Abstract
We examine changes among adolescent girls in substance use during pregnancy and the postpartum period. Three separate latent growth curve analyses assessed the impact of psychosocial, behavioral, and sociodemographic factors on resumption of or change in use of cigarettes, alcohol, and marijuana. The Vulnerable Populations Model for Research and Clinical Practice (Flaskerud & Winslow, 1998) provided the theoretical foundation for this study. This is a secondary analysis of data from a sample of 305 ethnic minority females (245 Latina, 60 African-American), aged 13–18 years, who were pregnant at baseline and were participating in an HIV prevention study conducted in inner-city alternative schools in Los Angeles County. Data collected at four time points captured changes in substance use from pregnancy through the postpartum period. Baseline predictors included ethnicity/race, partner substance use, childhood abuse history, religiosity, acculturation, depressive symptoms, length of gestation at baseline, and prior substance use. Common predictors of greater resumption and/or greater level of use included greater history of use prior to pregnancy, partner substance use, childhood abuse, and a longer time since childbirth. African Americans were more likely to be smoking at baseline when they were still pregnant and to use marijuana postpartum; Latinas were more likely to use alcohol over the course of pregnancy and postpartum. Other variables exerted an influence on specific substances. For instance, religiosity impacted cigarette and alcohol use. Findings may assist prenatal care providers to identify and counsel pregnant adolescents at risk for perinatal substance use and to prevent resumption or initiation of substance use following childbirth.
Keywords: parenting teens, adolescent substance use, latent growth curve models
Substance use during pregnancy and the postpartum period is a major health concern for the fetus/newborn and family, with policy implications for healthcare in the U.S. (Button, Maughan, & McGuffin, 2007; Knopik et al., 2006; Suarez, Felkner, Brender, Canfield, & Hendricks, 2008). Data from a large national survey show that 4% of pregnant women aged 15–44 years had used some type of illicit drug (e.g., marijuana, hashish, cocaine, crack, heroin, PCP, LSD) in the past month as compared to 10% of non-childbearing women of similar age (Substance Abuse and Mental Health Services Administration [SAMHSA], 2007). The same study identified tobacco and alcohol as the most commonly reported substances used during pregnancy, 16.5% and 11.8%, respectively. In another large study, nearly 16% of pregnant 15- to 17-year-olds reported use of alcohol in the past month, averaging 24 drinks during that month (SAMHSA, 2008). Examination of ethnic/racial differences reveals that non-Hispanic white adult women, regardless of pregnancy and parenting status, report substance use at the highest rates, followed by Hispanics and non-Hispanic blacks (Muhuri & Gfroerer, 2008).
Few studies have described the trajectory of substance use among pregnant and parenting teens over time, although several cross-sectional studies with adolescents and/or adults have assessed substance use during pregnancy and the various factors associated with and predicting use (De Genna, Larkby, & Cornelius, 2007; Goodman & Huang, 2002; Muhuri & Gfroerer, 2008). In this paper, we present findings from a 12-month prospective study examining patterns and predictors of substance use in pregnant adolescents from Latino and African-American backgrounds.
Pregnancy has been shown to moderate substance use in general. Past 30-day use of alcohol, cigarettes, marijuana, psychotherapeutics, or cocaine was reported to be substantially lower among pregnant women age 18 to 44, especially in the second and third trimesters, than among those who were parenting or nonpregnant (Muhuri & Gfroerer, 2008). Substance use in adolescent mothers tends to decrease or cease until the pregnancy ends, and then gradually resume in the first few months postpartum, although often at a lower level than pre-pregnancy (Gilchrist, Hussey, Gillmore, Loir, & Morrison, 1996; Koniak-Griffin, Lesser, Uman, & Nyamathi, 2003). Bailey and colleagues (Bailey, Hill, Hawkins, Catalano, & Abbott, 2008) reported that pregnancy decreased the probability of binge drinking, daily smoking, and marijuana use in young adult women, but use returned to pre-pregnancy levels within 2 years postpartum. Carmichael and Ahluwalia (2000) found that 25.6% of women in their population-based adult and adolescent sample smoked cigarettes before pregnancy; 44.5% of these women quit during pregnancy, but half of those who quit had relapsed within 2–6 months after delivery. Independent correlates associated with increased risk of postpartum relapse included African-American ethnicity, multiparity (having ≥2 previous births), late or no prenatal care, and stressful life events. In a sample of low-income, pregnant adult Latinas age 18 to 40 (N=100), 43% reported alcohol use in the 3 months prior to recognition of the current pregnancy; of these, 8% continued drinking after learning they were pregnant (Chambers et al., 2005).
Theoretical framework
The Vulnerable Populations Model for Research and Clinical Practice (Flaskerud & Winslow, 1998) provided the theoretical foundation for this investigation. The model relates resource availability and relative risk to health status. Within the context of this model, adolescent mothers from ethnic/racial minority backgrounds represent a vulnerable population that has limited resources and faces increased relative risk for health problems such as depression and perinatal substance use compared with other populations (e.g., white middle-class women). The purpose of this study is to determine and describe predictors of individual differences in the trajectory and resumption of substance use among a group of inner-city, pregnant adolescents of ethnic minority backgrounds, and to examine their substance use over a period of 12 months during late pregnancy and up to at least 6 months postpartum.
The psychosocial, behavioral, and sociodemographic variables selected for examination in this study fall within the domains of this model (e.g., religiosity and family intactness are indicators of resource availability; low self-esteem, romantic partner drug use, depressive symptoms, prior history of abuse and/or substance use represent relative risk). Perreira and Cortes (2006) examined a nationally representative cohort of pregnant adult and adolescent women with hospital birth data from 20 U.S. cities (N=4185). They reported that all women were more likely to report prenatal substance use if their newborn’s father also reported substance use. Paternal alcohol and illicit drug use were associated most strongly with maternal alcohol use. Similarly, analyses of data from the National Longitudinal Study of Adolescent Health support the significant influence that romantic partners have on female adolescents’ involvement in high risk behaviors (e.g., smoking cigarettes, getting drunk) (Haynie, Giordano, Manning & Longmore, 2005) Greater acculturation has been identified as a risk factor for substance use in adult and adolescent populations. Immigrant youth of varying ethnic origins living in the U.S. less than 6 years report lower lifetime and recent use of alcohol and marijuana (p < 0.001) than those living in the U.S. more than 6 years (Blake, Ledsky, Goodenow, & O’Donnell, 2001). Harrison and Sidebottom (2009) found that pre-pregnancy alcohol and drug use among adolescent and adult prenatal patients from four urban clinics was much higher among U.S.-born women than immigrants and among unmarried than married women. Older age and current smoking were predictors of both alcohol and drug use continuation. Pre-pregnancy alcohol use frequency, depression, and physical/sexual abuse by someone other than an intimate partner predicted alcohol use continuation, while drug use continuation was also predicted by pre-pregnancy drug use frequency and race (higher for American Indians and African Americans) (Harrison & Sidebottom, 2009).
In another sample of pregnant adolescents attending a prenatal clinic (De Genna et al., 2007), earlier age at first drink and use of alcohol during first coitus were found to predict problem drinking in the year before pregnancy; the latter variable also significantly predicted drinking during the first trimester. Socioeconomic status was a significant predictor of alcohol use before and during pregnancy, while externalizing problems were a risk factor for alcohol use during the first trimester. Earlier drinkers were more likely to continue use during pregnancy. African-American adolescents were significantly less likely to use alcohol during first coitus, but not less likely to use alcohol during pregnancy.
