Abstract
Objective
To determine whether benzodiazepines are associated with an increased risk of hip fracture.
Design
Case-control study.
Participants
All incident cases of hip fracture not related to traffic accidents or cancer in patients over 65 years of age. 245 cases were matched to 817 controls.
Setting
Emergency department of a university hospital.
Main outcome measures
Exposure to benzodiazepines and other potential risk or protective factors or lifestyle items.
Results
The use of benzodiazepines as determined from questionnaires, medical records, or plasma samples at admission to hospital was not associated with an increased risk of hip fracture (odds ratio 0.9, 95% confidence interval 0.5 to 1.5). Hip fracture was, however, associated with the use of two or more benzodiazepines, as determined from questionnaires or medical records but not from plasma samples. Of the individual drugs, only lorazepam was significantly associated with an increased risk of hip fracture (1.8, 1.1 to 3.1).
Conclusion
Except for lorazepam, the presence of benzodiazepines in plasma was not associated with an increased risk of hip fracture. The method used to ascertain exposure could influence the results of case-control studies.
What is already known on this topic
Benzodiazepines increase the risk of elderly people falling in a dose dependent way
Their role in hip fracture remains disputed, with increased risk sometimes attributed to drugs with a longer half life or those used to induce sleep
What this study adds
Benzodiazepines were not associated with hip fracture either as a group or according to half life or to characterisation as hypnotic or anxiolytic
Patients using two or more benzodiazepines may be at higher risk
Patients using lorazepam or certain other benzodiazepines may also be at a higher risk of fracture
Introduction
Hip fracture is common in elderly people, resulting in important morbidity and mortality. Hip fracture is usually due to the combination of an acute event, usually a fall, with a chronic condition, such as osteoporosis. Risks can therefore pertain to falling1 or to a propensity to fracture after a fall.2 Many risk factors for hip fracture have been proposed or recognised, such as increasing age, low body weight, low intake of calcium and dairy products, age at menopause, number of children, osteoporosis, and a personal and family history of fractures.3,4 Associated diseases, handicaps, and drugs could also play a part. The use of certain psychotropic drugs such as tricyclic antidepressants and selective serotonin reuptake inhibitors has been suggested as a risk factor for falling and hip fractures.1,5 The role of benzodiazepines is more disputed: some studies have found an association between benzodiazepines, especially the longer acting ones, and hip fracture3,6,7 and others have not.8,9 Studies have also related hip fracture with dosage of benzodiazepine rather than the half life of the various formulations.10 Some of these discrepancies could be related to difficulties in ascertaining exposure especially in elderly people, in part because of cognitive factors, which may also by themselves be a risk factor for falling and could influence the use of benzodiazepines.11,12 One study found that falls in elderly people were associated with the presence of benzodiazepines in blood, but it did not consider fractures.13 We therefore aimed to determine the association between benzodiazepines and other factors with the risk of hip fracture in elderly people, taking into account cognitive aspects and the status of exposure as ascertained from the presence of benzodiazepines in blood.
Participants and methods
From January 1996 to July 1997 we assessed all patients aged over 65 presenting to the emergency departments of the Pellegrin and Saint André university hospitals in Bordeaux, France, for inclusion in our study. A blood sample was obtained at admission after informed written consent had been obtained. The samples were frozen for later analysis.
Cases were all elderly people admitted to the hospitals with acute hip fracture resulting from a fall that was not associated with cancer, a traffic accident, or aggression. Hip fracture was ascertained from x ray films and orthopaedic consultation.
Controls were elderly people admitted to the same hospitals for acute disease without hip fracture not known to be associated with the use of benzodiazepines, a contraindication, or a disorder of equilibrium. Controls were matched with cases for age (within 5 years), sex, and week of admission. We attempted to match each case with four controls.
Our study was designed to detect a twofold increase in risk with an α risk of 0.05 and a β risk of 0.10 (90% statistical power). Assuming a 20% exposure rate in the control population and a 4 to 1 control to case ratio, this required 300 cases and 1200 controls.
