Abstract
Background
The contribution provided by the popliteus tendon in patients undergoing TKA is poorly defined. Some authors believe the popliteus tendon is essential to a well-functioning arthroplasty, while others do not believe it provides a critical function.
Questions/purposes
The purposes of this study were to (1) evaluate the effect of resecting the popliteus tendon on knee ligament balancing in extension and flexion intraoperatively during posterior stabilized TKA; and (2) evaluate the effect of resecting the popliteus tendon on load distribution on the tibial plateau as determined by an in vitro single limb stance model during TKA.
Methods
We randomized 18 patients scheduled for a TKA into two groups, A and B. Once component trials were in place, the senior surgeon removed himself from the operating table to allow for a blinded trial. The first assistant then cut the popliteus tendon in Group A patients but not in Group B patients. The senior surgeon then returned to the table to reevaluate the subjective balance of the ligamentous structures of the knee in both extension and in flexion. A parallel cadaveric study was also completed using a sophisticated instrumented tibial plateau sensor in three knees.
Results
The senior surgeon was unable to detect a difference in the knee stability between knees with transected popliteal tendons and those with intact popliteal tendons. In vitro studies showed there was no change in load distribution between the medial and lateral plateaus once the popliteus tendon was transected.
Conclusions
Resection of the popliteus tendon does not appear to change the static balance of the knee.
Level of Evidence
Level II, prognostic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
The popliteus originates from the lateral femoral condyle, just distal to the lateral epicondyle, near the origin of the lateral collateral ligament. It inserts broadly in a triangular-shaped fashion along the posteromedial tibial surface for a distance of approximately 10 cm. The broad attachment forms the floor of the interior part of the popliteus fossa [9, 12]. The popliteus tendon runs between the fibrous capsule and synovial lining to the lateral surface of the lateral femoral condyle [12]. In extension, the popliteus tendon is posterior to the lateral collateral ligament and in flexion it resides just anterior to the lateral collateral ligament [12]. The popliteus muscle-tendon unit is an important part of the posterolateral corner of the native knee [4, 9, 11]. It is considered one of the main structures assisting in dorsolateral stability of the native knee [12]. It helps unlock the knee, rotates the tibia internally on the femur, and it prevents excessive external rotation of the tibia during knee flexion among other functions [9]. In general, the resection of a popliteus tendon in a native knee without symptomatic pathology is ill-advised.
However, the precise function of the popliteus tendon in patients with TKA is less well defined. In TKAs, the popliteus may not have the same critical function, as the arthroplasty itself may have more inherent stability in combination with arthroplasty patients often being lower demand. However, the tendon reportedly causes pain and discomfort by snapping over the femoral component during gait [2]. This snapping may occur if the joint line is elevated in patients with severe preoperative flexion contracture [2], so some surgeons will occasionally resect this tendon [10, 13]. Tendon snapping occasionally occurs after the knee has been balanced and the components have been placed so it important to understand the effect sectioning the tendon will have on soft tissue balance and whether it influences stability.
The purposes of this study were to (1) evaluate the effect of resecting the popliteus tendon on knee ligament balancing in extension and flexion intraoperatively during TKA; and (2) evaluate the effect of resecting the popliteus tendon on load distribution on the tibial plateau as determined by an in vitro single limb stance model during TKA.
Patients and Methods
Over a 2 month period at our tertiary care hospital, we enrolled 18 patients (six men and 12 women) scheduled for TKA and randomized each patient to either Group A (popliteus tendon resected) or Group B (popliteus tendon not resected). The sample size was determined by selecting a convenient number of patients to participate in the study over a two month time period. Only the first assistant surgeon was aware of the patient’s group via a randomly selected envelope at the beginning of the operation (Appendix 1). Randomization occurred by a simple system where nine externally identical envelopes were stuffed with assignment to Group A and nine envelopes were stuffed with assignment to Group B. These envelopes were shuffled and stored inside a larger container, and for each patient an envelope was chosen at random by first assistant surgeon. The average age was 73.2 years (range, 50–85 years). Eight patients had right-sided surgery, and 10 patients had left-sided surgery. We prior obtained institutional review board approval and patient informed consent.
