Abstract
Summary
Prospective Observational Scientific Study Investigating Bone Loss Experience in Europe (POSSIBLE EU®) is an ongoing longitudinal cohort study that utilises physician- and patient-reported measures to describe the characteristics and management of postmenopausal women on bone loss therapies. We report the study design and baseline characteristics of 3,402 women recruited from general practice across five European countries.
Purpose
The POSSIBLE EU® is a study describing the characteristics and management of postmenopausal women receiving bone loss medications.
Methods
Between 2005 and 2008, general practitioners enrolled postmenopausal women initiating, switching or continuing treatment with bone loss treatment in France, Germany, Italy, Spain and the UK. Patients and physicians completed questionnaires at study entry and at 3-month intervals, for 1 year.
Results
Of 3,402 women enrolled (mean age 68.2 years [SD] 9.83), 96% were diagnosed with low bone mass; 55% of these using dual energy X-ray absorptiometry. Most women (92%) had comorbidities. Mean minimum T score (hip or spine) at diagnosis was −2.7 (SD 0.89; median −2.7 [interquartile range, −3.2, −2.2]) indicating low bone mineral density. Almost 40% of the women had prior fractures in adulthood, mostly non-vertebral, non-hip in nature, 30% of whom had at least two fractures and more than half experienced moderate/severe pain or fatigue. Bisphosphonates were the most common type of bone loss treatment prescribed in the 12 months preceding the study.
Conclusions
POSSIBLE EU® characterises postmenopausal women with low bone mass, exhibiting a high rate of prevalent fracture, substantial bone fragility and overall comorbidity burden. Clinical strategies for managing osteoporosis in this population varied across the five participating European countries, reflecting their different guidelines, regulations and standards of care.
Keywords: Cohort studies, Osteoporosis, Postmenopausal osteoporosis, Prospective studies
Introduction
Postmenopausal osteoporosis is a systemic skeletal disease resulting in increased bone fragility and fracture risk subsequent to a decrease in bone mass and the degradation of bone microarchitecture [1, 2]. Osteoporosis increases the risk of fractures, adversely affecting quality of life, which can result in pain, fatigue and a reduction in activities of daily living [1, 2].
Despite the availability of several treatment options, osteoporosis compromises the health of a significant number of postmenopausal women [1, 2]. Treatment initiation in this population may be inconsistent and is often delayed until the late stages of disease [3]. In addition, almost half of patients do not comply or persist with bone loss medications within the first year of treatment [4]. Poor adherence to treatments may be associated with poor outcomes, including an increased risk of fractures [5]. Furthermore, the thresholds for diagnostic assessment and treatment vary across countries because of differing national guidelines and regulatory requirements, although the European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis recently provided some guidance for national level guideline development [5]. Understanding how osteoporosis treatments are being used and how they are perceived by patients in Europe will help provide further insights into the management of osteoporosis care.
The Prospective Observational Scientific Study Investigating Bone Loss Experience in Europe (POSSIBLE EU®) is a longitudinal cohort study conducted in Europe between 2005 and 2008. It is broadly similar to the recently described POSSIBLE US™ study conducted in US patients [6]. POSSIBLE EU® is designed to describe the use of current bone loss treatments by postmenopausal women who are initiating or switching bone loss therapies, or who have been on such therapy for some time. Through the retrospective and prospective collection of clinical and patient experience data, POSSIBLE EU® will provide insights about bone loss therapies and how they were used by postmenopausal women in Europe between 2005 and 2008. It will also report on the relationship between patient characteristics and patient behaviours (e.g. medication adherence) and important outcomes (e.g. fractures, health-related quality of life and treatment satisfaction).
In addition to describing the design of the POSSIBLE EU® study, this paper describes the characteristics and management of postmenopausal women in Europe receiving bone loss medications.
Materials and methods
Study design and primary outcomes
POSSIBLE EU® was initiated in December 2005, with enrolment completed in March 2008. The study was conducted by a total of 215 investigators at 196 sites in five European countries: France, Germany, Italy, Spain and the UK. The study was non-interventional and designed to provide insights into routine clinical practice while minimising the impact of data collection on clinical management of participating women. A local or central institutional ethics committee approved the protocol for each site. All patients provided written informed consent. Data collected in this study included: a medical history, including fractures experienced during adulthood and bone loss treatments; health-related quality of life and perceptions about medications in general and, for women already receiving bone loss treatments, patient-reported experience of treatment side effects, treatment persistence and adherence, perceptions about osteoporosis medications and satisfaction with treatment. Patients were being followed for 1 year.
Given the observational nature of this study, the term ‘bone loss’ was used in the protocol and data collection forms as a generic term to capture data on ’bone loss prevention medication’. More specific clinical terms (e.g. low bone mass, low bone mineral density, osteoporosis and osteopenia) were reserved for situations in which a clinical diagnosis was made or a clinical measure was available (e.g. when a T score was available by which to assign a diagnosis of osteoporosis or osteopenia as per World Health Organization criteria).
Treatment status cohorts
The investigators assigned patients to one of three cohorts based on prescribed bone loss treatment at study entry. These cohorts were defined as follows:
Inception—newly starting treatment with a bone loss therapy (no previous therapy within 12 months of entry).
Switch—received therapy at any given time during the previous 12 months and changed therapy as of study entry visit (including changes in dosing frequency, mode of administration and/or addition of a new bone loss therapy).
Established—had been receiving the same therapy for at least 12 months before study entry (with or without changes in dosage).
Enrolment goals overall were preset for these cohorts: at least 50% of patients were to be in the inception cohort, with at least 75% distributed across the inception and switch cohorts.
Role of the steering committee
This study is managed under the auspices of a steering committee consisting of clinicians and content area experts (e.g. epidemiology, patient outcomes, health-related quality of life and pharmacoeconomics).
