Abstract
INTRODUCTION:
Parents have a fundamental role in promoting the healthy weight of their children.
OBJECTIVES:
To determine parental perceptions of their child’s body weight, eating and physical activity (PA) behaviours, and to test a predictive model of parental perceptions regarding their child’s PA and healthy eating behaviours.
METHODS:
A random-digit telephone survey was conducted among parents of children four to 12 years of age living in the Champlain region of Ontario. Descriptive statistics were used to summarize the responses. Path analysis was used to identify predictors of parental perceptions of PA and healthy eating.
RESULTS:
The study sample consisted of 1940 parents/caregivers. Only 0.2% of parents reported their child as being obese; 8.6% reported their child as being overweight. Most parents perceived their child to be physically active and eating healthily. Approximately 25% of parents reported that their child spent 2 h/day or more in front of a screen, and that their child consumed less than three servings of fruits and vegetables daily, and regularly consumed fast food. Variables that correlated with PA perceptions included time spent reading/doing homework, interest in PA, perceived importance of PA, frequency of PA, level of parental PA, participation in organized sport, child weight and parental concern for weight. Variables that predicted perceptions regarding healthy eating were parental education, household income, preparation of home-cooked meals, fruit and vegetable intake, and concern for and influence on the child’s weight.
CONCLUSIONS:
Parents in the present study sample did not appear to understand, or had little knowledge of the recommendations for PA and healthy eating in children. Parents appeared to base their judgment of healthy levels of PA or healthy eating behaviours using minimal criteria; these criteria are inconsistent with those used by health professionals to define adequate PA and healthy eating. The present survey highlights an important knowledge gap between scientific opinion and parental perceptions of the criteria for healthy PA and eating behaviours.
Keywords: Children, Nutrition, Parents, Perceptions, Physical activity, Survey
Abstract
INTRODUCTION :
Les parents jouent un rôle fondamental dans la promotion du poids santé de leur enfant.
OBJECTIFS :
Déterminer les perceptions qu’ont les parents des comportements liés au poids, à l’alimentation et à l’activité physique (AP) et mettre à l’essai un modèle prédictif de perceptions parentales au sujet des comportements de leur enfant à l’égard de l’AP et d’une saine alimentation.
MÉTHODOLOGIE :
Les chercheurs ont mené une enquête téléphonique à composition aléatoire chez les parents d’enfants de quatre à 12 ans qui vivaient dans la région de Champlain, en Ontario. Ils ont utilisé des statistiques descriptives pour résumer les réponses, de même que l’analyse causale pour déterminer les prédicteurs des perceptions des parents par rapport à l’AP et à une saine alimentation.
RÉSULTATS :
L’échantillon à l’étude se composait de 1 940 parents ou tuteurs. Seulement 0,2 % des parents ont déclaré leur enfant obèse, tandis que 8,6 % ont indiqué qu’il faisait de l’embonpoint. La plupart des parents percevaient que leur enfant était physiquement actif et qu’il avait une saine alimentation. Environ 25 % ont déclaré que leur enfant passait au moins deux heures par jour devant un écran, qu’il consommait moins de trois portions de fruits et légumes par jour et qu’il consommait régulièrement des aliments prêts-à-manger. Les variables corrélées avec les perceptions par rapport à l’AP incluaient le temps consacré à lire et à faire des devoirs, l’intérêt envers l’AP, l’importance perçue de l’AP, la fréquence d’AP, le degré d’AP de la part des parents, la participation à des activités sportives organisées, le poids de l’enfant et les préoccupations qu’avaient les parents envers ce poids. Les variables prédictives des perceptions de saine alimentation étaient l’éducation des parents, le revenu familial, la préparation de repas maison, la consommation de fruits et légumes et les préoccupations et les influences à l’égard du poids de l’enfant.
CONCLUSIONS :
Les parents du présent échantillon à l’étude ne semblaient pas comprendre ou connaissaient peu les recommandations relatives à l’AP et à une saine alimentation chez les enfants. Les parents semblaient fonder leur jugement quant à un taux sain d’AP ou à des comportements de saine alimentation sur des critères minimaux. Ces critères ne correspondent pas à ceux utilisés par les professionnels de la santé pour définir une AP suffisante et une saine alimentation. La présente enquête fait ressortir d’importantes disparités de connaissances entre l’avis des scientifiques et les perceptions qu’avaient les parents des critères de comportement liés à une saine AP et à une saine alimentation.
Obesity is the most common childhood disorder that has reached an epidemic proportion in the developed world (1–3). Overweight or obese children are at risk for both metabolic/medical and psychological comorbidities including insulin resistance, metabolic syndrome, diminished self-esteem, and reduced well-being and quality of life (4). Canadian school-age youth are among the most obese in the world (ranked 27 of 29 developed nations) (5), and more than two-thirds of obese children will become obese adults (6–8). These sobering data underscore the significant long-term health implications of childhood obesity in Canada.
Inactivity and poor dietary practices are widespread among today’s youth, and experts believe that increasing obesity rates are reflective of an obesogenic social environment. Many factors contribute to the development of such a social setting including greater access to sedentary leisure time activities, lower rates of active transportation, perceived unsafe environments for outdoor play and pressures on schools to place a greater emphasis on academic achievement at the expense of physical education. An increased exposure to poor-quality food due to an overabundance of nutritionally unbalanced snacks, convenience and fast foods (9); superfluous advertising of nutrient-poor, high-sugar foods aimed at children (10); and the lower cost of calorically dense, less nutritionally valuable food choices (11) are also considered to be important contributing factors to this modern epidemic. Parents and the family have considerable influence over their children’s physical activity (PA) and eating behaviours (12–16). Awareness that their child is at risk or has poor lifestyle habits is an important prerequisite for the motivation to act (17); between 60% and 80% of parents fail to recognize their child’s status as overweight or obese and, furthermore, the majority do not report concern for their child’s health (18–22). Thus, those less-concerned parents are unlikely to take steps to provide a healthier lifestyle or environment for their children. However, little is known about the factors that influence parents’ perceptions of their child’s weight, PA and eating habits.
We performed a regional survey to assess parental perceptions of PA and eating patterns of their school-age children. The objectives of the present study were the following: to describe parental perceptions of their child’s body weight status, eating and PA behaviours; and to test a predictive model of parental perceptions of their child’s PA and healthy eating behaviours.
