Abstract
This study examined reasons for non-use of condoms among an online survey sample of 462 non-condom using MSM to 1) identify major domains, themes and categories encompassing reasons for non-use of condoms, and 2) examine whether reasons varied by role-in-sex (insertive or receptive) and meeting venue (online or offline). A thematic analysis was completed on participant responses to an open-ended question about reasons for non-condom use. Preference for not using condoms and contextual factors were the top two reasons given for not using condoms, followed by a reasoned judgment based on risk assessment, relationship status and interpersonal communication. No major differences were found between men who reported non-condom use at last receptive and insertive anal intercourse. By contrast when meeting online, men were more likely to report reasons for non-condom use that corresponded to individual preference and mutual agreement not to use condoms. When meeting offline, men were more likely to cite reasons related to context and relationships. In developing HIV prevention interventions for this population, researchers should address both venues separately, as reasons why men engage in non-use of condoms appear to differ.
Keywords: Men who have Sex with Men, condom use, sex roles, Internet
Introduction
In the USA, HIV/AIDS cases among Men-who-have-Sex-with-Men (MSM) have been increasing, with MSM accounting for over half (53%) of all reported HIV infections in 2006 (Centers for Disease Control 2008; Hall et al. 2008). Sexual risk-taking behaviour, such as engaging in unprotected anal intercourse (UAI), poses a high risk for contracting HIV. Although condoms are known to be effective in reducing the risk of transmission, high proportions of MSM continue to report non-use or inconsistent use of condoms (Sanchez et al. 2006; Osmond et al. 2007; Truong et al. 2006; Carter 2007). Given the changing landscape of sexual exchanges (e.g., the emergence of the Internet for sex seeking) and HIV (e.g., the availability of highly active antiretroviral therapies), there is a continuing need to update understanding of factors associated with non-use or inconsistent use of condoms among MSM.
In a review of research from the 1990s on the behavioural response of MSM to the AIDS epidemic, Stall et al. (2000) suggested that variables associated with sexual risk-taking behaviour among MSM could be organised into three categories: individual, interpersonal, and situational/societal. More recent research also reflects these three categories.
Individual factors are determinants that are unique to each individual, such as demographic characteristics, mental health factors, and personal beliefs about sexual pleasure. High rates of UAI have been found, for instance, among young Internet-using MSM (Horvath, Rosser and Remafedi 2008), less educated MSM (Denning and Campsmith 2005), and HIV-positive MSM (Holtgrave, Crosby and Shouse 2006). Unprotected receptive anal intercourse (URAI) among HIV positive MSM has been associated with less anxiety and greater loneliness than unprotected insertive anal intercourse (UIAI) (Parsons et al. 2003). Frequently mentioned reasons among MSM for non-condom use include dislike of condoms, enjoyment of skin-to-skin feeling and concern about diminished pleasure (Carballo-Diéguez and Bauermeister 2004).
Interpersonal factors occur between sexual partners that predict sexual practices, such as relationship status, intimacy issues, and interpersonal communication. Wolitski and others (2003) found that MSM in regular relationships felt a responsibility to protect the health of their partners by practicing safer sex, which may extend to non-primary partners (Klausner et al. 2006). However, other studies associate a heightened level of intimacy in primary relationships with sexual risk-taking behaviour (Theodore et al. 2004). Interpersonal communication about condom use and HIV status is associated with lower rates of UAI (Horvath, Oakes and Rosser 2008; Wilson et al. 2008), however inconsistent disclosure and ascertainment of HIV status appears more risky than consistently adopting or not adopting a strategy (Horvath, Nygaard and Rosser 2009; Parsons et al. 2005).
Situational/societal factors are contextual determinants of risky sexual behaviour. Alcohol and/or drug use before or during sex, for example, can be major predictors of risky sexual encounters (Hirshfield et al. 2004; McKirnan et al. 2001; Holtgrave et al. 2006; Wilson et al. 2008; Hirshfield, Remien and Chiasson 2006; Miamiaga et al. 2008). Unavailability or breakage of condoms have also been cited as obstacles to condom use (Carballo-Diéguez and Dolezal, 1996).
While individual, interpersonal and situational variables involved in non-condom use have been well-researched in offline studies, they have not been established in online HIV prevention studies. In addition, two under-researched areas include whether non-use of condoms varies by role-in-sex (receptive or insertive) and meeting venue (online or offline).
Increased awareness among MSM of HIV status and variation in risk potentially makes role-in-sex an important factor in decisions about whether to use condoms. URAI poses a higher risk for contracting HIV than UIAI (Detels et al. 1989). Knowledge of this may influence individual perceptions of HIV risk and affect condom use behaviour (Parsons et al. 2003; Belcher et al. 2005). Some HIV-positive MSM assume the role of receptive partner to reduce risk of HIV transmission, a strategy termed ‘strategic positioning’ (Van de Ven et al. 2002; Remien, Carballo-Diéguez and Wagner 1995; Valdiserri et al. 1988).
Seeking sex online has been associated with more sexual risk-taking behaviour than seeking sex in traditional venues (Benotsch, Kalichman and Cage 2002; Liau, Millett and Marks 2006; Rosser et al. 2009a, 2009b). Men who seek sex online appear younger, more likely to have a STI, less likely to identify as gay, and more likely to be polysubstance users (Grov, Parsons and Bimbi 2007; Mimiaga et al. 2008). Meeting partners online for sex has also been associated with methamphetamine use, higher numbers of sexual partners, and higher rates of UAI (Benotsch, Kalichman and Cage 2002; Liau, Millett and Marks 2006). Other researchers conclude that meeting venue may not be as important in determining risky sexual behaviour as other factors, and that the Internet may have little or no influence on UAI (Mettey et al. 2003; Bolding et al. 2005). A further complication is that many MSM may seek sexual partners both online and offline, providing greater opportunity to engage in UAI (Horvath, Rosser and Remafedi 2008). Given the contradictory evidence there is need for further study of differences in sexual risk-taking behaviour by meeting venue.