Before beginning the operation, ROM, alignment, and an assessment of stability of the ACL, PCL, LCL, and MCL were recorded by the senior surgeon (RTT). Ligamentous stability was graded on a scale of 0 to 3 + [1]. Those without any asymmetry as compared to the contralateral leg and a stable ligamentous exam were graded 0. Grade 1 laxity was assigned to patients with gapping between 0 and 5 mm during stress testing, grade 2 was assigned to patients with 6-10 mm of gapping during stress testing, and grade 3 was assigned to patients with greater than 10 mm of gapping during stress testing. Pseudolaxity with firm endpoint was considered grade 0. Mean preoperative extension was 3.8° (range, −1° to 15°), mean preoperative flexion was 118.5° (range, 95°–125°), and mean preoperative alignment was −0.6°, with valgus being positive (range, −10° to 15°). ACL mean laxity was 0.2 on a scale of 0 to 4 (range, 0–2); no patient had PCL laxity; MCL mean laxity was 0.3 (range, 0–1); and LCL mean laxity was 0.2 (range, 0–1).
The senior surgeon was initially blinded to their randomization outcome. The posterior-stabilized TKA was performed by the senior surgeon and first assistant surgeon in the usual standard fashion, recording the amount of distal femur resected. The mean depth of distal femoral resection was 9.6 mm (range, 8–14 mm). All trial components were put into place and the senior surgeon analyzed the stability of the knee both in flexion and extension, in accordance with standard practice. Once the senior surgeon was satisfied with the ligamentous balance of the knee, the popliteus tendon was identified. The senior surgeon then moved away from the operating table to the corner of the operating room, turning his back to the operating table as to not be able to visualize the next step. Once the senior surgeon was “blinded,” the first assistant surgeon was given 60 seconds to either resect the popliteus tendon for those patients randomized to Group A, or perform sham maneuvers during the allotted time (turning on cautery but not actually cutting tissue, etc) for Group B.
The senior surgeon then returned to the operating table and analyzed the stability of the knee in flexion and extension to observe any change in the knee balance. The senior surgeon’s analysis was recorded as none, small, medium, or large. Once the senior surgeon had reported his analysis, it was revealed whether or not the tendon had actually been resected. For Group A, the knee was again analyzed to see if a difference could be detected. For Group B, the tendon was resected and stability was then reanalyzed, using the same system of identification of change (none, small, medium, large). This left all knees with a resected popliteus tendon. The remainder of the arthroplasty was carried out in the usual fashion. No followup beyond the time of operation was completed.
For the in vitro study, three fresh-frozen cadaveric knees were evaluated. This portion of the study was completed as a pilot study to help generate hypotheses. Using a standard medial parapatellar approach, the DePuy TKA system (DePuy Orthopaedics, Inc, Warsaw, IN) was used according to the senior author’s usual practice. The ACL and PCL ligaments were sacrificed. The distal femur was cut to 5° of valgus using an intramedullary alignment guide and the proximal tibia was cut perpendicular to the tibial axis with no posterior slope. The patella was left unresurfaced. The popliteus tendon was also dissected out for ease of resection once loaded in the material testing machine.
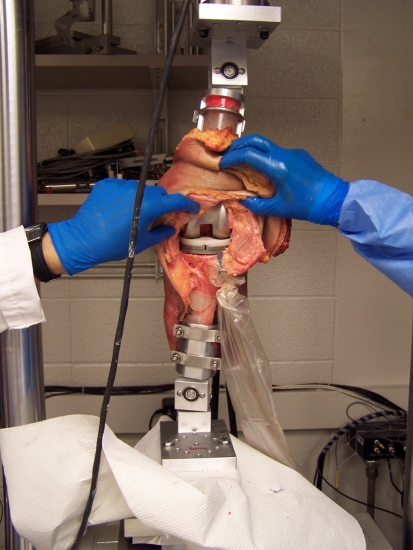
An Instrumented Dual Tibial Plateau Sensor (NK Biotechnical Corp, Golden Valley, MN) was inserted into the proximal portion of the tibia (Fig. 1). The tibial prosthesis included two independent plates, medial and lateral, which utilized strain gauge technology to measure force and the location of peak force during compressive loads. The trial polyethylene inserts were not posterior stabilized. The proximal femur and distal tibia were cut to approximately 15 cm and potted in cylindrical bone cement molds and the specimen was attached to a material testing machine (Model 312; MTS Corp, Eden Prairie, MN). The tibia and femur were mounted on custom hardware in a fixed position of 20° of flexion to simulate single-limb stance. The specimen was loaded axially with 100 pounds of force and the custom hardware restricted the knee to varus-valgus and rotational displacements (Fig. 1). The medial and lateral plateau force distributions were measured with the popliteus tendon intact. The tendon was then resected and the medial-lateral plateau force distribution was again measured.