METHODS
A random-digit telephone survey was conducted between May 29 and July 4, 2007. A random sampling methodology was implemented using publicly available telephone listings.
Subjects
Respondents were eligible to participate if they were parents or primary caregivers of a child four to 12 years of age; a resident of the Champlain region of Ontario and were able to complete the survey in English or French. Up to 10 call attempts per household were made. If there was more than one child between four and 12 years of age living in the home, the respondent was asked to reference the child whose birthday was next in the calendar year when responding.
Data instrument
A structured telephone survey consisting of 36 items was developed by health professionals, public health epidemiologists and child obesity experts, and was finalized with input from a survey research firm with extensive experience in the design and conduct of health-related telephone surveys. The survey design committee consulted existing questionnaires addressing similar topics such as the Speaking of Food and Healthy Living questionnaire commissioned by the Dietitians of Canada and Kraft Canada Inc, and adapted relevant questions including open-ended and skip-pattern items. The survey was developed to have an average completion time of approximately 12 min to 13 min, and included sections related to parent’s/primary caregiver’s demographics, parental perceptions of the child’s PA level, eating habits and body weight, as well as concerns regarding the health effects of being overweight and their perceived degree of influence over these behaviours. Given that the objectives of the study were to understand parental perceptions, respondents were not prompted with details defining ‘active’, ‘inactive’, ‘good’ or ‘excellent’ eating habits.
The survey was pilot tested in the five regions of Champlain by experienced interviewers using a computer-assisted telephone interview system. Following the administration of 20 surveys, word refinement, item clarification and removal, and alterations to response options were performed. The final version of the questionnaire (English and French) can be found at www.ccpnetwork.ca/en_priorities_schoolchildren.php.
Analysis
LISREL version 8.8 (Scientific Software International Inc, USA) was used to examine the relationship between the demographic characteristics (ie, the parent’s age, marital status, education, household income, population size, sex, number of children living in the home, and the child’s age and sex) and parents’ perceptions of their children’s PA levels and eating habits.
Path analyses:
The hypothesized relationship between study variables and parental perceptions of PA and healthy eating behaviours was examined using path analysis. Path analysis is a statistical technique for estimating the magnitude and significance (indirect and direct) of hypothetically causal relationships among sets of variables (23).
Path analyses were conducted using weighted least-squares procedures in LISREL 8.8 to explore the determinants of parental perception of their child’s PA and healthy eating behaviours. Given that the variables were ordinal, an asymptotic covariance matrix was analyzed, and all variables that were found to have significant relationships (P<0.05) with the dependent variables (child’s PA and healthy eating habits) were retained and tested in the final path analyses. The path model for PA was calculated using two sets of ordinary least-squares regression equations. The first set explored the relationship between the demographic characteristics as independent variables and perceptual factors as dependant variables. The second set, in which the parent’s perception of the child’s PA level was the dependent variable, included demographic variables and the aforementioned perceptual factors as independent variables. Similarly, the first set of analyses related to the path model for healthy eating explored demographic characteristics as independent variables and factors linked to eating habits, as well as concern regarding the child’s weight and influence on the child’s weight as dependent variables. The second set defined parental perception of the child eating healthy as the dependent variable, and demographic variables as well as the previously described eating behaviour factors as independent variables.
For each variable found to be significant in the proposed model, beta- (path) correlation coefficients, or standardized regression coefficients, were reported. The beta-coefficients measure the relative strength and sign of the effect from a causal variable to an outcome variable in the model and, thus, in the present case help to describe the amount of variance in parental perceptions explained by any given variable. These coefficients indicate the direct effect of a variable assumed to be a cause on another variable assumed to be an effect, and it is generally accepted that standardized coefficients that are greater than 0.8 are large, between 0.5 and 0.8 are moderate and less than 0.5 are small (23).
RESULTS
Study participants
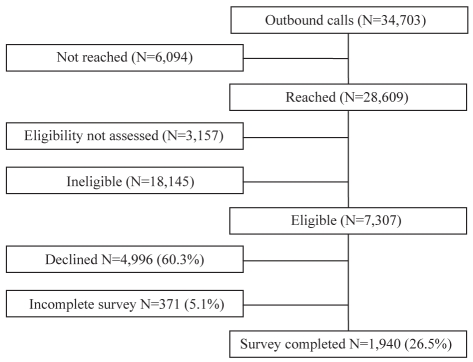
A total of 28,609 households were contacted and 7307 (25.5%) persons met the eligibility criteria (Figure 1). Sixty-eight per cent (n=4996) of parents declined participation in the survey due to lack of interest, and an additional 5.1% (n=371) of parents did not complete the full survey. The study sample consisted of 1940 telephone surveys representing 26.5% of eligible parents.
Figure 1).
Summary of recruitment flow
Table 1 presents a summary of the demographic characteristics of study participants. Based on the 2006 Statistics Canada Census data (24) for the Champlain region, the current surveyed population was quite comparable with regard to the following Census data: median age: 39.5 years; family characteristics: 72% married, 12% common-law and 15% single parent; median income: $64,555; and education: 33.7% high school or less, 29.7% some or all college/vocational school/apprenticeship, and 36.6% university bachelors degree or more. The majority (75.4%) of respondents to our survey were female.
TABLE 1.
