Abstract
Background
Twin data permit decomposition of comorbidity into genetically and environmentally derived correlations. No previous twin study includes all major forms of anxiety disorder.
Aims
To estimate the degree to which genetic and environmental risk factors are shared rather than unique to dimensionally scored panic disorder, generalised anxiety disorder, phobias, obsessive–compulsive disorder and post-traumatic stress disorder.
Method
Data obtained from 2801 young-adult Norwegian twins by means of the Composite International Diagnostic Interview were analysed with the Mx program.
Results
A multivariate common factor model fitted best. The latent liability to all anxiety disorders was substantially more heritable (54%) than the individual disorders (23% to 40%). Most of the genetic effect was common to the disorders. Genes contributed just over 50% to the covariance between liabilities.
Conclusions
The five anxiety disorders all share genetic and environmental risk factors. This has implications for the revision of the anxiety disorder section in DSM–V.
Prior twin studies have consistently shown that genetic risk factors contribute substantially to the aetiology of the five individual anxiety disorders: panic disorder, generalised anxiety disorder (GAD), phobias, obsessive–compulsive disorder (OCD) and post-traumatic stress disorder (PTSD).1–8 As expected given the sharing of symptoms of anxiety across these disorders, epidemiological studies have consistently shown substantial levels of comorbidity.3,4,9–15 It is therefore of considerable interest to understand the sources of this comorbidity. In particular, to what degree does it result from genetic v. environmental risk factors common to all the anxiety disorders? Although many twin studies have examined the relationship between anxiety disorders and other disorders, for example GAD and major depression,13–15 only two have examined solely anxiety disorders.3,4 Neither study, however, included all five forms of anxiety disorder: one examined panic disorder, GAD and PTSD,3 whereas the other examined panic disorder, GAD and four subtypes of phobia.4 Our study examines the structure of the genetic and environmental risk factors for all the anxiety disorders assessed in an epidemiological sample of young-adult Norwegian twins.
Method
Sample
Twins were ascertained for this study from the Norwegian Institute of Public Health Twin Panel (NIPHTP), established in 1992. The twins were identified through the Medical Birth Registry, established 1 January 1967, which receives mandatory notification of all births in Norway. The first NIPHTP questionnaire study was conducted in 1992. A follow-up study of all Norwegian twins born 1967–79 was conducted in 1998. Altogether, 12 700 twins received the second questionnaire, and 8045 (63%) responded after one reminder. The sample included 3334 complete pairs (53%). The NIPHTP is described in detail elsewhere.16
As an extension of the 1998 questionnaire study an interview study of Axis I and Axis II mental health disorders – Mental Health in Twins (MHT) – was started in 1999. All complete pairs from the questionnaire study in which both twins had agreed to further contact (3153 pairs) were invited. An additional 68 pairs were drawn directly from the NIPHTP sample. Altogether, 1391 pairs (43%) and 19 single twins were interviewed. There were valid anxiety data for 1385 pairs – 219 male monozygotic (MZ), 117 male dizygotic (DZ), 446 female MZ, 264 female DZ and 339 opposite-gender DZ – and for 21 single twins. Age when interviewed was 19–36 years, mean 28.1 years. Among non-participants was a small percentage of twin pairs in which one or both twins could not be traced, and an unknown proportion for whom migration, illness or other circumstances made participation impossible. Informed consent was obtained from all participants after complete description of the study. Zygosity was determined by molecular methods based on the genotyping of 24 microsatellite markers in all but 385 pairs, for whom zygosity was determined from questionnaire information. The estimated misclassification rate in the entire sample, based on comparison between questionnaire information and the results of DNA analysis, was 0.7%.
Measures
Axis I disorders according to DSM–IV were assessed using a computerised version of the Composite International Diagnostic Interview (CIDI).17,18 The interviews took place between June 1999 and May 2004 and were conducted face to face except for 231 telephone interviews (8.3%). The majority of the 28 interviewers were psychology students in their final training or experienced psychiatric nurses. All received a standardised training programme by teachers certified by the World Health Organization and passed a user licence test for the CIDI. They were supervised during the data collection period. Each twin in a pair was interviewed by different interviewers masked to the results of the co-twin.
For the five lifetime anxiety disorders (including subthreshold scores) here examined (panic disorder, GAD, phobias, OCD and PTSD), DSM–IV diagnoses were assigned without hierarchical rules. Preliminary analyses indicated that the prevalence rates for the full diagnostic categories for four of the diagnoses (panic disorder, GAD, OCD and PTSD) were not high enough to produce stable estimates for twin modelling with our sample size. Moreover, the limited prevalence rates required the collapsing of agoraphobia, social phobia and the other forms of phobias. Using empirically validated methods, detailed below, we therefore defined subthreshold diagnostic groups. Full anxiety disorders were scored ‘2’, subthreshold anxiety disorders were scored ‘1’ and the remainder of the sample was scored ‘0’.
Criteria for defining subthreshold cases
The process of generating subthreshold data took place in two steps. Initially we used only data from the CIDI interview as criteria. However, preliminary standard error of the mean (s.e.m.) testing showed that not even a careful relaxation based on the single CIDI items gave sufficiently high subthreshold prevalences for three of the variables to arrive at stable analytic solutions. As a second step it was therefore decided to extend the subthreshold groups using available questionnaire data as criteria as well.
CIDI-based criteria
Several possible combinations of endorsed interview items, judged to reflect the essential symptoms of the disorder but representing a lower symptom level than the full diagnosis, were tried for all of the disorders except phobias. As a crude empirical tool for selecting some of these combinations we used mental health scores from a questionnaire. A study from 1998 of the twins later invited to participate in the study reported here, included a five-item abbreviated version of the global Symptom Checklist SCL–25. This short version (SCL–5) has been shown to correlate at 0.92 with the original instrument,19 and correlates substantially with all the CIDI-based anxiety disorders.
