Abstract
Objectives
The purpose of this study was to assess the effectiveness of contemporary automatic external defibrillator (AED) use.
Background
In the PAD (Public Access Defibrillation) trial, survival was doubled by focused training of lay volunteers to use an AED in high-risk public settings.
Methods
We performed a population-based cohort study of persons with nontraumatic out-of-hospital cardiac arrest before emergency medical system (EMS) arrival at Resuscitation Outcomes Consortium (ROC) sites between December 2005 and May 2007. Multiple logistic regression was used to assess the independent association between AED application and survival to hospital discharge.
Results
Of 13,769 out-of-hospital cardiac arrests, 4,403 (32.0%) received bystander cardiopulmonary resuscitation but had no AED applied before EMS arrival, and 289 (2.1%) had an AED applied before EMS arrival. The AED was applied by health care workers (32%), lay volunteers (35%), police (26%), or unknown (7%). Overall survival to hospital discharge was 7%. Survival was 9% (382 of 4,403) with bystander cardiopulmonary resuscitation but no AED, 24% (69 of 289) with AED application, and 38% (64 of 170) with AED shock delivered. In multivariable analyses adjusting for: 1) age and sex; 2) bystander cardiopulmonary resuscitation performed; 3) location of arrest (public or private); 4) EMS response interval; 5) arrest witnessed; 6) initial shockable or not shockable rhythm; and 7) study site, AED application was associated with greater likelihood of survival (odds ratio: 1.75; 95% confidence interval: 1.23 to 2.50; p < 0.002). Extrapolating this greater survival from the ROC EMS population base (21 million) to the population of the U.S. and Canada (330 million), AED application by bystanders seems to save 474 lives/year.
Conclusions
Application of an AED in communities is associated with nearly a doubling of survival after out-of-hospital cardiac arrest. These results reinforce the importance of strategically expanding community-based AED programs.
Keywords: automatic external defibrillator, cardiac arrest, cardiopulmonary resuscitation, defibrillation, resuscitation
Currently more than 200,000 automated external defibrillators (AEDs) are sold yearly for public use in the U.S. (1). This expenditure totals approximately $500 million per year in equipment and training. Anecdotal reports document a high rate of survival after out-of-hospital cardiac arrest (OHCA) when trained persons with a job-related duty to respond use AEDs (2– 4) or where health care professionals are in high concentration (5). This question was studied by the large, community-based, randomized PAD (Public Access Defibrillation) trial-trained volunteers (6,7) at both control and AED sites and showed a doubling the number of survivors (30 vs. 15; relative risk: 2.0; 95% confidence interval [CI]: 1.07 to 3.77; p = 0.03) at sites with AEDs compared with sites without AEDs.
There is little information about the clinical or public health impact of the ongoing investment in AEDs and training for the public at large. Several before-and-after comparisons of survival after implementation of PAD programs using AEDs showed favorable results (8 –11), whereas others did not (12–14). These inconsistent findings have challenged the value of AED implementation as a community strategy to improve survival after cardiac arrest (15–23). In a randomized trial of private AED placement in homes of patients who have undergone myocardial infarction (24), survival was not improved in patients whose home was equipped with an AED and a family member trained to use an AED compared with patients with cardiopulmonary resuscitation (CPR) training and no AED.
In recent years, emergency medical services (EMS) recordings of initial cardiac arrest rhythms show a striking decline in the incidence of ventricular tachycardia (VT) or ventricular fibrillation (VF) that may benefit from AED use. Initial VT/VF rhythms accounted for 70% to 80% of cardiac arrests 20 years ago (25), but now constitute only 10% to 30% of arrests (8,25,26). Non-VT/VF arrests (asystole and pulseless electrical rhythms) do not benefit from AEDs, and furthermore, their use may delay life-saving measures such as bystander CPR in such patients.
Although an in-hospital registry of cardiac arrest and resuscitation exists in the U.S. (27), there have been no large registries of the out-of-hospital experience to assess the value of bystander AED. The Resuscitation Outcomes Consortium (ROC) (28) established a population-based registry for OHCA and resuscitation called the ROC Epistry Cardiac Arrest registry (26,29). In this report, we use this registry to test the hypothesis that despite the decreasing frequency of VT/VF as an initial rhythm and despite possible delays or errors associated with AED application, cardiac arrest patients who have an AED applied before EMS arrival experience better survival than those without an AED applied.
Methods
Design and setting
The ROC Epistry Cardiac Arrest registry is a prospective, multicenter, multiregional, population-based international cohort study of nontramatic OHCA (28,29). We report on patients treated by 1 or more of 215 ROC EMS agencies in 7 U.S. sites (Alabama, Dallas, Iowa, Milwaukee, Pittsburgh, Portland, and Seattle-King County) and 3 Canadian sites (Ottawa-OPALS, Toronto, and British Columbia) between December 1, 2005, and April 30, 2007 (26). One ROC site, San Diego, did not participate and was omitted from this analysis (see Figure 1 for a map of the sites).
Figure 1. Map of Sites Contributing to the Resuscitation Outcomes Consortium Epistry Database.

San Diego was excluded from this analysis because of a lack of data. OPALS/B.C. = Ontario Prehospital Advanced Life Support/British Columbia; UWCTC = University of Washington Clinical Trials Center.