In this study, we report the results of reasons for non-use of condoms among an online sample of non-condom using MSM from the Men’s INTernet Sex (MINTS-II) study. Our primary aims were to: 1) identify domains, themes, and categories of reasons for non-use of condoms reported by a large sample of Internet-using MSM, and 2) examine whether reasons varied by two key factors: role-in-sex (insertive or receptive) and meeting venue (online or offline). We wanted to update understanding of reasons for non-use of condoms among MSM using an online survey, with its practical advantages of greater anonymity, reduced potential for social desirability bias, and recruiting a large sample of men nationally (Zhang et al. 2008). Given that previous research has suggested sexual risk behaviour may be influenced by individual perceptions of HIV risk (Parsons et al. 2003; Belcher et al. 2005) and differences in online and offline sex-seeking (Benotsch, Kalichman and Cage 2002; Liau, Millett and Marks 2006; Rosser et al. 2009a, 2009b), we also wanted to explore variations in reasons for non-condom use by sexual role and meeting venue as part of formative research to inform Internet-based HIV prevention intervention development. We also hoped to advance understanding of online cultures, specifically among men who use the Internet to seek sex with men.
Methods
Participants
This study uses data from the Men’s INTernet Sex (MINTS-II) study, a large online survey of 2716 MSM conducted by researchers at the University of Minnesota. The sample comprises 462 of 546 men (85%) who reported not using a condom in their last sexual encounter and provided reasons for non-condom use. Participants ranged in age from 18 to 65 (Table 1). The sample was racially diverse; most had more than a high school education; 42 (9.1%) reported a diagnosis with HIV.
Table 1.
Demographic characteristics of sample (N=462)
| N(%) | |
|---|---|
| Gender | |
| Male | 459(99.4) |
| F2M | 3(0.6) |
| Age | |
| 18–25 | 183(39.6) |
| 26–29 | 96(20.8) |
| 30–39 | 124(26.8) |
| 40–49 | 45(9.7) |
| 50–59 | 13(2.8) |
| 60+ | 1(0.2) |
| Race | |
| Asian | 66(14.3) |
| Black | 86(18.6) |
| Latino | 123(26.6) |
| White | 119(25.8) |
| Other | 68(14.7) |
| Education | |
| <12 years | 17(3.7) |
| 12–15 years | 205(44.4) |
| 16 years | 138(29.9) |
| 16 + years | 101(21.9) |
| HIV Diagnosis | |
| No | 415(89.8) |
| Yes | 42(9.1) |
Percentages reflect incomplete data for 5 participants
Procedures
Participants were recruited to the MINTS-II study using banner advertisements on the website gay.com. A full description of study methods is reported elsewhere (Rosser et al. 2009a). To be eligible for participation, individuals needed to identify themselves as male, 18 years or older, living in the USA and having engaged in sex with another man in their lifetime. Eligible participants completed an online survey consisting of up to 170 questions. Data collection occurred between June and September 2005.
Measures
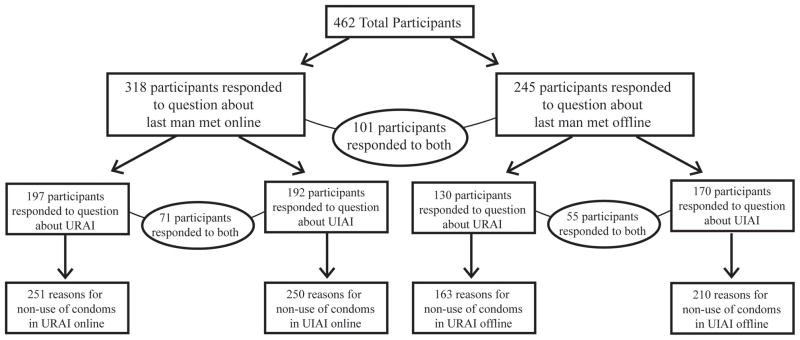
The participant sample for this study was derived from a series of questions on the MINTS-II survey that began by asking men to recall the last time they met a man for sex in each of two venues: “via the internet” and “not via the internet.” To control for order effects, the presentation was randomised so that half were presented with the online venue first and the other half the offline venue first. Follow-up questions employed automatic branching and skip patterns to probe, depending on the previous answer, the underlying conditions of each participant’s sexual encounter. In this way the pool was narrowed further by participants’ responses to specific questions that identified those who had engaged in UIAI and URAI. These participants were then asked whether they or their partner used a condom, and if the response was “no”, they were asked to answer the key open-ended question for this study: “why not?” Thus, we were able to examine responses about reasons for non-use of condoms for each of four separate scenarios: ‘online/URAI,’ ‘online/UIAI,’ ‘offline/URAI,’ and ‘offline/UIAI’ (Figure).
Figure.
Participant Flow Diagram
Analyses
A thematic analysis was completed by hand on responses to the open-ended question. Separate analyses were performed for each of the four scenarios. Rather than assume an individual, interpersonal and contextual framework, repeating ideas were identified and responses were organised into categories. In cases where responses contained multiple reasons, each reason was assigned to its relevant category.
Inter-rater reliability was assessed. A second rater independently coded all responses for each of the four scenarios. Wide coding discrepancies between raters were discussed until a consensus was reached and codes were revised. Inter-rater agreement was 97.6% (offline/URAI), 98.0% (offline/UIAI), 97.4% (online/URAI) and 94.4% (online/UIAI).
Categories were organised into themes, and themes into domains. These groupings were re-evaluated and finalised. Comparisons were conducted using a content analysis approach which employs counts and percentages to determine the relative importance of statements and ideas. Two-sample chi-square tests were performed using R statistical software to assess proportional differences in reasons for non-use of condoms by meeting venue and sexual role, applying Yates’ continuity correction for values under 10.
Results
A total of 462 participants provided reasons for non-use of condoms. Among participants who met their last partner online, 197/218 (90%) provided a reason for non-use during URAI and 192/213 (90%) provided a reason for non-use during UIAI. For those who met their last partner offline, 130/190 (68%) provided a reason for non-use during URAI and 170/201 (85%) provided a reason for non-use during UIAI.
