Abstract
Background
Total hip arthroplasty (THA) has been associated with high survival rates, but debate remains concerning the best fixation mode of THA.
Questions/purposes
We conducted a randomized controlled trial (RCT) with 250 patients with a mean age of 64 years between October 1987 and January 1992 to compare the results of cementless and cemented fixation.
Patients and Methods
Patients were evaluated for revision of either of the components. One hundred twenty-seven patients had died (51%) and 12 (4.8%) were lost to followup. The minimum 17-year followup data (mean, 20 years; range, 17–21 years) for 52 patients of the cementless group and 41 patients of the cemented group were available for evaluation.
Results
Kaplan-Meier survivorship analysis at 20 years revealed lower survival rates of cemented compared with cementless THA. The cementless tapered stem was associated with a survivorship of 99%. Age younger than 65 years and male gender were predictors of revision surgery.
Conclusions
The efficacy of future RCTs can be enhanced by randomizing patients in specific patient cohorts stratified to age and gender in multicenter RCTs. Including only younger patients might improve the efficacy of a future RCT with smaller sample sizes being required. A minimum 10-year followup should be anticipated, but this can be expected to be longer if the difference in level of quality between the compared implants is smaller.
Level of Evidence
Level I, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Electronic supplementary material
The online version of this article (doi:10.1007/s11999-010-1459-5) contains supplementary material, which is available to authorized users.
Introduction
During the early 1980s, with THA becoming a much more established procedure, concerns surrounding the use of cement fixation started to surface. The longevity of the first-generation cementing techniques was being questioned, especially for young, active patients [12, 17, 50, 60, 62]. The more frequent occurrence of osteolysis, which in retrospect was erroneously attributed to ‘cement disease’, promoted the renewed interest in improved cementing techniques, improved cemented stem designs with different surface roughness and implant geometry, and in cementless fixation with ingrowth or ongrowth of bone to the stem. The first generation of cementless femoral stems produced mixed survivorships with problems being related to fixation failure, thigh pain, wear, and osteolysis [9, 11, 15, 18, 51]. Subsequent generations of uncemented femoral stems have been developed to address these complications and have achieved longevity at least comparable to that of their cemented counterparts with 10 or more years of followup [1, 2, 19, 21, 22, 29, 39, 43, 46, 48]. The authors of one paper suggested arthroplasties performed without cement were preferable to those with cement, especially in younger, more active individuals [53]. To date, there is no consensus on the best fixation mode for THA. In Sweden, most surgeons prefer to use cement fixation, whereas in North America and Australia, most surgeons prefer cementless fixation except when patients have severe osteoporosis or Dorr C-type morphologic features of the femur [3, 24, 27, 30, 37, 38, 47, 63]. Nonetheless, THA is reportedly one of the most cost-effective operations [52].
A RCT seemed to be the best way to determine whether cemented or cementless fixation was superior in THA, minimizing selection bias and other confounding variables [35, 52]. We initiated such a RCT in 1987 for patients with osteoarthritic hips who met strict inclusion criteria. A THA system with a similar geometry and alloy for cemented and cementless fixation was chosen. At that time, titanium alloy was thought to provide the best fixation, also for cemented THA [6, 35, 52]. Short-term followup analyses at a minimum of 2 years (2-5 years) clearly showed the efficacy of cemented and cementless THAs in relieving pain and restoring function [52]. However, at midterm followup (mean, 6.3 years), issues such as increased polyethylene wear and loosening of the cemented and cementless acetabular sockets and the cemented stem were observed [35]. Because many patients undergoing THA live 20 or more years after their surgical procedure, long-term followup is critical.
The purpose of this study was to present longer-term followup of our RCT and to answer the following questions: (1) which mode of fixation, cemented or cementless, provided the best long-term overall socket and stem implant survivorship; (2) were there patient (age and gender), surgeon, or implant factors associated with poorer outcomes; and (3) were there lessons that we might learn from this unique RCT with up to 22 years of followup?
Patients and Methods
The study was performed between October 1987 and January 1992 [35, 52]. Briefly, patients with any age between 18 and 75 years were eligible for the study if they had osteoarthritis of the hip and were undergoing a unilateral primary THA that was performed by the two senior surgeons (RB, CR) using a direct lateral approach (Supplemental Table 1. Supplemental Website Materials; supplemental materials are available with the online version of CORR). Randomization was computer-generated and stratified by surgeon. At initiation of the study, a total sample size of 300 patients was calculated to provide 80% power to detect a difference between the two groups of 3.25 points or greater in the Harris hip score and 10% in the 10-year revision rate [35]. Patients were evaluated for revision of either of the components and for availability to followup at a minimum of 17 years. If the patients did not have a minimum 17-year followup, they either were contacted by phone or the family physician was contacted for information regarding revision status and survivorship of the patient. Patients who had revision surgery of only one component, thereby leaving the other component in place, also were evaluated for the same criteria to determine the status of the retained component. We obtained prior approval of the Institutional Review Board of our hospital and all patients had signed informed consent for participation in the study.
