During the past 16 months, all patients treated with renal homotransplantation at the Colorado General and Denver Veterans Administration hospitals have been administered heterologous antilymphocyte globulin intramuscularly, usually for the first 4 postoperative months. This agent was used as an adjunct to the standard immunosuppressive drugs, azathioprine and prednisone. The preparation of the globulin from the serum of immunized horses (2), the toxicity of this agent (4, 14), and the evidence that it is of value at least early after human kidney transplantation (11, 14) have already been described.
Two more questions will be examined. The first concerns the fate of these patients subsequent to the discontinuance of antilymphocyte globulin. To determine this, the courses of 20 consecutive patients who received renal homografts 10 to 16 months ago from various blood relatives have been reviewed. The survivors have been followed up for 6 to 12 months after their last injections of horse protein.
Second, these and subsequent recipients of consanguineous kidney transplants have been studied to find out what effect non-conformity between the antigens of donor and recipient lymphocytes had upon both early and late homograft function and upon the need for immunosuppressive therapy. This information was desirable to determine to what extent histoincompatibilities could be consistently overridden with the therapeutic regimen being tested.
Two other small groups of patients have been included because of their important bearing upon one or both of these questions. The first group consisted of 6 recipients of cadaveric homografts. The donor-recipient antigen match in each instance was poor. The other, a heterogenous group, consisted of 4 patients who were given globulin therapy for the first time long after transplantation in an effort to halt the chronic rejection of their cadaveric or consanguineous homografts. In the survivors among the latter patients, a follow-up period of 1 year is available since the last injections of globulin.
METHODS
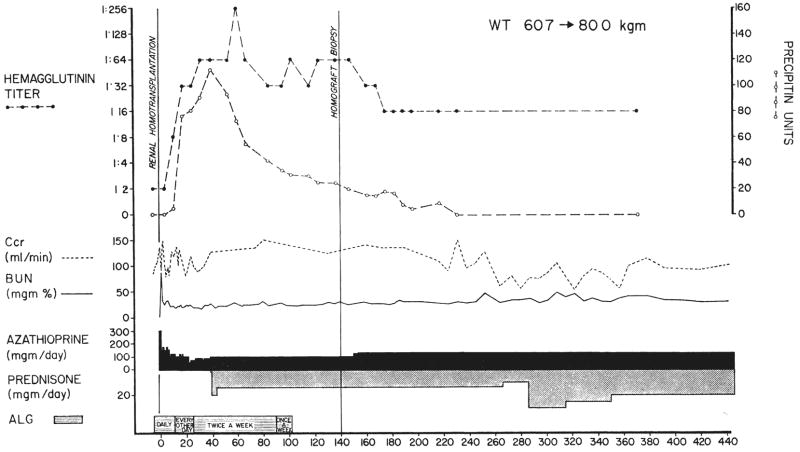
In Figure 1 is shown the way in which antilymphocyte globulin was used during a 4 month period for new patients undergoing transplantation. The regimen was the same when either living or cadaveric donors were utilized, except that preoperative treatment was omitted in the latter. Therapy was also similar in the patients who were treated late after transplantation. It consisted initially of daily injections with a dose schedule which was progressively attenuated (Fig. 1). In vitro, the globulin agglutinated human white cells to a dilution of 1:4,000 to 1:32,000. Individual doses were 1 to 5 milliliters, depending upon the weight of the patient and the leukoagglutinin titer of the globulin. The protein concentration in the injectate was 4.6 to 10.8 grams per hundred milliliters. In 15 per cent of the patients, the course of globulin therapy was prematurely stopped after 4 to 15 weeks because of anaphylactic reactions or for other reasons.
Fig. 1.
The course of a patient who received antilymphocyte globulin (ALG) before and for the first 4 months after renal homotransplantation. The donor was an older brother. The Terasaki match was grade A. There was no early rejection. Prednisone therapy was started 40 days postoperatively because of the high rises in the serologic titers which warned against a possible anaphylactic reaction. Note the insidious onset of late rejection after cessation of globulin therapy. This was treated by increasing the maintenance dose of steroids. This delayed complication occurred in only 2 of the original 20 patients.
Globulin was used as an adjuvant to azathioprine and prednisone. The former drug was started the day before operation and continued indefinitely thereafter in doses judged to be nontoxic on the basis of frequent white blood cell determinations. Prednisone was given if rejection developed in spite of treatment with azathioprine and globulin, in a few instances as prophylactic immunosuppression from the day of operation, or in some instances because the recipient had alarming increases of precipitin or hemagglutinin titers (Fig. 1). The ultimate quantities of prednisone administered generally provided a good indication of the difficulties in controlling rejection, since maintenance doses were quickly arrived at which were as small as possible consistent with retention of stable homograft function.
In the first 20 patients with homotransplantation between blood relatives, the recipients were 7 to 47 years of age and weighed 12 to 75.5 kilograms. The donors were siblings in 13 instances, parents in 5, a maternal uncle in 1, and a cousin in the other. All donors and recipients had undergone tissue typing. This analysis, performed by Terasaki and his associates (17), was based on the demonstration with a panel of human antisera of antigens in circulating lymphocytes. Compatibility, as studied with a given group of antisera, was said to exist if both donor and recipient possessed the same antigen, if the antigen was not present in either, or if it was found in the recipient but not in the donor.
