Abstract
Background
Controversy exists regarding the outcome of THA after prior pelvic osteotomy.
Questions/purposes
We conducted a retrospective chart and radiographic review to obtain outcome measures for perioperative complications, acetabular and femoral component revisions, Harris hip score, and survivorship and compared these outcomes for patients presenting with developmental dysplasia of the hip treated surgically using THA with and without prior pelvic osteotomy.
Patients and Methods
We performed 103 primary THAs in 87 patients with osteoarthritis secondary to developmental dysplasia of the hip with a minimum 3-year followup. Previous pelvic osteotomy was performed in 52 hips (Salter, 40; Chiari, nine; Salter and Chiari, three), and 51 hips had no previous surgery (control group).
Results
The pelvic osteotomy group did not have higher rates of femoral or acetabular intraoperative fracture or dislocation compared with the control group. The overall revision rate was 28.8% in the pelvic osteotomy group compared with 19.6% in the control group. The revision rate for aseptic loosening was 23.1% in the pelvic osteotomy group compared with 17.6% in the control group. Harris hip scores (range, 20–87) were not compromised, and overall survivorship rates 8 years postoperatively were not different at any time between the pelvic osteotomy (83.3%) and control (88.4%) groups.
Conclusions
Prior pelvic osteotomy did not lead to a higher perioperative complication rate, higher revision rate, compromised Harris hip score, or shortened survivorship in eventual THA in developmental dysplasia of the hip.
Level of Evidence
Level III, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Developmental dysplasia of the hip (DDH) provides a considerable challenge for THA owing to anterolateral acetabular bone deficiency, proximal femoral malrotation, the presence of soft tissue contractures, and shortened lower extremity [10, 22]. THA for DDH is associated with increased complication rates [4, 8] owing to the presence of infection [7, 10, 20], dislocation [5, 8, 9], and nerve palsy [14, 26], resulting in worse outcomes compared with THA for primary osteoarthritis [4, 8].
Pelvic osteotomy (PO) in DDH should delay the requirement for THA and allow subsequent hip reconstruction with acceptably low complication rates and long-term survival [6, 17]. Salter [24] described a redirectional osteotomy of the acetabulum on the head of the femur, which, in effect, is achieved by varization, retroversion, and, if possible, medialization, to help improve the anterolateral deficiency and stabilize the hip mechanically to improve overall function. Chiari [2, 3] described a medial displacement osteotomy for increased coverage of the dysplastic hip. Excellent results were reported after these osteotomies, and they may delay the progression of secondary osteoarthritis until THA for salvage is required [1, 15, 17]. Although the number of Chiari osteotomies has decreased in recent years, a relatively large number of patients with previous PO, such as the Salter, are still encountered.
Despite the evidence that these POs may delay the progression of secondary osteoarthritis, the resulting altered anatomy of the pelvis and proximal femur may result in a THA that is more technically difficult [25]. Controversy remains on this point as some investigators have shown the possibility of triple innominate osteotomy (TIO) worsening the outcome of THA, whereas others reported a previous osteotomy does not compromise the results of THA if it is properly performed [12, 21, 23].
There exist relatively few published studies quantitatively investigating the outcomes of THA after PO [12, 18, 21, 23]. Prior studies generally have small study populations with limited periods of followup. Only one study examined a moderately large number of THA outcomes after PO using the Chiari technique [12], whereas no study exists assessing the outcome of THA after a previous Salter osteotomy. Moreover, the longest average followup time to date in the literature for THA after any osteotomy technique was 6.9 years. This paucity of information leaves the surgeon with little evidence-based guidance in optimizing patient care.
We, therefore, aimed to quantitatively assess perioperative complication rate, acetabular and femoral component revision rate, Harris hip score (HHS), and survivorship to compare the outcome of patients presenting with DDH treated surgically using THA with and without prior PO. This is the largest study to date with the longest followup time examining the effect on THA of prior PO.
Patients and Methods
This investigation was a retrospective chart and radiographic review of patients with a diagnosis of DDH comparing those with prior Salter or Chiari PO with those who did not have this procedure performed previously. The authors obtained institutional ethics board approval for the study.