Demographic characteristics of survey respondents and their children
| Variable | Overall |
|---|---|
| Age of child, years | |
| 4–6 | 634 (32.7) |
| 7–9 | 516 (30.8) |
| 10–12 | 708 (36.5) |
| Sex of child | |
| Male | 990 (51.0) |
| Children 4–12 years of age who live in the home, mean ± SD | 1.69±0.79 |
| Sex of respondent | |
| Female | 1462 (75.4) |
| Age of respondent, years | |
| 19–24 | 27 (1.4) |
| 25–34 | 486 (25.1) |
| 35–44 | 1107 (57.1) |
| 45–54 | 289 (14.9) |
| 55–64 | 24 (1.2) |
| Marital status of respondent | |
| Married | 1467 (75.6) |
| Common-law or living with partner | 205 (10.6) |
| Divorced, separated or single | 248 (13.8) |
| Education level of respondent | |
| High school graduate or less | 442 (22.8) |
| Some or all postsecondary (college/technical/vocational) | 900 (46.4) |
| Some or all university bachelor’s degree or graduate studies | 593 (30.6) |
| Household income ($) before taxes | |
| Less than 20,000 | 90 (4.6) |
| 20,000 to less than 40,000 | 253 (13.0) |
| 40,000 to less than 60,000 | 325 (16.8) |
| 60,000 to less than 80,000 | 326 (16.8) |
| 80,000 to less than 100,000 | 266 (13.7) |
| 100,000 to less than 120,000 | 187 (9.6) |
| 120,000 or more | 232 (12.0) |
| Don’t know | 54 (2.8) |
| Refused to respond | 207 (10.7) |
Data presented as n (%) unless otherwise indicated. The sum of responses may not always add up to 100%; responses less than 1% may not have been reported
Parental perceptions of their child’s PA behaviours and eating habits
Table 2 presents the respondent’s perceptions of their child’s PA behaviours. The majority of parents considered their child to be ‘active’ or ‘very active’. It was a widely held view among survey respondents that their child was active during most days of the week, outside of school hours. Approximately 25% of respondents reported that their child spent an average of 2 h/day or more in front of a screen (television, video or Internet). Table 3 presents a summary of the responses regarding eating habits. More than 80% of respondents considered their child to have ‘good’ or ‘excellent’ eating habits.
TABLE 2.
Respondent’s perceptions of their child’s physical activity habits
| Question | Overall, % |
|---|---|
| How physically active would you consider your child to be? | |
| Very active | 57.7 |
| Active | 32.0 |
| Somewhat active | 9.6 |
| Inactive | 0.7 |
| On average, outside of school hours, how many days of the week is your child physically active? | |
| 0 | 0.7 |
| 1–2 | 5.7 |
| 3–5 | 25.1 |
| >5 | 68.5 |
| On average, for how many minutes per day is your child physically active outside of school hours? | |
| 1–15 | 0.9 |
| 16–30 | 6.2 |
| 31–60 | 20.6 |
| >60 | 71.7 |
| In the past month, has your child done any of the following? | |
| Played outdoors | 99.1 |
| Participated in a team sport | 71.8 |
| Been involved in family outings (walking, hiking, biking) | 93.7 |
| Participated in other recreational/physical activities | 87.2 |
| On average, how many hours per day does your child spend watching TV or movies, playing video or computer games, or surfing the Internet? | |
| None | 4.2 |
| <2 h | 71.3 |
| 2–3 h | 19.8 |
| >3 h | 4.5 |
| On average, how many hours per day does your child spend reading or doing homework? | |
| None | 4.8 |
| <2 | 83.7 |
| 2–3 | 7.8 |
| >3 | 1.2 |
| Not applicable/too young | 2.4 |
| How important is it to you for your child to be physically active? | |
| Very important | 81.9 |
| Important | 17.0 |
| Somewhat important | 0.9 |
| What reasons discourage or limit your child from participating in physical activity? | |
| Time | 13.7 |
| Health barriers, illness or physical challenge | 14.1 |
| Safety concerns | 1.7 |
| Location or transportation | 4.8 |
| Equipment availability | 1.3 |
| Child’s lack of interest | 8.0 |
| Expenses or cost | 5.4 |
| Too tired | 2.6 |
| Weather | 13.1 |
| No reason | 37.6 |
| How physically active do you (the parent) consider yourself to be? | |
| Inactive | 5.0 |
| Somewhat active | 33.0 |
| Active | 42.0 |
| Very active | 20.0 |
The sum of responses may not always add up to 100%; responses less than 1% may not have been reported. Multiple responses were possible for certain questions. TV Television
TABLE 3.
Respondent’s perceptions of their child’s eating habits
| Question | Overall, % |
|---|---|
| How would you rate your child’s eating habits? | |
| Poor | 2.6 |
| Fair | 14.8 |
| Good | 56.7 |
| Excellent | 25.8 |
| On average, how many servings of fruit and vegetables (excluding potatoes) does your child consume daily? | |
| 0 | 1.0 |
| 1–2 | 24.3 |
| 3–5 | 57.9 |
| 6 or more | 16.0 |
| On average, how many times per week does your child eat breakfast? | |
| 0 | 0.5 |
| 1–2 | 2.1 |
| 3–5 | 5.0 |
| >5 | 92.7 |
| On average, how many times per week does your family eat supper prepared outside of the home? | |
| <1 | 43.6 |
| 1–2 | 53.5 |
| 3–5 | 2.5 |
| On average, how many times per week does your child eat supper in front of the television? | |
| 0 | 59.2 |
| 1–2 | 24.5 |
| >3 | 15.9 |
| On average, how many cans/bottles/cups of soft drinks, sports drinks, or fruit-flavoured drinks that are not 100% fruit juice does your child consume per week? | |
| 0 | 30.9 |
| 1–3 | 42.1 |
| 4–6 | 13.6 |
| 7 or more | 12.4 |
| On average, on how many days per week does your child eat fast foods? | |
| 0 | 47.1 |
| 1–2 | 50.4 |
| 3–5 | 2.2 |
| To what extent do you agree that your child influences your purchase of unhealthy foods? | |
| Strongly disagree | 9.9 |
| Disagree | 24.9 |
| Neither agree nor disagree | 14.5 |
| Agree | 34.1 |
| Strongly agree | 16.1 |
The sum of responses may not always add up to 100%; responses less than 1% may not have been reported. Multiple responses were possible for certain questions
Correlation analyses
Parental perception of their children’s PA levels showed that the older their children were, the more likely parents considered their children to be less active (r=–0.17; P<0.001). On the other hand, parents who were married/common-law compared with those who were not were more likely to consider their children to be active (r=–0.07; P<0.001). In terms of parental perception of their children’s eating habits, results showed that those with household incomes of more than $60,000 per year (versus less than $60,000; r=0.03; P<0.01) and those who had at least a grade 12 education (versus lower than grade 12; r=0.06; P<0.01) were more likely to consider their children’s eating habits to be favourable. Therefore, the aforementioned demographics were included in the final path analyses. Correlation analyses between PA opportunities and parental perception of their child’s PA showed that if parents reported that their child participated in a team sport (r=0.23; P<0.01); had been involved in family outings such as walking, hiking and/or biking (r=0.23; P<0.01) and/or participated in other recreation/PA (r=0.22; P<0.01), they were more likely to consider their child to be active. As for barriers, results showed that if parents reported health barriers (r=–0.01; P<0.01), child’s lack of interest (r=–0.49; P<0.01) and/or bad weather (r=–0.06; P<0.01), they were more likely to consider their children to be less active. The present analyses also showed that the perceived increase in child activity was significantly related to the number of days children were active outside of school (r=0.41; P<0.01), the average minutes per day of activity outside of school (r=0.37; P<0.01), time spent by the children watching television (r=–0.28; P<0.01), time spent doing homework or reading (r=–0.12; P<0.05), the importance placed on the children’s activity level by the parents (r=0.25; P<0.001), the perceived activity level of the parents themselves (r=0.21; P<0.01), their children’s weight status (r=–0.29; P<0.001), their concern about their children’s weight (r=–0.24; P<0.01), their perceived influence over their children’s weight (r=0.07; P<0.05) and their concern over their children developing a chronic disease (r=–0.08; P<0.05).