Our study was approved by the regional ethics committee and registered with the National Commission on Computers and Freedom. It was conducted according to good clinical practice and the declaration of Helsinki.
Data retrieval and ascertainment
Questionnaires were administered to cases and controls during an interview with a trained research assistant within a week of admission. Data were also retrieved from medical records; this included telephoning the patients' doctors.
We retrieved data on age, sex, height, weight, body mass index, place of residence, marital status, address (by postal code), hospital, date and time of admission, and date and time of fracture. We also obtained data on a personal and family history of fracture, surgery, associated diseases, age at menopause, number of children, and diet, including the intake of dairy products (milk, yoghurt, cheese, and others), with use assessed from 0 (every day) to 3 (never)). We also considered physical impairments (sight, hearing) and dependency scores. We used the four item activities of daily living test for people living at home14 and Katz's six item activities of daily living score for those living in an institution.15 Additionally, the combined binary threshold scoring of individual items defined the presence or absence of dependence.
We determined exposure to benzodiazepines in three ways: with a structured patient questionnaire during an interview with a research assistant,16 mentioning the brand names of all benzodiazepines marketed in France; by consulting medical records; and by assay of a plasma sample taken at admission for our study or for standard tests. Benzodiazepines in the plasma were identified by using high pressure liquid chromatography with diode array detection (HPLC-DAD, HP 1090, Hewlett-Packard) and quantified by high pressure liquid chromatography with ultraviolet detection. Exposure to benzodiazepines was defined as the use of a benzodiazepine at the time of fracture or admission to hospital or the presence of benzodiazepines in the plasma at admission. The use of other drugs was determined from the questionnaire and medical records but not from plasma samples.
Data analysis
We coded the data, input them into EpiInfo version 6.0, and analysed them with Excel, Systat, and Egret. We performed univariate analyses after a descriptive analysis, followed by multivariate conditional logistic regression with the significant univariate relation (at P<0.1) and then systematically determined the presence of benzodiazepines in plasma. We considered as significant a P value of less than 0.05 or an odds ratio with a 95% confidence interval that did not include 1.
We applied Student's t test for normally distributed continuous variables; the Mann-Whitney U test for non-normally distributed continuous variables; Fisher's exact test for dichotomous variables, or the χ2 test for polychotomous variables; and conditional (matched) logistic regression for univariate and multivariate analysis.
Results
Population
We identified 1136 patients (319 cases, 817 controls). We could find no matched controls for 74 cases: we therefore included 245 cases and 817 matched controls (3.3 controls per case) in our study.
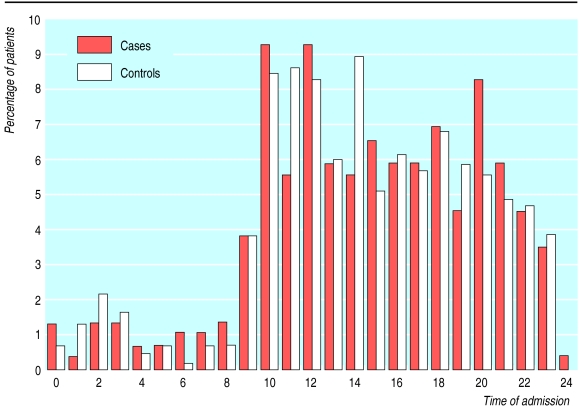
The median delay between fracture and admission to hospital was two hours, and over 65% of cases were admitted within three hours of known time of fracture. The time of admission showed a similar distribution for cases and controls (figure).
Comparisons between cases with or without controls
The greater the age of the patient the more difficult it was to find matched controls. Matching decreased from 100% for patients aged 65 to 70 to 44% for those over 90. Unmatched cases were older (88 (SD 4.7) v 81 (SD 6.8) years, P<0.001) and were more often female (99.6% v 76%, P<0.01) than matched cases. They were not, however, more exposed to benzodiazepines than matched cases, whether exposure was determined from plasma samples (34% v 34%), questionnaire (30% v 24%), or medical records (34% v 33%). Our results are derived from the cases with matched controls.