From 1987 to 2002, the senior author (JPW) performed 182 primary THAs in 143 patients with osteoarthritis secondary to DDH. Patients were included who had a minimum 3-year followup after uncemented THA using a posterolateral approach. Sixty-eight hips were excluded for the following reasons. Fourteen were lost to followup owing to patient death, geographic move, or nonreturn to clinic for examination. Twenty hips were excluded because they had undergone ipsilateral knee arthroplasty. Twenty-six hips were excluded because they had undergone ipsilateral femoral osteotomy. Eight hips were excluded because the technique of the PO was not identified. To eliminate some of the variables in the study group, 11 hips additionally were excluded: four had cemented arthroplasties, six had very severe dysplasia graded as Crowe III or IV, and in one hip surgery was performed through an anterior surgical approach. Finally, the total number of exclusions was 79 hips (56 patients), leaving 103 hips (87 patients) eligible for the study.
All hips were divided into two groups (Table 1): those that had prior PO before THA (PO group) and those that did not (control group). Fifty-two hips (45 patients) had a previous PO, including Salter osteotomy (40 hips), Chiari osteotomy (nine hips), and Salter and Chiari osteotomy (three hips). Fifty-one hips (42 patients) comprised the control group. In the control group, only two patients had prior surgery of any kind on the affected hip; namely, one patient had adductor tenotomy and soft tissue release for early-onset arthritis and one patient had closed reduction of the hip as a child with subsequent development of avascular necrosis of the femoral head. The average age of patients at the time of THA was younger (p = 0.0006) in the PO group (41 years; range, 25–58 years) than in the control group (47 years; range, 27–66 years). The minimum followup after THA was 3 years (mean, 7.3 years; range, 3–15 years) in the PO group and 3 years (mean, 8.3 years; range, 3–17 years) in the control group. There was no difference in patient gender between the two groups (p = 0.926) or the distribution of Crowe I and II classifications [4] (p = 0.704). In the PO group, the mean interval from previous osteotomy to primary THA was 19.3 years (range, 1–40 years).
Table 1.
Patient and surgical details
| Variable | PO group | Control group | p Value |
|---|---|---|---|
| Number of hips | 52 | 51 | |
| Number of patients | 45 | 42 | |
| Male:female | 2:43 | 2:40 | 0.926 |
| Crowe classification | 0.704 | ||
| Class I | 48 (92.3%) | 46 (90.2%) | |
| Class II | 4 (7.7%) | 5 (9.8%) | |
| Age at THA (years)* | 41 (25–58) | 47 (27–66) | 0.0006 |
| Followup after THA (years)* | 7.3 (3–15) | 8.5 (3–17) | 0.203 |
| Osteotomy to primary THA (years)* | |||
| Total | 19.3 (1–40) | ||
| Chiari | 7.1 (1–20) | ||
| Salter | 22.6 (4–40) | ||
| Chiari plus Salter | 12.7 (3–18) |
* Values are expressed as means, with ranges in parentheses; PO = pelvic osteotomy.
Patients were placed in the lateral decubitus position and the affected extremity prepared with Betadine® (Purdue Products L.P., Stamford, CT, USA) and draped free. All patients, with the exception of one, had a posterolateral approach with standard exposure, including transsection of the piriformis tendon and release of the proximal portion of the gluteus maximus tendon. After capsulotomy, a Steinmann pin was inserted above the hip into the lateral wall of the pelvis, a mark made on the greater trochanter, and the interval measured for later reference for leg length. A right angle osteotomy of the femoral neck was performed to accommodate the femoral component. The acetabulum thereby was exposed and the labrum excised. A Capener gouge was used to remove the subchondral bone and the center of the acetabulum, and then conical reamers of increasing diameters were used to shape the acetabulum to receive the truncated cone-shaped acetabular component. When there was uniform contact between the reamer and the acetabular bone, a cup of that size was selected. In the early part of the series, a screw ring acetabular component was used with standard polyethylene; later in the series, a macrotextured beaded cup was impacted into position and matched to a polyethylene liner with a 10° shelf. On the femoral side, a reamed broached system was used with sequential reaming until uniform cortical content was achieved. A broach matching the size of that reamer then was used to prepare the cancellous bone of the proximal femur to receive the femoral component, which had proximal fins to control rotation. The hip could be trialed from the broach to determine leg length and stability. Acetabular components less than 50 mm in diameter had polyethylene liners of 22-mm inside diameter only; acetabular components greater than 50 mm in diameter could receive either a 22-mm or 28-mm outside diameter polyethylene component.
