Abstract
Background
The hospital cost of total knee arthroplasty (TKA) in the United States is a major growing expense for the Centers for Medicare & Medicaid Services (CMS). Many hospitals are unable to deliver TKA with profitable or breakeven economics under the current Diagnosis-Related Group (DRG) hospital reimbursement system.
Questions/purposes
The purposes of the current study were to (1) determine revenue, expenses, and profitability (loss) for TKA for all patients and for different payors; (2) define changes in utilization and unit costs associated with this operation; and (3) describe TKA cost control strategies to provide insight for hospitals to improve their economic results for TKA.
Results
From 1991 to 2009, Lahey Clinic converted a $2172 loss per case on primary TKA in 1991 to a $2986 profit per case in 2008. The improved economics was associated with decreasing revenue in inflation-adjusted dollars and implementation of hospital cost control programs that reduced hospital expenses for TKA. Reduction of hospital length of stay and reduction of knee implant costs were the major drivers of hospital expense reduction.
Conclusions
During the last 25 years, our economic experience with TKA is concerning. Hospital revenues have lagged behind inflation, hospital expenses have been reduced, and our institution is earning a profit. However, the margin for TKA is decreasing and Managed Medicare patients do not generate a profit. The erosion of hospital revenue for TKA will become a critical issue if it leads to economic losses for hospitals or reduced access to TKA.
Level of Evidence
Level III, Economic and Decision Analyses. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
The prevalence of TKA in the United States increased each year between 1991 and 2008, and demand for primary TKA is projected to grow to 3.48 million procedures per year by 2030 [11]. During a similar interval, Medicare hospital payment for joint arthroplasty increased 30% [16], and inflation rose 59% (consumer price index) [23]. Medicare payments to hospitals for TKAs increased at a rate lower than inflation over this time interval [18].
As hospital revenues for joint arthroplasties increased at a rate less than inflation, hospital expenses for joint arthroplasty increased at a rate greater than inflation. A hospital’s ability to break even or profit on joint arthroplasties during this period depended on being able to control expenses required to deliver care. During the 1980s and 1990s, hospital costs in the United States were controlled partially by utilization review, which was an attempt to reduce the volumes and costs of services and supplies associated with care.
We evaluated and compared the hospital economics of TKA at Lahey Clinic in 1991 and 2008. Project goals included (1) determining revenue, expenses, and profitability (loss) for TKA for all patients and for different payors; (2) defining changes in utilization and unit costs associated with this operation; and (3) describing TKA cost control strategies to provide insight for hospitals to improve their economic results for TKA.
Patients and Methods
We reviewed the records of 125 consecutive patients who had TKA in 1991. All patients undergoing a primary TKA were eligible for inclusion in the study. Exclusion criteria included patients who had unicompartmental arthroplasty, bilateral TKAs, revision TKA, a secondary operative procedure during the index hospitalization, a medical complication requiring an extended hospitalization, and patients for whom there were inadequate economic data. From 1991, 42 patients who had a primary unilateral TKA were eligible for the study (Table 1). We also reviewed the records of 428 consecutive patients who had a primary unilateral TKA (CPT 27447) in 2008. The same set of exclusion criteria was applied to 2008 patients as with 1991 patients. None of the 2008 patients had a secondary operative procedure during the index hospitalization, and all patients had sufficient economic information to be included in the study. In 2008, the Centers for Medicare and Medicaid Services (CMS) changed the method of hospital reimbursement for joint arthroplasty operations for Medicare patients. The Diagnosis Related Group (DRG) system was replaced by the Medical Severity–Diagnosis Related Group (MS-DRG) system, which included MS-DRG 470 (major joint replacement of lower extremity without major comorbidities) and MS-DRG 469 (major joint replacement of lower extremity with major comorbidities). Fifteen patients in MS-DRG 469 with major comorbidities were excluded. From 2008, 413 patients who had a primary unilateral TKA were eligible for the study (Table 1).
Table 1.