Non-benzodiazepine risk or protective factors
Although we matched cases and controls to within 5 years, cases were slightly older than controls (81 (6.8) v 79 (7.6) years, P<0.001), and age increased the risk of hip fracture within the matching interval (odds ratio 1.22, 95% confidence interval 1.14 to 1.29). The body mass index was lower in cases than in controls (index above 25: 0.43, 0.27 to 0.70). Cases and controls did not differ in lifestyle or family status; age at menopause; use of hormone replacement therapy; number of children; previous medical, surgical, or obstetric history; family history of fractures; use of alcohol, tobacco, and coffee; or dependency scores for either instrument. A low intake of dairy products was associated with hip fracture (odds ratio per point (scale 0-12 points) less use 1.1, 1.01 to 1.23). Mobility was significantly less in cases who lived in institutions than in their matched controls (71% v 45% normal mobility, P<0.001). The risk of hip fracture was increased with impaired hearing (1.56, 1.04 to 2.34) and deafness (2.42, 1.05 to 5.41). Similar proportions of cases (72%) and controls (70%) were able to complete the questionnaires.
Mean number of non-benzodiazepine drugs used was similar in cases (4.2) and controls (4.1). The use of any diuretic was associated with a lower risk of hip fracture (0.71, 0.52 to 0.96). Tricyclic antidepressants (2.07, 1.12 to 3.82)—but not selective serotonin reuptake inhibitors—and antacids (2.24, 1.16 to 4.33) were associated with an increased risk of fracture.
Use of benzodiazepines
The use of benzodiazepines, whether determined from questionnaires, medical records, or blood samples, was not associated with an increased risk of hip fracture (table 1). Benzodiazepines were used by 34% of cases and 36% of controls, according to the questionnaire. They were mentioned in the medical records of 33% of cases and 29% of controls and were found in the blood samples of 36% of cases and 32% of controls.
Table 1.
Conditional logistic regression analysis for use of benzodiazepines as determined by questionnaire, medical record, or plasma sample in 245 cases of hip fracture and 817 matched controls
| Use of benzodiazepines | Crude odds ratio (95% CI) |
|---|---|
| Questionnaire or medical record | |
| In questionnaire | 1.00 (0.92 to 1.09) |
| In medical record | 1.19 (0.88 to 1.63) |
| One drug (versus 0) | 0.98 (0.72 to 1.34) |
| Two drugs (versus 0) | 2.22 (1.16 to 4.24) |
| Three drugs (versus 0) | 1.06 (0.11 to 10.3) |
| Two or more drugs (versus 0 or 1) | 2.10 (1.14 to 3.87) |
| Short half life drug | 1.06 (0.77 to 1.46) |
| Long half life drug | 1.17 (0.70 to 1.96) |
| Plasma sample | |
| In plasma | 1.06 (0.78 to 1.43) |
| One drug (versus 0) | 0.98 (0.71 to 1.36) |
| Two drugs (versus 0) | 1.52 (0.82 to 2.81) |
| Two or more drugs (versus 0 or 1) | 1.54 (0.83 to 2.80) |
| Short half life drug | 1.10 (0.79 to 1.55) |
| Long half life drug | 0.93 (0.56 to 1.55) |
Duration of half life was not associated with hip fracture. More cases than controls reported using two or more benzodiazepines, compared with none or one (7.4% v 3.7% determined from questionnaires and medical records; 7.4% v 4.3% determined from blood samples). This reported risk was not significant when the data came from blood samples, which showed that even more controls than cases used two benzodiazepines (table 2).
Table 2.