Physician selection
Physicians and sites were chosen on the basis of: (a) a willingness or ability to take part in the study and (b) being representative of their country with respect to a range of characteristics, including broad geographical region, urban/rural distribution, gender of physician and size of practice (partnership size). Lists of general practitioners (GPs) in each of the five countries were obtained from commercial agencies and supplemented with a list of GPs participating in established research panels in France (MG Recherche) and the UK (Profiad).
Patient recruitment
Patients were invited to participate in the study during routine clinical visits to their GPs. Women were eligible to participate if they were ≥18 years old, ambulatory, ≥1 year postmenopausal (i.e. no vaginal bleeding or spotting for ≥12 months) from any cause and initiating or receiving ongoing bone loss therapy. Eligible therapies included the following: bisphosphonates, selective oestrogen-receptor modulators, calcitonin, parathyroid hormone, strontium ranelate and any other therapies with a marketing authorisation for the treatment of osteoporosis or commonly used to treat bone loss. Patients receiving therapy with calcium and/or vitamin D (singly or together) were included only when these agents were administered in combination with an eligible therapy. Women taking hormone replacement therapy alone were not eligible for inclusion. Women were excluded if they were participating in or had just completed other research studies, or if they were taking experimental treatments. Also, women with medical conditions that could impact their ability to participate in this study (e.g. receiving treatment for cancer) were excluded.
Patient retention
Approaches to retain patients in the study were designed to encourage continued patient participation while having minimal impact on clinical practice and patient behaviour. A combination of reminder cards and newsletters were used to encourage patients to return subsequent questionnaires on time. Investigators also reminded patients of the importance of continued participation in the study during routine visits.
Data collection
Investigators at study sites reported data for each patient at study entry and at 3-month intervals during the follow-up period, regardless of whether the patient visited the practice after study enrolment. Data collected at baseline included basic demographics, a low bone mass diagnosis, fracture history during adulthood, bone loss treatment and comorbidities during adulthood and concomitant medications. Investigators coded all fractures according to 22 different locations (or ‘Other’ and ‘Unknown’).
Patients completed a patient-reported outcome (PRO) questionnaire at enrolment, either at the study site or at home. Subsequent PRO data were collected from patients via questionnaires mailed to their homes at 3-month intervals. These PRO questionnaires were designed specifically for each cohort to reflect differences in prior treatment history. In general, the baseline PRO data collected included current bone loss treatments with information on side effects and adherence, patient satisfaction with and views on medications (general and bone loss as appropriate), health status, general pain and fatigue questions, risk factors for low bone mass and personal situation. Patient-reported fatigue was assessed using the following question: “During the past month, how would you describe the level of fatigue you usually experienced?” Patient-reported pain was assessed using the following question: “During the past month, how would you describe the level of pain usually experienced?” In addition, health-related quality of life was assessed using the EQ-5D [7–9], and using a disease-specific health-related quality of life instrument—the Osteoporosis Assessment Questionnaire short form [10] (data not shown).
Data storage and quality assurance
Data quality was assessed by ongoing review of the following: data return rates, data quality checks, quality of completion, consistency checks on data provided by physicians and patients, review of cohort allocation and ongoing review of medication coding. Data checks were performed to verify data and queries sent to the study sites. Data reported by patients were not queried.
Statistical analysis
Descriptive statistics are presented. Two analysis sets were defined: the full analysis set, which enrolled women with baseline physician-reported data; and the PRO analysis set, which enrolled women with a PRO completion date within the time window of −2/+8 weeks of the indicated enrolment date. Unless otherwise noted, data described in the text are from the full analysis set. Data on comorbidities were collected based on a list of 28 prespecified conditions and could be classified (yes/no) as ‘ever experienced during adulthood,’ ‘ongoing’ and ‘currently treated’.
Results
Site and patient enrolment
Overall, data were collected from 3,402 women who had consented to participate in the POSSIBLE EU® study. Of these, 2925 completed baseline PRO within the specified time limit, thereby comprising the PRO analysis set. Across the five countries, France, Germany and UK each contributed similar numbers of patients and sites, whereas Italy and Spain each contributed slightly fewer patients (Fig. 1). Among the countries, Germany, France, Italy and the UK had, for the most part, a single investigator per site, with a few sites having more than one investigator. In contrast, in Spain, multiple investigators were involved per site.
Fig. 1.
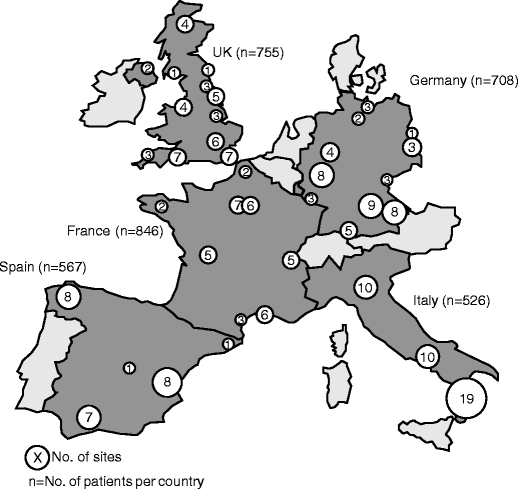
Distribution of sites by country
Demographics
Table 1 summarises patient characteristics across the cohorts. The percentage of patients across each cohort was 53% (inception), 31% (established) and 17% (switch). Overall, the mean age of these women was 68.2 years (SD 9.81) at enrolment; their median age at onset of menopause was 50 years (25th and 75th percentiles, 46, 52). Most were white; and most (86%) were ‘economically inactive’, i.e. not in paid employment. For the most part, these women were either living with other people (i.e. spouses, family or others; 67%); few were in assisted care facilities.
Table 1.