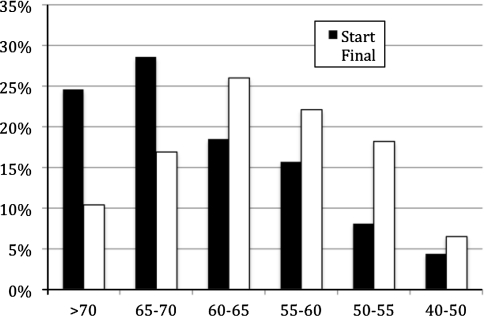
A total of 250 patients were randomized to either a cementless (N = 126) (Fig. 1) or cemented (N = 124) (Fig. 2) THA (Supplemental Table 1. Supplemental Website Materials; supplemental materials are available with the online version of CORR). The patient demographics in both groups were comparable at the time of randomization and at final followup (Supplemental Table 2. Supplemental Website Materials; supplemental materials are available with the online version of CORR) [35]. The minimum followup was 17 years (mean, 19.5 years; range, 17–22 years). One hundred twenty-seven patients had died (51%), and 12 (4.8%) were lost to followup. Fifty-five female patients (47%) had died in comparison to 73 male patients (55%) (p = 0.098) at a mean of 13 years (range, 1–21 years) after the index procedure. The percentage of patients who had died differed between age groups. Greater than 80% of the patients who were older than 70 years at the time of surgery had died, whereas the death rate of the 50- to 65-year-old patient population varied from 10% to 35%. Thirty-one patients (12%) refused to continue with all of the health-related quality-of-life followups, but they continued to attend our regular followup clinics. Minimum 17-year followup data for 12 patients (4.8%) with a primary THA were not available and these patients were considered lost to followup. At initiation of the study, 53% of all data were from patients 65 years or older, but at final followup, only 36% of all available data were from patients 65 years or older (Fig. 3). The data of only 14% (older than 70 years) to 35% (65–70 years) of patients 65 years or older were still available at final followup, whereas the data of 50% to 70% of patients between 50 and 65 years of age were available for evaluation at a minimum of 17 years. After 17 years, 60% of the available data were from patients between 50 and 65 years at the time of surgery (Fig. 3). The minimum 17-year followup data for 52 patients of the cementless group and 41 patients of the cemented group were available. Their mean age at final followup was 80 years (range, 61–96 years). Results for deceased patients and those lost to followup were not included as failed results in the survivorship analysis.
Fig. 1.
An overview of the followup for patients in the cementless group is shown.
Fig. 2.
An overview of the followup for patients in the cemented group is shown.
Fig. 3.
An age group representation at the beginning of the study and at final followup is shown.
The Mallory-Head total hip system (Biomet, Warsaw, IN, USA) seemed ideal for a RCT because the distinct cemented and cementless components were inserted with common instrumentation [6]. Both surgeons were experienced hip surgeons and had been using both systems before the presented study [46]. Both femoral stems were made from titanium (Ti) alloy. The ultrahigh-molecular-weight polyethylene (UHMWP) used was sterilized by gamma-in-air sterilization. All femoral heads were 28 mm in diameter and fabricated from Ti alloy hardened by ion implantation, a technique popular in 1987. The cemented acetabular socket was nonmodular and backed with a Ti alloy metal backing. The modular, cementless, HexLox acetabular component featured a Ti alloy shell and nonhemispheric UHMWP/shell interface. The cementless acetabular and femoral components had a plasma spray ongrowth surface.
At initiation of the study, patients were requested to attend the clinic every 2 years after the first postoperative year. Patients were assessed using validated disease-specific scores of which the Harris hip score was used throughout the followup period [35]. AP radiographs of the pelvis and cross-table lateral radiographs of the hip were made preoperatively and at each followup. Component stability and wear of the polyethylene liner were assessed by one observer (KC) according to previously described criteria [13, 23, 25, 26, 29, 31, 36, 40, 45, 46]. A cementless stem was considered unstable if there was progressive subsidence or a circumferential radiolucent or radiodense line around the porous coating [31, 45, 46]. A cemented stem was considered unstable in the presence of cement cracks, subsidence, or fracture of the stem [22, 23]. The stem was classified as possibly loose if only radiolucent lines without migration were present [25, 26, 36]. The location of radiolucent lines around the cup was recorded in the three zones as described by DeLee and Charnley [13]. The radiolucent lines were categorized as no radiolucency or radiolucency greater than 2 mm [29]. Osteolysis was defined as a circular or oval area of distinct bone loss. Evidence of migration was measured on two consecutive radiographs. The acetabular component was considered loose if there was 3 mm or greater migration from either the interteardrop or vertical lines, or a change of 4° or greater in the abduction angle [40]. The cup was considered possibly loose if there were radiolucent lines in the three zones without migration being seen on two consecutive radiographs.
The different research questions were evaluated with the following statistical methods: (1) Similar to the Australian National Joint Replacement Registry, we made the distinction between major (component) and minor revisions (liner and head exchange) [3]. The Kaplan-Meier (K-M) predicted survivorship method was used to generate survivorship curves with 95% confidence intervals and to determine predicted cumulative survivorship at 5, 10, 15, and 20 years. Cox regression and K-M were used repeatedly with multiple end-point variables: any revision THA, aseptic revision THA, aseptic acetabular cup revision, aseptic femoral stem revision, and aseptic liner/head exchange. (2) As with the Australian National Joint Replacement Registry, age at surgery was dichotomized (younger than 65 or 65 years or older) to be analyzed as a categorical variable. Cross-tabulation with chi square and Fisher’s exact test was used to determine significance in the distribution of age and gender across THA groups. This statistical method also was used to investigate revision rates across THA group, age category, and gender. Cox regression analysis was performed with THA fixation group, age, and gender as covariates to determine their effect on failure. (3) Based on the revision rates observed in this study, sample size calculations were made to assess the effect of excluding older patients (65 years or older) from a future RCT or changing the length of time for which patients are maximally followed up. Sample size calculations were done using nQuery Advisor 5.0 (Statistical Solutions, Saugus, MA, USA). Rather than assuming an exponential distribution for the events or dropouts, observed event and dropout rates at 1 to 20 years were used as input. Also, it was assumed that patients were followed for a fixed time (unless they dropped out early) and that after this fixed time, patients no longer are followed up, even if the study is still ongoing at that time. Sample size calculations were done using data for the whole population and for patients younger than 65 years. The calculations also were made for followups of 7, 10, and 15 years. The required number of patients per group to achieve 80% statistical power when assessing a log rank test at the 5% significance level was calculated. Finally, the Mann-Whitney U test for nonparametric data was used to determine differences in Harris hip score outcome between the two THA groups.