In these 20 patients as well as in most others included in the statistical analysis of results, the most weight was given to mismatches in the named groups (Table I). Also considered, however, were mismatches between unclassified antigens. On the basis of the foregoing results, a summary grade of A to D was given according to the excellence of the antigen match. An A or B grade indicates that no incompatibilities existed in any of the 6 major groups. In all C or D matches, there was at least 1 such group incompatibility. Differentiations between A and B and between C and D grades were made on the basis of the total number of individual antisera mismatched from donor to recipient.
TABLE I.
CADAVERIC HOMOTRANSPLANTATION IN PATIENTS TREATED WITH ANTILYMPHOCYTE GLOBULIN
| CD No. | 1 (D-11, P-LA1, VR-7D) |
2 (D-Mac, P-LA2, VR-8A) |
3–4 (D-3, VR-4A) |
5 (D-9, P-4D, VR-6B) |
6 (D-6, P-4C, VR-9A) |
7 (D-7, VR-4B) |
Unclassified | Preformed antibodies |
Summary, grade |
Survival, mos. |
Present creatinine clearance, ml/min. |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 10 | + | − | − | − | − | − | Many | No | C | 11 | 15 |
| 11 | − | − | − | + | − | − | Many | No | C − | Died— 3½ | * |
| 12 | − | + | − | − | − | − | Many | No | D | Died— 3½ | * |
| 13 | + | − | − | − | − | − | Many | Yes | D | 5½ | 95 |
| 14 | + | − | − | − | − | − | Many | No | C | 4½ | 47 |
| 15 | − | − | + | − | + | − | Many | No | D | 3 | 55 |
The antigenic incompatibilities between donors and recipients are shown, and the probable correspondence of the Terasaki groups to those of Dausset (D), Payne (P), and van Rood (VR) are indicated in parentheses. The unclassified antigens were also considered in deciding upon a summary grade.
These 2 patients received homografts from a common donor. Both died after 3½ months within a 24 hour period. The cause of death in each was multiple pulmonary embolization, a fatal complication not seen in our institutions after renal transplantation since 1964.
CD, cadaveric.
The results obtained with the globulin-treated recipients of related homografts were compared extensively with those obtained in past consanguineous homotransplantations at our institutions. The retrospective control series consisted of 3 consecutive groups of 32, 14, and 25 patients who were operated upon from November 1962 to April 1966. By dividing the patients in this way, a perspective was obtained of the influence of increased experience upon mortality. In addition, there were differences in the way in which prednisone was used in each of the 3 groups. These variables, which have already been discussed at length (14), did not have a demonstrable effect upon the results during the first postoperative year. Consequently, the 3 series were pooled for some of the statistical comparisons with the globulin-treated patients. In all the statistical analyses, drug doses were expressed as milligrams per kilogram per day. Measures of renal function and circulating white blood cells were compiled by average weekly values, since these determinations were not available for each day.
RESULTS
Recipients of Related Homografts
Survival
Nineteen of the first 20 patients are still alive with good function of the original transplants. In 12 of them, 12 to 16 months have elapsed since operation; in the other 7 patients, the period since operation has been 10 to 12 months. The only death occurred 42 days after operation as a direct consequence of a surgical error. This particular patient has been described elsewhere (14).
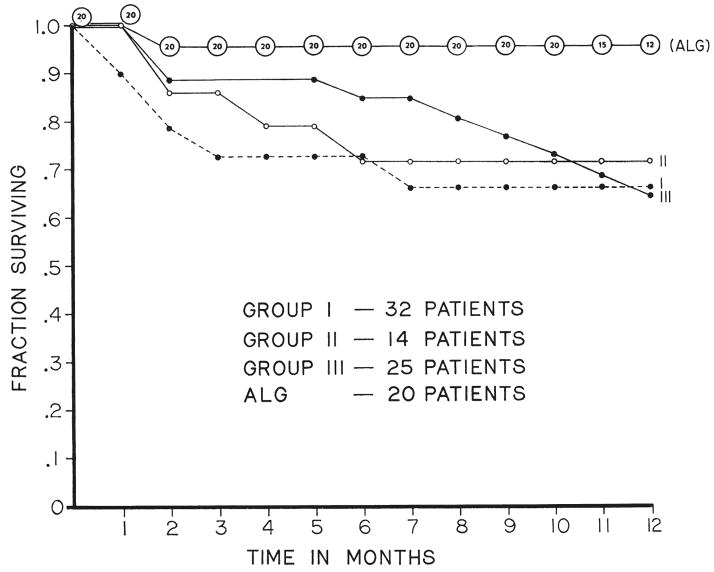
In Figure 2, the survival curve is compared with those of each of the 3 retrospective control series. The 5 per cent mortality rate in the globulin-treated patients contrasted with a 28 to 31 per cent loss rate in each of the earlier groups during the first 12 months.
Fig. 2.