Baseline characteristics by cohort
| All patients | Inception cohort | Established cohort | Switch cohort | |
|---|---|---|---|---|
| Variable | (n = 3,402) | (n = 1,787) | (n = 1,041) | (n = 574) |
| Age, years | ||||
| Number | 3,402 | 1,787 | 1,041 | 574 |
| Mean (SD) | 68.2 (9.83) | 67.4 (10.12) | 68.9 (9.27) | 69.5 (9.71) |
| Age at menopause, years | ||||
| Number | 3,278 | 1,737 | 1,006 | 535 |
| Mean (SD) | 48.5 (5.50) | 48.4 (5.40) | 48.7 (5.36) | 48.2 (6.06) |
| Race/ethnicity | ||||
| Number | 3,402 | 1,787 | 1,041 | 574 |
| Caucasian/white, n (%) | 3,331 (97.9) | 1,747 (97.8) | 1,014 (97.4) | 570 (99.3) |
| Black, n (%) | 6 (0.2) | 3 (0.2) | 3 (0.3) | 0 |
| Asiana, n (%) | 9 (0.3) | 3 (0.2) | 5 (0.5) | 1 (0.2) |
| Other, n (%) | 3 (<0.1) | 2 (0.1) | 1 (<0.1) | 0 |
| Missing, n (%) | 53 (1.6) | 32 (1.8) | 18 (1.7) | 3 (0.5) |
| Living arrangements at baseline (%) | ||||
| Numberb | 2,925 | 1,525 | 907 | 493 |
| Alone, n (%) | 861 (29.4) | 435 (28.5) | 272 (30.0) | 154 (31.2) |
| With spouse/family/others, n (%) | 1,963 (67.1) | 1,049 (68.8) | 591 (65.2) | 323 (65.5) |
| Nursing home/residential care, n (%) | 12 (0.4) | 9 (0.6) | 3 (0.3) | 0 |
| Hostel, shelter, group or boarding home, n (%) | 20 (0.7) | 11 (0.7) | 7 (0.8) | 2 (0.4) |
| Unknown/missing, n (%) | 69 (2.4) | 21 (1.4) | 34 (3.7) | 14 (2.8) |
| Employment status | ||||
| Numberb | 2,925 | 1,525 | 907 | 493 |
| Working full-time, n (%)c | 169 (5.8) | 108 (7.1) | 39 (4.3) | 22 (4.5) |
| Working part-time, n (%)c | 127 (4.3) | 67 (4.4) | 41 (4.5) | 19 (3.9) |
| Economically inactive, n (%) | 2,523 (86.3) | 1,307 (85.7) | 788 (86.9) | 428 (86.8) |
| Unknown/missing, n (%) | 106 (3.6) | 43 (2.8) | 39 (4.3) | 24 (4.9) |
| Comorbid conditions, n d | ||||
| Number | 3,402 | 1,787 | 1,041 | 574 |
| No, n (%) | 280 (8.2) | 166 (9.3) | 82 (7.9) | 32 (5.6) |
| Yes, n (%) | 3,119 (91.7) | 1,620 (90.7) | 958 (92.0) | 541 (94.3) |
| Unknown/missing, n (%) | 3 (<0.1) | 1 (<0.1) | 1 (<0.1) | 1 (0.2) |
| Number of comorbiditiese, n | 10,556 | 5,379 | 3,217 | 1,960 |
| Mean (SD) no. per patient | 3.4 (2.01) | 3.3 (1.97) | 3.4 (2.05) | 3.6 (2.08) |
| No. patients with comorbid conditions, currently or previously experienced, n e | 3,402 | 1,787 | 1,041 | 574 |
| Back pain, n (%) | 1,677 (49.3) | 891 (49.9) | 511 (49.1) | 275 (47.9) |
| Hypertension, n (%) | 1,566 (46.0) | 831 (46.5) | 471 (45.2) | 264 (46.0) |
| Osteoarthritis, n (%) | 1,240 (36.4) | 619 (34.6) | 370 (35.5) | 251 (43.7) |
| Hyperlipidaemia, n (%) | 1,169 (34.4) | 613 (34.3) | 362 (34.8) | 194 (33.8) |
| Upper GI (GERD, reflux, dyspepsia), n (%) | 754 (22.2) | 335 (18.7) | 234 (22.5) | 185 (32.2) |
| Depression, n (%) | 640 (18.8) | 313 (17.5) | 194 (18.6) | 133 (23.2) |
| Vision impairment, n (%) | 399 (11.7) | 205 (11.5) | 120 (11.5) | 74 (12.9) |
| Lower GI (IBS, Crohn's disease), n (%) | 302 (8.9) | 131 (7.3) | 101 (9.7) | 70 (12.2) |
| Cancer, n (%) | 300 (8.8) | 147 (8.2) | 94 (9.0) | 59 (10.3) |
| Diabetes, n (%) | 296 (8.7) | 180 (10.1) | 72 (6.9) | 44 (7.7) |
| Asthma, n (%) | 249 (7.3) | 109 (6.1) | 97 (9.3) | 43 (7.5) |
| Thromboembolic diseases, n (%) | 231 (6.8) | 124 (6.9) | 67 (6.4) | 40 (7.0) |
| COPD, n (%) | 214 (6.3) | 114 (6.4) | 71 (6.8) | 29 (5.1) |
| Angina, n (%) | 194 (5.7) | 100 (5.6) | 59 (5.7) | 35 (6.1) |
| Other inflammatory disorders, n (%) | 192 (5.6) | 96 (5.4) | 55 (5.3) | 41 (7.1) |
| Rheumatoid arthritis, n (%) | 171 (5.0) | 74 (4.1) | 62 (6.0) | 35 (6.1) |
| Vitamin D deficiency, n (%) | 158 (4.6) | 73 (4.1) | 49 (4.7) | 36 (6.3) |