Results
Seventy-nine of the 238 hips available for followup (33%) were revised. The survivorship of cementless THA was significantly better than cemented THA from the 10-year followup term (p = 0.020) (Supplemental Table 3. Supplemental Website Materials; supplemental materials are available with the online version of CORR). Forty-two of 42 (100%) cementless stems and 23 of 24 (96%) primary cementless sockets were radiographically stable at a minimum of 17 years. Twenty of 21 (95%) cemented stems were radiographically stable whereas only four of eight (50%) surviving cemented cups were radiographically stable after more than 17 years. None of the implants was revised for instability problems.
Cemented THA, age younger than 65 years at the time of surgery, and male gender predicted higher risk of revision and lower survivorship (Table 1). Age was associated with the largest risk of revision (p < 0.001; risk = 3.21). Considering only aseptic socket revisions, age was the only predictor for an increased risk of revision (p = 0.035; risk = 9.39) indicating that patients younger than 65 years at the time of surgery were 9.39 times more likely to undergo a major socket revision. Cemented stem fixation (risk = 2.3) and younger age (risk = 2.5) were predictors for stem failure. None of the covariates were predictive for liner/head exchange. Age at the time of surgery significantly influenced the revision rates of the THA systems with significantly more revisions in the younger age group (p < 0.001) (Table 2). In this age group, cementless sockets had significantly lower major revision rates (p = 0.01) (Table 3). In the older age group, there was no difference in revision rates between groups (Supplemental Table 4. Supplemental Website Materials; supplemental materials are available with the online version of CORR). The cementless stems had significantly lower failure rates regardless of age at the time of surgery (Table 3). The overall revision rates between genders were similar (Supplemental Table 5. Supplemental Website Materials; supplemental materials are available with the online version of CORR). In males, the K-M survivorship of cementless stems was better (p < 0.001). However, the survivorship of both THA systems was similar (p = 0.4) owing to the similar survivorships of the sockets (p = 0.2) (Table 4). In females, the survivorship of the cementless THA was better (p = 0.001) on the femoral and acetabular sides (Table 4).
Table 1.
Cox regression analysis of cemented fixation, age, and gender as risk factors for revision
| Variables | All aseptic revision THRs | Aseptic acetabular cup revisions | Aseptic femoral stem revisions | Aseptic liner/head exchanges | ||||
|---|---|---|---|---|---|---|---|---|
| Significance level | Risk* | Significance level | Risk* | Significance level | Risk* | Significance level | Risk* | |
| THR group (cemented) | p = 0.006 | 1.91 | p = 0.937 | p = 0.002 | 2.3 | p = 0.894 | ||
| Age (< 65 years) | p < 0.001 | 3.21 | p = 0.035 | 9.39 | p = 0.001 | 2.54 | p = 0.239 | |
| Gender (male) | p = 0.011 | 1.83 | p = 0.064 | p = 0.051 | p = 0.465 | |||
*risk to revision is reported only for variables that were significant in each Cox regression analysis.
Table 2.
Revision rates stratified per age group (< or ≥ 65 years)
| Revision rate | THR revisions | Stem revisions | Socket revisions | Liner exchanges | ||||
|---|---|---|---|---|---|---|---|---|
| < 65 years | ≥ 65 years | < 65 years | ≥ 65 years | < 65 years | ≥ 65 years | < 65 years | ≥ 65 years | |
| Sample size (number) | 117 | 133 | 117 | 133 | 117 | 133 | 117 | 133 |
| Revisions (number) | 55 | 36 | 13 | 10 | 41 | 20 | 8 | 1 |
| Revision rate (%) | 47.0% | 27.1% | 11.1% | 7.5% | 35.0% | 15.0% | 6.8% | 0.8% |
| Revision rate significanceβ | p < 0.001 | p = 0.383 | p < 0.001 | p = 0.014 | ||||
β= Significance for revision rate determined by two-way cross tabulation with Fisher’s Exact test for significance.
Table 3.
Revision rates for patients younger than 65 years at time of surgery
| Survivorship | THR revisions | Stem revisions | Socket revisions | Liner exchanges | ||||
|---|---|---|---|---|---|---|---|---|
| Cementless | Cemented | Cementless | Cemented | Cementless | Cemented | Cementless | Cemented | |
| Revision rate | 36.7% | 57.9% | 0.0% | 22.8% | 23.3% | 47.4% | 13.3% | 0.0% |
| Significance levelβ | p = 0.040 | p < 0.001 | p = 0.011 | p = 0.006 | ||||
| Kaplan-Meier survivorship | ||||||||
| 5 years | 1 | 0.945 ± 0.031 | 1 | 0.945 ± 0.031 | 1 | 0.945 ± 0.031 | 1 | 1 |
| 10 years | 0.912 ± 0.038 | 0.795 ± 0.055 | 1 | 0.867 ± 0.047 | 0.929 ± 0.034 | 0.849 ± 0.049 | 0.982 ± 0.018 | 1 |
| 15 years | 0.706 ± 0.062 | 0.506 ± 0.071 | 1 | 0.770 ± 0.062 | 0.793 ± 0.056 | 0.580 ± 0.073 | 0.890 ± 0.047 | 1 |
| 20 years | 0.557 ± 0.075 | 0.297 ± 0.0763 | 1 | 0.675 ± 0.086 | 0.714 ± 0.067 | 0.345 ± 0.084 | 0.780 ± 0.076 | 1 |
| Significance levelγ | p = 0.018 | p < 0.001 | p = 0.010 | p = 0.024 | ||||
β= Significance for revision rate determined by two-way cross tabulation with Fisher’s Exact test for significance; γ = significance for Kaplan-Mieier survivorship determined by Breslow (generalized Wolcoxon) test of equality of survival distributions.