In terms of parental support for healthy eating and parents’ perceptions of their children’s eating habits, results showed that if parents reported preparing home-cooked meals (r=0.19; P<0.05) and eating meals as a family by sitting together at the table (r=0.13; P<0.01), they were more likely to rate their children’s eating habits more favourably. In addition, results also showed that the perceived quality of their children’s eating habits was significantly related to the amount of fruits and vegetables they perceived their children to eat (r=0.35; P<0.01), soft drink consumption (r=–0.14; P<0.01), their children’s weight status (r=–0.01; P<0.01), their concern about their children’s weight (r=–0.19; P<0.01), their perceived influence over their children’s weight (r=0.15; P<0.01) and their concern over their children developing a chronic disease (r=–0.11; P<0.05). These significant variables were included in the final path analyses.
Path analyses: Parental perceptions of their child’s PA and eating habits
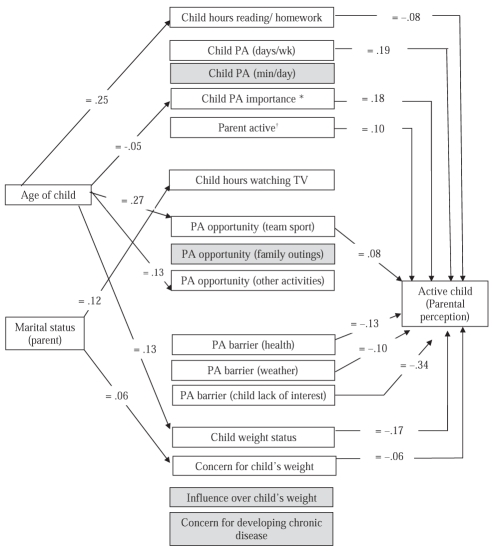
The path diagram (Figure 2) showed that older children’s parents perceived them to engage in more reading/homework and to be more overweight or obese – both of which were associated with a decrease in the perception that their child was active. Parents of younger children believed PA was more important for their child; parents of older children reported that their child participated in more team sports. In both cases, these perceptions were associated with the belief that their child was more active. Single parents were less likely to express concern about their child’s weight and their child’s level of activity. Parents who perceived their child to be more active also considered themselves to be more active, and reported that their child did not experience health issues, weather and/or lack of interest as PA barriers. Among the variables explored in the PA path analyses, the strongest correlation (β=–0.34) was found between a perceived lack of interest on the part of the child and parental perception of child PA. Note that while the age of the child predicted PA opportunities as defined by ‘other activities’ and marital status predicted hours of watching television, neither of these potential mediating variables had a subsequent effect on parental perception of their child’s activity levels, as determined through the path analyses (Figure 2).
Figure 2).
Final path analysis predicting parental perception of their child’s physical activity (PA) levels (variables that were identified in the correlation analyses but that did not have a significant beta-coefficient are in shaded boxes). *Parental preception of the importance of PA for the child; †Parental perception of their own PA level. TV Television; wk Week
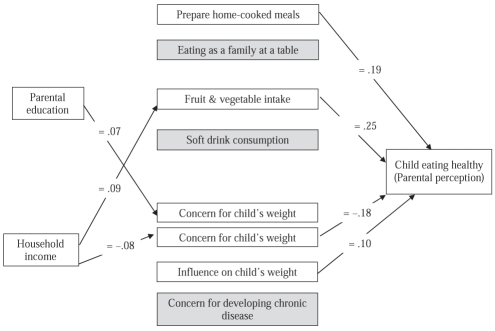
The path analysis for eating habits (Figure 3) showed that parents with higher education levels believed they had greater influence over their child’s weight, which in turn increased their perception that their child was eating healthily. Respondents with higher household incomes believed that their child ate more servings of fruits and vegetables, which was also associated with an increased perception that their child was eating healthily. Conversely, the path analyses indicated that parents from households with lower incomes were more concerned with their child’s weight, which was correlated with a decreased perception that their child was eating healthily. Finally, parents believed that the preparation of home-cooked meals would lead to more positive eating habits, regardless of parental education and/or income.
Figure 3).
Final path diagram predicting parental perception of their child’s eating habits (variables that were identified in the correlation analyses but that did not have a significant beta-coefficient are in shaded boxes)
Perceptions of overweight and obesity, and risk of chronic illness
Table 4 presents information regarding parents’ perceptions of their child’s body weight, risk of chronic disease and self-esteem. Only 0.2% of parents reported their child as being obese, and 8.6% reported their child as being overweight. Parents of female children were more likely to report that their child was ‘about the right weight’ (87%) than parents of male children (79%) (data not presented). Few parents were concerned about their child’s weight, yet 50% of survey respondents reported being concerned about the risk of their child developing a chronic illness. Interestingly, 43% of parents identified media (Internet, television and/or radio) as the most likely place they would acquire the knowledge and skills they needed to promote PA and healthy eating in their family. This was followed by print materials (27.2%), health care professionals (25.2%) and their child’s school (19%). Given that most parents did not identify their child as obese or overweight, path analysis was not used to explore perceptions related to the child’s weight.
TABLE 4.