Number of benzodiazepines found in cases (n=245) and controls (n=817). Values are numbers (percentages)
| No of benzodiazepines | Questionnaire and medical records
|
Blood samples
|
|||
|---|---|---|---|---|---|
| Controls | Cases | Controls | Cases | ||
| 0 | 511 (62.6) | 147 (60.2) | 535 (65.5) | 148 (60.4) | |
| 1 | 276 (33.8) | 80 (32.7) | 247 (30.3) | 79 (32.2) | |
| 2 | 27 (3.3) | 17 (6.9) | 35 (4.3) | 17 (6.9) | |
| 3 | 3 (0.4) | 1 (0.4) | 0 | 1 (0.4) | |
Only lorazepam in plasma was significantly associated with hip fractures (1.8, 1.1 to 3.1). Although clobazam, loprazolam, nitrazepam, and temazepam had similarly increased odds ratios, because there were few users of these drugs their larger confidence intervals included 1. The other benzodiazepines were not associated with an increased risk of hip fracture (table 3). Cases were similar to controls in plasma concentration of individual benzodiazepines and of all benzodiazepines (table 4).
Table 3.
Presence of individual benzodiazepines in blood samples
| Exposed as % of total population
|
Odds ratios | |||
|---|---|---|---|---|
| Controls (n=817) | Cases (n=245) | |||
| Alprazolam | 12 (1.5) | 3 (1.2) | 0.8 (0.2 to 2.7) | |
| Bromazepam | 64 (7.8) | 21 (8.6) | 1.02 (0.6 to 1.7) | |
| Chlordiazepoxide | 1 (0.1) | 0 | ||
| Clobazam | 3 (0.4) | 3 (1.2) | 3.1 (0.6 to 15.6) | |
| Clorazepate | 68 (8.3) | 13 (5.3) | 0.6 (0.3 to 1.1) | |
| Clotiazepam | 1 (0.1) | 0 | ||
| Diazepam | 1 (0.1) | 0 | ||
| Flunitrazepam | 12 (1.4) | 5 (2.0) | 1.4 (0.5 to 4.4) | |
| Loflazepate | 0 | 1 (0.4) | ||
| Loprazolam | 3 (0.4) | 4 (1.6) | 2.7 (0.5 to 13.6) | |
| Lorazepam | 44 (5.4) | 25 (10.2) | 1.8 (1.1 to 3.1) | |
| Nitrazepam | 3 (0.4) | 2 (0.8) | 2.2 (0.4 to 13.4) | |
| Oxazepam | 15 (1.8) | 5 (2.0) | 0.7 (0.2 to 2.2) | |
| Prazepam | 1 (0.1) | 1 (0.4) | ||
| Temazepam | 4 (0.5) | 4 (1.6) | 2.7 (0.7 to 10.9) | |
| Triazolam | 0 | 0 | ||
| Zolpidem | 35 (4.3) | 15 (6.1) | 1.3 (0.7 to 2.5) | |
| Zopiclone | 48 (5.9) | 14 (5.7) | 0.7 (0.4 to 1.4) | |
Table 4.
Plasma concentrations of benzodiazepines (μg/ml) with more than five users. Values are means (95% confidence intervals) unless stated otherwise
| Cases | Controls | P value* | ||
|---|---|---|---|---|
| Alprazolam | 10.9 (0.3 to 423.0) | 9.1 (1.2 to 71.3) | 1.00 | |
| Bromazepam | 137.0 (16.2 to 1159.9) | 139.8 (24.9 to 785.0) | 0.63 | |
| Clorazepate | 295.9 (7.3 to 11939.7) | 242.3 (25.9 to 2266.9) | 0.08 | |
| Flunitrazepam | 6.3 (2.0 to 19.4) | 5.7 (0.9 to 34.4) | 0.30 | |
| Lorazepam | 17.3 (4.6 to 64.3) | 16.0 (2.5 to 100.5) | 0.58 | |
| Oxazepam | 56.8 (0.3 to 12771.7) | 144.0 (15.6 to 1330.1) | 0.50 | |
| Zolpidem | 75.2 (10.3 to 546.3) | 60.3 (5.7 to 634.5) | 0.24 | |
| Zopiclone | 40.4 (7.6 to 215.5) | 26.8 (4.4 to 163.3) | 0.23 | |
| All | 66.7 (2.4 to 1823.6) | 78.3 (3.8 to 1625.7) | 0.43 |
Mean values and upper and lower bounds of the 95% confidence intervals computed after logarithmic transformation.
