Abstract
Background
Control of distraction rate with an intramedullary skeletal kinetic distractor (ISKD) may be problematic and a high distraction rate may result in insufficient bone regenerate.
Questions/purposes
Are distraction problems preventable when using the ISKD, and what are the risk factors for and radiologic types of insufficient bone regenerate during ISKD lengthening?
Patients and Methods
We analyzed 37 consecutive ISKD femoral lengthening procedures in 35 patients with a mean age 33 ± 11 years and minimum followup of 12 months (average, 27 ± 9 months; range, 12–55 months). The average length gain was 42.8 ± 12.9 mm.
Results
Eight patients had problems during distraction: seven had “runaway nails” and one had a nondistracting nail. Insufficient bone regenerate developed in eight patients. Important risk factors were a distraction rate greater than 1.5 mm/day (9.1 times higher risk), age 30 years or older, smoking, and lengthening greater than 4 cm. Less important risk factors identified were creation of the osteotomy at the site of previous trauma or surgery and acute correction of associated deformities. We proposed a radiologic classification for failure of bone regeneration: partial regenerate failure (Type I) or complete failure resulting in a segmental defect subdivided according to a length of 3 cm or less (Type IIa) or greater than 3 cm (Type IIb).
Conclusions
Distraction problems with the ISKD were related mostly to internal malfunction of the lengthening mechanism. A distraction rate greater than 1.5 mm/day should be avoided in femoral intramedullary lengthening. Smoking should be a contraindication for femoral lengthening.
Level of Evidence
Level II, prognostic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Insufficient bone regeneration and nonunion are known complications of limb lengthening techniques [6, 7, 22]. The biology of bone regeneration and healing and factors that affect its rate during limb lengthening using different forms of external fixators were studied extensively in animal models and clinical settings (Table 1) [1, 3, 6, 7, 9, 10, 16–18, 22, 24, 28, 30–32]. One of the most critical factors affecting bone regeneration is the distraction rate and rhythm [1, 6, 17, 30]. Radiologic types of insufficient bone regeneration with limb lengthening using external fixators and treatment options have been described [21, 22].
Table 1.
Factors affecting bone regeneration and healing with distraction osteogenesis
| Group | Individual risk factors |
|---|---|
| Patient factors | Age |
| Smoking | |
| Nutritional status | |
| Metabolic diseases | |
| Etiology of shortening | |
| Drugs (nonsteroidal antiinflammatory drugs and cancer chemotherapy) | |
| Local factors | Vascular status |
| Previous surgical procedures | |
| Site of lengthening or distraction osteogenesis (femur or tibia) | |
| Technical (osteotomy) factors | Site of osteotomy (metaphyseal versus diaphyseal) |
| Osteotomy technique (osteotomy versus corticotomy) and the preservation of the blood supply (periosteal tissue) | |
| Initial diastasis | |
| Acute correction of associated deformities | |
| Biomechanical factors | Fixator stability |
| Fixator type (circular, unilateral) | |
| Postoperative factors | Latency period |
| Distraction rate and rhythm | |
| Distraction length | |
| Local infection |
During the last two decades, totally implantable lengthening nails were introduced to eliminate external fixator-associated complications with lower limb lengthening such as pin tract infection, transfixation of soft tissue and muscle contractures, joint stiffness, malalignment, neurovascular injuries, and refractures [2, 4, 11, 22, 23, 25]. These lengthening nails provide many advantages such as earlier rehabilitation, reduced risk of deep infections, reduced pain, and more rapid return to normal joint motion and activity, and therefore, improved patient comfort [2, 4, 11–13, 15, 26].
The intramedullary skeletal kinetic distractor (ISKD) is a mechanically activated nail with an internal ratchet mechanism. Lengthening is achieved by rotation around the long axis of the bone by 3° to 9° [4, 13, 15]. These ratcheting mechanisms may cause difficulties in controlling the distraction rate and rhythm, and there are reports of nails with high distraction rates (so-called “runaway nail”) [19, 26], which may predispose to insufficient bone regeneration [1, 17, 24].
Treatment options for insufficient bone regenerate after intramedullary lower limb lengthening are limited only to bone grafting with or without exchange nailing [8, 20, 26, 27]. No description is available for the possible morphologic types of regenerate failure or a working classification to facilitate treatment decisions and postoperative workup according to this morphology.
The aims of this study are to answer the following questions: (1) What are the risk factors for distraction problems with femoral lengthening using the ISKD nail? (1) What are the major risk factors for insufficient bone regenerate after intramedullary femoral lengthening? (3) Can a radiologic classification system of insufficient bone regeneration with lengthening nails be described?
