.99 (0.98-1.002) | 0.76 (0.60-0.96) | 1.01 (0.96-1.06) | 0.99 (0.97-1.01) | 0.99 (0.97-1.001) |
| Elders (≥65 y) | 472 | 1.00 (0.99-1.02) | 1.02 (0.96-1.07) | 0.98 (0.89-1.07) | 1.00 (0.97-1.03) | 1.03 (0.996-1.06) |
| United States | 2,610 | 0.99 (0.98-1.004)† | 1.04 (0.97-1.11) | 1.04 (0.98-1.09) | 0.99 (0.97-1.01) | 0.99 (0.97-1.01) |
| Canada | 1,046 | 1.00 (0.99-1.01) | 0.94 (0.85-1.04) | 0.97 (0.91-1.03) | 1.00 (0.98-1.02) | 1.00 (0.98-1.02) |
| Overall | 3,656 | 1.00 (0.99-1.01) | 1.00 (0.95-1.05) | 1.00 (0.97-1.04) | 1.00 (0.99-1.01) | 1.00 (0.98-1.01) |
TBI, Traumatic brain injury; BLS, basic life support; ALS, advanced life support.
In addition to interval, multivariable logistic regression models included the following covariates: age, sex, mode of transport, site, GCS score, SBP, respiratory rate, shock index, mechanism of injury, field intravenous or intraosseous fluid administration, tracheal intubation attempt, use of a rescue airway, field hemorrhage control, and hospital level. For each time interval point estimate, 95% confidence intervals are listed in parentheses.
Results for 2-step instrumental variable analyses for US trauma patients: OR 1.00 (95% CI 0.997 to 1.001).
Adjusted ORs for mortality among the subgroups are presented in Table 4. In multivariable logistic regression models, there was no demonstrable association between time and mortality for any subgroup. The only subgroup that met criteria for using instrumental variable analyses to assess total EMS time was trauma patients transported in the United States (F statistic 46.4), and these results were not qualitatively different (OR 1.00; 95% CI 0.997 to 1.001).
Sensitivity Analysis
Using a random-effects model with sites as clusters, the lack of association between total EMS time and mortality persisted (OR 0.99; 95% CI 0.999 to 1.0003). In a hierarchical, non-nested linear probability model integrating EMS agencies (up to 2) and hospital as clusters, there remained no association between total EMS time and mortality (linear probability estimate −0.0004; 95% CI −.001 to 0.0003).
When the sample was expanded to include injured adults transported to all types of hospitals (restricted to those with outcomes available; n=5,356), there remained no association between total EMS time and mortality (OR 1.00 per minute; 95% CI 0.99 to 1.00), or between other intervals and mortality (data not shown). Among the 460 children transported to Level I or II trauma centers with outcome information available, there was no association between mortality and total EMS time or other intervals (data not shown).
Of the 1,385 patients who died at the scene after injury, there were 914 adults with interval data available for analysis. Of these patients, 722 (79%) were declared dead without attempted resuscitation, 130 (14%) had attempted resuscitation with no documented vital signs, and 62 (7%) had attempted resuscitation with documented initial vital signs. The median (IQR) activation and response intervals for patients who died in the field were 1.00 minute (0.43 to 1.67 minutes) and 4.92 minutes (3.27 to 7.38 minutes) for those without resuscitation; 1.03 minutes (0.58 to 1.67 minutes) and 5.00 minutes (3.62 to 7.69 minutes) for patients with resuscitation attempted and no vital signs; and 1.00 minute (0.32 to 1.57 minutes) and 4.58 minutes (3.40 to 7.33 minutes) for patients with resuscitation attempted and initial measurable vital signs. These intervals were slightly longer than the median activation interval (0.98 minutes; IQR 0.27 to 1.62 minutes) and response interval (4.28 minutes; IQR 3.00 to 6.30 minutes) for patients transported to a hospital (P<.001). When we reevaluated the multivariable models with both the primary sample and patients who died in the field after attempted resuscitation, there remained no statistical association between time and mortality for activation (OR 1.00; 95% CI 0.97 to 1.04) or response (OR 1.00; 95% CI 0.99 to 1.04) intervals. These results persisted when all patients who died in the field (with or without a resuscitation attempt) were included in the models (data not shown).
LIMITATIONS
Previous studies have demonstrated an apparent association between increasing out-of-hospital time and decreased mortality (ie, the appearance that longer times decrease mortality),7-10,16 even after accounting for injury severity. This phenomenon is at least partly explained by EMS providers moving and driving faster for patients believed to have serious injury and spending more time on calls with patients recognized as having minor injury (ie, less urgency to get such patients to a hospital). The association between increasing injury severity and decreased on-scene and transport intervals has been previously demonstrated.6,7,44 This type of confounding, which is unlikely to be fully accounted for with available variables (ie, unmeasured confounding), was the primary reason we considered instrumental variable models in addition to logistic regression. Although the instrumental variables strategy ultimately could not be used for most analyses, the subgroup analysis that met criteria for such analysis generated results similar to those of logistic regression models.
Detailed hospital-based information, including measures of injury severity (eg, Injury Severity Score), was not available in the Resuscitation Outcomes Consortium Epistry-Trauma database. We used field-based information to adjust for confounding by injury severity, though it is possible that these measures did not fully account for such relationships. We also did not have longer term (eg, 30-day survival) or functional outcomes for these patients, either of which may have altered the results. In addition, the exclusion of patients enrolled in the concurrent clinical trial and those with missing data could have introduced bias to the results.
There was substantial variability in intervals between sites and heterogeneity in our patient population. Such differences likely reflect geographic variation (eg, rural land mass), variability in EMS agencies, EMS system differences, population variation in injury mechanisms (eg, penetrating trauma), and response to injury, plus other factors. A large meta-analysis similarly demonstrated time differences among trauma patients cared for by urban/suburban versus rural ground ambulance crews, especially for activation, response, and transport intervals.45 Although the inclusion criteria were designed to reduce heterogeneity and isolate a field-identified high-risk trauma population, some variability between patients and sites was unavoidable. This variability may have further reduced our ability to demonstrate an association between time and outcome, though we believe inclusion of such a broad and heterogeneous group of sites increased the generalizability of our findings.
In addition to variation in intervals, there was also likely variation in field care, hospital care, and injury characteristics between sites, EMS agencies, and hospitals. We attempted to account for this possibility by using fixed-effects models, with sites as clusters. There was likely clustering present on many levels (eg, EMS agencies, hospitals, providers), with overlap between clusters (non-nested), which produced challenges in fully accounting for such potentially correlated data. However, different model specification (ie, hierarchical) to account for non-nested multilevel clustering (ie, EMS agency, hospital) and using random-effects models did not qualitatively change our study results. It is also possible that addressing the study question using sites with mature EMS systems and relatively short EMS intervals could have suppressed a demonstrable association between time and outcome. That is, most patients had a total EMS time well below 60 minutes, which may have precluded the ability to fully test the “golden hour” premise based on a 60-minute cut point. A nonlinear relationship between time and outcome could also exist, though categorical terms for the total EMS interval and response interval did not suggest such a relationship.