In research involving non-childbearing adult and adolescent women, similar and additional correlates of substance use have been reported. For example, in a large retrospective study involving over 4,500 adult women, adverse childhood experiences (including physical and sexual abuse) increased the likelihood 2- to 4-fold of early drinking and smoking (Dube et al., 2003). Among adolescent girls, depressive symptoms have been associated with higher levels of alcohol, marijuana, and cigarette use; these positive associations may be due to shared risk factors for depression and substance use (Fleming, Mason, Mazza, Abbott, & Catalano, 2008). High self-esteem has been posited as protective against adolescent substance use, especially among Hispanics. Zamboanga and associates (Zamboanga, Schwartz, Hernandez Jarvis, & Van Tyne, 2009) observed that self-esteem was the most important protective factor against substance use (i.e., cigarette, alcohol, and marijuana) in Hispanic early adolescents (ages 11–15). However, inconsistencies have been observed across studies examining the relationship between (global) self-esteem and drug use among other adolescent populations, possibly because researchers do not appear to have established a consensus as to what is or is not self-esteem (Donnelly, Young, Pearson, Penhollow, & Hernandez, 2008).
Limited evidence suggests that church attendance and family structure serve to protect or reduce risk of substance use. Adolescents who attend church at least once monthly reportedly may engage in smoking or drinking but are significantly less likely to use marijuana and cocaine as compared to those who infrequently or never attend church (Jang & Johnson, 2001; Chu, 2007). Some comparisons of youth living in intact vs. disrupted families have suggested that living with both parents may have a protective effect on adolescents’ illicit drug use (Grunbaum, Kann, Kinchen, Williams, & Ross, 2002; Jeynes, 2001; National Center on Addiction and Substance Abuse, 2003; Sutherland & Shepherd, 2001). Newer research, however, shows that this issue is much more complex than originally believed, as the impact varies with gender, number of family transitions, quality of relationship with parent, changes in socioeconomic resources, possible disruption of peer relationships, and other factors (Krohn, Hall, & Lizotte, 2009; Hair, Park, Ling, & Moore, 2009).
Hypotheses
Based upon the theoretical model and other past research, it was hypothesized that substance use as represented by smoking, and alcohol and marijuana use among Latino and African-American adolescents in pregnancy and the postpartum period would:
Be positively associated with prior use of drugs, depressive symptoms, a history of childhood abuse, current partner’s use of drugs, and higher acculturation; and negatively associated with self-esteem, religiosity, and having an intact family, as suggested by the Vulnerable Populations Model.
Be positively associated with a greater length of time since giving birth.
Methods
Participants and Procedures
Participants included in this secondary analysis represent a subsample from a larger prospective study examining the effects of a four-session (8-hour), theory-based HIV prevention program (Project CHARM, Children’s Health and Responsible Mothering; Principal Investigator: D. Koniak-Griffin) on pregnant and parenting adolescents. The intervention focused on maternal protectiveness as an impetus to reduce or eliminate sexual risk-taking behavior, adolescents’ vulnerability to HIV/AIDS, and taking on sexual responsibility and accountability. Although substance use was not a major focus of the program, participants learned how drug use may play a role in increasing risk for HIV. Further details of this randomized controlled trial involving 497 adolescents (aged 13–18 years, predominantly from underrepresented minority groups) have previously been reported (Koniak-Griffin, Lesser, Nyamathi, et al., 2003).
The subsample used in the current study included only the 305 Latina and African-American adolescents (245 Latinas, 60 African Americans) who were pregnant at baseline. The adolescents in the larger sample who had already given birth when they entered the study (n=168) were not eligible for this analysis, as this study focused on the trajectory of substance use from pregnancy through the postpartum period; those who did not identify as Latina or African American (n=24) were also excluded. The original sample and the subsample displayed similar characteristics in terms of age distribution, ethnic/racial characteristics, and other key variables (e.g., marital status). Table 1 presents the characteristics of participants in the current study. Although the large majority of participants in this sample (80%) were Latino, no significant differences were found between this ethnic group and the African Americans on sociodemographic characteristics such as age, marital status, socioeconomic status, or grade in school. Because baseline and follow-up assessments were conducted in small groups, there were minimal amounts of missing data. The very small amounts of missing data were imputed using the EM (expected-maximization) algorithm (Arbuckle, 1996; Tang & Bentler, 1998).
Table 1.
Demographics and Summary Statistics of Predictor Variables in the Latent Growth Model (LGM)
| Variables (range) | Mean (%) | SD | Factor Loading | |
|---|---|---|---|---|
| Demographicsa | ||||
| Age (13–18 years) | 16.51 | 1.07 | –––– | |
| Grade in school (7–12) | 10.37 | 1.11 | –––– | |
| Predictors | ||||
| Prior smoking (0–1) | (61%) | –––– | ||
| Prior drinking (0–3) | 1.62 | 1.08 | –––– | |
| 0 = 28%, 1 = 2%, 2 = 51%, 3 = 19% | ||||
| Prior marijuana use (0–3) | 1.36 | 1.11 | –––– | |
| 0 = 37%, 1 = 2%, 2 = 49%, 3 = 12% | ||||
| Drug-using boyfriend | ||||
| Heroin | (2%) | –––– | .28b | |
| Methamphetamines | (5%) | –––– | .69 | |
| Cocaine | (6%) | –––– | .52 | |
| Abuse history (0–4) | ||||
| Physical | 1.21 | 0.69 | .58 | |
| Sexual | 1.30 | 0.79 | .50 | |
| Depression (0–60) | 19.60 | 10.07 | –––– | |
| Self-esteem (1–4) | 2.97 | 0.70 | –––– | |
| Intact family | (37%) | –––– | –––– | |
| Religiosity (1–5) | 2.56 | 1.10 | –––– | |
| Acculturation (1–5) | 3.77 | 0.95 | –––– | |
| Weeks pregnant (7 – 40) | 25.57 | 6.95 | –––– | |
| In Control Group | (27%) | –––– | –––– | |
| African American | (20%) | –––– | –––– |
Not included in LGM.
All factor loadings significant, p ≤ .001.
All informed consent procedures were approved by the University of California’s institutional review board, and full informed consent was obtained before data collection. Parental consent was waived, as participation in the study entailed no more than minimal risk such that adolescents might reasonably assume on their own, and obtaining parental consent would have presented an undue hardship to some young women. As part of the informed consent process, adolescents were advised about the procedures to protect and maintain confidentiality of data and assured that school officials would not have access to their questionnaires. A Certificate of Confidentiality was issued by the federal government for this study. Participants were recruited from pregnant minor or young parents’ programs within alternative schools of four school districts of Los Angeles County. Schools were randomly assigned by site to either the intervention or comparable length control condition. Questionnaires were read to small groups of adolescents by specially trained research staff within the classroom setting, in the absence of school officials. Participants completed their own questionnaires as the items were read to them. Data were collected over a period of 12 months: at baseline and at 3-, 6-, and 12-month follow-ups, with $15 compensation provided per administration. The majority of questionnaires were administered within the classroom; however, some follow-up postpartum evaluations were conducted in homes for participants who were no longer attending school. As outlined above, at baseline all participants were currently pregnant. By the 3-month follow-up, 60% had delivered their babies. Only 4% remained pregnant at the 6-month data collection. Additional details have been previously reported (Koniak-Griffin, Lesser, Nyamathi et al., 2003).