Patients and Methods
We obtained approval of the Institutional Review Board for this prospective study (#2948). We analyzed prospectively collected data for all patients who had intramedullary femoral lengthening at our institution from July 2002 to June 2008. Thirty-five patients had 37 femoral lengthening procedures using the ISKD nail (Orthofix, Valley, Germany). The indications for femoral lengthening were shortening between 20 and 80 mm. Contraindications were open physis, the presence of active infection, irregular or too narrow medullary canal, or too short femur for the available ISKD nails. The mean age of the patients at the time of the lengthening procedure was 33 ± 11 years (range, 16–61 years). They were followed up for a minimum of 12 months (average, 27 ± 9 months; range, 12–55 months).
The length gain was 42.8 ± 12.9 mm (range, 25–70 mm) with a median of 40 mm, and the distraction rate was 1.2 ± 0.4 mm (range, 0.7–2.8 mm). Twenty-two patients with 23 ISKD nails had posttraumatic shortening (one patient had 10-cm femoral shortening and two-stage femoral ISKD lengthenings), 11 patients had congenital shortening, one patient had bilateral cosmetic femoral lengthening, and one patient required lengthening after tumor (chondrosarcoma) resection.
Eighteen limbs had acute correction of associated deformities through the osteotomy site: posttraumatic (n = 15), congenital (n = 2), and posttumor resection (n = 1). Excluding the patient with posttumor shortening, deformities ranged from an average 6° varus to 8° valgus malalignment and 17° external to 26° internal rotation. The patient with the history of chondrosarcoma had a severe complex deformity (15° varus, 68° procurvatum, and 14° external rotation). This complex deformity was the result of a failed trial of lengthening using an external fixator. Additionally, the patient had a history of local radiotherapy and nine previous surgical procedures at another institution.
The osteotomy for lengthening was performed at the same level of a previous surgical intervention or previous trauma in nine patients. Twelve femoral lengthenings were performed with a tibial ISKD nail as a result of a narrow femoral medullary canal (the smallest diameter of tibial ISKD nails is 10.7 mm in contrast to 12.5 mm for femoral nails). Five patients were smokers.
Radiologic workup included preoperative bilateral full-length standing radiographs of the lower limbs to assess the frontal plane alignment and plane radiographs for the lengthened side. Preoperative CT was used in all patients to calculate the length and torsional differences. CT was requested to assess the quality of the regenerate in four patients with insufficient bone regenerate.
The operative procedures were performed with the patient in the lateral decubitus position and all nails were inserted through antegrade portals. The first step was to implant two parallel 5-mm Schanz screws in the proximal and distal fragments of the femur to control rotation, taking care that they did not interfere with nail insertion. A percutaneous multiple drill hole transverse osteotomy was performed in the shaft area according to preoperative planning. The medullary canal then was overreamed by an average 2 mm and the nail was inserted and locked proximally and distally. With the help of the Schanz screws, 20 rotations between the proximal and distal fragments were performed and the monitor of the ISKD nail was used intraoperatively to detect at least one pole change of a magnet fixed on the distal part of the ratchet mechanism of the nail.
Postoperatively, the patients were allowed partial weightbearing with 15 kg from the first postoperative day. The patients were instructed to follow up the distraction process through the external monitor of the ISKD nail at least five times daily with the aim of a distraction rate of 1 mm/day from the fifth postoperative day. In case of an increased distraction rate, the patients were instructed to reduce their activity level and weightbearing, whereas in case of a decreased distraction rate, they were advised to increase their activities and to perform manual rotations of the femur assisted by their partners or family members. All patients were followed up weekly during the distraction phase and then every 6 weeks during the consolidation phase. Radiographic control was performed at each followup and the distraction gap was measured and compared with the readings of the external monitor of the nail.
We evaluated two main outcomes: distraction problems and insufficient bone regenerate. Nondistracting nails were defined as nails that fail to distract in situ despite the compliance of the patients with all previous instructions. We defined runaway nails as ISKDs distracting with a speed greater than 1.5 mm/day despite the compliance of the patients with all previous instructions and even complete bed rest. A distraction rate of 1.5 mm/day was reported by Schiller et al. [24] to disrupt angiogenic cascade and new vessel formation required for bone regeneration and healing. Accordingly, we divided patients into two groups: patients with a normal distraction rate versus patients with distraction problems (runaway or nondistracting ISKDs). We compared both groups regarding the degree of medullary overreaming obtained from the operative records and the distance between the tip of the nail and the osteotomy site. Also, the length of the thick part of the nail engaged in the distal fragment was measured from the postoperative radiographs, particularly identifying those with less than 80 mm or greater than 125 mm engaged distally, which may predispose to runaway or nondistracting ISKDs, respectively [26].
To study the problem of regenerate failure, we divided the patients into two groups: patients with insufficient bone regenerate requiring surgery versus patients with normal bone regenerate. The incidence and risk factors applicable to our patients were analyzed (Table 1). Patients were further subdivided according to age into two groups (younger than 30 years or 30 years or older) to compare the incidence of insufficient bone regenerate in each age group. Similarly, our median of length gain was 40 mm and therefore patients were subdivided into two groups (40 mm or less or greater than 40 mm).