| Renal disease, n (%) | 139 (4.1) | 64 (3.6) | 44 (4.2) | 31 (5.4) |
| Hyperthyroidism, n (%) | 135 (4.0) | 82 (4.6) | 33 (3.2) | 20 (3.5) |
| Heart valve problems, n (%) | 107 (3.1) | 60 (3.4) | 25 (2.4) | 22 (3.8) |
| Congestive heart failure, n (%) | 91 (2.7) | 46 (2.6) | 22 (2.1) | 23 (4.0) |
| Ulcers, n (%) | 90 (2.6) | 40 (2.2) | 31 (3.0) | 19 (3.3) |
| Neuromuscular dysfunction, n (%) | 74 (2.2) | 40 (2.2) | 18 (1.7) | 16 (2.8) |
| Chronic liver disease, n (%) | 72 (2.1) | 46 (2.6) | 22 (2.1) | 4 (0.7) |
| Coagulopathy | 43 (1.3) | 22 (1.2) | 14 (1.3) | 7 (1.2) |
| Seizure disorders, n (%) | 31 (0.9) | 17 (1.0) | 6 (0.6) | 8 (1.4) |
| Hyperparathyroidism, n (%) | 16 (0.5) | 6 (0.3) | 9 (0.9) | 1 (0.2) |
| Paget’s disease, n (%) | 6 (0.2) | 1 (<0.1) | 4 (0.4) | 1 (0.2) |
| Diagnosed with low bone mass, n (%) | 3,260 (95.8) | 1,695 (94.9) | 1,007 (96.7) | 558 (97.2) |
| Patients diagnosed with low bone mass by method, n f | 3,260 | 1,695 | 1,007 | 558 |
| DXA, n (%) | 1,784 (54.7) | 926 (54.6) | 565 (56.1) | 293 (52.5) |
| X-ray, n (%) | 813 (24.9) | 446 (26.3) | 224 (22.2) | 143 (25.6) |
| Clinical (including family and fracture history), n (%) | 360 (11.0) | 157 (9.3) | 126 (12.5) | 77 (13.8) |
| Ultrasound, n (%) | 138 (4.2) | 73 (4.3) | 46 (4.6) | 19 (3.4) |
| Other, n (%) | 143 (4.4) | 84 (5.0) | 37 (3.7) | 22 (3.9) |
| Unknown/missing, n (%) | 22 (0.7) | 9 (0.5) | 9 (0.9) | 4 (0.7) |
| Diagnosis based on DXA, n g | 1,784 | 926 | 565 | 293 |
| Osteopenic, n (%) | 548 (30.7) | 311 (33.6) | 157 (27.8) | 80 (27.3) |
| Osteoporotic, n (%) | 1,216 (68.2) | 605 (65.3) | 403 (71.3) | 208 (71.0) |
| Unknown/missing, n (%) | 20 (1.1) | 10 (1.1) | 5 (0.9) | 5 (1.7) |
| Minimum T score (lowest value at hip or spine) at diagnosis, n | 1,529 | 844 | 439 | 246 |
| Mean (SD) | −2.7 (0.89) | −2.7 (0.87) | −2.8 (0.91) | −2.7 (0.88) |
| Time since diagnosis (years), n | 3,257 | 1,696 | 1,003 | 558 |
| Mean (SD) | 3.3 (4.10) | 1.9 (3.47) | 4.8 (3.98) | 4.8 (4.54) |
| Number of patients with fracture before baseline | ||||
| Number, n | 3,402 | 1,787 | 1,041 | 574 |
| With fracture, n (%) | 1,317 (38.7) | 630 (35.3) | 435 (41.8) | 252 (43.9) |
COPD chronic obstructive pulmonary disease, DXA dual energy X-ray absorptiometry, GI gastrointestinal, GERD gastro-oesophageal reflux disease
aIncludes Chinese, Bangladeshi, Indian and Pakistani
bBased on patient-reported outcome (PRO) analysis set
cPart-time work defined as working for pay <32 h/week; full-time as working for pay ≥32 h/week
dHas the patient (currently or previously) experienced any of the following comorbid conditions during adulthood (≥18 years of age)
eNumber of comorbid conditions currently or previously experienced by patients. Patients may have experienced more than one comorbid condition. Percentages are based on the total number of patients in the full analysis set
fPercentages based on number of patients with a low bone mass diagnosis reported
gPercentages based on number of patients with a method of bone loss diagnosis reported as DXA
Table 2 provides a general summary of patient characteristics by country, irrespective of cohort. The mean age at enrolment ranged from 63.8 years in Spain to 71.3 years in Germany. Spain had the lowest proportion of ‘economically inactive’ women (75%), and Italy and Germany had the highest (94% and 92%, respectively). The proportions of women living alone or with others appeared to vary slightly between countries, with the highest levels of living with other people being reported in Italy and Spain (76% and 79%, respectively), compared with 59% in Germany.
Table 2.