Instruments and Variables
The instrument packet contained a combination of questionnaires and individual items designed to measure background characteristics such as age, race/ethnicity, length of gestation, family composition (intact vs. parents divorced or separated), and various psychosocial variables.
Substance Use
Prior use
At baseline participants estimated their prior use by responding to the questions: “During your life, how many days have you had at least one drink of alcohol?” and “During your life, how many times have you used marijuana (weed) or hashish?” Response categories were the same for alcohol and marijuana: never = 1; one or two times/days = 2; 3 to 9 times/days = 3; 10 to 19 times/days = 4; 20 to 39 times/days = 5; 40 to 99 times/days = 6; 100 or more times/days = 7. The response categories were recoded as: 0 = none/never used, 1 = mild use (1 to 9 times), 2 = moderate use (10 to 19 times), and 3 = heavy use (more than 19 times). The higher options were rarely chosen. Prior cigarette smoking was defined as having “ever smoked cigarettes regularly, that is, at least one cigarette every day for one month” with 0 = no, 1 = yes. (Lifetime measures similar to those for alcohol and marijuana were not available.)
Current use dependent variables
Frequency of current use of alcohol, marijuana, and cigarettes was estimated using response categories similar to those for prior use; however, the interval for measurement varied: i.e., participants were asked about use during the past month at baseline and the 12-month follow-up; whereas, the 3-month follow-up assessed frequency of daily use during the past 2 months, and the 6-month follow-up evaluated frequency of daily use in the past 3 months. For cigarettes, the item was worded: During the past month, on the days you smoked, how many cigarettes did you smoke per day (none = 1, less than 1 = 2, 1 per day = 3, 2–5 per day = 4, 6 to 10/day = 5, 11 to 20/day = 6, more than 1 pack = 7). For alcohol the item was worded: During the past month, on how many days did you have at least one drink of alcohol: 0 days = 1, 1 or 2 days = 2, 3 to 5 days = 3, 6 to 9 days = 4, 10 to 19 days = 5, 20 to 29 days = 6, all 30 days = 7. For marijuana, they were asked how many times they used marijuana and this ranged from 1–6, as follows: 0 times = 1, 1 or 2 times = 2, 3 to 9 times = 3, 10 to 19 times = 4, 20 to 39 times = 5, 40 or more times = 6. Responses based on a greater number of months were scaled so that the responses were equivalent if necessary.
Drug-using boyfriend
The participants were asked whether they had a current boyfriend who used heroin, cocaine, or methamphetamines. These three items were used as indicators of a latent variable labeled “Drug-using boyfriend.” The participants were queried about this because the content of the intervention included information about HIV-risk behaviors. High-risk male partners, including injecting drug users and other heavy substance users, are believed to increase HIV risk for their female partners (Koniak-Griffin, Lesser, Nyamathi, et al., 2003).
Psychosocial and Behavioral Variables
History of physical/sexual abuse
This was measured by responses to the question, “Have you ever been physically abused by an adult (where an adult caused you to have a scar, black and blue marks, welts, bleeding or broken bones)?” Sexual abuse was assessed by response to the question, “Have you ever been sexually abused by someone (that is, someone in your family or someone else) who did sexual things to you that you did not want or forced you to touch them sexually?” The options for both questions ranged from 0 to 4 (“Never” = 0, “Once” = 1, “2 or 3 times” = 2, “4 to 10 times” = 3, “More than 10 times” = 5). These two items were used as indicators of a latent variable representing abuse history.
Depressive symptoms
The 20-item Center for Epidemiological Studies Depression Scale (CES-D) was used to assess symptoms of clinical depression (Radloff, 1977). On this scale, the participant reports how frequently he/she experienced a symptom in the past 7 days. Each item is rated from 0 to 3 (0 = rarely; 1 = some of the time; 2 = occasionally; 3 = most of the time). In the larger CHARM study, the coefficient alpha was .84 (Koniak-Griffin, Lesser, Uman, et al., 2003), and it was .84 in the smaller subsample as well.
Global self-worth
Global self-worth was measured by a subscale of the Self-Perception Profile for Children, a self-reporting inventory for assessing children’s and adolescents’ perceptions of themselves in various specific domains of their life, as well as their sense of global self-worth (Harter, 1985). The scale consists of five items. A typical item is: “Some teenagers are often disappointed with themselves BUT other teenagers are pretty pleased with themselves.” Responses for each question were coded in two parts: part A indicates which part of the statement they agree with; part B indicates 0 if “sort of true for me” or 1 if “really true for me.” Cronbach’s alpha was 0.72 in the larger sample (Koniak-Griffin, Lesser, Uman, et al., 2003) and the same in the subsample.
Religiosity
Religiosity was measured by participants’ self-report of the number of times they attended religious services in 1 year and their perceived degree of religiosity. Response options ranged from 0 (“Not at all”) to 5 (“More than once a week”). On the second measure, “How religious are you?” the response options ranged from “Not at all” (0) to “Very religious” (4). A composite of the two measures comprised the religiosity score.
Acculturation
Acculturation was measured by the Acculturation Rating Scale for Mexican Americans (ARSMA)(Cuellar, Harris, & Jasso, 1980), which was administered to evaluate Latinas’ language preference and their degree of reading and writing skills (range = 1–5). This measure was used because the large majority of Latinas in the study were of Mexican or Mexican-American origin (see Table 1). African-American participants did not complete this measure; however, a score of 5 was assigned to them because the rating reflects a high level of acculturation.
Intact family
The dichotomous intact family variable was measured by a single question, “Are your parents divorced or separated?” (Yes = 1, No = 0).
Pregnancy/Postpartum status
The pregnancy status of each participant was determined at the beginning of the study by asking “When is your baby due?” The date given was used to calculate the length of gestation in weeks at the time of the baseline questionnaire. Higher values indicate that the adolescent was further along in her pregnancy. Adolescents varied in their length of gestation at baseline when they were recruited for the study, and this variable helped to control for length of pregnancy in predicting substance use.
Intervention group membership
Group membership (HIV-prevention intervention group vs. control) was also included as a control variable, as membership could possibly have impacted their substance use behaviors even though substance use was not a major focus of either the experimental (HIV-prevention intervention) or control condition (general health promotion program).
Analysis
Latent growth curve (LGC) modeling was used to predict the trajectory of changes in substance use through pregnancy and the postpartum period using the previously identified variables as predictors. Separate models assessed predictors of change in cigarette smoking, alcohol use, and marijuana use. LCG modeling is ideal for studying longitudinal change in behavior, as it provides a means of studying individual differences reflected in developmental functions. The intercept corresponds to the initial status of the participants’ substance use at Time 1 (baseline). The intercept is a constant for any individual across time and represents information concerning the mean of the collective individual intercepts that characterize each individual’s growth curve. The second factor, labeled slope, represents the rate of change (increase or decrease) in substance use over the period of study.
The EQS structural equations program (Bentler, in press)was used to assess the latent growth models and also provided information on the relationships among the psychosocial, behavioral, and sociodemographic variables and prior use of each of the three substances. Goodness-of-fit of the models was assessed with the maximum-likelihood χ2 statistic; the Comparative Fit Index (CFI); the Satorra-Bentler χ2 (S-B χ2), the Robust Comparative Fit Index (RCFI), and the root mean squared error of approximation (RMSEA) (Bentler, in press; Bentler & Dudgeon, 1996; Hu & Bentler, 1999; Steiger, 1990). The RMSEA should be less than 0.06, and values at or above .95 for the CFI and RCFI are desirable (Hu & Bentler, 1999). The Robust S-B χ2 was used in addition to the maximum likelihood χ2 because it is more appropriate when the data depart from multivariate normality. Mardia’s normalized multivariate kurtosis estimates were high in all three models: z-statistic = 48.23, 72.64, and 45.89 for cigarettes, alcohol, and marijuana, respectively, rejecting multivariate normality (Bentler & Dudgeon, 1996). Standard errors were corrected for the extent of their nonnormality using the robust scaled statistics (Bentler & Dijkstra, 1985). This was essential because the skewness in the data reflected the little to no substance use by many of the girls in the study.