Probability according to Mann-Whitney U test.
Multivariate analysis including the significant risk or protective factors and benzodiazepine in plasma did not change the odds ratios from the univariate analyses. In particular, benzodiazepines in plasma were not associated with an increased risk of hip fracture (0.9, 0.5 to 1.5).
Discussion
Exposure to benzodiazepines does not increase the risk of hip fracture in people aged over 65. This applies to benzodiazepines regardless of half life.
Hip fracture usually results from falls.17 Factors that influence the risk of hip fracture are those that influence the risk of falling (for example, tricyclics, vertigo) and the propensity of bone to break after a fall (for example, bone mineral density or a cushion of fat tissue).1,2,4
Age and other risk factors
Hip fracture seems to be the main cause of admission to hospital in elderly people; we found it difficult to find people aged over 90 admitted to the emergency department for other reasons. Age probably increases both the risk of falling and the consequences of the fall. Most other factors that we found were associated with hip fracture were expected.3 Weight or body mass index are known protectors against hip fracture: poor nutrition influences both weight and bone density, and increased weight is an important factor in bone modelling and strength. Additionally, a good layer of subcutaneous fat protects the bone from fracture.18 The use of fewer dairy products related to less chronic intake of calcium, protein, and vitamin D was also associated with an increased risk of hip fracture.19,20 Decreased mobility protected against hip fracture, presumably by decreasing the risk of falling.21 Sensory handicaps (vision, hearing) were associated with an increased risk of fracture.17,22 Hearing loss may be associated with hip fracture because ossicular demineralisation denotes osteoporosis,23 and it may also be related to repeated orthostatic hypotension, itself a risk factor for falling.24 Additionally, decreased sensory input could lead to a decreased awareness of the environment, although we did not include fractures related to incidents involving vehicles.
We also confirmed a protective effect from diuretics25 and an increased risk from tricyclic antidepressants26,27—but not selective serotonin reuptake inhibitors, unlike two previous studies.5,27 The association of antacids with hip fracture may be related to the large quantities of aluminium they often contain, which interfere with calcium metabolism and make bone more fragile.28
Our findings must, however, remain tentative for two reasons—firstly, the study of the associations (positive or negative) of various drug groups with hip fracture was not the main objective of our study, and, secondly, these could be confounded by the use of hospital controls with possibly a higher exposure to these drugs than the general population.
Benzodiazepines overall
We found no association between the use of benzodiazepines and an increased risk of hip fractures, whether the information on exposure came from questionnaires, medical records, or plasma samples. An increased risk of hip fractures of more than 1.5-fold associated with benzodiazepines seems improbable from the confidence intervals we obtained.
The validity of our result depends on how much our control population is representative of the general population. Much has been said about the choice of controls from the community or hospital,29 including for the study of hip fracture.30 Because the controls were admitted to hospital they were obviously ill and therefore had a higher probability of using drugs, perhaps including benzodiazepines, than a healthy control population. This could reduce the ability to detect an association between benzodiazepines and hip fractures. The prevalence of benzodiazepine use in our control population was around 35%, higher than the 17% found by Kirby et al.31 However, in a representative cohort of people aged over 65 from the same region as our study who were not admitted to hospital,32 the overall use of benzodiazepines was greater than one third of the population33: at the latest ascertainment (A Fourrier, personal communication, 2000) 37% of elderly people living at home and 43% of living in institutions were taking benzodiazepines. These values are even higher than the ones found in our controls. Additionally, we excluded all patients admitted because of diagnosis associated with the use of psychotropic drugs. Finally, the use of community controls would not have been compatible with plasma sampling: to avoid bias related to sampling time we would have had to sample elderly people at home within the same time frame as the cases, including during the night.
Number and type of benzodiazepines
The association between reported use of two or more benzodiazepines and an increased risk of hip fracture became non-significant when we considered only benzodiazepines found in the blood samples. Two or more benzodiazepines were found in blood samples mostly of controls; this could indicate ascertainment bias or recall bias in cases compared with controls. Using objective data from blood samples avoided this bias.