Six types of cementless prostheses were used, but the distribution of the different types of acetabular and femoral components was virtually identical between the groups (Table 2). For the PO group, the THA femoral head sizes used were either 22 mm in diameter (23 hips) or 28 mm in diameter (29 hips). Similarly, for the control group, the femoral heads were either 22 mm in diameter (24 hips) or 28 mm in diameter (27 hips). No titanium heads were used.
Table 2.
Distribution of types of hip prostheses used in the study
| Prosthesis type | PO group | Control group | ||
|---|---|---|---|---|
| Acetabular | Femoral | Acetabular | Femoral | |
| St Michael’s Hospital | 33 | 33 | 33 | 33 |
| Reflection (Smith and Nephew, Inc, Memphis, TN) | 15 | 0 | 14 | 0 |
| Transcend (Wright Medical Technology, Inc, Arlington, TN) | 3 | 3 | 3 | 3 |
| Secur-Fit (Stryker Orthopaedics, Mahwah, NJ) | 1 | 0 | 1 | 0 |
| Synergy (Smith and Nephew, Inc, Memphis, TN) | 0 | 13 | 0 | 11 |
| Echelon (Smith and Nephew, Inc, Memphis, TN) | 0 | 3 | 0 | 4 |
No titanium heads were used in PO or control groups; PO = pelvic osteotomy.
Crowe classification of hip dysplasia was determined from radiographs [4]. Intraoperative or postoperative complications were recorded, namely, fracture, hip dislocation, infection, deep venous thrombosis, and nerve damage. Revision rates were calculated for each group. Time until revision THA and cause of revision were recorded. Clinical measurements for computing HHS [11, 27] were obtained 6 weeks preoperatively, 1 year postoperatively, and at the latest followup. Pain and functional scores were extracted for analysis (Table 3). For survivorship analysis, failure of the component was defined as revision of the component for any reason or placement on a waiting list for revision. Two research fellows (KT, NA) who were not involved in the surgery conducted independent observations of different radiographs and extracted data from patient charts.
Table 3.
Complications and revision surgery
| Variable | PO group | Control group | p Value |
|---|---|---|---|
| Number of complications | 7 (13.5%) | 6 (11.8%) | 0.795 |
| Fracture | 1 (1.9%) | 3 (5.9%) | 0.298 |
| Dislocation | 4 (7.7%) | 2 (3.9%) | 0.414 |
| Other | 3 (5.8%) | 1 (2%) | 0.261 |
| Infection | 2 (3.8%) | 0 (0%) | |
| Deep venous thrombosis | 0 (0%) | 1 (2%) | |
| Nerve damage | 1 (1.9%) | 0 (0%) | |
| Number of revisions | 15 (28.8%) | 10 (19.6%) | 0.274 |
| Acetabulum | 13 (25.0%) | 9 (17.6%) | |
| Femur | 0 (0%) | 0 (0%) | |
| Acetabulum and femur | 2 (3.8%) | 1 (2%) | |
| Primary to revision (years)* | 8.2 (3–14) | 9.1 (5–14) | 0.464 |
| Cause for revision | 15 (28.8%) | 10 (19.6%) | 0.581 |
| Loosening | 12 (23.1%) | 9 (17.6%) | |
| Dislocation | 2 (3.8%) | 1 (2%) | |
| Infection | 1 (1.9%) | 0 (0%) |
* Values are expressed as means, with ranges in parentheses; PO = pelvic osteotomy.