TKA patient data
| Variable | 1991 | 2008 | ||||
|---|---|---|---|---|---|---|
| All patients | All patients | Medicare only | Managed Medicare | Major private health plans | Other | |
| Primary unilateral TKA | 125 | 428 | 186 | 96 | 95 | 51 |
| Without major comorbidities | 413 (96.5%) | 180 (96.8%) | 91 (94.8%) | 94 (98.9%) | 48 (94.1%) | |
| With major comorbidities | 15 (3.5%) | 6 (3.2%) | 5 (5.2%) | 1 (1.1%) | 3 (5.9%) | |
| Study patients | 42 | 413 | 180 | 91 | 94 | 48 |
| Age (years) | ||||||
| Median | 69 | 69 | 73 | 74 | 61 | 58 |
| Range | 53–87 | 36–90 | 47–90 | 61–88 | 36–82 | 39–82 |
| Gender | ||||||
| Male | 16 (38%) | 163 (40%) | 63 (35%) | 36 (39%) | 36 (39%) | 26 (55%) |
| Female | 26 (62%) | 250 (60%) | 117 (65%) | 55 (61%) | 58 (61%) | 22 (45%) |
| Diagnosis | ||||||
| Osteoarthritis | 39 (93%) | 403 (98%) | 177 (98%) | 89 (98%) | 90 (96%) | 46 (97%) |
| Rheumatoid arthritis | 3 (7%) | 4 (1%) | 2 (1%) | 1 (1%) | 1 (1%) | 0 (0%) |
| Lupus | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) |
| Other | 0 (0%) | 6 (2%) | 1 (1%) | 1 (1%) | 3 (3%) | 2 (3%) |
| Operating surgeons | 2 | 8 | ||||
| Knee implants | ||||||
| PCA Modular | 30 | |||||
| Duracon | 12 | |||||
| PFC Sigma | 413 | 180 | 91 | 94 | 48 | |
| Duration of hospital stay (days) | 9.0 | 3.7 | 3.6 | 3.5 | 3.9 | 4.2 |
In the 1991 cohort, the median age was 69 years (range, 53–87 years), and there were 16 men and 26 women. Thirty-nine patients (93%) had osteoarthritis and three patients (7%) had rheumatoid arthritis. In the 2008 cohort, the median age was 69 years (range, 36–90 years), and there were 163 men and 250 women. In 2008, 403 patients (98%) had osteoarthritis, four patients (1%) had rheumatoid arthritis, and six patients had other diagnoses (Table 1).
All patients studied had a primary unilateral TKA at Lahey Clinic. Two surgeons performed the operations in 1991, and 8 surgeons performed the operations in 2008. All TKAs involved three-compartment resurfacing in which a condylar, cruciate-retaining, or cruciate-sacrificing (substituting) nonporous-coated knee implant was inserted with bone cement. In 1991, the PCA Modular® (Howmedica, Rutherford, NJ) (30 patients) and the Duracon® (Howmedica) knee implants (12 patients) were used. In 2008, the PFC Sigma® knee implant (DePuy Orthopaedics, Warsaw, IN) was used for all patients. The average hospital stay was 9 days in 1991 and 3.7 days in 2008 (Table 1).
Hospital revenue, hospital expenses, and hospital profit (loss) for TKA were evaluated and compared in 1991 and 2008. To compare data from 1991 to data from 2008, 1991 US dollars were converted to inflation-adjusted 2008 US dollars with the consumer price index for all urban consumers obtained from the Bureau of Labor Statistics [23].
In 1991, hospital revenue for TKA for all 42 patients was provided through the Medicare DRG system administered by the Health Care Financing Administration (DRG-209; major joint replacement of lower extremity). In 2008, hospital revenue for TKA for these 413 patients is reported in four payor categories: Medicare fee for service (FFS) (180), Managed Medicare (91), major private health plans (94), and other payors (48). Hospital payment for Medicare FFS patients was provided through the Medicare MS-DRG system administered by CMS (MS-DRG 470; major joint replacement of lower extremity without major comorbidities).
Hospital expenses for TKA were determined by different methods in 1991 and 2008. In 1991, hospital cost data were established using government-mandated, hospital-specific, cost-to-charge ratios. This method of determining hospital cost was generally accepted in 1991. In 2008, a resource-based hospital accounting system (TSI Inc, Cambridge, MA) provided actual hospital cost data for each procedure. Direct and indirect costs were assigned to hospital services based on cost data within the system.