Table 4.
Revision rates of the stem, socket, and THR system stratified to gender
| Gender | THR revisions | Stem revisions | Socket revisions | Liner exchanges | ||||
|---|---|---|---|---|---|---|---|---|
| Cementless | Cemented | Cementless | Cemented | Cementless | Cemented | Cementless | Cemented | |
| Males | ||||||||
| Revision rate | 32.9% | 34.9% | 0.0% | 19.0% | 22.9% | 30.2% | 10.0% | 0.0% |
| RR SLβ | p = 0.854 | p < 0 .001 | p = 0.330 | p = 0.014 | ||||
| K-M SLγ | p = 0.429 | p < 0.001 | p = 0.226 | p = 0.025 | ||||
| Females | ||||||||
| Revision rate | 14.0% | 38.3% | 0.0% | 18.3% | 10.5% | 33.3% | 3.5% | 0.0% |
| RR SLβ | p = 0.003 | p = 0.001 | p = 0.003 | p = 0.239 | ||||
| K-M SLγ | p = 0.001 | p = 0.001 | p = 0.001 | p = 0.222 | ||||
β= Significance for revision rate determined by two-way cross tabulation with Fisher’s Exact test for significance; γ = Significance for Kaplan-Mieier Survivorship determined by Breslow (generalized Wolcoxon) test of equality of survival distributions. RR SL = revision rate significance level; K-M SL = Kaplan-Meier significance level.
Sample size calculations were made using data for the whole population (aged 18–75 years) and for patients younger than 65 years. The required number of patients per group to achieve 80% statistical power when assessing a log rank test at the 5% significance level was calculated (Table 5). This calculation showed that the number of patients that should be included to detect a difference in survivorship between both THA designs depends on the expected followup period and the age of the patient population. Including only patients younger than 65 years in a RCT that is planned for at least 10 or 15 years of followup would require 60 and 40 patients, respectively, in each treatment group. However, the numbers would have to be 110 and 100 patients if patients 65 years or older also are included.
Table 5.
Sample size calculations for estimated length of followups
| Patient group | Length of followup (years) | ||
|---|---|---|---|
| 7 | 10 | 15 | |
| All ages included | 140* | 110 | 100 |
| Only age < 65 years included | 135^ | 63 | 40 |
* minimum calculated number of patients that should be included in a RCT with an anticipated followups of 7, 10, and 15 years if all ages are included, and when only patients < 65 years old are included^.
Discussion
RCTs are considered the gold standard for study design in evidence-based medicine [28]. Despite the lack of consensus on the best fixation mode for THA, we are not aware of any RCT that compared long-term survivorship of two different fixation modes in THA. The purpose of this study was threefold. First, we compared the long-term survivorship of the Mallory-Head THA either implanted with or without cement. Second, we aimed to evaluate which parameters might influence the long-term survivorship of both THA designs. Third, we assessed our long-term experience with this single-center RCT to set up guidelines for any future RCTs on THA.
We note several limitations. First, one of the risks of initiating a long-term followup trial of a THA system is that the implant has become obsolete at finalization of the trial. Moreover, the failure mechanisms observed in this study are implant-specific and related to the known flaws of the designs used. However, some valid conclusions regarding the long-term survivorship can be drawn. Second, the calculated sample sizes for future RCTs can be considered as the minimum sample sizes because they are based on the comparison of designs that are in retrospect associated with important flaws and shortcomings. Comparing designs with a higher level of quality can require more patients be included or extending the followup time. Third, a possible criticism is whether the results are generalizable to other cemented or cementless THAs or to all surgeons. However, the identification of gender and age as important variables for implant survivorship are in agreement with the intermediate findings of the registries, which can be considered representative of the orthopaedic community at large [3, 38, 47].
The Ti alloy, tapered stem was associated with an excellent 20-year survivorship with only one revision being performed for a periprosthetic fracture. None of the stems was revised for aseptic loosening. With this stem design, a survivorship at least comparable or even better than that of other cementless and cemented stem designs could be achieved [1, 2, 4, 5, 7, 8, 10, 21, 22, 29, 32, 34, 39, 43, 48, 49, 56, 58, 61, 62, 64]. It generally is accepted that a cemented metal-backed socket, a Ti femoral head, and a Ti alloy cemented stem inserted with a ream-and-broach technique are not optimal features for a cemented design to obtain good long-term survivorship. This also was shown in our study. The cementless socket design had a better survivorship than the cemented socket but less optimal results as compared with newer-generation cementless sockets [20, 32–34, 41, 44, 57, 59]. Initial cementless fixation was not the problem, but rather polyethylene wear and periacetabular osteolysis. The use of a single offset stem and a Ti alloy femoral head probably also contributed to the wear rates in our patients [14, 16, 42, 54, 55].