The Mann-Whitney U test was performed to evaluate differences between PO and control groups for complication rates and revision rates. HHS statistical comparisons were performed using one-way ANOVA. For complication rates, revision rates, and HHS values, differences within groups were analyzed using paired t tests as appropriate. Survivorship analysis was performed using the Kaplan-Meier [13] method combined with the log-rank test in which revision for any reason was the end point for each group. For all statistical tests above, a p value less than 0.05 was taken as significant.
A post hoc power analysis was performed to determine if there were enough patients in the PO and control groups to be able to detect all statistical differences that actually exist between them, ie, to avoid Type II error. For this power analysis, a two-sided Z test with pooled variance was used, and the revision rate was chosen as the parameter of comparison. This power analysis yielded a value of 19.4% for the study with the revision rate chosen as the parameter of comparison between the PO and control groups. Usually, a good study design is considered to be one in which there is an adequate number of patients per group yielding a power of at least 80%. In the current investigation, however, 340 patients per group would have been required to achieve 80% power, which was not feasible given the scope of the investigation.
Results
There was no difference (p = 0.795) in overall complication rate for the PO (13.5%) and control (11.8%) groups (Table 3). The numbers of intraoperative fractures were similar (p = 0.298) between the control group (three hips; one acetabular fracture, two undisplaced calcar fractures) and the PO group (one hip; femoral fracture distal to lesser trochanter). The dislocation rate also was similar (p = 0.414) (PO group: four hips [Salter, three; Chiari, one]; control group: two hips). Early revision was required for acetabulum component malposition in one hip (control group) within a few months. Late revision was required for recurrent dislocations in two hips in the PO group. Two patients in the PO group had infections. One patient had a deep infection and underwent revision of both components at 5 years, whereas the other had a superficial infection. One patient in the PO group had severe axonal injury to the left sciatic nerve with no stretch component to the injury after THA, manifesting as profound foot drop on awakening from surgery and at subsequent followups. However, the patient recovered fully, with no residual functional deficit noted at the 7-year followup.
There was no difference in acetabular revision rates between the groups. Twenty-five hips had revision arthroplasties. At the time this study was completed, no patients were waiting for a revision owing to aseptic loosening. The PO group had 15 total revisions (acetabular, 13; acetabular and femoral, two), whereas the control group had 10 revisions (acetabular, nine; acetabular and femoral, one) (p = 0.274) (Table 3). The PO group had 12 acetabular components (Salter, nine; Chiari, three) revised for aseptic loosening or wear, two hips (Salter) for dislocation, and one hip (Salter) for infection. In the control group, seven hips were revised for definite loosening, two hips for excessive polyethylene wear, and one hip for dislocation. The femoral revision rates were the same. The PO group had one femoral stem revised for aseptic loosening (1.9%) and one femoral stem for infection (1.9%), whereas the control group had one hip (2%) revised for aseptic loosening. In all three cases of femoral revision, the corresponding acetabular components also needed to be revised for the same reason.
One year after THA and at last followup, the total HHS, pain, and function scores in the PO and control groups improved (p < 0.05) compared with scores before THA (Table 4). However, there was no difference (0.438 < p < 0.998) in clinical results between PO and control groups before THA, after THA, or at the last followup (Table 4).
Table 4.
HHS results
| Time | Domain | HHS (points) | p Value (PO vs control) | |
|---|---|---|---|---|
| PO | Control | |||
| Before THA | Total | 51 | 49 | 0.627 |
| After THA (1 year) | 85* | 87* | 0.499 | |
| Latest followup | 85* | 87* | 0.438 | |
| Before THA | Pain | 20 | 20 | 0.998 |
| After THA (1 year) | 40* | 40* | 0.531 | |
| Latest followup | 40* | 41* | 0.493 | |
| Before THA | Function | 24 | 24 | 0.829 |
| After THA (1 year) | 38* | 38* | 0.689 | |
| Latest followup | 38* | 37* | 0.720 | |
* p < 0.05 (versus before THA); PO = pelvic osteotomy; HHS = Harris hip score.