When individual benzodiazepines were considered, however, lorazepam, and also possibly temazepam,6 loprazolam, nitrazepam, and clobazam, were associated with hip fracture. The other benzodiazepines even seemed to have a non-significant protective effect. Although these drugs may be more sedative than others, we found no association with other sedative drugs used as hypnotics such as zolpidem and zopiclone. Half life, dose, or plasma concentrations, did not seem to account for these differences. These findings should remain tentative until a common factor is found between these “at risk” drugs and other benzodiazepines.
We did not confirm the reported associations between hip fracture and longer life benzodiazepines or with greater doses,10 or the association between falls and the presence of benzodiazepines in serum found by Ryynanen et al.13 However, not all falls result in fracture, and the risk factors for fracture and falling could differ or interact: the contrast between the uniformity with which studies found that benzodiazepines dose dependently increased the risk of falling and the many contradictions between studies of hip fracture raise the possibility that benzodiazepines may exert a dual effect. They may on the one hand increase the risk of falling and on the other decrease the risk of fracture when the fall occurs, so that the final association would be a result of the relative influence of both effects. The protective effect could be related to the muscle relaxant property of benzodiazepines: falling while relaxed decreases the risk of injury. In our study only the controls used non-benzodiazepine myorelaxants. We could not find a study of the relative myorelaxant properties of the different benzodiazepines, but this could be an indication for future studies and may explain the apparent differences in risks between different benzodiazepines.
Effects of ascertainment of exposure status
Our study assessed dependency indices and dietary factors, which are usually not included in database studies, and ascertained exposure. Drug exposure is often difficult to confirm, especially in elderly people. Doctors are not always aware of their patients' complete drug regimen, and patients themselves may be unaware of what they take because of cognitive impairment or because they may receive drugs without their knowledge. This is especially true in elderly people and for hypnotic drugs. Therefore we used the presence of benzodiazepine in blood at the time of admission as our main measure of exposure. In this instance where the risk of benzodiazepines is thought to be associated with an immediate increased risk of falling, blood samples provide the best indication of exposure. Our detection method using high performance liquid chromatography with diode array detection is routinely used to identify the use of drugs. Its only drawback could be a relatively low sensitivity, and subtherapeutic blood concentrations may have been missed in certain cases. However, the detection and identification of a drug in a blood sample indicates clear current exposure to that drug. The main difference between our cases and controls was that a larger proportion of controls had two or more benzodiazepines in their blood. This could indicate that ascertainment bias increases apparent multidrug exposure in cases and confirms that hard data on exposure is needed.
Figure.
Time of admission with hip fracture for 245 elderly patients and 817 matched controls
Acknowledgments
We thank the patients and the staff of the emergency department.
Footnotes
Funding: This study was supported by a grant from the Agence du médicament, Paris, and by the department of Pharmacology, Victor Segalen University, Bordeaux, France.
Competing interests: CP now works for SmithKline Beecham Vaccines in Belgium, which has no interest in benzodiazepines. AC now works for the French Social Security as Medical Inspector in Guérande (near Nantes).