Fig. 1.
A photograph shows the setup for the cadaveric study with instrumented tibial plateau sensor visible and the specimen under load of the material testing machine.
All data were analyzed using basic statistical techniques including mean, median, and standard deviation.
Results
The senior surgeon was unable to detect a difference in the knee stability in flexion and extension in all 18 cases comprising all of the members of Groups A and B. Even after learning the popliteus tendon had been resected, the senior surgeon was unable to manually or visibly perceive any change in the stability of the knee.
For the in vitro study, the mean medial tibial plateau load with the tendon intact was 64% (range, 51%–75%) and with the tendon resected was 63% (range, 49%–80%). The difference between these means was 1% difference in load.
Discussion
There is a vast amount of literature surrounding the native knee and the effects of an injury to the popliteus tendon and posterolateral corner of the knee [3]. These reports on both the isolated popliteus tendon rupture as well as posterolateral corner injuries are relatively common and provide the surgeon with insight on diagnosis and management [5]. The precise contribution the popliteus tendon provides in patients undergoing TKA is poorly defined, as shown by the relative paucity of literature discussing popliteus tendon dysfunction after TKA as compared to popliteus tendon dysfunction in native knees. Several studies describe the effects of sequential soft tissue releases [6–8]. Additionally, case reports have described postoperative treatment of snapping a popliteus tendon after total knee arthroplasty via arthroscopic versus open release [1]. These reports, however, do not provide any information about the stability of the knee after this tendon is released in any type of randomized fashion. Our study seeks to provide information as to whether there is risk of causing instability after resecting the popliteus tendon. The purposes of this study were to (1) evaluate the effect of resecting the popliteus tendon on knee ligament balancing in extension and flexion intraoperatively during TKA; and (2) evaluate the effect of resecting the popliteus tendon on load distribution on the tibial plateau as determined by an in vitro single limb stance model during TKA.
This study has limitations. First, the in vivo portion of the study is limited by the skill of the senior surgeon to detect any difference in stability. We know of no data documenting the intra- and interobserver variability in assessing stability. However, given the experience and surgical volume of the senior surgeon (> 2000 primary TKAs over the past 17 years), we believe this individual can reliably determine stability. Second, the sample size is small for the in vivo portion of the study; however, given the surgeon never noticed a difference in knee stability in any of the patients, we anticipate even if we expanded our sample size to 100 patients, minimal difference would be noted. Third, the in vivo portion of the study was completed with a posterior stabilized design which could alter the results, however, in our opinion, the inherent constraint in the posterior stabilized implant did not play a major role in providing varus/valgus stability. A secondary study would be valuable to determine if our results would be the same with a nonposterior stabilized implant. Fourth, the in vitro portion of the study is also limited by sample size. The cadaveric sample size was kept small because it was considered a pilot study and since the results showed almost no change in these first three samples, it was determined that a larger sample would be very unlikely to show a meaningful difference and therefore the study was discontinued. Three samples provide a 35% power to detect a 5% difference. The in vitro study is also limited since it only is analyzing the knee in the position of single-limb stance. This model ignores any difference seen in flexion, which could be assessed in the in vivo model.
A prior study by Whiteside [13] used angular deflection to determine the effect of sequential release of ligaments and tendons to understand the effect of selective lateral ligament release on stability in TKA, and concluded the popliteus tendon had little effect on the stability of the knee when other ligamentous were left in good condition. Our results agree with those prior findings [13]. Data from our cadaveric study show minimal change in the load distribution between the medial and lateral tibial plateaus after sectioning the popliteus tendon.
The popliteus tendon can snap over the posterior lateral condyle of the femoral component. It is a safe and reasonable practice to resect the popliteus tendon, especially when it is necessary to resect extra distal femur in the face of a marked preoperative flexion contracture to prevent snapping of the tendon. It should be kept in mind, in both the in vivo and in vitro study, only the popliteus tendon was resected. The posterolateral capsule was left alone. Removing the tendon does not appear to change the static balance of the knee. We conclude the sectioning of the popliteus tendon can be performed after components are cemented into place if need be, without destabilizing the knee. This, however, should not be an excuse for sloppy surgery. Resection of the popliteus tendon should be a planned maneuver when deemed appropriate by a skilled surgeon.