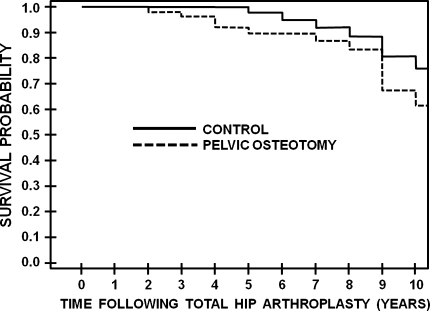
Survivorship analysis using Kaplan-Meier curves revealed no difference between the PO and control groups (Fig. 1). The 8-year overall THA survival rate against revision of either the acetabular and/or femoral components for any reason was 83.3% ± 5.9% (95% confidence interval) for the PO group and 88.4% ± 5.5% (95% confidence interval) for the control group (p = 0.091). More specifically, the 8-year survival rate of the acetabular cup for revision for any reason was 85.3% ± 5.7% (95% confidence interval) for the PO group and 88.4% ± 5.5% (95% confidence interval) for the control group (p = 0.143). The 8-year survival rate of the femoral stem for revision for any reason was 94.8% ± 3.6% (95% confidence interval) for the PO group and 100% ± 0% (95% confidence interval) for the control group (p = 0.249).
Fig. 1.
Kaplan-Meier cumulative survivorship curves compare the probability of not revising the acetabular and/or femoral component for any reason between the PO and control groups. The differences were not significant by the log-rank test (p = 0.091).
Discussion
We evaluated the effect of previous PO on the outcome of THA performed for degenerative arthritis secondary to DDH compared with THA without prior PO. A history of having a prior Salter or Chiari osteotomy resulted in similar outcomes, including complication rate, revision rate, HHS, or survivorship compared with outcomes for a population of patients undergoing THA without prior surgery.
Several limitations should be noted. First, patient data were obtained from the clinical practice of only one surgeon. Thus, the generalizability of the findings may be hindered, future work requiring additional data from multiple centers. Even so, this is the largest series to date reported in the literature regarding THA after Salter and Chiari osteotomy. Second, because Chiari osteotomy can change the biomechanical features of the hip and alter the success of later THA [18], followup times of more than 10 years may be required to fully determine its clinical success [16, 19, 28]. Moreover, the retrospective nature of the study for the period of 1987 to 2002 limited our average followup to 8 years, although this is the longest to date in the literature. Third, there was a good deal of heterogeneity in the final cohort with regard to the degree of DDH and the variety of prostheses used. These factors are beyond the surgeon’s control but are dependent on patients’ conditions and needs. Fourth, the HHS system as a clinical outcome measure does not consider how the score is affected by individual patient differences, such as age, health, or personal issues. Even so, the validity of the HHS system has been assessed systematically against other outcome scores with good results [27]. Fifth, the failure rate was high in both groups but higher in the group that had a previous PO for several reasons. The mean age of these patients was younger, as they were almost uniformly young active patients. Also, we used first-generation cementless acetabular implants. Some of these were screw ring implants with an average survival of approximately 10 years before revision, whereas the remainder were a macrotextured conical-shaped implant usually placed without screws. In both types of implants, bone ingrowth proved to be uncertain, probably leading to the high failure rate. The same macrotexture was on the femoral components, and these proved to be exceptionally durable with greater than 98% survival rate at 10 to 15 years, but the same unfortunately was not true for the acetabular component. Moreover, approximately 50% of the patients received 22-mm cobalt-chrome heads. Thus, the small diameter head coupled with a small diameter cup and relatively thin polyethylene, while producing substantial linear wear, also might have contributed to the high failure rate of the acetabular components. Sixth, the correlation was not examined between patient activity level during employment, exercise, or hobbies and arthroplasty failure rates. This would have required the use of a separate validated questionnaire to measure the intensity, frequency, duration, and nature of patient employment, exercise, and/or hobbies. This was beyond the scope of our study. Even so, the HHS function score, as presented currently, is an implicit indicator of before and after THA activity level. Seventh, the post hoc power analysis yielded a value of 19.4%, indicating our study was unable to detect all the statistical differences actually present. However, the required 340 patients per group to achieve an 80% power were not feasible given the scope and nature of our review. Even so, our study offers the largest patient series regarding THA after Salter and Chiari osteotomy. Finally, intraobserver and interobserver reliability were not assessed regarding the outcome measures obtained independently by two of the authors (KT, NA) from radiographs. Any substantial disagreements, however, were adjudicated by the Fellows through mutual consultation, and a final value for the particular radiographic parameter was determined.