Most respondents gave a single reason; some provided multiple reasons. Responses averaged 15 words and ranged from short two-word expressions to several sentences. Shorter responses were often easier to code than longer responses, which could be complex and coded into more than one category. Responses that were nonsensical (e.g., “we had sex spac [sic] without condoms”), tangential to the question (e.g., “1st time. 2 other time no.”), or did not fall into a specific category or theme (e.g., “It was a couple and I did not realise at first one of them did not use a condom”), were placed in a miscellaneous category.
Domains, Themes and Categories
At the highest level, the three domains common to offline studies also emerged from our data: Individual, Contextual and Interpersonal. The individual domain had the highest proportion of reasons for non-condom use, followed by the contextual and interpersonal.
Within domains, responses clustered into seven themes: (i) Individual Preference, (ii) Assessment of Risk, (iii) Didn’t worry or think about it, (iv) Time and Situation, (v) Relationship and Trust, (vi) Interpersonal Communication and Dynamics, and (vii) Love, Intimacy and Desire. Within some themes, responses were further broken down for comparative analysis into categories (Tables 2 and 3). Across the comparisons (online vs. offline, URAI vs. UIAI), individual preference and contextual factors were the top two thematic reasons, followed by a reasoned judgment based on risk assessment, relationship status and interpersonal communication.
Table 2.
Comparison of Receptive and Insertive Role-in-Sex (N=462)
| URAI n(%theme) | UIAI n(%theme) | URAI n(%total) | UIAI n(%total) | χ2 | |
|---|---|---|---|---|---|
| A. INDIVIDUAL DOMAIN | 195(47) | 226(49) | 0.36 | ||
| (i)Individual Preference | 103(25) | 137(30) | 2.63 | ||
| Didn’t want to use a condom | 44(43) | 53(39) | 0.40 | ||
| Feel and comfort | 26(25) | 41(30) | 0.64 | ||
| Preference for bareback | 27(26) | 27(19) | 1.43 | ||
| Sexual difficulty, loss of erection or latex allergy | 6(6) | 16(12) | 1.77† | ||
| (ii)Assessment of Risk | 82(20) | 74(16) | 2.06 | ||
| Knew HIV status/Believed or confirmed HIV negative | 53(65) | 51(69) | 0.32 | ||
| HIV positive status | 7(9) | 8(11) | 0.04† | ||
| Coitus interruptus | 16(19) | 8(11) | 1.64† | ||
| New on the block/First sexual experience | 6(7) | 3(4) | 0.28† | ||
| Lower risk for insertive partner | 0(0) | 4(5) | 2.64† | ||
| (iii)Didn’t worry or think about it | 10(2) | 15(3) | 0.56 | ||
| B. CONTEXTUAL DOMAIN | 103(25) | 106(23) | 0.40 | ||
| (iv)Time and Situation | 103(25) | 106(23) | 0.40 | ||
| In the heat of the moment | 42(41) | 46(43) | 0.15 | ||
| Availability of condoms | 40(39) | 40(38) | 0.03 | ||
| Condom broke or slipped off | 2(2) | 2(2) | 0.23† | ||
| Alcohol and/or drug use | 19(18) | 18(17) | 0.08 | ||
| C. INTERPERSONAL DOMAIN | 89(21) | 86(19) | 1.07 | ||
| (v)Relationship and Trust | 45(10) | 51(11) | 0.01 | ||
| In a monogamous relationship | 7(16) | 6(12) | 0.29† | ||
| In a relationship that may or may not be monogamous | 5(11) | 5(10) | 0.04† | ||
| Familiarity, Trust and Reciprocity | 33(73) | 40(78) | 0.34 | ||
| (vi)Interpersonal Communication and Dynamics | 27(7) | 20(5) | 2.02 | ||
| Resistance from partner | 0(0) | 4(20) | 3.61† | ||
| Mutual agreement | 12(44) | 9(45) | 0.07† | ||
| No discussion | 15(56) | 7(35) | 1.21† | ||
| (vii)Love, Intimacy and Desire | 17(4) | 15(3) | 0.44 | ||
| MISCELLANEOUS | 27(7) | 42(9) | 2.04 | ||
| TOTALS | 414(100) | 460(100) | |||
Note: Some responses included multiple reasons, which is reflected in the total number of reasons categorised; percentages are rounded to the nearest whole number; N=number of participants; n= number of reasons;
P<0.05;
Yates’ continuity correction was used for values under 10.
Table 3.
Comparison of Online and Offline Meeting Venue (N=462)
| Online | Offline | ||||
|---|---|---|---|---|---|
| n(%theme) | n(%total) | n(%theme) | n(%total) | χ2 | |
| A. INDIVIDUAL DOMAIN | 260(52) | 161(43) | 6.53* | ||
| (i)Individual Preference | 151(30) | 89(24) | 4.23* | ||
| Didn’t want to use a condom | 63(42) | 34(38) | 0.29 | ||
| Feel and comfort | 39(26) | 28(32) | 0.88 | ||
| Preference for bareback | 36(24) | 18(20) | 0.42 | ||
| Sexual difficulty, loss of erection or latex allergy | 13(8) | 9(10) | 0.03† | ||
| (ii)Assessment of Risk | 96(19) | 60(16) | 1.38 | ||
| Knew HIV status/Believed or confirmed HIV negative | 59(62) | 45(75) | 3.05 | ||
| HIV positive status | 10(10) | 5(8) | 0.02† | ||
| Coitus interruptus | 17(18) | 7(12) | 0.62† | ||
| New on the block/First sexual experience | 7(7) | 2(3) | 0.46† | ||
| Lower risk for insertive partner | 3(3) | 1(2) | 0.002† | ||
| (iii)Didn’t worry or think about it | 13(3) | 12(3) | 0.30 | ||
| B. CONTEXTUAL DOMAIN | 108(22) | 101(27) | 3.58 | ||
| (iv)Time and Situation | 108(23) | 101(27) | 3.58 | ||
| In the heat of the moment | 54(48) | 34(34) | 5.71* | ||
| Availability of condoms | 41(38) | 39(39) | 0.009 | ||
| Condom broke or slipped off | 4(4) | 0(0) | 2.10† | ||
| Alcohol and/or drug use | 9(10) | 28(28) | 12.17**† | ||
| C. INTERPERSONAL DOMAIN | 95(19) | 80(22) | 0.83 | ||
| (v)Relationship and Trust | 44(9) | 52(14) | 5.82* | ||
| In a monogamous relationship | 3(14) | 10(19) | 2.17† | ||
| In a relationship that may or may not be monogamous | 6(14) | 4(8) | 0.56† | ||
| Familiarity, Trust and Reciprocity | 35(72) | 38(73) | 0.14 | ||
| (vi)Interpersonal Communication and Dynamics | 32(6) | 15(4) | 2.35 | ||
| Resistance from partner | 2(0) | 2(13) | 0.06† | ||
| Mutual agreement | 18(65) | 3(20) | 4.06*† | ||
| No discussion | 12(35) | 10(67) | 3.49 | ||
| (vii)Love, Intimacy and Desire | 19(4) | 13(3) | 0.06 | ||
| MISCELLANEOUS | 38(7) | 31(8) | 0.16 | ||
| TOTALS | 501(100) | 373(100) | |||
Note: Some responses included multiple reasons, which is reflected in the total number of reasons categorised; percentages are rounded to the nearest whole number; N=number of participants; n= number of reasons;
P<0.05,
P < 0.001;
Yates’ continuity correction was used for values under 10.