The radiologic workup was reviewed by two authors (MK, SH) and compared with the different shapes of callus formation described by Li et al. [21]. We identified two main types of failure of bone regeneration: either a partial failure resulting in a partial bony defect (Type I) or a complete circumferential failure causing complete segmental bone defect (Type II). Complete failure was further subdivided according to the length of the defect: 3 cm or less or greater than 3 cm (Types IIa and IIb, respectively) (Table 2; Fig. 1).
Table 2.
Proposed classification for insufficient bone regenerate with intramedullary femoral lengthening
| Class | Defect length | Failure of bone regenerate formation | Defect character |
|---|---|---|---|
| I | Any | Partial failure of regenerate formation | Partial cortical defect |
| IIa | 3 cm or less | Complete failure of regenerate formation | Complete segmental defect |
| IIb | Greater than 3 cm | Complete failure of regenerate formation | Complete segmental defect |
Fig. 1A–I.
These images illustrate the different types of insufficient bone regenerate that we observed with intramedullary femoral lengthening. (A) Anteroposterior and (B) lateral radiographs and (C) a CT scan obtained 24 months after lengthening show partial failure of regenerate formation (Type I) with a partial defect in the anterolateral cortex of the femur. (D) Anteroposterior and (E) lateral radiographs obtained at 5-month followup after 2.5-cm femoral lengthening show complete failure of regenerate formation with a segmental defect less than 3 cm (Type IIa). (F) Axial and (G) coronal CT scans show complete failure of regenerate formation with a segmental defect. (H) Anteroposterior and (I) lateral radiographs obtained at 2-month followup after 6-cm intramedullary femoral lengthening show complete failure of bone regenerate formation and a complete bony defect greater than 3 cm (Type IIb).
We used the Mann-Whitney U test to detect significant differences for continuous variables between different groups. Chi square test was used for categorical variables and relative risk was calculated for variables suitable for 2 × 2 contingency tables. Data were shown in the form of mean ± SD. A p value less than 0.05 was considered statistically significant. We performed all statistical analyses using SPSS program (SPSS 15.0; SPSS Inc, Chicago, IL). Post hoc power analysis was performed for goodness-of-fit tests, ie, contingency tables with effect size = 0.5, α = 0.05, total sample size of 37, and degree of freedom = 1, and we found a statistical power of 86% for our analyses (G*Power 3.0.10; Franz Faul, Universität Kiel, Germany).
Results
The desired lengthening was achieved in all patients. The healing index for patients with normal consolidation (n = 29) was 1.2 ± 0.3 months/cm (range, 0.6–2.1 months/cm). None of our patients had restriction of ROM of the hip or knee compared with the preoperative range.
Distraction problems were encountered in eight femora: seven had runaway nails and one had a nondistracting nail. The level of the osteotomy and extent of overreaming had no major influence on the incidence of distraction problems. Of four patients with less than 80 mm of the thick portion of the nail engaged in the distal fragment, only one had a runaway nail. Furthermore, of 21 patients with greater than 125 mm engaged distally, only one had a nondistracting nail and was managed successfully with manipulation under anesthesia (Table 3).
Table 3.
Comparisons among patients with and without runaway nail
| Variable | Runaway nail (greater than 1.5 mm/day; n = 7) | Nails with average distraction rate (n = 30) | Relative risk | p Value |
|---|---|---|---|---|
| Length of the distal thick part of the nail (cm) | 12.4 ± 7 | 13.6 ± 4.3 | 0.67 | |
| Length of the distal thick part less than 80 mm (n = 4) | n = 1 | n = 3 | 1.4 | 0.822 |
| Distance between the tip of the nail and the osteotomy (cm) | 17.4 ± 6.6 | 19.3 ± 4.3 | 0.644 | |
| Overreaming (mm) | 2 ± 0.3 | 2 ± 0.8 | 0.278 |
Eight patients (21.6%) had insufficient bone regenerate that required surgical intervention. Distraction rates were significantly higher (p = 0.016) with five runaway nails. Furthermore, the incidence of insufficient regenerate was greater in patients 30 years or older (46.7% versus 7.1%, RR = 4.7, p = 0.068), with lengthening greater than 40 mm (37.5% versus 9.5%, RR = 3.9, p = 0.041), and in smokers (37.5% versus 6.9%, RR = 3.8, p = 0.025). Acute correction of associated deformities and osteotomy at the level of previous surgery or trauma increased the risk of insufficient regenerate by 1.8 and 1.9 times, respectively (p = 0.376 and 0.327, respectively) (Table 4).
Table 4.
