Abstract
Background
A dramatic increase in the demand for TKA is expected. The current burden of revision TKA is well known but the incidence and etiology of nonrevision reoperations after primary TKA is not.
Questions/purposes
We determined the rate, reason, timing, and predictors of nonrevision reoperation after TKA.
Methods
Using our institutional joint arthroplasty database, we identified 10,188 TKA performed on 7,613 patients between April 2000 and March 2008. A nonrevision reoperation was defined as any procedure requiring anesthetic in which components with bony interfaces were not removed or exchanged. Procedures after revision TKA were excluded. Potential risk factors investigated included age, gender, laterality, and simultaneous bilateral versus staged bilateral versus unilateral TKA. The minimum followup was 1 year (median, 4.1 years; range, 1.1 to 9.1 years).
Results
Three hundred fifty-three patients of 7,613 (4.6%) underwent 434 nonrevision reoperations on 384 of 10,188 (3.8%) knees. The most common indication for nonrevision reoperation was stiffness (58%; 252 of 434), followed by patellar clunk (12%; 53), infection (12%; 52), wound revision (6%; 26), hematoma (4.4%; 19), among others. The median time to reoperation was 74.5 days (range, 1–3058 days) but varied widely. Younger patients and those with unilateral TKA were more likely to have a nonrevision reoperation.
Conclusions
The majority of nonrevision reoperations are performed for stiffness. Patellar clunk and infection also result in a large number of nonrevision reoperations. In weighing the future economic and workforce burden of TKA, nonrevision reoperations need to be acknowledged, and preventive measures need to be implemented.
Level of Evidence
Level II, prognostic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
The future demand for TKA is projected to increase substantially over the next few years [10]. Coupled with these projections, the demand for TKA is expected to increase in the face of a decreasing joint surgeon population [5]. Despite adequate survivorship and high functional outcomes, complications after TKA can and do occur, leading to delayed discharge, readmission, reoperation, and revision of the prosthesis. To fully understand the current and future burden of TKA, it is necessary to establish the incidence of orthopaedic complications resulting in any additional treatment.
Second to revisions, reoperations in which the prosthesis is retained may create a large burden on the orthopaedic society. Reoperations may include manipulation under anesthesia (MUA), irrigation and débridement (I&D), arthroscopy, open reduction internal fixation (ORIF), and others. While incidences of individual complications requiring such reoperations have been reported [1, 2, 4, 6, 7, 9, 11, 12, 14, 21, 25, 29] (Table 1), the comprehensive profile of indications for nonrevision reoperation (NRR) following primary TKA is unreported. Knowledge of the incidence, indication, timing, and predictors of NRR will allow for an efficient use of resources in targeting the most common causes for reoperation, continuing research in preventing these complications, and identifying patients at the greatest risk so preventative measures may be taken.
Table 1.
Published rate of individual NRR after TKA
| Publication | Indication | Reoperation | Current study |
|---|---|---|---|
| Dajani et al. [1] | Patellar Clunk | 15/21546 (0.06%) | 49/10188 (0.5%) |
| Fukunaga et al. [2] | 5/121 (4.9%) | ||
| Hozack et al. [4] | 3 (Case Report) | ||
| Ip et al. [6] | 1/80 (1.25%) | ||
| Koh et al. [9] | 12 (Case Report) | ||
| Lonner et al. [12] | 6/150 (4.0%) | ||
| Kim J et al. [7] | Stiffness | 13/1000 (1.3%) | 238/10188 (2.3%) |
| Mauerhan et al. [14] | 81/745 (10.9%) | ||
| Parvizi et al. [21] | 112/10000 (1.2%) | ||
| Rubinstein and DeHaan [25] | 37/800 (4.6%) | ||
| Kurtz et al. [11] | Infection | 1080/69663 (1.6%) | 48/10188 (0.5%) |
| Webb et al. [29] | 12/483 (2.5%) |
NRR = nonrevision reoperation; TKA = total knee arthroplasty.
This study was undertaken to identify (1) the incidence of NRR after primary TKA; (2) the indications for NRR; (3) the timing of such procedures after primary TKA; and (4) demographic and/or surgical risk factors predisposing for NRR.