Individual Domain
Theme 1: Individual Preference
Personal or partner preferences for not using condoms fell into four distinct categorical patterns. The first, Didn’t want to use a condom, describes a general preference for sex without condoms, and includes statements such as, ‘Didn’t want to use one’ and ‘because I don’t like them.’ The second category, Feel and comfort, includes more detailed statements of preference. Examples include statements of displeasure with the feel of condoms (e.g., ‘he did not like the feeling of condoms’), emphasis on the sensation of sex without a condom (e.g., ‘[It] Feels better... more Sensation’; ‘I am turned on by bringing my partner to orgasm. He is able to get there faster without a condom. And I really like the feeling of a bare penis over a condomed [sic] penis’), or reports of discomfort with condoms (e.g., ‘we started with a condom but it was uncomfortable for him so i [sic] removed it’). The third category, Preference for bareback, includes statements like ‘I enjoy barebacking’ and ‘we both agreed not too [sic] he was into bare back and so am I’. A final category, Sexual difficulty, loss of erection or latex allergy, was used to code responses when participants complained of erectile difficulty (e.g., ‘i [sic] cant use them i [sic] go soft’) or latex allergy/sensitivity when using condoms (e.g., ‘His anus is extremely sensitive to latex.’).
Theme 2: Assessment of Risk
Responses here indicated a reasoned judgement based on factors that participants perceived as lessening their risk of contracting HIV. These responses were often descriptive and complex, offering several reasons why condoms were not used or why it was low risk:
We have had sex in the past multiple times, I trusted him with being truthful about his HIV status (negative), and I know my risk of exposure to HIV infection as an unprotected top is significantly low. In addition to the fact that I prefer to have sex without using a condom for reason of increased pleasure and sensation.
Five distinct categories emerged. The first, Knew HIV status/Believed or confirmed HIV negative, included respondents who knew their HIV status without specifying whether they were HIV positive or negative (e.g., ‘We both know our HIV status and wanted the pleasure.’), believed their partner was HIV negative (e.g., ‘He told me he was HIV- and I believed him.’), and had recently been confirmed HIV negative (e.g., ‘he showed me his papers for HIV testing-he got tested every 3 months’). Negotiated safety was also observed in some responses (e.g., ‘After a while of being monogomous [sic] and having been tested we quit using condoms’). A second category, HIV positive status, included responses that indicated knowledge that both partners were HIV positive (e.g., ‘because he’s positive and i’m [sic] positive so we decided for him not to use a condom’). Responses that indicated reliance on withdrawal before ejaculation (e.g., ‘had him pull out before cumming and he was hardly precumming’) made up a third category, Coitus interruptus. A fourth category, New on the block/First sexual experience, consisted of respondents who didn’t use a condom because it was the first time they or their partner had sex, or they were new to the ‘gay scene’ (e.g., ‘never had sex and was new to the expereince [sic]’; ‘I wasnt [sic] thinking about AIDS and I was new in the Gay Lifestyle. I didnt [sic] have anyone to guide me.’). The responses of several men who stated that condom use was unnecessary because ‘topping’ reduced the risk of HIV infection were placed in a fifth category, Lower risk for insertive partner.
Theme 3: Didn’t worry or think about it
A third theme within the individual domain we attributed to a small proportion of responses that may suggest less concern over possible long-term effects of HIV or sexually transmitted infections. Examples included: ‘Back then, didn’t worry about it.’ and ‘General stupidity, didn’t think about it.’.
Contextual Domain
Theme 4: Time and Situation
This theme consists of four categories that were external to the respondent and his ability to control his own behaviour: In the heat of the moment, Availability of condoms, Condom broke or slipped off and Alcohol and/or drug use.
Some men were caught up in the moment, situation or mood (e.g., ‘we did not have time’; ‘It happened very fast in a hot tub, he made the move’). Others cited the ‘spontaneity’ of sex in a specific situation.
We were being rather rough and wrestling around when he pinned me. Then his penis pressed against my hole and he playfully teased me, before long we were in an all out fuck session.
Some respondents referred to an unavailability of condoms (e.g., ‘Condom in the car’), condom failure (e.g., ‘tried to but condom broke’) and/or the influence of drugs and/or alcohol.
No real answer I guess. When we talked on the phone we were all about using protection, but when we got to his bed we were drunk. It had crossed my mind but I didn’t push the issue.
Interpersonal Domain
Theme 5: Relationship Status
This theme consists of three categories. Responses that emphasised Being in a monogamous relationship were separated from those that did not specify an exclusive, committed relationship. The category In a relationship that may or may not be monogamous includes responses such as ‘He is my partner’ and ‘we had been dating for several months before it progressed to fucking.’ The category Familiarity, trust and reciprocity includes reasons pertaining to trust in one’s partner, or knowledge of a person through a mutual friend or talking online or on the phone. Also included are responses about the reciprocity of non-use (e.g., ‘I had originally fucked him without a condom so it became a moot point’).