Comparisons of patients with normal consolidation versus insufficient bone regenerate*
| Variable | Normal regenerate group (n = 29) | Insufficient regenerate group (n = 8) | Relative risk | p Value | |
|---|---|---|---|---|---|
| Age (years) | 31.7 ± 11.3 | 38.1 ± 10.8 | 0.15 | ||
| Age groups | Younger than 30 years (n = 15) | n = 14 | n = 1 | 0.21 | 0.068 |
| 30 years or older (n = 22) | n = 15 | n = 7 | 4.7 | ||
| Lengthening magnitude (mm) | 40.6 ± 11.7 | 50.5 ± 14.9 | 0.103 | ||
| Lengthening groups | 40 mm or less (n = 21) | n = 19 | n = 2 | 0.25 | 0.041† |
| Greater than 40 mm (n = 16) | n = 10 | n = 6 | 3.9 | ||
| Distraction index (mm/day) | 1.1 ± 0.3 | 1.7 ± 0.6 | 0.016 | ||
| Runaway nail (n = 7) | n = 2 | n = 5 | 9.1 | < 0.0001† | |
| Etiology | Posttraumatic (n = 23) | n = 18 | n = 5 | 0.133 | |
| Congenital (n = 11) | n = 10 | n = 1 | |||
| Cosmetic (n = 2) | n = 1 | n = 1 | |||
| Posttumor resection (n = 1) | n = 0 | n = 1 | |||
| Acute correction of deformities (n = 18) | n = 13 | n = 5 | 1.8 | 0.376 | |
| Osteotomy at the level of previous trauma or surgery (n = 9) | n = 6 | n = 3 | 1.9 | 0.327 | |
| Smoking (n = 5) | n = 2 | n = 3 | 3.8 | 0.025† | |
| Tibial ISKD nail for femoral lengthening (n = 12) | n = 9 | n = 3 | 1.3 | 0.729 | |
* Runaway nails are those with a distraction rate greater than 1.5 mm/day; †statistically significant p values; ISKD = intramedullary skeletal kinetic distractor.
Radiologically, failure of regenerate formation was classified as Type I (n = 3), Type IIa (n = 2), or Type IIb (n = 3). In all cases with partial failure, the defect was located at the anterolateral cortex of the femur (Fig. 1). Patients with Type I and Type IIa failure were managed with reamed exchange nailing and/or autologous iliac bone grafting and osteogenic protein 1 (Fig. 2). Particular attention was paid during reamed exchange nailing, especially in patients with Type IIa defects to prevent loss of gained length by applying an external fixator before nail exchange. Patients with Type IIb failure were managed by segmental bone transport using an external fixator over the lengthening nail (“monorail technique,” n = 2) (Fig. 3) or partial prosthetic diaphyseal replacement (n = 1, the patient with the history of chondrosarcoma resection) (Fig. 4). The postrevision weightbearing and rehabilitation protocol was more careful for patients with complete defects (Table 5).
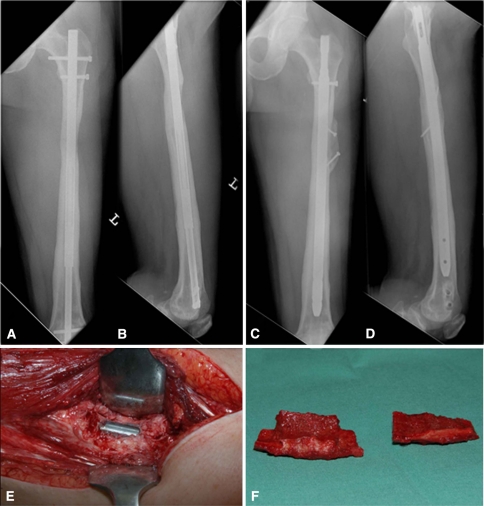
Fig. 2A–F.
A 40-year-old patient had 6-cm bilateral cosmetic femoral lengthening using the ISKD nail. One side uneventfully consolidated and insufficient bone regenerate developed on the other side mainly owing to a high distraction rate (1.9 mm/day), age older than 30 years, and length gain greater than 4 cm. (A) Anteroposterior and (B) lateral radiographs show partial regenerate failure (Type I). (C) Anteroposterior and (D) lateral radiographs obtained 7 months after exchange nailing and iliac bone grafting + osteogenic protein-1 show good union of the tricortical autologous iliac bone graft. (E) An intraoperative photograph of the partial defect in the bone regenerate and (F) the harvested tricortical iliac autograft ready to be fitted in the defect site are shown.
Fig. 3A–F.
A 25-year-old patient had posttraumatic femoral shortening and 6-cm femoral lengthening using the ISKD nail. There was complete failure of regenerate formation (Type IIb) mainly caused by a high distraction rate (1.7 mm/day), smoking, lengthening greater than 4 cm, osteotomy at the site of previous trauma, and acute correction of associated deformity. Followup (A) AP and (B) lateral radiographs show complete absence of regenerate that caused a segmental femoral defect. (C) Anteroposterior and (D) lateral radiographs show the segmental bone transport using an external fixator with the nail in place, the “monorail technique.” The new osteotomy site was made in a healthy area, with a distraction rate of 1 mm/day, and the patient stopped smoking. (E) Anteroposterior and (F) lateral radiographs show consolidation of the newly formed regenerate and healing of the docking site after 7 months.