The duration of time from EMS dispatch through delivery to the receiving hospital represents only a portion of the time from actual injury event to definitive care. We did not know the time of injury and were therefore unable to measure the interval from injury onset to hospital arrival, which may represent a critical window for a small portion of patients (eg, those who die in the field). Our definition for total EMS time and the “golden hour” in this study was based on the assumption that the time between injury onset and 911 notification was short, though this may not have been the case with all patients (eg, unwitnessed injury events, rural areas, lack of immediate telephone access, or call coverage). Time to hospital arrival may also be different from the time to definitive care (eg, for patients requiring operative intervention or other important hospital-based interventions), which may also have affected the ability to demonstrate an association between time and outcome.
Finally, the use of instrumental variable analysis is predicated on having an available instrument that fulfills all the required criteria and assumptions. Unfortunately, after geocoding of all injury census tracts to generate the distance measure in this sample, distance did not ultimately have a strong correlation with EMS intervals. There was only one subgroup that met our predefined criteria to use distance as an instrument (F test >10), and this analysis produced similar results to those from logistic regression models. Despite the fact that we could use instrumental variable methods in only a small portion of the analysis, we believe these results support our overall findings of no demonstrable association between time and outcome.
DISCUSSION
In this study, we were unable to support the contention that shorter out-of-hospital times (as measured from receipt of 911 call to hospital arrival) improve survival among injured adults with field-based physiologic abnormality. This finding persisted across many subgroups, including level of first responding EMS provider, mode of transport, country, age, injury type, and more severe physiologic derangement. Our findings are consistent with those of previous studies that similarly have failed to demonstrate a relationship between out-of-hospital time and outcome using different patient populations, trauma and EMS systems, regions, data sources, and confounders.4-10 However, we believe our findings are unique because of the field-based inclusion criteria for a recognized high-risk subset of injured patients, the sampling design of Epistry (population-based data from a large number of EMS agencies and sites across North America), sensitivity analyses that included deaths in the field and non–trauma center patients, and rigorous data collection for EMS times that accounted for multiple EMS agencies caring for the same patient.
It is possible that other factors, such as unmeasured confounders, selection bias, statistical approach, inclusion criteria, intervals assessed, or heterogeneity in the sample (variance), precluded our ability to show such an association. Although it is likely that minutes do affect outcome for certain severely injured individuals, demonstrating this relationship across a field-defined population of injured persons using EMS intervals has generally produced inconclusive results. The 2 previous studies from Quebec suggesting an association between total out-of-hospital time and mortality were conducted with retrospectively defined samples of seriously injured patients2,3 and have not been replicated in other settings. Although a cornerstone of trauma systems, the “golden hour” premise has proven challenging to consistently demonstrate across larger samples of trauma patients and specific EMS intervals. One must also consider the possibility that assessing the influence of EMS time on outcome is not feasible through an observational study design because of inherent forms of bias and unmeasured confounding. Because more rigorous study designs (ie, randomized controlled trials or quasi-experimental designs) are generally not practical, feasible, or ethical for addressing this study question, adequately testing the hypothesis that shorter intervals improve outcomes may not be possible.
The only condition in which rapid EMS response has been shown to consistently improve survival is nontraumatic cardiac arrest.18,19 Although several studies have demonstrated the survival benefit of trauma systems and trauma centers,2,35,46-49 the benefit of advanced out-of-hospital trauma care (eg, advanced airway intervention and intravenous fluid resuscitation) remains unclear. Further, there is a growing body of literature questioning the benefit of out-of-hospital advanced life support practices in trauma patients.4,50-54 Although some seriously injured individuals may require time-dependent EMS interventions to survive (eg, airway obstruction, respiratory arrest, external hemorrhage at a compressible site), faster application of such interventions may not have a measureable effect on outcomes for most trauma patients. It is also plausible that the “golden hour” is primarily dependent on the timeliness of hospital-based interventions (ie, initiation of definitive care after arrival at an ED), rather than out-of-hospital care. Although the relationship between hospital time and outcome among seriously injured patients also remains unproven, such a possibility would lend credence to the “golden hour” concept and be consistent with the previously demonstrated hospital-based effect on survival.35
The relationship between duration of on-scene time and outcomes in trauma also remains unclear. In this study, we were unable to demonstrate a significant relationship between time on-scene and mortality. Previous studies have suggested that on-scene time is affected by injury severity, plus the number and type of EMS interventions.44,55,56 As with response intervals, many urban EMS systems are held to specific standards for the acceptable duration of on-scene care. As the scope of practice among EMS providers increases (eg, rapid sequence tracheal intubation, advanced airway management, use of additional medications), such standards may help to contain the opportunity for very long on-scene times. However, our results do not suggest an important association between shorter scene times and improved survival.
Similarly, there has been little information to evaluate the potential effect of transport times on outcomes in trauma. Patients perceived by EMS providers to have serious injury are frequently transported to the hospital by “lights and siren” to facilitate rapid arrival at a trauma center. The demonstrated survival benefit of treating seriously injured patients in trauma centers2,35,46-49 suggests that time lost bypassing nontrauma hospitals is recouped by the benefits of specialized care provided for injured persons at major trauma centers. One previous study found that although transport times to trauma centers were higher for patients bypassing other local facilities, longer transport times were not associated with adverse outcomes.57 Our findings support this conclusion and further substantiate the practice of transporting patients presumed to have serious injury to trauma centers, despite longer transport times.
Although the association between out-of-hospital time and outcome remains unsubstantiated beyond persons in cardiac arrest, there is a public expectation of rapid EMS response and care after activation of the 911 system. In the setting of a perceived “emergency,” the public may not necessarily value whether faster EMS time and expeditious care have been shown to save lives for the majority of clinical conditions. However, meeting these expectations costs money (eg, establishment of fire houses and positioning of EMS crews to achieve predefined response intervals), can place EMS providers, patients, and the nearby public at risk,20-22 and is a common reason (ie, emergency vehicle crashes) for tort claims against EMS agencies.58 In an increasingly costly and competitive health care environment, these factors must be contemplated when seeking to further “optimize” EMS systems.
Among injured patients with physiologic abnormality prospectively sampled from a diverse group of sites and EMS systems across North America, there was no association between EMS intervals and mortality.
Editor’s Capsule Summary.
What is already known on this topic
The “golden hour” concept in trauma is pervasive despite little evidence to support it.
What question this study addressed
Is there an association between various emergency medical services (EMS) intervals and inhospital mortality in seriously injured adults?
What this study adds to our knowledge
In 3,656 injured patients with substantial perturbations of vital signs or mental status, transported by 146 EMS agencies to 51 trauma centers across North America, no association was found among any EMS interval and mortality.
How this might change clinical practice
This study suggests that in our current out-of-hospital and emergency care system time may be less crucial than once thought. Routine lights-and-sirens transport for trauma patients, with its inherent risks, may not be warranted.
Acknowledgments
The authors thank the many contributing EMS agencies, EMS providers, study coordinators, staff, and investigators (see Appendix E2, available online at http://www.annemergmed.com) for their willingness to participate in and support this project and for their continued dedication to improving the EMS care and outcomes for their patients.
