We found no sex differences in cervical-predominant involvement in ankylosing spondylitis but a strong association between hip arthritis and worse spinal involvement.
Abstract
Purpose:
To re-examine the patterns of radiographic involvement in ankylosing spondylitis (AS).
Materials and Methods:
This prospective study had institutional review board approval, and 769 patients with AS (556 men, 213 women; mean age, 47.1 years; age range, 18–87 years) provided written informed consent. Radiographs of the cervical spine, lumbar spine, pelvis, and hips were scored by using the Bath Ankylosing Spondylitis Radiology Index (BASRI) by an experienced radiologist. Differences in sacroiliitis grade between right and left sacroiliac joints, frequency of cervical- and lumbar-predominant involvement by sex, frequency of progression to complete spinal fusion, and association between hip arthritis and spinal involvement were computed for the cohort overall and for subgroups defined according to duration of AS in 10-year increments.
Results:
Symmetric sacroiliitis was seen in 86.1% of patients. Lumbar predominance was more common during the first 20 years of the disease, after which the cervical spine and lumbar spine were equally involved. Men and women were equally likely to have cervical-predominant involvement. Complete spinal fusion was observed in 27.9% of patients with AS for more than 30 years and in 42.6% of patients with AS for more than 40 years. Patients with BASRI hip scores of 2 or greater had significantly higher BASRI spine scores.
Conclusion:
There were no sex differences in cervical-predominant involvement in AS. Hip arthritis was strongly associated with worse spinal involvement.
© RSNA, 2010
Introduction
Ankylosing spondylitis (AS) is a chronic inflammatory disease of the axial skeleton, including the sacroiliac joints (1). The natural history of radiographic patterns in AS is poorly understood, and previous radiography-based studies that assessed the natural history of AS have shown conflicting data. The purpose of this study was to re-examine the patterns of radiographic involvement in AS in a large well-characterized cohort enrolled in the Prospective Study of Outcomes in Ankylosing Spondylitis trial (2–4).
Materials and Methods
Study Subjects
This prospective study was approved by the institutional review boards of each participating institution, and all patients provided written informed consent. Patients examined for this study were part of a large cohort enrolled at five institutions to characterize the genetic risk for susceptibility and severity of AS. Patients were recruited from the clinics of the investigators, local rheumatologists, from patient support and advocacy groups, and from the community by advertisements (2–4). Enrollment occurred between February 2002 and January 2009. All patients included in this cohort were 18 years of age or older and had disease that met the modified New York criteria for AS. The modified New York criteria were proposed in 1984; the diagnosis of definite AS is made when the sacroiliitis grade is 2 or greater bilaterally or 3 or greater unilaterally in the presence of one clinical criterion (5). Clinical criteria included low back pain and stiffness for more than 3 months that improves with exercise but not rest, limitation of the lumbar spine in the sagittal and frontal planes, and limitation of chest expansion relative to normal values corrected for age and sex (6).
All patients completed extensive personal and medical history questionnaires. Patients underwent a clinical evaluation that included a physical examination at each site by a study rheumatologist (M.H.W., M.M.W., J.D.R., J.C.D.). Clinical data collected at enrollment included age, sex, ethnicity, education level, marital status, smoking history (current or former smoker [including pack-years of smoking] or nonsmoker), and comorbid medical conditions. Additional data gathered included duration of AS, age at onset of AS symptoms, a family history of AS in a first-degree relative, a history of inflammatory bowel disease, iritis, total hip arthroplasty, and human leukocyte antigen (HLA)-B27 status. We did not focus on past treatments of the participants because no treatment is known to affect the severity of radiographic involvement (7,8). The cohort included 769 patients (556 [72.3%] men, 213 women; mean age, 47.1 years; range, 18–87 years) with a diagnosis of AS, of whom 622 (81%) were white. For the 556 men, the mean age was 48 years (range, 18–87 years), and for the 213 women, the mean age was 45 years (range, 18–80 years). The mean age at onset of AS was 23.8 years, and the mean duration of AS was 23.3 years. HLA-B27 was present in 663 (86.2%) of the patients, and iritis was reported for 267 (34.7%). A history of inflammatory bowel disease was reported for 38 (4.9%) of the patients. The median Bath Ankylosing Spondylitis Radiology Index (BASRI) spine score was 7, and the median BASRI lumbar and cervical spine scores were both 2.
