Abstract
Photoactivation and binding of photoactive chemicals to proteins is a known prerequisite for the formation of immunogenic photoantigens and the induction of photoallergy. The intensive use of products and the availability of new chemicals, along with an increasing exposure to sun light contribute to the risk of photosensitizing adverse reactions. Dendritic cells (DC) play a pivotal role in the induction of allergic contact dermatitis. Human peripheral blood monocyte derived dendritic cells (PBMDC) were thus perceived as an obvious choice for the development of a novel in vitro photosensitization assay using the modulation of cell surface protein expression in response to photosensitizing agents. In this new protocol, known chemicals with photosensitizing, allergenic or non-allergenic potential were pre-incubated with PBMDCs prior to UVA irradiation (1 J/cm2). Following a 48 h incubation, the expression of the cell surface molecules CD86, HLA-DR and CD83 was measured by flow cytometry. All tested photosensitizers induced a significant and dose-dependent increase of CD86 expression after irradiation compared to non-irradiated controls. Moreover, the phototoxicity of the chemicals could also be determined. In contrast, (i) CD86 expression was not affected by the chosen irradiation conditions, (ii) increased CD86 expression induced by allergens was independent of irradiation and (iii) no PBMDC activation was observed with the non-allergenic control. The assay proposed here for the evaluation of the photoallergenic potential of chemicals includes the assessment of their allergenic, phototoxic and toxic potential in a single and robust test system and is filling a gap in the in vitro photoallergenicity test battery.
Introduction
Phototoxicity, photoirritancy and photoallergy are topically induced health hazards that can be induced by (simulated) sun light (UV/vis radiation) in the presence of photoreactive agents, generally referred to as “photosensitizers”. The cosmetic and pharmaceutical industries have a particular interest in the identification and evaluation of the photosensitizing potential of new substances before their market launch.
The 7th Amendment to the Cosmetics Directive (Directive 76/768/EEC) aims for the complete replacement of animal testing by 2013. However, due to the public concern regarding the use of animals and the increasing test volume owing to the number of newly developed chemicals the need for innovative in vitro alternatives was recognized well before the acceptance of the amendment. Years ago industrial research groups have developed and validated the 3T3 Neutral Red Uptake (NRU) phototoxicity test [1]. These activities resulted in the acceptance by the EU and the OECD acute phototoxicity test guideline No. 432. This guideline test can be performed on fibroblasts or keratinocytes in order to identify the phototoxic potential of a chemical [2]. As an adjunct test the improved protocol of the Photo-red blood cell (RBC) test can be performed as a more mechanistically oriented test system [3]. Reconstructed three dimensional skin models have also been proposed for further evaluation (unpublished prevalidation data). But to date no accepted alternative is available to identify the photoallergenic potential of a new chemical.
Cutaneous photoallergy is understood as a cell mediated delayed hypersensitivity reaction similar to contact allergy where the hapten is a photosensitizer that requires light energy for its activation into a protein reactive compound that may form so called photoantigens and induce an immune response [4].
Briefly, the absorption of (simulated) sun light (incl. UVA radiation) leads to an excitation of a single electron from its ground state to a higher energy level and to the formation of an unstable intermediate or of reactive photometabolites. The activated photohapten may then form a complete photoantigen through covalent binding to a self protein [5]. This photoantigen may then be captured, processed and the derived photohapten-modified peptides presented by dendritic or Langerhans cells to naive T cells in a draining lymph node. This will eventually induce the production of memory and helper T cells, resulting in an antigen-specific immune response (sensitization) [6], [7]. After a further challenge with the same or a cross-reacting photohapten, the immune system will mount an elicitation reaction whose main clinical symptoms are characterized by eczema, papulovesicles, blisters and pruritus. In rare cases ”photosensitization” may generalize beyond the sun exposed area as a persistent light reaction independent from the photosensitizing material [8], [9].
In contrast to the immunologically mediated reaction induced by photoallergens, phototoxic or photoirritant compounds provoke an acute reaction after the first exposure. Upon light exposure, photoirritants generate singlet oxygen and other reactive oxygen species (ROS) that can lead to harmful oxidation of functional cell components and to tissue damage. Moreover, many photosensitizers can induce both phototoxic and photoallergenic reactions [10].
Dendritic cells (DC) play a pivotal role in the initiation and regulation of immune responses. As professional antigen presenting cells they are specialized in the uptake and processing of antigens thereby triggering the complex biological processes leading to specific T cell activation and maturation. During these processes DCs undergo diverse phenotypical and functional changes such as reduced phagocytic ability, upregulated cell surface expression of co-stimulatory molecules and adhesion proteins, such as CD86, CD83, CD54, CD40, and MHC II antigens. In parallel with a modulation of their chemokine receptor pattern, activated and antigen loaded DCs then migrate from the peripheral tissue to draining local lymph nodes [11].
The measurement of these phenotypical and functional DC modifications was central to the development of several in vitro test protocols for the detection of sensitizers [12], [13], [14]. Different approaches based on peripheral blood monocyte derived DCs (PBMDCs) or DC-like cell lines such as THP-1, U937 and MUTZ-3 are currently being evaluated and/or validated [15].
We have used DCs derived from peripheral blood primary monocytes to develop an in vitro assay for the detection of the photoallergenic potential of chemicals. The modulation of the cell surface molecules CD86, CD83 and HLA-DR was measured after DC exposure to known photoallergenic and phototoxic as well as allergenic and non-allergenic chemicals or to irradiation only. Reproducible and specific results were obtained. Moreover the inter-donor variability of basal CD86 expression was minimal. The test protocol proposed here represents a promising assay for predicting the photoallergenic potential of chemicals including the assessment of their allergenic and toxic/phototoxic potential.
Materials and Methods
Chemicals
Chlorpromazine hydrochloride (CPZ, CAS no. 69-09-0), 6-methylcoumarin (6-MC, CAS no. 92-48-8), musk ambrette (MA, CAS no. 83-66-9), sparfloxacin (SPFX, CAS no. 110871-86-8), ketoprofen (KP, CAS no. 22071-15-4) and olaquindox (OLQ, CAS no. 23696-28-8) were applied as known photoallergenic and phototoxic agents. Nickel sulphate (NI, CAS no. 10101-97-0) and α-hexyl cinnamaldehyde (HCA, CAS no. 101-86-0) were used as known allergens and p-hydroxybenzoic acid (HBA, CAS no. 99-96-7) was chosen as negative control (all purchased from Sigma, Germany). Stock solutions of chemicals were prepared in dimethylsulfoxide or ethanol and further diluted in culture medium immediately before use. The final concentration of dimethylsulfoxide or ethanol never exceeded 0.25%.
Cell culture medium
Culture medium was RPMI 1640 containing 10% heat inactivated (30 min, 56°C) fetal calf serum (FCS Gold, PAA, Austria), 4 mM L-glutamin, penicillin 100 IU/ml, streptomycin 100 µg/ml (all purchased from PAA, Austria).