Overview of baseline characteristics by country
| Parameter | France (n = 846) | Germany (n = 708) | Italy (n = 526) | Spain (n = 567) | UK (n = 755) |
|---|---|---|---|---|---|
| Age, years | |||||
| Number | 846 | 708 | 526 | 567 | 755 |
| Mean (SD) | 68.4 (9.90) | 71.3 (8.93) | 66.5 (9.72) | 63.8 (9.16) | 69.5 (9.77) |
| Age at menopause, years | |||||
| Number | 828 | 681 | 521 | 554 | 694 |
| Mean (SD) | 49.6 (4.48) | 48.6 (5.94) | 48.9 (4.58) | 47.9 (5.19) | 47.1 (6.59) |
| Most common living arrangements at baseline | |||||
| Numbera, n | 654 | 626 | 459 | 499 | 687 |
| Alone, n (%) | 222 (33.9) | 226 (36.1) | 99 (21.6) | 89 (17.8) | 225 (32.8) |
| With spouse/family/others, n (%) | 415 (63.5) | 369 (58.9) | 348 (75.8) | 392 (78.6) | 439 (63.9) |
| Most common employment status | |||||
| Numbera, n | 654 | 626 | 459 | 499 | 687 |
| Economically inactive, n (%) | 569 (87.0) | 576 (92.0) | 432 (94.1) | 374 (74.9) | 572 (83.3) |
| Diagnosed with low bone mass, n (%) | 801 (94.7) | 685 (96.8) | 517 (98.3) | 543 (95.8) | 714 (94.6) |
| Most common methods of low bone mass diagnosis | |||||
| Number of patients, n b | 801 | 685 | 517 | 543 | 714 |
| DXA, n (%) | 471 (58.8) | 332 (48.5) | 263 (50.9) | 269 (49.5) | 449 (62.9) |
| X-ray, n (%) | 149 (18.6) | 194 (28.3) | 185 (35.8) | 177 (32.6) | 108 (15.1) |
| Clinical (including family and fracture history), n (%) | 155 (19.4) | 34 (5.0) | 26 (5.0) | 37 (6.8) | 108 (15.1) |
| Ultrasound | 0 | 55 (8.0) | 29 (5.6) | 30 (5.5) | 24 (3.4) |
| Other n (%) | 20 (2.5) | 65 (9.5) | 11 (2.1) | 25 (4.6) | 22 (3.1) |
| Unknown/missing, n (%) | 6 (0.7) | 5 (0.7) | 3 (0.6) | 5 (0.9) | 3 (0.4) |
| Type of low bone mass diagnosis by DXA, n c | 471 | 332 | 263 | 269 | 449 |
| Osteopenic | 200 (42.5) | 67 (20.2) | 83 (31.6) | 76 (28.3) | 122 (27.1) |
| Osteoporotic | 263 (55.8) | 265 (79.8) | 177 (67.3) | 189 (70.3) | 322 (71.7) |
| Unknown | 8 (1.7) | 0 | 3 (1.1) | 4 (1.5) | 5 (1.1) |
| Minimum T score (across all hip/spine measurements) at diagnosis, n | 437 | 277 | 239 | 193 | 383 |
| Mean (SD) | −2.6 (0.89) | −3.0 (0.97) | −2.8 (0.79) | −2.7 (0.76) | −2.8 (0.90) |
| Number of patients with fracture before baseline | |||||
| Number, n | 846 | 708 | 526 | 567 | 755 |
| With fracture, n (%) | 301 (35.6) | 311 (43.9) | 148 (28.1) | 167 (29.5) | 390 (51.7) |
| Number of previous fractures by location | |||||
| Numberd | 412 | 501 | 196 | 217 | 584 |
| Hip, n (%) | 37 (9.0) | 21 (4.2) | 21 (10.7) | 10 (4.6) | 50 (8.6) |
| Vertebral (spine), n (%) | 88 (21.4) | 158 (31.5) | 55 (28.1) | 41 (18.9) | 89 (15.2) |
| Non-vertebral/non-hipe, n (%) | 284 (68.9) | 321 (64.1) | 118 (60.2) | 166 (76.5) | 445 (76.2) |
DXA dual energy X-ray absorptiometry
aBased on patient-reported outcome (PRO) analysis set
bPercentages based on the number of patients with a bone loss diagnosis reported
cPercentages based on the number of patients with a method of bone loss diagnosis reported as DEXA
dNumber of fractures reported. Patients may have experienced more than one location of prior fractures
eIncludes all fracture locations other than hip and vertebral (spine)
Comorbid conditions
Most women (92%) experienced, either currently or previously, at least one of the prespecified comorbid conditions, with a mean (SD) number per patient 3.4 (2.01; Table 1) and a median of three conditions (25th and 75th percentiles, 2, 5) per patient. The two most common comorbidities were back pain (49%) and hypertension (46%). Although upper gastrointestinal comorbid conditions were reported in 22% of all patients, they were more commonly reported in the switch cohort (32%) than in the other two cohorts (19% inception, 23% established; Table 1). Osteoarthritis was also reported more frequently in the switch cohort (44%) than in the other two cohorts (35% inception, 36% established; Table 1).
Diagnosis
Of 3,402 women, 96% had a diagnosis of low bone mass (Table 1). Among those diagnosed, the most common methods of diagnosis were dual energy X-ray absorptiometry (DXA; 55%), followed by traditional X-ray (25%) and clinical history (11%; Table 1). Use of DXA for diagnosis permitted further characterisation of low bone mass as either osteopenic (31%) or osteoporotic (68%; Table 1). Among patients for whom DXA results were available at diagnosis, the mean minimum T score across all sites (i.e. femoral neck, total hip and lumbar spine) was −2.7 (SD 0.89; Table 1; median −2.7 [interquartile range. −3.2, −2.2]) with little variation across cohorts. Of the patients for whom no DXA results were available at diagnosis (43%), 55% were diagnosed by X-ray. Bone marker and vitamin D tests were rarely performed in these patients in the 3 months prior to study entry (in 3% and 3% of patients, respectively).
Table 2 shows country-level differences in both diagnostic approaches and level of disease progression in the study populations. The highest rate of diagnosis by DXA was in the UK (63%) and the lowest in Germany (49%). The highest use of X-rays was in Italy (36%) versus 15% in the UK; diagnosis by ‘other means’ was highest in Germany (10%) and lowest in Italy (2%). The mean minimum T scores (at diagnosis) ranged from −3.0 in Germany to −2.6 in France (Table 2), and the proportion of women with T scores in the osteoporotic range was highest in Germany (80%) and lowest (56%) in France.
Fractures
Fractures of the fingers, face, skull and toes were excluded. Overall, 1,317 (39%) women had experienced fractures during adulthood (Table 2 and Fig. 2); 12% of these women had at least two fractures. The corresponding percentages were slightly higher among women in the established cohort (42% and 14%, respectively) and those in the switch cohort (44% and 15%, respectively), compared with values in the inception cohort (35% and 9%, respectively). Among the 1,910 fractures reported and characterised by location (hip, vertebral and non-hip, non-vertebral [NHNV]), 70% occurred in NHNV locations, with 23% of fractures being in the spine and 7% in the hip (Fig. 2). Among patients diagnosed with osteopenia, 32% had a previous fracture compared with 37% of patients diagnosed with osteoporosis. Among patients who had no DXA at baseline, 43% had a previous fracture. Fracture type and prevalence by country is described in Table 2.
Fig. 2.