Radiographic Evaluation
Radiographs were obtained in all patients at the time of enrollment. Images included an anteroposterior image of the pelvis, anteroposterior and lateral images of the lumbar spine, and a lateral image of the cervical spine. All of these images were reviewed simultaneously. Radiographs were scored by a single subspecialty-trained radiologist (T.J.L., with 20 years of experience in musculoskeletal imaging) using the BASRI scores. The radiologist was blinded to any and all clinical data, including severity and length of disease. Sacroiliac joints were graded according to the New York criteria established in 1966 (9), which describe five grades of sacroiliitis from 0 to 4 (0 = no disease, 1 = suspicious for disease, 2 = minimal disease, 3 = moderate disease, and 4 = severe disease). All patients had sacroiliitis scores of either grade 2 or higher bilaterally or grade 3 or higher unilaterally, meeting the modified New York criteria for AS. We examined the symmetry of sacroiliac joint changes by computing the difference in grades between the right and left sacroiliac joints.
The lumbar spine was defined as extending from the lower border of T12 to the upper border of S1, and the cervical spine was defined as extending from the lower border of C1 to the upper border of C7. The lumbar and cervical spine were graded separately on a scale from 0 to 4 (0 = no change; 1 = no definite change; 2 = any number of indications of erosions, squaring, or sclerosis, with or without syndesmophytes, on one or two vertebrae; 3 = syndesmophytes on three or more vertebrae, with or without fusion involving two vertebrae; and 4 = fusion involving three or more vertebrae) (Figs 1–3). The BASRI spine score is the sum of the mean scores for the right and left sacroiliac joints, the lumbar spine, and the cervical spine and has a possible range of 2 to 12 (10). The hips were graded on a scale of 0 to 4 (0 = no change, 1 = focal joint space narrowing, 2 = circumferential joint space narrowing > 2 mm, 3 = circumferential joint space narrowing ≤ 2 mm or bone-on-bone apposition of < 2 cm, and 4 = bone deformity or bone-on-bone apposition of ≥ 2 cm) (11). The BASRI score of the most severely affected hip was used for this study.
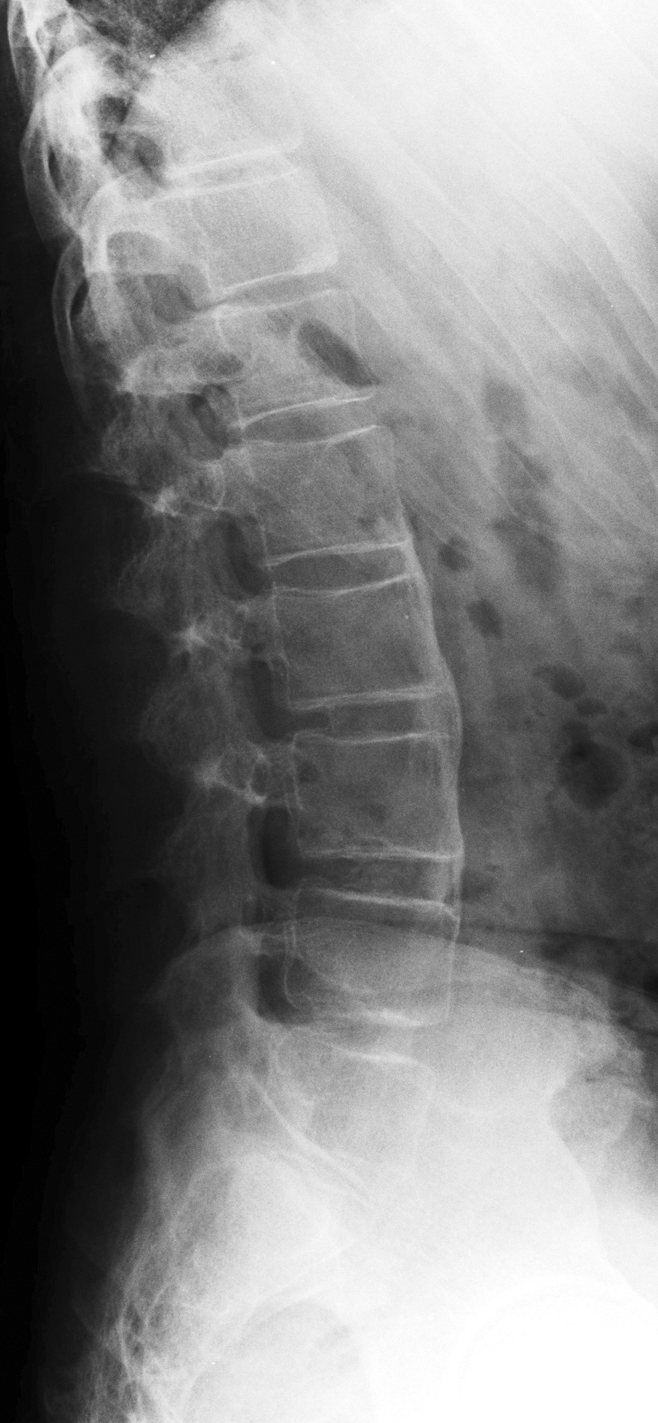
Figure 1:

Lateral radiograph of lumbar spine in a patient with AS and a BASRI lumbar spine score of 2. Syndesmophytes are present anteriorly at the superior and inferior aspects of the L4 vertebral body.
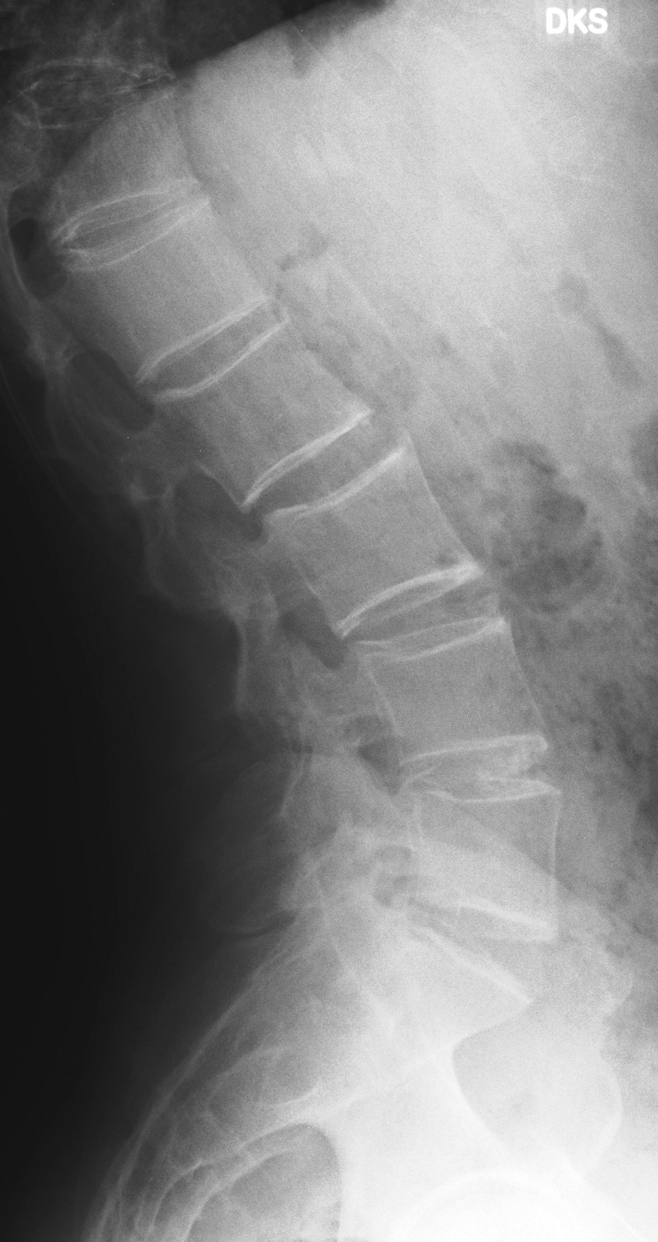
Figure 3:
Lateral radiograph of lumbar spine in a patient with AS and a BASRI lumbar spine score of 4 shows bridging syndesmophytes at multiple levels.