The ROC sites obtained institutional review board approval to conduct this research with a waiver of written consent under minimal risk criteria. The ROC Epistry Cardiac Arrest registry was approved by the Institutional Review Board of the University of Washington (Data Coordinating Center), 100 U.S. institutional review boards, and 34 Canadian research ethics boards.
Inclusion and exclusion criteria
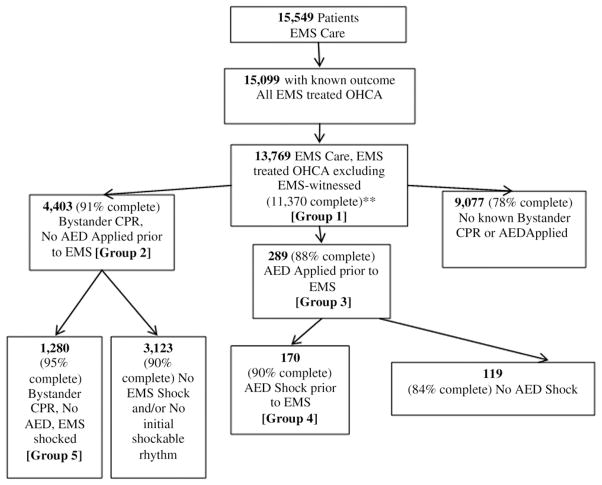
The current study included persons with nontraumatic OHCA regardless of the cause that occurred before EMS arrival who received attempts at external defibrillation (by lay responders or emergency personnel) or chest compressions by organized EMS personnel. We excluded both EMS-witnessed arrests because an AED would not be applied before EMS arrival in this group and arrests that occurred in healthcare facilities, because the intent in the current study was to evaluate whether randomized trial results from the PAD trial would translate broadly to a heterogeneous set of communities (Fig. 2). We also excluded persons if resuscitation was not attempted, for example, because the person had “do not resuscitate” status, terminal illness, or evidence of prolonged death such as rigor mortis. Finally, we excluded those subjects enrolled in the concurrent ROC CPR Feedback trial (n = 160) because those results have not yet been reported and more recent large scale trials (30,31).
Figure 2. Flow Chart of Patients by Group and Percent With Complete Data for the Logistic Regression Model.
Patients who arrested in a health care facility were excluded. **Complete cases were those with known data for all variables used in the multivariate analysis. AED = automatic external defibrillator; CPR = cardiopulmonary resuscitation; EMS = emergency medical services; OHCA = out-of-hospital cardiac arrest.
Data definitions
Details of data definitions, data collection, and quality assessment methods have been published previously (29). Information about each OHCA was collected using a uniform set of data definitions developed by the ROC investigators and derived from the Utstein data elements. The data elements included information about patient demographics, arrest circumstances, characteristics of care, and survival status. AED application before EMS arrival was defined as AED application (with or without delivery of a shock) by a person outside the EMS, whereas AED shock defined the subgroup in which the AED was applied before EMS arrival and delivered a shock. Shockable first rhythm was defined as either shock on application of AED by a bystander before EMS arrival or a first rhythm of VF/VT recorded by EMS. EMS response time was defined as the time from 911 call received at EMS dispatch to the first EMS vehicle arrival at the scene. Public location was defined as a street or highway, public building, place of recreation, industrial place, or other public property. Non-public location was defined to include a home residence, farm or ranch, residential institution, or other private property. Health care facilities, which include hospitals, medical clinics, and other healthcare institutions, but do not include nursing homes, were excluded from this analysis. The primary outcome was survival to hospital discharge as determined from available records (usually hospital records).
Data analysis
Statistical analyses were conducted using R software, version 2.1.1 (R Foundation for Statistical Computing, Vienna, Austria). All tests were 2-sided with a significance level of 0.05.
Analyses determined the association between survival and AED application before EMS arrival. We focused on AED application because this application would reflect both the potential favorable effects of early shock on survival and the unfavorable effects of possible delay in performing CPR or calling EMS because of an AED search and application. Because no single clinical group provides the ideal comparison, we stratified the data according to whether CPR was performed before EMS arrival and initial rhythm characteristics in descriptive analyses. We present arrest and outcome characteristics for non–EMS-witnessed subjects as 7 groups (Fig. 2, Table 1): Group 1, All EMS care, no EMS witnessed; Group 2, bystander CPR, no AED applied before EMS arrival; Group 3, AED application before EMS arrival; Group 4, AED application and AED shock before EMS arrival (subset of Group 3); Group 5, bystander CPR before EMS arrival, no AED application, and a shock delivered by EMS upon initial assessment (subset of Group 2); Group 6, public location arrests and Group 7, bystander-witnessed arrests (subset of Group 2).
Table 1.