Survival curve of the first 20 patients treated with antilymphocyte globulin (ALG) compared to that in 3 previous series of consanguineous transplantations at our institutions. Follow-up periods for the globulin-treated group were 10 to 16 months. The numbers in the upper curve indicate the patients at risk for each monthly interval.
Histocompatibility
Five, 11, and 4 of the 20 patients had A, B, and C antigen matches, respectively, with their donors. This spectrum was not significantly different from that in retrospective series 3, in which the same kind of information was available for all patients.
A similar distribution was found in the 80 per cent of those in retrospective series 1 and 2, in which typing was obtained at some time after transplantation.
Immunosuppression and homograft function
For both the retrospective control and the test series, the average renal function and the doses of azathioprine and prednisone used to protect the homografts were determined for the first 4 postoperative months and for the 6 subsequent months. Inclusion of any patient in the analysis was contingent upon survival for 10 months, a condition that was met in 19 of the 20 globulin-treated patients. In contrast, 11,4, and 6 of the 32, 14, and 25 patients in control groups, 1, 2, and 3, respectively, were excluded because of their failure to live this long, thereby eliminating a number of highly unfavorable patients. The introduction of this harsh bias did not obscure the favorable showing of the globulin-treated patients.
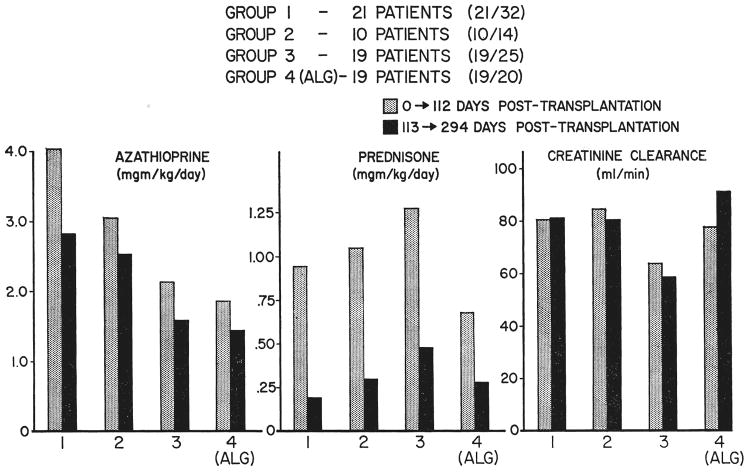
During the time when control groups 1 to 3 were compiled, a progressive tendency existed to use smaller doses of azathioprine during the early postoperative period (Fig. 3) in an effort to reduce the incidence of bone marrow depression. This continued into the globulin-treated series. The linear downward trend was statistically significant, p<.005. After 4 months, dose differences in the 4 series were in the same direction, p < .005, but less marked (Fig. 3).
Fig. 3.
The average azathioprine and prednisone doses per kilogram per day and the creatinine clearances for the first 16 postoperative weeks, shaded area, and for the subsequent 6 months, solid area. Shown are the retrospective control series 1, 2, and 3, and the antilymphocyte globulin (ALG) series, group 4. Inclusion in the analysis was contingent upon survival for 294 days, a condition which was met with the highest regularity in the patients in the ALG group.
The average daily dose of prednisone during the first 4 postoperative months was 0.95, 1.05, and 1.28 milligrams per kilogram in the 3 control series. In the globulin-treated patients, the average value was 0.68 milligram per kilogram, a reduction which was statistically significant in relation to groups 2 and 3, p<.025 and .005, but not in relation to group 1. During the ensuing 6 months, steroid consumption remained low in the patients of the globulin group (Fig. 3), a particularly encouraging finding since the globulin therapy had been stopped.
The advantage of using smaller doses of the standard immunosuppressive agents in the globulin-treated patients was not at the cost of reduced homograft function. In the first 4 months, as well as in the subsequent half year, the creatinine clearances of the antilymphocyte globulin group compared favorably with the 3 control series (Fig. 3). The blood urea nitrogen and plasma creatinine analyses showed similar results.
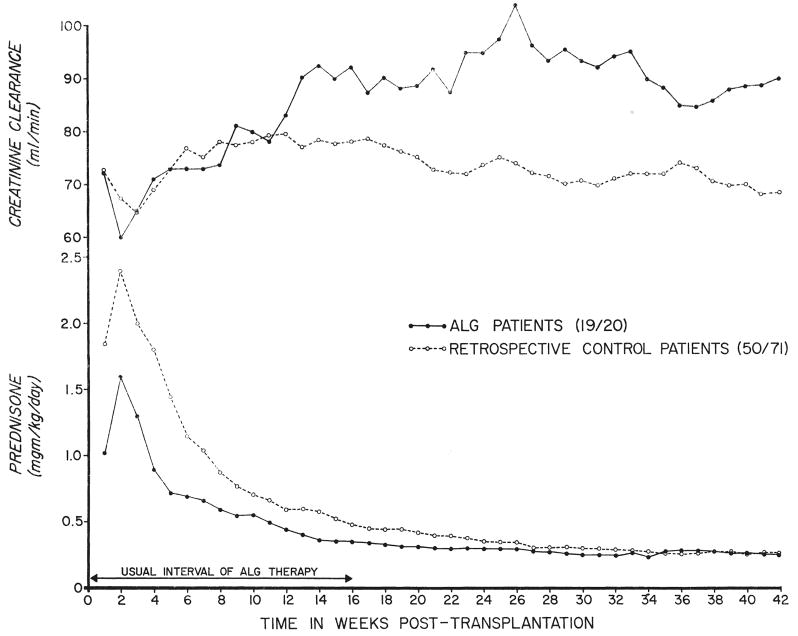
A more dynamic view of the functional characteristics of the homografts was obtained by pooling the creatinine clearances of all the retrospective control patients and comparing these with similar week-to-week data from the globulin series (Fig. 4). During the first 10 postoperative months, the performance of the latter homografts was consistently better than that of the pooled controls, although in both groups, the clearances tended to decline slightly after some months. These studies showed that patients in the globulin series tended to retain superior function long after the heterologous protein therapy had been stopped.