Figure 2:
Lateral radiograph of lumbar spine in a patient with AS and a BASRI lumbar spine score of 3. Bridging syndesmophytes are present anteriorly at L1 and L2. There are also nonbridging syndesmophytes at the anterior and superior aspects of L3.
In making comparisons of different regions of spinal involvement, we defined patients as having cervical-predominant involvement if their cervical spine BASRI score was at least two grades higher than their lumbar spine BASRI score (eg, cervical spine BASRI score/lumbar spine BASRI score, 4/0, 4/1, 4/2, 3/0, 3/1, or 2/0). Lumbar-predominant involvement was defined as when the lumbar spine BASRI score was at least two grades higher than the cervical spine BASRI score (eg, 0/4, 1/4, 2/4, 0/3, 1/3, or 0/2). We defined equal cervical and lumbar involvement as when BASRI scores were the same in both spinal regions (eg, 4/4, 3/3, 2/2, 1/1, or 0/0). Patients whose cervical and lumbar BASRI scores differed by one grade were excluded from these analyses to provide more distinct groups for comparison.
Fifty patients were selected as a computer-generated simple random sample without replacement for evaluation of intraobserver reliability. Thirty-two (64%) of these patients were men. Their median duration of AS was 22.1 years (range, 2–48 years), their median BASRI spine score was 6 (range, 2–12), and 22 (44%) patients had radiographic hip involvement. All features were closely similar to those of the entire cohort.
Statistical Analysis
We computed frequencies of each radiographic feature for the cohort overall and for subgroups defined according to duration of AS in 10-year increments. The duration of AS was calculated as the difference in years between the onset of persistent musculoskeletal symptoms of AS and the date of the radiographs. For some questions, we limited the analysis to the clinically relevant subgroup. For example, to investigate whether women were more likely than men to have cervical-predominant involvement, we limited the analysis to patients with 20 years or more of AS, to allow sufficient time for differences in sites of spinal involvement to become manifest (12). We used ordinal logistic regression to test if women and men differed in the likelihood of cervical-predominant, lumbar-predominant, or equal lumbar and cervical involvement, adjusting for the potential confounding factors of age, ethnicity (white versus “other”), presence of HLA-B27, smoking status, and history of iritis. We used median regression to test the association between BASRI spine scores and hip scores, adjusting for the potential confounders of age, sex, ethnicity, and age of onset of AS. The results of median regression provided an adjusted estimate of the median BASRI spine score for patients at each level of severity of hip arthritis (grades 0–4). Models were repeated by using the duration of AS (as a continuous variable) in place of age. Age and duration of AS were highly correlated, and therefore could not be included together in the same model because of collinearity. Analyses were performed by using software (SAS, version 9.2; SAS Institute, Cary, NC). P < .05 was considered to indicate a significant difference.
Results
Sacroiliac Joint Involvement
Bilateral symmetric sacroiliac joint involvement was observed in 80.2% of the patients as early as in the first decade of AS (Table 1). For all disease durations, a total of 662 patients (86.1%) displayed bilateral symmetric sacroiliitis. A significant asymmetry (defined as a difference of two or more grades between the right and left sacroiliac joints) was rarely seen, even in early AS.
Table 1.
Difference in Sacroiliitis Grades between Right and Left Sacroiliac Joints according to Decade of AS
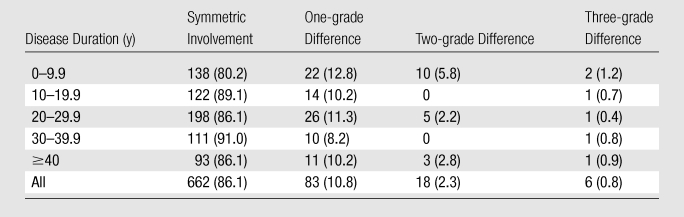
Note.—Data are numbers of patients, with percentages in parentheses.