Hospital expenses were allocated to 17 service centers or accounting groups such as the laboratory, operating room (OR), or radiology department, for which charges and costs are available. The anesthesiology service center included operative anesthetics used for each case and the technical cost of femoral nerve blocks. All patients received general anesthesia in 1991 and 391 patients received general anesthesia in 2008. In 2008, all patients also received a femoral nerve block. The blood bank service center included blood type tests and transfusion costs. The electrocardiology service center included perioperative electrocardiograms. The hospital room service center included all hospital floor-related costs during a patient stay from nursing to meals to dressing change supplies. Intravenous therapy included intravenous and peripherally inserted central catheter placement costs. Daily phlebotomy draws and laboratory work such as complete blood count, international normalized ratio, and basic metabolic profile were included in the laboratory service center. The OR service center includes staff and administrative expenses and was applied based on half-hourly charges for OR use. The orthopaedic appliance service center included splinting, casting, or application of continuous passive motion devices. Pathology included pathologic evaluation of OR specimens. The pharmacy service center included perioperative medications such as antibiotics, analgesics, anticoagulatants, etc, administered during a patient’s hospital course. The initial physical therapy/occupational therapy (PT/OT) evaluation and daily ROM, gait training, and therapeutic activities were all included in the PT/OT service center. Perioperative chest radiographs and postoperative knee radiographs were among the costs included in the radiology service center. The recovery room cost includes staff and administrative expenses. Postoperative ventilatory support, continuous positive airway pressure, and pulse oximetry were included in the respiratory therapy service center. Supplies (medical and operative) include specific products with variable cost purchased by the hospital for the TKA. The cost of knee implants is included in the supplies (medical and operative) service center. Specific implant prices are not provided as a result of purchasing agreements with implant manufacturers. Noninvasive scans of the lower extremity to evaluate for thromboembolic disease accounted for the vascular laboratory service center. The other service center included miscellaneous services/testing performed postoperatively such as hemodialysis, cancer screening, and endoscopy studies (Table 2).
Table 2.
Hospital expense allocation
| Service center | Actual cost | Inflation-adjusted cost (2008 dollars) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| 1991 | 2008 | Change from 1991 to 2009 | 1991 | Change from 1991 to 2009 | |||||
| All patients | All patients | Medicare Only | Managed Medicare | Major private health plans | Other | All patients | All patients | All patients | |
| Anesthesiology | $111 | $861 | $843 | $871 | $869 | $890 | 678% | $175 | 392% |
| Blood bank | $151 | $271 | $305 | $301 | $213 | $203 | 80% | $238 | 14% |
| Electrocardiography | $30 | $9 | $6 | $11 | $7 | $19 | −70% | $47 | −81% |
| Hospital room | $3711 | $3373 | $3271 | $3059 | $3594 | $3899 | −9% | $5866 | −42% |
| Intravenous therapy | $107 | $46 | $44 | $39 | $60 | $39 | −57% | $169 | −73% |
| Laboratory | $215 | $203 | $202 | $199 | $198 | $220 | −6% | $340 | −40% |
| Operating room | $2110 | $2,069 | $1996 | $2004 | $2078 | $2,431 | −2% | $3336 | −38% |
| Orthopaedic appliances | $642 | $116 | $118 | $105 | $117 | $126 | −82% | $1015 | −89% |
| Pathology | $94 | $3 | $4 | $13 | −97% | $148 | −98% | ||
| Pharmacy | $169 | $110 | $110 | $92 | $112 | $139 | −35% | $268 | −59% |
| Physical/occupational therapy | $371 | $410 | $369 | $360 | $476 | $522 | 11% | $587 | −30% |
| Radiology | $119 | $55 | $57 | $71 | $39 | $47 | −54% | $189 | −71% |
| Recovery room | $422 | $885 | $866 | $926 | $842 | $966 | 110% | $667 | 33% |
| Respiratory therapy | $58 | $13 | $14 | $11 | $7 | $24 | −78% | $92 | −86% |
| Supplies (medical and operative) | $3424 | $2553 | $2553 | $2553 | $2553 | $2584 | −25% | $5413 | −53% |
| Vascular laboratory | $89 | $9 | $8 | $16 | $1 | $15 | −90% | $141 | −94% |
| Other | $4 | $19 | $29 | $11 | $21 | 423% | $6 | 231% | |
| Total hospital cost | $11,826 | $11,002 | $10,793 | $10,629 | $11,184 | $12,136 | −7% | $18,695 | −41% |
Results
In 1991, hospital revenue per case for the 42 primary TKAs performed was $15,261 in inflation-adjusted dollars. In 2008, hospital revenue per case for the 413 primary TKAs was $13,988. From 1991 to 2008, hospital revenue per case decreased 8% in inflation-adjusted dollars. In 1991, hospital cost per case was $18,695 in inflation-adjusted dollars, whereas in 2008, hospital expense per case was $11,002. From 1991 to 2008, hospital expense per case decreased 41% in inflation-adjusted dollars. Primary TKA at Lahey Clinic was not profitable in 1991. The hospital lost $3434 per case in inflation-adjusted dollars. In 2008, primary TKA was profitable and the hospital earned $2986 per case (Table 3).