Fig. 4.
Average creatinine clearances and daily prednisone doses for the 19 of 20 globulin-treated patients who lived for at least 10 months after receipt of homografts from blood relatives. These results are compared with pooled data from the 50 of 71 patients previously observed who had lived for this long after similar intrafamilial homotransplantation. Note the superior function and the smaller steroid doses of the globulin-treated patients who, because of their greater incidence of survival, were a less highly selected group than the included recipients in the retrospective control series.
White cell counts
The average leukocyte counts during the first 10 postoperative months were higher in the globulin-treated patients than in any of the retrospective control series and probably reflected the smaller doses of azathioprine mentioned earlier. Lymphopenia was not a feature in patients who were receiving antilymphocyte globulin.
Rejection
A rejection during the first 4 postoperative months was not observed in 8 of the 19 recipients in whom operation was satisfactory. In the others, rejection was easily reversed with an increase in prednisone dosage. A secondary rise in blood urea nitrogen to as high as 150 milligrams per hundred milliliters was seen in only 1 of the latter patients and to as high as 100 milligrams per hundred milliliters in 1 other.
In 2 patients, mild late rejections were diagnosed after cessation of antilymphocyte globulin (Fig. 1). The patients were also managed without difficulty by an elevation in the maintenance dose of steroids. Their antigen matches were A and B, respectively.
Infectious complications
The patient with unrelieved uremia consequent to a technically unsuccessful transplantation had pneumonitis at the time of death. In another, meningococcemia developed 8 months after transplantation from which the patient recovered. There were 2 examples of transient pneumonitis of undetermined cause and 1 example of herpes zoster.
Histocompatibility, Therapy, and Function
Thirty-eight instances of consanguineous transplantation were reviewed in which antilymphocyte globulin therapy was used. These included the 19 recipients already described who have lived from 10 to 16 months after transplantation as well as 19 of 21 subsequently treated patients who have a follow up of at least 9 postoperative weeks. In the 2 excluded patients of the latter consecutive series, death resulted from technical errors after 2 and 25 days. In the included patients, the average daily doses of azathioprine and prednisone were determined for the first 63 days as well as the blood urea nitrogens, creatinines, creatinine clearances, and white blood cell counts. In this way, a cross sectional view was developed in which homograft function and the therapy needed to maintain this function could be interrelated. These data were then pooled for the 11, 19, and 8 patients who had A, B, and C matches, respectively, with their donors.
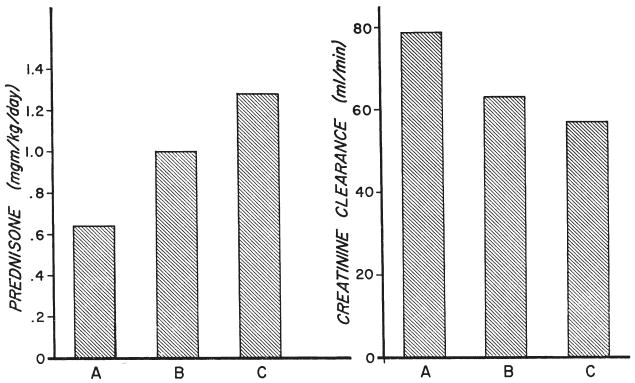
The average prednisone doses with A, B, and C matches were .64, 1, and 1.28 milligrams per kilogram per day, respectively, whereas the creatinine clearances were 79, 64, and 57 milliliters per minute (Fig. 5). The trends in both the measure of renal function and in the steroid doses of the 3 groups were statistically significant, p<.05 and .025. A similar superiority of homograft function in the A as opposed to the B and C matches was evident in the blood urea nitrogens and plasma creatinines. The white blood cell counts and azathioprine doses were not significantly different in the 3 subgroups.
Fig. 5.
The average daily prednisone doses and creatinine clearances per week for the first 9 weeks after transplantation are shown for the 38 globulin-treated patients, grouped according to the histocompatibility with their donors. The A, B, and C rating indicates progressively less favorable antigenic matches. There was a positive correlation between the quality of the match and the level of the creatinine clearances as well as an inverse correlation between the excellence of the match and the average doses of prednisone.