Progression of Spinal Involvement
There was lumbar-predominant involvement in 19.4% and 29.5% of patients during the 1st and 2nd decades of AS, respectively (Table 2). BASRI scores of 0 (no radiographic changes) for the lumbar and cervical spines were included in the “equal” category, whereas data in patients with one-grade differences were deleted from comparison. Over all of the durations of AS, 66.7% of the patients had equal lumbar and cervical involvement. Cervical-predominant involvement was observed in 5.2% of the patients in early AS.
Table 2.
Cervical- and Lumbar-predominant Disease according to Decade of AS
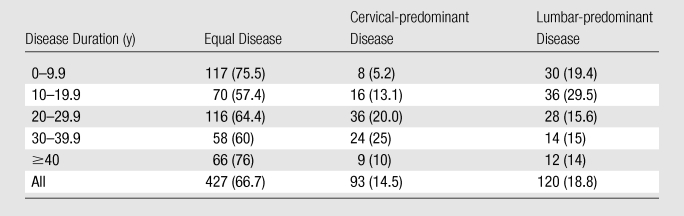
Note.—Data are numbers of patients, with percentages in parentheses. Cervical and lumbar BASRI scores that differed by one grade were excluded from this analysis.
Sex Association of Cervical Involvement
The frequency of cervical and lumbar-predominant involvement in 277 men and 86 women was calculated in patients with AS for more than 20 years. This calculation was limited a priori to participants with AS with longer durations of disease because cervical predominance is not frequently observed in early AS (12). The patients with a one-grade difference in cervical and lumbar predominance were omitted from the analysis. Cervical-predominant involvement was seen in 19.9% of men and 16% of women with AS for more than 20 years. Lumbar-predominant involvement was seen in 15.5% of men and 13% of women with AS for more than 20 years (Table 3). The results did not change when adjusted for sex differences in potential confounders. After adjustment for age, ethnicity, iritis, presence of HLA-B27, and smoking status, men and women had similar odds of having cervical-predominant involvement (adjusted odds ratio [OR] for men vs women = 1.24; 95% confidence interval [CI]: 0.67, 1.88; P = .66). After adjustment for duration of AS instead of age, the results were similar (adjusted OR = 1.11; 95% CI: 0.67, 1.86; P = .68). In this model, the duration of AS was not associated with the likelihood of cervical-predominant disease (adjusted OR = 0.995 per year of AS; 95% CI: 0.97, 1.02; P = .67), but the group was limited to those with 20 or more years of AS.
Table 3.
Frequency of Cervical- and Lumbar-predominant Involvement according to Sex
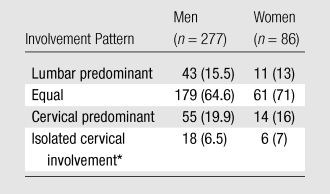
Note.—Data are numbers of patients, with percentages in parentheses. This analysis was limited to patients with AS for 20 or more years. P = .56 for the comparison of lumbar, equal, and cervical disease predominance between men and women; P = .88 for the comparison of isolated cervical involvement between men and women.
Isolated cervical involvement was defined as a cervical spine score of 3 or greater along with a lumbar spine score of 0 or 1.
We also examined sex differences in isolated cervical involvement, defined as a cervical spine score of 3 or greater along with a lumbar spine score of 1 or 0. Isolated cervical involvement was rare, but 6.5% of men with AS for more than 20 years had isolated cervical involvement, compared with 7% of women (Table 3). Adjustment for age, ethnicity, iritis, presence of HLA-B27, and smoking status did not alter the association (adjusted OR for men vs women = 1.02; 95% CI: 0.37, 2.78; P = .97). In a multivariate model that adjusted for duration of AS instead of age, results were similar. Duration of AS was not associated with likelihood of isolated cervical disease (adjusted OR = 0.97; 95% CI: 0.92, 1.03; P = .26) among patients with AS for 20 or more years.