Table 3.
TKA hospital economic data
| Variable | 1991 | 2008 | |||||
|---|---|---|---|---|---|---|---|
| All patients | All patients | Medicare FFS only | Managed Medicare | Major private health plans | Other | ||
| $ (1991) | $ (2008) | $ (2008) | $ (2008) | $ (2008) | $ (2008) | $ (2008) | |
| Number of patients | 42 | 413 | 180 | 91 | 94 | 48 | |
| Total hospital revenue | $405,468 | $640,964 | $5,777,129 | $2,525,886 | $996,834 | $1,704,713 | $549,697 |
| Base payment | $405,468 | $5,221,403 | $1,970,159 | $996,834 | $1,704,713 | $549,697 | |
| IME payment | $363,640 | $363,640 | |||||
| Capital payment | $192,087 | $192,087 | |||||
| Hospital revenue per case | $9654 | $15,261 | $13,988 | $14,033 | $10,954 | $18,135 | $11,452 |
| Base payment per case | $9654 | $15,261 | $12,643 | $10,945 | $10,954 | $18,135 | $11,452 |
| IME payment per case | $880 | $2020 | |||||
| Capital payment per case | $465 | $1067 | |||||
| Hospital expense | $496,697 | $785,178 | $4,543,751 | $1,942,672 | $967,215 | $1,051,337 | $582,528 |
| Hospital expense per case | $11,826 | $18,695 | $11,002 | $10,793 | $10,629 | $11,184 | $12,136 |
| Hospital profit (loss) | $(91,229) | $(144,214) | $1,233,379 | $583,214 | $29,619 | $653,376 | $(32,831) |
| Hospital profit (loss) per case | $(2172) | $(3434) | $2986 | $3240 | $325 | $6951 | $(684) |
FFS = fee for service; IME = indirect medical education.
In 1991, all 42 patients evaluated were Medicare FFS patients. Hospital revenue was $15,261 per case in inflation-adjusted dollars based on the DRG-209 hospital payment schedule. In 2008, 180 patients were Medicare FFS patients. Hospital revenue per case was $14,033 in actual dollars, which was composed of a base payment ($10,945), an indirect medical education (IME) payment ($2020), and a capital expense payment ($1067). The hospital revenue per case for this group decreased 8% in inflation-adjusted dollars over the study period. Meanwhile, hospital expenses per case decreased 42.2% in inflation-adjusted dollars from $18,695 in 1991 to $10,793 in 2008. The decrease in hospital expenses offset the decrease in hospital revenue allowing Lahey Clinic to convert a loss in 1991 to a profit in 2008 of $3240 per case (Table 3).
Our economic results for TKA for 91 Managed Medicare patients varied considerably from our experience with Medicare FFS patients. Hospital revenue per case was 22% less, hospital expense per case was similar, and hospital profitability per case was 90% less ($325 versus $3240) than Medicare FFS patients (Table 3). The primary reason for less profitability among managed Medicare patients is less revenue per case. Lahey Clinic did not receive an IME payment or a capital expense payment for Managed Medicare patients.
When hospital expenses were allocated to 17 service centers, the hospital room, OR, and supplies (medical and operative) service centers represented the largest percentage of hospital expense for primary TKA. These three service centers accounted for 78.2% of hospital cost in 1991 and 72.7% of hospital cost in 2008. From 1991 to 2008, the hospital cost allocation to the hospital room service center decreased 42% in inflation-adjusted dollars, which was associated with a reduction in hospital length from of stay from 9 days to 3.7 days (Tables 2, 4). The hospital cost allocation to the OR service center decreased 38% in inflation-adjusted dollars during the study period and was associated with a reduction in operative time (Tables 2, 4). The supplies (medical and operative) service center decreased 53% in inflation-adjusted dollars from 1991 to 2008. This decrease was associated with a reduction of the knee implant cost secondary to the implementation of a single price-case purchasing agreement (Tables 2–4).