Generation of peripheral blood monocyte derived dendritic cells (PBMDC)
Peripheral blood mononuclear cells were isolated from buffy coats of healthy donors by ficoll (Lymphocyte Seperation Medium, PAA, Austria) gradient density centrifugation. Buffy coats were randomly and anonymously obtained as residual product from whole blood preservation production. CD1a−/CD14+ monocytes were further enriched by positive depletion using anti-CD14-Ig coupled magnetic microbeads (Miltenyi, Germany). PBMDCs were generated by culture of purified monocytes (1×106/ml) in culture medium supplemented with 100 IU/ml of interleukin-4 (IL-4) and 200 IU/ml of granulocyte–macrophage colony-stimulating factor (GM-CSF) for five days as previously described [16].
Chemical treatment and irradiation of PBMDCs
PBMDCs (7.5×105/ml) were seeded in 24-well plates at day 5 and solutions of test chemicals were added. As a first step, the phototoxicity or cytotoxicity of the chemicals included in the test set was evaluated within a large concentration range limited only by their solubility. The concentration inducing phototoxicity or cytotoxicity around 20% was first determined. The final test range was then defined by choosing a minimum of 4 lower and one higher test concentrations. Irradiation experiments were performed using an UV solar simulator (SOL 500, Dr. Hönle, Germany) equipped with a H1 filter. The H1 filtered spectral output (50% transmission at a wavelength of 335 nm) comprises visible light, UVA and a small amount of UVB (17.3% transmission at 320 nm) and is described elsewhere [1]. The H1 filtered spectrum is later referred to as UV or UVA. The irradiances of UVA light were measured with a calibrated UVA-meter (type No. 37, Dr. Hönle) prior to each experiment. The distance of the UV solar simulator to cell culture plate was 30 cm and irradiation was performed through the cover lid of cell culture plate (Greiner Bio-one, Germany). During the irradiation procedure a ventilator was used to maintain a constant ambient temperature. Chemical treated cells were immediately exposed to simulated sunlight (UVA radiation of 0.5 J/cm2 to 4 J/cm2) or kept in the dark and then incubated for 48 h at 37°C/5% CO2.
Flow cytometry analysis
Treated PBMDCs were harvested at day 7 (48 h after exposure to the test chemicals) and washed with cold phosphate-buffered saline (PBS). Cells were stained with monoclonal fluorochrome-coupled antibodies (mAb) or with isotype-matched control antibodies. The following mAbs were used: Anti-CD86-APC (clone 2331, FUN-1, lot no. 32914), anti-HLA-DR-APC-Cy7 (clone L243, lot no. 41538) and anti-CD83-FITC (clone HB15e, lot no. 15128). All mAbs were purchased from Becton Dickinson, USA. Dead cells were determined and excluded from further analysis by 7-AAD staining.
PBMDCs were incubated for 15 minutes with mAbs and 10 minutes with 7-AAD. 1×104 cells were analyzed for each sample with a FACS Canto II (Becton Dickinson, USA) and the results were processed by FACS DIVA software (Becton Dickinson, USA).
Data analysis and statistics
Changes of surface marker expression after treatment (ΔCD86) were calculated relative to untreated controls according to the following formula:
The relative fluorescence intensity (RFI) of HLA-DR was calculated based on the mean fluorescence intensity (MFI) relative to untreated controls according to the following formula:
For each test compound data obtained on PBMDCs obtained from at least 5 blood donors were analyzed and are presented as mean values with standard deviation (mean ± SD). When indicated in the figure legends, the significance of the difference between the irradiated ΔCD86 values and the corresponding non-irradiated ΔCD86 values (obtained with test concentrations inducing <20% cytotoxicity) was analyzed using Wilcoxon test, and p-values ≤0.05 were considered to be significant.
Results
UV-light sensitivity of PBMDCs
In particular ultraviolet radiation (UVA and UVB) can induce various biological effects including a modulation of the human immune response through phenotypical and functional changes in antigen presenting cells or even functional damage of macrophages, Langerhans or dendritic cells, which can result in an impaired antigen presentation capacity and a suppression of the immune response.
In order to develop an in vitro photosensitization assay, irradiation conditions compatible with the envisaged biological test system should first be determined. The effects of two irradiation schemes (measured UVA intensities of 1.7 and 3.4 mW/cm2) on PBMDCs were first assessed by exposing the cells to a serial of increasing UVA doses.
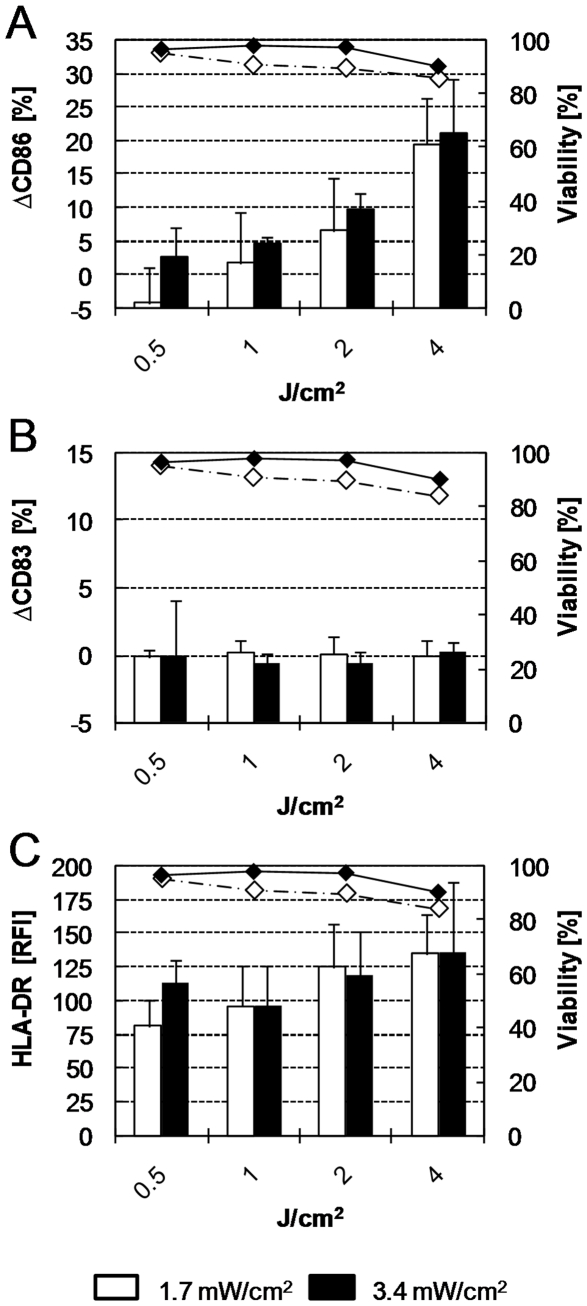
The viability of PBMDCs irradiated with 0.5 to 2 J/cm2 UVA applied with an intensity of 3.4 mW/cm2 was not decreased (Fig. 1A, black diamonds). Slight cytotoxic effects (viability decreasing from 97% to 90.3%) were observed when the irradiation dose was increased to 4 J/cm2. Similar cytotoxic effects were observed when the same radiation doses were applied with an intensity of 1.7 mW/cm2.