References
- 1.Cumming RG. Epidemiology of medication-related falls and fractures in the elderly. Drugs Aging. 1998;12:43–53. doi: 10.2165/00002512-199812010-00005. [DOI] [PubMed] [Google Scholar]
- 2.Jacqmin-Gadda H, Fourrier A, Commenges D, Dartigues JF. Risk factors for fractures in the elderly. Epidemiology. 1998;9:417–423. [PubMed] [Google Scholar]
- 3.Cummings SR, Nevitt MC, Browner WS, Stone K, Fox KM, Ensrud KE, et al. Risk factors for hip fracture in white women. Study of the Osteoporotic Fractures Research Group. N Engl J Med. 1995;332:767–773. doi: 10.1056/NEJM199503233321202. [DOI] [PubMed] [Google Scholar]
- 4.Grisso JA, Kelsey JL, O'Brien LA, Miles CG, Sidney S, Maislin G, et al. Risk factors for hip fracture in men. Hip Fracture Study Group. Am J Epidemiol. 1997;145:786–793. doi: 10.1093/oxfordjournals.aje.a009171. [DOI] [PubMed] [Google Scholar]
- 5.Liu B, Anderson G, Mittmann N, To T, Axcell T, Shear N. Use of selective serotonin-reuptake inhibitors of tricyclic antidepressants and risk of hip fractures in elderly people. Lancet. 1998;351:1303–1307. doi: 10.1016/s0140-6736(97)09528-7. [DOI] [PubMed] [Google Scholar]
- 6.Cumming RG, Klineberg RJ. Psychotropics, thiazide diuretics and hip fractures in the elderly. Med J Aust. 1993;158:414–417. doi: 10.5694/j.1326-5377.1993.tb121839.x. [DOI] [PubMed] [Google Scholar]
- 7.Ray WA, Griffin MR, Downey W. Benzodiazepines of long and short elimination half-life and the risk of hip fracture. JAMA. 1989;262:3303–3307. [PubMed] [Google Scholar]
- 8.Weintraub M, Handy BM. Benzodiazepines and hip fracture: the New York State experience. Clin Pharmacol Ther. 1993;54:252–256. doi: 10.1038/clpt.1993.145. [DOI] [PubMed] [Google Scholar]
- 9.Wysowski DK, Baum C, Ferguson WJ, Lundin F, Ng MJ, Hammerstrom T. Sedative-hypnotic drugs and the risk of hip fracture. J Clin Epidemiol. 1996;49:111–113. doi: 10.1016/0895-4356(95)00057-7. [DOI] [PubMed] [Google Scholar]
- 10.Herings RM, Stricker BH, de Boer A, Bakker A, Sturmans F. Benzodiazepines and the risk of falling leading to femur fractures. Dosage more important than elimination half-life. Arch Intern Med. 1995;155:1801–1807. [PubMed] [Google Scholar]
- 11.Slemenda C. Prevention of hip fractures: risk factor modification. Am J Med. 1997;103:65–73S. doi: 10.1016/s0002-9343(97)90028-0. [DOI] [PubMed] [Google Scholar]
- 12.Franssen EH, Souren LE, Torossian CL, Reisberg B. Equilibrium and limb coordination in mild cognitive impairment and mild Alzheimer's disease. J Am Geriatr Soc. 1999;47:463–469. doi: 10.1111/j.1532-5415.1999.tb07240.x. [DOI] [PubMed] [Google Scholar]
- 13.Ryynanen OP, Kivela SL, Honkanen R, Laippala P, Saano V. Medications and chronic diseases as risk factors for falling injuries in the elderly. Scand J Soc Med. 1993;21:264–271. doi: 10.1177/140349489302100406. [DOI] [PubMed] [Google Scholar]
- 14.Barberger-Gateau P, Commenges D, Gagnon M, Letenneur L, Sauvel C, Dartigues JF. Instrumental activities of daily living as a screening tool for cognitive impairment and dementia in elderly community dwellers. J Am Geriatr Soc. 1992;40:1129–1134. doi: 10.1111/j.1532-5415.1992.tb01802.x. [DOI] [PubMed] [Google Scholar]
- 15.Katz S, Akpom CA. A measure of primary sociobiological functions. Int J Health Serv. 1976;6:493–508. doi: 10.2190/UURL-2RYU-WRYD-EY3K. [DOI] [PubMed] [Google Scholar]
- 16.Moore N, Masson H, Noblet C, Joannidès R. What medicines do patients really take? A comparison of free form vs oriented questionnaires. Post Marketing Surveillance. 1993;7:355–362. [Google Scholar]
