Abstract
Shoulder impingement is a common condition presumed to contribute to rotator cuff disease. Impingement can occur externally with the coracoacromial arch or internally with the glenoid rim. Normal scapulothoracic motions that occur during arm elevation include upward rotation, posterior tilting, and either internal or external rotation. These scapulothoracic motions and positions are the result of coupled interactions between sternoclavicular and acromioclavicular joints. The sternoclavicular and acromioclavicular joints both contribute to scapulothoracic upward rotation. Posterior tilting is primarily an acromioclavicular joint motion. The sternoclavicular and acromioclavicular joint motions offset one another regarding final scapulothoracic internal/external rotation position. This manuscript discusses these coupled interactions in relation to shoulder muscle function. Two case examples are presented to demonstrate application of understanding these interactions and potential mechanisms of movement abnormalities in targeting treatment interventions for movement based subgroups of impingement patients.
Keywords: Rotator cuff disease, human movement system, exercise, physical therapy
Shoulder impingement is a common condition believed to contribute to the development or progression of rotator cuff disease (Michener et al. 2003, van der Windt et al. 1995). A number of impingement categories have been identified including subacromial impingement or “external impingement”; internal impingement, which can be further divided into anterior or posterior (Edelson & Teitz 2000); and coracoid impingement. Charles Neer described subacromial impingement as the compression and abrasion of the bursal side of the rotator cuff beneath the anterior acromion, and developed the anterior acromioplasty as a treatment (Neer 1983). External impingement is now understood as a much broader category than that described by Neer, and could include compression or abrasion of the cuff tendons or tendon of the long head of the biceps brachii beneath any aspect of the coracoacromial arch (Neer 1983). The coracoacromial arch includes not just the acromial undersurface, but also the coracoacromial ligament, and the undersurface of the acromioclavicular (AC) joint.
Internal impingement was first described as a condition noted in overhead athletes, identified in part due to poor outcomes of acromioplasty in this population (Paley et al. 2000). Posterior internal impingement has been postulated to be contact or entrapment of the articular side of the supra or infraspinatus tendons with the posterior/superior glenoid labral complex in a position of glenohumeral abduction and external rotation (Paley et al. 2000, Heyworth & Williams 2009). Articular surface contact of the cuff with the glenoid labral complex can occur anterior/superiorly as well (Edelson & Teitz 2000). Articular surface tears are also common in patients without substantive overhead sports exposure (Budoff et al. 2003, Heyworth & Williams 2009). Impingement of the subscapularis tendon between the coracoid process and lesser tuberosity of the humerus has also been identified as an impingement category, although less commonly discussed in the literature (Okroro et al 2009).
All categories of impingement are potential mechanisms for the development or progression of rotator cuff disease, or long head biceps tendinopathy (Soslowsky et al. 2002). Physical exam findings consistent with impingement can also be associated with labral tears in internal impingement (Budoff et al. 2003) or develop secondary to instability or as a delayed consequence of adhesive capsulitis. There are multiple mechanisms by which impingement may occur, including excess or reduced motion and abnormal patterns of motion at particular portions of the range of motion (Michener et al. 2003). In addition, anatomic abnormalities of the humerus or acromion have been implicated in impingement (Zuckerman et al. 1992). It should be noted that rotator cuff disease can develop without impingement, through tensile overload or intrinsic tissue degeneration (Soslowsky et al. 2002). Regardless of the initial precipitating factor, however, impingement, abnormal shoulder motions, and associated rotator cuff disease often are found in the presence of partial or full thickness rotator cuff tears. In other words, even if rotator cuff disease or tearing did not initiate from impingement or abnormal motion, impingement and abnormal motion are likely to contribute to disease progression.
The purpose of this manuscript is to identify recent advances in understanding of normal and abnormal biomechanics of the shoulder as related to rehabilitation of shoulder impingement. In particular, contributions of sternoclavicular (SC) and AC joint motions to overall scapulothoracic (ST) motion during arm elevation will be discussed. How this biomechanical knowledge can assist in planning targeted interventions for motion based subgroups of shoulder pain patients will be illustrated with two brief case examples.
NORMAL SHOULDER MOTION
During normal motion, the scapula will upwardly rotate and posteriorly tilt on the thorax during elevation of the arm in flexion, abduction, scapular plane abduction, or unrestricted overhead reaching (McClure et al. 2001, Braman et al. 2009, Ludewig et al. 2009). Throughout this manuscript, elevation will be used to refer to raising the arm overhead in any of these planes. Scapulothoracic internal or external rotation is less consistent during arm elevation, differing in pattern depending on what plane the arm is elevated in, and depending on what portion of the elevation range of motion is considered (Ludewig et al. 2009). The scapula must adjust in the transverse plane for the intended plane of elevation. For flexion, the scapula will internally rotate somewhat early in the motion, whereas for coronal plane abduction, it will externally rotate at the initiation of the motion. Based on the limited end range data available (McClure et al. 2001, Braman et al. 2009, Ludewig et al. 2009), it appears some external rotation of the scapula will occur near end range for each of these planes of elevation.