Characterization of All EMS-Treated Victims and Various Subgroups of Interest
| Group 1: EMS-Treated OHCA, Excluding EMS Witnessed | Group 2: Bystander CPR, No AED Applied Before EMS | Group 3: AED Applied Before EMS | Group 4: AED Shock Before EMS | Group 5: Bystander CPR, No AED, EMS Shocked | Group 6: Public Location Only | Group 7: Bystander Witnessed Only | |
|---|---|---|---|---|---|---|---|
| n | 13,769 | 4,403 | 289 | 170 | 1,280 | 2,193 | 5,630 |
| Median age, yrs | 67 (26) | 65 (27) | 62 (24) | 60 (20) | 63 (22) | 60 (21) | 68 (24) |
| Gender | |||||||
| Male | 8,826 (64%) | 2,838 (64%) | 212 (73%) | 141 (83%) | 987 (77%) | 1,814 (83%) | 3,783 (67%) |
| Unknown | 27 (0%) | 10 (0%) | 0 (0%) | 0 (0%) | 2 (0%) | 6 (0%) | 10 (0%) |
| Median EMS response time, min | 5.3 (2.9); 9 | 5.4 (2.8); 9.3 | 5.6 (3.4); 11 | 5.3 (3.2); 9.6 | 5.3 (2.7); 8.9 | 5 (3); 9 | 5.4 (3); 9.1 |
| Public location | 2,193 (16%) | 888 (20%) | 171 (59%) | 130 (76%) | 468 (37%) | 2,193 (100%) | 1,285 (23%) |
| Witnessed bystander | 5,630 (41%) | 2,278 (52%) | 180 (62%) | 130 (76%) | 980 (77%) | 1,285 (59%) | 5,630 (100%) |
| Unknown first rhythm | 1,273 (9%) | 278 (6%) | 25 (9%) | 13 (8%) | 42 (3%) | 156 (7%) | — |
| Shockable | 3,278 (24%) | 1,341 (30%) | 170 (59%) | 170 (100%) | 1,280 (100%) | 1,054 (48%) | 2,122 (38%) |
| Unknown | 808 (6%) | 175 (4%) | 5 (2%) | 0 (0%) | 0 (0%) | 118 (5%) | 229 (4%) |
| Transported to hospital | 8,106 (59%) | 2,553 (58%) | 224 (78%) | 146 (86%) | 999 (78%) | 1,746 (80%) | 3,861 (69%) |
| Survival to hospital discharge | 907 (7%) | 382 (9%) | 69 (24%) | 64 (38%) | 286 (22%) | 368 (17%) | 641 (11%) |
Values are n, n (interquartile range), n (%), and n (interquartile range); 90%. Group 1 = all patients receiving EMS care for presumed cardiac arrest, excluding EMS-witnessed arrests. Group 2 = all non–EMS-witnessed arrests in which a bystander performed CPR. No AED applied before EMS. Group 3 = all non–EMS-witnessed arrests in which an AED was applied before EMS arrival. This was the primary multivariate analysis group. Group 4 = all non–EMS-witnessed arrests in which an AED applied before EMS arrival provided a shock. Group 5 = all non–EMS-witnessed arrest in which a bystander performed CPR, but the first shock was provided by EMS. Group 6 = all non–EMS-witnessed cardiac arrests treated by EMS in a public location. Group 7 = all bystander-witnessed cardiac arrests (must be non–EMS-witnessed).
AED = automatic external defibrillator; CPR = cardiopulmonary resuscitation; EMS = emergency medical services; IQR = interquartile range; OHCA = out-of-hospital cardiac arrest.
In addition, multiple logistic regression analysis determined the association between survival and AED application before EMS arrival after accounting for potential confounding factors. The primary inferential analysis consisted of a multiple logistic regression analysis for the 11,370 of 13,769 Group 1 arrests with complete data (Fig. 2). Survival to hospital discharge was regressed on a binary indicator of whether an AED was applied before EMS arrival adjusting for: 1) age and gender; 2) bystander CPR performed; 3) location of arrest (public or private); 4) EMS response interval; 5) arrest witnessed; 6) initial rhythm shockable, not shockable, or unknown; and 7) ROC site. Adjustment for initial rhythm also was included because it is likely a surrogate for other unmeasured confounders. Secondary analyses investigated potential clustering by site via generalized estimating equations (32) and generalized linear mixed models (33). Interaction by site was investigated by adding interactions between site and all other covariates in the multiple regression model. This analytical approach is essentially equivalent to fitting the multivariate model separately in each site, but provides additional power via simultaneous estimation of coefficients. A likelihood ratio test was used to compare the model with and without interactions.
We also addressed potential confounding in the observed relationship between AED application and survival through a propensity analysis to account for a subject’s probability of receiving bystander AED application (34). We estimated propensity scores as predicted probabilities from a logistic regression model with AED application as the outcome and the covariates discussed previously as predictors. We then created 6 strata based on the following quantiles of the score: 0.75, 0.90, 0.925, 0.95, and 0.975. These quantiles were chosen so that there were sufficient subjects in each stratum who both had an AED applied and survived. A Mantel-Haenszel chi-square test then was performed to estimate the odds ratio (OR) for survival with AED application versus without, stratified by propensity score.
We also addressed potential confounding by performing sensitivity analyses restricted to Groups 2 and 3—those who received bystander CPR but had no bystander AED applied, and those who had a bystander AED applied, because these 2 groups are least confounded with regard to the relationship between AED application and survival. Both the complete-case multiple regression model and the propensity score analysis were reproduced in this reduced population.
These complete-case analyses would provide a valid estimate of the association between AED application before EMS arrival and survival if data were missing completely at random (35), an assumption that cannot be tested fully. Hence, we used multiple imputations (36) of missing covariates to permit multivariate analysis of all 13,769 subjects who had known outcome status, addressing in part the limitation of missing covariate data. Analysis was carried out with the R mice package (The R Project for Statistical Computing) using 50 imputations.
Next, we also conducted a post hoc subgroup analysis to determine whether the OR for survival with AED applied versus not applied varied within subgroups of location (private or public). For this analysis, an interaction between AED application; and location was added to the original logistic regression model including all other covariates. Significance was determined via a likelihood ratio test comparing the model with interaction with the one without interaction.