Figure 1. Effects of UVA radiation on the expression of CD86, CD83, HLA-DR and viability of PBMDCs.
Cells were exposed to the indicated UVA doses (X axis) with intensities of 1.7 mW/cm2 (open columns) and 3.4 mW/cm2 (black columns). The expression of CD86 (A), CD83 (B), HLA-DR (C) was analyzed by flow cytometry 48 h later. The corresponding cell viability (right Y axis) is indicated for radiation intensities of 1.7 mW/cm2 (open diamonds, dashed line) and 3.4 mW/cm2 (black diamonds, solid line). Mean values ± standard deviation of at least 5 independent donors are indicated. RFI: Relative fluorescence intensity.
The impact of irradiation on the chosen biomarkers (CD86, CD83 and HLA-DR) expression was examined. No relevant increase in CD86 expression could be detected at irradiation doses <1 J/cm2. Higher doses induced a dose-dependent increase in CD86 expression (ΔCD86) up to 20% (Fig. 1A, black columns). On the other hand, the expression of the maturation marker CD83 was not affected under these irradiation conditions (Fig. 1B).
With an irradiation intensity of 1.7 mW/cm2 the HLA-DR expression first decreased (at 0.5 J/cm2) to nearly 75% of the non-irradiated control, and then increased in a dose-dependent manner up to 140% of control (Fig. 1C, white columns). A similar pattern (without initial decrease at 0.5 J/cm2) was observed when a radiation intensity of 3.4 mW/cm2 was used (Fig. 1C, black columns).
The radiation conditions (dose and intensity) to be used in the photosensitization assay should neither induce cytotoxicity nor relevant alterations in cell surface protein expression but still provide enough energy to activate photosensitizers. Our data indicate that a radiation dose of 1 J/cm2 applying an intensity of 3.4 mW/cm2 fulfils the first two conditions. These radiation conditions (1 J/cm2 UVA with 3.4 mW/cm2) were considered as appropriate and used for all further experiments.
Analysis of inter-donor variability of the basal expression level of the chosen biomarkers in non-irradiated and irradiated PBMDCs
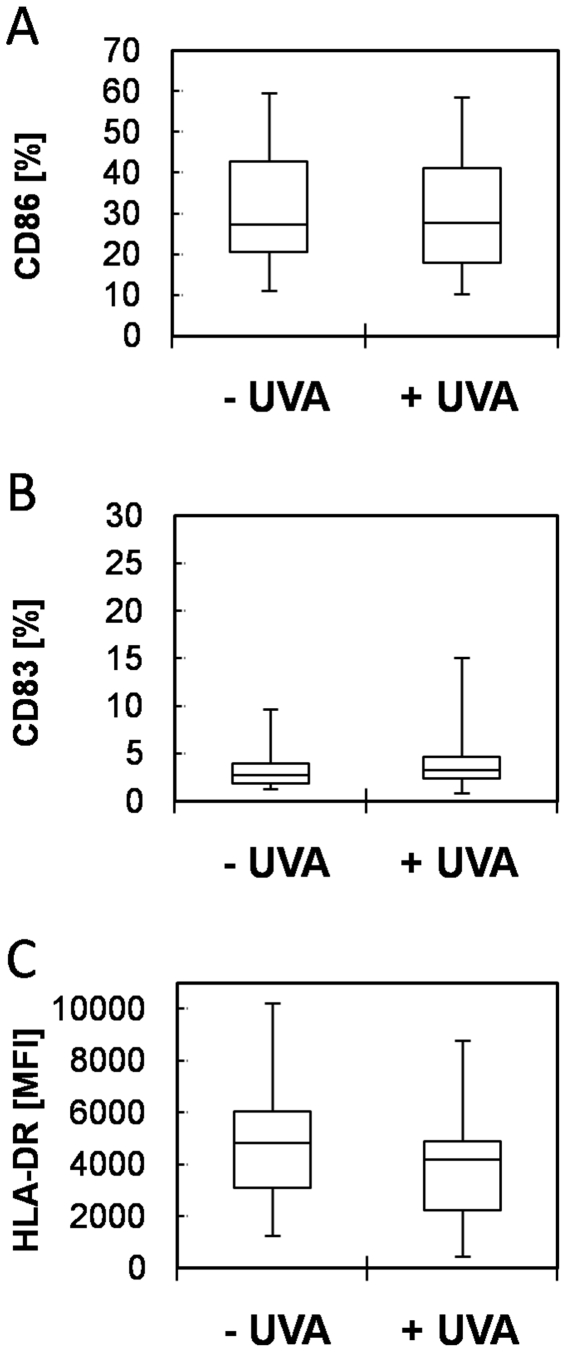
Donor to donor variability in the basal expression of maturation markers by PBMDCs has been reported in previous studies [14], [17] as a critical point. To evaluate the magnitude of that variability, we investigated the basal CD86, CD83 and HLA-DR surface expression in non-irradiated and irradiated PBMDCs obtained from more than 40 different donors. The CD86 expression level of both control and irradiated cells was relatively low (median values below 30%) with a very limited variance (Fig. 2A). These results were confirmed during a second study performed in our laboratory. The analysis of an extensive data pool over multiple projects, extensive time periods and different laboratory personnel revealed a very stable basal expression of CD86 among donors (n = 397) [18]. Moreover, the overall CD83 expression was low (2.75% without irradiation and 3.3% with irradiation) indicating the immature status of the cells and a very limited variability (Fig. 2B). The HLA-DR expression of the same pool of donors was not influenced by UVA irradiation (as compared to controls, see Fig. 2C) but the extent of donor to donor variability was greater than that observed for CD86 and CD83.
Figure 2. CD86, CD83 and HLA-DR expression of PBMCDs irradiated with 1 J/cm2 UVA.
The expression of CD86 (A), CD83 (B), HLA-DR (C) was analyzed by flow cytometry on non-irradiated (- UVA) or irradiated (1 J/cm2 UVA with 3.4 mW/cm2) PBMDCs. Box plots indicate median (horizontal line), 1st, 3rd quartile (box) and maxima/minima-values (T-bars) of at least 40 independent donors. MFI: Mean fluorescence intensity.
Induction of CD86 expression in response to photoallergens after irradiation
To evaluate whether this in vitro photosensitization assay can detect photosensitizing chemicals using the chosen irradiation conditions (1 J/cm2 UVA at 3.4 mW/cm2), the following potential photosensitizers were selected and tested: chlorpromazine (CPZ, psychoactive agent), 6-methylcoumarin (6-MC, fragrance), musk ambrette (MA, fragrance), sparfloxacin (SPFX, antibiotic), ketoprofen (KP, nonsteroidal anti-inflammatory drug), olaquindox (OLQ, antibiotic and feed additive). The non-photoallergenic allergens α-hexylcinnamaldehyde (HCA) and nickel sulphate (NI) as well as the non-allergenic 4-hydroxybenzoic acid (HBA) were used as control substances.