A number of alternative combinations of subthreshold criteria were tested for each of the disorders, comparing mean SCL–5 scores between the groups of cases meeting the various sets of criteria. Comparisons of SCL–5 scores were also made between cases with a full diagnosis, groups with symptoms meeting the various subthreshold definitions, and the remaining sample. As a precondition for a set of subthreshold criteria to be chosen, the cases meeting these criteria were required to have mean SCL–5 scores lower than those from the full diagnosis group and higher than those from the remaining sample. More than one combination of subthreshold criteria was sometimes chosen for the same disorder; for instance, alternative relaxations would be either a reduction of the required number of symptoms or a reduction of the required duration of the period experiencing these symptoms. The degree of relaxation for the various alternatives was balanced by comparing the SCL–5 mean scores for the groups of participants meeting each of the alternative criteria. The set of CIDI-based subthreshold criteria, initially selected according to clinical judgement and empirically shown to be associated with poor general mental health, is given in the Appendix.
No subthreshold group was defined for phobias, which were highly prevalent. However, like the other disorders, phobia was trichotomised. Mean SCL–5 scores were much lower for participants with phobias (0.39 higher than healthy participants) than for participants with any other anxiety disorder (1.10 s.d. higher than healthy participants). Participants with two or more phobic disorders scored 0.72 s.d. higher. These results imply that most people with a single phobia are not severely mentally ill. Thus, rather than relaxing the criteria for the already prevalent phobia scores, the criterion for the top phobia score (2) was restricted to ‘two or more types of phobia diagnoses’. A single phobia diagnosis was scored 1. The mean SCL–5 score of subthreshold scorers for any anxiety disorder diagnosis or people with one full phobia disorder was 0.45 s.d. higher than that of healthy participants.
Extending the subthreshold groups using questionnaire items
Included in the 1998 questionnaire were questions about symptoms of panic disorder and OCD, enquiring both about the situation at the time of the study and about symptoms earlier in life, and seven items tapping GAD-related symptoms. Logistic regression analysis was used to select combinations of questionnaire items that best predicted the full CIDI-based panic disorder and OCD diagnoses. For panic disorder the single item ‘Can suddenly get extremely afraid or panic without a reason’, endorsed for either ‘now’ or ‘earlier in life’, was found to best predict a panic disorder diagnosis. The tetrachoric correlation between this questionnaire score and a full DSM panic disorder diagnosis was 0.68. The frequency of participants reporting panic-like spells, now or earlier in life, was 6.5%.
From three items made to tap OCD symptoms, the combination of two items, ‘I check and inspect too often, for instance electric burners and locked doors’ (‘now’) and ‘I’m often bothered by “stupid” ideas, which keep coming back' (‘now’ or ‘earlier’), best predicted OCD diagnosis. The tetrachoric correlation between having endorsed both these items and OCD diagnosis was 0.46. The frequency of positive questionnaire scores was 6.1%.
Linear regression analysis was used to select questionnaire items that best predicted GAD, scored as an ordinal variable. A sum of seven items, weighted according to the result from the regression analysis, was computed. The items from SCL–5 were [Have, during the past 14 days, been bothered by] ‘feeling fearful’, ‘feeling tense or keyed up’ and ‘worrying too much about things’. Other questionnaire items were: ‘How often, during the past month, have you used sedatives/tranquillisers?’ ‘Have you, during the last month, been bothered by nervousness (irritable, agitated, tense or restless)?’ ‘Do you on the whole feel energetic and fit or tired and worn out?’ ‘Have you, during the past month, had problems with sleeping in or other sleep problems?’ The upper 7.5% were scored as subthreshold GAD if not already having a GAD diagnosis. The tetrachoric correlation between this dichotomised questionnaire-based indicator and GAD diagnosis was 0.56. The correlation between this indicator and the other full anxiety disorders varied from 0.34 to 0.51.
No questionnaire data were available to predict PTSD.
Statistical analysis
The phenotypic correlation structure was examined using confirmatory factor analysis. First, we tested whether the structure could be explained by a single factor. Then possible gender differences were explored by constraining the anxiety disorder factor loadings to be equal in men and women. Finally, we explored whether adding subthreshold cases might have changed the multivariate structure of the disorders by comparing results using trichotomous (including subthreshold scores) and dichotomous (full or no diagnosis) data. Model fit is assessed by the root mean squared error of approximation (RMSEA) where good-fitting models have a value under 0.05.20
Our twin modelling assumed that liability to illness is continuous and normally distributed in the population, with individuals who exceed a first theoretical threshold expressing a subsyndromal form, and those who exceed a higher threshold expressing the full disorder. Resemblance in twin pairs is assessed using a polychoric correlation.21 Using the multiple threshold model in the PRELIS program,22 we tested for deviations from an underlying bivariate normal distribution of the ordinal three-category data. This test was used for examining whether the subthreshold and fully syndromal cases reflect quantitatively different levels of liability on the same underlying dimension.
Individual differences in liability are assumed to arise from three sources: additive genetic ‘A’, from genes whose allelic effects combine additively; common environment ‘C’, which includes all sources similarly influencing both twins; and specific environment ‘E’, which includes environmental experiences not shared by co-twins and measurement error. Monozygotic co-twin similarity is due to identical genes, A, and, by definition, common environment, C. Dizygotic pairs share (on average) half of their A and all of their C.