An initial confirmatory factor analysis (CFA) was performed among all of the hypothesized independent measured and latent variables with each hypothesized latent construct predicting its measured indicators. All latent constructs and the single-item variables were correlated with no assignment of temporal ordering. This analysis assessed the adequacy of the proposed factor structure (measurement model) and the relationships among the latent and measured variables. Then an LGM for each substance was tested in which the independent variables predicted the trajectories of the resumption of substance use among the pregnant and postpartum adolescents. All possible predictive paths from the independent variables to the growth curve latent variables were included and gradually dropped if they were nonsignificant.
Results
Substance Use Rates During Pregnancy and Postpartum
Baseline substance use rates, when all participants were still pregnant, were low although most had some degree of experience with the substances before their pregnancies (see Table 1). Four percent reported smoking cigarettes, 2% drinking alcohol, and 2.6% using marijuana. Only cigarette smoking and marijuana use were reported by African Americans, whereas Latinas reported using all three substances. Preliminary analyses ascertained that use of the three substances increased significantly over time as assessed at 3, 6, and 12 months after baseline (see Table 2). If there had been no increase in use, then LGM would not have been appropriate. Once it was established that rates increased, then LGM was used to determine which background predictors influenced the trajectories of increased use (slopes) as well as initial levels (intercepts).
Table 2.
Substance use over time among 305 adolescents pregnant at baseline (245 Latinas, 60 African Americans)
| Latinas | African Americans | Total | p | |
|---|---|---|---|---|
| Mean/S.D. | Mean/S.D. | Mean/S.D. | ||
| Cigarettes | ||||
| Baseline | 1.04 (0.24) | 1.22 (0.96)* | 1.08 (0.48) | .01 |
| 3 months | 1.21 (0.91) | 1.25 (0.93) | 1.22 (0.91) | .75 |
| 6 months | 1.41 (1.18) | 1.53 (1.55) | 1.44 (1.26) | .51 |
| 12 months | 1.49 (1.24) | 1.65 (1.72) | 1.52 (1.35) | .40 |
| Alcohol | ||||
| Baseline | 1.02 (0.15) | 1.00 (.00) | 1.02 (0.14) | .22 |
| 3 months | 1.12 (0.46) | 1.02 (0.13) | 1.10 (0.42) | .08 |
| 6 months | 1.36 (0.75) | 1.32 (0.79) | 1.35 (0.76) | .70 |
| 12 months | 1.39 (0.70) | 1.52 (1.03) | 1.42 (0.78) | .27 |
| Marijuana | ||||
| Baseline | 1.04 (0.30) | 1.10 (0.66) | 1.05 (0.39) | .30 |
| 3 months | 1.06 (0.30) | 1.15 (0.76) | 1.08 (0.43) | .15 |
| 6 months | 1.22 (0.73) | 1.42 (1.04) | 1.26 (0.81) | .10 |
| 12 months | 1.21 (0.69) | 1.55 (1.23)* | 1.28 (0.83) | .01 |
African-Americans significantly higher than Latinas. Possible ranges: cigarettes (1–7), alcohol and marijuana (1–6).
Confirmatory Factor Analysis
Fit indexes for the three initial separate CFA models (that did not yet include the substance use measures at baseline, 3, 6, and 12 months, but did include prior use of the particular substance) are uniformly excellent: Cigarettes: ML χ2 = 42.11, 31 df; CFI = .97, RMSEA = .034; S-B χ2 = 35.30, 31 df; RCFI = .99, RMSEA = .021; Alcohol: ML χ2 = 34.17, 31 df; CFI = .99, RMSEA = .018; S-B χ2 = 31.46, 31 df; RCFI = .99, RMSEA = .007; Marijuana: ML χ2 = 42.59, 31 df; CFI = .97, RMSEA = .004; S-B χ2 = 37.83, 31 df; RCFI = .98, RMSEA = .027. Correlations are reported in Table 3. Of note, lifetime smoking and drinking were significantly and positively correlated with a substance-using boyfriend (p ≤ .001, p ≤ .01 respectively), a history of abuse (p ≤ .001, p ≤ .01 respectively), and depressive symptoms (p ≤ .001, p ≤ .05 respectively). Prior marijuana use was significantly correlated with a history of abuse (p ≤ .001), depressive symptoms (p ≤ .01), and greater acculturation (p ≤ .01). Other significant relationships are evident as well (see Table 3).
Table 3.
Correlations among independent variables in Latent Growth Curve analysis
| Independent Variables | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Prior smoking | --- | ||||||||||||
| 2. Prior drinking | N/A | --- | |||||||||||
| 3. Prior marijuana use | N/A | N/A | --- | ||||||||||
| 4. Drug-using boyfriend | .24*** | .16** | .12 | --- | |||||||||
| 5. Abuse history | .43*** | .20** | .25*** | .26** | --- | ||||||||
| 6. Depression | .18*** | .12* | .17** | .23*** | .28*** | --- | |||||||
| 7. Self-Esteem | −.11 | −.07 | −.02 | −.14* | −.20** | −.41*** | --- | ||||||
| 8. Intact family | .01 | −.06 | −.09 | −.12* | −.11 | .02 | −.06 | --- | |||||
| 9. Religiosity | −.07 | −.14** | −.10 | −.12* | .04 | .03 | .07 | .12* | --- | ||||
| 10. Acculturation | .03 | .11* | .23*** | .05 | .12 | .07 | .15** | −.18*** | −.02 | --- | |||
| 11. Weeks pregnant | .00 | .01 | −.05 | −.00 | −.11 | −.18*** | .14** | −.00 | .10 | −.04 | --- | ||
| 12. In Control Group | .02 | .03 | −.04 | −.17*** | −.08 | −.01 | −.02 | .05 | .01 | .01 | .11* | --- | |
| 13. African American | .11* | −.11 | .02 | −.18*** | .06 | .04 | .23*** | −.24*** | .06 | .64*** | −.01 | .03 | --- |
p ≤ .05;
p ≤ .01;
p ≤ .001.
Latent Growth Models
Figures 1 through 3 present the significant predictive paths in the final trimmed LGMs. For readability, the figures do not depict the significant relationships among the predictors. They are available in Table 3. The fit indexes of the path models are excellent: Cigarettes: ML χ2 = 155.95, 128 df; CFI = .97, RMSEA = .028; S-B χ2 = 136.05, 128 df; RCFI = .98, RMSEA = .014; Alcohol: ML χ2 = 135.19, 112 df; CFI = .96, RMSEA = .026; S-B χ2 = 124.54, 112 df; RCFI = .97, RMSEA = .019; Marijuana: ML χ2 = 138.72, 122 df; CFI = .98, RMSEA = .021; S-B χ2 = 131.79, 122 df; RCFI = .99, RMSEA = .016. These models are larger and more complex due to the addition of the 4 time periods in addition to mean structures of the individual variables.