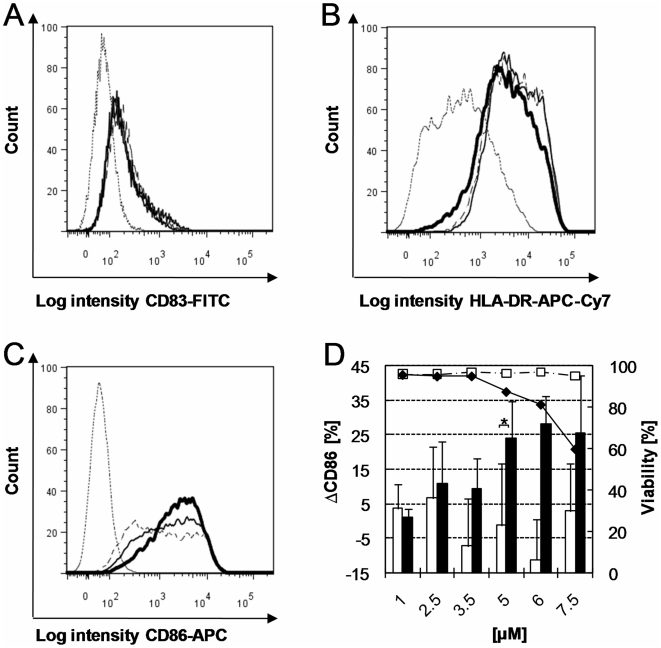
PBMDCs were first exposed to increasing concentrations of CPZ (known photosensitizer with photoallergenic and phototoxic properties) with and without irradiation. CD86, CD83 and HLA-DR surface expression of photosensitizer treated, non-irradiated as well as photosensitizer treated, irradiated cells and controls were compared (Fig. 3). Minor or irrelevant modifications in CD83 expression were observed (CPZ treated, irradiated cells versus irradiated control, Fig. 3A) and only a slight increase in HLA-DR expression was induced by CPZ under irradiation (Fig. 3B). In contrast, a marked increase in CD86 expression was observed under those same conditions (Fig. 3C). CD86 modulation calculated as the difference between the results obtained for the treated sample and the corresponding untreated control (ΔCD86) revealed a dose-effect relationship in response to CPZ after irradiation (Fig. 3D, black columns). Increasing concentrations from 2.5 µM to 5 µM induced a 2.2-fold increase of ΔCD86 (11% to 24%). This represents a very significant increase in CD86 expression compared to the low ΔCD86 values obtained without irradiation at 5 µM. Negative ΔCD86 values were due to biological variability. Moreover CPZ treatment induced dose-related cytotoxic effects with irradiation but had no cytotoxic effect without irradiation.
Figure 3. Expression of CD83, HLA-DR, CD86 and viability of PBMDCs exposed to CPZ and UVA radiation.
Histogram overlays show CD83 (A), HLA-DR (B) and CD86 expression (C) measured by flow cytometry on irradiated (1 J/cm2 with 3.4 mW/cm2) PBMDCs. In each histogram the dotted line and thin dashed line indicate the results obtained with the isotype control or untreated control respectively. The results obtained with PBMDCs exposed to CPZ are indicated by a solid line (2.5 µM) or a heavy solid line (5 µM). D: ΔCD86 measured on PBMDCs exposed to the indicated CPZ concentrations (X axis) with (black columns) or without (open columns) UVA radiation (1 J/cm2 with 3.4 mW/cm2). The viability (right Y axis) of non-irradiated (open squares, dashed line) and irradiated cells (black diamonds, solid line) is also indicated. Mean values for cell viability and mean ± standard deviation for ΔCD86 expression of at least 5 independent donors are shown. Negative ΔCD86 values were due to biological variability. Asterisk indicates significant difference between irradiated and non-irradiated ΔCD86 values (p<0.05, Wilcoxon test).
Since CD86 was markedly upregulated in response to irradiated CPZ (in contrast to CD83 and HLA-DR), it was chosen as the sole marker for the analysis of the following experiments.
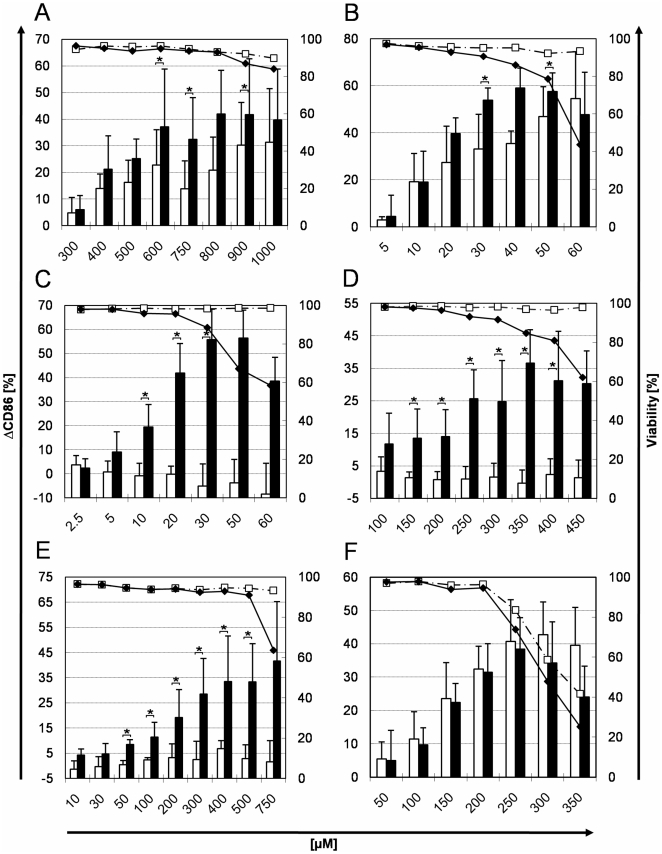
6-MC (responsible for photocontact dermatitis reactions) induced a dose-dependent increase in CD86 expression after irradiation (>40% ΔCD86, Fig. 4A). The difference with the ΔCD86 obtained without irradiation was significant at concentrations >600 µM.
Figure 4. CD86 expression and viability of PBMDCs exposed to photoallergens and allergens with and without irradiation.
PBMDCs were incubated with the indicated (X axis) concentrations of photoallergens and allergens with or without exposure to 1 J/cm2 UVA. The ΔCD86 values (columns) and the cell viability (lines) were measured by flow cytometry without (open columns/squares) or with UVA irradiation (black columns/diamonds) after exposure to the following compounds: A: 6-methylcoumarin. B: musk ambrette. C: sparfloxacin. D: ketoprofen. E: olaquindox. F: α-hexylcinnamaldehyde. Mean values for cell viability and mean ± standard deviation for the ΔCD86 expression values measured on the PBMCDs from at least 5 independent donors are shown. Negative ΔCD86 values were due to biological variability. Asterisk indicates significant difference between irradiated and non-irradiated ΔCD86 values (p<0.05, Wilcoxon test).
6-MC without irradiation induced a ΔCD86 increase >20% compared to the untreated control. No cytotoxic effects were detected within the tested concentration range without irradiation. Under irradiation, a slight cytotoxicity (16%) was detected at the highest test concentration.