Univariate twin studies use data on co-twin similarity for a single trait or illness. Multivariate studies use observed similarity between the same trait in co-twins, between one trait in one twin and another trait in the co-twin, and between the various traits observed within individuals. Besides yielding estimates of A, C and E for individual disorders, multivariate analyses estimate the extent to which variation in comorbid disorders results from the same genetic or environmental factors v. genetic and environmental factors specific to each disorder.
We used single-factor multivariate models because these served our purpose of dividing genetic and environmental variance into that shared between anxiety disorders and that specific to each disorder. We tested two forms of this model: an independent pathway and a common pathway model.23 The latter is nested under the former and differs in that all common variance, genetic and environmental, is assumed to be mediated through one single latent phenotype. The best-fitting of these two models was chosen using Akaike's information criterion (AIC).24
Ideally, quantitative and qualitative gender-specific effects would be tested as part of our multivariate modelling. This was not feasible with these data because multivariate analyses are especially vulnerable to the combination of low prevalences and modest sample size (especially in our male DZ pairs). For some of the sets of disorders we could not find any pair with two affected twins (e.g. PTSD in one twin and OCD in the other). Such empty cells destabilised solutions. We therefore evaluated gender-specific effects for one disorder at a time, assuming that we could ignore such effects in multivariate models unless they were robustly detected across single disorders. Briefly, no evidence for any qualitative gender effect (which allows for gender-specific sources of genetic or environmental effects) or quantitative gender effect (which permits differing estimates of genetic and environmental effects by gender) was found for panic disorder, GAD or OCD. Modelling indicated some support for qualitative gender effects for phobia and quantitative gender effects for PTSD. In the light of these modest and inconsistent findings, we excluded gender effects from our multivariate modelling.
Twin models are often simplified by dropping insignificant paths. However, Sullivan & Eaves have shown that in the presence of low power – as is the case in these analyses – full models may better approximate reality than do simpler best-fit models.25 This is because, with low power, the effects originally distributed among several parameters may be aggregated into a few inflated parameters with unrealistically small confidence intervals. With the limited power of our data, we present results from the full best-fitting multivariate model with no attempt at further simplification. The Mx computer program was used for the analyses.26 Raw data analysis was applied and the thresholds (prevalences) were permitted to vary between men and women.
Results
Prevalence and phenotypic correlational structure
The prevalence estimates for the full and subthreshold definitions of panic disorder, GAD, phobia, OCD and PTSD are shown in Table 1. The phenotypic polychoric correlations between these disorders are presented in Table 2. Most vary between 0.35 and 0.55. In both men and women, panic disorder and GAD were the most strongly and OCD and PTSD the least strongly intercorrelated disorders. By confirmatory factor analysis, a single-factor solution allowing estimates to differ across genders fitted the data very well (χ210 = 6.86, P = 0.739, RMSEA = 0.000). Factor loadings were similar across genders except for a lower loading for OCD in women (Table 2). Constraining the factor loadings to equality in men and women hardly worsened the fit (χ215 = 11.66, P = 0.705, RMSEA = 0.000). We performed the same analysis on our dichotomous data eliminating subthreshold cases. The results were similar to those seen including the subthreshold cases (Table 2).
Table 1.
Prevalence estimates for men and women
| Men, % (n = 1011) | Women, % (n = 1759) | |||||
|---|---|---|---|---|---|---|
| Subthreshold disorder | One full disorder | More than one full disorder | Subthreshold disorder | One full disorder | More than one full disorder | |
| Panic disorder | 7.8 | 1.0 | – | 14.7 | 3.9 | – |
| Generalised anxiety disorder | 5.9 | 0.9 | – | 13.1 | 3.0 | – |
| Phobiasa | – | 10.7 | 2.2 | – | 18.5 | 12.4 |
| Obsessive–compulsive disorder | 4.0 | 1.5 | – | 7.1 | 2.4 | – |
| Post-traumatic stress disorder | 7.2 | 0.7 | – | 9.5 | 2.8 | – |
Includes agoraphobia and social and specific phobias, subthreshold not defined.
Gender differences were significant (P<0.006) for all disorders.
Table 2.
Phenotypic correlations between five anxiety disorders and loadings from a single-factor confirmatory factor analysis
| Correlationsa | Factor loading (95% CI) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | Men | Women | Total | Total, dichotomous | |
| 1 Panic disorder | 0.57 | 0.50 | 0.53 | 0.42 | 0.77 (0.68–0.87) | 0.74 (0.67–0.80). | 0.74 (0.6–0.80) | 0.75 (0.64–0.85) | |
| 2 Generalised anxiety disorder | 0.52 | 0.47 | 0.48 | 0.40 | 0.72 (0.61–0.83) | 0.70 (0.63–0.77) | 0.71 (0.65–0.77) | 0.70 (0.59–0.82) | |
| 3 Phobias | 0.49 | 0.44 | 0.47 | 0.38 | 0.66 (0.56–0.76) | 0.67 (0.61–0.73) | 0.66 (0.61–0.72) | 0.69 (0.61–0.78) | |
| 4 Obsessive–compulsive disorder | 0.32 | 0.39 | 0.35 | 0.36 | 0.68 (0.55–0.81) | 0.51 (0.42–0.60) | 0.56 (0.49–0.64) | 0.52 (0.37–0.66) | |
| 5 Post-traumatic stress disorder | 0.39 | 0.36 | 0.39 | 0.24 | 0.56 (0.42–0.69) | 0.54 (0.47–0.62) | 0.55 (0.49–0.62) | 0.65 (0.59–0.76) | |
Male correlation matrix in upper triangle, female matrix in lower triangle. Test of single factor structure (entering male and female correlation matrix): χ210 = 6.86, P = 0.739, RMSEA = 0.000. Test of invariance across gender: χ215 = 11.66, P = 0.705, RMSE = 0.000.