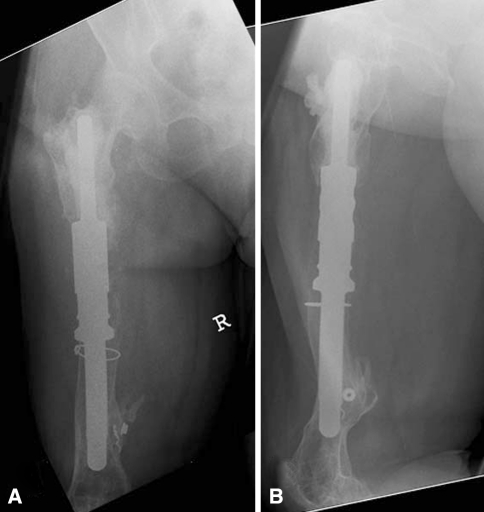
Fig. 4A–B.
Our 61-year-old patient with a history of chondrosarcoma resection and radiotherapy had a trial of 5-cm femoral lengthening using an ISKD. There was complete failure of bone regeneration mainly resulting from previous local radiotherapy, the patient’s age, osteotomy at the site of previous surgery, correction of complex associated deformities, and lengthening greater than 4 cm. (A) Anteroposterior and (B) lateral plain radiographs show partial diaphyseal prosthetic replacement, which was the preferred treatment owing to the poor local biologic situation and general health of the patient.
Table 5.
Patients with insufficient bone regenerate
| Patient number | Age (years) | Etiology of shortening | Lengthening (cm) | Defect type | Distraction rate (mm/day) | Time to revision (months)* | Risk factors for insufficient bone regenerate | Treatment |
|---|---|---|---|---|---|---|---|---|
| 1 | 34 | Posttraumatic | 6.5 | I | 1 | 11 | Age† Smoking Lengthening‡ |
Autologous iliac bone grafting + OP1 |
| 2 | 40 | Cosmetic | 6 | I | 1.9 | 29 | Age† High distraction rate§ Lengthening‡ |
Reamed exchange nailing + autologous bone grafting + OP1 |
| 3 | 38 | Congenital | 4.5 | I | 2.8 | 10 | Age† High distraction rate§ Lengthening‡ |
Reamed exchange nailing + autologous bone grafting + OP1 |
| 4 | 36 | Posttraumatic | 2.5 | IIa | 2 | 7 | Age† Correction of associated deformity High distraction rate§ |
Reamed exchange nailing |
| 5 | 39 | Posttraumatic | 3.4 | IIa | 1.2 | 11 | Age† Correction of associated deformity |
Autologous iliac bone grafting + OP1 |
| 6 | 61 | Posttumor resection | 5 | IIb | 1 | 11 | Age† Local radiotherapy Osteotomy at same site of previous operative intervention Correction of associated complex deformity Lengthening‡ |
Femoral diaphyseal prosthetic replacement |
| 7 | 25 | Posttraumatic | 6 | IIb | 1.7 | 7 | Smoking Osteotomy at the same site of previous trauma Correction of associated deformity High distraction rate§ Lengthening‡ |
Segment transport using external fixator over the lenghtening nail |
| 8 | 41 | Posttraumatic | 6.5 | IIb | 1.6 | 12 | Age† Smoking Osteotomy at the same site of previous trauma Correction of associated deformity High distraction rate§ Lengthening‡ |
Segment transport using external fixator over the lenghtening nail |
* The time between the index lengthening procedure and the first revision to manage insufficient bone regenerate and nonunion; †age 30 years or older; ‡lengthening magnitude greater than 40 mm; §distraction rate greater than 1.5 mm/day.
Discussion
The control of distraction rate and rhythm with the ISKD nail may be a problem causing regenerate failure [19, 26]. The aim of our study was to examine the risk factors of distraction problems, insufficient bone regeneration, and radiologic types of the latter complication in 37 consecutive femoral lengthening procedures using the ISKD nail.
There are some limitations in this study. Smoking as a risk factor was not sufficiently recorded in the form of number of cigarettes per day and for how long the patient was a smoker (smoking index). Second, the number of patients who had developed insufficient bone regenerate was too small to conclude specific treatment guidelines. Third, the intraobserver and interobserver reliability of our radiologic classification were not verified.
The incidence of insufficient bone regenerate was high in our study (21.6%). The most important risk factor was a distraction index greater than 1.5 mm/day (nine times higher risk). Distraction rates of 1.5 mm/day have been found to be inhibitory for new vessel formation and for effective bone healing in a rat model of limb lengthening [24].