MA, a known allergenic and photoallergenic fragrance [19] was tested with PBMDCs isolated from 6 different donors. A dose-related increase in CD86 expression (ΔCD86) was observed with or without irradiation, the increase being nevertheless significantly higher after irradiation (Fig. 4B). ΔCD86 values exceeded 50% at 30 µM whereas cell viability decreased below 80% at 50 µM under irradiation. On the other hand, non-irradiated MA had no cytotoxic effect over the whole tested concentration range.
SPFX, an extreme phototoxic chemical with weak photoallergenic properties [20] induced a significant ΔCD86 increase (Fig. 4C) under irradiation conditions compared to non-irradiated cells. At low concentrations (≤10 µM) it already induced a ΔCD86 level >20% without cytotoxic effect. At higher doses with irradiation, it was relatively cytotoxic (>30% cytotoxicity at 50 µM). In contrast, without irradiation, no relevant cytotoxicity was detected.
Exposure to KP, a photoallergenic nonsteroidal anti-inflammatory drug, induced after irradiation a dose-dependent increase of ΔCD86 >25% without cytotoxic effects up to 300 µM (Fig. 4D, black columns and black diamonds). At high doses (>350 µM), irradiated KP induced phototoxic effects. On the other hand, KP alone (without irradiation) had no relevant effect on the CD86 expression or on the cell viability.
OLQ, a photoallergenic feed additive and antibiotic, induced under radiation conditions a dose-related increase in CD86 expression (ΔCD86) values >30% at concentrations >400 µM (Fig. 4E, black columns) and cytotoxicity was detected at the highest test concentration only (750 µM). In contrast, non-irradiated OLQ treatment resulted in limited CD86 modulation (ΔCD86<10%) and did not influence cell viability.
To determine whether the described photosensitization assay is able to distinguish photosensitizers from allergens and non-allergens, non-photosensitizing allergens (for example HCA and NI) were used as controls. As expected, the fragrance compound HCA induced relevant and analogous increases of CD86 expression with or without irradiation (ΔCD86±UV >30% at 200 µM, see Fig. 4F). The cytotoxic effects were similarly induced at concentrations >200 µM under both conditions.
Likewise, NI induced very similar dose-dependent increases of the CD86 expression with or without irradiation (ΔCD86>55% at 200 µM, see Fig. 5A). The radiation condition had no impact on the relatively weak NI induced cytotoxicity observed at 300 µM.
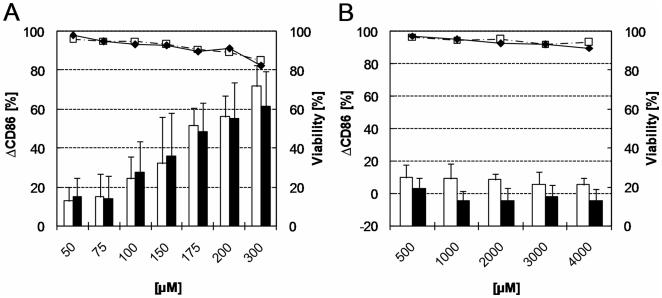
Figure 5. CD86 expression and viability of PBMDCs exposed to nickel sulphate and p-hydroxybenzoic acid.
PBMDCs were incubated with the indicated (X axis) concentrations of nickel sulphate (A) and p-hydroxybenzoic acid (B) with or without exposure to 1 J/cm2 UVA. The ΔCD86 values (columns) and the cell viability (lines) were measured by flow cytometry without (open columns/squares) or with UVA irradiation (black columns/diamonds) after exposure to the test compounds. Mean values for cell viability and mean ± standard deviation for the ΔCD86 values measured on the PBMCDs from at least 5 independent donors are shown. Negative ΔCD86 values were due to biological variability. Asterisk indicates significant difference between irradiated and non-irradiated ΔCD86 values (p<0.05, Wilcoxon test).
HBA, a non-allergenic and non-photoallergenic compound was chosen as negative control. Cell viability and the modulation of CD86 expression (ΔCD86) in response to 500 µM–4 mM HBA with or without irradiation are shown in Fig. 5B. As expected, no relevant modulation of the CD86 expression (ΔCD86<10%) was measured with or without irradiation and no cytotoxic effect was observed up to the highest test concentration (4 mM).
Discussion
The objective of this study was to develop and evaluate an in vitro model for the detection and characterization of the photoallergenic potential of chemicals. The in vitro approach presented here uses the modulation of certain proteins expressed on the surface of PBMDCs exposed to photoallergens with and without irradiation as a readout system.
First, radiation conditions compatible with the envisaged photosensitization assay had to be defined. The applied UVA dose should have no relevant impact on the chosen surface markers (CD86, HLA-DR and CD83) as well as on the viability of the PBMDCs. Initially, the radiation conditions proposed for the 3T3 NRU phototoxicity test [2] were adapted to our system. Dose-dependent increases in CD86 and HLA-DR (but not CD83) expression were observed at radiation doses >1 J/cm2 UVA. A 10–15% cytotoxicity was induced at 4 J/cm2 (UV induced apoptosis, see Timares et al. [21]). This is similar to the results published by Mittelbrunn et al. [22] who reported a partial maturation of PDMDCs and approx. 33% cytotoxicity after irradiation with 5 J/cm2 UVA and 0.4 J/cm2 UVB generated by a xenon solar simulator.
In contrast, a radiation dose of 1 J/cm2 had no effect on the three chosen activation markers or on the PBMDCs viability. These radiation conditions (1 J/cm2 UVA, 3.4 mW/cm2) were considered as appropriate and used for all further experiments.
Donor to donor variability in the basal expression of maturation markers by PBMDCs has been reported as a critical point in previous studies [14], [17], [23], [24] and was often considered as an obstacle to the use of PBMDCs for the development of in vitro sensitization tests and DC-like cell lines were perceived as better alternatives [15]. The magnitude of that variability was investigated by measuring the expression of CD86, CD83 and HLA-DR on non-irradiated and irradiated, immature PBMDCs. Their expression levels were shown to be very similar in cells isolated from a large set of different donors. This limited donor variability was already published by Coutant et al. [25] and has been extensively studied and recently confirmed by our group (n = 397; median CD86 expression 26.7%, 1st quartile 17.7%, 3rd quartile 40.5%) [18]. However, an intrinsic variability of primary cells is to be expected due to the diversity in individual immune responses to allergens in the population. In order to take advantage of this existing but limited variability, we decided to test the photoallergenic potential of a chemical with PBMDCs obtained from a minimum of 5 independent donors.
CPZ, a known photosensitizer with photoallergenic and phototoxic properties, was tested with and without irradiation and the induced modulation of CD86, CD83 and HLA-DR expressions as well as cell viability were measured by flow cytometry and compared 48 h after treatment. Only minor modifications of HLA-DR and CD83 expressions could be detected. In contrast, CD86 measurements revealed a significant dose-effect relationship in response to CPZ after irradiation. Moreover, CPZ treatment induced dose-related cytotoxic effects with irradiation but had no cytotoxic effect without irradiation. CD86 induction was thus perceived as a suitable endpoint for photoallergen detection. This is consistent with the numerous reports indicating CD86 as one of the most promising amongst frequently tested DC activation markers in skin sensitization testing [15].