Finally, we calculated the excess lives saved that were attributable to use of the bystander AED, then extrapolated this to the U.S. and Canada based on the ROC catchment area. The excess of lives saved was the difference between the observed number who survived when bystander AEDs were applied and the estimated number who would have survived had there not been bystander AEDs. The number who would have survived had there not been bystander AEDs was estimated by: 1) applying the estimated OR from the multivariate analysis to the observed odds among cases in which a bystander AED was applied to obtain the odds of survival had there not been bystander AED application; and 2) converting these odds back to a survival probability and multiplying by the number of patients who had an AED applied. We estimated the total population served to be approximately 21 million people by examining the census tracts of the EMS agencies. The extrapolation was based on the assumption that the ROC covers 21 million people and that the combined population of the U.S. and Canada is 330 million.
Results
During the 17-month study period, 15,549 persons experienced a nontraumatic OHCA and were treated by EMS in the study regions, and of these, 15,099 (97.1%) had a known outcome status. Of these, 1,330 arrests were excluded because they were witnessed by EMS (Fig. 2). Thus, the final cohort included 13,769 individuals (Group 1), among whom 2.1% (289) had an AED applied before EMS arrival (Group 3) and constituted the primary subgroup for analysis. In this group, an AED was applied by healthcare workers (32%), lay volunteers (35%), police (26%), or unknown (7%).
Table 1 characterizes the 5 subgroups of non–EMS-witnessed cases (Groups 1 through 5). The same groups are identified in Figure 2. The entire cohort included only 438 individuals who were younger than 18 years. The EMS response interval was similar across all groups, with a median response interval of 5.3 minutes (interquartile range, 4.0 to 6.9) for all non–EMS-witnessed cardiac arrests. Public location and bystander-witnessed arrests before EMS arrival also are shown in Table 1 and were more common among those with placement of an AED before EMS arrival, especially among those who received an AED shock. In addition, the proportion of OHCA in which an AED was applied before EMS arrival varied across ROC sites, ranging from 1% to 7%.
Overall survival and by subgroup
Table 1 shows the overall survival by subgroup. Overall survival was 7% among all EMS-treated OHCAs occurring before EMS arrival (Group 1; n = 13,769). Survival was 9% when CPR was performed before EMS arrival, but an AED was not applied (Group 2). Of the cases in which an AED was applied before EMS arrival (Group 3), 24% (69 of 289) survived, and of those who received a shock from an AED applied before EMS arrival (Group 4), 38% (64 of 170) survived. Survival was 40% with application of an AED by a lay person, 16% for health care workers, and 13% for police. Forty-one of the 289 AED applied arrests occurred in residential institutions where healthcare workers were present.
The survival of patients who had an AED applied before EMS arrival but no AED shock was 3.5%, and this rate was not different from the 2.3% (n = 2,887) survival among patients who received bystander CPR without an AED applied and had a nonshockable rhythm at presentation (p < 0.34). The rates reported exclude those with an unknown initial rhythm. Controlling for the covariates included in the model for the primary analysis did not change this conclusion (p < 0.60).
Logistic regression model
A logistic regression model was applied to all cases with complete information from Group 1 (n = 11,370). The unadjusted OR of survival associated with AED application before EMS arrival (with or without shock) was 4.74 (95% CI: 3.53 to 6.36). After adjusting for age, gender, bystander CPR performed, type of location, EMS response interval, witness status, initial rhythm, and ROC site, AED application before EMS arrival was associated with an OR of survival of 1.75 (95% CI: 1.23 to 2.50; p < 0.002). This OR was attenuated slightly to 1.62 (95% CI: 1.16 to 2.26; p < 0.007) when we used a stratified propensity score analysis to adjust for these covariates instead of multiple regression. In the reduced population that included only those who received treatment from a bystander, the complete-case OR was 1.68 (95% CI: 1.19 to 2.39; p < 0.004) and the propensity score OR was 1.73 (95% CI: 1.25 to 2.39; p < 0.002). Propensity score models predicted AED application well, with C statistics of 0.91 and 0.82, respectively, for the 2 models. Generalized estimating equation and generalized linear mixed model analyses that accounted for clustering by site produced similar estimates.
Of those cases with missing data (n = 2,399), 87% lacked witnessed status, bystander CPR status, or both (574 witnessed, 809 CPR, and 699 both). Thirty-six of the excluded cases were cases in which an AED was applied before EMS arrival. In the analysis of all 13,769 patients with survival data, using multiple imputation for missing covariate data, the OR of survival associated with an AED applied before EMS arrival was similar to that found in other analyses: 1.75 (95% CI: 1.27 to 2.41; p < 0.001).
Site-specific analysis of bystander AED use
When multiple regression was performed on complete cases with stratification by site, nearly all of the site-specific OR estimates were more than 1, but many were not significantly different from 1, likely because of the number of subjects receiving bystander AED application at individual sites was small (Table 2). This stratified model fit the data better than the model not stratified by site (p < 0.003). However, it required that a large number of ORs be estimated using a limited amount of data on bystander AED application.
Table 2.