Theme 6: Interpersonal Communication and Dynamics
Three categories comprise this theme. Resistance from partner includes statements such as, ‘he pulled it off’ or ‘we didn’t have anal sex. he put my penis inside of him but I stopped it.’ A second category, Mutual agreement, includes respondents who communicated directly with their partner about condom use and mutually agreed not to use a condom (e.g., ‘We made an agreement it would be without a condom beforehand.’). A third category, No discussion, includes cases where condoms were never discussed (e.g., ‘the use of a condom wasn’t brought up.’)
Theme 7: Love, Intimacy and Desire
Reasons that pertained to love, mutual affection, attraction, desire and fantasy appear uncategorised under this theme as no clear breakdown emerged. One respondent stated ‘we were too horny,’ and another ‘He chose not to and I did not object, because I viewed him as sexy, and I wanted him anyway he was willing to give himself to me.’ Other respondents referred to love and intimacy:
Probably because he stated that he enjoyed it better without a condom, and I was in love with him, so I allowed him to do it without a condom. There is a heightened sensation without a condom, so it is better enjoyed by both partners, it is a more intimate act.
Comparison of Reasons for Non-use of Condoms across Sexual Role and Meeting Venue
There were no statistically significant differences in reasons for non-use of condoms by sexual role. However, there were significant differences between reasons among men who first met online versus offline. Men who first met online offered proportionately more reasons that fell into the individual domain than men who met offline (χ2(1, N = 874) = 6.53, p<.05) and also cited proportionately more reasons of individual preference (χ2(1, N = 874) = 4.23, p<.05). Assessment of HIV risk was important to both groups, although as a general trend men who met offline more often mentioned reasons that were categorised as knew HIV status/believed or confirmed HIV negative. Men who met offline were somewhat more inclined to provide reasons that fell into the contextual domain, and offered a significantly higher proportion of reasons categorised as alcohol and/or drug use (χ2(1, N = 209) = 2.17, p<.001). Men who met online, however, were proportionately more likely to mention the contextual reason of being in the heat of the moment (χ2(1, N = 209) = 5.71, p<.05). There was little difference overall with respect to the interpersonal domain, but at the thematic level men who met offline provided a significantly higher proportion of reasons having to do with relationship and trust (χ2(1, N = 874) = 5.82, p<.05). Additionally, within the interpersonal communication and dynamics theme, men who met online reported a significantly higher proportion of reasons categorised as mutual agreement than men who met offline (χ2(1, N = 47) = 4.06, p<.05).
Discussion
There were two aims of this study. The first was to identify major reasons for non-use of condoms among MSM. Our study identified seven thematic reasons which we further collapsed into three domains (individual, contextual, interpersonal). The results highlight the importance of individual factors in decisions not to use condoms. It is clear that some individuals enter a sexual experience with negative preconceived ideas about condoms based on past experience and personal preference. For others, a reasoned judgment based on perception of risk takes place. In cases where perceived risk is low, harm reduction strategies involving HIV serodisclosure, serosorting, strategic positioning, and negotiated safety are, as reported in other studies, being used instead of condoms (Belcher et al. 2005; Van de Ven et al. 2002; Holtgrave, Crosby and Shouse 2006). Contextual factors, such as acting in the heat of the moment, condom availability, and substance use, are also influential and of similar importance to interpersonal factors.
While we have sought to disentangle the reasons for non-condom use in order to map a general landscape that we hope will inform the development of HIV prevention interventions, it’s important to point out that the domains, themes and categories identified are not mutually exclusive and interactions and overlap may occur between them. A full understanding of the dynamic interplay of reasons that underlie non-use of condoms among MSM will require further research.
From the breath of reasons given by MSM in this study, it’s clear that no one reason adequately explains why some MSM fail to use condoms. HIV prevention interventionists interested in developing inventories of reasons for non-condom use should consider using as their basis, the seven thematic reasons identified in this study, possibly with examples from some of the subcategories. Some researchers have already made significant progress in developing and testing offline cognitive behavioural therapy based HIV/AIDS intervention strategies based on self-justifications supplied by MSM to explain their non-use of condoms during UAI (Gold and Rosenthal 1998; Dilley et al. 2007). With increasing use of the Internet by MSM seeking sexual partners there is a need for online interventions that can reach large numbers of at-risk MSM. The reasons for non-condom use identified in this study should be of value in the design of such online HIV risk reduction interventions.
Our second aim was to expand the literature on reasons for non-condom use by examining two under-studied areas: whether reasons varied by role-in-sex and by online/offline venue. While a number of studies have focused on differential rates of URAI and UIAI (Parsons et al. 2003; Van de Ven et al. 2002; Valdiserri et al. 1988), to our knowledge few have examined differences in reasons for non-condom use by role-in-sex. This analysis went beyond looking at rates of risk behaviour to try to understand men’s beliefs about why they or their partner didn’t use a condom. Surprisingly, no significant differences were found between men who reported non-condom use at last URAI and UIAI. We recommend that future HIV prevention interventions continue to regard MSM who engage in URAI and UIAI as one target population.
By contrast some differences were identified between men who reported non-use of condoms with last partner first met online or offline. Specifically, more responses among men who met online were categorised as Individual Preference, which may suggest that when meeting partners online, the men in this study focussed more on their own preferences or their partner’s preferences, including the sensory aspects of sex or the kind of sexual experience. Halkitis, Parsons and Wilton (2003) have shown that most men who seek partners for the purpose of barebacking believe the Internet is the most popular and effective way of doing so. Others, too, have found that men who seek partners for UAI are more likely to do so online (Liaue, Millet, and Marks, 2006).
Additionally, more respondents who met partners online reported a mutual agreement not to use condoms. One possible explanation is that men who prefer condomless sex and seek partners online may choose men with profiles stating preference for unprotected sex, or negotiate unprotected sex. Put another way, at least two distinct online cultures may be emerging, one which emphasises safer sex, and the other (seen in ‘barebacking’ sites) which emphasises condomless sex. Depending on where an MSM looks online, he may experience dramatically different attitudes toward condom use.
The finding that participants who met their last partner offline were more likely to cite drug and alcohol use could reflect the context in which partners met – for instance, the men in this study who met at a party or bar may have been more exposed to alcohol and drug use than those who met online and later had to travel to meet for sex.