Further chemicals with documented photoallergenic and phototoxic potentials were used to evaluate the performance of the proposed in vitro photosensitization assay. The ΔCD86 values induced by the photoallergens after irradiation were always more than 15% higher than the corresponding values obtained without irradiation. This difference (15%) between the ΔCD86 values measured with and without irradiation could be used as a putative cut off value for detecting photoallergens. As an alternative, a statistically significant difference between the ΔCD86 values obtained with or without irradiation might be considered. Further tests with an extensive set of chemicals will be necessary to get a robust cut off value.
When testing CPZ it was observed that the induction of CD86 expression appeared at doses close to or overlapping with those inducing cytotoxic effects as a result of both photoallergenic and phototoxic reactivity. In another study, we could demonstrate that the presence of 33% dead cells induced the unspecific upregulation of the CD86 expression [18]. These unspecific cytotoxic effects due to damaged and/or dead cells have to be excluded and we propose that data obtained with test concentrations inducing >20% cytotoxicity should not be considered for the determination of photoallergenicity.
Using our assay, MA a known allergenic and photoallergenic fragrance [19], [26] induced a dose-related increase in CD86 expression with or without irradiation, the increase being significantly higher after irradiation. We could thus classify MA as an allergen and a photoallergen with phototoxic properties. This is consistent with available in vivo data indicating that contact dermatitis to MA can be exacerbated by irradiation [19], [27]. Moreover, the validated 3T3 NRU phototoxicity test also classified MA as phototoxic [28].
The fragrance 6-MC was detected as a potent photoallergen consistent with other in vivo and in vitro data indicating a role of photodimerized 6-MC esters in 6-MC photoallergenicity [29], [30]. Using our protocol, the highest test concentration induced a slight phototoxic effect suggesting a pronounced cytotoxicity at concentrations >1 mM. Though cytotoxicity of irradiated 6-MC was also detected in the THP-1 cell line based in vitro approach described by Hoya et al. [31] and its phototoxicity partially attributed to the formation of singlet oxygen [32], it was concluded that 6-MC is a photoallergen only. Here, non-irradiated 6-MC also resulted in a relevant CD86 induction indicating an allergenic potential consistent with Buehler et al. [33] who considered 6-MC as contact allergen with weak phototoxic potential.
An inverse correlation between phototoxic effects and photoallergenicity was demonstrated for some flouroquinolone antibiotics. For example, SPFX is known as an extreme phototoxic chemical with weak photoallergenic properties [20]. Its weak photoallergenicity is likely outweighed by its strong phototoxicity, e.g. when high concentrations are applied in medical formulations. In our test, irradiated SPFX induced a relevant CD86 modulation already at low concentrations (≤10 µM) without cytotoxic effect, thus indicating a photoallergenic potential. Interestingly, photohaptenic properties were also described by Hino et al. [34] where SPFX treatment of THP-1 cells only resulted in enhanced HLA-DR but not CD86 or CD54 expression.
In recent years, increasing incidences of photoallergic reactions to non-steroidal anti-inflammatory drugs, mainly KP, were reported. Our in vitro test clearly classified KP as a photoallergen and phototoxin consistent with previous in vivo and in vitro studies [35]. KP is also known to elicit contact dermatitis [36]. Since allergenic and photoallergenic concentrations are not necessarily identical, we hypothesized that higher KP concentrations would be required in our assay to reveal KP's allergenic potential (without irradiation) than its photoallergenic potential. Indeed, KP induced a dose-dependent increase of CD86 expression after irradiation whereas without irradiation it had no relevant effect on the CD86 expression or on the cell viability.
Using our test protocol, the photoallergenic feed additive OLQ induced significant and dose-related increases in CD86 expression and cytotoxicity was detected at the highest test concentration. In contrast, non-irradiated OLQ treatment resulted in limited CD86 modulation and did not influence cell viability. Since the ΔCD86 values obtained with or without irradiation showed a difference of more than 30% our results are consistent with the photoallergenic and phototoxic properties deduced from other studies [9], [37].
HCA demonstrated a very similar and dose-dependent CD86 induction with and without irradiation and we thus concluded that HCA has no photoallergenic but an allergenic potential. HCA was classified as a contact sensitizer serving as a positive control in the LLNA and tested in other in vitro sensitizations tests [15], [38]. The cytotoxicity was also similar under both conditions indicating only toxic (but no phototoxic) properties at high concentrations. This result is also consistent with data obtained from a photohaemolysis test [39].
NI induced similar dose-dependent increases of the CD86 expression under both conditions and irradiation had no influence on its relatively weak cytotoxicity. This is the reaction pattern expected for non-photosensitizing allergens such as NI (and HCA) and our in vitro results were in complete agreement with its clinical relevance (induction of allergic contact dermatitis) or its use as a model for metal allergens [40], [41], [42].
HBA was tested as a typical non-allergenic and non-photoallergenic compound. As expected, no relevant modulation of the CD86 expression was detected with or without irradiation and no cytotoxic effect was observed up to the highest test concentration. These results are again in full agreement with already published in vitro tests and LLNA study results [43], [44].
All tested chemicals possessing a photoallergenic potential could be clearly distinguished from allergens. Chemicals with a photoallergenic potential also showed phototoxic effects at higher concentration ranges that could be clearly determined in our in vitro assay. However, it may not be excluded that highly phototoxic drugs are able to induce additional photoallergic reactions since many drugs are able to bind to biomolecules after activation. This consideration is constantly supported by reports describing photoallergic reactions induced by drugs considered as photoirritants. However, the chemical process leading to protein photobinding should be intensively investigated since our present understanding is insufficient for a clear distinction of photoallergens and photoirritants in vitro [45]. In addition photopatch tests do not lead to an unambiguous clinical determination of photoallergic and phototoxic reactions since multiple factors may influence dermal responses to chemicals, e.g. pre-existing skin disorders or cross reactions [46].
Due to the 7th Amendment of the European Cosmetic Directive, the cosmetic industry needs to finalize the development of alternatives to animal tests by 2013. In vitro assays have already been developed for acute phototoxicity testing and the OECD proposes to use the validated 3T3 NRU phototoxicity test which can be performed on fibroblasts or keratinocytes [47]. However, these cell types play different roles in the induction of photoallergy and a DC based assay would represent a critical and major addition to the available test panel.
In summary, this novel in vitro photosensitization assay based on primary PBMDCs yields reproducible and specific results allowing a precise determination of the photosensitizing characteristics of the tested compounds. The described assay represents a promising and robust test system for predicting the photoallergenic potential of chemicals including the assessment of their allergenic and toxic/phototoxic potential and is filling a gap in the in vitro photoallergenicity test battery.
Acknowledgments
We are grateful to Dr. Pierre Aeby for valuable discussions and his critical review of the manuscript.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
Funding: The authors have no support or funding to report.