Funding and support: By Annals policy, all authors are required to disclose any and all commercial, financial, and other relationships in any way related to the subject of this article that might create any potential conflict of interest. See the Manuscript Submission Agreement in this issue for examples of specific conflicts covered by this statement. The Resuscitation Outcome Consortium was supported by a series of cooperative agreements to 10 regional clinical centers and 1 data coordinating center (5U01 HL077863, HL077881, HL077871, HL077872, HL077866, HL077908, HL077867, HL077885, HL077877, HL077873) from the National Heart, Lung, and Blood Institute, in partnership with the National Institute of Neurological Disorders and Stroke, US Army Medical Research and Material Command, the Canadian Institutes of Health Research-Institute of Circulatory and Respiratory Health, Defence Research and Development Canada, the Heart and Stroke Foundation of Canada, and the American Heart Association.
APPENDIX E1
Instrumental variables analysis
Instrumental variable analysis is an analytic strategy used in observational research to account for both measured and unmeasured confounders, allowing improved estimation of causal effect, provided an appropriate instrument is available and certain assumptions are met.37-39 Instrumental variable analysis was proposed in our study as a potential analytic solution to the dilemma of unmeasured confounding (eg, injury severity, patient acuity, and the phenomenon of shorter times for sicker patients with inherently worse prognosis) that may not have been fully accounted for in measured predictor variables. Martens et al37 observed that through certain assumptions, the causal effect of the exposure (in this case, time) on the outcome can be captured through the relationship between the exposure and the instrumental variable. Specifically, McClellan et al38 observed that it is possible to mimic randomization of patients to the likelihood of receiving a certain treatment according to the association between treatment and the instrumental variable. This process eliminates unmeasured confounders and allows for the estimation of causal effect in terms of the likelihood. A Hausman test is also generally used to determine whether a single equation model is sufficient versus use of a 2-step instrumental variable analysis to remove bias associated with unobserved confounders.
In essence, 2 relevant equations are estimated:
| (1) |
| (2) |
where Y is the outcome of interest, T is the predictor of interest (eg, time), X represents other confounders, Z is the instrumental variable, and E and F are error terms. The key assumptions in instrumental variable analyses are (1) Z and T are highly correlated such that T can be predicted from Z; (2) there is no confounding of the Z and T association; and (3) Z and Y are uncorrelated (except through Z’s influence on T).
We proposed using distance as an instrumental variable because of its perceived correlation with time, lack of correlation with survival (except through time), and demonstrated success in previous trauma research with instrumental variable analyses.40,41 In this situation, if we assume distance to be Z and time T, we then use the instrumental variable model to estimate the likelihood of different intervals according to distance; this likelihood is then used to estimate the causal effect of time on outcome. Because a weak instrument can introduce bias to an analysis, the F statistic is typically used to assess adequate correlation between T (time) and Z (distance) after accounting for X (important confounders), with F greater than 10 indicating an adequate instrument.39 In this study, we tested the appropriateness of distance as an instrument for all intervals in the primary sample and for total EMS time in all subgroups. Only the subgroup of trauma patients treated in the United States fulfilled criteria for using distance as an instrument (F test >10), which restricted our use of instrumental variable analysis to this subgroup of patients.
APPENDIX E2
ROC Epistry contributors
Alabama Resuscitation Center, University of Alabama at Birmingham, Birmingham, AL: Jeffrey D. Kerby, MD, PhD, Principal Investigator
Core Investigators: Todd B. Brown, MD, MSPH, Thomas Terndrup, MD
Coordinators: Shannon W. Stephens, EMT-P, Carolyn R. Williams, BSN, BSME
EMS Investigators/Collaborators: Joe E. Acker, EMT-P, MPH, Michael L. Minor, EMT-P
Hospital Investigators/Collaborators: Paul A. MacLennan, PhD, Patrick R. Pritchard, MD, Sandra Caldwell, MA, Katherine R. Lai, BS
Participating EMS Agencies: Alabama LifeSaver, Bessemer Fire and Rescue, Birmingham Fire and Rescue, Center Point Fire District, Chelsea Fire and Rescue, American Medical Response, Homewood Fire Dept., Pelham Fire Dept., Rocky Ridge Fire Dept., Regional Paramedic Services, Trussville Fire Dept., Vestavia Hills Fire and Rescue
Dallas Center for Resuscitation Research, University of Texas Southwestern Medical Center, Dallas, TX: Ahamed H. Idris, MD, Principal Investigator
Core Investigators: Fernando Benitez, MD, Raymond Fowler, MD, Dorothy Lemecha, MD, Joseph Minei, MD, Paul Pepe, MD, Michael Ramsay, MD, Robert Simonson, MD, Jane Wigginton, MD
Coordinators: Dixie Climer, RN, Melinda Moffat, RN, Kate Newman, RN, Pamela Owens, Andrea Bennett, BS
EMS Investigators/Collaborators: Richard Black, EMT-P, Debra Cason, RN, Billy Craft, EMT-P, Lucy Detamble, RN, Ryan Dykes, EMT-P, Tony Harvey, EMT-P, Suzanne Hewitt, RN, Marshal Isaacs, MD, Joe Kay, EMT-P, Tami Kayea, EMT-P, Richard La-Chance, EMT-P, Thomas Lehman, Paul Mayer, MD, Jeffrey Metzger, MD, Danny Miller, EMT-P, Kenneth Navarro, EMT-P, Steven Parker, EMT-P, Karen Pickard, RN, Warren Porter, EMT-P, TJ Starling, EMT-P, Tommy Tine, EMT-P, Chris Vinson, EMT-P
Hospital Investigators/Collaborators: David Abebefe, MD, Steven Arze, MD, Sean Black, MD, Matthew Bush, MD, Michael Forman, MD, Jeffery Goodloe, MD, Ralph Kelly, DO, Gregory Lachar, MD, Alicia Mangram, MD, Marc Morales, MD, Edward Thornton, MD, Robert Wiebe, MD
Participating EMS Agencies: Carrollton Fire Dept., Dallas Fire and Rescue, DeSoto Fire Dept., Duncanville Fire Dept., Farmers Branch Fire Dept., Garland Fire Dept., Highland Park Dept. of Public Safety, Irving Fire Dept., Lancaster Fire Dept., Mesquite Fire Dept., Plano Fire Dept., University Park Fire Dept.