One curious finding was the lower response rate among men who met offline and engaged in URAI. While no evidence explains this difference, we can speculate that men who met through traditional venues and engaged in URAI may have had less of an idea as to why their partner did not use a condom than men who sought out a partner online with similar preferences. It could again be a result of two different cultures. It may be that online sex seeking is a more deliberate process which includes detailing profiles including the degree of condom use preferred. By contrast, meeting offline may involve a more intuitive culture where men might find themselves in situations where sex occurs (supposedly) without pre-meditation.
While we can speculate about the various circumstances behind these venue-specific findings, more research is needed to explore these differences in depth. In developing HIV prevention interventions for this population, we believe researchers should address both venues separately since the reasons for non-condom use appear to differ by venue.
As our data shows, responses to this online survey, which is one of the first and largest conducted, are clearly interpretable and analysable. The open-ended questions, which were answered by respondents in privacy and under conditions of their own choosing, allowed for a certain richness and depth of reflection. The anonymity of participants when discussing a sensitive topic was also a major advantage. The short and choppy nature of some responses, characteristic of qualitative Internet data (Ross et al. 2007), made for easy coding. Additionally, online surveys have the advantage, as has been pointed out elsewhere (Zhang et al. 2008), of rapidly collecting large amounts of data from many respondents.
Limitations
There were at least six limitations to this study. First, because respondents are unable to ask questions during online surveys, questions may occasionally be misinterpreted. For example, even though respondents were specifically asked about non-condom use during URAI and UIAI, three indicated they hadn’t used condoms because they engaged in oral sex; another because he was rimming (‘Listen if I’m rimming WHAT [sic] do you think’).
Second, some responses were difficult to interpret (e.g., ‘we had sex spac [sic] without condoms’) or indicated confusion (e.g., ‘confused question.’). In an alternate format, such as interviews, the meanings of such responses could be clarified.
Third, recruitment from an online dating and social networking site may have resulted in a pool of participants more likely to be single or in open-relationships than in monogamous relationships. This may explain the relatively low number of respondents, compared to other studies (Golombok, Sketchley and Rust 1989; Ross 1990), who associated non-use of condoms with being in a monogamous relationship. This may also reflect the placement of questions on non-condom use in the latter part of the survey in a section framed on casual relationships. Additionally, the recruitment of participants online could have affected the differences in reasons for non-condom use between meeting venues.
Fourth, this study asked only about reasons at last anal intercourse. While this focused responses on a single event that was consistent for all respondents, other potentially useful information was not collected, such as whether respondents consistently didn’t use condoms, the influence of preceding sexual encounters, the relational context and type of sexual encounter, how much time passed between meeting and sexual encounter, or whether there are specific instances in which MSM do or do not use condoms. Because of potential cross-over and multiple understandings of last sex, there is also a possibility that the role of meeting place may lose its significance. We encourage future research to address this by limiting analysis to partner met for first time. Additionally, data were collected only from men who didn’t use condoms, which suggests that we cannot assume from this analysis that men who consistently use condoms differ from men who don’t use condoms based on the reasons provided. We also shouldn’t assume that the findings from our sample of non-users are transferable to all MSM who look for partners online and offline.
Fifth, while differences in reasons for non-condom use between the 85% who responded and the 15% who did not might exist, missing data prohibited an exploration of this difference. In addition, our use of an inter-subject cross-sectional design, whereby reasons provided by the same men sometimes appeared in several variables, may have had implications for the independence of samples. However, this design also has the advantage of avoiding potential bias that can be introduced through the use of independent samples, such that we find genuine differences in reasons for non-use of condoms and not differences due to sampling.
Sixth, since this study used qualitative response data, even with high inter-rater agreement there is always some subjectivity concerning how responses are categorised, which in turn may limit somewhat the distinctiveness of categories. Moreover, since participants who respond to questions on an online survey cannot be asked to elaborate, this somewhat limited our ability to look at the fine-grained complexities of men’s reasoning and the interrelatedness between categories. Nonetheless, we believe the large amount of data yielded by the online survey was sufficient to capture the general landscape of reasons for non-use of condoms.
Conclusions
The reasons MSM give for non-use of condoms appear complex. Researchers wanting to examine reasons for non-use of condoms should consider including the seven themes identified by this study. Some minor differences were found between reasons for non-use of condoms among men who engage in URAI and UIAI and more major ones between online and offline meeting venue. Differences in reasons for non-use of condoms found in this study underscore the range and diversity of motivational factors behind sexual risk-taking that exist among MSM with respect to meeting venue.
Acknowledgments
The Men’s Internet Sex (MINTS-II) study was funded by the National Institutes of Mental Health Center for Mental Health Research on AIDS, grant number 5 R01 MH063688-05. This paper was undertaken as a project in partial fulfilment of the first author’s Masters in Public Health. The first author gratefully acknowledges the assistance of her examination committee (Simon Rosser, Keith Horvath, and Alexander Rothman), Gene Danilenko, Kate Nygaard, Masaki Utsumiya and Michael Wilkerson from the Men’s Internet Study, and Amanda Kolpin for her assistance with inter-rater reliability. All research was carried out with the approval of the University of Minnesota Institutional Review Board, study number 0405S59661.