Total complications in our study showed no difference between the PO (13.5%) and control (11.5%) groups. An earlier investigation showed lower perioperative complications, with one of 28 hips (3.5%) having THA after previous Chiari osteotomy compared with five of 50 hips (10%) in a matched control group [12]. This may be partly attributable to our longer average followup (8 years) compared with the earlier study (5 years), which may have allowed complications time to develop and be detected.
Our revision data showed 25 total revision surgeries. However, there was no difference in isolated acetabular (PO, 25.0%; control, 17.6%), isolated femoral (PO, 0%; control, 0%), or combined acetabular plus femoral (PO, 3.8%; control, 1.9%) revisions. Hashemi-Nejad et al. reported revision of acetabular components in one of 28 hips (3.6%) having THA after previous Chiari osteotomy compared with six of 50 hips (12%) in a diagnosis-matched control group [12]. Other investigations using TIO and Ganz osteotomies, respectively, showed one (7.7%) postTHA revision of 13 hips attributable to dislocation and two (4.9%) postTHA revisions in 41 patients attributable to aseptic acetabular (one hip) and femoral (one hip) loosening [21, 23].
Total, pain, and function outcomes (HHS) showed prior PO in patients did not compromise THA success when compared with patients without prior PO at 1-year or latest followup. Patients at both followup times showed improvement in total, pain, and function (HHS) scores compared with before THA. This improvement of total HHS for PO (before THA, 51; last followup, 85) and control (before THA, 49; last followup, 87) groups was similar to improvement reported in a previous series on 47 hips requiring autogenous grafting for severe acetabular deficiency, which showed a total HHS of 46 before THA and 74 after THA [9]. Similarly, a study of 13 hips having THA after TIO showed increased total HHS after TIO (before THA, 40; after THA, 76) and nonosteotomized controls (before THA, 28; after THA, 88), although after THA, control subjects did better in the total and pain HHS components [23]. Thus, patient quality of life after THA can be improved to some degree regardless of whether they have a prior osteotomy.
Overall survival rates of THA in our study were satisfactory at a mean followup of nearly 8 years (83.3% [PO] compared with 88.4% [control]). Our results for individual acetabular and femoral component survival rates for the PO and control groups (range, 85.3%–100%) are comparable to those of a previous study, showing similar values for the femoral (after Chiari, 97%; control, 96%) and acetabular (after Chiari, 89%; control, 84%) components with an average followup of 5 years [12].
We reported the outcome of uncemented THA with and without prior PO, having the longest followup and the largest study size published to date. This is also the first series reporting on THA outcome after Salter osteotomy. Patients undergoing THA who have had prior Chiari and Salter PO had no differences in complication rate, revision rate, HHS, or survivorship compared with patients without prior PO. We speculate some patients with prior PO may show improved results after THA, as positioning the acetabular component in a more hemispheric socket (achieved after osteotomy) may be easier than a grossly shallow socket. This, however, would need to be observed conclusively in a future investigation.