In this randomized controlled design we found age and gender to be important prognosticators for THA failure. This is in concert with some prospective reports and the registry data, however there were some interesting findings [3, 5, 47, 63]. First, we were not able to identify a difference in survivorship of sockets in the older age group. In other words, the cemented socket was more likely to survive the elderly patient, thereby obscuring the real shortcomings of the implant. This finding questions the efficacy of including elderly patients in long-term RCTs. Second, as a group, males did not have higher revision rates than females. However, there were differences between fixation modes within gender. The requirements of implants to withstand the activity level of patients thus are gender-specific with the most strenuous requirements being for male patients. As with age, the distinction between genders should be made in reports on THA survivorship.
Some lessons can be learned from our RCT. First, only 73% of the calculated patients who had met the inclusion criteria actually participated in the trial. This problem might be easier to overcome in a multicenter trial. Second, at a minimum of 10 years, the difference in Harris hip score between groups was greater than 3.25, as the study was designed to find. However, this difference was not significant (p = 0.129) because of large variations. This indicates that multiple scores should be used, as the variability is probably score dependent. Third, the goal to identify a difference in survivorship of greater than 10% between groups was achieved by no earlier than 10 years of followup. The difference in survivorship between the stems was apparent at an early followup interval of 6 years [35], but because the cementless socket also has nonoptimal features, it took 10 years before the survivorship of the cementless THA was better than the cemented THA. This followup term might even be markedly longer in case one would be comparing implants with improved design features. Fourth, older patients generally have lower activity levels and they are more likely to die before implant failure. Only 26% of all revisions were in the age group 65 years or older. We conclude that the efficacy of this RCT would have been greater if only patients younger than 65 years would have been included because 50% fewer patients would have been recruited without changing the conclusions of the study. However, the life expectancy of the contemporary patient population probably is higher than that of the same patient cohort from 20 years ago. We hypothesize that also including patients between 65 and 70 years of age probably would not decrease the efficacy of a future RCT.
We found that cementless tapered stems were associated with an excellent 20-year survivorship. We suggest that future projects can be enhanced by randomizing patients in specific patient cohorts stratified to age and gender in multicenter RCTs to speed up the recruitment process. Including only patients younger than 65 to 70 years might improve the efficacy of a RCT as this would require a considerably smaller patient cohort with the highest risk for revision and the best chance for long-term followup availability. A minimum 10-year followup period should be anticipated. Improving the efficacy of a RCT is not only cost- and time-efficient but also minimizes the number of subjects that are exposed to any potential risks or flaws associated with the investigated implants.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgments
We thank Andreas Laupacis for his outstanding work in setting up this study. We also thank Ann Belmans, department of Biostatistics, KU Leuven, Belgium, for excellent support and advice in the statistical evaluations of this study.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Aldinger PR, Jung AW, Breusch SJ, Ewerbeck V, Parsch D. Survival of the cementless Spotorno stem in the second decade. Clin Orthop Relat Res. 2009;467:2297–2304. doi: 10.1007/s11999-009-0906-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aldinger PR, Jung AW, Pritsch M, Breusch S, Thomsen M, Ewerbeck V, Parsch D. Uncemented grit-blasted straight tapered titanium stems in patients younger than fifty-five years of age: fifteen to twenty-year results. J Bone Joint Surg Am. 2009;91:1432–1439. doi: 10.2106/JBJS.H.00297. [DOI] [PubMed] [Google Scholar]
- 3.Australian Orthopaedic Association. National Joint Replacement Registry Annual Report 2008. Available at: http://www.dmac.adelaide.edu.au/aoanjrr/publications.jsp?section=reports2008. Accessed January 6, 2009.
- 4.Belmont PJ, Jr, Powers CC, Beykirch SE, Hopper RH, Jr, Engh CA, Jr, Engh CA. Results of the anatomic medullary locking total hip arthroplasty at a minimum of twenty years: a concise follow-up of previous reports. J Bone Joint Surg Am. 2008;90:1524–1530. doi: 10.2106/JBJS.G.01142. [DOI] [PubMed] [Google Scholar]
- 5.Berry DJ, Harmsen WS, Cabanela ME, Morrey BF. Twenty-five-year survivorship of two thousand consecutive primary Charnley total hip replacements: factors affecting survivorship of acetabular and femoral components. J Bone Joint Surg Am. 2002;84:171–177. doi: 10.2106/00004623-200202000-00002. [DOI] [PubMed] [Google Scholar]
- 6.Biomet Inc. Product Information Manual, Mallory-Head Total Hip Arthroplasty. Warsaw, IN: Biomet Inc; 1990.