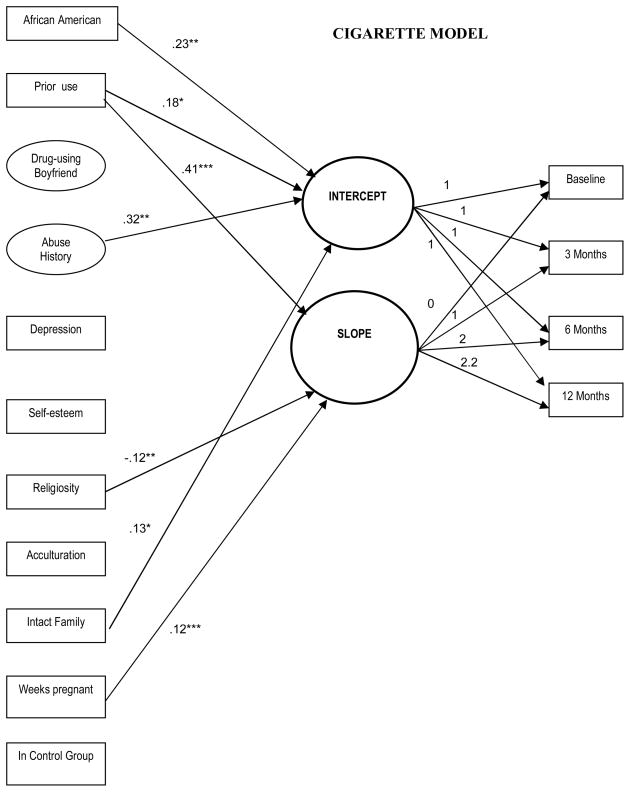
Figure 1.
Final structural path model predicting cigarette use. Regression coefficients are standardized. Circles designate latent variables; rectangles represent single-indicator items. Single-headed arrows represent regressions. Correlations are not depicted among predictors for readability. *p < .05; **p < .01; ***p < .001.
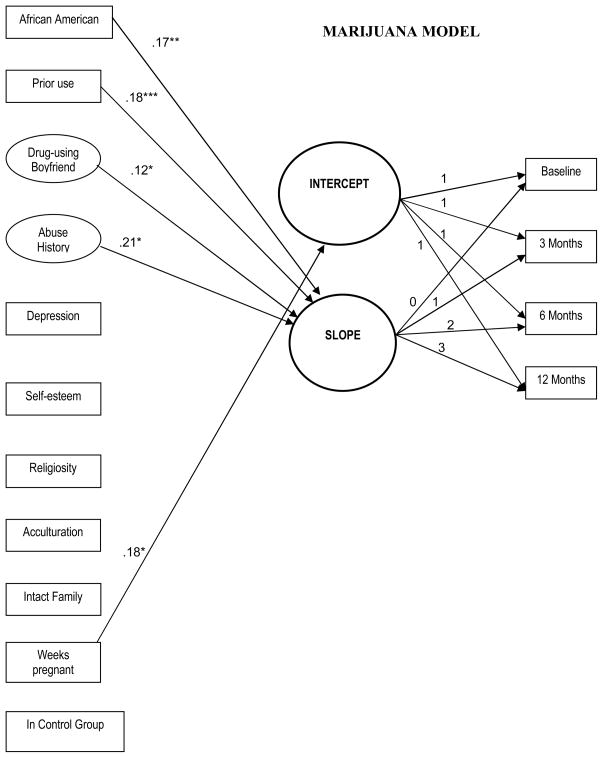
Figure 3.
Final structural path model predicting marijuana use. Regression coefficients are standardized. Circles designate latent variables; rectangles represent single-indicator items. Single-headed arrows represent regressions. Correlations are not depicted among predictors for readability. *p < .05; **p < .01; ***p < .001.
In the cigarette model (Figure 1), prior smoking (p ≤ .05), abuse history (p ≤ .05), and being African American (p ≤ .01) predicted greater initial levels of smoking during pregnancy. Over the period of the study, prior smoking (p ≤ .001), less religiosity (p ≤ .05), and childbirth (p ≤ .05) significantly influenced the resumption of and increased cigarette smoking. In other words, the further along the adolescent was in her pregnancy at baseline, the sooner she would resume smoking. Note that due to the flattening out of the linear trend in resumption of cigarette smoking by 12 months, the fixed estimate at 12 months is not 3 but 2.5.
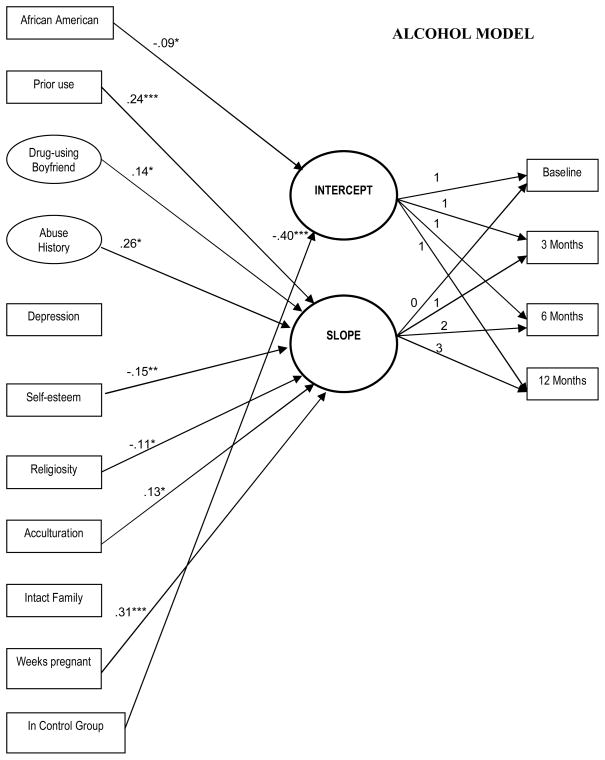
In the alcohol model (Figure 2) few variables predicted the initial level of alcohol use, partially due to the fact that drinking was rare at baseline. Being African American and being in the control group had significant negative effects on the level of use of alcohol at baseline. However, several variables influenced resumption and/or more drinking behavior during the postpartum period: a history of alcohol use (p ≤ .001), a history of abuse, having a drug-using boyfriend, a higher level of acculturation, less religiosity (all p ≤ .05), and lower self-worth (p ≤ .01). As the women gave birth, they were much more likely to increase their use of alcohol (p ≤ .001).
Figure 2.
Final structural path model predicting alcohol use. Regression coefficients are standardized. Circles designate latent variables; rectangles represent single-indicator items. Single-headed arrows represent regressions. Correlations are not depicted among predictors for readability. *p < .05; **p < .01; ***p < .001.
In the marijuana model (Figure 3), only a later stage of pregnancy predicted level of marijuana use at baseline. The steepness of the slope was impacted by abuse history, having a substance-using boyfriend (both p ≤ .05), prior use of marijuana (p ≤ .001) and being African American (p ≤ .01).
Discussion
The Vulnerable Populations Model provided a broad perspective for informing and modeling factors influencing Latina and African-American young mothers’ resumption or initiation of substance use. The unique design of this longitudinal study facilitated our understanding of behavior change in use of substances across time by not only considering levels of use but also predicting steeper resumption and initiation trajectories that could only be discerned through the latent growth models. Major findings demonstrate that although the majority of these pregnant, inner-city adolescents never used, discontinued, or decreased their frequency of use of cigarettes, alcohol, and marijuana during gestation, many resumed or initiated use of these substances within 6 months following childbirth. Resumption and increases were predicted by elements of the Vulnerable Population Model (Hypothesis One) as well as the prediction of Hypothesis Two.