Respondents’ perception, concern and judgment on child body weight, chronic illness and self-esteem
| Question | Overall, % |
|---|---|
| Do you feel your child is the following: | |
| Underweight | 8.9 |
| About the right weight | 82.3 |
| Overweight | 8.6 |
| Obese | 0.2 |
| How concerned are you about your child’s weight? | |
| Not at all | 58.4 |
| Not very | 15.2 |
| Somewhat | 16.2 |
| Very | 10.1 |
| How do you judge whether your child’s weight is healthy? | |
| Information from doctor/other health care professional | 42.1 |
| Comparison to other children | 11.3 |
| Height/weight | 45.3 |
| Exercise/lack of exercise | 13.4 |
| Diet/overeating/undereating/poor diet | 8.4 |
| Body mass index/growth chart | 9.2 |
| Genetics/family history | 3.1 |
| How much influence do you feel you have over your child’s weight? | |
| Don’t know | 52.0 |
| None at all | 35.1 |
| Very little | 6.7 |
| Some | 4.3 |
| A great deal | 2.0 |
| How concerned are you about the risk of your child developing a chronic illness, such as heart disease or diabetes? | |
| Not at all | 25.3 |
| Not very | 22.4 |
| Somewhat | 28.5 |
| Very | 23.4 |
| Compared with other children the same age, how would you rate your child’s self-esteem? | |
| Poor | 38.9 |
| Fair | 49.1 |
| Good | 9.8 |
| Excellent | 1.8 |
The sum of responses may not always add up to 100%; responses less than 1% may not have been reported. Multiple responses were possible for certain questions
DISCUSSION
To our knowledge, the present study is the largest survey of parent perceptions of child weight, PA and eating behaviours conducted in Canada. Despite consistent reports of inactivity and unhealthy eating habits of Canadian children, including the region surveyed in the present study, most parents in the current study believed that their children were of normal weight, and were physically active and eating healthily. Following the application of a path analysis, we were able to identify beliefs that may underlie these perceptions, and demonstrate that parents do not necessarily apply the same criteria when assessing the health behaviours of their children.
Our data showed that only 8.6% of the parents categorized their child as being overweight, and less than 1% identified their child as being obese. This is in stark contrast to the 26% of children in the Champlain region who are estimated to be overweight or obese (25). This finding is consistent with previous research that showed most parents do not perceive their children as being overweight (20,26–30). Two previous Canadian surveys (31,32) identified the same discrepancy between population levels of childhood obesity and parental perceptions.
Ninety per cent of parents in the present study reported their child to be ‘active’ or ‘very active’, which is consistent with a 2004 Ipsos-Reid survey (32). Despite these perceptions, it is known that more than 50% of Canadian children are not sufficiently active for optimal growth (33), and 90% of Canadian children and youth are not meeting the guidelines set forth in Canada’s Physical Activity Guide for Children and Youth, as determined by direct measures (34). In Canada, a child is deemed sufficiently active if they adhere to the recommendations of the Canadian Physical Activity Guide for Children of 90 min of moderate to vigorous PA per day (35). While approximately 90% of our surveyed population indicated that their child was very active or active, more than 30% reported that their child participated in PA less than five days/week and for less than 60 min/day, suggesting that the parental definition of active is not based on guidelines. Our path analyses further identified that parents’ reported frequency of child activity plays a role in predicting the perception of their child’s PA level but not in minutes/day, suggesting that the overall parental perception of their child’s PA is based on their biased perception of their child’s PA frequency. Parents in our survey reported a high degree of sports participation by their child (72%), in keeping with Canadian Fitness and Lifestyle Research Institute (Ottawa, Ontario) data for children and youth (36). This was identified as a predictor of parental perception of their child’s activity level; however, family outings (eg, hiking, biking, walking) or other recreational or physical activities were not predictive of parental perception.
Inconsistencies were found between what parents viewed to be important factors stimulating or impeding PA and the scientific evidence. Parents appear to attribute physical inactivity to time spent reading or doing homework rather than time spent in front of a screen. Previous studies (37,38) have shown screen time to be inversely associated with children’s PA levels, and positively associated with children being overweight (39–42). Interestingly, parental perception of the time their child spends reading or doing homework was found to negatively affect perception of their child’s PA level, but the same was not true for screen time. The Canadian Paediatric Society (43), Obesity Canada (44) and the American Association of Pediatrics (45) recommend that families reduce screen time and limit daily television watching to less than 1 h/day for preschool children and less than 2 h/day for school-age children. Canada’s Report Card on Physical Activity for Children and Youth (46) specifically noted that Canadian children and youth were not meeting recommended screen time. Although 24.3% of parents in our survey reported their child spent 2 h/day or more in front of a screen, this was not a factor in influencing their perception of their child’s activity level.
While more than 80% of parents polled in our survey believed that their child had ‘very good’ to ‘excellent’ eating habits, this perception is not consistent with National level population data from the Canadian Community Health Survey. The survey identified that 23% of children’s caloric intake was from ‘other food’ not falling into one of the four food groups, and that approximately 70% of children were not meeting the recommended intake for fruit and vegetables (47). This is consistent with our survey findings, in which 25% of parents reported that their child ate less than three servings of fruit and vegetables daily, with only 16% of their children meeting ‘Eating Well with Canada’s Food Guide’ recommendations of six or more fruits or vegetables each day (48). The inconsistencies between parents’ positive perceptions of their child’s healthy eating behaviours and reported fruit and vegetable intake suggest parents are not necessarily using this information when assessing their child’s eating habits. Furthermore, recommendations from health professional organizations and childhood obesity advocate groups not only identify high fruit and vegetable consumption, but eating meals as a family at a table without distractions (eg, television), as well as limiting fast food and nonfruit juice intake as markers of healthy eating habits and obesity protection (49–55). Despite this, more than 50% of parents reported that their child has supper prepared outside the home and/or eats fast foods one or more times each week; nearly 40% reported that their child eats supper in front of the television one or more times per week, and almost 25% of parents reported that their child consumes soft drinks, sports drinks or fruit-flavoured drinks that are not 100% juice four or more times per week. In spite of these variables being deemed important by child obesity advocates and health professionals, our data suggests that these do not appear to be factors considered by parents when they assess the healthfulness of their children’s eating habits. While evidence indicates that the home environment and parental role modelling can have a striking effect on health behaviours and on child weight (14), and that socialization of health-related behaviours occurs within the family, with parents’ beliefs, attitudes and behaviours substantially affecting children’s health behaviours (56), the results of our survey showed that 42% of parents reported little control over their child’s weight and 52% reported not knowing whether they played a role at all. This is a troubling finding given the plethora of scientific literature consistently reporting the integral role of parents either through modelling behaviour or through parental support and encouragement, which are positively correlated with children’s activity level (13,57,58) and healthy eating habits (12,56,59). The results of our survey identify the need for clear messaging surrounding the importance of the parent or caregiver role.