Recipients of Cadaveric Homografts
Transplantation was performed 11, 6, 6, 5½, 4½, and 3 months ago. No attempt was made at preoperative antigen matching. Each donor-recipient combination was later shown to have a high degree of incompatibility (Table I). In 1 patient, preformed antibodies against donor tissue were detectable. The second and third patients, who were 6 and 45 years old, had a common donor.
Partial or complete acute tubular necrosis was evident postoperatively in 4 of the 6 patients, but excellent function was ultimately achieved in all. The 2 patients who received kidneys from the same donor both died after 103 days of multiple pulmonary emboli, an unusual coincidence since this complication has not led to a fatality after renal transplantation in our institutions since 1964. The clots originated from the veins of the legs in the older patient, who had good renal function until just before death, and from the vena cava of the child. In the latter instance, anuria had developed suddenly, 3 days before death. At autopsy, the anastomosis of the renal vein to vena cava was found to be occluded by the thrombus.
The homografts were examined by K. A. Porter of London, England. The first of these 2 kidneys contained only a small amount of cellular infiltration which was principally subcapsular. No vascular or glomerular lesions were present. The second kidney had tubular and interstitial changes which were secondary to the venous occlusion. There was no evidence of damage from rejection.
The other 4 patients still have life-sustaining urine excretion by their homografts after 3, 4½, 5½ and 11 months. In 3 patients, function is good, but the patient who has survived the longest has a blood urea nitrogen of 60 to 80 milligrams per hundred milliliters and a creatinine clearance of 10 to 20 milliliters per minute. This patient had excellent function until 7 weeks after cessation of globulin therapy, when a deterioration of function began. It was then discovered that he had also stopped taking azathioprine and prednisone. The rejection was halted, but not reversed, after resumption of therapy with a standard immunosuppression course combined with a second 3 month course of globulin therapy.
Late Globulin Therapy
The 4 patients in the group in which globulin administration was combined with reductions in prednisone dosage have previously been described (11, 14). Two recipients had received cadaveric grafts 7 and 9 months before globulin therapy was started. One patient who had a creatinine clearance of 3 to 5 milliliters per minute died before the 4 month course was completed. Because of septic complications, the other had all immunosuppressive therapy, including globulin, stopped after 4 weeks of heterologous protein injections. He has subsequently received a second homograft from a related donor.
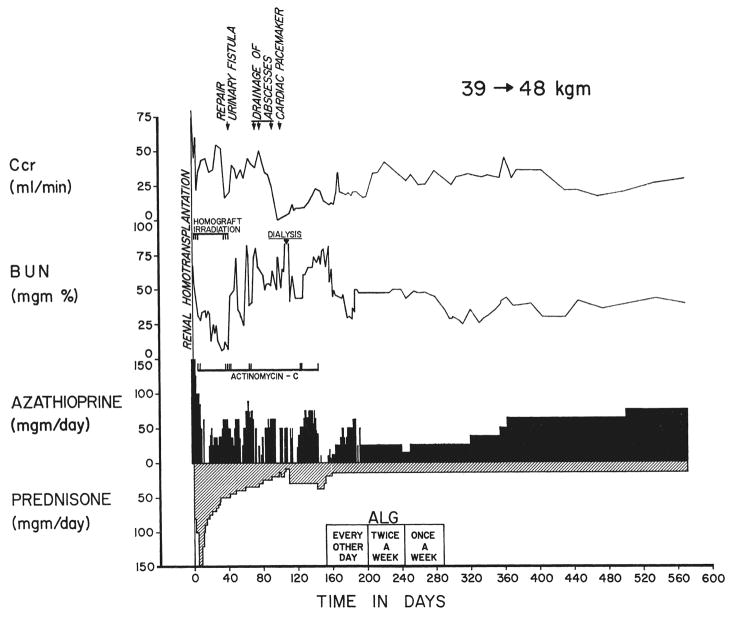
The other 2 patients, who had received maternal homografts 5 and 11 months previously, required 1 and 1.3 milligrams per kilogram per day of prednisone to maintain stable function. In both instances, their antigen matches with their donors were B. During the courses of globulin treatment, the steroid doses were drastically reduced without precipitating chronic rejection. During the subsequent year, renal function has remained relatively stable at its previous subnormal levels (Fig. 6). Both patients are now receiving a daily prednisone dose of .31 milligram per kilogram.
Fig. 6.
Course of a 20 year old woman who received a course of heterologous globulin therapy beginning 5 months after transplantation of a homograft from her mother. Previously, reductions in prednisone dosage led to slow rejection. As she was treated with antilymphocyte globulin, prednisone was reduced to 15 milligrams per day without incident. During the year since the completion of globulin therapy, her function has remained relatively stable at a prednisone dose of 15 milligrams per day. Her antigenic match with her donor was grade B. In this instance, the multiple early postoperative complications made any hope for survival dependent upon rapid reduction of the steroid quantities.
DISCUSSION
The first suggestion that antilymphocyte serum or its derivatives might eventually have clinical utility was made by Woodruff (20) in 1964. Shortly thereafter, important further contributions were made by Gray, Jeejeebhoy, Monaco, and Levey and their associates. All of these investigators emphasized the efficacy with which serum therapy mitigated or prevented the rejection of skin homografts in mice or rats. Many of the subsequent steps which were necessary before such foreign protein could be used in man were carried out in dogs in our own and other laboratories, as reviewed previously (14).