Multivariate Analysis of Survival by Site: Cases With Complete Data Only
| n | AED Applied Before EMS | Adjusted OR* (95% CI) | |
|---|---|---|---|
| Alabama | 119 | 5 | NA |
| Dallas, Texas | 423 | 8 | NA |
| Iowa | 452 | 32 | 0.69 (0.21–2.31) |
| Milwaukee, Wisconsin | 957 | 19 | 4.85 (1.58–14.84) |
| Ottawa, Ontario, Canada | 2,204 | 46 | 1.78 (0.66–4.81) |
| Pittsburgh, Pennsylvania | 440 | 38 | 1.21 (0.33–4.43) |
| Portland, Oregon | 548 | 17 | 1.72 (0.49–6.10) |
| Seattle/KC, Washington | 1,316 | 27 | 0.99 (0.38–2.57) |
| Toronto, Ontario, Canada | 3,010 | 41 | 3.65 (1.63–8.18) |
| Vancouver, British Columbia, Canada | 1,901 | 20 | 1.51 (0.55–4.19) |
| Overall | 11,370 | 253 |
Versus no AED applied.
CI = confidence interval; KC = King County; NA = not available; OR = odds ratio; other abbreviations as in Table 1.
Post hoc subgroup analysis of location of AED application
Table 3 presents survival by the type of location of the OHCA. Of the 288 OHCA in which AED application took place, 59% (171 of 288) occurred in public sites and 41% (117 of 288) occurred in private locations. Survival was 35% (59 of 171) among public location OHCAs with AED application, 20% (177 of 888) among public location OHCAs with bystander CPR but no AED application, 9% (10 of 117) among private location OHCAs with AED application, and 6% (204 of 3,510) among private location OHCAs with bystander CPR but no AED application. Although the absolute survival differences observed for AED application were greater in public settings than in private settings, the positive survival association of AED application did not differ significantly according to type of location (adjusted OR, 1.39 private and 1.86 public; p = 0.53 for interaction between AED and location).
Table 3.
Survival to Hospital Discharge by Type of Location
| AED Applied Before EMS | Survival (%) | Bystander CPR, No AED Applied Before EMS | Survival (%) | Adjusted OR* (95% CI)† | |
|---|---|---|---|---|---|
| Public | 171 | 35 | 888 | 20 | 1.86 (1.26–2.75) |
| Street/highway | 14 | 36 | 210 | 13 | |
| Public building | 48 | 38 | 169 | 21 | |
| Place of recreation | 41 | 49 | 135 | 24 | |
| Industrial place | 18 | 22 | 54 | 15 | |
| Other public place | 50 | 24 | 320 | 23 | |
| Private | 117 | 9 | 3,510 | 6 | 1.39 (0.62–3.09) |
| Home residence | 71 | 11 | 2,805 | 7 | |
| Farm/ranch | 1 | 0 | 7 | 0 | |
| Residential institution | 41 | 5 | 668 | 2 | |
| Other private place | 4 | 0 | 30 | 10 | |
Extrapolated estimate of lives saved
We extrapolated survival in the approximately 21 million people in the ROC’s covered area to the entire population of the U.S. and Canada (330 million). We estimate that currently, 474 lives are saved per year by bystander application of an AED to those who experience an OHCA.
Discussion
This observational study, drawn from a large set of heterogeneous communities, provides strong evidence that AED application before EMS arrival is associated with improved survival after OHCA. Multiple analytical approaches designed to account for confounding consistently demonstrated a significant survival benefit of AED application with an OR of approximately 1.8. This OR is comparable with the 2-fold AED survival benefit demonstrated in the randomized and controlled PAD trial (6) in which volunteers received special training in AED use at high-risk AED-equipped sites.
In combination, the results underscore the critical importance of early defibrillation and continue to encourage innovative approaches to achieve this critical link in the chain of survival. Such approaches may include implanted monitors with electronic alert to a bystander and the EMS system. Another strategy includes mandatory registration of all public access defibrillators with local EMS dispatch. The dispatcher could coach 1 person to start CPR and another bystander to retrieve the closest AED. Also, placement of all AEDs may be guided by a model that considers health risk, population density, and rate of cardiac arrest in similar buildings.
The current investigation involves a catchment population of 21 million persons who reside in urban, suburban, and rural areas across North America and are served by more than 200 EMS agencies with a variety of operating models and training levels. Moreover, laypersons, persons with health care training, and police all provided AED application. Success of 40% by lay persons emphasizes that speed is more important than training. Thus, we believe the results of the current study provide the best information to date supporting the generalizability of the PAD trial (6), and so represent a meaningful community-based approach to improve survival after an OHCA.
In both the current study and the PAD trial, most of the survivors who received AED application experienced an OHCA in public as opposed to private locations in part because more AED application occurred in public sites, but primarily because survival was better in public locations. In contrast to the robust association in public sites, the PAD study and the current investigation did not observe this independent survival association in private locations. Similarly, a randomized trial evaluating home AED placement did not demonstrate survival benefit in part potentially because of the low OHCA event rate. Nonetheless, of 14 patients in the home AED trial where an AED shock was delivered, 26.8% survived, which is similar to the 38% in the current study. Taken together, the results highlight an established role in public settings and suggest a need for additional study to optimize private AED deployment, especially if resources are limited.
The primary analysis was performed for AED application rather than AED shock. This approach allowed for the possibility of adverse effects of AED application such as delay in performing CPR or in calling 911. Particularly for patients with non-VT/VF arrest, the AED offers no obvious benefit and the potential for delay in other important links in the chain of survival.
The results of the current study need to be viewed in light of existing data on meaningful survival after hospital discharge and long-term survival. Better resuscitation is associated with better survival (37), functional status (38), and health-related quality of life (39–41). It is reasonable to expect similar or better survival in the present study because defibrillation was provided earlier than if delivered by EMS.