Table 4.
TKA hospital expense allocation
| Service center | Allocation of hospital cost for TKA (%) | ||
|---|---|---|---|
| 1991 | 2008 | Change from 1991 to 2008 | |
| Anesthesiology | 0.9% | 7.8% | 6.9% |
| Blood bank | 1.3% | 2.5% | 1.2% |
| Electrocardiography | 0.3% | 0.1% | −0.2% |
| Hospital room | 31.4% | 30.7% | −0.7% |
| Intravenous therapy | 0.9% | 0.4% | −0.5% |
| Laboratory | 1.8% | 1.8% | 0.0% |
| Operating room | 17.8% | 18.8% | 1.0% |
| Orthopaedic appliances | 5.4% | 1.1% | −4.4% |
| Pathology | 0.8% | 0.0% | −0.8% |
| Pharmacy | 1.4% | 1.0% | −0.4% |
| Physical/occupational therapy | 3.1% | 3.7% | 0.6% |
| Radiology | 1.0% | 0.5% | −0.5% |
| Recovery room | 3.6% | 8.0% | 4.5% |
| Respiratory therapy | 0.5% | 0.1% | −0.4% |
| Supplies (medical and operative) | 29.0% | 23.2% | −5.8% |
| Vascular laboratory | 0.8% | 0.1% | −0.7% |
| Other | 0.0% | 0.2% | 0.1% |
Discussion
TKA substantially improves quality-adjusted life expectancy for patients with arthritic knees, and TKAs are cost-effective in the United States across all risk groups [15, 25]. However, TKA is an expensive operation, its prevalence is increasing, and the CMS Medicare program has been challenged by the rising cost of TKA [3]. We evaluated and compared the hospital economics of TKA at Lahey Clinic in 1991 and 2008. Project goals included (1) determining revenue, expenses, and profitability (loss) for TKA for all patients and for different payors; (2) defining changes in utilization and unit costs associated with this operation; and (3) describing our cost control strategies to provide insight for hospitals to improve their economic results for TKA.
Limitations to the study include the fact that the number of qualified patients in 1991 was small and the fact that we excluded unqualified patients in both years to focus on patients who had a routine, uncomplicated primary TKA. This approach allowed us to focus on patients with routine economics and to compare similar patient groups, which enabled us to generate results that maybe more meaningful to readers looking to compare their TKA economic experience with ours. A second limitation was the use of different methods to collect financial data in 1991 and 2008. However, the resource-based hospital accounting system used in 2008 did not exist in 1991. Additionally, the method using government-mandated, hospital-specific, cost-to-charge ratios in 1991 was the accepted methodology for calculating hospital cost data at that time. Third, we converted costs to 2008 dollars using the CPI to compare 1991 and 2008 data. The CPI was used to adjust for inflation because it is a well-established and standardized index that is universally accepted for adjusting for inflation.
In this study, between 1991 and 2008, Lahey Clinic converted a $2172 loss per case for primary TKA into a $2986 profit per case. The Medicare program provides payment for more TKAs in the United States than any other healthcare payer and the largest patient cohort in this study was the Medicare patient group (69% [313 of 455]). It has been reported that some hospitals cannot make a profit when delivering medical and surgical services with current Medicare payment schedules [9, 20]. Therefore, we evaluated the economic results of our Medicare FFS patients and our Managed Medicare patients separately. For Medicare FFS patients who had TKAs, an economic turnaround was noted similar to our results for all patients. In sharp contrast, the profit recorded for Managed Medicare TKA patients was only $325 per case, which is a breakeven proposition. Our economic success with TKA was primarily the result of the hospital cost control programs implemented by surgeons and hospital administrators. Our disappointing breakeven experience with Managed Medicare was primarily the result of insufficient hospital revenue to generate a profit on TKA.