- 17.Boonen S, Dequeker J, Pelemans W. Risk factors for falls as a cause of hip fracture in the elderly. Acta Clin Belg. 1993;48:190–194. doi: 10.1080/17843286.1993.11718306. [DOI] [PubMed] [Google Scholar]
- 18.Lauritzen JB, Askegaard V. Protection against hip fractures by energy absorption. Dan Med Bull. 1992;39:91–93. [PubMed] [Google Scholar]
- 19.Brunelli MP, Einhorn TA. Medical management of osteoporosis. Fracture prevention. Clin Orthop. 1998;348:15–21. [PubMed] [Google Scholar]
- 20.Slovik DM. The vitamin D endocrine system, calcium metabolism, and osteoporosis. Spec Top Endocrinol Metab. 1983;5:83–148. [PubMed] [Google Scholar]
- 21.Thapa PB, Brockman KG, Gideon P, Fought RL, Ray WA. Injurious falls in nonambulatory nursing home residents: a comparative study of circumstances, incidence, and risk factors. J Am Geriatr Soc. 1996;44:273–278. doi: 10.1111/j.1532-5415.1996.tb00913.x. [DOI] [PubMed] [Google Scholar]
- 22.Lichtenstein MJ, Griffin MR, Cornell JE, Malcolm E, Ray WA. Risk factors for hip fractures occurring in the hospital. Am J Epidemiol. 1994;140:830–838. doi: 10.1093/oxfordjournals.aje.a117331. [DOI] [PubMed] [Google Scholar]
- 23.Haboubi NY, Hudson PR. Factors associated with Colles' fracture in the elderly. Gerontology. 1991;37:335–338. doi: 10.1159/000213281. [DOI] [PubMed] [Google Scholar]
- 24.Hansen S. Postural hypotension—cochleo-vestibular hypoxia—deafness. Acta Otolaryngol Suppl. 1988;449:165–169. [PubMed] [Google Scholar]
- 25.Jones G, Nguyen T, Sambrook PN, Eisman JA. Thiazide diuretics and fractures: can meta-analysis help? J Bone Miner Res. 1995;10:106–111. doi: 10.1002/jbmr.5650100115. [DOI] [PubMed] [Google Scholar]
- 26.Johansson C, Skoog I. A population-based study on the association between dementia and hip fractures in 85-year olds. Aging (Milano) 1996;8:189–196. doi: 10.1007/BF03339676. [DOI] [PubMed] [Google Scholar]
- 27.Thapa PB, Gideon P, Cost TW, Milam AB, Ray WA. Antidepressants and the risk of falls among nursing home residents. N Engl J Med. 1998;339:875–882. doi: 10.1056/NEJM199809243391303. [DOI] [PubMed] [Google Scholar]
- 28.Cumming RG, Klineberg RJ. Aluminium in antacids and cooking pots and the risk of hip fractures in elderly people. Age Ageing. 1994;23:468–472. doi: 10.1093/ageing/23.6.468. [DOI] [PubMed] [Google Scholar]
- 29.Wacholder S, Silverman DT, McLaughlin JK, Mandel JS. Selection of controls in case-control studies. II. Types of controls. Am J Epidemiol. 1992;135:1029–1041. doi: 10.1093/oxfordjournals.aje.a116397. [DOI] [PubMed] [Google Scholar]
- 30.Moritz DJ, Kelsey JL, Grisso JA. Hospital controls versus community controls: differences in inferences regarding risk factors for hip fracture. Am J Epidemiol. 1997;145:653–660. doi: 10.1093/oxfordjournals.aje.a009163. [DOI] [PubMed] [Google Scholar]
- 31.Kirby M, Denihan A, Bruce I, Radic A, Coakley D, Lawlor BA. Benzodiazepine use among the elderly in the community. Int J Geriatr Psychiatry. 1999;14:280–284. [PubMed] [Google Scholar]
- 32.Dartigues JF, Gagnon M, Barberger-Gateau P, Letenneur L, Commenges D, Sauvel C, et al. The Paquid epidemiological program on brain ageing. Neuroepidemiology. 1992;11(suppl 1):14–18. doi: 10.1159/000110955. [DOI] [PubMed] [Google Scholar]
- 33.Emeriau JP, Fourrier A, Dartigues JF, Begaud B. Drug prescriptions for the elderly. Bull Acad Natl Med. 1998;182:1419–1428. [PubMed] [Google Scholar]