- 7.Bourne RB, Rorabeck CH, Patterson JJ, Guerin J. Tapered titanium cementless total hip replacements: a 10- to 13-year followup study. Clin Orthop Relat Res. 2001;393:112–120. doi: 10.1097/00003086-200112000-00013. [DOI] [PubMed] [Google Scholar]
- 8.Buckwalter AE, Callaghan JJ, Liu SS, Pedersen DR, Goetz DD, Sullivan PM, Leinen JA, Johnston RC. Results of Charnley total hip arthroplasty with use of improved femoral cementing techniques: a concise follow-up, at a minimum of twenty-five years, of a previous report. J Bone Joint Surg Am. 2006;88:1481–1485. doi: 10.2106/JBJS.E.00818. [DOI] [PubMed] [Google Scholar]
- 9.Callaghan JJ, Dysart SH, Savory CG. The uncemented porous-coated anatomic total hip prosthesis: two-year results of a prospective consecutive series. J Bone Joint Surg Am. 1988;70:337–346. [PubMed] [Google Scholar]
- 10.Callaghan JJ, Liu SS, Firestone DE, Yehyawi TM, Goetz DD, Sullivan J, Vittetoe DA, O’Rourke MR, Johnston RC. Total hip arthroplasty with cement and use of a collared matte-finish femoral component: nineteen to twenty-year follow-up. J Bone Joint Surg Am. 2008;90:299–306. doi: 10.2106/JBJS.G.00095. [DOI] [PubMed] [Google Scholar]
- 11.Campbell AC, Rorabeck CH, Bourne RB, Chess D, Nott L. Thigh pain after cementless hip arthroplasty: annoyance or ill omen. J Bone Joint Surg Br. 1992;74:63–66. doi: 10.1302/0301-620X.74B1.1732268. [DOI] [PubMed] [Google Scholar]
- 12.Collis DK. Cemented total hip replacement in patients who are less than fifty years old. J Bone Joint Surg Am. 1984;66:353–359. [PubMed] [Google Scholar]
- 13.DeLee JB, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res. 1976;121:20–32. [PubMed] [Google Scholar]
- 14.Devane PA, Horne JG. Assessment of polyethylene wear in total hip replacement. Clin Orthop Relat Res. 1999;369:59–72. doi: 10.1097/00003086-199912000-00007. [DOI] [PubMed] [Google Scholar]
- 15.Dodge BM, Fitzrandolph R, Collins DN. Noncemented porous-coated anatomic total hip arthroplasty. Clin Orthop Relat Res. 1991;269:16–24. [PubMed] [Google Scholar]
- 16.Dolhain P, Tsigaras H, Bourne RB, Rorabeck CH, Mac Donald SJ, Mc Calden R. The effectiveness of dual offset stems in restoring offset during total hip replacement. Acta Orthop Belg. 2002;68:490–499. [PubMed] [Google Scholar]
- 17.Dorr LD, Takei GK, Conaty JP. Total hip arthroplasties in patients less than forty-five years old. J Bone Joint Surg Am. 1983;65:474–479. [PubMed] [Google Scholar]
- 18.Engh CA, Bobyn JD, Glassman AH. Porous-coated hip replacement: the factors governing bone ingrowth, stress shielding, and clinical results. J Bone Joint Surg Br. 1987;69:45–55. doi: 10.1302/0301-620X.69B1.3818732. [DOI] [PubMed] [Google Scholar]
- 19.Engh CA, McGovern TF, Engh CA Jr, Macalino GE. Clinical experience with the anatomic medullary locking (AML) prosthesis for total hip replacement. In: Morrey BF, ed. Biological, Material, and Mechanical Considerations of Joint Replacement. New York, NY: Raven Press; 1993:167–184.
- 20.Firestone DE, Callaghan JJ, Liu SS, Goetz DD, Sullivan PM, Vittetoe DA, Johnston RC. Total hip arthroplasty with a cemented, polished, collared femoral stem and a cementless acetabular component: a follow-up study at a minimum of ten years. J Bone Joint Surg Am. 2007;89:126–132. doi: 10.2106/JBJS.E.01214. [DOI] [PubMed] [Google Scholar]
- 21.Garcia-Cimbrelo E, Cruz-Pardos A, Madero R, Ortega-Andreu M. Total hip arthroplasty with use of the cementless Zweymuller Alloclassic system: a ten to thirteen-year follow-up study. J Bone Joint Surg Am. 2003;85:296–303. doi: 10.2106/00004623-200302000-00017. [DOI] [PubMed] [Google Scholar]
- 22.Grubl A, Chiari C, Gruber M, Kaider A, Gottsauner-Wolf F. Cementless total hip arthroplasty with a tapered, rectangular titanium stem and a threaded cup: a minimum ten-year follow-up. J Bone Joint Surg Am. 2002;84:425–431. doi: 10.2106/00004623-200203000-00014. [DOI] [PubMed] [Google Scholar]
- 23.Gruen TA, McNeice GM, Amstutz HC. “Modes of failure” of cemented stem type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res. 1979;141:17–27. [PubMed] [Google Scholar]
- 24.Hallan G, Lie SA, Furnes O, Engesaeter LB, Vollset SE, Havelin LI. Medium- and long-term performance of 11516 uncemented primary femoral stems from the Norwegian arthroplasty register. J Bone Joint Surg Br. 2007;89:1574–1580. doi: 10.1302/0301-620X.89B12.18969. [DOI] [PubMed] [Google Scholar]
- 25.Harris WH, McCarthy JC, Jr, O’Neill DA. Femoral component loosening using contemporary techniques of femoral cement fixation. J Bone Joint Surg Am. 1982;64:1063–1067. [PubMed] [Google Scholar]
- 26.Harris WH, McGann WA. Loosening of the femoral component after use of the medullary-plug cementing technique: follow-up note with a minimum five-year follow-up. J Bone Joint Surg Am. 1986;68:1064–1066. [PubMed] [Google Scholar]
- 27.Hooper GJ, Rothwell AG, Stringer M, Frampton C. Revision following cemented and uncemented primary total hip replacement: a seven-year analysis from the New Zealand Joint Registry. J Bone Joint Surg Br. 2009;91:451–458. doi: 10.1302/0301-620X.91B4.21363. [DOI] [PubMed] [Google Scholar]