The administration of heterologous anti-lymphocyte globulin in man has a number of disadvantages. The intramuscular injections are painful. Moreover, there may be manifold signs of systemic toxicity. Fever is almost invariable. Hives, pruritis, rashes, and thrombocytopenia have all been documented. Anaphylactic reactions have occurred at some time during globulin therapy in 20 per cent of our patients. Serologic evidence of host antibody formation against the horse protein can eventually be demonstrated in almost every patient. These toxic manifestations have recently been reviewed by Kashiwagi and his associates.
In spite of the frequency of these side reactions, the risks imposed by repeated globulin injections do not appear to be excessive. Well over 2,000 doses have now been given by us to 60 patients without a drug-related mortality. The various complications have been managed without undue difficulty. The fear of nephrotoxicity from such therapy was largely dispelled by the results from homograft biopsies obtained in the first 8 patients after a 4 month course of treatment. There was no evidence of either Masugi or serum sickness nephritis in any of the kidneys (14). Nevertheless, a clear warning that such a complication might occasionally occur was given in the report by Monaco and his associates who observed serum sickness nephritis in a normal volunteer who was being administered rabbit gamma G globulin.
The benefits of antilymphocyte globulin seem impressive enough to outweigh its adverse effects. With its use, the early mortality and homograft loss rate after renal transplantation, at least when related donors were used, has been reduced to 5 per cent during the first postoperative year. Apparently, the improvement can be largely ascribed to the uniformly effective prevention of rejection without the need for high dose steroid therapy. This was achieved with a very low incidence of septic complications.
Since the globulin therapy was confined to the first 4 postoperative months, the fate of the patients after its discontinuance has been a point of interest. Recently (14), it was speculated that any benefit conferred during the earlier period might outlast the interval of treatment, but not necessarily because of a continuing immunosuppressive effect. Instead, the successful management of patients during this time could permit or aid the evolution of the state of host-graft non-reactivity which often occurs weeks or months after transplantation (13). This poorly understood alteration in the relation between host and graft was termed “adaptation” by Woodruff (21) who first demonstrated its development in animals. The consequence of the change is that patients often require progressively less stringent immunosuppression to retain stable homograft function.
To a considerable degree, this hope was realized in the recipients of consanguineous homografts. Only 2 of the 19 patients followed up for 6 to 10 months after their last globulin injections required upward adjustments of steroid therapy. In the others, prednisone doses have either remained at about the same level or have been reduced even further. In this connection, the long term courses of the 2 patients still surviving after late globulin therapy are of particular interest. Both had homografts which exhibited deterioration of function whenever an attempt was made to reduce maintenance doses of prednisone. During globulin therapy, the quantities of steroids were drastically attenuated without incident. Afterward, renal function has remained stable in both patients for longer than a year.
These comments on the effectiveness of antilymphocyte globulin, for preventing rejection of homografts from related donors, have not touched on the important question of histocompatibility. In these patients, there was a spectrum of antigenic mismatching which has not yet reflected itself in an equivalent mortality distribution since recipients of badly, moderately, and well matched grafts have survived with equal frequency. Nevertheless, the price of early survival was higher in patients with unfavorable compatibility. Their difficulties with acute rejection and their consequent need for larger quantities of steroids were greater than in the well matched grafts.
The firm correlation between the quality of antigenic matching and the smoothness of the early convalescence was a striking feature of these patients. In the past, similar, but far less consistent, observations have been made in our institutions by Terasaki (12, 18) and in other centers by Terasaki (5,16,17), Rapaport, and Stickel and their associates. However, in every large series of this kind, a significant number of patients have had courses which were not consonant with the results of the compatibility examination. One possible explanation was that important antigens were not being measured by the analyses. Another factor which has usually been neglected is the variable immunologic reactivity which was found by Wilson and Kirkpatrick in victims of uremia. In candidates for renal homotransplantation, these investigators found that the induction of delayed or immediate cutaneous hypersensitivity or of humoral antibody formation ranged from normal to profoundly depressed. After transplantation, those patients with pre-existing intact immunologic capabilities tended to have early and vigorous rejection, whereas those who did not usually had late and indolent rejections.
The more consistent results reported herein could be explained in terms of a partial elimination of this host variability by treatment with antilymphocyte globulin. The observations in our patients (14) and those of Monaco and his co-workers support the possibility that such therapy in man prevents, or partially suppresses, the appearance of delayed hypersensitivity reactions, even when these have been previously established. Thus, positive skin tests to tuberculin or other allergens become negative within 3 or 4 days after the institution of globulin injections. Of the various expressions of immunologic potential, delayed cutaneous hypersensitivity is believed to be the most similar to homograft rejection.