There are limitations to the present study that should be noted. First, the survey response rate was 26.5%. While this response rate is similar to that typically observed for telephone-based surveys, it may result in a biased study sample (60,61). Second, because it was our intent to gather specific information from this population, we created a survey instrument that has not been formally validated. In addition, the study was based on self-report data and, therefore, did not include direct measurement of actual body weight, PA or eating behaviours. Although self-reported height and weight might have been beneficial, recent data illustrating the significant issues with under-reporting of weight and over-reporting of height (62) questions the usefulness of such information. Few parents in our survey reported their child to be overweight or obese, but both national and region-specific statistics indicate that approximately 30% of children are overweight or obese. This discrepancy may be associated with biases in self-report or, alternatively, it is possible that the children of parents surveyed in the Champlain region may have been healthier than the population average. However, there is no information available to suggest that parents of healthier children are more likely than parents of overweight or obese children to respond to telephone-based surveys. We must also note that the demographics of our surveyed population closely match the 2006 Statistics Canada Census data (24) for families in the Champlain region. Finally, it should be noted that path analysis can evaluate causal hypotheses and establish correlations among variables, but it cannot be used to establish causality.
Information gathered from the present study will be used to inform the development of a public relations campaign designed to engage parents of school-age children in the Champlain region of Ontario and to support a regional ‘call to action’ to address healthy active living among Champlain children and youth. The campaign will seek to offer parents solutions on how to increase PA levels and improve eating habits among their children, and to empower parents – as part of a larger community – to take action for improving the activity levels and eating habits of their children, and in doing so, inspire others to follow. Data from the present study suggest health communications messages should address the knowledge gap between parental perceptions of what defines their child’s weight status, PA level and healthy eating behaviours against what is recommended by health organizations and paediatric health advocates. Parents’ perception of their own inability to impact their child’s weight needs to be reconciled. Their pivotal importance as role models of healthy behaviours, and their ability to shape, modify and facilitate their child’s healthy active living habits through practicing healthy behaviours themselves or being strong advocates and supporters of their child’s healthy lifestyle habits, should be considered an important target in future media campaigns. Our survey findings have also proved to be useful in directing the identification of barriers to PA and eating to be addressed at the school level. The “Champlain Declaration: A Call to Action for Physically Active & Healthy Eating Environments in Schools” has been signed by the nine directors of education and four medical officers of health in the Champlain region, formalizing the commitment to work in partnership to create healthy school environments so that school-age children in the Champlain region can be physically active and make healthy food choices at school on a daily basis.
CONCLUSIONS
In the present study, the parents surveyed did not appear to understand/have knowledge of current recommendations for PA and healthy eating behaviours in children. Parents’ knowledge about healthy amounts of PA or appropriate eating behaviours is not consistent with the body of knowledge applied by health professionals.
Acknowledgments
The present survey was conducted as part of the Champlain Healthy School-aged Children Initiative, a priority initiative of the Champlain Cardiovascular Disease Prevention Network (CCPN). The partner organizations who conducted the survey include the Eastern Ontario Health Unit; Ottawa Public Health; Renfrew County & District Public Health; Leeds, Grenville and Lanark District Health Unit; Children’s Hospital of Eastern Ontario Research Institute; Heart & Stroke Foundation of Ontario; the University of Ottawa Heart Institute and the Champlain Local Health Integration Network. The authors thank Dr Chris Blanchard for providing them with expert guidance and for his significant contribution in assisting with performing the path analyses for the manuscript.
REFERENCES
- 1.Reilly JJ, Dorosty AR, Emmett PM. Prevalence of overweight and obesity in British children: Cohort study. BMJ. 1999;319:1039. doi: 10.1136/bmj.319.7216.1039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Strauss RS, Pollack HA. Epidemic increase in childhood overweight, 1986–1998. JAMA. 2001;286:2845–8. doi: 10.1001/jama.286.22.2845. [DOI] [PubMed] [Google Scholar]
- 3.Whitaker RC, Dietz WH. Role of the prenatal environment in the development of obesity. J Pediatr. 1998;132:768–76. doi: 10.1016/s0022-3476(98)70302-6. [DOI] [PubMed] [Google Scholar]
- 4.Zametkin AJ, Zoon CK, Klein HW, Munson S. Psychiatric aspects of child and adolescent obesity: A review of the past 10 years. J Am Acad Child Adolesc Psychiat. 2004;43:134–50. doi: 10.1097/00004583-200402000-00008. [DOI] [PubMed] [Google Scholar]