University of Iowa Carver College of Medicine-Iowa Resuscitation Network, University of Iowa, Iowa City, IA: Richard Kerber, MD, Principal Investigator
Core Investigators: Steve Hata, MD, Dianne Atkins, MD
Coordinators: Melanie Kenney, RN, MA, CPNP, Catherine Rost, Alexander Drum, EMT-P, Michael Hartley, EMT-P
Participating EMS Agencies: Area Ambulance Service, Davenport Hospital Ambulance Corporation, Covenant Health System - Covenant Ambulance, Covenant Health System - Mercy Oelwein, Covenant Health System - Sartori, City of Dubuque Fire Dept., Dallas County Emergency Medical Services, West Des Moines Emergency Medical Services, Des Moines Fire Dept. EMS, Henry County Health Center Emergency Medical Services, Johnson County Ambulance, Siouxland Paramedics, Inc., Waterloo Fire Rescue
Milwaukee Resuscitation Research Center, Medical College of Wisconsin, Milwaukee, WI: Tom P. Aufderheide, MD, Principal Investigator
Core Investigators: Ronald G. Pirrallo, MD, MHSA, Karen J. Brasel, MD, MPH, Andrea L. Winthrop, MD, John P. Klein, PhD
Coordinators: David J. Kitscha, BS, MS, Barbara J. Burja, BA, EMT, Chris von Briesen, BA, CCRC, Christopher W. Sparks, EMT, Sara Kaebisch, BS
EMS Investigators/Collaborators: John Chianelli, MS, Rosemarie Forster, MSOLQ, RHIA, EMT-P, Michael Milbrath, EMT-P, Lauryl Pukansky, BS, RHIA, Kenneth Sternig, MS-EHS, BSN, EMT-P, Eugene Chin, RN, EMT-P, Nancy Frieberg, RN, EMT-P, Kim Krueger, RN, EMT-P, Del Szewczuga, RN, EMT-P Thomas Duerr, Rebecca Funk, BS, RHIA, EMT-B, Gail Jacobsen, BS, Janis Spitzer, Richard Demien, James Martins, John Cohn, Russell R. Spahn, MA, EMT-P, Mike Jankowski, BA, EMT-P, Timothy James, William E. Wentlandt Jr., MBA, EFO, David Berousek, Brian M. Satula, BA, NREMT, Jay B. Behling, BS, EMT-B, Dean K. Redman, BA, EFO, Steven Hook, BS, CFOD, Andrew Neargarder, Jim Singer, RN
Hospital Investigators/Collaborators: Thomas Reminga, MD, Dennis Shepherd, MD, Peter Holzhauer, MD, Jonathan Rubin, MD, Craig Skold, MD, Orlando Alvarez, MD, Heidi Harkins, MD, Edward Barthell, MD, William Haselow, MD, Albert Yee, MD, John Whitcomb, MD, Eduardo E. Castro, MD, Steven Motarjeme, MD
Participating EMS Agencies: Cudahy Fire Dept., Flight for Life, Franklin Fire Dept., Greendale Fire Dept., Greenfield Fire Dept., Hales Corners Fire Dept., Milwaukee County Airport Fire Dept., Milwaukee Fire Dept., North Shore Fire Dept., Oak Creek Fire Dept., South Milwaukee Fire Dept., St. Francis Fire Dept., Wauwatosa Fire Dept., West Allis Fire Dept.
Ottawa/OPALS/British Columbia RCC, Ottawa Health Research Institute, University of Ottawa, Ottawa, Ontario and St. Paul’s Hospital, University of British Columbia, British Columbia, Canada: Ian Stiell, MD, Principal Investigator
Core Investigators: Jim Christenson, MD, Morad Hameed, MD, Jean Denis Yelle, MD, Martin Osmond, MD, Christian Vaillancourt, MD, David Evans, MD, Riyad Abu-Laban, MD
Coordinators: Cathy Clement, RN, Tammy Beaudoin, CCHRA, Barb Boychuk, RN, Sarah Pennington, RN, Helen Connolly, RN, Patrick Lefaivre, PCP, Jane Banek, CCHRA, Angela Marcantonio, Rina Marcantonio, CCHRA, Christine Leclair, RN, Julie Cummins, RN
EMS Investigators/Collaborators: Matthew Stempien, MD, Jonathan Dreyer, MD, Douglas Munkley, MD, Justin Maloney, MD, Paul Colella, MD, Andrew Affleck, MD, David Waldbillig, MD, Paul Bradford, MD, Martin Lees, MD, Vincent Arcieri, MD, Ann Wilson, BSc, ACP, Kenneth Boyle, EMCA, RRT, CMA, Lorraine Luinstra-Toohey, BScN, MHA, John Trickett, BScN, Nicole Sykes, BScN, RN, Elaine Graham, ACP, Kieran Ballah, EMCA, Cathy Hedges, A-EMCA, ACP, Paul Mathers, A-EMCA, Dug Andrusiek, MSc, Dan Bishop, ACP, Ron Straight, ACP, Brian Twaites, ACP, Stuart Donn, PhD
Participating EMS Agencies: A.A. and M. Volunteer Ambulance Service, Burlington Fire and Rescue, Cambridge Fire Dept., Cornwall Fire and Rescue, Cornwall SDG Emergency Medical Services, Essex-Windsor Emergency Medical Services, Essex-Windsor Fire and Rescue, Frontenac Paramedic Service, Halton Emergency Medical Services, Harrow Ambulance Service Ltd., Kawartha Lakes Emergency Medical Services, Kawartha Lakes Fire and Rescue, Kingston Fire and Rescue, Kitchener Fire Dept., Lambton County Emergency Medical Services, Lasalle Fire Dept., London Fire Dept., Niagara Emergency Medical Services, Niagara Falls Fire and Rescue, Northumberland Emergency Medical Service, Oakville Fire Dept., Ottawa Fire and Rescue, Ottawa Paramedic Service, Peterborough Emergency Medical System, Peterborough Fire Dept., Prescott-Russell Emergency Medical Services, Sarnia Fire Services, St. Catharine’s Fire and Rescue, Sudbury Emergency Medical Services, Sudbury Fire and Rescue, SunParlour Emergency Services Inc., Superior North Emergency Medical Services, Tecumseh Fire Dept., Thames Emergency Medical Services, Thunder Bay Fire and Rescue, Waterloo Fire and Rescue, Waterloo Regional Emergency Medical Services, Welland Fire and Rescue, Windsor Fire and Rescue, British Columbia Ambulance Service, Abbotsford Fire Dept., Aggassiz Valley Fire Dept., Burnaby Fire Dept., Campbell River Fire Dept., Central Saanich Fire Dept., City of North Vancouver Fire Dept., Coquitlam Fire Dept., Delta Fire Dept., Esquimalt Fire Dept., Kamloops Fire Dept., Kelowna Fire Dept., Lake Country V Fire Dept., Langford Fire Dept., Langley City Fire Dept., Langley Township Fire Dept., Maple Ridge Fire Dept., Mission Fire Dept., Nanaimo Fire Dept., New Westminster Fire Dept., North Vancouver District Fire Dept., Oak Bay Fire Dept., Peachland Valley Fire Dept., Pitt Meadows Fire Dept., Port Coquitlam Fire Rescue, Port Moody Fire Dept., Prince George Fire Dept., Prince Rupert Fire Dept., Qualicum Beach Fire Dept., Richmond Fire Dept., Saanich Fire Dept., Sooke V Fire Dept., Squamish Fire Dept., Surrey Fire Dept., Trail Fire Dept., Vancouver Fire Dept., Victoria Fire Dept., West Vancouver Fire Dept., Whistler Fire Dept., White Rock Fire Dept.