Patients and Methods
We retrospectively identified from our institutional joint arthroplasty registry 7613 patients who underwent 10,188 primary TKAs from April 2000 to March 2008. Procedure type in the registry is stored by Current Procedural Terminology (CPT) codes. Registry data also contain date of birth, gender, laterality, and date of surgery. A NRR was defined as any procedure requiring a minimum of regional anesthesia without the resection or exchange of components in contact with a bony interface (femoral, tibial, or patellar components) in which primary TKA was the index arthroplasty. We used 75 CPT codes associated with NRR, including MUA, revision of one component, I&D, arthroscopy, ORIF, arthrotomy, fasciotomy, wound revision, decompression, and closed reduction under anesthesia, to query the registry and identify those patients undergoing a NRR. Sixty-five of the CPT codes returned patients, but only 15 of them (Table 2) provided patients who underwent NRR with primary TKA as the index knee arthroplasty. Medical records were reviewed to confirm the registry data for the NRR patients. This study evaluated the incidence of NRR after primary TKA only and patients undergoing revision TKA were excluded. We required a minimum 1-year followup for patients who had surgery (median, 4.1 years; range, 1.1 to 9.1 years). Institutional Review Board approval was acquired before initiation of this research.
Table 2.
CPT codes, with associated procedure descriptions, identifying nonrevision reoperations after TKA
| CPT code | Procedure |
|---|---|
| 10060 | Incision and drainage abscess, simple/single |
| 10180 | Incision and drainage complex postoperative wound infection |
| 12021 | Treatment superficial wound dehiscence with packing |
| 13160 | Secondary closure wound dehiscence, extensive |
| 27244 | Open treatment inter/per/subtrochanteric fracture |
| 27301 | Incise/drain abscess/hematoma thigh/knee |
| 27310 | Arthrotomy with exploration, knee |
| 27506 | Open treatment femoral shaft fracture with implant |
| 27507 | Open treatment femoral shaft fracture with plate-screws |
| 27570 | Manipulate knee joint, general anesthesia |
| 27894 | Decompression fasciotomy, anterior-lateral-posterior compartments |
| 29874 | Knee arthroscopy/remove loose body |
| 29875 | Knee arthroscopy/synovectomy, limited |
| 29876 | Knee arthroscopy/synovectomy, major, 2 components |
| 29877 | Knee arthroscopy/débridement/chondroplasty |
| 27486 | Revision of TKA, with or without allograft, 1 component |
CPT = current procedural terminology.
Indication for reoperation, laterality, components exchanged, attending surgeon, age, gender, unilateral versus bilateral, date of arthroplasty, and date of reoperation were collected from the preoperative dictations, operative report, and postoperative course from the medical records. Indications were categorized into stiffness, patellar clunk, infection, hematoma, delayed wound healing, periprosthetic fracture, compartment syndrome, synovitis, osteophytes, loose body, patellofemoral impingement, and poor patellar tracking. For reporting of results, “other” refers to the latter five indications.
Time to reoperation was the difference between the confirmed dates of surgery for primary TKA to NRR. Median days to reoperation are reported to provide a more accurate representation of the distribution of the timing of NRR. The incidence of NRR is reported as a function of days to reoperation as well.
To assess age and gender as predisposing factors for NRR, two cohorts were formed from the primary TKA population: those patients included in the NRR incidence analysis (NRR group) and all others (control group). Age was calculated from the date of first primary TKA performed at our institution. The patients had an average age of 65 years and 4849 of 7613 (64%) were female (Table 3). To assess the timing of multiple arthroplasties and laterality as a predisposing factor for NRR, we compared rate of NRR per side and for simultaneous bilateral, staged bilateral or unilateral TKA. A bilateral TKA was considered staged if both knees were replaced on different days within 3 months of each other. Forty-eight of 7613 (0.6%) patients had 96 of 10,188 (0.9%) knees replaced in a staged bilateral fashion, 1887 (25%) patients had 3774 (37%) knees replaced bilaterally in one stage, and 5678 (75%) patients had 6318 (62%) knees replaced unilaterally. Patients undergoing simultaneous bilateral TKA (63.2 years; 95% CI: 62.9–63.5) were younger than patients undergoing both staged bilateral (66.8 years; 95% CI: 64.8–68.8) and unilateral (66.2 years; 95% CI: 65.9–66.4) TKA (p = 0.0073 and p < 0.001, respectively). In total, 5178 (51%) TKAs were on the right knee and 5010 (49%) were on the left knee.