Progression to Complete Spinal Fusion
The frequency of a BASRI score of 12 was tabulated in patients with AS for 30 or more years. Progression to complete spinal fusion was seen in only 34 (27.9%) of 122 patients with a disease duration between 30 and 40 years (mean age, 56.1 years ± 7.1 [standard deviation]) and in only 46 (42.6%) of 108 patients with a disease duration of 40 or more years (mean age, 65.6 years ± 8.4). The intraobserver reliability of the total BASRI spine score, based on two readings of the radiographs in 50 patients performed at least 3 months apart, was 0.987 (95% CI: 0.98, 0.991).
Association between Hip Arthritis and Spinal Involvement
Median BASRI spine scores were compared according to the grade of the most severely affected hip (Table 4). In unadjusted analyses, the median BASRI spine scores were higher among patients with higher hip scores. Adjusting for the duration of AS, patients with hip scores of 2, 3, or 4 (BASRI hip score of 2 = circumferential joint space narrowing > 2mm, 3 = circumferential joint space narrowing ≤ 2 mm or bone-on-bone apposition of < 2 cm, 4 = bone deformity or bone-on-bone apposition of ≥ 2 cm) had median BASRI spine scores that were more than two points higher than those of patients with a hip score of 0. Results were similar after further adjustment for sex, ethnicity, and age of onset of AS. Increased duration of AS was also associated with worse BASRI spine scores (estimate, 0.15 per year [95% CI: 0.12, 0.17]).
Table 4.
Median BASRI Spine Scores and Median Difference in BASRI Spine Scores according to Score of the Worst Hip
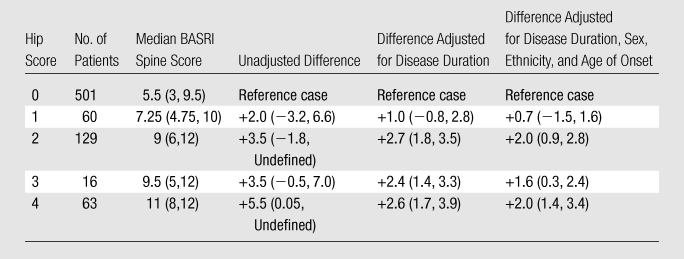
Note.—Data in parentheses are 95% CIs.
Discussion
Our findings demonstrate that the majority of patients have symmetric sacroiliitis even in early AS. This observation confirms those by Helliwell et al (13), who compared radiographs in 91 patients with classic AS with those in seven patients with reactive arthritis and found that 85% of the patients with AS had symmetric sacroiliitis, compared with 43% of those with reactive arthritis. We also found radiographic changes similar to those observed in previous studies (14) that indicate that lumbar radiographic findings typically precede cervical findings. According to our data, cervical spine involvement was not as evident until after 20 or more years of disease. Over all the durations of AS, most patients had equal lumbar and cervical involvement, although much of the “equal” involvement seen in the first 2 decades was the result of patients without any lumbar or cervical changes. When we examined data for all patients over all disease durations, there was a trend toward lumbar predominance over cervical predominance (18.8% versus 14.5%). Brophy et al (12), in a natural history observational cohort of 571 patients with AS, reported that more patients had lumbar involvement than cervical disease at all points in the disease duration at the time of cross-sectional analysis. Additionally, they reported that 75% of patients had cervical spinal involvement whereas 85% had lumbar spinal involvement after 25 years of disease, suggesting that lumbar spine involvement may precede cervical disease.
In our study, both men and women were equally likely to have cervical-predominant involvement. When further examining sex differences in isolated cervical involvement, frequencies were similar in women and men in our study. Our findings contrast with those of Resnick et al (15), who studied 98 patients with definite AS and found that radiographic changes in the cervical spine were more common in women. Braunstein et al (16), in a small cohort of patients with AS, noted that three women and four men had cervical involvement. These observers could not find any notable association between cervical spine disease and female sex. In our study, the close similarity in the percentages of men and women with cervical-predominant disease (19.9% versus 16%) indicates that the absence of a statistical difference is not due to limited power. It is unclear why our results with respect to sex associations with cervical spine involvement differ from those reported in the literature, but this may be due to differences in patient selection or the representativeness of the samples studied.