Pittsburgh Resuscitation Network, the University of Pittsburgh, Pittsburgh, PA: Clifton Callaway, MD, PhD, Principal Investigator
Core Investigators: Samuel Tisherman, MD, Jon Rittenberger, MD, David Hostler, PhD
Coordinators: Joseph Condle, Mitch Kampmeyer, Timothy Markham, Maureen Morgan
EMS Investigators/Collaborators: Paul Sabol, Gina Sicchitano, Scott Sherry, Anthony Shrader, Greg Stull, Manuel Torres, MS, William Groft, Robert McCaughan, Rodney Rohrer, John Cole, MD, David Fuchs, MD, Francis Guyette, MD, MS, William Jenkins, MD, Ronald Roth, MD, Heather Walker, MD
Hospital Investigators/Collaborators: Alain Corcos, MD, Ankur Doshi, MD, Adrian Ong, MD, Andrew Peitzman, MD
Participating EMS Agencies: Washington Ambulance and Chair, Pittsburgh Bureau of Emergency Medical Services, Pittsburgh Bureau of Fire, Mutual Aid Ambulance Service, STAT Medevac
Portland Resuscitation Outcomes Consortium, Oregon Health and Science University, Portland, OR: Jerris R. Hedges, MD, MS, Principal Investigator
Core Investigators: Craig D. Newgard, MD, MPH, Mohamud R. Daya, MD, MS, Robert A. Lowe, MD, MPH
Coordinators: Denise Griffiths, BS, John Brett, EMT-P, Dana Zive, MPH, Abdolaziz Yekrang, MPA, MA, Yoko Nakamura, MD, Brooke Frakes, BS, Aaron Monnig, EMT-P
EMS Investigators/Collaborators: Jonathan Jui, MD, MPH, Terri A. Schmidt, MD, MS, Ritu Sahni, MD, Craig R. Warden, MD, MPH, Marc D. Muhr, EMT-P2, John A. Stouffer, EMT-P, Kyle Gorman, MBA, EMT-P, Pontine Rosteck EMT-P, Karl Koenig EMT-P, Jan Lee EMT-P, Roxy Barnes EMT-P, Heather Tucker, EMT-P, Brad Allen, EMT-P, TJ Bishop, EMT-P, Adam Glaser, EMT-P
Hospital Investigators/Collaborators: Martin A. Schreiber, MD, Jim Anderson, MD, Ameen I. Ramzy, MD, K. Dean Gubler, DO, Lynn K. Wittwer, MD, Samantha Underwood, MS, Brooke Barone, BS, Denise Haun-Taylor, RN, Elizabeth Bryant, RN, Joanne Miller, ARNP
Participating EMS Agencies: American Medical Response - Clackamas, Clark, and Multnomah Counties, Camas Fire Dept., Clackamas County Fire District #1, Clark County Fire District #6, Lake Oswego Fire Dept., Life-Flight, MetroWest Ambulance, North Country Ambulance, Tualatin Valley Fire and Rescue, Vancouver Fire Department, Portland Fire and Rescue, Portland International Airport Fire Department, Gresham Fire and Emergency Services
UCSD-San Diego Resuscitation Research Center, University of California at San Diego, San Diego, CA: Daniel Davis, MD, Principal Investigator
Core Investigators: David Hoyt, MD, Raul Coimbra, MD, PhD, Gary Vilke, MD
Coordinators: Donna Kelly, RN, Lana McCallum-Brown, RN
EMS Investigators/Collaborators: Bruce Haynes, MD, Brad Schwartz, MD
Hospital Investigators/Collaborators: Michael Sise, MD, Frank Kennedy, MD, Fred Simon, MD, Gail Tominaga, MD, John Steele, MD
Participating EMS Agencies: Alpine Fire Protection District, American Medical Response, Barona Fire Dept., Bonita/Sunnyside Fire Protection, Borrego Springs Fire Protection District, Carlsbad Fire Dept., Chula Vista Fire Dept., Coronado Fire Dept., CSA-17 ALS Transporting Agency, Deer Springs, Del Mar Fire Dept., East County Fire Protection District, El Cajon Fire Dept., Elfin Forest CSA 107, Encinitas Fire Protection District, Escondido Fire Dept., Federal Fire Dept. San Diego, Imperial Beach Fire Dept., Julian-Cuyamaca Fire Dept., La Mesa Fire Dept., Lakeside Fire Protection District, Lemon Grove Fire Dept., Mercy Air, Miramar Fire Dept., National City Fire Dept., North County Fire, Oceanside Fire Dept., Pala Fire Dept., Poway Fire Dept., Ramona Fire Dept., Rancho Santa Fe Fire Protection District, San Diego Rural Fire Protection District, San Marcos Fire Dept., San Miguel Fire Protection District, Santee Fire Dept., Solana Beach Fire Dept., Sycuan Fire Dept., Valley Center/Mercy Ambulance, Viejas Fire Dept., Vista Fire Dept.
Seattle-King County Center for Resuscitation Research at the University of Washington, University of Washington, Seattle, WA: Peter J. Kudenchuk, MD, Principal Investigator
Core Investigators: Tom D. Rea, MD, Eileen Bulger, MD, Mickey S. Eisenberg, MD, Michael Copass, MD
Coordinators: Michele Olsufka, RN, Sally Ragsdale, ARNP, Debi Solberg, RN, MN, Susan Damon, RN, Randi Phelps, Jeanne O’Brien, RN, MN
EMS Investigators/Collaborators: Earl Sodeman, Marty LaFave, James Boehl, Dave Jones, Gary Somers, Deborah Ayrs, Adrian Whorton, Sam Warren, Jim Fogarty, Jonathan Larsen, Mike Helbock
Participating EMS Agencies: Bellevue Fire Dept., Redmond Fire Dept., Seattle Fire Dept., Shoreline Fire Dept., King Co Medic 1, Vashon Island Medic One, Bothell Fire Dept., Burien Fire Dept., Kirkland Fire Dept., Renton Fire Dept., Snoqualmie Fire Dept., Duvall Fire Dept., Eastside Fire and Rescue, Enumclaw Fire Dept., Fall City Fire Dept., Skyway Fire Dept., Kent Fire Dept., Maple Valley Fire and Life Safety, Mercer Island Fire Dept., King County Fire District #44, North Highline Fire Dept., Northshore/Kenmore Fire Dept., Port of Seattle Fire Dept., King County Fire District #47, King County Fire District #40, SeaTac Fire Dept., Skykomish Fire Dept., Snoqualmie Pass, South King Co Medic 1, South King Fire and Rescue, Tukwila Fire Dept., Valley Regional Fire Authority, Vashon Island Fire and Rescue, Woodinville Fire Dept.