A unique and important feature of this investigation is that it enables an assessment of how readily clinical trial evidence (from the PAD trial) has been translated into community-based practice. Given the observed survival benefits in the current investigation, AED application before EMS arrival provides a viable means to improve public health. In the current investigation, AED application before EMS arrival occurred in 2.1% of all OHCAs. However, use varied from 1% to 7% across the ROC network sites, a finding that offers a framework for efforts aimed at further implementation of AED programs. A recent study emphasized the importance of locating AEDs in places of high cardiac arrest frequency (42). This may be 1 contributor to site-specific differences in AED survival. Hence, an overall goal of 5% seems realistic, with some communities already exceeding this percentage of rapid AED use. Such an increase has the potential to double the population-attributable benefit (the number of lives saved) of early AED application. The 1,280 patients in Group 5, in which EMS shocked the patient, might have had even better survival than (22%) if a bystander had applied an AED. The survival of 38% with shock by a bystander using the AED should encourage broader awareness of the AED, which may prompt increased use by bystanders even for those lacking medical training.
The strengths of this report include: 1) the large and heterogeneous set of communities, EMS systems, and OHCA population base; 2) uniform data collection across multiple communities, enabling a multivariate analysis using the important clinical outcome of hospital survival; 3) the contemporary nature of the data and incidence of VT/VF; 4) the assessment of the survival association of AED application and whether a shock was delivered, a unique aspect of the current study; and 5) compared with other reports (2,3,5,6), the relatively large number of patients with AED applied (n = 289).
The study limitations include the lack of information regarding: 1) underlying health status before cardiac arrest; 2) long-term survival; 3) detailed neuropsychiatric assessment of survivors; 4) the extent and type of PAD programs within the network; 5) the training of lay volunteers and health care workers and placement of AEDs; 6) complete data for all cases; and 7) the findings from the AED-recorded electrocardiography records. An additional limitation of this analysis is the observational nature of the data. Because randomization was not used to determine which subjects received AED application, there is no guarantee that those who received it were comparable with those who did not. We tried to minimize this potential confounding by adjusting for all measured confounders in our multiple logistic regression model and by conducting propensity score analyses. However, there may have been other, unmeasured characteristics that also were confounders, such as the physical place of AEDs. Our inability to account for these leaves open the possibility that our results were biased.
Conclusions
Cardiac arrest is a treatable condition. This investigation supports a significant and important beneficial impact of PAD programs in community-based settings. On average, early AED defibrillation before EMS arrival seems to nearly double a victim’s odds of survival after OHCA. These results support strategic expansion of PAD programs particularly in public locations across the United States and Canada as a continuing major public health initiative.
Acknowledgments
The Resuscitation Outcomes Consortium (ROC) is supported by a series of cooperative agreements to 10 regional clinical centers and 1 data coordinating center (5U01 HL077863, HL077881, HL077871 HL077872, HL077866, HL077908, HL077867, HL077885, HL077887, HL077873, and HL077865) from the National Heart, Lung and Blood Institute in partnership with the National Institute of Neurological Disorders and Stroke; the U.S. Army Medical Research & Material Command; The Canadian Institutes of Health Research (CIHR)–Institute of Circulatory and Respiratory Health; Defence Research and Development Canada; the American Heart Association; and the Heart and Stroke Foundation of Canada. Some ROC site emergency medical systems have received equipment or concessions from automatic external defibrillator manufacturers. The ROC coordinating center accepts support for receptions from corporations. Dr. Weisfeldt receives salary support from NIH via the ROC. Dr. Ornato is an unpaid Science Advisory Board member of Zoll. Dr. Rea received research support from Medtronic, Inc., and Philips, Inc. Dr. Aufderheide is a consultant for Medtronics, Inc., and JoLife, Inc. Dr. Nichol is a co-principal investigator of the ROC Data Coordinating Center (NHLBI); principal investigator of the randomized trial of hemofiltration after resuscitation from cardiac arrest (NHLBI); co-investigator of the randomized field trial of cold saline IV after resuscitation after cardiac arrest (NHLBI); principal investigator of the randomized trial of CPR training aid in community (Asmund S. Laerdal Foundation for Acute Medicine); has received travel expenses from Innercool Therapies Inc., Radiant Medical Inc., and the American Heart Association; and is a consultant for Triage Wireless.