- 28.Hoppe DJ, Schemitsch EH, Morshed S, Tornetta P, III, Bhandari M. Hierarchy of evidence: where observational studies fit in and why we need them. J Bone Joint Surg Am. 2009;91(suppl 3):2–9. doi: 10.2106/JBJS.H.01571. [DOI] [PubMed] [Google Scholar]
- 29.Hozack WJ, Rothman RH, Eng K, Mesa J. Primary cementless hip arthroplasty with a titanium plasma sprayed prosthesis. Clin Orthop Relat Res. 1996;333:217–225. doi: 10.1097/00003086-199612000-00023. [DOI] [PubMed] [Google Scholar]
- 30.Johnsen SP, Sørensen HT, Lucht U, Søballe K, Overgaard S, Pedersen AB. Patient-related predictors of implant failure after primary total hip replacement in the initial, short- and long-terms: a nationwide Danish follow-up study including 36, 984 patients. J Bone Joint Surg Br. 2006;88:1303–1308. doi: 10.1302/0301-620X.88B10.17399. [DOI] [PubMed] [Google Scholar]
- 31.Johnston RC, Fitzgerald RH, Jr, Harris WH, Poss R, Muller ME, Sledge CB. Clinical and radiographic evaluation of total hip replacement: a standard system of terminology for reporting results. J Bone Joint Surg Am. 1990;72:161–168. [PubMed] [Google Scholar]
- 32.Kim YH, Kim JS, Yoon SH. Long-term survivorship of the Charnley Elite Plus femoral component in young patients. J Bone Joint Surg Br. 2007;89:449–454. doi: 10.1302/0301-620X.89B4.18665. [DOI] [PubMed] [Google Scholar]
- 33.Klaassen M, Martinez-Villalobos M, Pietrzak WS, Mangino GP, Guzman DC. Midterm survivorship of a press-fit, plasma-sprayed, tri-spike acetabular component. J Arthroplasty. 2009;24:391–399. doi: 10.1016/j.arth.2007.10.034. [DOI] [PubMed] [Google Scholar]
- 34.Klapach AS, Callaghan JJ, Goetz DDm Olejniczak JP, Johnston RC. Charnley total hip arthroplasty with use of improved cementing techniques: a minimum twenty-year follow-up study. J Bone Joint Surg Am. 2001;83:1840–1848. doi: 10.2106/00004623-200112000-00012. [DOI] [PubMed] [Google Scholar]
- 35.Laupacis A, Bourne R, Rorabeck C, Feeny D, Tugwell P, Wong C. Comparison of total hip arthroplasty with and without cement: a randomized trial. J Bone Joint Surg Am. 2002;84:1823–1828. doi: 10.2106/00004623-200210000-00013. [DOI] [PubMed] [Google Scholar]
- 36.Loudon JR, Charnley J. Subsidence of the femoral prosthesis in total hip replacement in relation to the design of the stem. J Bone Joint Surg Br. 1980;62:450–453. doi: 10.1302/0301-620X.62B4.7430222. [DOI] [PubMed] [Google Scholar]
- 37.Mäkelä K, Eskelinen A, Pulkkinen P, Paavolainen P, Remes V. Cemented total hip replacement for primary osteoarthritis in patients aged 55 years or older: results of the 12 most common cemented implants followed for 25 years in the Finnish Arthroplasty Register. J Bone Joint Surg Br. 2008;90:1562–1569. doi: 10.2106/JBJS.G.00870. [DOI] [PubMed] [Google Scholar]
- 38.Mâkelä KT, Eskelinen A, Pulkkinen P, Paavolainen P, Remes V. Total hip arthroplasty for primary osteoarthritis in patients fifty-five years of age or older: an analysis of the Finnish arthroplasty registry. J Bone Joint Surg Am. 2008;90:2160–2170. doi: 10.2106/JBJS.G.00870. [DOI] [PubMed] [Google Scholar]
- 39.Mallory TH, Lombardi AV Jr, Leith JR, Fujita H, Hartman JF, Capps SG, Kefauver CA, Adams JB, Vorys GC. Minimal 10-year results of a tapered cementless femoral component in total hip arthroplasty. J Arthroplasty. 2001;16(8 suppl 1):49–54. [DOI] [PubMed]
- 40.Massin P, Schmidt L, Engh CA. Evaluation of cementless acetabular component migration: an experimental study. J Arthroplasty. 1989;4:245–251. doi: 10.1016/S0883-5403(89)80020-8. [DOI] [PubMed] [Google Scholar]
- 41.McCalden RW, MacDonald SJ, Rorabeck CH, Bourne RB, Chess DG, Charron KD. Wear rate of highly cross-linked polyethylene in total hip arthroplasty: a randomized controlled trial. J Bone Joint Surg Am. 2009;91:773–782. doi: 10.2106/JBJS.H.00244. [DOI] [PubMed] [Google Scholar]
- 42.McGrory BJ, Morrey BF, Cahalan TD, An KN, Cabanela ME. Effect of femoral offset on range of motion and abductor muscle strength after total hip arthroplasty. J Bone Joint Surg Br. 1995;77:865–869. [PubMed] [Google Scholar]
- 43.McLaughlin JR, Lee KR. Total hip arthroplasty with an uncemented tapered femoral component. J Bone Joint Surg Am. 2008;90:1290–1296. doi: 10.2106/JBJS.G.00771. [DOI] [PubMed] [Google Scholar]
- 44.McNulty DE, Liao YS, Haas BD. The influence of sterilization method on wear performance of the low contact stress total knee system. Orthopedics. 2002;25(2 suppl 2):s243–s246. [DOI] [PubMed]
- 45.Mulliken BD, Bourne RB, Rorabeck CH, Nayak N. A tapered titanium femoral stem inserted without cement in a total hip arthroplasty: radiographic evaluation and stability. J Bone Joint Surg Am. 1996;78:1214–1225. doi: 10.2106/00004623-199608000-00012. [DOI] [PubMed] [Google Scholar]
- 46.Mulliken BD, Rorabeck CH, Bourne RB. Uncemented revision total hip arthroplasty: a 4-to-6-year review. Clin Orthop Relat Res. 1996;325:156–162. doi: 10.1097/00003086-199604000-00017. [DOI] [PubMed] [Google Scholar]
- 47.National Joint Registry. National Joint Registry for England and Wales: 4th Annual Report. Available at: http://www.njrcentre.org.uk/NjrCentre/Portals/0/Documents/England/Reports/NJR_AR_4.pdf. Accessed January 6, 2009.