Toronto Regional Resuscitation Research Out of Hospital Network (Toronto Regional RESCUeNET), University of Toronto, Toronto, Ontario, Canada: Arthur Slutsky, Principal Investigator
Core Investigators: Laurie Morrison, Paul Dorian
Coordinators: Craig Beers, Blair Bigham, Dina Braga, Grace Burgess, Bruce Cameron, Suzanne Chung, Pete De Maio, Steve Driscoll, Lynne Fell, Jamie Frank, Mark McLennan, Lesley Ann Molyneaux, Welson Ryan, Angela Schotsman, Jacob Simonini, Lynda Turcotte, Flo Veel, Amy Wassenaar, Cathy Zahn
EMS Investigators/Collaborators: Dana Bradshaw, Rob Burgess, Bruce Cameron, Sandra Chad, Sheldon Cheskes, Allan Craig, Steve Dewar, Tim Dodd, Rob Duquette, Marty Epp, Michael Feldman, Verena Jones, Russell MacDonald, Larry MacKay, Steve McNenley, Judy Moore, Philip Moran, Michael Murray, Michael Nemeth, Russ Olnyk, Tyrone Perreira, Richard Renaud, Karen Roche, Jennifer Shield, Doug Silver, Jacob Stevens, Rick Verbeek, Tim Waite, Ken Webb, Michelle Wels-ford
Hospital Investigators/Collaborators: Rosemarie Farrell, Jamie Hutchison
Participating EMS Agencies: Ajax Fire and Emergency Services, Barrie Fire and Emergency Service, Beausoleil First Nation Emergency Medical Services, Bradford West Gwillimbury Fire and Emergency Services, Brampton Fire and Emergency Services, Brock Township Fire Dept., Caledon Fire and Emergency Services, City of Hamilton Emergency Services – EMS, City of Hamilton Emergency Services – Fire, City of Orillia Fire Dept., Clarington Emergency and Fire Services, County of Simcoe Paramedic Services, Durham Regional Emergency Medical Services, Innisfil Fire and Rescue Service, Mississauga Fire and Emergency Services, Mnjikaning Fire Rescue Service, Muskoka Ambulance Service, Muskoka Ambulance Communication Center, New Tecumseth Fire Dept., OrngeTransport Medicine, Oro Medonte Fire and Emergency Services, Oshawa Fire Services, Pickering Fire Services, The Ramara Township Fire and Rescue Service, Peel Regional Paramedic Services, Toronto EMS, Toronto Fire Services, Township of Essa Fire Dept., Township of Georgian Bay Fire Dept., Township of Scugog Fire Dept., Township of Uxbridge Fire Dept., Wasaga Beach Fire Dept., Whitby Fire and Emergency Services, Durham Regional Basehospital, Sunnybrook Osler Center for Prehospital Care, Hamilton Health Sciences Paramedic Base Hospital Program, Simcoe Muskoka Basehospital
Steering Committee Chair, Myron Weisfeldt, MD, Johns Hopkins University School of Medicine, Baltimore, MD, Co-Chair-Cardiac, Joseph P. Ornato, MD, Virginia Commonwealth University Health System, Richmond, VA, Co-Chair-Trauma, David B. Hoyt, MD, University of California at San Diego, San Diego, CA, replacing Col. John B. Holcomb, MD, Commander, U.S. Army ISR
National Heart, Lung, and Blood Institute, Bethesda, MD: Tracey Hoke, MD, George Sopko, MD, MPH, David Lathrop, PhD, Alice Mascette, MD, Patrice Desvigne Nickens, MD
Clinical Trial Center, University of Washington, Seattle, WA: Al Hallstrom, PhD, Graham Nichol, MD, MPH, Scott Emerson, MD, PhD, Judy Powell, BSN, Gena Sears, BSN, Berit Bardarson, RN, Lois Van Ottingham, BSN, Anna Leonen, MS, Robert B. Ledingham, MS, Chris Finley, Richard Moore, BS, Ben Bergsten-Buret
Footnotes
Presented as an abstract at the Society for Academic Emergency Medicine Annual Meeting, May 2008, Washington, DC.
Reprints not available from the authors.
Contributor Information
Craig D. Newgard, Center for Policy and Research in Emergency Medicine, Department of Emergency Medicine, Oregon Health & Science University, Portland, OR.
Robert H. Schmicker, Department of Biostatistics, University of Washington Clinical Trial Center, University of Washington, Seattle, WA.
Jerris R. Hedges, Department of Medicine, John A. Burns School of Medicine, University of Hawaii–Manoa, Honolulu, HI.
John P. Trickett, Department of Emergency Medicine, University of Ottawa, Ottawa, Ontario, Canada.
Daniel P. Davis, Department of Emergency Medicine, University of California at San Diego, San Diego, CA.
Eileen M. Bulger, Department of Surgery, University of Washington Clinical Trial Center, University of Washington, Seattle, WA.
Tom P. Aufderheide, Department of Emergency Medicine, Medical College of Wisconsin, Milwaukee, WI.
Joseph P. Minei, Department of Surgery, University of Texas Southwestern Medical Center, Dallas, TX.
J. Steven Hata, Department of Anesthesia, Division of Critical Care, University of Iowa, Iowa City, IA.
K. Dean Gubler, Legacy Emanuel Trauma Program, Portland, OR.
Todd B. Brown, Department of Emergency Medicine, University of Alabama at Birmingham, Birmingham, AL.
Jean-Denis Yelle, Department of Surgery , University of Ottawa, Ottawa, Ontario, Canada.
Berit Bardarson, Department of Biostatistics, University of Washington Clinical Trial Center, University of Washington, Seattle, WA.
Graham Nichol, Department of Biostatistics, University of Washington–Harborview Center for Prehospital Emergency Care, University of Washington, Seattle, WA.