Distraction problems with the use of ISKD nails have been reported [19, 26]. Kubiak et al. [19] have explained failure of distraction by the anterior cortical impingement resulting from the use of a straight nail in a curved femur and by the compressive forces created by the soft tissue that prevent lengthening. Simpson et al. [26] reported 15 out of 33 lengthened femora with distraction problems (runaway nails = 7, nondistracting nails = 8). They found an osteotomy placed with less than 80 mm or greater than 125 mm of the thick part of the nail engaged in the distal fragment was more likely to cause uncontrolled lengthening or a nondistracting nail, respectively. Furthermore, overreaming by 2.5 to 3 mm was reported to prevent a nondistracting nail. In contrast we could not corroborate a relationship between distraction problems and the length of nail engagement in the distal fragment. In our series, 21 patients had greater than 125 mm of the thick part of the nail engaged distally and only one had a nondistracting nail develop. So far, the cause of these distraction problems seems not to be fully understood. An internal mechanical malfunction in the lengthening mechanism of the nail cannot be ruled out.
Age 30 years or older, lengthening magnitude greater than 4 cm, and smoking were associated with a higher risk of insufficient bone regeneration. Age and lengthening magnitude are known factors affecting the consolidation index [6, 7]. Patients younger than 20 years and those between 20 and 29 years achieve healing considerably faster than older patients [7]. Additionally, Zheng et al. [32] found nicotine exposure decreased blood flow and bone formation during distraction osteogenesis with decreased osteoblastic bone morphogenetic protein.
Creation of the osteotomy at the same site of previous trauma or surgery and acute correction of associated deformities may complicate regenerate formation. The potential deleterious effect of previous trauma or surgery on the local soft tissue and periosteum, and therefore on bone regeneration, may be responsible [3, 6]. Acute correction of associated deformities also can be traumatic to the local blood supply, especially if initial diastasis took place [21].
We had a significantly greater incidence of insufficient bone regenerate that necessitated operative intervention in comparison to other authors (Table 6). In comparison to these studies, we had the highest incidence of runaway nails. Simpson et al. [26] reported nearly the same rate of runaway nails; however, the distraction indices were not reported, therefore, we cannot compare both groups regarding rates of distraction. They also reported patients with uncontrolled lengthening had much slower consolidation. Five of these cases underwent exchange nailing and one required bone grafting [26].
Table 6.
Literature review of studies of lower limb lengthening using totally implantable lengthening nails
| Study | Nail used | Lengthening procedures (number) | Lengthened bone | Insufficient bone regenerate | Treatment |
|---|---|---|---|---|---|
| Cole et al. [4], 2001 | ISKD | 20 | Femoral (n = 6) Tibia (n = 14) |
— | |
| Hankemeier et al. [15], 2004 | ISKD | 4 | Femoral (n = 3) Tibial (n = 1) |
— | |
| Kubiak et al. [19], 2007 | ISKD | 11 | Femoral | — | |
| Simpson et al. [26], 2009 | ISKD | 33 | Femoral | 3 | Bone grafting |
| Baumgart et al. [2], 1997 | Fitbone | 12 | Femoral | — | |
| Singh et al. [27], 2006 | Fitbone | 24 | Femoral (n = 13) Tibial (n = 11) |
3 Tibial | Bone grafting + exchange nailing (n = 1) Bone grafting (n = 2) |
| Garcia-Cimbrelo et al. [8], 2002 | Albizzia | 24 | Femoral | 2 | Exchange reamed nailing and bone grafting |
| Guichet et al. [12], 2003 | Albizzia | 41 | Femoral | 1 (slight defect in the anterolateral side) | Percutaneous bone grafting |
ISKD = Intramedullary Skeletal Kinetic Distractor.
In our study, three patients had complete failure of regenerate formation and segmental femoral defects greater than 3 cm in length where there is an indication for segmental bone transport [5, 14, 29]. The decision-making in cases with Type IIb defects according to our classification should be based on the local biologic situation and the general health of the patient. If the patient is relatively young and has good local tissue quality, segmental bone transport using an external fixator over the lengthening nail (monorail technique) is a good option, but in case of a poor local biologic situation as with our patient with a history of local radiotherapy, diaphyseal prosthetic replacement is a good alternative to allow early mobilization. On the other hand, patients with partial defects or complete defects less than 3 cm can be managed effectively with bone grafting and/or exchange nailing. The location of the defect in patients with partial failure of regenerate formation was always in the anterolateral cortex, which is explained by the effect of the surgical exposure for corticotomy on the blood supply [3, 6].
The main disadvantage of the ISKD nail is the inability to accurately control the distraction rate. A lengthening nail with better control of distraction rate is needed. A distraction rate greater than 1.5 mm/day should be avoided during intramedullary femoral lengthening. We believe smoking is a contraindication for intramedullary lower limb lengthening and that the osteotomy level should be chosen away from areas of previous trauma or surgery when technically possible. Moreover, we caution that acute correction of associated deformities through the same osteotomy may jeopardize regenerate healing.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at the Trauma Department, Hannover Medical School, Hannover, Germany.