Table 3.
Summary of the TKA patient population and those patients undergoing NRR, separated further by indication
| Variable | All TKAs | At least one NRR | Stiffness | Patellar clunk | Infection | Wound | Hematoma | Periprosthetic fracture | Compartment syndrome | Other |
|---|---|---|---|---|---|---|---|---|---|---|
| Number of procedures | NA | 434 | 252 | 53 | 52 | 26 | 19 | 15 | 11 | 6 |
| Number of knees (% of TKAs) | 10,188 | 384 (3.77%) | 238 (2.34%) | 49 (0.48%) | 48 (0.47%) | 24 (0.24%) | 18 (0.17%) | 14 (0.14%) | 4 (0.04%) | 6 (0.08%) |
| Number of patients (% of TKAs) | 7613 | 353 (4.64%) | 218 (2.86%) | 44 (0.58%) | 45 (0.59%) | 24 (0.32%) | 18 (0.24%) | 13 (1.7%) | 4 (0.05%) | 6 (0.11%) |
| Age (years)* | 65.44 ± 0.23 | 60.38 ± 1.11 | 58.3 ± 1.41 | 64.77 ± 3.06 | 61.66 ± 3.3 | 66.25 ± 3.81 | 59.55 ± 5.47 | 67.92 ± 4.32 | 69.5 ± 6.51 | 55.5 ± 8.88 |
| Number of females (% of patients) | 4849 (63.39%) | 225 (63.74%) | 141 (64.68%) | 32 (72.73%) | 33 (73.33%) | 10 (41.67%) | 8 (44.44%) | 9 (69.23%) | 3 (75.00%) | 4 (66.6%) |
| Number of right knees (% of knees) | 5178 (50.82%) | 207 (53.91%) | 118 (49.58%) | 30 (61.22%) | 29 (60.42%) | 16 (66.67%) | 10 (55.56%) | 7 (50.00%) | 1 (25.00%) | 5 (83.33%) |
| Unilateral TKA | ||||||||||
| Number of procedures | NA | 328 | 198 | 41 | 37 | 15 | 15 | 9 | 8 | 5 |
| Number of knees | 6318 | 297 (4.70%) | 191 (3.02%) | 37 (0.59%) | 36 (0.57%) | 14 (0.22%) | 14 (0.22%) | 9 (0.14%) | 3 (0.05%) | 5 (0.08%) |
| Number of patients | 5678 | 291 (5.13%) | 190 (3.35%) | 35 (0.62%) | 35 (0.62%) | 14 (0.25%) | 14 (0.25%) | 9 (0.16%) | 3 (0.05%) | 5(0.09%) |
| Simultaneous bilateral TKA | ||||||||||
| Number of procedures | NA | 105 | 54 | 12 | 15 | 10 | 4 | 6 | 3 | 1 |
| Number of knees | 3774 | 86 (2.28%) | 47 (1.25%) | 12 (0.32%) | 12 (0.32%) | 9 (0.24%) | 4 (0.11%) | 5 (0.13%) | 1 (0.03%) | 1 (0.03%) |
| Number of patients | 1887 | 61 (3.23%) | 28 (1.48%) | 9 (0.48%) | 10 (0.53%) | 9 (0.48%) | 4 (0.22%) | 4 (0.21%) | 1 (0.05%) | 1 (0.05%) |
| Staged bilateral TKA | ||||||||||
| Number of procedures | NA | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 |
| Number of knees | 96 | 1 (1.04%) | 0 | 0 | 0 | 1 (1.04%) | 0 | 0 | 0 | 0 |
| Number of patients | 48 | 1 (2.08%) | 0 | 0 | 0 | 1 (2.08%) | 0 | 0 | 0 | 0 |
* Values are expressed as mean ± 95% confidence interval; NRR = nonrevision reoperation; NA = not applicable.