These economic results for primary TKA may not be applicable to all hospitals. Lahey Clinic is a teaching hospital and is owned by an integrated group practice in which physicians and hospital administrators have aligned incentives to control hospital costs and deliver health care at a profit. Nonteaching hospitals receive less revenue for TKA than teaching hospitals because they do not receive IME payments for Medicare FFS patients. In 2008, if Lahey Clinic were not a teaching hospital, there would have been 29% less profit for TKA for all patients and 62% less profit for Medicare FFS patients. Furthermore, many nonteaching hospitals, in addition to not receiving IME payments, do not include capital expense payments with hospital revenue. This would have resulted in a profit of only $641 per case for all patients and $153 per case for Medicare FFS patients.
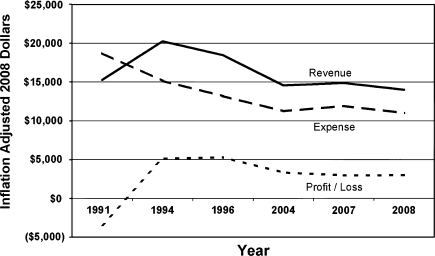
To better understand the trend of hospital economic results for TKA, we examined our revenue, expense, and profit (loss) at six time points from 1991 to 2008. All the information is from our hospital, and all patients were cared for by our group practice [6, 7, 12, 13]. The trends are concerning and perhaps alarming. In inflation-adjusted dollars, hospital revenue for TKA increased from 1991 to 1994, and it decreased from 1994 to 2008. Hospital revenue for TKA has not kept pace with inflation. In inflation-adjusted dollars, hospital expense for TKA decreased consistently from 1991 to 2008. Hospital cost has been actively managed at our hospital. In inflation-adjusted dollars, our profit (loss) for TKA improved from 1991 to 1994 and decreased steadily from 1994 to 2008. Despite effective cost control strategies, our hospital profit (loss) for TKA peaked with hospital revenue in 1994, and profit decreased from 1994 to 2008. Our experience with the Managed Medicare patients is most concerning because we have a well-managed, high-quality, low-cost TKA system, but we cannot make a profit as a result of low hospital revenue for Managed Medicare patients. Considering the projections of a major increase in the prevalence of knee osteoarthritis and TKA in the United States in the next two decades [8, 11], we are concerned about the deteriorating economics of TKA (Fig. 1).
Fig. 1.
TKA economic trends are shown from 1991 to 2008.
We identified several areas where changes in utilization and unit costs could be made to improve economic results for TKA. In 1992, in response to economic losses for TKA on Medicare patients, orthopaedic surgeons and hospital administrators worked in partnership to develop and implement hospital cost control programs for TKA. Clinical pathways were created for hospital care reducing the hospital length of stay. Early discharge to postacute care facilities used cost shifting to reduce hospital length of stay and hospital cost for TKA [4]. Every activity and supply used for TKA was evaluated for the potential to reduce cost without reducing quality [2]. This may not occur in all hospitals. From 1991 to 2008, hospital expenses decreased $824 per case in actual dollars and $7693 per case in inflation-adjusted dollars. These cost control strategies reduced the hospital cost of TKA at Lahey Clinic and were critical in delivering primary TKA for a profit.
During the period of this study, in an effort to achieve and maintain profitability for delivery of primary TKAs, several cost control programs were implemented. Utilization control programs included clinical or critical hospital pathways to improve and reduce hospital length of stay [4], standardization of OR routines to reduce length of operation, elimination of routine pathologic evaluation of surgical specimens without compromising patient care [10, 14, 21], elimination of wound drains, implementation of urinary catheter protocol that decreased urinary catheter utilization, elimination of routine postoperative radiographs as supported by the literature [1, 19, 24], elimination of routine postoperative noninvasive testing for thromboembolic disease [22], and reduction in use of autologous transfusions. Methods used to reduce unit costs of services and supplies associated with TKAs included standardized OR packs to reduce the cost of OR supplies, “just in time delivery” of OR supplies to reduce inventory and cost of supplies, stocking knee implants on consignment, and reducing the cost of knee implants. Strategies for controlling the cost of knee implants included surgeon cost awareness discussions, vendor discounting programs, implant standardization, competitive bid purchasing of implants, and developing a single-price/case-price implant purchasing program [2, 3, 5].