Testing the assumption of a single dimension of liability
To examine further whether full-criteria and subthreshold diagnoses reflected the same underlying liability, we applied the multiple threshold model to all bivariate combinations – within individuals, between twins within disorder, and cross-twin cross-disorder – testing 45 relationships in each of five zygosity groups. The mean probability value for these 225 tests was 0.43, close to 0.50 expected; 7.6% of the values exceeded 0.05, close to chance expectations.
Multivariate model fitting and results
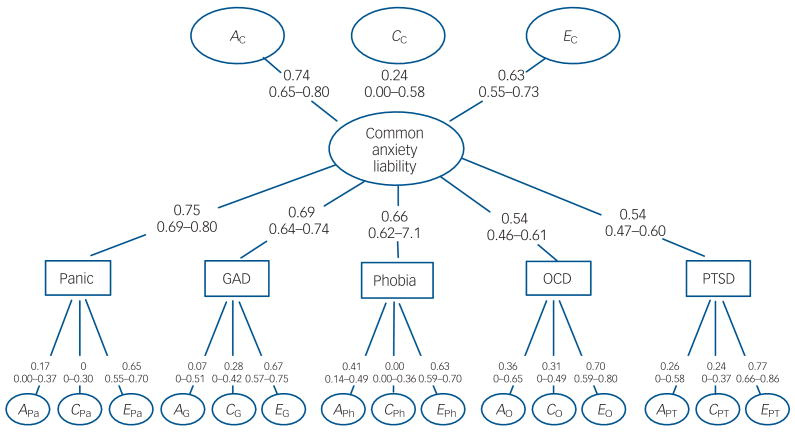
The common pathway model provided a better fit to the data than the independent pathway model (Δχ27 = 11.60, P = 0.11, ΔAIC = −2.40). The results for the full common pathway model are shown in Fig. 1, where squaring the path coefficients gives the proportions of variance explained. The latent phenotypic factor – a general liability to all anxiety disorders – is substantially influenced by genetic factors, with an estimated heritability of 54%. In contrast, the contribution of shared environment was small (6%) and not statistically significant. Individual-specific environment equalled 40%.
Fig. 1.
Parameter estimates for five anxiety disorders from a full multivariate common pathway model. A, additive genetic factors; C, environmental factors shared by co-twins; E, environmental non-shared factors; GAD, generalised anxiety disorder; OCD, obsessive–compulsive disorder; PTSD, post-traumatic stress disorder. Subscripts Pa, G, Ph, O and Pt denote panic, GAD, phobias, OCD and PTSD respectively; subscript C denotes ‘common’ (i.e. common to all disorders). Note: some of the confidence intervals are approximate.
The paths from the common factor to the individual disorders closely mirror those found in the confirmatory factor analysis (Table 2), with highest loadings seen for panic disorder and GAD scores and lowest loadings for OCD and PTSD scores. The genetic and environmental effects specific to each anxiety disorder score are seen in the lower part of Fig. 1. Disorder-specific genetic effects are negligible for panic disorder and GAD, intermediate but non-significant for OCD and PTSD and strongest for phobia. A more informative way to interpret these results is seen in Table 3, which presents estimated total heritability and the percentage of genetic effects for each disorder score resulting from the common factor and unique to each disorder score. Total heritabilities were generally modest, ranging from 23% for PTSD to 40% for phobias. The proportions of genetic effects unique to each disorder score were more variable, ranging from 4% for GAD to 40% for phobia and 45% for OCD.
Table 3.
Magnitude and origin of genetic, shared environmental and individual-specific environmental effects for five anxiety disorders from the best-fit common factor model
| Standardised variance estimates | ||||||
|---|---|---|---|---|---|---|
| Genetic | Shared environment | Individual-specific environment | ||||
| Common | Specific | Common | Specific | Common | Specific | |
| Panic disorder | ||||||
| Variancea | 0.30 (91%) | 0.03 (9%) | 0.03 (100%) | 0.00 (0%) | 0.22 (34%) | 0.42 (66%) |
| 95% CIb | 0.10–0.42 | 0.00–0.14 | 0.00–0.13 | 0.00–0.09 | 0.20–0.30 | 0.30–0.49 |
| Generalised anxiety disorder | ||||||
| Variance | 0.26 (96%) | 0.01 (4%) | 0.03 (27%) | 0.08 (73%) | 0.17 (28%) | 0.44 (72%) |
| 95% CI | 0.19–0.36 | 0.00–0.20 | 0.00–0.17 | 0.00–0.18 | 0.12–0.20 | 0.32–0.56 |
| Phobias | ||||||
| Variance | 0.24 (60%) | 0.16 (40%) | 0.03 (100%) | 0.00 (0%) | 0.18 (31%) | 0.40 (69%) |
| 95% CI | 0.02–0.24 | 0.00–0.15 | 0.00–0.13 | 0.13–0.24 | 0.35–0.49 | 0.08–0.33 |
| Obsessive–compulsive disorder | ||||||
| Variance | 0.16 (55%) | 0.13(45%) | 0.02 (17%) | 0.10 (83%) | 0.11 (18%) | 0.49 (82%) |
| 95% CI | 0.05–0.22 | 0.00–0.42 | 0.00–0.10 | 0.00–0.21 | 0.07–0.16 | 0.35–0.64 |
| Post-traumatic stress disorder | ||||||
| Variance | 0.16 (70%) | 0.07 (30%) | 0.02 (25%) | 0.06 (75%) | 0.12 (17%) | 0.58 (83%) |
| 95% CI | 0.08–0.24 | 0.00–0.36 | 0.00–0.09 | 0.00–0.17 | 0.09–0.17 | 0.44–0.73 |
Percentages in parentheses are proportions of common and specific variance for each major type of effect (genetic, shared environmental and individual-specific environmental).