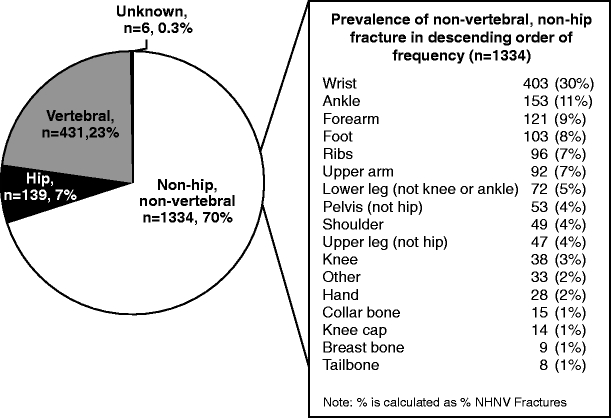
Prior fracture in adulthood by location (full analysis set). Percentages in the pie chart are reported as percentage of total number of fractures; percentages in the table are reported as percent of non-hip, non-vertebral fractures. Overall, 1,910 prior fractures were reported in this population
Bone loss medication at baseline
Women in the established and switch cohorts were most commonly prescribed bisphosphonates in the 12 months prior to the study (Table 3). Women in the switch cohort received a broader range of bisphosphonates and other products such as strontium ranelate.
Table 3.
Bone loss treatments during the 12 months preceding baseline
| Parameter | Established cohort (n = 1,041) | Switch cohort (n = 574) |
|---|---|---|
| Taken any bone loss treatments within 12 months of baseline? n (%) | ||
| Yes | 1,034 (99.3) | 570 (99.3) |
| Noa | 7 (0.7) | 4 (0.7) |
| Bone loss treatments, n b | 1,034 | 570 |
| Bisphosphonate, n (%) | 894 (86) | 541 (95) |
| Alendronate | 536 (52) | 366 (64) |
| Risedronate | 263 (25) | 256 (45) |
| Ibandronate | 67 (6) | 147 (26) |
| Clodronate | 23 (2) | 9 (2) |
| Etidronate | 21 (2) | 41 (7) |
| Pamidronate | 1 (0.1) | 3 (0.5) |
| Zoledronate | 0 | 2 (0.4) |
| Neridronate | 0 | 1 (0.2) |
| Unknown bisphosphonates | 0 | 1 (0.2) |
| Strontium, n (%) | 43 (4) | 118 (21) |
| Strontium ranelate | 43 (4) | 118 (21) |
| Selective oestrogen-receptor modulator, n (%) | 102 (10) | 75 (13) |
| Raloxifene | 102 (10) | 75 (13) |
| Calcitonin, n (%) | 4 (0.4) | 8 (1) |
| Calcitonin | 4 (0.4) | 8 (1) |
| Others, n (%) | 4 (0.4) | 5 (0.9) |
| Hydroxyapatite | 3 (0.3) | 5 (0.9) |
| Disodium monoflurophosphate and calcium | 1 (0.1) | 0 |
| Parathyroid hormone | 0 | 6 (1) |
| Teriparatide | 0 | 6 (1) |
Patients could receive more than one medication so percentages may add up to >100%
aIncludes patients that have unknown/missing bone loss treatment
bIndicates the number of patients
Patient-reported outcomes
Figure 3 describes the pain and fatigue data for the PRO analysis set. Fifty-nine percent of women reported experiencing moderate to severe pain and 54% reported experiencing moderate to severe fatigue over the previous month. Reports of pain and fatigue were similar across cohorts.
Fig. 3.
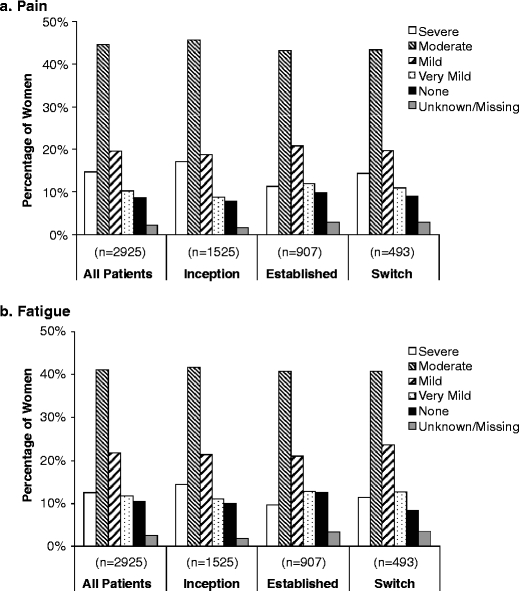
Percentages of women reporting pain and fatigue of various severities, based on the PRO analysis set. Patients graded their pain and fatigue over the past month according to a five-point scale (none, very mild, mild, moderate and severe) in response to the following questions: “During the past month, how would you describe the level of fatigue you usually experienced?” and “During the past month, how would you describe the level of pain usually experienced?”
Discussion
The cohort of postmenopausal women enrolled in POSSIBLE EU® describes a cross-section of the women who received bone loss treatment in five large European countries within the primary care setting between 2005 and 2008. Broad country-level comparisons of patient age, living arrangements and work status suggest variation in how patients are treated or selected for participation in the study, e.g. participants from Spain are younger and more likely to be employed, while participants from Germany are likely to be older and less likely to be employed. This may reflect differences in the health-care systems of the countries included in this study (e.g. in Spain, all bone loss medications are reimbursed whereas in Germany there are certain restrictions, such as the requirement for a DXA-based diagnosis, which, in turn, is only reimbursed in patients with prior fractures). Other factors that may contribute to the differences observed include country-specific treatment guidelines [11–15], physician attitudes about osteoporosis and the study design (e.g. how sites and investigators were selected).