One of the most tightly controlled TKA service centers from 1991 to 2008 was the supplies (medical and operative) service center, which included knee implants. The allocation of hospital cost for TKA to the supplies (medical and operative) service center decreased 25%, from $3424 to $2553, and this service center decreased from 29% of hospital cost in 1991 to 23.2% of the hospital cost in 2008. Control of knee implant cost was a critical factor in cost reduction of this service center [3, 5]. Orthopaedic Network News reported, from 1991 to 2008, the average selling price of cemented, nonporous-coated knee implants using a modular tibial implant increased 92% from $2827 to $5428 [17]. If this average selling price for knee implants were substituted for the supplies (medical and operative) service center, for all patients, Lahey Clinic would have made a profit of $111 per patient in 2008 instead of realizing a $2986 profit per patient. If this average selling price for knee implants were substituted for the supplies (medical and operative) service center for Managed Medicare patients, Lahey Clinic would have lost $2550 per patient in 2008 instead of realizing a profit of $325 profit per patient. The considerable change in profitability associated with these substitutions suggests the cost of the knee implant can determine hospital profitability or loss for TKAs.
TKA can be a profitable hospital service at a teaching hospital. We realized a profit on TKA when treating all patients and Medicare FFS patients, but we broke even on TKA for Managed Medicare patients. We are concerned that hospital revenue for TKA increased at a rate lower than inflation during the last 18 years. If hospital revenue for all TKA operations decreases to the Managed Medicare levels, it will be difficult to make a profit on TKA. In our experience, the most successful action we initiated to achieve profitability for TKA was hospital expense control. We successfully reduced hospital length of stay and implant cost.
TKA has a remarkable history of clinical success in relieving pain and improving function for patients with arthritic knees. We have a responsibility to maintain access to this treatment for our patients. Hospitals and surgeons should collaborate to deliver TKA at a profit so it will be available to all patients with painful arthritic knees. Government healthcare administrators and healthcare payors should provide adequate reimbursement for hospitals and surgeons to continue the delivery of high-quality TKAs.
Acknowledgments
We thank Christopher Lucchesi, Lahey Clinic Finance, and John Garfi, Orthopaedic Clinical Research Specialist, who made valuable contributions to this project.
Footnotes
One of the authors (WLH) has a product development agreement with DePuy Orthopaedics, Inc (Warsaw, IN).
Each author certifies that his or her institution approved or waived approval for the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Glaser D, Lotke P. Cost-effectiveness of immediate postoperative radiographs after uncomplicated total knee arthroplasty: a retrospective and prospective study of 750 patients. J Arthroplasty. 2000;15:475–478. doi: 10.1054/arth.2000.4338. [DOI] [PubMed] [Google Scholar]
- 2.Healy WL, Finn D. The hospital cost and the cost of the implant for total knee arthroplasty: a comparison between 1983 and 1991 for one hospital. J Bone Joint Surg Am. 1994;76:801–806. doi: 10.2106/00004623-199406000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Healy WL, Iorio R. Implant selection and cost for total joint arthroplasty: conflict between surgeons and hospitals. Clin Orthop Relat Res. 2007;457:57–63. doi: 10.1097/BLO.0b013e31803372e0. [DOI] [PubMed] [Google Scholar]
- 4.Healy WL, Iorio R, Ko J, Appleby D, Lemos DW. Impact of cost reduction programs on short-term patient outcome and hospital cost of total knee arthroplasty. J Bone Joint Surg Am. 2002;84:348–353. doi: 10.2106/00004623-200203000-00003. [DOI] [PubMed] [Google Scholar]
- 5.Healy WL, Iorio R, Lemos MJ, Patch DA, Pfeifer BA, Smiley PM, Wilk RM. Single price/case price purchasing in orthopaedic surgery: experience at the Lahey Clinic. J Bone Joint Surg Am. 2000;82:607–612. doi: 10.2106/00004623-200005000-00001. [DOI] [PubMed] [Google Scholar]
- 6.Healy WL, Iorio R, Richards JA, Lucchesi C. Opportunities for control of hospital costs for total joint arthroplasty after initial cost containment. J Arthroplasty. 1998;13:504–507. doi: 10.1016/S0883-5403(98)90048-1. [DOI] [PubMed] [Google Scholar]
- 7.Iorio R, Healy WL, Richards JA. Comparison of the hospital cost of primary and revision total knee arthroplasty after cost containment. Orthopedics. 1999;22:195–199. doi: 10.3928/0147-7447-19990201-08. [DOI] [PubMed] [Google Scholar]
- 8.Iorio R, Robb WJ, Healy WL, Berry DJ, Hozack WJ, Kyle RF, Lewallen DG, Trousdale RT, Jiranek WA, Stamos VP, Parsley BS. Orthopaedic surgeon workforce and volume assessment for total hip and knee replacement in the United States: preparing for an epidemic. J Bone Joint Surg Am. 2008;90:1598–1605. doi: 10.2106/JBJS.H.00067. [DOI] [PubMed] [Google Scholar]
- 9.Jacoby J. Medicare and the Mayo Clinic. Boston Globe. January 6, 2010.