Hypothesis One: Vulnerable Population Model
For all three substances, more pre-pregnancy use, which is a risk in this population, predicted greater use and a steeper resumption curve in the postpartum period for cigarettes, and steeper slopes for alcohol and marijuana. Results of this study support the findings of previous studies of substance use among pregnant adolescents (Gilchrist et al., 1996; Teagle & Brindis, 1998; Wiemann & Berenson, 1998) and of national surveys on past-month substance use among pregnant adolescent and adult women (SAMHSA, 2005). However, the rate of perinatal substance use reported in our sample was far below national rates, which might be explained by differences in ages, sampling and methodology. Our sample is quite young. In addition, because participants in this study were attending special prenatal and parenting programs, it is also possible that the protected educational environment influenced their behaviors.
These findings also substantiate other previous research suggesting that those who reported use of alcohol and cigarettes prior to pregnancy had a greater propensity for later and regular use of these substances (Young et al., 2002). The more rapid resumption of smoking or other substances, especially among those who had a prior history of use (a relative risk), may be attributed to habit and possibly to stressors associated with the transition to parenthood. Similar findings have also been described in other studies of pregnant and parenting substance use (Fang et al., 2004; MacLean, Estable, Sims-Jones, & Edwards, 2002) where transitions to motherhood and transitions to become nonsmokers were in conflict.
Another important predictor of resumption and use emerged for all three substances: past history of childhood physical and/or sexual abuse. Abuse predicted higher initial usage of cigarettes and predicted a steeper slope for both alcohol and marijuana. Our findings demonstrate the detrimental impact that childhood maltreatment and sexual abuse may have on adolescents’ health risk behaviors. Other researchers have reported potential negative effects of childhood physical and sexual abuse on adults, e.g., alcoholism, eating disorders, severe obesity, depression, suicide, sexual promiscuity, antisocial and abusivebehavior, and certain chronic diseases (Arnow, Hart, Hayward, Dea, & Barr-Taylor, 2000; Chartier, Walker, & Naimark, 2007; MacMillan et al., 2001; Thomas, Hyppönen, & Power, 2008). The finding in our study of an impact on use of all substances reinforces the pervasive and negative effect of abuse, which increases vulnerability to a variety of dysfunctional outcomes.
In the case of both alcohol and marijuana use, having a partner who used illicit drugs also significantly affected the behavior of adolescent mothers, providing support for Hypothesis One. This finding demonstrates the importance of examining dyadic influences in substance use studies involving adolescent mothers. Another important predictor variable found in the smoking and alcohol models was religiosity as measured by church attendance and self-perception of religiousness. Congruent with findings of other studies, religiosity, a resource in the Vulnerable Populations Model, was a protective factor that had an inverse relationship with a more rapid use of cigarettes and alcohol (Jang & Johnson, 2001; Sinha, Cnaan, & Gelles, 2007; Wills, Yaeger, & Sandy, 2003).
Our findings only provided partial support for the components of the Vulnerable Population Model. For instance, depressive symptoms as reflected in the CES-D did not predict any levels or acceleration of substance use over time. However, depression was correlated with prior use of all substances, so its impact may have been indirect and antecedent to initial drug use. Depression was also significantly associated with a history of childhood abuse, low self-worth and having a substance-using boyfriend. Available data do not allow examination of the predictive relationship between depressive symptoms and early onset of substance use; i.e., which one preceded the other. Research suggests that depressive symptoms and substance use share associations with important risk and protective factors, such as parental psychopathology, parenting problems, child exposure to violence, school problems, sexual activity, and love relationships (Harrison & Sidebottom, 2009; Barnet, Duggan, Wilson, & Joffe, 1995). Other predictors that were considered in the model included a higher acculturation level and lower self-esteem, which were predictors of a steeper alcohol slope only, and not living in an intact family. An intact family actually predicted more smoking, which was counter to our predictions. We also found some ethnic differences. African Americans’ intercepts were lower for alcohol but higher for cigarettes, and the slope for African American ethnicity was steeper for use of marijuana. Our findings differ from earlier reports that Hispanic and Black women do not differ significantly for smoking during pregnancy (Perreira & Cortes, 2006). The impact of socioeconomic background on the ethnic differences observed in our sample is unknown. Further research is recommended to understand these differences.
Hypothesis Two: Postnatal Use Increases over Time
As predicted by Hypothesis 2, a later gestational status (more weeks pregnant at baseline) was a major predictor of use of all three substances over time. Once the baby was born, the adolescent would be more likely to return to, or possibly initiate, use of cigarettes, alcohol, and/or marijuana. In the case of alcohol, the slope was particularly steep; for marijuana, the influence was on the intercept. This finding is a reminder to health care providers of young mothers that these adolescents are vulnerable to resuming health risk behaviors such as illicit substance use postpartum, and more so over time, and that continuing patient education during well-baby check-ups may be a necessary part of their interactions with these teen mothers.
Limitations
There were several limitations to this study that warrant consideration. First, the substance use data were based upon self-report rather than direct physiologic measures. Participants’ self-reporting of substance use could not be verified or quantified precisely, thus underestimation is a possibility. Because the reporting periods for substance use varied somewhat at different evaluation points, selected substance use items needed to be equalized through statistical procedures. Second, the variables selected for the current analyses were confined to those in the original investigation. Other critical factors found to influence perinatal substance use were unexamined; for example, stressful life events (Carmichael & Ahluwalia, 2000); current psychopathology and unemployment (e.g., Havens, Simmons, Shannon, & Hansen, 2009). The wording of the question evaluating parental marital status and whether the girl resided in an intact family restricted examination of other possible family constellations (e.g., unmarried parents living together, step-parents or other caregiver status). Third, although gestational stage was included as a control, variations in gestational stage of participants enrolling in the study created differences in the length of pregnancy and time from childbirth evaluated among subjects within the 1-year trajectory profiled in this study. The different timings of the transition from pregnant to postpartum status is an important limitation in our findings, particularly at the 6-month (96% postpartum) and 12-month follow-up evaluations, because past research shows that length of time from childbirth influences reinstitution of substance use among adolescent mothers. However, inclusion of a variable representing weeks pregnant at baseline helps to control for this problem. Finally, this sample may not be representative of other pregnant and parenting teens due to geographical, ethnic, and socioeconomic considerations.
Conclusion
Despite these limitations, findings of this study have several important implications for clinical practice. It is particularly important for prevention efforts to be strengthened during the prenatal period in order to avert postpartum resumption of use among young mothers with a history of substance use prior to pregnancy, even if they are currently abstaining from substances. Pregnancy and the early postpartum period offer a window of opportunity to assist adolescents in maintaining their positive behavior changes. Smoking, alcohol, and marijuana cessation programs should be integrated into prenatal care programs and teen parenting curricula. Our findings also suggest that involving male partners in these efforts may be beneficial, because their behavior has a strong impact on young mothers’ return to use. Young fathers also may benefit from prevention efforts directed toward maintaining family health through substance-free environments.
The findings of this study demonstrate that from pregnancy through the postpartum period many young mothers, particularly those with a prior history of substance use, return to using the same drugs or increase their usage over time, although often to levels lower than reported prior to pregnancy. Particularly important predictors of resumption or initiation of substance use include past history of substance use, length of time following delivery (postpartum status), having a partner who uses drugs, and past childhood abuse. Maternal protectiveness may serve as a motivator for positive behavior for some young mothers. The growth curve analysis used in this study provided a powerful means of modeling behavior change at an individual level and has utility for behavioral change research.