In POSSIBLE EU®, 84% of the women with a diagnosis of low bone mass were diagnosed through imaging methods. Slightly more than half (55%) of all women were diagnosed using DXA. This contrasts with experience in the USA, where 71% of the 4,994 women enrolled in POSSIBLE US™ had a diagnostic DXA at, or before, study enrolment [6]. This is also in line with findings from a recent global study, which showed that the frequency of bone density testing was 51% in Europe compared with 85% in Canada [16]. Interestingly, in our study, although the German group had the lowest percentage of enrolees for whom DXA findings were available at the time of diagnosis, this group also contained the highest percentage of women with T scores in the osteoporosis range. This finding highlights that in certain parts of Europe, DXA may be used less often for initial case-finding and more often for documenting the level of bone mass in patients who have more severe, and possibly more apparent disease progression. The same may be true regarding the use of laboratory tests for the assessment of bone markers and vitamin D levels, which were rarely performed in this population. Another possibility for the underutilisation of DXA in certain European countries is that these patients may have been diagnosed using either DXA or computed tomography, a common means of diagnosis in local medical practice. As this was not an explicit option on the case report form, it may be that a high number of patients were reported as diagnosed using either X-ray (Table 2) or other means.
It has been suggested that osteoporosis treatment in the EU is generally triggered by either a prior fragility fracture or the identification of ‘significant’ risk factors [5]. Our data were somewhat in line with this suggestion, as 39% of the study population had at least one prior fracture. These data are also in agreement with other multinational European observational studies [17]. Inter-country variations, however, suggest that different paradigms or attitudes exist for determining when to initiate therapy. Interestingly, 31% of the women in whom DXA was performed had a diagnosis of osteopenia and, of these, 32% had a previous fracture; despite this, however, they were prescribed bone loss treatment. In most of these countries, access to bone loss treatment is restricted to those diagnosed with osteoporosis and/or prior fracture. This finding invites further investigation to better understand this observation.
Results from the sibling study, POSSIBLE US™, were recently published [6]. While broadly similar, the design of the two studies differs in a few key aspects, which include broad country differences given the geographic regions represented and differences associated with treatment by either specialists or GPs or by only GPs. Indeed, in POSSIBLE US™ the physicians selected for participation were the top 40% of office-based primary care physicians (including obstetrics/gynaecology) who prescribed medication for postmenopausal women with osteoporosis, whereas in POSSIBLE EU® physicians/sites were chosen only on the bases of their willingness to participate or if they represented their country across a broad range of characteristics. The two studies started nearly a year apart, with POSSIBLE EU® starting in December 2005 and POSSIBLE US™ in October 2004. Other differences in study design will inform the interpretation of data collected during the follow-up phases of each study. Compared with the women in POSSIBLE US™, the women in the EU® study are older and overall less healthy, with more substantial osteoporosis (mean minimum T score at diagnosis, −2.7 versus −2.1 [CI, −2.2, −2.1] in POSSIBLE US™). As expected with observational studies, patients in both of these studies differ from those who commonly participate in clinical trials, presenting with greater degrees of comorbidity and variability in prior treatment experience.
Women in POSSIBLE EU® reported moderate to severe pain and fatigue. Further exploration of the comorbidity data and health-related quality of life gathered in this study may provide useful insight into this disease state.
POSSIBLE EU® is one of the larger cohorts available for examining bone loss treatment in postmenopausal women in European countries. There are other ongoing/completed observation studies in Europe, but most of the more recent studies are country specific [18–20]. As this study is observational, it was designed to minimise the influence of the study on patient and physician behaviours. For example, there were no scheduled office visits for this study and, after consent was obtained, the only communication with participating patients was through mailed questionnaires and reminders. However, this study has certain limitations, mainly unquantifiable factors that may have affected either the physicians’ selection of patients for study recruitment or self-selection on the patients’ part to create a study population that may not fully represent the general population of interest. In addition, the process of site selection and measures used to remind participating patients may have contributed to bias. Furthermore, it is also likely that the ratio of newly treated, switching and established patients in the study cohort differs from that found in actual practice, although such differences should have little, if any, impact on our ability to address the primary objectives of this study, which are to examine relationships between patient characteristics and patient behaviours (e.g. medication adherence) and important outcomes (e.g. fractures, quality of life and treatment satisfaction).
In summary, POSSIBLE EU® is a large study aimed at describing the characteristics of postmenopausal women who received bone loss treatment in primary care practices in five European countries between 2005 and 2008. Use of DXA for diagnosis varied among countries, but was the main basis for a diagnosis of osteoporosis. The participants had substantial prevalence of fractures and pain. Future analyses will examine quality of life in greater detail, quantify medication adherence and identify key correlates (e.g. medication beliefs, treatment satisfaction and patient-reported side effects), characterise fractures and compare practice patterns across countries and with clinical guidelines.
Acknowledgments
The steering committee thanks the investigators and patients who contributed to this study. The steering committee comprises the following: Nick Freemantle (Chair), Cyrus Cooper, Adolfo Díez-Pérez, Francis Guillemin, Rob Horne, Bengt Jonsson, Luc Martinez, Sergio Ortolani, Johannes Pfeilschifter and Christian Roux.
The study was funded by Amgen Ltd, UK. Helen M. Wilfehrt, PhD, Amgen (Europe) GmbH, Switzerland and Sally Wade, Wade Outcomes Research and Consulting, Salt Lake City, UT, USA, assisted the authors in writing this manuscript. Valerie Easton, formerly of Amgen Ltd, Cambridge, UK, contributed statistical assistance. Alison Dobson of Amgen Ltd, Cambridge, UK, provided statistical programming support.