Descriptive statistics were utilized to portray the incidence of reoperation, time to reoperation, and proportions of each indication. In order to assess any surgical or demographic variations between the NRR group and control group, univariate statistics were used. Differences were assessed in the NRR and control groups for age, gender, and unilateral versus bilateral TKA. Differences in the continuous variable (age), were assessed with the Student’s t-test. Differences in categorical variables (gender and number of joints), were assessed with Chi-square test. Ninety-five percent confidence intervals (CI) were calculated with an alpha level of 0.05.
Results
Three hundred and fifty-three (4.6%; 353/7613) patients underwent a reoperation in which the original components were maintained. These 353 patients had a NRR on 384 of 10,188 (3.8%) knees and underwent a total of 434 procedures. The burden of NRR per primary TKA is 4.3% (434/10,188).
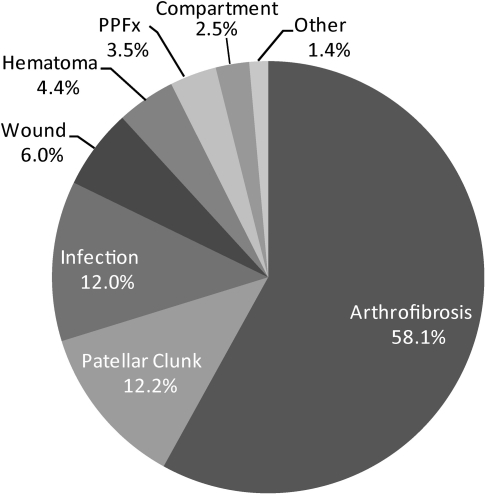
Stiffness was the most common indication for NRR and was responsible for 252 procedures (58% of all NRRs) on 238 knees and 218 patients (Fig. 1). All but five of the procedures for stiffness were MUA. Of the remaining five procedures, four occurred due to an inability to manipulate the knee and resulted in an open synovectomy and exchange of the polyethylene liner, and the last was an arthroscopic synovectomy. Patellar clunk (12.2%) and infection (12.0%) provided the second and third most common indications for reoperation, respectively (Fig. 1). Fifty arthroscopic and three open débridements of parapatellar fibrotic tissue were performed to treat patellar clunk in 49 knees and 44 patients. One arthroscopic and 51 open I&Ds were performed to treat infection in 48 knees and 45 patients. The remaining indications for reoperation (reported with proportion of NRRs and number of knees) included 26 wound revisions (6%; 24 knees), 19 hematoma evacuations (4.4%; 18 knees), 15 ORIFs for periprosthetic fractures (3.5%; 14 knees), 11 fasciotomies for compartment syndromes (2.5%; four knees), two synovectomies for synovitis (0.5%; two knees), and one procedure each for removal of osteophytes, removal of loose bodies, relief of patellofemoral impingement, and correction of poor patellar tracking (0.23%).
Fig. 1.
A pie chart illustrates the proportion of indications for all NRRs. PPFx = periprosthetic fracture.
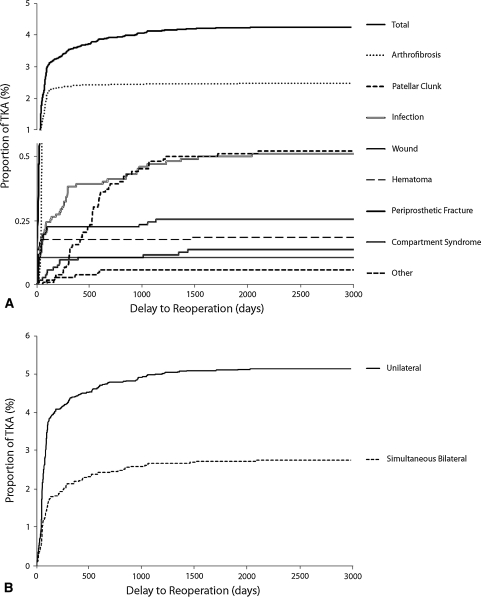
The median time to NRR was 75 days (range, 1–3058 days), with 84% performed within the first postoperative year (Fig. 2). The median time to NRR for stiffness was 63 days, with 69% performed within the first 3 postoperative months and 97% performed within the first year. The median time to NRR was 527 days for patellar clunk, 137 days for infection, 46 days for wound, 14 days for hematoma, and 198 days for periprosthetic fracture.
Fig. 2A–B.