- 48.Parvizi J, Sharkey PF, Hozack WJ, Orzoco F, Bissett GA, Rothman RH. Prospective matched-pair analysis of hydroxyapatite-coated and uncoated femoral stems in total hip arthroplasty: a concise follow-up of a previous report. J Bone Joint Surg Am. 2004;86:783–786. doi: 10.1302/0301-620X.86B6.15356. [DOI] [PubMed] [Google Scholar]
- 49.Purtill JJ, Rothman RH, Hozack WJ, Sharkey PF. Total hip arthroplasty using two different cementless tapered stems. Clin Orthop Relat Res. 2001;393:121–127. doi: 10.1097/00003086-200112000-00014. [DOI] [PubMed] [Google Scholar]
- 50.Ranawat CS, Atkinson RE, Salvati EA, Wilson PD., Jr Conventional total hip arthroplasty for degenerative joint disease in patients between the ages of forty and sixty years. J Bone Joint Surg Am. 1984;66:745–752. [PubMed] [Google Scholar]
- 51.Ritter MA, Keating EM, Faris PM. A porous polyethylene-coated femoral component of a total hip arthroplasty. J Arthroplasty. 1990;5:83–88. doi: 10.1016/S0883-5403(06)80014-8. [DOI] [PubMed] [Google Scholar]
- 52.Rorabeck CH, Bourne RB, Laupacis A, Feeny D, Wong C, Tugwell P, Leslie K, Bullas R. A double-blind study of 250 cases comparing cemented with cementless total hip arthroplasty: cost-effectiveness and its impact on health-related quality of life. Clin Orthop Relat Res. 1994;298:156–164. [PubMed] [Google Scholar]
- 53.Rothman RH, Cohn JC. Cemented versus cementless total hip arthroplasty: a critical review. Clin Orthop Relat Res. 1990;254:153–169. [PubMed] [Google Scholar]
- 54.Sakalkale DP, Sharkey PF, Eng K, Hozack WJ, Rothman RH. Effect of femoral component offset on polyethylene wear in total hip arthroplasty. Clin Orthop Relat Res. 2001;388:125–134. doi: 10.1097/00003086-200107000-00019. [DOI] [PubMed] [Google Scholar]
- 55.Schmalzried TP, Shepherd EF, Dorey FJ, Jackson WO, dela Rosa M, Fa’vae F, McKellop HA, McClung CD, Martell J, Moreland JR, Amstutz HC. The John Charnley Award: wear is a function of use, not time. Clin Orthop Relat Res. 2000;381:36–46. doi: 10.1097/00003086-200012000-00005. [DOI] [PubMed] [Google Scholar]
- 56.Schramm M, Keck F, Hohmann D, Pitto RP. Total hip arthroplasty using an uncemented femoral component with taper design: outcome at 10-year follow-up. Arch Orthop Trauma Surg. 2000;120:407–412. doi: 10.1007/PL00013771. [DOI] [PubMed] [Google Scholar]
- 57.Shen FW, McKellop HA. Interaction of oxidation and crosslinking in gamma-irradiated ultrahigh molecular-weight polyethylene. J Biomed Mater Res. 2002;61:430–439. doi: 10.1002/jbm.10203. [DOI] [PubMed] [Google Scholar]
- 58.Skutek M, Bourne RB, Rorabeck CH, Burns A, Kearns S, Krishna G. The twenty to twenty-five-year outcomes of the Harris design-2 matte-finished cemented total hip replacement: a concise follow-up of a previous report. J Bone Joint Surg Am. 2007;89:814–818. doi: 10.2106/JBJS.F.00837. [DOI] [PubMed] [Google Scholar]
- 59.Spak RT, Stuchin SA. Cementless porous-coated sockets without holes implanted with pure press-fit technique: average 6-year follow-up. J Arthroplasty. 2005;20:4–10. doi: 10.1016/j.arth.2004.09.025. [DOI] [PubMed] [Google Scholar]
- 60.Stauffer RN. Ten-year follow-up study of total hip replacement. J Bone Joint Surg Am. 1982;64:983–990. [PubMed] [Google Scholar]
- 61.Suckel A, Geiger F, Kinzl L, Wulker N, Garbrecht M. Long-term results for the uncemented Zweymuller/Alloclassic hip endoprosthesis: a 15-year minimum follow-up of 320 hip operations. J Arthroplasty. 2009;24:846–853. doi: 10.1016/j.arth.2008.03.021. [DOI] [PubMed] [Google Scholar]
- 62.Sutherland CJ, Wilde AH, Borden LS, Marks KE. A ten-year follow-up of one hundred consecutive Muller curved-stem total hip-replacement arthroplasties. J Bone Joint Surg Am. 1982;64:970–982. [PubMed] [Google Scholar]
- 63.Swedish Hip Arthroplasty Register. Annual Report 2006. Available at: www.jru.orthop.gu.se/. Accessed January 6, 2009.
- 64.Teloken MA, Bissett G, Hozack WJ, Sharkey PF, Rothman RH. Ten to fifteen-year follow-up after total hip arthroplasty with a tapered cobalt-chromium femoral component (tri-lock) inserted without cement. J Bone Joint Surg Am. 2002;84:2140–2144. doi: 10.2106/00004623-200212000-00003. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Below is the link to the electronic supplementary material.