Abbreviations and Acronyms
- AED
automatic external defibrillator
- CPR
cardiopulmonary resuscitation
- EMS
emergency medical services
- OHCA
out-of-hospital cardiac arrest
- OR
odds ratio
- VF
ventricular fibrillation
- VT
ventricular tachycardia
References
- 1.Shah JS, Maisel WH. Recalls and safety alerts affecting automated external defibrillators. JAMA. 2006;296:655–60. doi: 10.1001/jama.296.6.655. [DOI] [PubMed] [Google Scholar]
- 2.Valenzuela TD, Roe DJ, Nichol G, Clark LL, Spaite DW, Hardman RG. Outcomes of rapid defibrillation by security officers after cardiac arrest in casinos. N Engl J Med. 2000;343:1206–9. doi: 10.1056/NEJM200010263431701. [DOI] [PubMed] [Google Scholar]
- 3.Page RL, Joglar JA, Kowal RC, et al. Use of automated external defibrillators by a U.S. airline. N Engl J Med. 2000;343:1210–6. doi: 10.1056/NEJM200010263431702. [DOI] [PubMed] [Google Scholar]
- 4.White RD, Hankins DG, Bugliosi TF. Seven years’ experience with early defibrillation by police and paramedics in an emergency medical services system. Resuscitation. 1998;39:145–51. doi: 10.1016/s0300-9572(98)00135-x. [DOI] [PubMed] [Google Scholar]
- 5.Caffrey SL, Willoughby PJ, Pepe PE, Becker LB. Public use of automated external defibrillators. N Engl J Med. 2002;347:1242–7. doi: 10.1056/NEJMoa020932. [DOI] [PubMed] [Google Scholar]
- 6.PAD Investigators. Public-access defibrillation and survival after out-of-hospital cardiac arrest. N Engl J Med. 2004;351:637–46. doi: 10.1056/NEJMoa040566. [DOI] [PubMed] [Google Scholar]
- 7.Christenson J, Nafziger S, Compton S, et al. The effect of time on CPR and automated external defibrillator skills in the public access defibrillation trial. Resuscitation. 2007;74:52–62. doi: 10.1016/j.resuscitation.2006.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ko PC, Ma MH, Yen ZS, Shih CL, Chen WJ, Lin FY. Impact of community-wide deployment of biphasic waveform automated external defibrillators on out-of-hospital cardiac arrest in Taipei. Resuscitation. 2004;63:167–74. doi: 10.1016/j.resuscitation.2004.04.002. [DOI] [PubMed] [Google Scholar]
- 9.Capucci A, Aschieri D, Piepoli MF. Out-of-hospital early defibrillation successfully challenges sudden cardiac arrest: the Piacenza Progetto Vita project. Ital Heart J. 2002;3:721–5. [PubMed] [Google Scholar]
- 10.Culley LL, Rea TD, Murray JA, et al. Public access defibrillation in out-of-hospital cardiac arrest. Circulation. 2004;109:1859–63. doi: 10.1161/01.CIR.0000124721.83385.B2. [DOI] [PubMed] [Google Scholar]
- 11.Colquhoun MC, Chamberlain DA, Newcombe RG, et al. A national scheme for public access defibrillation in England and Wales: early results. Resuscitation. 2008;78:275–80. doi: 10.1016/j.resuscitation.2008.03.226. [DOI] [PubMed] [Google Scholar]
- 12.Myerburg RJ, Fenster J, Velez M, et al. Impact of community-wide police car deployment of automated external defibrillators on survival from out-of-hospital cardiac arrest. Circulation. 2002;106:1058–64. doi: 10.1161/01.cir.0000028147.92190.a7. [DOI] [PubMed] [Google Scholar]
- 13.Pell JP, Sirel JM, Marsden AK, Ford I, Walker NL, Cobbe SM. Potential impact of public access defibrillators on survival after out of hospital cardiopulmonary arrest: retrospective cohort study. BMJ. 2002;325:515. doi: 10.1136/bmj.325.7363.515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Groh WJ, Newman MM, Beal PE, Fineberg NS, Zipes DP. Limited response to cardiac arrest by police equipped with automated external defibrillators: lack of survival benefit in suburban and rural Indiana. The Police as Responder Automated Defibrillation Evaluation (PARADE) Acad Emerg Med. 2001;8:324–30. doi: 10.1111/j.1553-2712.2001.tb02109.x. [DOI] [PubMed] [Google Scholar]
- 15.Pell JP, Walker A, Cobbe SM. Cost-effectiveness of automated external defibrillators in public places: con. Curr Opin Cardiol. 2007;22:5–10. doi: 10.1097/HCO.0b013e3280118fec. [DOI] [PubMed] [Google Scholar]
- 16.Gold LS, Eisenberg M. Cost-effectiveness of automated external defibrillators in public places: pro. Curr Opin Cardiol. 2007;22:1–4. doi: 10.1097/HCO.0b013e32801173c1. [DOI] [PubMed] [Google Scholar]
- 17.Maisch S, Friederich P, Goetz AE. Public access defibrillation: limited use by trained first responders and laymen. Anaesthesist. 2006;55:1281–90. doi: 10.1007/s00101-006-1098-0. [DOI] [PubMed] [Google Scholar]
- 18.Amit G, Zalzstein E, Ilia R, Katz A. Automatic external defibrillator (AED) and public access defibrillation (PAD) Harefuah. 2006;145:375–9. [PubMed] [Google Scholar]
- 19.Einav S, Weissman C, Kark J, Lotan C, Matot I. Future shock: automatic external defibrillators. Curr Opin Anaestesiol. 2005;18:175–80. doi: 10.1097/01.aco.0000162837.79215.a7. [DOI] [PubMed] [Google Scholar]
- 20.Clare C. Do public access defibrillation (PAD) programmes lead to an increase of patients surviving to discharge from hospital following out of hospital cardiac arrest? A literature review. Int J Nurs Stud. 2006;43:1057–62. doi: 10.1016/j.ijnurstu.2005.11.020. [DOI] [PubMed] [Google Scholar]