References
- 1.Spielmann H, Balls M, Dupuis J, Pape WJ, Pechovitch G, et al. The International EU/COLIPA In Vitro Phototoxicity Validation Study: Results of Phase II (Blind Trial). Part 1: The 3T3 NRU Phototoxicity Test. Toxicology in Vitro. 1998;12:305–327. doi: 10.1016/s0887-2333(98)00006-x. [DOI] [PubMed] [Google Scholar]
- 2.OECD . Paris: Organisation for Economic Co-operation and Development; 2004. OECD Guideline for Testing of Chemicals, no. 432: In Vitro 3T3 NRU phototoxicity test. [Google Scholar]
- 3.Pape WJ, Maurer T, Pfannenbecker U, Steiling W. The red blood cell phototoxicity test (photohaemolysis and haemoglobin oxidation): EU/COLIPA validation programme on phototoxicity (phase II). Altern Lab Anim. 2001;29:145–162. doi: 10.1177/026119290102900208. [DOI] [PubMed] [Google Scholar]
- 4.Gould JW, Mercurio MG, Elmets CA. Cutaneous photosensitivity diseases induced by exogenous agents. J Am Acad Dermatol. 1995;33:551–573; quiz 574–556. doi: 10.1016/0190-9622(95)91271-1. [DOI] [PubMed] [Google Scholar]
- 5.Pendlington RU, Barratt MD. Molecular basis of photocontact allergy. Int J Cosmet Sci. 1990;12:91–103. doi: 10.1111/j.1467-2494.1990.tb00524.x. [DOI] [PubMed] [Google Scholar]
- 6.Tokura Y. Immune responses to photohaptens: implications for the mechanisms of photosensitivity to exogenous agents. J Dermatol Sci. 2000;23(Suppl 1):S6–9. doi: 10.1016/s0923-1811(99)00071-7. [DOI] [PubMed] [Google Scholar]
- 7.Goossens A. Photoallergic contact dermatitis. Photodermatol Photoimmunol Photomed. 2004;20:121–125. doi: 10.1111/j.1600-0781.2004.00092.x. [DOI] [PubMed] [Google Scholar]
- 8.Stephens TJ, Bergstresser PR. Fundamental Concepts in Photoimmunology and Photoallergy. Journal of Toxicology: Cutaneous and Ocular Toxicology. 1985;4:193–218. [Google Scholar]
- 9.Schauder S, Schroder W, Geier J. Olaquindox-induced airborne photoallergic contact dermatitis followed by transient or persistent light reactions in 15 pig breeders. Contact Dermatitis. 1996;35:344–354. doi: 10.1111/j.1600-0536.1996.tb02415.x. [DOI] [PubMed] [Google Scholar]
- 10.Mang R, Stege H, Krutmann J. Mechanisms of phototoxic and photoallergic reactions. In: Frosch PJ, Menné T, Lepoittevin J-P, editors. Contact Dermatitis. 4th ed. Heidelberg: Springer Verlag; 2006. pp. 97–103. [Google Scholar]
- 11.Toebak MJ, Gibbs S, Bruynzeel DP, Scheper RJ, Rustemeyer T. Dendritic cells: biology of the skin. Contact Dermatitis. 2009;60:2–20. doi: 10.1111/j.1600-0536.2008.01443.x. [DOI] [PubMed] [Google Scholar]
- 12.Aeby P, Basketter D, Diembeck W, Eschrich D, Gerberick F, et al. Dendritic cell research projects. Altex. 2006;23(Suppl):226–228. [Google Scholar]
- 13.Casati S, Aeby P, Basketter DA, Cavani A, Gennari A, et al. Dendritic cells as a tool for the predictive identification of skin sensitisation hazard. Altern Lab Anim. 2005;33:47–62. doi: 10.1177/026119290503300108. [DOI] [PubMed] [Google Scholar]
- 14.Basketter D, Maxwell G. In vitro approaches to the identification and characterization of skin sensitizers. Cutan Ocul Toxicol. 2007;26:359–373. doi: 10.1080/15569520701622993. [DOI] [PubMed] [Google Scholar]
- 15.dos Santos GG, Reinders J, Ouwehand K, Rustemeyer T, Scheper RJ, et al. Progress on the development of human in vitro dendritic cell based assays for assessment of the sensitizing potential of a compound. Toxicol Appl Pharmacol. 2009;236:372–382. doi: 10.1016/j.taap.2009.02.004. [DOI] [PubMed] [Google Scholar]
- 16.Sallusto F, Lanzavecchia A. Efficient presentation of soluble antigen by cultured human dendritic cells is maintained by granulocyte/macrophage colony-stimulating factor plus interleukin 4 and downregulated by tumor necrosis factor alpha. J Exp Med. 1994;179:1109–1118. doi: 10.1084/jem.179.4.1109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Aiba S, Terunuma A, Manome H, Tagami H. Dendritic cells differently respond to haptens and irritants by their production of cytokines and expression of co-stimulatory molecules. Eur J Immunol. 1997;27:3031–3038. doi: 10.1002/eji.1830271141. [DOI] [PubMed] [Google Scholar]
- 18.Reuter H, Spieker J, Gerlach S, Engels U, Pape W, et al. In vitro detection of contact allergens: Development of an optimized protocol using human peripheral blood monocyte-derived dendritic cells. Toxicol In Vitro. 2010 doi: 10.1016/j.tiv.2010.09.016. [DOI] [PubMed] [Google Scholar]
- 19.Kroon S. Musk Ambrette, a new cosmetic sensitizer and photo sensitizer. Contact Dermatitis. 1979;5:337–338. doi: 10.1111/j.1600-0536.1979.tb04896.x. [DOI] [PubMed] [Google Scholar]
- 20.Tokura Y, Nishijima T, Yagi H, Furukawa F, Takigawa M. Photohaptenic properties of fluoroquinolones. Photochem Photobiol. 1996;64:838–844. doi: 10.1111/j.1751-1097.1996.tb01844.x. [DOI] [PubMed] [Google Scholar]
- 21.Timares L, Katiyar SK, Elmets CA. DNA damage, apoptosis and langerhans cells–Activators of UV-induced immune tolerance. Photochem Photobiol. 2008;84:422–436. doi: 10.1111/j.1751-1097.2007.00284.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mittelbrunn M, Tejedor R, de la Fuente H, Garcia-Lopez MA, Ursa A, et al. Solar-simulated ultraviolet radiation induces abnormal maturation and defective chemotaxis of dendritic cells. J Invest Dermatol. 2005;125:334–342. doi: 10.1111/j.0022-202X.2005.23824.x. [DOI] [PubMed] [Google Scholar]
- 23.Ryan CA, Hulette BC, Gerberick GF. Approaches for the development of cell-based in vitro methods for contact sensitization. Toxicol In Vitro. 2001;15:43–55. doi: 10.1016/s0887-2333(00)00059-x. [DOI] [PubMed] [Google Scholar]
- 24.Tuschl H, Kovac R, Weber E. The expression of surface markers on dendritic cells as indicators for the sensitizing potential of chemicals. Toxicol In Vitro. 2000;14:541–549. doi: 10.1016/s0887-2333(00)00051-5. [DOI] [PubMed] [Google Scholar]