References
- Belcher L, Sternberg MR, Wolitski RJ, Halkitis P, Hoff C the Seropositive Urban Men’s Study Team. Condom use and perceived risk of HIV transmission among sexually active HIV-positive men who have sex with men. AIDS Education and Prevention. 2005;17(1):79–89. doi: 10.1521/aeap.17.1.79.58690. [DOI] [PubMed] [Google Scholar]
- Benotsch EG, Kalichman S, Cage M. Men who have met sex partners via the Internet: Prevalence, predictors, and implications for HIV prevention. Archives of Sexual Behavior. 2002;31(2):177–83. doi: 10.1023/a:1014739203657. [DOI] [PubMed] [Google Scholar]
- Bolding G, Davis M, Hart G, Sherr L, Elford J. Gay men who look for sex on the Internet: Is there more HIV/STI risk with online partners? AIDS. 2005;19:961–8. doi: 10.1097/01.aids.0000171411.84231.f6. [DOI] [PubMed] [Google Scholar]
- Carballo-Diéguez A, Bauermeister J. Barebacking: Intentional condomless anal sex in HIV-risk contexts - reasons for and against it. Journal of Homosexuality. 2004;47:1–16. doi: 10.1300/J082v47n01_01. [DOI] [PubMed] [Google Scholar]
- Carballo-Diéguez A, Dolezal C. HIV risk behaviors and obstacles to condom use among Puerto Rican men in New York City who have sex with men. American Journal of Public Health. 1996;86(11):1619–22. doi: 10.2105/ajph.86.11.1619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter M. [(accessed January 24, 2009)];Inconsistent condom use by UK’s gay men, with many putting themselves or others at risk of HIV. 2007 http://www.aidsmap.com/en/news/51CC5AD0-D3EF-440B-9602-4B4A26DF076A.asp.
- Centers for Disease Control. [(accessed May 8, 2009)];Estimates of new HIV infections in the United States : CDC HIV/AIDS facts. 2008 http://www.cdc.gov/hiv/topics/surveillance/resources/factsheets/pdf/incidence.pdf.
- Denning PH, Campsmith ML. Unprotected anal intercourse among HIV-positive men who have a steady male sex partner with negative or unknown HIV serostatus. American Journal of Public Health. 2005;95(1):152–8. doi: 10.2105/AJPH.2003.017814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Detels R, English P, Visscher BR, Jacobsen L, Kingsley LA, Chmiel JS, Dudley JP, Eldred LJ, Ginzburg HM. Seroconversion, sexual activity, and condom use among 2915 HIV seronegative men followed for up to 2 years. Journal of Acquired Immune Deficiency Syndromes. 1989;2(1):77–83. [PubMed] [Google Scholar]
- Dilley JW, Woods WJ, Loeb L, Nelson K, Sheon N, Mullan J, Adler B, Chen S, McFarland W. Brief cognitive counseling with HIV testing to reduce sexual risk among men who have sex with men: Results from a randomized controlled trial using paraprofessional counselors. Journal of Acquired Immune Deficiency Syndromes. 2007;44(5):569–77. doi: 10.1097/QAI.0b013e318033ffbd. [DOI] [PubMed] [Google Scholar]
- Gold RS, Rosenthal DA. Examining self-justifications for unsafe sex as a technique of AIDS education: The importance of personal relevance. International Journal of STD & AIDS. 1998;9:208–213. doi: 10.1258/0956462981922052. [DOI] [PubMed] [Google Scholar]
- Golombok S, Sketchley J, Rust J. Condom use among homosexual men. AIDS Care. 1989;1(1):27–33. doi: 10.1080/09540128908260231. [DOI] [PubMed] [Google Scholar]
- Grov C, Parsons JT, Bimbi DS. Sexual risk behavior and venues for meeting sex partners: An intercept survey of gay and bisexual men in LA and NYC. AIDS and Behavior. 2007;11:915–26. doi: 10.1007/s10461-006-9199-y. [DOI] [PubMed] [Google Scholar]
- Hall HI, Song R, Rhodes P, et al. Estimation of HIV incidence in the United States. JAMA. 2008;300(5):520–29. doi: 10.1001/jama.300.5.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halkitis PN, Parsons JT, Wilton L. Barebacking among gay and bisexual men in New York City: Explanations for the emergence of intentional unsafe behaviour. Archives of Sexual Behavior. 2003;32(4):351–57. doi: 10.1023/a:1024095016181. [DOI] [PubMed] [Google Scholar]
- Hirshfield S, Remien RH, Chiasson MA. Crystal methamphetamine use among men who have sex with men: Results from two national online studies. Journal of Gay and Lesbian Psychotherapy. 2006;10(3):85–93. [Google Scholar]
- Hirshfield S, Remien RH, Humberstone M, Walavalker I, Chiasson MA. Substance use and high-risk sex among men who have sex with men: A national online study in the USA. AIDS Care. 2004;16(8):1036–47. doi: 10.1080/09540120412331292525. [DOI] [PubMed] [Google Scholar]
- Holtgrave DR, Crosby R, Shouse RL. Correlates of unprotected anal sex with casual partners: A study of gay men living in the southern United States. AIDS and Behavior. 2006;10:575–8. doi: 10.1007/s10461-006-9116-4. [DOI] [PubMed] [Google Scholar]
- Horvath KJ, Nygaard K, Rosser BRS. Ascertaining partner HIV status and its association with sexual risk behavior among Internet-using men who have sex with men. AIDS and Behavior. 2009 doi: 10.1007/s10461-009-9633-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horvath KJ, Oakes JM, Rosser BRS. Sexual negotiation and HIV serodisclosure among men who have sex with men with their online and offline partners. Journal of Urban Health. 2008;85(5):744–58. doi: 10.1007/s11524-008-9299-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horvath KJ, Rosser BRS, Remafedi G. Sexual risk taking among young Internet-using men who have sex with men. American Journal of Public Health. 2008;98(6):1059–67. doi: 10.2105/AJPH.2007.111070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klausner JD, Pollack LM, Wong W, Katz MH. Same-sex domestic partnerships and lower-risk behaviors for STDs, including HIV infection. Journal of Homosexuality. 2006;51(4):137–44. doi: 10.1300/J082v51n04_07. [DOI] [PubMed] [Google Scholar]
- Liau A, Millett G, Marks G. Meta-analytic examination of online sex-seeking and sexual risk behavior among men who have sex with men. Sexually Transmitted Diseases. 2006;33(9):576–84. doi: 10.1097/01.olq.0000204710.35332.c5. [DOI] [PubMed] [Google Scholar]