Acknowledgments
We thank all participants of the study and those individuals who assisted us in completing this study including Ms. Emily Miller, Dr. Rafael Sierra, and Dr. Mark Pagnano.
Appendix
Data Forms and Flowcharts Used for Study


Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Abate J. Dislocations and soft tissue injuries of the knee. In: Browner BD, Levine AM, Jupiter JB, Trafton PG, Krettek C, editors. Skeletal Trauma. 4. Philadelphia, PA: WB Saunders; 2009. pp. 2784–2790. [Google Scholar]
- 2.Allardyce TJ, Scuderi GR, Insall JN. Arthroscopic treatment of popliteus tendon dysfunction following total knee arthroplasty. J Arthroplasty. 1997;12:353–355. doi: 10.1016/S0883-5403(97)90037-1. [DOI] [PubMed] [Google Scholar]
- 3.Covey DC. Injuries of the posterolateral corner of the knee. J Bone Joint Surg Am. 2001;83:106–118. doi: 10.1302/0301-620X.83B1.10865. [DOI] [PubMed] [Google Scholar]
- 4.Chun YM, Kim SJ, Kim HS. Evaluation of the mechanical properties of posterolateral structures and supporting posterolateral instability of the knee. J Orthop Res. 2008;26:1371–1376. doi: 10.1002/jor.20596. [DOI] [PubMed] [Google Scholar]
- 5.Guha AR, Gorgees KA, Walker DI. Popliteus tendon rupture: a case report and review of the literature. Br J Sports Med. 2003;37:358–360. doi: 10.1136/bjsm.37.4.358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kanamiya T, Whiteside LA, Nakamura T, Mihalko WM, Steiger J, Naito M. Effect of selective lateral ligament release on stability in knee arthroplasty. Clin Orthop Relat Res. 2002;404:24–31. doi: 10.1097/00003086-200211000-00005. [DOI] [PubMed] [Google Scholar]
- 7.Krackow KA, Mihalko WM. Flexion-extension joint gap changes after lateral structure release for valgus deformity correction in total knee arthroplasty: a cadaveric study. J Arthroplasty. 1999;14:994–1004. doi: 10.1016/S0883-5403(99)90016-5. [DOI] [PubMed] [Google Scholar]
- 8.Matsueda M, Gengerke TR, Murphy M, Lew WD, Gustilo RB. Soft tissue release in total knee arthroplasty: cadaver study using knees without deformities. Clin Orthop Relat Res. 1999;366:264–273. doi: 10.1097/00003086-199909000-00034. [DOI] [PubMed] [Google Scholar]
- 9.Nyland J, Lachman N, Kocabey Y, Brosky J, Altun R, Caborn D. Anatomy, function, and rehabilitation of the popliteus musculotendinous complex. J Orthop Sports Phys Ther. 2005;35:165–179. doi: 10.2519/jospt.2005.35.3.165. [DOI] [PubMed] [Google Scholar]
- 10.Peters CL, Severson E, Crofoot C, Allen B, Erickson J. Popliteus tendon release in the varus or neutral knee: prevalence and potential etiology. J Bone Joint Surg Am. 2008;90(Suppl 4):40–46. doi: 10.2106/JBJS.H.00687. [DOI] [PubMed] [Google Scholar]
- 11.Seebacher JR, Inglis AE, Marshall JL, Warren RF. The structure of the posterolateral aspect of the knee. J Bone Joint Surg Am. 1982;64:536–541. [PubMed] [Google Scholar]
- 12.Ullrich K, Krudwig WK, Witzel U. Posterolateral aspect and stability of the knee joint. I. Anatomy and function of the popliteus muscle-tendon unit: an anatomical and biomechanical study. Knee Surg Sports Traumatol Arthrosc. 2002;10:86–90. doi: 10.1007/s00167-001-0268-5. [DOI] [PubMed] [Google Scholar]
- 13.Whiteside LA. Selective ligament release in total knee arthroplasty of the knee in valgus. Clin Orthop Relat Res. 1999;367:130–140. doi: 10.1097/00003086-199910000-00016. [DOI] [PubMed] [Google Scholar]