References
- 1.Aronson J. Basic science and biological principles of distraction osteogenesis. In: Robert Rozbruch S, Ilizarov S, editors. Limb Lengthening and Reconstruction Surgery. New York, NY: Informa Healthcare; 2007. pp. 19–42. [Google Scholar]
- 2.Baumgart R, Betz A, Schweiberer L. A fully implantable motorized intramedullary nail for limb lengthening and bone transport. Clin Orthop Relat Res. 1997;343:135–143. doi: 10.1097/00003086-199710000-00023. [DOI] [PubMed] [Google Scholar]
- 3.Brutscher R, Rahn BA, Ruter A, Perren SM. The role of corticotomy and osteotomy in the treatment of bone defects using the Ilizarov technique. J Orthop Trauma. 1993;7:261–269. doi: 10.1097/00005131-199306000-00011. [DOI] [PubMed] [Google Scholar]
- 4.Cole JD, Justin D, Kasparis T, DeVlught D, Knobloch C. The intramedullary skeletal kinetic distractor (ISKD): first clinical results of a new intramedullary nail for lengthening of the femur and tibia. Injury. 2001;32(suppl 4):SD129–139. doi: 10.1016/s0020-1383(01)00116-4. [DOI] [PubMed] [Google Scholar]
- 5.DeCoster TA, Gehlert RJ, Mikola EA, Pirela-Cruz MA. Management of posttraumatic segmental bone defects. J Am Acad Orthop Surg. 2004;12:28–38. doi: 10.5435/00124635-200401000-00005. [DOI] [PubMed] [Google Scholar]
- 6.Fink B, Krieger M, Strauss JM, Opheys C, Menkhaus S, Fischer J, Ruther W. Osteoneogenesis and its influencing factors during treatment with the Ilizarov method. Clin Orthop Relat Res. 1996;323:261–272. doi: 10.1097/00003086-199602000-00036. [DOI] [PubMed] [Google Scholar]
- 7.Fischgrund J, Paley D, Suter C. Variables affecting time to bone healing during limb lengthening. Clin Orthop Relat Res. 1994;301:31–37. [PubMed] [Google Scholar]
- 8.Garcia-Cimbrelo E, Curto de la Mano A, Garcia-Rey E, Cordero J, Marti-Ciruelos R. The intramedullary elongation nail for femoral lengthening. J Bone Joint Surg Br. 2002;84:971–977. doi: 10.1302/0301-620X.84B7.12984. [DOI] [PubMed] [Google Scholar]
- 9.Gravel CA, Le TT, Chapman MW. Effect of neoadjuvant chemotherapy on distraction osteogenesis in the goat model. Clin Orthop Relat Res. 2003;412:213–224. doi: 10.1097/01.blo.0000069002.56218.99. [DOI] [PubMed] [Google Scholar]
- 10.Guichet JM, Braillon P, Bodenreider O, Lascombes P. Periosteum and bone marrow in bone lengthening: a DEXA quantitative evaluation in rabbits. Acta Orthop Scand. 1998;69:527–531. doi: 10.3109/17453679808997792. [DOI] [PubMed] [Google Scholar]
- 11.Guichet JM, Casar RS. Mechanical characterization of a totally intramedullary gradual elongation nail. Clin Orthop Relat Res. 1997;337:281–290. doi: 10.1097/00003086-199704000-00032. [DOI] [PubMed] [Google Scholar]
- 12.Guichet JM, Deromedis B, Donnan LT, Peretti G, Lascombes P, Bado F. Gradual femoral lengthening with the Albizzia intramedullary nail. J Bone Joint Surg Am. 2003;85:838–848. doi: 10.2106/00004623-200305000-00011. [DOI] [PubMed] [Google Scholar]
- 13.Hankemeier S, Gosling T, Pape HC, Wiebking U, Krettek C. Limb lengthening with the Intramedullary Skeletal Kinetic Distractor (ISKD) Oper Orthop Traumatol. 2005;17:79–101. doi: 10.1007/s00064-005-1123-5. [DOI] [PubMed] [Google Scholar]
- 14.Hankemeier S, Liodakis E, Kenawey M, Krettek C. What is new in the management of bone defects? In: Meßmer K, Jähne J, Neuhaus P, eds. What Is New in Surgery? [in German]. Landsberg, Germany: Verlagsgruppe Hüthig Jehle Rehm GmbH; 2009:291–300.