Confidence intervals are approximate.
The estimated shared environmental effects specific to each disorder score were modest and none reached significance. They vary, being estimated at zero for panic disorder and phobia scores, and to account for 8% of total variance in liability for GAD scores and 10% for OCD scores. As seen in Table 3, for three of the anxiety disorder scores – GAD, OCD and PTSD – most of the shared environmental effects appeared to be disorder-specific. For the remaining two disorder scores – panic disorder and phobia – the very modest shared environmental effects were entirely common to all disorders. Non-shared environment contributed to the comorbidity with about two-thirds of the genetic contribution.
Discussion
Our analyses had four noteworthy results. First, in an epidemiological sample of young-adult twins, confirmatory factor analysis found that a single factor could well explain the observed comorbidity between lifetime diagnoses of the five forms of anxiety disorder (including subthreshold scores), both when diagnosed using traditional DSM–IV criteria and when including empirically derived subthreshold cases. Loadings on this common factor were strongest for panic disorder and GAD and weakest for OCD and PTSD. Second, a common pathway multivariate twin model fitted the data well. The latent liability common to all anxiety disorder scores was substantially heritable (54%) with only a minimal and non-significant estimated contribution from the shared environment. Third, the total heritability of the five anxiety disorder scores was generally moderate and ranged from 23% for PTSD to 40% for phobia. Fourth, the pattern of disorder-specific loadings for the five individual disorder scores was variable and informative. All five anxiety disorder scores derived the majority of their genetic risk from the common factor. Panic disorder and GAD had minimal disorder-specific genetic effects, indicating that these two disorders best indexed the genetic liability common to all anxiety disorder scores. In contrast, OCD derived almost half its genetic effect from factors specific to that disorder score. Although modest in overall magnitude, for three of the variables – GAD, OCD and PTSD – the majority of the shared environmental influences seemed to be disorder-specific in nature.
Interpretation and comparison with prior results
Epidemiological studies from New Zealand,9 the USA,10 Australia11 and Holland12 have all shown correlations and factor loadings for the anxiety disorders that correspond well with our results. Our heritability estimates for panic disorder, GAD, phobia and OCD are similar to or slightly lower than those previously reported.1–8 A meta-analysis of previous twin studies estimated heritabilities of 0.43 for panic disorder, 0.32 for generalised anxiety disorder and 0.20–0.37 for various types of phobias.2 A review of twin studies on obsessive–compulsive disorders reported heritabilities of 0.27 to 0.47.8 Analyses of the only large twin sample with PTSD data, the Vietnam Era Twin Registry, have shown a heritability of 0.35,3 compared with our estimate of 0.23. Our results may be lower because the rates of severe trauma – a prerequisite for a PTSD diagnosis – were probably much lower in our community sample than in a cohort of male war veterans. This would be likely to reduce heritability, since our sample would contain individuals at high genetic risk of PTSD that would not be manifested owing to the absence of trauma exposure.
Our multivariate findings can be usefully compared with those from the two most comparable prior studies. Chantarujikapong et al found that a single-factor independent pathway model best fitted lifetime PTSD and symptoms of GAD and panic disorder in 3371 male pairs from the Vietnam Era Twin Registry.3 Their results agreed with ours in finding nearly all genetic effects on GAD to be shared with the other anxiety disorders and approximately a third of the genetic risk of PTSD to be disorder-specific. Their results differed, however, in finding a much higher proportion of genetic effects on panic disorder to be disorder-specific (49% in their study v. 9% in ours). Hettema et al analysed data on panic disorder, GAD, agoraphobia and social, animal and situational phobias in approximately 5000 twins in the USA.4 Their results differed from ours in suggesting that two genetic factors were required to explain the observed patterns of comorbidity. Their results concurred with ours in finding that GAD and panic disorder shared nearly all genetic risk factors whereas at least some subtypes of phobias were strongly influenced by genetic factors only weakly related to panic disorder and GAD.
A notable result from our model fitting is the higher heritability for the common anxiety disorder factor than for any of the individual disorders. This is, however, not unexpected from a psychometric perspective. Unreliability of measurement, which is a concern for some anxiety disorders, especially when assessed in non-clinical populations,27–29 will more substantially attenuate the heritability of the individual disorders than the latent common factor.
Implications for DSM–V
These results have four implications for those pondering the structure of anxiety disorders in the fifth edition of the DSM. First, despite strong evidence that GAD and major depressive disorder are genetically closely related,13–15 our results suggest that GAD is also strongly related genetically to the other anxiety disorders. Thus, genetic findings alone cannot justify its removal from the anxiety disorders and placement within the mood disorders. The genetic relationship between major depression and GAD may be non-specific and indicative of a broad shared genetic liability across a wide range of internalising disorders.30 Second, our results provide some support for the aetiological coherence of the anxiety disorders. All five dimensionally scored disorders do have appreciable loadings on the common factor. However, third, OCD and PTSD do differ from the other three anxiety disorders in that they have the lowest loadings on the common factor, and appear to have appreciable disorder-specific genetic and shared environmental influences. Thus, these two disorders in our data are the least closely related to the common factor. Fourth, the results for phobias are somewhat anomalous: on the one hand this disorder has a relatively high loading on the common factor, but on the other it has the greatest disorder-specific genetic risk factors. This might be the result of combining the different phobias, which may have partially distinct genetic and environmental risk factors as suggested by prior findings.4,31,32 However, we also cannot exclude the possibility that our deviating findings for phobia to some extent reflect our choice of a common pathway model, which in terms of AIC value was only marginally favourable to the independent pathway model. The latter, on which previous estimates were based, produced somewhat different results.