Graphs show the rate of NRR as a function of time from primary TKA separated by (A) indication and (B) bilateral versus unilateral primary TKA.
The incidence of NRR was similar (p = 0.98) between women and men: 4.6% (225 of 4849) and 4.6% (128 of 2764), respectively. The average age of patients was lower (p < 0.001) in the NRR group (60 years; 95% CI, 59.3–61.5 years) than in the control group (66 years; 95% CI, 65.5–65.9 years). More than 3% (61 of 1887) of patients had NRR on 86 of 3747 (2.3%) knees after simultaneous bilateral TKA. One patient (2%; 1 of 48) had NRR on a single knee (1%; 1 of 96) after staged bilateral TKA. After unilateral TKA, 291 of 5678 (5.1%) patients had NRR on 297 of 6318 (4.7%) knees. Knees replaced independently had a greater (p < 0.001) likelihood of having a NRR than simultaneous bilateral knees. The reoperation rate was similar (p = 0.07) for right and left TKA: 4% (207 of 5178) and 3.5% (177 of 5010), respectively.
Sufficient incidences of NRR after staged bilateral TKA did not exist to compare the reoperation rates in this group to simultaneous bilateral or unilateral TKA.
Discussion
In 2005, approximately 523,000 TKAs were performed nationally [5]. Separately, the American Academy of Orthopaedic Surgeons (AAOS) and Kurtz et al. [10] have provided projections for the future demand of TKA. In 2002, the AAOS had suggested an annual replacement load of 474,000 by the year 2030. In 2007, Kurtz et al. [10] described an annual demand of 3.5 million by 2030. While these projections vary widely, they both suggest a strong increase in demand for TKA. In conjunction with this demand increase, the number of adult reconstruction surgeons is decreasing [5]. As the demand for TKA increases, so will the resulting complications necessitating further treatment. To better understand the future technological and economic burden of TKA, we investigated the rate and reason of NRR after primary TKA. Further, the timing of multiple TKAs, laterality, age, and gender were explored as potential risk factors for NRR.
We recognize limitations to our study. First, our study was retrospective, and analysis of data has the potential of being less accurate. The dataset used for this analysis does not track those patients who sought treatment for a complication at another institution. Second, the minimum 1-year followup is likely too short since 84% of NRRs were performed within the first postoperative year. Therefore, it is expected the incidence of NRR reported here is an underestimate. Third, from the provided dataset, a complete assessment of risk factors for NRR is not possible. Comparison between simultaneous bilateral and unilateral TKA is not conclusive since the selection parameters for performing simultaneous bilateral versus unilateral TKA were unknown. An accurate rate of NRR after staged bilateral TKA cannot be reported due to the low volume of patients undergoing this procedure. Presenting comorbidities, indication for TKA, operative time, component type, and other surgical variables are necessary in making a complete assessment of risk factors.
Based on our data, 3.8% of replaced knees will require an average 1.12 NRR as the primary surgical treatment after TKA. Moreover, 4.6% of patients undergoing TKA will require a NRR. Currently, the annual number of revision TKA is 7.3% the burden of primary TKA [5] with a reported revision rate of 2.8% within the first five years [19]. By 2030, due to a decreased age, increased body mass, and increased activity in the TKA patient population, the burden of revision TKA is expected to rise to 7.7% of primary TKA. A similar increase in the burden of NRR can be expected due to the same factors.