REFERENCES
- 1.Lerner EB, Moscati RM. The golden hour: scientific fact or medical “urban legend”? Acad Emerg Med. 2001;8:758–760. doi: 10.1111/j.1553-2712.2001.tb00201.x. [DOI] [PubMed] [Google Scholar]
- 2.Sampalis JS, Denis R, Lavoie A, et al. Trauma care regionalization: a process-outcome evaluation. J Trauma. 1999;46:565–581. doi: 10.1097/00005373-199904000-00004. [DOI] [PubMed] [Google Scholar]
- 3.Samplais JS, Lavoie A, Williams JI, et al. Impact of on-site care, prehospital time, and level of in-hospital care on survival in severely injured patients. J Trauma. 1993;34:252–261. doi: 10.1097/00005373-199302000-00014. [DOI] [PubMed] [Google Scholar]
- 4.Stiell IG, Nesbitt LP, Pickett W, et al. The OPALS major trauma outcome study: impact of advanced life-support on survival and morbidity. CMAJ. 2008;178:1141–1152. doi: 10.1503/cmaj.071154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pepe PE, Wyatt CH, Bickell WH, et al. The relationship between total prehospital time and outcome in hypotensive victims of penetrating injuries. Ann Emerg Med. 1987;16:293–297. doi: 10.1016/s0196-0644(87)80174-9. [DOI] [PubMed] [Google Scholar]
- 6.Petri RW, Dyer A, Lumpkin J. The effect of prehospital transport time on the mortality from traumatic injury. Prehosp Disaster Med. 1995;10:24–29. doi: 10.1017/s1049023x00041625. [DOI] [PubMed] [Google Scholar]
- 7.Lerner EB, Billittier AJ, Dorn JM, et al. Is total out-of-hospital time a significant predictor of trauma patient mortality? Acad Emerg Med. 2003;10:949–954. doi: 10.1111/j.1553-2712.2003.tb00650.x. [DOI] [PubMed] [Google Scholar]
- 8.Pons PT, Markovchick VJ. Eight minutes or less: does the ambulance response time guideline impact trauma patient outcome? J Emerg Med. 2002;23:43–48. doi: 10.1016/s0736-4679(02)00460-2. [DOI] [PubMed] [Google Scholar]
- 9.Di Bartolomeo S, Valent F, Rosolen V, et al. Are pre-hospital time and emergency department disposition time useful process indicators for trauma care in Italy? Injury. 2007;38:305–311. doi: 10.1016/j.injury.2006.10.005. [DOI] [PubMed] [Google Scholar]
- 10.Osterwalder JJ. Can the “golden hour of shock” safely be extended in blunt polytrauma patients? Prehosp Disaster Med. 2002;17:75–80. doi: 10.1017/s1049023x00000212. [DOI] [PubMed] [Google Scholar]
- 11.Feero S, Hedges JR, Simmons E, et al. Does out-of-hospital EMS time affect trauma survival? Am J Emerg Med. 1995;13:133–135. doi: 10.1016/0735-6757(95)90078-0. [DOI] [PubMed] [Google Scholar]
- 12.Gervin AS, Fischer RP. The importance of prompt transport in salvage of patients with penetrating heart wounds. J Trauma. 1982;22:443–446. doi: 10.1097/00005373-198206000-00001. [DOI] [PubMed] [Google Scholar]
- 13.Ivatury RR, Nallathambi MN, Roberge RJ, et al. Penetrating thoracic injuries: in-field stabilization versus prompt transport. J Trauma. 1987;27:1066–1072. [PubMed] [Google Scholar]
- 14.Clevenger FW, Yarborough DR, Reines HD. Resuscitative thoracotomy: the effect of field time on outcome. J Trauma. 1988;28:441–445. doi: 10.1097/00005373-198804000-00004. [DOI] [PubMed] [Google Scholar]
- 15.Grossman DC, Kim A, MacDonald SC, et al. Urban-rural differences in prehospital care of major trauma. J Trauma. 1997;42:723–729. doi: 10.1097/00005373-199704000-00024. [DOI] [PubMed] [Google Scholar]
- 16.Pons PT, Haukoos JS, Bludworth W, et al. Paramedic response time: does is affect patient survival? Acad Emerg Med. 2005;12:594–600. doi: 10.1197/j.aem.2005.02.013. [DOI] [PubMed] [Google Scholar]
- 17.Blackwell TH, Kaufman JS. Response time effectiveness: comparison of response time and survival in an urban EMS system. Acad Emerg Med. 2002;9:288–295. doi: 10.1111/j.1553-2712.2002.tb01321.x. [DOI] [PubMed] [Google Scholar]
- 18.Eisenberg MS, Bergner L, Hallstrom A. Cardiac resuscitation in the community: importance of rapid provision and implications for program planning. JAMA. 1979;241:1905–1907. doi: 10.1001/jama.241.18.1905. [DOI] [PubMed] [Google Scholar]
- 19.De Maio VJ, Stiell IG, Wells GA, et al. Optimal defibrillation response intervals for maximum out-of-hospital cardiac arrest survival rates. Ann Emerg Med. 2003;42:242–250. doi: 10.1067/mem.2003.266. [DOI] [PubMed] [Google Scholar]
- 20.Ambulance crash-related injuries among emergency medical services workers—Unites States, 1991-2002. MMWR Morb Mortal Wkly Rep. 2003;52:154–156. [PubMed] [Google Scholar]
- 21.Kahn CA, Pirrallo RG, Kuhn EM. Characteristics of fatal ambulance crashes in the United States: an 11-year retrospective analysis. Prehosp Emerg Care. 2001;5:261–269. doi: 10.1080/10903120190939751. [DOI] [PubMed] [Google Scholar]
- 22.Becker LR, Zaloshnja E, Levick N, et al. Relative risk of injury and death in ambulances and other emergency vehicles. Accid Anal Prev. 2003;35:941–948. doi: 10.1016/s0001-4575(02)00102-1. [DOI] [PubMed] [Google Scholar]
- 23.Newgard CD, Sears GK, Rea TD, et al. The Resuscitation Outcomes Consortium Epistry-Trauma: design, development, and implementation of a North American epidemiologic out-of-hospital trauma registry. Resuscitation. 2008;78:170–178. doi: 10.1016/j.resuscitation.2008.01.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Davis DP, Garberson LA, Andrusiekc D, et al. A descriptive analysis of emergency medical service systems participating in a large, out-of-hospital resuscitation research network. Prehosp Emerg Care. 2007;11:369–382. doi: 10.1080/10903120701537147. [DOI] [PubMed] [Google Scholar]
- 25.Committee on Trauma . Resources for Optimal Care of the Injured Patient. American College of Surgeons; Chicago, IL: 2006. [Google Scholar]
- 26.Cottington EM, Young JC, Shufflebarger CM, et al. The utility of physiologic status, injury site, and injury mechanism in identifying patients with major trauma. J Trauma. 1988;28:305–311. doi: 10.1097/00005373-198803000-00005. [DOI] [PubMed] [Google Scholar]
- 27.Esposito TJ, Offner PJ, Jurkovich GJ, et al. Do prehospital trauma center triage criteria identify major trauma victims? Arch Surg. 1995;130:171–176. doi: 10.1001/archsurg.1995.01430020061010. [DOI] [PubMed] [Google Scholar]
- 28.Kane G, Engelhardt R, Celentano J, et al. Empirical development and evaluation of out of hospital trauma triage instruments. J Trauma. 1985;25:482–489. doi: 10.1097/00005373-198506000-00002. [DOI] [PubMed] [Google Scholar]
- 29.Norcross ED, Ford DW, Cooper ME, et al. Application of American College of Surgeons’ field triage guidelines by pre-hospital personnel. J Am Coll Surg. 1995;181:539–544. [PubMed] [Google Scholar]
- 30.Henry MC, Hollander JE, Alicandro JM, et al. Incremental benefit of individual American College of Surgeons trauma triage criteria. Acad Emerg Med. 1996;3:992–1000. doi: 10.1111/j.1553-2712.1996.tb03340.x. [DOI] [PubMed] [Google Scholar]