Acknowledgments
This project used data from a grant funded by the National Institute of Nursing Research (R01-NR04375) (DK-G). Partial support was also provided by the National Institute on Drug Abuse (NIDA P01 DA01070-36) (JAS). The authors thank Gisele Pham for editorial and production assistance and Carmen Turner for editorial assistance.
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/adb
Contributor Information
Gwendolyn V. Spears, School of Nursing, University of California Los Angeles
Judith A. Stein, Department of Psychology, University of California Los Angeles
Deborah Koniak-Griffin, School of Nursing, University of California Los Angeles.
References
- Arbuckle JL. Full information estimation in the presence of incomplete data. In: Marcoulides GA, Schumacker RE, editors. Advanced structural equation modeling: Issues and techniques. Mahwah, NJ: Erlbaum; 1996. pp. 243–277. [Google Scholar]
- Arnow BA, Hart S, Hayward C, Dea R, Barr-Taylor C. Severity of child maltreatment, pain complaints and medical utilization among women. Journal of Psychiatric Research. 2000;34:413–421. doi: 10.1016/s0022-3956(00)00037-6. [DOI] [PubMed] [Google Scholar]
- Bailey J, Hill K, Hawkins J, Catalano R, Abbott R. Men’s and women’s patterns of substance use around pregnancy. Birth. 2008;35:50–59. doi: 10.1111/j.1523-536X.2007.00211.x. [DOI] [PubMed] [Google Scholar]
- Barnet B, Duggan AK, Wilson MD, Joffe A. Association between postpartum substance use and depressive symptoms, stress, and social support in adolescent mothers. Pediatrics. 1995;96(4 Pt 1):659–666. [PubMed] [Google Scholar]
- Bentler PM. EQS structural equations program manual. Encino, CA: Multivariate Software; in press. [Google Scholar]
- Bentler PM, Dijkstra T. Efficient estimation via linearization in structural models. In: Krishnaiah PR, editor. Multivariate analysis VI. Amsterdam: North-Holland; 1985. pp. 9–42. [Google Scholar]
- Bentler PM, Dudgeon P. Covariance structure analysis: Statistical practice, theory, and directions. Annual Review of Psychology. 1996;47:563–592. doi: 10.1146/annurev.psych.47.1.563. [DOI] [PubMed] [Google Scholar]
- Blake SM, Ledsky R, Goodenow C, O’Donnell L. Recency of immigration, substance use and sexual behavior among Massachusetts adolescents. American Journal of Public Health. 2001;91:794–798. doi: 10.2105/ajph.91.5.794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Button T, Maughan B, McGuffin P. The relationship of maternal smoking to psychological problems in the offspring. Early Human Development. 2007;83:727–732. doi: 10.1016/j.earlhumdev.2007.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carmichael SL, Ahluwalia IB. Correlates of postpartum smoking relapse: Results from the pregnancy risk assessment monitoring system (PRAMS) American Journal of Preventive Medicine. 2000;19:193–196. doi: 10.1016/s0749-3797(00)00198-7. [DOI] [PubMed] [Google Scholar]
- Chambers CD, Hughes S, Meltzer SB, Wahlgren D, Kassem N, Larson S, et al. Alcohol consumption among low-income pregnant Latinas. Alcoholism, Clinical and Experimental Research. 2005;29:2022–2028. doi: 10.1097/01.alc.0000187160.18672.f9. [DOI] [PubMed] [Google Scholar]
- Chartier MJ, Walker JR, Naimark B. Childhood abuse, adult health, and health care utilization: Results from a representative community sample. American Journal of Epidemiology. 2007;165:1031–1038. doi: 10.1093/aje/kwk113. [DOI] [PubMed] [Google Scholar]
- Chu D. Religiosity and desistance from drug use. Criminal Justice and Behavior. 2007;34:661–679. [Google Scholar]
- Cuellar I, Harris L, Jasso R. An acculturation scale for Mexican-American normal and clinical populations. Hispanic Journal of Behavioral Sciences. 1980;2:199–217. [Google Scholar]
- De Genna N, Larkby C, Cornelius M. Early and adverse experiences with sex and alcohol are associated with adolescent drinking before and during pregnancy. Addictive Behaviors. 2007;32:2799–2810. doi: 10.1016/j.addbeh.2007.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donnelly J, Young M, Pearson R, Penhollow TM, Hernandez A. Area specific self-esteem, values, and adolescent substance use. Journal of Drug Education. 2008;38:389–403. doi: 10.2190/DE.38.4.f. [DOI] [PubMed] [Google Scholar]
- Dube SR, Felitti VJ, Dong M, Chapman DP, Giles WH, Anda RF. Childhood abuse, neglect, and household dysfunction and the risk of illicit drug use: The adverse childhood experiences study. Pediatics. 2003;111:564–572. doi: 10.1542/peds.111.3.564. [DOI] [PubMed] [Google Scholar]
- Fang WL, Goldstein AO, Butzen AY, Hartsock SA, Hartmann KE, Helton M, et al. Smoking cessation in pregnancy: a review of postpartum relapse prevention strategies. Journal of the American Board of Family Practice. 2004;17:264–275. doi: 10.3122/jabfm.17.4.264. [DOI] [PubMed] [Google Scholar]
- Flaskerud JH, Winslow BJ. Conceptualizing vulnerable populations health-related research. Nursing Research. 1998;47:69–78. doi: 10.1097/00006199-199803000-00005. [DOI] [PubMed] [Google Scholar]
- Fleming CB, Mason WA, Mazza JJ, Abbott RD, Catalano RF. Latent growth modeling of the relationship between depressive symptoms and substance use during adolescence. Psychology of Addictive Behaviors. 2008;22:186–197. doi: 10.1037/0893-164X.22.2.186. [DOI] [PubMed] [Google Scholar]
- Gilchrist LD, Hussey JM, Gillmore MR, Lohr MJ, Morrison DM. Drug use among adolescent mothers: Pre-pregnancy to 18 months postpartum. Journal of Adolescent Health. 1996;19:337–344. doi: 10.1016/S1054-139X(96)00052-3. [DOI] [PubMed] [Google Scholar]
- Goodman E, Huang B. Socioeconomic status, depressive symptoms, and adolescent substance use. Archives of Pediatrics and Adolescent Medicine. 2002;156:448–453. doi: 10.1001/archpedi.156.5.448. [DOI] [PubMed] [Google Scholar]
- Grunbaum JA, Kann L, Kinchen SA, Williams B, Ross JG. Youth risk behavior surveillance - United States, 2001. Journal of School Health. 2002;72:313–328. doi: 10.1111/j.1746-1561.2002.tb07917.x. [DOI] [PubMed] [Google Scholar]
- Hair EC, Park MJ, Ling TJ, Moore KA. Risky behaviors in late adolescence: Co-occurrence, predictors, and consequences. Journal of Adolescent Health. 2009;45:253–261. doi: 10.1016/j.jadohealth.2009.02.009. [DOI] [PubMed] [Google Scholar]
- Harrison P, Sidebottom A. Alcohol and drug use before and during pregnancy: An examination of use patterns and predictors of cessation. Maternal and Child Health Journal. 2009;13:386–394. doi: 10.1007/s10995-008-0355-z. [DOI] [PubMed] [Google Scholar]
- Harter S. Manual for the self-perception profile for children. Denver, CO: University of Denver; 1985. [Google Scholar]