The most common indication for reoperation was stiffness, but also included were patellar clunk, infection, improper wound closure, hematoma, periprosthetic fracture, compartment syndrome, and others. The incidence of MUA has been reported as 1.3% to 13.5% [7, 14, 25, 30]. Our analysis provides an incidence of 2.3% of knees having a NRR for stiffness. Reported incidence of patellar clunk syndrome after TKA varies widely (0%–13.3%) and depends upon femoral component design [1, 2, 4, 6, 9, 12]. The incidence reported here (0.5%) suggests an improvement in component design and technique. Although the overall rate of reoperation for patellar clunk was lower than most studies, we suspect patellar clunk would not have been the second most common indication for reoperation had we not earlier used a prosthesis (Proven Knee from StelKast) that was posterior cruciate substituting with a large box. Early models of similar implants have been associated with a high incidence of patellofemoral problems [4]. Several reports suggest arthroscopic débridement for patellar clunk alleviates the patient’s symptoms [1, 28]. The incidence of NRR for infection was 48/10188 (0.5%) and infection is a devastating complication. NRR is typically only the first treatment method for acute postoperative, acute hematogenous, and/or superficial infections. Kurtz et al. [11] reported the incidence of infection in the Medicare population as 2%, 1.5% within the first 2 postoperative years and 0.5% in 2 to 10 postoperative years. More than 80% of the procedures for infection in this study were performed in the first 2 postoperative years. A logarithmic increase in procedures for infection was seen that does not plateau until 5 years (Fig. 1). In the literature, the reported success of I&D in eradicating infections is 16% to 80% and is heavily dependent upon the timing of presentation [3, 16, 20, 27]. Infection remains a difficult complication to treat and will provide a large treatment burden for the knee arthroplasty population both through NRR and revision TKA.
A younger age predicted a patient will have a NRR after primary TKA. Among the multiple indications for NRR, patients with stiffness were the youngest. One report suggests young age predicts stiffness after TKA [21]. Knees replaced as part of a simultaneous bilateral arthroplasty were less likely to have a NRR. Similarly, patients undergoing simultaneous bilateral TKA were less likely to undergo a NRR. Malinzak et al. [13] reported bilateral knees replaced simultaneously are less likely to develop infection than unilateral arthroplasties. Ritter et al. [24] were unable to detect differences of prosthetic survival at 10 years and patient mortality at 3 months in patients undergoing simultaneous bilateral TKA. The current findings, like others reported [13, 24], are likely the result of a selection bias for simultaneous bilateral arthroplasty in healthier, younger patients. Moreover, this institution regimented discharge to inpatient rehabilitation for simultaneous bilateral arthroplasty while many unilateral arthroplasty patients were discharged home. This supervised rehabilitation may explain the lower rate of MUA among the simultaneous bilateral patients who were younger and therefore at greater risk of developing stiffness [21]. Simultaneous bilateral arthroplasty remains a controversial procedure, with conflicting reports [8, 15, 17, 18, 22–24, 26, 31]. Our results do little to resolve this issue; however, the knowledge of decreased risk of NRR is interesting. Gender and laterality did not predict NRR.
The incidence of NRR after primary TKA at this institution is 3.8%. The burden of revision for primary TKA has been reported as 7.3% [5]. This study reports the burden of NRR for primary TKA as 4.3% (434 of 10,188). Generalizing these results to the entire TKA population, the combined reoperation burden is approximately 12% of primary arthroplasty surgery. As it is expected that the absolute incidence of revision will increase, it should be expected that the absolute incidence of NRR will increase. This will pose a substantial burden on the dwindling adult reconstruction orthopaedic community. Further research is needed to truly identify those patients at high-risk for complications leading to NRR. Those findings in conjunction with technological improvement will minimize orthopaedic complications, specifically stiffness, patellar clunk, and infection, requiring reoperations.
Footnotes
Javad Parvizi is a consultant for Stryker Orthopaedics (Mahwah, NJ) and has intellectual properties on SmarTech (Philadelphia, PA); Peter F. Sharkey is a consultant for Stryker Orthopaedics.