- 25.Coutant KD, de Fraissinette AB, Cordier A, Ulrich P. Modulation of the activity of human monocyte-derived dendritic cells by chemical haptens, a metal allergen, and a staphylococcal superantigen. Toxicol Sci. 1999;52:189–198. doi: 10.1093/toxsci/52.2.189. [DOI] [PubMed] [Google Scholar]
- 26.Gerberick GF, Ryan CA. A predictive mouse ear-swelling model for investigating topical photoallergy. Food Chem Toxicol. 1990;28:361–368. doi: 10.1016/0278-6915(90)90110-9. [DOI] [PubMed] [Google Scholar]
- 27.Wojnarowska F, Calnan CD. Contact and photocontact allergy to musk ambrette. Br J Dermatol. 1986;114:667–675. doi: 10.1111/j.1365-2133.1986.tb04874.x. [DOI] [PubMed] [Google Scholar]
- 28.Spielmann H, Liebsch M, Pape WJ, Balls M, Dupuis J, et al. EEC/COLIPA in vitro photoirritancy program: results of the first stage of validation. Curr Probl Dermatol. 1995;23:256–264. doi: 10.1159/000424321. [DOI] [PubMed] [Google Scholar]
- 29.DeLeo VA, Suarez SM, Maso MJ. Photoallergic contact dermatitis. Results of photopatch testing in New York, 1985 to 1990. Arch Dermatol. 1992;128:1513–1518. doi: 10.1001/archderm.128.11.1513. [DOI] [PubMed] [Google Scholar]
- 30.Kato S, Seki T, Katsumura Y, Kobayashi T, Komatsu K, et al. Mechanism for 6-methylcoumarin photoallergenicity. Toxicol Appl Pharmacol. 1985;81:295–301. doi: 10.1016/0041-008x(85)90166-8. [DOI] [PubMed] [Google Scholar]
- 31.Hoya M, Hirota M, Suzuki M, Hagino S, Itagaki H, et al. Development of an in vitro photosensitization assay using human monocyte-derived cells. Toxicol In Vitro. 2009;23:911–918. doi: 10.1016/j.tiv.2009.03.010. [DOI] [PubMed] [Google Scholar]
- 32.Allen SK, Todd A, Allen JM. Photochemical formation of singlet molecular oxygen ((1)O2) in illuminated 6-methylcoumarin solutions. Biochem Biophys Res Commun. 1997;235:615–618. doi: 10.1006/bbrc.1997.6848. [DOI] [PubMed] [Google Scholar]
- 33.Buehler EV, Newmann EA, Parker RD. Use of the occlusive patch to evaluate the photosensitive properties of chemicals in guinea-pigs. Food Chem Toxicol. 1985;23:689–694. doi: 10.1016/0278-6915(85)90158-9. [DOI] [PubMed] [Google Scholar]
- 34.Hino R, Orimo H, Kabashima K, Atarashi K, Nakanishi M, et al. Evaluation of photoallergic potential of chemicals using THP-1 cells. J Dermatol Sci. 2008;52:140–143. doi: 10.1016/j.jdermsci.2008.06.002. [DOI] [PubMed] [Google Scholar]
- 35.Bosca F, Miranda MA. Photosensitizing drugs containing the benzophenone chromophore. J Photochem Photobiol B. 1998;43:1–26. doi: 10.1016/s1011-1344(98)00062-1. [DOI] [PubMed] [Google Scholar]
- 36.Diaz RL, Gardeazabal J, Manrique P, Raton JA, Urrutia I, et al. Greater allergenicity of topical ketoprofen in contact dermatitis confirmed by use. Contact Dermatitis. 2006;54:239–243. doi: 10.1111/j.0105-1873.2006.00797.x. [DOI] [PubMed] [Google Scholar]
- 37.Neumann NJ, Blotz A, Wasinska-Kempka G, Rosenbruch M, Lehmann P, et al. Evaluation of phototoxic and photoallergic potentials of 13 compounds by different in vitro and in vivo methods. J Photochem Photobiol B. 2005;79:25–34. doi: 10.1016/j.jphotobiol.2004.11.014. [DOI] [PubMed] [Google Scholar]
- 38.Dearman RJ, Wright ZM, Basketter DA, Ryan CA, Gerberick GF, et al. The suitability of hexyl cinnamic aldehyde as a calibrant for the murine local lymph node assay. Contact Dermatitis. 2001;44:357–361. doi: 10.1034/j.1600-0536.2001.044006357.x. [DOI] [PubMed] [Google Scholar]
- 39.Placzek M, Fromel W, Eberlein B, Gilbertz KP, Przybilla B. Evaluation of phototoxic properties of fragrances. Acta Derm Venereol. 2007;87:312–316. doi: 10.2340/00015555-0251. [DOI] [PubMed] [Google Scholar]
- 40.Rustemeyer T, von Blomberg BM, van Hoogstraten IM, Bruynzeel DP, Scheper RJ. Analysis of effector and regulatory immune reactivity to nickel. Clin Exp Allergy. 2004;34:1458–1466. doi: 10.1111/j.1365-2222.2004.02045.x. [DOI] [PubMed] [Google Scholar]
- 41.Schnuch A, Geier J, Lessmann H, Uter W. [Decrease in nickel sensitization in young patients–successful intervention through nickel exposure regulation? Results of IVDK, 1992-2001]. Hautarzt. 2003;54:626–632. doi: 10.1007/s00105-003-0510-9. [DOI] [PubMed] [Google Scholar]
- 42.Forte G, Petrucci F, Bocca B. Metal allergens of growing significance: epidemiology, immunotoxicology, strategies for testing and prevention. Inflamm Allergy Drug Targets. 2008;7:145–162. doi: 10.2174/187152808785748146. [DOI] [PubMed] [Google Scholar]
- 43.Sakaguchi H, Ashikaga T, Miyazawa M, Kosaka N, Ito Y, et al. The relationship between CD86/CD54 expression and THP-1 cell viability in an in vitro skin sensitization test–human cell line activation test (h-CLAT). Cell Biol Toxicol. 2009;25:109–126. doi: 10.1007/s10565-008-9059-9. [DOI] [PubMed] [Google Scholar]
- 44.Scholes EW, Basketter DA, Sarll AE, Kimber I, Evans CD, et al. The local lymph node assay: results of a final inter-laboratory validation under field conditions. J Appl Toxicol. 1992;12:217–222. doi: 10.1002/jat.2550120312. [DOI] [PubMed] [Google Scholar]
- 45.Lovell WW, Jones PA. Evaluation of mechanistic in vitro tests for the discrimination of photoallergic and photoirritant potential. Altern Lab Anim. 2000;28:707–724. doi: 10.1177/026119290002800506. [DOI] [PubMed] [Google Scholar]
- 46.Palmer RA, White IR. Photopatch testing. In: Frosch PJ, Menné T, Lepoittevin J-P, editors. Contact Dermatitis. 4th ed. Heidelberg: Springer Verlag; 2006. pp. 433–439. [Google Scholar]
- 47.Spielmann H, Muller L, Averbeck D, Balls M, Brendler-Schwaab S, et al. The second ECVAM workshop on phototoxicity testing. The report and recommendations of ECVAM workshop 42. Altern Lab Anim. 2000;28:777–814. doi: 10.1177/026119290002800603. [DOI] [PubMed] [Google Scholar]