Limitations
These results should be interpreted in the context of eight potential methodological limitations. Our sample consisted of young-adult Norwegian twins, and these results may not generalise to other populations. Despite our substantial sample size, limited prevalence for all the anxiety disorders except phobias required that we use subthreshold cases to permit meaningful model fitting. These cases were empirically defined, and for three variables where questionnaire data were used to extend the subthreshold groups, the questionnaire data correlated moderately to highly with the diagnostic data. Their addition did not appreciably alter the results of confirmatory factor analysis. Multiple threshold analyses showed that they reflected the same liability dimensions as the syndromal DSM–IV cases. However, our results might still have differed somewhat if based on DSM-defined disorders only.
As detailed elsewhere,33 only pairs who had participated in a previous questionnaire study were invited to the MHT study. Thus, considerable attrition, taking place in two steps, might imply recruitment bias of the results. However, unpublished results have shown only a moderate selection towards superior mental health in previously completed questionnaires. Biometric genetic analyses of mental health variables from the questionnaires did not differ between MHT participants and non-participants. Accordingly, substantial recruitment bias of the biometric genetic analyses in this study is unlikely. Univariate analyses suggested that there could be quantitative and qualitative gender differences for phobias and PTSD that we were unable to incorporate into our multivariate model. Therefore, results for these variables should be interpreted as an approximate average across genders rather than fully valid for men and women specifically. Qualitative gender-specific effects if ignored will bias the estimates of heritability upwards. However, most of the heritability estimates for our modelling were somewhat lower than expected from previous results. It is unlikely that our results were substantially biased by our inability to model gender effects.
Phobia subtypes may be partly influenced by different genes.4,31,32 Results from a twin study suggest a particularly strong familial covariance between agoraphobia and panic anxiety.34 Given low rates of certain subtypes, especially in our male participants, we could not include phobia subtypes in our multivariate models. Therefore, our results for phobias are inevitably averaged across the subtypes.
Because our analyses included only anxiety disorders, they cannot address the important question of whether the genetic and environmental risk factors common to all anxiety disorders are specific only to anxiety disorders or shared with other internalising disorders. The specification of genetic or environmental effects common to two or more phenotypes does not exclude the possibility of causal relationships between these phenotypes. If phenotype X causes phenotype Y, genetic or environmental factors primarily affecting X will be mediated through X and indirectly affect Y. Our twin modelling and data are not informative on possible causal relationships between the anxiety disorders. Such causal relationship will only be expressed as genetic or environmental variance common to the disorders.
Finally, the observed genetic covariance structure as well as the diagnosis-specific genetic variance might perhaps be further decomposed into effects of genes coding for possible endophenotypes. The latter are by definition more fundamental and genetically more homogeneous than complex phenotypes such as anxiety disorders. Possible endophenotypes might include behavioural characteristics such as ‘behavioural inhibition’,35 biological factors such as gamma-aminobutyric acid type A receptor diversity,36 or perhaps a combination of the two such as sensitivity to hypercapnia.37 Although our study, not informative on such factors, first and foremost needs replication based on diagnostic data, future twin studies of diagnostic anxiety data together with endophenotypic data may further extend our understanding of the comorbidity among anxiety disorders.
Acknowledgments
Funding: This study was supported by NIH grants MH-068643 (principal investigator K.S.K.) and MH-65322 (principal investigator M.C.N.). The twin programme of research at the Norwegian institute of Public Health is supported by grants from the Norwegian Research Council, the Norwegian Foundation for Health and Rehabilitation, the Foundation of Borderline Research, and the European Commission under the programme Quality of Life and Management of the Living Resources of the Fifth Framework Programme (number QLG2-CT-2002-01254). Genotyping of the twins was performed at the Starr Genotyping Resource Centre at Rockefeller University.
The authors thank Dr Jack Hettema for valuable advice and the twins for their participation.
Appendix
Subthreshold criteria
Panic disorder
Meeting criteria for panic attack.
OR
Confirming ‘ever had an attack when all of a sudden you felt frightened, anxious or very uneasy? Some people call it a panic attack’ without being in danger, AND endorsing four or more of the 17 types of symptoms listed in the interview.
Generalised anxiety disorder
Two of the six DSM criteria were relaxed in various ways.
-
(A) Felt worried, tense or anxious over longer than 3 months (originally 6 months); worried 2–3 days a week (originally ≥4 days); worried about everyday events, but did not perceive the worrying to be ‘excessive, that is, stronger than in other people in similar situation’ (originally required to be ‘excessive’).
(E) Anxiety interfered at least ‘somewhat’ (originally at least ‘a lot’) with life/daily activities; reported at least three of seven types of symptoms (originally in DSM–IV, three of six types of listed symptoms are required. An extra type of symptom, ‘feels like having a lump in one's throat’ is added in the CIDI).
OR
-
As (i), except (A): the period lasted 6 months, and (E): only two types of symptoms were required.
OR
As (i), except (A): worrying was also perceived by the individual to be excessive and (E): only two types of symptoms were required.
Obsessive–compulsive disorder
Endorsing any of the CIDI OCD screening questions about clearly obsessive or compulsive symptoms.
Post-traumatic stress disorder
Three of the six DSM criteria were relaxed:
(C) Reported at least one type (originally ≥3) of avoidance reaction.
(D) Reported at least one symptom (originally ≥2) of increased arousal.
(E) Duration criterion (>1 month) dropped.
From fully diagnosed and subthreshold PTSD cases, 13% and 12% respectively reported only a type of traumatic event not listed in the interview.
Footnotes
Declaration of interest: None.
Contributor Information
Kristian Tambs, Department of Mental Health, Norwegian Institute of Public Health, Oslo, Norway, and Virginia Institute for Psychiatric and Behavioral Genetics, Virginia Commonwealth University, Richmond, Virginia, USA.