Our data revealed that less than one-half of patients had complete spinal fusion after 40 or more years of disease. This observation refutes the previous belief that most patients with AS will eventually experience spinal fusion over the course of their disease. This finding raises the question as to whether AS is truly a linearly progressive disease with an approximate 35% change every 10 years as demonstrated by Brophy et al (12). We cannot make conclusions on radiographic differences that may be caused by treatment because there is no treatment, to date, that is known to affect the severity of radiographic involvement in AS (7,8).
Last, our findings of the positive correlation between BASRI hip and BASRI spine scores concur with a strong association of hip disease with more severe axial involvement noted in previous studies. Brophy et al (12,17) reported that hip involvement is a marker for cervical disease and a major prognostic marker for long-term severe disease. Doran et al (18) also noted that radiologic hip involvement is significantly associated with higher scores of spinal radiologic change.
The strength of our study lay in its large well-characterized cohort, which allowed us to observe patterns of radiographic involvement. The cohort was sufficiently large to enable us to stratify results according to decade of AS to observe how patterns of involvement may change over the course of AS. However, the study was cross sectional, and we cannot conclude that our results regarding the evolution of patterns of involvement across decades of AS would be the same had patients been followed longitudinally. We used BASRI for grading radiographic changes because it is disease specific, valid, simple, and rapid to perform (10). Owing to the simplicity of this scoring system, the BASRI does not pick up minor radiographic changes. The score does not change with each additional erosion or sclerosis, and will always remain grade 2 until there is fusion between two vertebrae or three or more syndesmophytes are identified (19). Our study was limited by the use of one observer; however, the reliability was excellent. Using conventional radiographs may have also potentially limited our detection of early sacroiliitis because radiography is not as sensitive as magnetic resonance imaging in the detection of early inflammation (20).
In summary, we found no sex differences in cervical-predominant involvement but a strong association between hip arthritis and worse spinal involvement. Longitudinal studies, over decades, would be ideal for further evaluating the clinical importance and natural history of radiographic changes in patients with AS.
Advances in Knowledge.
Men and women were equally likely to have cervical-predominant involvement in ankylosing spondylitis.
Hip arthritis was strongly associated with worse spinal involvement.
Received March 17, 2010; revision requested May 4; revision received June 28; accepted July 7; final version accepted August 2.
Funding: This research was supported by the National Institutes of Health (grant P01-AR052915).
Supported by the Cedars-Sinai General Clinical Research Center (grant M01-RR00425) and the University of Texas at Houston General Clinical Research Center (grant M01-RR02558).
Authors stated no financial relationship to disclose.
Abbreviations:
- AS
- ankylosing spondylitis
- BASRI
- Bath Ankylosing Spondylitis Radiology Index
- CI
- confidence interval
- HLA
- human leukocyte antigen
- OR
- odds ratio
References
- 1.Khan M. Ankylosing spondylitis: clinical aspects. In: Calin A, Taurog J, eds. The spondylarthritides. Oxford, England: Oxford University Press, 1998 [Google Scholar]
- 2.Gensler LS, Ward MM, Reveille JD, Learch TJ, Weisman MH, Davis JC., Jr Clinical, radiographic and functional differences between juvenile-onset and adult-onset ankylosing spondylitis: results from the PSOAS cohort. Ann Rheum Dis 2008;67(2):233–237 [DOI] [PubMed] [Google Scholar]