Each author certifies that his/her institution has approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Dajani KA, Stuart MJ, Dahm DL, Levy BA. Arthroscopic treatment of patellar clunk and synovial hyperplasia after total knee arthroplasty. J Arthroplasty. 2010;25:97–103. doi: 10.1016/j.arth.2008.11.005. [DOI] [PubMed] [Google Scholar]
- 2.Fukunaga K, Kobayashi A, Minoda Y, Iwaki H, Hashimoto Y, Takaoka K. The incidence of the patellar clunk syndrome in a recently designed mobile-bearing posteriorly stabilised total knee replacement. J Bone Joint Surg Br. 2009;91:463–468. doi: 10.1302/0301-620X.91B4.21494. [DOI] [PubMed] [Google Scholar]
- 3.Hartman MB, Fehring TK, Jordan L, Norton HJ. Periprosthetic knee sepsis. The role of irrigation and debridement. Clin Orthop Relat Res. 1991;273:113–118. [PubMed] [Google Scholar]
- 4.Hozack WJ, Rothman RH, Booth RE, Jr, Balderston RA. The patellar clunk syndrome. A complication of posterior stabilized total knee arthroplasty. Clin Orthop Relat Res. 1989;241:203–208. [PubMed] [Google Scholar]
- 5.Iorio R, Robb WJ, Healy WL, Berry DJ, Hozack WJ, Kyle RF, Lewallen DG, Trousdale RT, Jiranek WA, Stamos VP, Parsley BS. Orthopaedic surgeon workforce and volume assessment for total hip and knee replacement in the United States: preparing for an epidemic. J Bone Joint Surg Am. 2008;90:1598–1605. doi: 10.2106/JBJS.H.00067. [DOI] [PubMed] [Google Scholar]
- 6.Ip D, Ko PS, Lee OB, Wu WC, Lam JJ. Natural history and pathogenesis of the patella clunk syndrome. Arch Orthop Trauma Surg. 2004;124:597–602. doi: 10.1007/s00402-003-0533-9. [DOI] [PubMed] [Google Scholar]
- 7.Kim J, Nelson CL, Lotke PA. Stiffness after total knee arthroplasty. Prevalence of the complication and outcomes of revision. J Bone Joint Surg Am. 2004;86:1479–1484. doi: 10.1302/0301-620X.86B7.15255. [DOI] [PubMed] [Google Scholar]
- 8.Kim YH, Choi YW, Kim JS. Simultaneous bilateral sequential total knee replacement is as safe as unilateral total knee replacement. J Bone Joint Surg Br. 2009;91:64–68. doi: 10.1302/0301-620X.91B1.21320. [DOI] [PubMed] [Google Scholar]
- 9.Koh YG, Kim SJ, Chun YM, Kim YC, Park YS. Arthroscopic treatment of patellofemoral soft tissue impingement after posterior stabilized total knee arthroplasty. Knee. 2008;15:36–39. doi: 10.1016/j.knee.2007.08.009. [DOI] [PubMed] [Google Scholar]
- 10.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780–785. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 11.Kurtz SM, Ong KL, Lau E, Bozic KJ, Berry D, Parvizi J. Prosthetic joint infection risk after TKA in the Medicare population. Clin Orthop Relat Res. 2010;468:52–56. doi: 10.1007/s11999-009-1013-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lonner JH, Jasko JG, Bezwada HP, Nazarian DG, Booth RE., Jr Incidence of patellar clunk with a modern posterior-stabilized knee design. Am J Orthop (Belle Mead NJ) 2007;36:550–553. [PubMed] [Google Scholar]
- 13.Malinzak RA, Ritter MA, Berend ME, Meding JB, Olberding EM, Davis KE. Morbidly obese, diabetic, younger, and unilateral joint arthroplasty patients have elevated total joint arthroplasty infection rates. J Arthroplasty. 2009;24(6 Suppl):84–88. doi: 10.1016/j.arth.2009.05.016. [DOI] [PubMed] [Google Scholar]
- 14.Mauerhan DR, Mokris JG, Ly A, Kiebzak GM. Relationship between length of stay and manipulation rate after total knee arthroplasty. J Arthroplasty. 1998;13:896–900. doi: 10.1016/S0883-5403(98)90196-6. [DOI] [PubMed] [Google Scholar]
- 15.Memtsoudis SG, Vougioukas VI, Ma Y, Gaber-Baylis LK, Girardi FP. Perioperative morbidity and mortality after anterior, posterior, and anterior/posterior spine fusion surgery. Spine (Phila Pa 1976). 2010 May 5. [Epub ahead of print]. [DOI] [PMC free article] [PubMed]