Nikolai Czajkowsky, Department of Mental Health, Norwegian Institute of Public Health, Oslo.
Espen Røysamb, Department of Mental Health, Norwegian Institute of Public Health, and Department of Psychology, University of Oslo, Norway.
Michael C. Neale, Virginia Institute for Psychiatric and Behavioral Genetics, Virginia Commonwealth University, Richmond, Virginia, USA.
Ted Reichborn-Kjennerud, Department of Mental Health, Norwegian Institute of Public Health, and Institute of Psychiatry, University of Oslo, Norway.
Steven H. Aggen, Virginia Institute for Psychiatric and Behavioral Genetics, Virginia Commonwealth University, Richmond, Virginia, USA.
Jennifer R. Harris, Division of Epidemiology, Norwegian Institute of Public Health, Oslo.
Ragnhild E. Ørstavik, Department of Mental Health, Norwegian Institute of Public Health, Oslo, Norway.
Kenneth S. Kendler, Virginia Institute for Psychiatric and Behavioral Genetics, Virginia Commonwealth University, Richmond, Virginia, USA.
References
- 1.Middeldorp CM, Birley AJ, Cath DC, Gillespie NA, Willemsen G, Statham DJ, et al. Familial clustering of major depression and anxiety disorders in Australian and Dutch twins and siblings. Twin Res Hum Genet. 2005;8:609–15. doi: 10.1375/183242705774860123. [DOI] [PubMed] [Google Scholar]
- 2.Hettema JM, Neale MC, Kendler KS. A review and meta-analysis of the genetic epidemiology of anxiety disorders. Am J Psychiatry. 2001;158:1568–78. doi: 10.1176/appi.ajp.158.10.1568. [DOI] [PubMed] [Google Scholar]
- 3.Chantarujikapong SI, Scherrer JF, Xian H, Eisen SA, Lyons MJ, Goldberg J, et al. A twin study of generalized anxiety disorder symptoms, panic disorder symptoms and post-traumatic stress disorder in men. Psychiatry Res. 2001;103:133–45. doi: 10.1016/s0165-1781(01)00285-2. [DOI] [PubMed] [Google Scholar]
- 4.Hettema JM, Prescott CA, Myers JM, Neale MC, Kendler KS. The structure of genetic and environmental risk factors for anxiety disorders in men and women. Arch Gen Psychiatry. 2005;62:182–9. doi: 10.1001/archpsyc.62.2.182. [DOI] [PubMed] [Google Scholar]
- 5.Kendler KS, Gardner CO, Prescott CA. Panic syndromes in a population-based sample of male and female twins. Psychol Med. 2001;31:989–1000. doi: 10.1017/s0033291701004226. [DOI] [PubMed] [Google Scholar]
- 6.Kendler KS, Gardner CO, Gatz M, Pedersen NL. The sources of co-morbidity between major depression and generalized anxiety disorder in a Swedish national twin sample. Psychol Med. 2007;37:453–62. doi: 10.1017/S0033291706009135. [DOI] [PubMed] [Google Scholar]
- 7.Skre I, Onstad S, Torgersen S, Lygren S, Kringlen E. A twin study of DSM–III–R anxiety disorders. Acta Psychiatr Scand. 1993;88:85–92. doi: 10.1111/j.1600-0447.1993.tb03419.x. [DOI] [PubMed] [Google Scholar]
- 8.Van Grootheest DS, Cath DC, Beekman AT, Boomsma DI. Twin studies in obsessive–compulsive disorders: a review. Twin Res Hum Gen. 2005;8:450–8. doi: 10.1375/183242705774310060. [DOI] [PubMed] [Google Scholar]
- 9.Krueger RF, Caspi A, Moffitt TE, Silva PA. The structure and stability of common mental disorders (DSM–III–R): a longitudinal epidemiological study. J Abnorm Psychol. 1998;107:216–27. doi: 10.1037//0021-843x.107.2.216. [DOI] [PubMed] [Google Scholar]
- 10.Krueger RF. The structure of common mental disorders. Arch Gen Psychiatry. 1999;56:921–6. doi: 10.1001/archpsyc.56.10.921. [DOI] [PubMed] [Google Scholar]
- 11.Slade T, Watson D. The structure of common DSM–IV and ICD–10 mental disorders in the Australian general population. Psychol Med. 2006;36:1593–600. doi: 10.1017/S0033291706008452. [DOI] [PubMed] [Google Scholar]
- 12.Vollebergh WAM, Iedema J, Bijl RV, de Graaf R, Smit F, Ormel J. The structure and stability of common mental disorders. The Nemesis Study. Arch Gen Psychiatry. 2001;58:597–603. doi: 10.1001/archpsyc.58.6.597. [DOI] [PubMed] [Google Scholar]
- 13.Kendler KS, Neale MC, Kessler RC, Heath AC, Eaves LJ. Depression and generalized anxiety disorder. Same genes, (partly) different environments? Arch Gen Psychiatry. 1992;49:716–22. doi: 10.1001/archpsyc.1992.01820090044008. [DOI] [PubMed] [Google Scholar]
- 14.Kendler KS, Gatz M, Gardner CO, Pedersen NL. A Swedish national twin study of lifetime major depression. Am J Psychiatry. 2006;163:109–14. doi: 10.1176/appi.ajp.163.1.109. [DOI] [PubMed] [Google Scholar]
- 15.Roy MA, Neale MC, Pedersen NI, Mathe AA, Kendler KS. A twin study of generalized anxiety disorder and depression. Psychol Med. 1995;25:1037–49. doi: 10.1017/s0033291700037533. [DOI] [PubMed] [Google Scholar]