- 5.Leitch K. Reaching for the Top. A report by the Advisor on Healthy Children and Youth. Ottawa: Minister of Health Canada; 2007. Report No: 4552. [Google Scholar]
- 6.Freedman DS, Khan LK, Dietz WH, Srinivasan SR, Berenson GS. Relationship of childhood obesity to coronary heart disease risk factors in adulthood: The Bogalusa Heart Study. Pediatrics. 2001;108:712–8. doi: 10.1542/peds.108.3.712. [DOI] [PubMed] [Google Scholar]
- 7.Magarey AM, Daniels LA, Boulton TJ, Cockington RA. Predicting obesity in early adulthood from childhood and parental obesity. Int J Obes Relat Metab Disord. 2003;27:505–13. doi: 10.1038/sj.ijo.0802251. [DOI] [PubMed] [Google Scholar]
- 8.Must A. Does overweight in childhood have an impact on adult health? Nutr Rev. 2003;61:139–42. doi: 10.1301/nr.2003.apr.139-142. [DOI] [PubMed] [Google Scholar]
- 9.Austin SB, Melly SJ, Sanchez BN, Patel A, Buka S, Gortmaker SL. Clustering of fast-food restaurants around schools: A novel application of spatial statistics to the study of food environments. Am J Public Health. 2005;95:1575–81. doi: 10.2105/AJPH.2004.056341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Harrison K, Marske AL. Nutritional content of foods advertised during the television programs children watch most. Am J Public Health. 2005;95:1568–74. doi: 10.2105/AJPH.2004.048058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Drewnowski A. Obesity, diets, and social inequalities. Nutr Rev. 2009;67(Suppl 1):S36–S39. doi: 10.1111/j.1753-4887.2009.00157.x. [DOI] [PubMed] [Google Scholar]
- 12.Ventura AK, Birch LL. Does parenting affect children’s eating and weight status? Int J Behav Nutr Phys Act. 2008;5:15. doi: 10.1186/1479-5868-5-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sallis JF, Prochaska JJ, Taylor WC. A review of correlates of physical activity of children and adolescents. Med Sci Sports Exerc. 2000;32:963–75. doi: 10.1097/00005768-200005000-00014. [DOI] [PubMed] [Google Scholar]
- 14.Lindsay AC, Sussner KM, Kim J, Gortmaker S. The role of parents in preventing childhood obesity. Future Child. 2006;16:169–86. doi: 10.1353/foc.2006.0006. [DOI] [PubMed] [Google Scholar]
- 15.Golan M, Weizman A, Apter A, Fainaru M. Parents as the exclusive agents of change in the treatment of childhood obesity. Am J Clin Nutr. 1998;67:1130–5. doi: 10.1093/ajcn/67.6.1130. [DOI] [PubMed] [Google Scholar]
- 16.Golan M, Kaufman V, Shahar DR. Childhood obesity treatment: Targeting parents exclusively v. parents and children. Br J Nutr. 2006;95:1008–15. doi: 10.1079/bjn20061757. [DOI] [PubMed] [Google Scholar]
- 17.Prochaska JO, DiClemente CC, Norcross JC. In search of how people change. Applications to addictive behaviors. Am Psychol. 1992;47:1102–14. doi: 10.1037//0003-066x.47.9.1102. [DOI] [PubMed] [Google Scholar]
- 18.Baughcum AE, Chamberlin LA, Deeks CM, Powers SW, Whitaker RC. Maternal perceptions of overweight preschool children. Pediatrics. 2000;106:1380–6. doi: 10.1542/peds.106.6.1380. [DOI] [PubMed] [Google Scholar]
- 19.Carnell S, Edwards C, Croker H, Boniface D, Wardle J. Parental perceptions of overweight in 3–5 y olds. Int J Obes (Lond) 2005;29:353–5. doi: 10.1038/sj.ijo.0802889. [DOI] [PubMed] [Google Scholar]
- 20.Eckstein KC, Mikhail LM, Ariza AJ, Thomson JS, Millard SC, Binns HJ. Parents’ perceptions of their child’s weight and health. Pediatrics. 2006;117:681–90. doi: 10.1542/peds.2005-0910. [DOI] [PubMed] [Google Scholar]
- 21.Maynard LM, Galuska DA, Blanck HM, Serdula MK. Maternal perceptions of weight status of children. Pediatrics. 2003;111(5 Part 2):1226–31. [PubMed] [Google Scholar]
- 22.Wake M, Salmon L, Waters E, Wright M, Hesketh K. Parent-reported health status of overweight and obese Australian primary school children: A cross-sectional population survey. Int J Obes Relat Metab Disord. 2002;26:717–24. doi: 10.1038/sj.ijo.0801974. [DOI] [PubMed] [Google Scholar]
- 23.Lleras C. Path Analysis. Encyclopedia of Social Measurement. 2005;3:25–30. [Google Scholar]
- 24.Statistics Canada . Champlain Health Integration Network, Ontario. 2006 Community Profiles. 2006 Census. Ottawa: Statistics Canada; 2007. Report No: Statistics Canada Catalogue no. 92-591-XWE. [Google Scholar]
- 25.PCCH Expert Panel for Child and Youth Overweight and Obesity . Ontario: 2008. A Proposed Service Delivery Framework for Healthy Weights for Children and Youth across the Continuum of Care. [Google Scholar]
- 26.West DS, Raczynski JM, Phillips MM, Bursac Z, Heath GC, Montgomery BE. Parental recognition of overweight in school-age children. Obesity (Silver Spring) 2008;16:630–6. doi: 10.1038/oby.2007.108. [DOI] [PubMed] [Google Scholar]
- 27.Akerman A, Williams ME, Meunier J. Perception versus reality: An exploration of children’s measured body mass in relation to caregivers’ estimates. J Health Psychol. 2007;12:871–82. doi: 10.1177/1359105307082449. [DOI] [PubMed] [Google Scholar]
- 28.Hirschler V, Gonzalez C, Talgham S, Jadzinsky M. Do mothers of overweight Argentinean preschool children perceive them as such? Pediatr Diabetes. 2006;7:201–4. doi: 10.1111/j.1399-5448.2006.00183.x. [DOI] [PubMed] [Google Scholar]
- 29.Campbell MW, Williams J, Hampton A, Wake M. Maternal concern and perceptions of overweight in Australian preschool-aged children. Med J Aust. 2006;184:274–7. doi: 10.5694/j.1326-5377.2006.tb00236.x. [DOI] [PubMed] [Google Scholar]
- 30.Jansen W, Brug J. Parents often do not recognize overweight in their child, regardless of their socio-demographic background. Eur J Public Health. 2006;16:645–7. doi: 10.1093/eurpub/ckl100. [DOI] [PubMed] [Google Scholar]
- 31.Dieticians of Canada Speaking of Food and Healthy Living. Children and Healthy Weights: Parents’ Perceptions. 2005.