- McKirnan D, Vanable P, Ostrow D, Hope B. Expectancies of sexual ‘escape’ and sexual risk among drug and alcohol-involved gay and bisexual men. Journal of Substance Abuse. 2001;13:137–54. doi: 10.1016/s0899-3289(01)00063-3. [DOI] [PubMed] [Google Scholar]
- Mettey A, Crosby R, DiClemente RJ, Holtgrave DR. Associations between internet sex seeking and STI associated risk behaviors among men who have sex with men. Sexually Transmitted Infections. 2003;79:466–68. doi: 10.1136/sti.79.6.466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mimiaga MJ, Reisner SL, Vanderwarker R, Gaucher MJ, O’Connor CA, Medeiros MS, Safren SA. Polysubstance use and HIV/STD risk behavior among Massachusetts men who have sex with men accessing Department of Public Health mobile van services: Implications for intervention development. AIDS Patients Care and STDS. 2008;22(9):745–51. doi: 10.1089/apc.2007.0243. [DOI] [PubMed] [Google Scholar]
- Osmond DH, Pollack LM, Paul JP, Catania JA. Changes in prevalence of HIV infection and sexual risk behavior in men who have sex with men in San Francisco: 1997–2002. American Journal of Public Health. 2007;97(9):1677–83. doi: 10.2105/AJPH.2005.062851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parsons JT, Halkitis PN, Wolitski RJ, Gomez CA the Seropositive Urban Men’s Team. Correlates of sexual risk behaviors among HIV positive men who have sex with men. AIDS Education and Prevention. 2003;15(5):383–400. doi: 10.1521/aeap.15.6.383.24043. [DOI] [PubMed] [Google Scholar]
- Parsons JT, Schrimshaw EW, Bimbi DS, Wolitiski RJ, Gomez CA, Halkitis PN. Consistent, inconsistent, and non-disclosure to casual sexual partners among HIV-seropositve gay and bisexual men. AIDS. 2005;19:S87–97. doi: 10.1097/01.aids.0000167355.87041.63. [DOI] [PubMed] [Google Scholar]
- Remien RH, Carballo-Diéguez A, Wagner G. Intimacy and sexual risk behavior in serodiscordant male couples. AIDS Care. 1995;7:429–38. doi: 10.1080/09540129550126380. [DOI] [PubMed] [Google Scholar]
- Ross MW. Reasons for non-use of condoms by homosexually active men during anal intercourse. International Journal of STD & AIDS. 1990;1:432–4. doi: 10.1177/095646249000100608. [DOI] [PubMed] [Google Scholar]
- Ross MW, Rosser BRS, McCurdy S, Feldman J. The advantages and limitations of seeking sex online: A comparison of reasons given for online and offline sexual liaisons by men who have sex with men. Journal of Sex Research. 2007;44(1):59–71. doi: 10.1080/00224490709336793. [DOI] [PubMed] [Google Scholar]
- Rosser BRS, Miner MH, Bockting WO, Ross MW, Konstan J, Gurak L, Stanton J, Carballo-Diéguez A, Mazin R, Coleman E. HIV risk and the Internet: Results of the Men’s INTernet Study (MINTS) AIDS and Behavior. 2009b;13(4):746–56. doi: 10.1007/s10461-008-9399-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosser BRS, Oakes JM, Horvath KJ, Konstan JA, Peterson JL. HIV Sexual Risk Behavior by Men who use the Internet to seek Sex with Men: Results of the Men’s INTernet Sex Study-II (MINTS-II) AIDS and Behavior. 2009a;13(3):488–98. doi: 10.1007/s10461-009-9524-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanchez T, Finlayson T, Drake A, Behel S, Cribbin M, DiNenno E, Hall T, Kramer S, Lansky A. Human immunodeficiency virus (HIV) risk, prevention, and testing behaviors – United States, National HIV Behavioral Surveillance System: Men who have sex with men, November 2003 – April 2005. MMWR Surveillance Summaries. 2006;55(SS-6):1–16. [PubMed] [Google Scholar]
- Stall RD, Hays RB, Waldo CR, Ekstrand M, McFarland W. The Gay ‘90s: A review of research in the 1990s on sexual behavior and HIV risk among men who have sex with men. AIDS. 2000;14:S101–14. [PubMed] [Google Scholar]
- Theodore PS, Durán REF, Antoni MH, Fernandez MI. Intimacy and sexual behavior among HIV-positive men who have sex with men in primary relationships. AIDS and Behavior. 2004;8(3):321–31. doi: 10.1023/B:AIBE.0000044079.37158.a9. [DOI] [PubMed] [Google Scholar]
- Truong HHM, Kellogg T, Klausner JD, Katz MH, Dilley J, Knapper K, Chen S, Prabhu R, Grant RM, Louie B, McFarland W. Increases in sexually transmitted infections and sexual behavior without a concurrent increase in HIV incidence among men who have sex with men in San Francisco: A suggestion of HIV serosorting? Sexually Transmitted Infections. 2006;82:461–6. doi: 10.1136/sti.2006.019950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valdiserri RO, Lyter D, Leviton LC, Callahan CM, Kingsley LA, Rinaldo CR. Variables influencing condom use in a cohort of gay and bisexual men. American Journal of Public Health. 1988;78(7):801–5. doi: 10.2105/ajph.78.7.801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van de Ven P, Kippax S, Crawford J, Rawstorne P, Prestage G, Grulich A, Murphy D. In a minority of gay men, sexual risk practice indicates strategic positioning for perceived risk reduction rather than unbridled sex. AIDS Care. 2002;14(4):471–80. doi: 10.1080/09540120208629666. [DOI] [PubMed] [Google Scholar]
- Wilson PA, Cook S, McGaskey J, Row M, Dennis N. Situational predictors of sexual risk episodes among men with HIV who have sex with men. Sexually Transmitted Infections. 2008;84:506–8. doi: 10.1136/sti.2008.031583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolitski RJ, Bailey CJ, O’Leary A, Gomez CA, Parsons JT. Self-perceived responsibility of HIV-seropositive men who have sex with men for preventing HIV transmission. AIDS and Behavior. 2003;7:363–72. doi: 10.1023/b:aibe.0000004728.73443.32. [DOI] [PubMed] [Google Scholar]
- Zhang D, Bi P, Hiller JE, Lv F. Web-based HIV/AIDS behavioral surveillance among men who have sex with men: potential and challenges. International Journal of Infectious Diseases. 2008;12:126–31. doi: 10.1016/j.ijid.2007.06.007. [DOI] [PubMed] [Google Scholar]