The foregoing considerations may explain why, in the intrafamilial transplantations, the addition of heterologous globulin therapy has made it more, rather than less, easy to detect the influence of antigenic matching upon the postoperative course. Nevertheless, the results have also made it clear that a considerable degree of histoincompatibility can be consistently overridden in related patients with the therapeutic regimen now being used. Whether or not the same conclusions will apply to homotransplantation between nonrelated people remains to be seen. There are not yet enough patients with cadaveric homotransplants to permit more than speculation about this issue.
Our experience is limited to 9 patients, the 6 renal homotransplantations herein reported and 3 recent orthotopic liver transplantations to be described elsewhere (10) in which survival was achieved beyond the first few postoperative days. In each of the recipients of the liver transplants, prednisone therapy was stopped or reduced to a dose of 5 milligrams per day or less within 1 postoperative month, despite the presence of major antigenic mismatches in 2 of the 3 patients. All 3 are still alive with good hepatic function from 5 weeks to 2½ months postoperatively.
There was a major antigenic mismatch in all 6 of the renal homotransplantations. Unfortunately, conclusions about these patients were obscured by 2 deaths within a day of each other, 3½ months after receipt of their homografts from a common donor. In both instances, the mortalities resulted from multiple pulmonary emboli which suggested some unrecognized peculiarity of the donor tissue. At autopsy, the kidneys had little, or no, evidence of rejection. In 3 of the other 4 patients, high steroid doses were used from the beginning because the poor or absent initial function, which resulted from acute tubular necrosis, made it impossible to know if rejection was occurring. Later, when prednisone was being reduced, delayed rejection was noted only in the patient who had stopped the medications.
In spite of this paucity of information, there seems little reason to doubt that anti-lymphocyte globulin will be of value in cadaveric transplantation. It is highly unlikely that it will be the kind of panacea which will permit the indiscriminate pairing of all donor-recipient combinations in the unrelated population. For a given recipient, however, it should expand the pool of cadaveric donors from which biologically-acceptable organs could be obtained.
SUMMARY
Twenty consecutive patients received renal homografts from blood relatives 10 to 16 months ago. All were treated with heterologous antilymphocyte globulin in progressively diminishing quantities for the first 4 postoperative months, and all recipients also received azathioprine as well as prednisone.
Nineteen or 95 per cent of these patients are alive with good function of their original homografts. In past similar instances, the death rate during comparable intervals was about 30 per cent. The improved results seem attributable to an extremely efficient prevention or treatment of early rejection without the need for such high doses of azathioprine and especially prednisone as were necessary prior to the use of globulin therapy. Infectious complications were reduced.
The 19 surviving patients have now been followed up for 6 to 10 months since they received their last globulin injection. Delayed rejection occurred in only 2 patients. In both, this was controlled with minor increases in the maintenance level of steroids. Two other patients, who were treated with globulin for the first time 5 and 11 months after transplantation, have subsequently had stable renal function for more than a year while receiving much smaller doses of prednisone than had previously been possible without precipitating rejection.
In the 19 surviving patients of the original consecutive series, as well as in 19 similarly treated recipients who were subsequently provided with consanguineous homografts, there was a spectrum of antigenic matches between the recipients and their donors. Until now, survival has been equivalent in patients with good, intermediate, or poor matches. However, the patients with the most compatible donors generally had the best renal function and required the smallest doses of prednisone. These results indicate that a considerable degree of histoincompatibility can be consistently overridden in intrafamilial transplantation by the combination of these agents, but at an increased cost.
There is not enough experience to date to know the extent to which adjuvant heterologous globulin therapy will influence results after transplantation between nonrelatives. Six patients with cadaver homotransplants have been treated, all with poor donor-recipient antigen compatibility. Two patients died but with little or no histologic evidence of homograft rejection. The others are alive after 3 to 11 months with poor to excellent function.
Acknowledgments
This work was supported by U. S. Public Health Service grants Nos. F05-TW-1154, AM 06283, AM 06344, HE 07735, AM 07772, AI 04152, FR 00051, and FR 00069.
Footnotes
Presented at the Sessions on Papers of General Interest, Clinical Congress of American College of Surgeons, 2 October 1967.