- 32.Sibbald B. CMA wants national children’s health strategy. CMAJ. 2006;175:567. doi: 10.1503/cmaj.061094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Canadian Pediatric Society, Healthy Active Living Commitee Healthy active living for children and youth. Paediatr Child Health. 2002;7:339–45. [PMC free article] [PubMed] [Google Scholar]
- 34.Canadian Fitness and Lifestyle Institute . Kids CANPLAY! Encouraging kids to be active at home, at school and in their communities. Ottawa: Resources and Services; 2008. [Google Scholar]
- 35.Public Health Agency of Canada, College of Family Physicians of Canada, Candian Pediatric Society, Canadian Society of Exercise Physiology . Canada’s Physical Activity Guide for Children. Ottawa: 2002. [Google Scholar]
- 36.Cameron C, Craig C, Paolin S. Trends from 1999–2004. Ottawa: Canadian Fitness and Lifestyle Research Institute; 2005. Local opportunities for physical activity and sport. [Google Scholar]
- 37.Jackson DM, Djafarian K, Stewart J, Speakman JR. Increased television viewing is associated with elevated body fatness but not with lower total energy expenditure in children. Am J Clin Nutr. 2009;89:1031–6. doi: 10.3945/ajcn.2008.26746. [DOI] [PubMed] [Google Scholar]
- 38.Swinburn B, Shelly A. Effects of TV time and other sedentary pursuits. Int J Obes (Lond) 2008;32(Suppl 7):S132–S136. doi: 10.1038/ijo.2008.249. [DOI] [PubMed] [Google Scholar]
- 39.Laurson KR, Eisenmann JC, Welk GJ, Wickel EE, Gentile DA, Walsh DA. Combined influence of physical activity and screen time recommendations on childhood overweight. J Pediatr. 2008;153:209–14. doi: 10.1016/j.jpeds.2008.02.042. [DOI] [PubMed] [Google Scholar]
- 40.Mark AE, Janssen I. Relationship between screen time and metabolic syndrome in adolescents. J Public Health (Oxf) 2008;30:153–60. doi: 10.1093/pubmed/fdn022. [DOI] [PubMed] [Google Scholar]
- 41.Must A, Bandini LG, Tybor DJ, Phillips SM, Naumova EN, Dietz WH. Activity, inactivity, and screen time in relation to weight and fatness over adolescence in girls. Obesity (Silver Spring) 2007;15:1774–81. doi: 10.1038/oby.2007.211. [DOI] [PubMed] [Google Scholar]
- 42.Olds T, Ridley K, Dollman J. Screenieboppers and extreme screenies: The place of screen time in the time budgets of 10–13 year-old Australian children. Aust N Z J Public Health. 2006;30:137–42. doi: 10.1111/j.1467-842x.2006.tb00106.x. [DOI] [PubMed] [Google Scholar]
- 43.Nieman P. Canadian Pediatric Society Statement: Impact of media on children and youth. Paediatr Child Health. 2003;8:301–6. doi: 10.1093/pch/8.5.301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lau DC, Douketis JD, Morrison KM, Hramiak IM, Sharma AM, Ur E. 2006 Canadian clinical practice guidelines on the management and prevention of obesity in adults and children. CMAJ. 2007;176:S1–S13. doi: 10.1503/cmaj.061409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.American Academy of Pediatrics Children, adolescents, and television. Pediatrics. 2001;107:423–6. doi: 10.1542/peds.107.2.423. [DOI] [PubMed] [Google Scholar]
- 46.Active Healthy Kids Canada . It’s Time to Unplug our Kids. Toronto, Ontario: Active Healthy Kids Canada; 2008. [Google Scholar]
- 47.Garriguet D. Canadians’ Eating Habits. Health Rep. 2007;18:17–32. [PubMed] [Google Scholar]
- 48.Health Canada . Eating Well with Canada’s Food Guide. Ottawa: 2007. [Google Scholar]
- 49.Welsh JA, Cogswell ME, Rogers S, Rockett H, Mei Z, Grummer-Strawn LM. Overweight among low-income preschool children associated with the consumption of sweet drinks: Missouri, 1999–2002. Pediatrics. 2005;115:e223–e229. doi: 10.1542/peds.2004-1148. [DOI] [PubMed] [Google Scholar]
- 50.American Diabetes Association . Childhood overweight evidence analysis project. < www.adaevidencelibrary.com/topiccfm?cat=349724> (Accessed on September 28, 2010). [Google Scholar]
- 51.American Academy of Pediatrics Committee on School Health Soft drinks in schools. Pediatrics. 2004;113(1 Pt 1):152–4. [PubMed] [Google Scholar]
- 52.Rampersaud GC, Bailey LB, Kauwell GP. National survey beverage consumption data for children and adolescents indicate the need to encourage a shift toward more nutritive beverages. J Am Diet Assoc. 2003;103:97–100. doi: 10.1053/jada.2003.50006. [DOI] [PubMed] [Google Scholar]
- 53.Gillman MW, Rifas-Shiman SL, Frazier AL, et al. Family dinner and diet quality among older children and adolescents. Arch Fam Med. 2000;9:235–40. doi: 10.1001/archfami.9.3.235. [DOI] [PubMed] [Google Scholar]
- 54.Neumark-Sztainer D, Hannan PJ, Story M, Croll J, Perry C. Family meal patterns: Associations with sociodemographic characteristics and improved dietary intake among adolescents. J Am Diet Assoc. 2003;103:317–22. doi: 10.1053/jada.2003.50048. [DOI] [PubMed] [Google Scholar]
- 55.Taveras EM, Rifas-Shiman SL, Berkey CS, et al. Family dinner and adolescent overweight. Obes Res. 2005;13:900–6. doi: 10.1038/oby.2005.104. [DOI] [PubMed] [Google Scholar]
- 56.Pearson N, Timperio A, Salmon J, Crawford D, Biddle SJ. Family influences on children’s physical activity and fruit and vegetable consumption. Int J Behav Nutr Phys Act. 2009;6:34. doi: 10.1186/1479-5868-6-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.DiLorenzo TM, Stucky-Ropp RC, Vander Wal JS, Gotham HJ. Determinants of exercise among children. II. A longitudinal analysis. Prev Med. 1998;27:470–7. doi: 10.1006/pmed.1998.0307. [DOI] [PubMed] [Google Scholar]
- 58.Ornelas IJ, Perreira KM, Ayala GX. Parental influences on adolescent physical activity: A longitudinal study. Int J Behav Nutr Phys Act. 2007;4:3. doi: 10.1186/1479-5868-4-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Benton D. Role of parents in the determination of the food preferences of children and the development of obesity. Int J Obes Relat Metab Disord. 2004;28:858–69. doi: 10.1038/sj.ijo.0802532. [DOI] [PubMed] [Google Scholar]
- 60.Kristal AR, White E, Davis JR, et al. Effects of enhanced calling efforts on response rates, estimates of health behavior, and costs in a telephone health survey using random-digit dialing. Public Health Rep. 1993;108:372–9. [PMC free article] [PubMed] [Google Scholar]
- 61.Tortora RD. Response Trends in a national random digit dial survey. Metodološki zvezki. 2004;1:21–32. [Google Scholar]
- 62.Gorber SC, Tremblay M, Moher D, Gorber B. A comparison of direct vs. self-report measures for assessing height, weight and body mass index: A systematic review. Obes Rev. 2007;8:307–26. doi: 10.1111/j.1467-789X.2007.00347.x. [DOI] [PubMed] [Google Scholar]