- 16.Harris JR, Magnus P, Tambs K. The Norwegian Institute of Public Health Twin Panel: a description of the sample and program of research. Twin Res. 2002;5:415–23. doi: 10.1375/136905202320906192. [DOI] [PubMed] [Google Scholar]
- 17.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (4th edn) (DSM–IV) APA; 1994. [Google Scholar]
- 18.Wittchen HU, Pfister H. DIA-X Interviews (M-CIDI): Manual fur Screening-Verfahren und Interview: Interviewheft Langsschnittuntersuchung (DIA-X-Lifetime); Erganzungsheft (DIA-X-Lifetime); Interviewheft Querschnittuntersuchung (DIA-X 12 Monate); Erganzungsheft (DIA-X 12 Monate); PC-Programm zur Durchfuhrung des Interviews (Langs- und Querschnittuntersuchung); Auswertungsprogramm. Swets & Zeitlinger; 1997. [Google Scholar]
- 19.Tambs K, Moum T. How well can a few questionnaire items indicate anxiety and depression? Acta Psychiatr Scand. 1993;87:364–7. doi: 10.1111/j.1600-0447.1993.tb03388.x. [DOI] [PubMed] [Google Scholar]
- 20.Bollen KA, Curran PJ. Latent Curve Models: A Structural Equation Approach. Wiley; 2006. [Google Scholar]
- 21.Olsson U. Maximum-likelihood estimation of polychoric correlation coefficient. Psychometrica. 1979;44:443–60. [Google Scholar]
- 22.Jöreskog KG, Sörbom D. Prelis 2 User's Reference Guide. Scientific Software International; 2002. [Google Scholar]
- 23.Neale MC, Cardon LR. Methodology for Genetic Studies of Twins and Families. Kluwer; 1992. [Google Scholar]
- 24.Akaike H. Statistical predictor identification. Ann Inst Stat Math. 1970;21:243–7. [Google Scholar]
- 25.Sullivan PF, Eaves LJ. Evaluation of analyses of univariate discrete twin data. Behav Genet. 2002;32:221–7. doi: 10.1023/a:1016025229858. [DOI] [PubMed] [Google Scholar]
- 26.Neale MC, Boker SM, Xie G, Maes H. Mx: Statistical Modeling. 5th. Department of Psychiatry, Virginia Commonwealth University; 1999. [Google Scholar]
- 27.Kendler KS, Karkowski LM, Prescott CA. Fears and phobias: reliability and heritability. Psychol Med. 1999;29:539–53. doi: 10.1017/s0033291799008429. [DOI] [PubMed] [Google Scholar]
- 28.Mannuzza OS, Fyer AJ, Martin LY, Gallops MS, Endicott J, Gorman J, et al. Reliability of anxiety assessment. I. Diagnostic agreement. Arch Gen Psychiatry. 1989;46:1093–101. doi: 10.1001/archpsyc.1989.01810120035007. [DOI] [PubMed] [Google Scholar]
- 29.Wittchen HU, Kessler RC, Zhao S, Abelson J. Reliability and clinical validity of UM–CIDI DSM–III–R generalized anxiety disorder. J Psychiatry Res. 1995;29:95–110. doi: 10.1016/0022-3956(94)00044-r. [DOI] [PubMed] [Google Scholar]
- 30.Hettema J. The nosologic relationship between generalized anxiety disorder and major depression. In: Goldberg DP, Kendler KS, Sirovatka P, Regier DA, editors. Diagnostic Issues in Depression and Generalized Anxiety Disorder: Refining the Research Agenda for DSM–V. American Psychiatric Association; 2008. [DOI] [PubMed] [Google Scholar]
- 31.Kendler KS, Myers J, Prescott C, Neale MC. The genetic epidemiology of irrational fears and phobias in men. Arch Gen Psychiatry. 2001;58:257–65. doi: 10.1001/archpsyc.58.3.257. [DOI] [PubMed] [Google Scholar]
- 32.Sundet JM, Skre I, Okkenhaug JJ, Tambs K. Genetic and environmental causes of the interrelationships between self-reported fears. A study of a non-clinical sample of Norwegian identical twins and their families. Scand J Psychol. 2003;44:97–106. doi: 10.1111/1467-9450.00326. [DOI] [PubMed] [Google Scholar]
- 33.Kendler KS, Aggen SH, Tambs K, Reichborn-Kjennerud T. Illicit psychoactive substance use, abuse and dependence in a population-based sample of Norwegian twins. Psychol Med. 2006;36:955–62. doi: 10.1017/S0033291706007720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tsuang M, Domschke K, Jerskey BA, Lyons MJ. Agoraphobic behaviour and panic attack: a study of male twins. J Anxiety Disord. 18:799–807. doi: 10.1016/j.janxdis.2003.10.001. [DOI] [PubMed] [Google Scholar]
- 35.Stein DJ, Vythilingum B. Social anxiety disorder: psychological and evolutionary underpinnings. CNS Spectrum. 2007;12:806–9. doi: 10.1017/s1092852900015534. [DOI] [PubMed] [Google Scholar]
- 36.Mohler H. GABA(A) receptor diversity and pharmacology. Cell Tissue Res. 2006;326:505–16. doi: 10.1007/s00441-006-0284-3. [DOI] [PubMed] [Google Scholar]
- 37.Battaglia M, Pesenti-Gritti P, Spatola CAM, Ogliari A, Tambs K. A twin study of the common vulnerability between heightened sensitivity to hypercapnia and panic disorder. Am J Med Genet B (Neuropsychiatr Genet) 147B:586–93. doi: 10.1002/ajmg.b.30647. [DOI] [PubMed] [Google Scholar]