- 15.Hankemeier S, Pape HC, Gosling T, Hufner T, Richter M, Krettek C. Improved comfort in lower limb lengthening with the intramedullary skeletal kinetic distractor: principles and preliminary clinical experiences. Arch Orthop Trauma Surg. 2004;124:129–133. doi: 10.1007/s00402-003-0625-6. [DOI] [PubMed] [Google Scholar]
- 16.Ilizarov GA. The tension-stress effect on the genesis and growth of tissues: Part I. The influence of stability of fixation and soft-tissue preservation. Clin Orthop Relat Res. 1989;238:249–281. [PubMed] [Google Scholar]
- 17.Ilizarov GA. The tension-stress effect on the genesis and growth of tissues: Part II. The influence of the rate and frequency of distraction. Clin Orthop Relat Res. 1989;239:263–285. [PubMed] [Google Scholar]
- 18.Kojimoto H, Yasui N, Goto T, Matsuda S, Shimomura Y. Bone lengthening in rabbits by callus distraction: the role of periosteum and endosteum. J Bone Joint Surg Br. 1988;70:543–549. doi: 10.1302/0301-620X.70B4.3403595. [DOI] [PubMed] [Google Scholar]
- 19.Kubiak EN, Strauss E, Grant A, Feldman D, Egol KA. Early complications encountered using a self-lengthening intramedullary nail for the correction of limb length inequality. Joint Dis Rel Surg. 2007;18:52–57. [Google Scholar]
- 20.Leidinger B, Winkelmann W, Roedl R. [Limb lengthening with a fully implantable mechanical distraction intramedullary nail] [in German] Z Orthop Ihre Grenzgeb. 2006;144:419–426. doi: 10.1055/s-2006-942169. [DOI] [PubMed] [Google Scholar]
- 21.Li R, Saleh M, Yang L, Coulton L. Radiographic classification of osteogenesis during bone distraction. J Orthop Res. 2006;24:339–347. doi: 10.1002/jor.20026. [DOI] [PubMed] [Google Scholar]
- 22.Paley D. Problems, obstacles, and complications of limb lengthening by the Ilizarov technique. Clin Orthop Relat Res. 1990;250:81–104. [PubMed] [Google Scholar]
- 23.Paley D, Herzenberg JE, Paremain G, Bhave A. Femoral lengthening over an intramedullary nail: a matched-case comparison with Ilizarov femoral lengthening. J Bone Joint Surg Am. 1997;79:1464–1480. doi: 10.2106/00004623-199710000-00003. [DOI] [PubMed] [Google Scholar]
- 24.Schiller JR, Moore DC, Ehrlich MG. Increased lengthening rate decreases expression of fibroblast growth factor 2, platelet-derived growth factor, vascular endothelial growth factor, and CD31 in a rat model of distraction osteogenesis. J Pediatr Orthop. 2007;27:961–968. doi: 10.1097/BPO.0b013e3181558c37. [DOI] [PubMed] [Google Scholar]
- 25.Simpson AH, Cole AS, Kenwright J. Leg lengthening over an intramedullary nail. J Bone Joint Surg Br. 1999;81:1041–1045. doi: 10.1302/0301-620X.81B6.9359. [DOI] [PubMed] [Google Scholar]
- 26.Simpson AH, Shalaby H, Keenan G. Femoral lengthening with the Intramedullary Skeletal Kinetic Distractor. J Bone Joint Surg Br. 2009;91:955–961. doi: 10.1302/0301-620X.91B7.21466. [DOI] [PubMed] [Google Scholar]
- 27.Singh S, Lahiri A, Iqbal M. The results of limb lengthening by callus distraction using an extending intramedullary nail (Fitbone) in non-traumatic disorders. J Bone Joint Surg Br. 2006;88:938–942. doi: 10.1302/0301-620X.88B7.17618. [DOI] [PubMed] [Google Scholar]
- 28.Tselentakis G, Kitano M, Owen PJ, Kuiper JH, Richardson JB, Evans GA. The behaviour of the periosteum during callotasis. J Pediatr Orthop B. 2003;12:277–283. doi: 10.1097/00009957-200307000-00008. [DOI] [PubMed] [Google Scholar]
- 29.Watson JT, Kuldjanov D. Bone defects. In: Rozbruch SR, Ilizarov S, editors. Limb Lengthening and Reconstruction Surgery. New York, NY: Informa Healthcare; 2007. pp. 185–201. [Google Scholar]
- 30.Yasui N, Kojimoto H, Sasaki K, Kitada A, Shimizu H, Shimomura Y. Factors affecting callus distraction in limb lengthening. Clin Orthop Relat Res. 1993;293:55–60. [PubMed] [Google Scholar]
- 31.Yasui N, Kojimoto H, Shimizu H, Shimomura Y. The effect of distraction upon bone, muscle, and periosteum. Orthop Clin North Am. 1991;22:563–567. [PubMed] [Google Scholar]
- 32.Zheng LW, Ma L, Cheung LK. Changes in blood perfusion and bone healing induced by nicotine during distraction osteogenesis. Bone. 2008;43:355–361. doi: 10.1016/j.bone.2008.04.002. [DOI] [PubMed] [Google Scholar]