- 10.Kocher MS, Erens G, Thornhill TS, Ready JE. Cost and effectiveness of routine pathological examination of operative specimens obtained during primary total hip and knee replacement in patients with osteoarthritis. J Bone Joint Surg Am. 2000;82:1531–1535. doi: 10.2106/00004623-200011000-00002. [DOI] [PubMed] [Google Scholar]
- 11.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780–785. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 12.Total Joint Arthroplasty Margin Analysis, 2004. Burlington, MA: Lahey Clinic; 2004. [Google Scholar]
- 13.Total Joint Arthroplasty Margin Analysis, 2007. Burlington, MA: Lahey Clinic; 2007. [Google Scholar]
- 14.Lawrence T, Moskal JT, Diduch DR. Analysis of routine histological evaluation of tissues removed during primary hip and knee arthroplasty. J Bone Joint Surg Am. 1999;81:926–931. doi: 10.1302/0301-620X.81B5.9566. [DOI] [PubMed] [Google Scholar]
- 15.Losira L, Walensky RP, Kessler CL, Emrani DS, Reichmann WM, Wright EA, Solomn DH, Yelim Paltier AD, Katz JN. Cost-effectiveness of total knee arthroplasty in the United States: patient risk and hospital volume. Arch Intern Med. 2009;169:1102–1103. doi: 10.1001/archinternmed.2009.144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mendenhall S. Hip and knee implants list prices rise 5.6% Orthopaedic Network News. 2009;20:1–7. [Google Scholar]
- 17.Mendenhall S. Hospital resources and implant cost management—a 2008 update. Orthopaedic Network News. 2009;20:17. [Google Scholar]
- 18.Mendenhall S. 2010 CMS payment update. Orthopaedic Network News. 2009;20:22–23. [Google Scholar]
- 19.Moskal JT, Diduch DR. Postoperative radiographs after total knee arthroplasty: a cost-containment strategy. Am J Knee Surg. 1998;11:89–93. [PubMed] [Google Scholar]
- 20.Olmos D. Mayo Clinic in Arizona to stop treating some Medicare patients. December 31, 2009. Available at: www.bloomberg.com/apps/news?p…d=aHoYSI84VdL0. Accessed March 3, 2010.
- 21.Pagnano MW, Forero JH, Scuderi GR, Harwin SF. Is the routine examination of surgical specimens worthwhile in primary total knee arthroplasty? Clin Orthop Relat Res. 1998;356:79–84. doi: 10.1097/00003086-199811000-00013. [DOI] [PubMed] [Google Scholar]
- 22.Schwarcz TH, Matthews MR, Hartford JM, Quick RC, Kwolek CJ, Minion DJ, Endean ED, Mentzer RM. Surveillance venous duplex is not clinically useful after total joint arthroplasty when effective deep venous thrombosis prophylaxis is used. Ann Vasc Surg. 2004;18:193–198. doi: 10.1007/s10016-004-0009-6. [DOI] [PubMed] [Google Scholar]
- 23.US Department of Labor. Bureau of Labor Statistics. CPI inflation calculator. Available at: www.bls.gov/data/inflation_calculator.htm. Accessed March 3, 2010.
- 24.Ververeli PA, Masonis JL, Booth RE, Hozack WJ, Rothman RH. Radiographic cost reduction strategy in total joint arthroplasty: a prospective analysis. J Arthroplasty. 1996;11:277–280. doi: 10.1016/S0883-5403(96)80078-7. [DOI] [PubMed] [Google Scholar]
- 25.Yao L. Knee replacements are determined to be cost effective. Wall Street Journal. June 23, 2009.