- 3.Ward MM, Hendrey MR, Malley JD, et al. Clinical and immunogenetic prognostic factors for radiographic severity in ankylosing spondylitis. Arthritis Rheum 2009;61(7):859–866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ward MM, Weisman MH, Davis JC, Jr, Reveille JD. Risk factors for functional limitations in patients with long-standing ankylosing spondylitis. Arthritis Rheum 2005;53(5):710–717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.van der Linden S, Valkenburg HA, Cats A. Evaluation of diagnostic criteria for ankylosing spondylitis: a proposal for modification of the New York criteria. Arthritis Rheum 1984;27(4):361–368 [DOI] [PubMed] [Google Scholar]
- 6.Goie The HS, Steven MM, van der Linden SM, Cats A. Evaluation of diagnostic criteria for ankylosing spondylitis: a comparison of the Rome, New York and modified New York criteria in patients with a positive clinical history screening test for ankylosing spondylitis. Br J Rheumatol 1985;24(3):242–249 [DOI] [PubMed] [Google Scholar]
- 7.van der Heijde D, Salonen D, Weissman BN, et al. Assessment of radiographic progression in the spines of patients with ankylosing spondylitis treated with adalimumab for up to 2 years. Arthritis Res Ther 2009;11(4):R127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.van der Heijde D, Landewé R, Baraliakos X, et al. Radiographic findings following two years of infliximab therapy in patients with ankylosing spondylitis. Arthritis Rheum 2008;58(10):3063–3070 [DOI] [PubMed] [Google Scholar]
- 9.Bennett PH, Wood PHN. Population studies of the rheumatic diseases. Amsterdam, the Netherlands: Excerpta Medica Foundation, 1968;456–457 [Google Scholar]
- 10.MacKay K, Mack C, Brophy S, Calin A. The Bath Ankylosing Spondylitis Radiology Index (BASRI): a new, validated approach to disease assessment. Arthritis Rheum 1998;41(12):2263–2270 [DOI] [PubMed] [Google Scholar]
- 11.MacKay K, Brophy S, Mack C, Doran M, Calin A. The development and validation of a radiographic grading system for the hip in ankylosing spondylitis: the Bath ankylosing spondylitis radiology hip index. J Rheumatol 2000;27(12):2866–2872 [PubMed] [Google Scholar]
- 12.Brophy S, Mackay K, Al-Saidi A, Taylor G, Calin A. The natural history of ankylosing spondylitis as defined by radiological progression. J Rheumatol 2002;29(6):1236–1243 [PubMed] [Google Scholar]
- 13.Helliwell PS, Hickling P, Wright V. Do the radiological changes of classic ankylosing spondylitis differ from the changes found in the spondylitis associated with inflammatory bowel disease, psoriasis, and reactive arthritis? Ann Rheum Dis 1998;57(3):135–140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gran JT, Skomsvoll JF. The outcome of ankylosing spondylitis: a study of 100 patients. Br J Rheumatol 1997;36(7):766–771 [DOI] [PubMed] [Google Scholar]
- 15.Resnick D, Dwosh IL, Goergen TG, et al. Clinical and radiographic abnormalities in ankylosing spondylitis: a comparison of men and women. Radiology 1976;119(2):293–297 [DOI] [PubMed] [Google Scholar]
- 16.Braunstein EM, Martel W, Moidel R. Ankylosing spondylitis in men and women: a clinical and radiographic comparison. Radiology 1982;144(1):91–94 [DOI] [PubMed] [Google Scholar]
- 17.Brophy S, Calin A. Ankylosing spondylitis: interaction between genes, joints, age at onset, and disease expression. J Rheumatol 2001;28(10):2283–2288 [PubMed] [Google Scholar]
- 18.Doran MF, Brophy S, MacKay K, Taylor G, Calin A. Predictors of longterm outcome in ankylosing spondylitis. J Rheumatol 2003;30(2):316–320 [PubMed] [Google Scholar]
- 19.Wanders AJ, Landewé RB, Spoorenberg A, et al. What is the most appropriate radiologic scoring method for ankylosing spondylitis? a comparison of the available methods based on the Outcome Measures in Rheumatology Clinical Trials filter. Arthritis Rheum 2004;50(8):2622–2632 [DOI] [PubMed] [Google Scholar]
- 20.Braun J, Bollow M, Eggens U, König H, Distler A, Sieper J. Use of dynamic magnetic resonance imaging with fast imaging in the detection of early and advanced sacroiliitis in spondylarthropathy patients. Arthritis Rheum 1994;37(7):1039–1045 [DOI] [PubMed] [Google Scholar]