- Havens JR, Simmons LA, Shannon LM, Hansen WF. Factors associated with substance use during pregnancy: Results from a national sample. Drug and Alcohol Dependence. 2009;99(1–3):89–95. doi: 10.1016/j.drugalcdep.2008.07.010. [DOI] [PubMed] [Google Scholar]
- Haynie DL, Giordano PC, Manning WD, Longmore MA. Adolescent romantic relationships and delinquency involvement. Criminology. 2005;43:177–210. [Google Scholar]
- Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- Jang SJ, Johnson BR. Neighborhood disorder, individual religiosity, and adolescent use of illicit drugs: A test of multilevel hypotheses. Criminology. 2001;39:106–136. [Google Scholar]
- Jeynes WH. The effects of recent parental divorce on their children’s consumption of marijuana and cocaine. Journal of Divorce & Remarriage. 2001;35:43–64. [Google Scholar]
- Knopik VS, Heath AC, Jacob T, Slutske WS, Bucholz KK, Madden PA, et al. Maternal alcohol use disorder and offspring ADHD: Disentangling genetic and environmental effects using a children-of-twins design. Psychological Medicine. 2006;36:1461–1471. doi: 10.1017/S0033291706007884. [DOI] [PubMed] [Google Scholar]
- Koniak-Griffin D, Lesser J, Nyamathi A, Uman G, Stein JA, Cumberland WG. Project CHARM: An HIV prevention program for adolescent mothers. Family and Community Health. 2003;26:94–107. doi: 10.1097/00003727-200304000-00003. [DOI] [PubMed] [Google Scholar]
- Koniak-Griffin D, Lesser J, Uman G, Nyamathi A. Teen pregnancy, motherhood, and unprotected sexual activity. Research in Nursing and Health. 2003;26:4–19. doi: 10.1002/nur.10062. [DOI] [PubMed] [Google Scholar]
- Krohn MD, Hall GP, Lizotte AJ. Family transitions and later delinquency and drug use. Journal of Youth and Adolescence. 2009;38:466–480. doi: 10.1007/s10964-008-9366-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lonardo Ra, Giordano PC, Longmore MA, Manning WD. Parents, friends, and romantic partners: Enmeshment in deviant networks and adolescent delinquency involvement. Journal of Youth & Adolescence. 2009;38:367–383. doi: 10.1007/s10964-008-9333-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacLean LM, Estable A, Sims-Jones N, Edwards N. Concurrent transitions in smoking status and maternal role. Journal of Nursing Scholarship. 2002;34:39–40. [Google Scholar]
- MacMillan HL, Fleming JE, Streiner DL, Lin E, Boyle MH, Jamieson E, et al. Childhood abuse and lifetime psychopathology in a community sample. American Journal of Psychiatry. 2001;158:1878–1883. doi: 10.1176/appi.ajp.158.11.1878. [DOI] [PubMed] [Google Scholar]
- Muhuri P, Gfroerer J. Substance use among women: Associations with pregnancy, parenting, and race/ethnicity. Maternal and Child Health Journal. 2008;13:376–385. doi: 10.1007/s10995-008-0375-8. Retrieved November 24, 2008, from http://www.springerlink.com/content/152552148rwx2241/ [DOI] [PubMed]
- National Center on Addiction and Substance Abuse. The formative years: Pathways to substance abuse among girls and young women ages 8–22. New York: Columbia University; 2003. [Google Scholar]
- Parker JS, Benson MJ. Parent-adolescent relations and adolescent functioning: Self-esteem, substance abuse, and delinquency. Adolescence. 2004;39:519–530. [PubMed] [Google Scholar]
- Perreira KM, Cortes KE. Race/ethnicity and nativity differences in alcohol and tobacco use during pregnancy. American Journal of Public Health. 2006;96:1629–1636. doi: 10.2105/AJPH.2004.056598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Sinha JW, Cnaan RA, Gelles RJ. Adolescent risk behaviors and religion: Findings from a national study. Journal of Adolescence. 2007;30:231–249. doi: 10.1016/j.adolescence.2006.02.005. [DOI] [PubMed] [Google Scholar]
- Steiger J. Structural model evaluation and modification: an interval estimation approach. Multivariate Behavioral Research. 1990;25:173–180. doi: 10.1207/s15327906mbr2502_4. [DOI] [PubMed] [Google Scholar]
- Suarez L, Felkner M, Brender J, Canfield M, Hendricks K. Maternal exposures to cigarette smoke, alcohol, and street drugs and neural tube defect occurrence in offspring. Maternal and Child Health Journal. 2008;12:394–401. doi: 10.1007/s10995-007-0251-y. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA) National Survey on Drug Use and Health. National and State Alcohol, Tobacco, and Other Drug Use; 2005. Retrieved April 19, 2007, from http://www.oas.samhsa.gov/nsduh/2k5nsduh/2k5Results.htm#TOC. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2006 national survey on drug use and health. 2007 Retrieved August 12, 2009 from http://www.drugabusestatistics.samhsa.gov/nsduh/2k6nsduh/2k6Results.cfm.
- Substance Abuse and Mental Health Services Administration, Office of Applied Studies. The NSUDH report: Alcohol use among pregnant women and recent mothers: 2002 to 2007. Rockville, MD: 2008. Sep 11, [Google Scholar]
- Sutherland I, Shepherd JP. Social dimensions of adolescent substance use. Addiction. 2001;96:445–458. doi: 10.1046/j.1360-0443.2001.9634458.x. [DOI] [PubMed] [Google Scholar]
- Tang ML, Bentler PM. Theory and method for constrained estimation in structural equation models with incomplete data. Computational Statistics & Data Analysis. 1998;27:257–270. [Google Scholar]
- Teagle SE, Brindis CD. Substance use among pregnant adolescents: A comparison of self-reported use and provider perception. Journal of Adolescent Health. 1998;22:229–238. doi: 10.1016/S1054-139X(97)00170-5. [DOI] [PubMed] [Google Scholar]
- Thomas C, Hypponen E, Power C. Obesity and type 2 diabetes risk in mid-adult life: The role of childhood adversity. Pediatrics. 2008;121:e1240–1249. doi: 10.1542/peds.2007-2403. [DOI] [PubMed] [Google Scholar]
- Wiemann CM, Berenson AB. Factors associated with recent and discontinued alcohol use by pregnant adolescents. Journal of Adolescent Health. 1998;22:417–423. doi: 10.1016/s1054-139x(97)00215-2. [DOI] [PubMed] [Google Scholar]
- Wills TA, Yaeger AM, Sandy JA. Buffering effect of religiosity for adolescent substance use. Psychology of Addictive Behaviors. 2003;17:24–31. doi: 10.1037/0893-164x.17.1.24. [DOI] [PubMed] [Google Scholar]
- Young SE, Corley RP, Stallings MC, Rhee SH, Crowley TJ, Hewitt JK. Substance use, abuse, and dependence in adolescence: Prevalence, symptom profiles and correlates. Drug and Alcohol Dependence. 2002;68:309–322. doi: 10.1016/s0376-8716(02)00225-9. [DOI] [PubMed] [Google Scholar]
- Zamboanga BL, Schwartz SJ, Hernandez Jarvis L, Van Tyne K. Acculturation and substance use among Hispanic early adolescents: Investigating the mediating roles of acculturative stress and self-esteem. Journal of Primary Prevention. 2009;30:315–333. doi: 10.1007/s10935-009-0182-z. [DOI] [PubMed] [Google Scholar]