Acknowledgments
We thank Jun Saito, MD, PhD, and Kazuhiko Inoue, MD, PhD, for valuable help during this study. We recognize Kerry Ann Griffith-Cunningham and Jane Morton, RN (Orthopaedics, St Michael’s Hospital) for their assistance in obtaining and keeping records of patient data. The assistance of Abdulaati Mahfud, MD (Martin Orthopaedic Biomechanics Lab, St Michael’s Hospital) in tracking down a few key references also is appreciated. Finally, we acknowledge Muhammad Mamdani, PharmD, MPH, MA, and Rosane Nisenbaum, PhD (Applied Health Research Centre, St Michael’s Hospital) for their consultation and work on some statistical matters.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Bohm P, Brzuske A. Salter innominate osteotomy for the treatment of development dysplasia of the hip in children: results of seventy-three consecutive osteotomies after twenty-six to thirty-five years of follow-up. J Bone Joint Surg Am. 2002;84:178–186. doi: 10.1302/0301-620X.84B4.12495. [DOI] [PubMed] [Google Scholar]
- 2.Chiari K. [Results of pelvic osteotomy as of the shelf method acetabular roof plastic] [in German] Z Orthop Ihre Grenzgeb. 1955;87:14–26. [PubMed] [Google Scholar]
- 3.Chiari K. Medial displacement osteotomy of the pelvis. Clin Orthop Relat Res. 1974;98:55–71. doi: 10.1097/00003086-197401000-00008. [DOI] [PubMed] [Google Scholar]
- 4.Crowe JF, Mani VJ, Ranawat CS. Total hip replacement in congenital dislocation and dysplasia of the hip. J Bone Joint Surg Am. 1979;61:15–23. [PubMed] [Google Scholar]
- 5.Fredin H, Sanzen L, Sigurdsson B, Unander-Scharin L. Total hip arthroplasty in high congenital dislocation: 21 hips with a minimum five-year follow-up. J Bone Joint Surg Br. 1991;73:430–433. doi: 10.1302/0301-620X.73B3.1670444. [DOI] [PubMed] [Google Scholar]
- 6.Ganz R, Klaue K, Vinh TS, Mast JW. A new periacetabular osteotomy for the treatment of hip dysplasias: technique and preliminary results. Clin Orthop Relat Res. 1988;232:26–36. [PubMed] [Google Scholar]
- 7.Garcia-Cimbrelo E, Munuera L. Low friction arthroplasty in severe acetabular dysplasia. J Arthroplasty. 1993;8:459–469. doi: 10.1016/S0883-5403(06)80211-1. [DOI] [PubMed] [Google Scholar]
- 8.Garvin KL, Bowen MK, Salvati EA, Ranawat CS. Long-term results of total hip arthroplasty in congenital dislocation and dysplasia of the hip: a follow-up note. J Bone Joint Surg Am. 1991;73:1348–1354. [PubMed] [Google Scholar]
- 9.Gerber SD, Harris WH. Femoral head autografting to augment acetabular deficiency in patients requiring total hip replacement: a minimum five-year and an average seven-year followup study. J Bone Joint Surg Am. 1986;68:1241–1248. [PubMed] [Google Scholar]
- 10.Gill TJ, Sledge JB, Muller ME. Total hip arthroplasty with use of an acetabular reinforcement ring in patients who have congenital dysplasia of the hip: results at five to fifteen years. J Bone Joint Surg Am. 1998;80:969–979. doi: 10.1302/0301-620X.80B6.8658. [DOI] [PubMed] [Google Scholar]
- 11.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737–755. [PubMed] [Google Scholar]
- 12.Hashemi-Nejad A, Haddad FS, Tong KM, Muirhead-Allwood SK, Catterall A. Does Chiari osteotomy compromise subsequent total hip arthroplasty? J Arthroplasty. 2002;17:731–739. doi: 10.1054/arth.2002.31974. [DOI] [PubMed] [Google Scholar]
- 13.Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53:457–481. doi: 10.2307/2281868. [DOI] [Google Scholar]