- 21.Myers JB, French D, Webb W. Lack of integration of automated external defibrillators with EMS response may reduce lifesaving potential of public-access defibrillation. Prehosp Emerg Care. 2005;9:339–43. doi: 10.1080/10903120590961969. [DOI] [PubMed] [Google Scholar]
- 22.Woollard MF. Public access defibrillators. BMJ. 2003;326:162. [PMC free article] [PubMed] [Google Scholar]
- 23.Becker L, Gold LS, Eisenberg M, White L, Hearne T, Rea T. Ventricular fibrillation in King County, Washington: a 30-year perspective. Resuscitation. 2008;79:22–7. doi: 10.1016/j.resuscitation.2008.06.019. [DOI] [PubMed] [Google Scholar]
- 24.Bardy GH, Lee KL, Mark DB, et al. Home use of automated external defibrillators for sudden cardiac arrest. N Engl J Med. 2008;358:1793–804. doi: 10.1056/NEJMoa0801651. [DOI] [PubMed] [Google Scholar]
- 25.Cobb LA, Fahrenbruch CE, Olsufka M, Copass MK. Changing incidence of out-of-hospital ventricular fibrillation. JAMA. 2002;288:3008–13. doi: 10.1001/jama.288.23.3008. [DOI] [PubMed] [Google Scholar]
- 26.Nichol G, Thomas E, Callaway CW, et al. Regional variation in out-of-hospital cardiac arrest incidence and outcome. JAMA. 2008;300:1423–31. doi: 10.1001/jama.300.12.1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Peberdy MA, Kaye W, Ornato JP, et al. Cardiopulmonary resuscitation of adults in the hospital: a report of 14720 cardiac arrests from the National Registry of Cardiopulmonary Resuscitation. Resuscitation. 2003;58:297–308. doi: 10.1016/s0300-9572(03)00215-6. [DOI] [PubMed] [Google Scholar]
- 28.Davis DP, Garberson LA, Andrusiek DL, et al. A descriptive analysis of emergency medical service systems participating in the Resuscitation Outcomes Consortium (ROC) network. Prehospital Emergency Care. 2007;11:369–82. doi: 10.1080/10903120701537147. [DOI] [PubMed] [Google Scholar]
- 29.Morrison LJ, Nichol G, Rea TD, et al. Rationale, development and implementation of the Resuscitation Outcomes Consortium epistry cardiac arrest. Resuscitation. 2008;78:161–9. doi: 10.1016/j.resuscitation.2008.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Aufderheide TP, Kudenchuk PJ, Hedges JR, et al. Resuscitation Outcomes Consortium (ROC) PRIMED cardiac arrest trial methods part 1: rationale and methodology for the impedance threshold device (ITD) protocol. Resuscitation. 2008;78:179–85. doi: 10.1016/j.resuscitation.2008.01.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Stiell IG, Callaway C, Davis D, et al. Resuscitation Outcomes Consortium (ROC) PRIMED cardiac arrest trial methods part 2: rationale and methodology for “analyze later vs. analyze early” protocol. Resuscitation. 2008;78:186–95. doi: 10.1016/j.resuscitation.2008.01.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zeger SL, Liang K-Y. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42:121–30. [PubMed] [Google Scholar]
- 33.Stiratelli R, Laird N, Ware J. Random effects models for serial observations with binary responses. Biometrics. 1984;40:961–71. [PubMed] [Google Scholar]
- 34.Rosenbaum PR, Rubin DB. Reducing bias in observational studies using subclassification of the propensity score. J Am Statist Assoc. 1984;386:516–24. [Google Scholar]
- 35.Rubin DB. Inference and missing data. Biometrika. 1976;63:581–92. [Google Scholar]
- 36.Schafer JL. Multiple imputation: a primer. Statist Meth Med Res. 1999;8:3–15. doi: 10.1177/096228029900800102. [DOI] [PubMed] [Google Scholar]
- 37.Bunch TJ, White RD, Gersh BJ, et al. Long-term outcomes of out-of-hospital cardiac arrest after successful early defibrillation. N Engl J Med. 2003;348:2626–33. doi: 10.1056/NEJMoa023053. [DOI] [PubMed] [Google Scholar]
- 38.Stiell IG, Wells GA, Field B, et al. Advanced cardiac life support in out-of-hospital cardiac arrest. N Engl J Med. 2004;351:647–56. doi: 10.1056/NEJMoa040325. [DOI] [PubMed] [Google Scholar]
- 39.Stiell IG, Nichol G, Wells GA, De Maio VJ, Nesbitt L, Blackburn J, et al. Health related quality of life is better for cardiac arrest survivors who received citizen CPR. Circulation. 2003;108:1939–44. doi: 10.1161/01.CIR.0000095028.95929.B0. [DOI] [PubMed] [Google Scholar]
- 40.Stiell IG, Nesbitt LP, Nichol G, et al. Comparison of the cerebral performance category score and the health utilities index for survivors of cardiac arrest. Ann Emerg Med. 2009;53:241–8. doi: 10.1016/j.annemergmed.2008.03.018. [DOI] [PubMed] [Google Scholar]
- 41.van Alem AP, Waalewijn RA, Koster RW, de Vos R. Assessment of quality of life and cognitive function after out-of-hospital cardiac arrest with successful resuscitation. Am J Cardiol. 2004;93:131–5. doi: 10.1016/j.amjcard.2003.09.027. [DOI] [PubMed] [Google Scholar]
- 42.Folke F, Lippert FK, Nielsen SL, et al. Location of cardiac arrest in a city center: strategic placement of automated external defibrillators in public locations. Circulation. 2009;120:510–7. doi: 10.1161/CIRCULATIONAHA.108.843755. [DOI] [PubMed] [Google Scholar]