- 16.Mont MA, Waldman B, Banerjee C, Pacheco IH, Hungerford DS. Multiple irrigation, debridement, and retention of components in infected total knee arthroplasty. J Arthroplasty. 1997;12:426–433. doi: 10.1016/S0883-5403(97)90199-6. [DOI] [PubMed] [Google Scholar]
- 17.Noble J, Goodall JR, Noble DJ. Simultaneous bilateral total knee replacement: a persistent controversy. Knee. 2009;16:420–426. doi: 10.1016/j.knee.2009.04.009. [DOI] [PubMed] [Google Scholar]
- 18.Oakes DA, Hanssen AD. Bilateral total knee replacement using the same anesthetic is not justified by assessment of the risks. Clin Orthop Relat Res. 2004;428:87–91. doi: 10.1097/01.blo.0000147133.75432.86. [DOI] [PubMed] [Google Scholar]
- 19.Ong KL, Lau E, Suggs J, Kurtz SM, Manley MT. Risk of subsequent revision after primary and revision total joint arthroplasty. Clin Orthop Relat Res. 2010 May 25. [Epub ahead of print]. [DOI] [PMC free article] [PubMed]
- 20.Parvizi J, Azzam K, Ghanem E, Austin MS, Rothman RH. Periprosthetic infection due to resistant staphylococci: serious problems on the horizon. Clin Orthop Relat Res. 2009;467:1732–1739. doi: 10.1007/s11999-009-0857-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Parvizi J, Tarity TD, Steinbeck MJ, Politi RG, Joshi A, Purtill JJ, Sharkey PF. Management of stiffness following total knee arthroplasty. J Bone Joint Surg Am. 2006;88(Suppl 4):175–181. doi: 10.2106/JBJS.F.00608. [DOI] [PubMed] [Google Scholar]
- 22.Pulido L, Parvizi J, Macgibeny M, Sharkey PF, Purtill JJ, Rothman RH, Hozack WJ. In hospital complications after total joint arthroplasty. J Arthroplasty. 2008;23(6 Suppl 1):139–145. doi: 10.1016/j.arth.2008.05.011. [DOI] [PubMed] [Google Scholar]
- 23.Restrepo C, Parvizi J, Dietrich T, Einhorn TA. Safety of simultaneous bilateral total knee arthroplasty. A meta-analysis. J Bone Joint Surg Am. 2007;89:1220–1226. doi: 10.2106/JBJS.F.01353. [DOI] [PubMed] [Google Scholar]
- 24.Ritter MA, Harty LD, Davis KE, Meding JB, Berend M. Simultaneous bilateral, staged bilateral, and unilateral total knee arthroplasty. A survival analysis. J Bone Joint Surg Am. 2003;85:1532–1537. doi: 10.2106/00004623-200308000-00015. [DOI] [PubMed] [Google Scholar]
- 25.Rubinstein RA, Jr, DeHaan A. The incidence and results of manipulation after primary total knee arthroplasty. Knee. 2010;17:29–32. doi: 10.1016/j.knee.2009.07.001. [DOI] [PubMed] [Google Scholar]
- 26.Severson EP, Mariani EM, Bourne MH. Bilateral total knee arthroplasty in patients 70 years and older. Orthopedics. 2009;32:316. doi: 10.3928/01477447-20090501-13. [DOI] [PubMed] [Google Scholar]
- 27.Silva M, Tharani R, Schmalzried TP. Results of direct exchange or debridement of the infected total knee arthroplasty. Clin Orthop Relat Res. 2002;404:125–131. doi: 10.1097/00003086-200211000-00022. [DOI] [PubMed] [Google Scholar]
- 28.Takahashi M, Miyamoto S, Nagano A. Arthroscopic treatment of soft-tissue impingement under the patella after total knee arthroplasty. Arthroscopy. 2002;18:E20. doi: 10.1053/jars.2002.31968. [DOI] [PubMed] [Google Scholar]
- 29.Webb BG, Lichtman DM, Wagner RA. Risk factors in total joint arthroplasty: comparison of infection rates in patients with different socioeconomic backgrounds. Orthopedics. 2008;31:445. doi: 10.3928/01477447-20080801-36. [DOI] [PubMed] [Google Scholar]
- 30.Yercan HS, Sugun TS, Bussiere C, Ait Si ST, Davies A, Neyret P. Stiffness after total knee arthroplasty: prevalence, management and outcomes. Knee. 2006;13:111–117. doi: 10.1016/j.knee.2005.10.001. [DOI] [PubMed] [Google Scholar]
- 31.Zeni JA, Jr, Snyder-Mackler L. Clinical outcomes after simultaneous bilateral total knee arthroplasty: comparison to unilateral total knee arthroplasty and healthy controls. J Arthroplasty. 2010;25:541–546. doi: 10.1016/j.arth.2009.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]