- 14.Lewallen DG. Neurovascular injury associated with hip arthroplasty. Instr Course Lect. 1998;47:275–283. [PubMed] [Google Scholar]
- 15.Macnicol MF, Lo HK, Yong KF. Pelvic remodelling after the Chiari osteotomy: a long-term review. J Bone Joint Surg Br. 2004;86:648–654. doi: 10.1302/0301-620X.86B5.14653. [DOI] [PubMed] [Google Scholar]
- 16.Mellerowicz HH, Matussek J, Baum C. Long-term results of Salter and Chiari hip osteotomies in developmental hip dysplasia: a survey of over 10 years follow-up with a new hip evaluation score. Arch Orthop Trauma Surg. 1998;117:222–227. doi: 10.1007/s004020050233. [DOI] [PubMed] [Google Scholar]
- 17.Millis MB, Murphy SB, Poss R. Osteotomies about the hip for the prevention and treatment of osteoarthrosis. Instr Course Lect. 1996;45:209–226. [PubMed] [Google Scholar]
- 18.Minoda Y, Kadowaki T, Kim M. Total hip arthroplasty of dysplastic hip after previous Chiari pelvic osteotomy. Arch Orthop Trauma Surg. 2006;126:394–400. doi: 10.1007/s00402-006-0141-6. [DOI] [PubMed] [Google Scholar]
- 19.Nakano S, Nishisyo T, Hamada D, Kosaka H, Yukata K, Oba K, Kawasaki Y, Miyoshi H, Egawa H, Kinoshita I, Yasui N. Treatment of dysplastic osteoarthritis with labral tear by Chiari pelvic osteotomy: outcomes after more than 10 years follow-up. Arch Orthop Trauma Surg. 2008;128:103–109. doi: 10.1007/s00402-007-0465-x. [DOI] [PubMed] [Google Scholar]
- 20.Okamoto T, Inao S, Gotoh E, Ando M. Primary Charnley total hip arthroplasty for congenital dysplasia: effect of improved techniques of cementing. J Bone Joint Surg Br. 1997;79:83–86. doi: 10.1302/0301-620X.79B1.6771. [DOI] [PubMed] [Google Scholar]
- 21.Parvizi J, Burmeister H, Ganz R. Previous Bernese periacetabular osteotomy does not compromise the results of total hip arthroplasty. Clin Orthop Relat Res. 2004;423:118–122. doi: 10.1097/01.blo.0000128287.98083.63. [DOI] [PubMed] [Google Scholar]
- 22.Perka C, Fisher U, Taylor WR, Matziolis G. Development hip dysplasia treated with total hip arthroplasty with a straight stem and a threaded cup. J Bone Joint Surg Am. 2004;86:312–319. doi: 10.2106/00004623-200402000-00014. [DOI] [PubMed] [Google Scholar]
- 23.Peters CL, Beck M, Dunn HK. Total hip arthroplasty in young adults after failed triple innominate osteotomy. J Arthroplasty. 2001;16:188–195. doi: 10.1054/arth.2001.20903. [DOI] [PubMed] [Google Scholar]
- 24.Salter RB. Innominate osteotomy in the treatment of congenital dislocation and subluxation of the hip. J Bone Joint Surg Br. 1961;43:518–539. [PubMed] [Google Scholar]
- 25.Scher MA, Jakim I. Combined intertrochanteric and Chiari pelvic osteotomies for hip dysplasia. J Bone Joint Surg Br. 1991;73:626–631. doi: 10.1302/0301-620X.73B4.2071647. [DOI] [PubMed] [Google Scholar]
- 26.Schmalzried TP, Amstutz HC, Dorey FJ. Nerve palsy associated with total hip replacement: risk factors and prognosis. J Bone Joint Surg Am. 1991;73:1074–1080. [PubMed] [Google Scholar]
- 27.Soderman P, Malchau H. Is the Harris hip score system useful to study the outcome of total hip replacement? Clin Orthop Relat Res. 2001;384:189–197. doi: 10.1097/00003086-200103000-00022. [DOI] [PubMed] [Google Scholar]
- 28.Yanagimoto S, Hotta H, Izumida R, Sakamaki T. Long-term results of Chiari pelvic osteotomy in patients with developmental dysplasia of the hip: indications for Chiari pelvic osteotomy according to disease stage and femoral head shape. J Orthop Sci. 2005;10:557–563. doi: 10.1007/s00776-005-0942-4. [DOI] [PubMed] [Google Scholar]