Disclosures
NF has received funding for research, consulting and or travel from Amgen, Eli Lilly, Servier, Pfizer and Sanofi Aventis. CC has recieved consultancy/advisory committee fees from Servier, Proctor and Gamble/Alliance, Eli Lilly, Merck, Sharp and Dohme, GSK/Roche, Amgen, Novartis. CR has received research grants and/or honoraria from Amgen, Alliance, MSD, Novartis, Roche and Servier. ADP has served as a speaker and consultant for Amgen. BJ has received funding for advisory boards from Amgen. SO has received funding for advisory boards from Amgen, consulting fees and grant/research support from the Institut International de Recherche Servier, speakers fees from GlaxoSmithKline and grant research/support from Nycomed. JP has received research grants/support for clinical studies from Amgen, GE Lunar, Roche Diagnostics and Novartis; consultancy or advisory committee fees from Amgen, GlaxoSmithKline, MSD Sharp & Dohme, Novartis, Nycomed, Procter & Gamble, Roche, Servier and Teva; and honorary fees for lectures from Amgen, Daiichi Sankyo, GE Lunar, GlaxoSmithKline, MSD Sharp & Dohme, Novartis, Nycomed, Orion Pharma, Procter & Gamble, Roche, Roche Diagnostics Servier and Teva. RH has received consultancy, advisory committee fees or educational grants from Amgen, GSK, Shire, Hayward Medical Communications, Proctor & Gamble, Gilead, Merck, Astrazeneca, Pfizer, Astellas, Novartis and Boehring Ingleheim. LM has received consultancy fees from Amgen, Sanofi, Pfizer, Roche and Novonordisk. SK, SS, GM and AM are employees of Amgen. The other authors have no conflicts of interest to declare.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
References
- 1.Siris ES, Bilezikian JP, Rubin MR, et al. Pins and plaster aren't enough: a call for the evaluation and treatment of patients with osteoporotic fractures. J Clin Endocrinol Metab. 2003;88:3482–3486. doi: 10.1210/jc.2003-030568. [DOI] [PubMed] [Google Scholar]
- 2.Roux C, Briot K, Horlait S, Varbanov A, Watts NB, Boonen S. Assessment of non-vertebral fracture risk in postmenopausal women. Ann Rheum Dis. 2007;66:931–935. doi: 10.1136/ard.2006.064071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.International Osteoporosis Foundation (2008) Osteoporosis in the European Union in 2008: ten years of progress and ongoing challenges. Available at http://www.iofbonehealth.org/publications/eu-policy-report-of-2008.html. Accessed 8 April 2009
- 4.Seeman E, Compston J, Adachi J, et al. Non-compliance: the Achilles' heel of anti-fracture efficacy. Osteoporosis Int. 2007;18:711–719. doi: 10.1007/s00198-006-0294-8. [DOI] [PubMed] [Google Scholar]
- 5.Kanis JA, Burlet N, Cooper C, et al. European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int. 2008;19:399–428. doi: 10.1007/s00198-008-0560-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Barrett-Connor E, Ensrud K, Tosteson A, et al. Design of the POSSIBLE US™ study: postmenopausal women’s compliance and persistence with osteoporosis medications. Osteoporosis Int. 2009;20:463–472. doi: 10.1007/s00198-008-0674-3. [DOI] [PubMed] [Google Scholar]
- 7.Brooks R. EuroQol: the current state of play. Health Policy. 1996;37:53–72. doi: 10.1016/0168-8510(96)00822-6. [DOI] [PubMed] [Google Scholar]
- 8.The EuroQol Group EuroQol—a new facility for the measurement of health-related quality of life. Health Policy. 1990;16:199–208. doi: 10.1016/0168-8510(90)90421-9. [DOI] [PubMed] [Google Scholar]
- 9.EuroQol Group EQ-5D. In. EuroQol Group Rotterdam, The Netherlands
- 10.Silverman S. The Osteoporosis Assessment Questionnaire (OPAQ): a reliable and valid disease-targeted measure of health-related quality of life (HRQOL) in osteoporosis. Qual Life Res. 2000;9:767–774. doi: 10.1023/A:1008934208764. [DOI] [Google Scholar]
- 11.Guideline for prevention and treatment of Op SINOSSI. Available at http://www.siommms.it. Last accessed 12 March 2009
- 12.Agence Francaise de Securite Sanitaire des Produits de Sante. Available at http://www.afssaps.fr/var/afssaps_site/storage/original/application/2f4831c7ee9d9bd6fda336a26b6500c6.pdf Last accessed 17 April 2009
- 13.Evidenz-basierte Konsensus-Leitlinien zur Osteporose (2009) Available at http://www.dv-osteologie.org/. Last accessed 17 April
- 14.National Institute for Health and Clinical Excellence (NICE) (2009) Available at http://www.nice.org.uk/guidance/index.jsp?action=byID&r=true&o=11621. Last accessed 14 April
- 15.Sociedad Española de Investigaciones Óseas y Metabolismo Mineral - SEIOMM (2009) Available at http://www.seiomm.org/documentos/osteoporosis_es_en.pdf. Last accessed 14 April
- 16.Lindsay R, Delmas P, Boonen S, Diez-Perez A, Dedrick R, Saag KG (2008) Regional differences in the management of osteoporosis in women. ASBMR abstract book 2008. SU287
- 17.Jakob F, Marín F, Martin-Mola E, et al. Characterization of patients with an inadequate clinical outcome from osteoporosis therapy: the Observational Study of Severe Osteoporosis (OSSO) QJM. 2006;99:531–543. doi: 10.1093/qjmed/hcl073. [DOI] [PubMed] [Google Scholar]
- 18.Sornay-Rendu E, Munoz F, Garnero P, Duboeuf F, Delmas PD. Identification of osteopenic women at high risk of fracture: the OFELY study. J Bone Miner Res. 2005;20:1813–1819. doi: 10.1359/JBMR.050609. [DOI] [PubMed] [Google Scholar]
- 19.Díez-Pérez A, González-Macías J, Marín F, et al. Prediction of absolute risk of non-spinal fractures using clinical risk factors and heel quantitative ultrasound. Osteoporos Int. 2007;18:629–639. doi: 10.1007/s00198-006-0297-5. [DOI] [PubMed] [Google Scholar]
- 20.Adami S, Isaia G, Luisetto G, et al. Osteoporosis treatment and fracture incidence: the ICARO longitudinal study. Osteoporos Int. 2008;19:1219–1223. doi: 10.1007/s00198-008-0566-6. [DOI] [PubMed] [Google Scholar]