- 31.Hannan EL, Farrell LS, Cooper A, et al. Physiologic trauma triage criteria in adult trauma patients: are they effective in saving lives by transporting patients to trauma centers? J Am Coll Surg. 2005;200:584–592. doi: 10.1016/j.jamcollsurg.2004.12.016. [DOI] [PubMed] [Google Scholar]
- 32.Baxt WG, Jones G, Fortlage D. The Trauma Triage Rule: a new, resource-based approach to the out-of-hospital identification of major trauma victims. Ann Emerg Med. 1990;19:1401–1406. doi: 10.1016/s0196-0644(05)82608-3. [DOI] [PubMed] [Google Scholar]
- 33.Zechnich AD, Hedges JR, Spackman K, et al. Applying the trauma triage rule to blunt trauma patients. Acad Emerg Med. 1995;2:1043–1052. doi: 10.1111/j.1553-2712.1995.tb03148.x. [DOI] [PubMed] [Google Scholar]
- 34.Lerner EB. Studies evaluating current field triage: 1966-2005. Prehosp Emerg Care. 2006;10:303–306. doi: 10.1080/10903120600723921. [DOI] [PubMed] [Google Scholar]
- 35.MacKenzie EJ, Rivara FP, Jurkovich GJ, et al. A national evaluation of the effect of trauma-center care on mortality. N Engl J Med. 2006;354:366–378. doi: 10.1056/NEJMsa052049. [DOI] [PubMed] [Google Scholar]
- 36.Spaite DW, Valenzuela TD, Meislin HW, et al. Prospective validation of a new model for evaluating emergency medical services systems by in-field observation of specific time intervals in prehospital care. Ann Emerg Med. 1993;22:638–645. doi: 10.1016/s0196-0644(05)81840-2. [DOI] [PubMed] [Google Scholar]
- 37.Martens EP, Pestman WR, de Boer A, et al. Instrumental variables applications and limitations. Epidemiology. 2006;17:260–267. doi: 10.1097/01.ede.0000215160.88317.cb. [DOI] [PubMed] [Google Scholar]
- 38.McClellan M, McNeil BJ, Newhouse JP. Does more intensive treatment of acute myocardial infarction in the elderly reduce mortality? JAMA. 1994;272:859–866. [PubMed] [Google Scholar]
- 39.Stock JH, Wright JH, Yogo M. A survey of weak instruments and weak identification in generalized methods of moments. 2002. J Business Econ Stat. 2002;20:518–529. [Google Scholar]
- 40.Pracht EE, Tepas JJ, Celso BG, et al. Survival advantage associated with treatment of injury at designated trauma centers: a bivariate probit model with instrumental variables. Med Care Res Rev. 2007;64:83–97. doi: 10.1177/1077558706296241. [DOI] [PubMed] [Google Scholar]
- 41.McConnell J, Newgard CD, Mullins RJ, et al. Mortality benefit of transfer to level I versus level II trauma centers for head-injured patients: analysis using instrumental variables. Health Serv Res. 2005;40:435–457. doi: 10.1111/j.1475-6773.2005.00366.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wears RL. Advanced statistics: statistical methods for analyzing cluster and cluster-randomized data. Acad Emerg Med. 2002;9:330–341. doi: 10.1111/j.1553-2712.2002.tb01332.x. [DOI] [PubMed] [Google Scholar]
- 43.Brasel KJ, Bulger E, Cook AJ, et al. Hypertonic resuscitation: design and implementation of a prehospital intervention trial. J Am Coll Surg. 2008;206:220–232. doi: 10.1016/j.jamcollsurg.2007.07.020. [DOI] [PubMed] [Google Scholar]
- 44.Spaite DW, Tse DJ, Valenzuela TD, et al. The impact of injury severity and prehospital procedures on scene time in victims of major trauma. Ann Emerg Med. 1991;20:1299–1305. doi: 10.1016/s0196-0644(05)81070-4. [DOI] [PubMed] [Google Scholar]
- 45.Carr BG, Caplan JM, Pryor JP, et al. A meta-analysis of prehospital care times for trauma. Prehosp Emerg Care. 2006;10:198–206. doi: 10.1080/10903120500541324. [DOI] [PubMed] [Google Scholar]
- 46.Mullins RJ, Veum-Stone J, Helfand M, et al. Outcome of hospitalized injured patients after institution of a trauma system in an urban area. JAMA. 1994;271:1919–1924. doi: 10.1001/jama.1994.03510480043032. [DOI] [PubMed] [Google Scholar]
- 47.Mullins RJ, Veum-Stone J, Hedges JR, et al. Influence of a statewide trauma system on location of hospitalization and outcome of injured patients. J Trauma. 1996;40:536–545. doi: 10.1097/00005373-199604000-00004. [DOI] [PubMed] [Google Scholar]
- 48.Mullins RJ, Mann NC, Hedges JR, et al. Preferential benefit of implementation of a statewide trauma system in one of two adjacent states. J Trauma. 1998;44:609–617. doi: 10.1097/00005373-199804000-00009. [DOI] [PubMed] [Google Scholar]
- 49.Demetriades D, Martin M, Salim A, et al. The effect of trauma center designation and trauma volume on outcome in specific severe injuries. Ann Surg. 2005;242:512–519. doi: 10.1097/01.sla.0000184169.73614.09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Liberman M, Mulder D, Samplais J. Advanced or basic life support for trauma: meta-analysis and critical review of the literature. J Trauma. 2000;49:584–599. doi: 10.1097/00005373-200010000-00003. [DOI] [PubMed] [Google Scholar]
- 51.Bickell WH, Wall MJ, Pepe PE, et al. Immediate versus delayed fluid resuscitation for hypotensive patients with penetrating torso injuries. N Engl J Med. 1994;331:1105–1109. doi: 10.1056/NEJM199410273311701. [DOI] [PubMed] [Google Scholar]
- 52.Wang HE, Peitzman AB, Cassidy LD, et al. Out-of-hospital endotracheal intubation and outcome after traumatic brain injury. Ann Emerg Med. 2004;44:439–450. doi: 10.1016/j.annemergmed.2004.04.008. [DOI] [PubMed] [Google Scholar]
- 53.Davis DP, Hoyt DB, Ochs M, et al. The effect of paramedic rapid sequence intubation on outcome in patients with severe traumatic brain injury. J Trauma. 2003;54:444–453. doi: 10.1097/01.TA.0000053396.02126.CD. [DOI] [PubMed] [Google Scholar]
- 54.Wang HE, Yealy DM. Out-of-hospital endotracheal intubation: where are we? Ann Emerg Med. 2006;47:532–541. doi: 10.1016/j.annemergmed.2006.01.016. [DOI] [PubMed] [Google Scholar]
- 55.Birk HO, Henriksen LO. Prehospital interventions: on-scene time and ambulance technicians’ experience. Prehosp Disaster Med. 2002;17:167–169. doi: 10.1017/s1049023x00000406. [DOI] [PubMed] [Google Scholar]
- 56.Cudnik M, Newgard CD, Wang H, et al. Endotracheal intubation increases out of hospital time in trauma patients. Prehosp Emerg Care. 2007;11:224–229. doi: 10.1080/10903120701205208. [DOI] [PubMed] [Google Scholar]
- 57.Sloan EP, Callahan EP, Duda J, et al. The effect of urban trauma system hospital bypass on prehospital transport times and level 1 trauma patient survival. Ann Emerg Med. 1989;18:1146–1150. doi: 10.1016/s0196-0644(89)80049-6. [DOI] [PubMed] [Google Scholar]
- 58.Wang HE, Faibanks RJ, Shah MN, et al. Tort claims and adverse events in emergency medical services. Ann Emerg Med. 2008;52:256–262. doi: 10.1016/j.annemergmed.2008.02.011. [DOI] [PubMed] [Google Scholar]