Contributor Information
THOMAS E. STARZL, Denver, Colorado
CARL G. GROTH, Stockholm, Sweden
PAUL I. TERASAKI, Los Angeles, California
CHARLES W. PUTNAM, Chicago, Illinois
LAWRENCE BRETTSCHNEIDER, Denver, Colorado
THOMAS L. MARCHIORO, Seattle, Washington
References
- 1.Gray JG, Monaco AP, Russell PS. Surgical Forum; Clinical Congress 1964. XV. Chicago: American College of Surgeons; 1964. Heterologous mouse antilymphocyte serum to prolong skin homografts; p. 142. [PubMed] [Google Scholar]
- 2.Iwasaki Y, Porter KA, Amend JR, Marchioro TL, Zühlke V, Starzl TE. The preparation and testing of horse antidog and antihuman antilymphoid plasma or serum as well as its protein fractions. Surg Gyn Obst. 1967;124:1. [PMC free article] [PubMed] [Google Scholar]
- 3.Jeejeebhoy HF. Immunological studies on the rat thymectomized in adult life. Immunology. 1965;9:417. [PMC free article] [PubMed] [Google Scholar]
- 4.Kashiwagi N, Brantigan CO, Brettschneider L, Groth CG, Starzl TE. Clinical reactions and serologic changes following the administration of heterologous antilymphocyte globulin to human recipients of renal homografts. Ann Int M. doi: 10.7326/0003-4819-68-2-275. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee HM, Hume DM, Vredevoe DL, Mickey MR, Terasaki PI. Serotyping for homotransplantation—IX, evaluation of leukocyte antigen matching with the clinical course and rejection types. Transplantation. 1967;5:1040. doi: 10.1097/00007890-196707001-00038. [DOI] [PubMed] [Google Scholar]
- 6.Levey RH, Medawar PB. Some experiments on the action of antilymphoid antisera. Ann N York Acad Sc. 1966;129:164. [Google Scholar]
- 7.Monaco AP, Wood ML, Russell PS. Effect of adult thymectomy on the recovery from immunologic depression induced by heterologous antilymphocyte serum. Science. 1965;149:423. doi: 10.1126/science.149.3682.432. [DOI] [PubMed] [Google Scholar]
- 8.Monaco AP, Wood ML, van der Werf BA, Russell PS. Effects of antilymphocyte serum on mice, dogs, and man. In: Wolstenholme GEW, O’Connor M, editors. Antilymphocytic Serum. London: J. & A. Churchill, Ltd; 1967. pp. 111–134. [Google Scholar]
- 9.Rapaport FT, Dausset J, Hamburger J, Hume DM, Kano K, Williams GM, Milgrom F. Serologic factors in human transplantation. Ann Surg. 1967;166:596. doi: 10.1097/00000658-196710000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Starzl TE, Groth CG, Brettschneider L, Moon JB, Fulginiti VA, Cotton EK, Porter KA. Extended survival in 3 cases of orthotopic homotransplantation of the human liver. Surgery. in press. [PMC free article] [PubMed] [Google Scholar]
- 11.Starzl TE, Marchioro TL, Porter KA, Iwasaki Y, Cerilli GJ. The use of heterologous antilymphoid agents in canine renal and liver homotransplantation and in human renal homotransplantation. Ann Surg Gyn Obst. 1967;124:301. [PMC free article] [PubMed] [Google Scholar]
- 12.Starzl TE, Marchioro TL, Terasaki PI, Porter KA, Faris TD, Herrmann TJ, Vredevoe DL, Hutt MP, Ogden DA, Waddell WR. Chronic survival after human renal homotransplantation. Ann Surg. 1965;162:749. doi: 10.1097/00000658-196510000-00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Starzl TE, Marchioro TL, Waddell WR. The reversal of rejection in human renal homografts with the subsequent development of homograft tolerance. Surg Gyn Obst. 1963;117:385. [PMC free article] [PubMed] [Google Scholar]
- 14.Starzl TE, Porter KA, Iwasaki Y, Marchioro TL, Kashiwagi N. The use of heterologous antilymphocyte globulin in human renal homotransplantation. In: Wolstenholme GEW, O’Connor MJ, editors. Antilymphocytic Serum. London: J. & A. Churchill, Ltd; 1967. pp. 4–34. [Google Scholar]
- 15.Stickel DL, Amos DB, Zmijewski CM, Glenn JF, Robinson RR. Human renal transplantation with donor selection by leukocyte typing. Transplantation. 1967;5:1024. [PubMed] [Google Scholar]
- 16.Terasaki PI, Mickey MR, McClelland JD. Histocompatibility Testing. Copenhagen: Munksgaard; 1968. Serotyping for homotransplantation—XIV, provisionary evaluation of various antisera in predicting clinical outcome of kidney transplantation. in press. [Google Scholar]
- 17.Terasaki PI, Vredevoe DL, Mickey MR. Serotyping for homotransplantation—X, survival of 196 grafted kidneys subsequent to typing. Transplantation. 1967;5:1057. doi: 10.1097/00007890-196707001-00041. [DOI] [PubMed] [Google Scholar]
- 18.Terasaki PI, Vredevoe DL, Porter KA, Mickey MR, Marchioro TL, Faris TD, Herrmann TJ, Starzl TE. Serotyping for homotransplantation—V, evaluation of a matching scheme. Transplantation. 1966;4:688. doi: 10.1097/00007890-196611000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wilson WEC, Kirkpatrick CH. Immunologic aspects of renal homotransplantation. In: Starzl TE, editor. Experience in Renal Transplantation. Philadelphia: W. B. Saunders Co; 1964. pp. 239–261. [Google Scholar]
- 20.Woodruff MFA, Anderson NF. The effect of lymphocyte depletion by thoracic duct fistula and by the administration of antilymphocyte serum on survival of skin homografts in rats. Ann N York Acad Sc. 1964;120:119. doi: 10.1111/j.1749-6632.1964.tb34710.x. [DOI] [PubMed] [Google Scholar]
- 21.Woodruff MFA, Woodruff HG. The transplantation of tissue; auto- and homotransplants of thyroid and spleen in the anterior chamber of the eye, and subcutaneously, in guinea pigs. Philos Tr R Soc London. 1950;234:559. [PubMed] [Google Scholar]