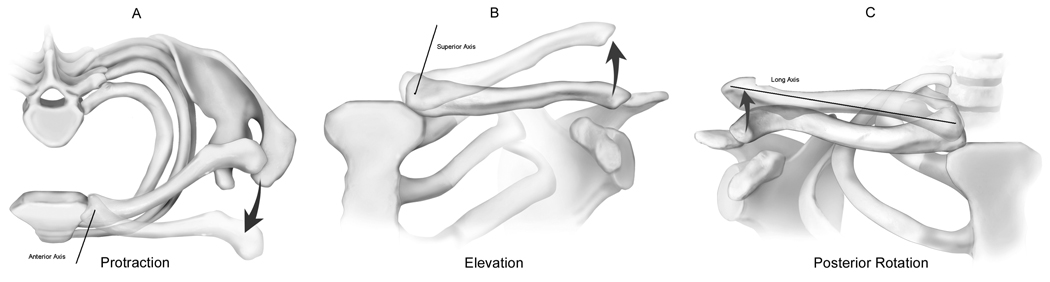
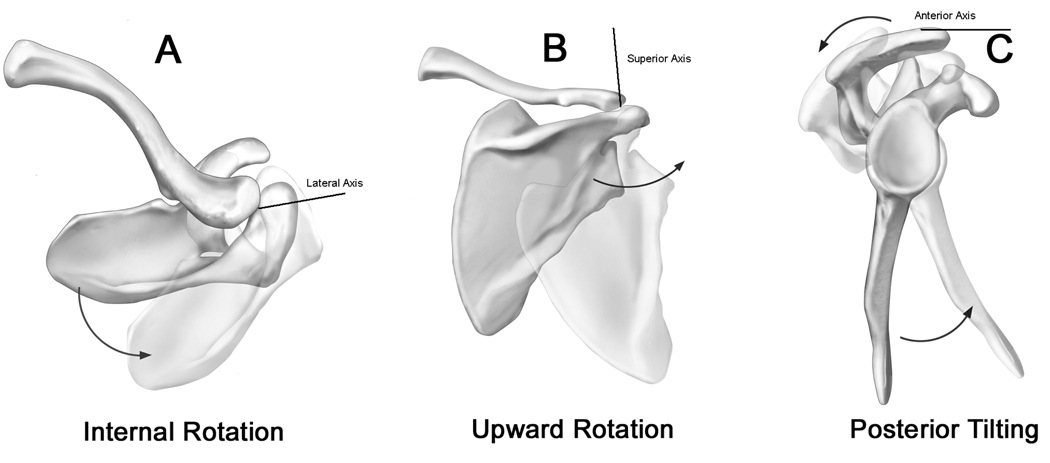
Recent investigations have added new knowledge on how SC and AC joint motions contribute to overall ST motion (Ludewig et al. 2004, Sahara et al. 2006, Sahara et al. 2007, Teece et al. 2008, Ludewig et al. 2009). The primary clavicular motion occurring at the SC joint during active arm elevation in any plane except extension is 30° of posterior long axis rotation (Sahara et al. 2007, Ludewig et al. 2009; Figure 1). Secondarily, the clavicle will retract ~ 15° at the SC joint during elevation, even with flexion (Ludewig et al. 2009). However, the clavicle also “adjusts” in the transverse plane (less retraction with flexion, more with abduction) similarly to the changes in scapular internal rotation with flexion versus abduction (Ludewig et al. 2009). Finally a small amount of clavicular elevation (typically below 10° in healthy subjects) will occur at the SC joint with humeral elevation in any plane (Sahara et al. 2007, Ludewig et al. 2009). Concurrent with clavicular motion relative to the thorax, measurable motion of the scapula relative to the clavicle is also occurring at the AC joint as the humerus is elevated in any plane (Sahara et al. 2007, Ludewig et al. 2009; Figure 2). Primary AC joint motions include upward rotation and posterior tilt of the scapula relative to the clavicle. Secondarily the scapula will internally rotate relative to the clavicle at the AC joint, even while abducting the arm (Sahara et al. 2007, Ludewig et al. 2009).
Figure 1.
Clavicular rotations relative to the thorax include protraction/retraction about a superiorly directed axis (A), elevation/depression about an anteriorly directed axis (B), and anterior/posterior rotation about a long axis (C). Adapted from Ludewig et al. 2009.
Figure 2.
Scapular rotations relative to the clavicle or thorax include internal/external rotation about a superiorly directed axis (A), upward/downward rotation about an axis perpendicular to the plane of the scapula directed anteriorly (B), and anterior/posterior tilting about a laterally directed axis (C). Adapted from Ludewig et al. 2009.
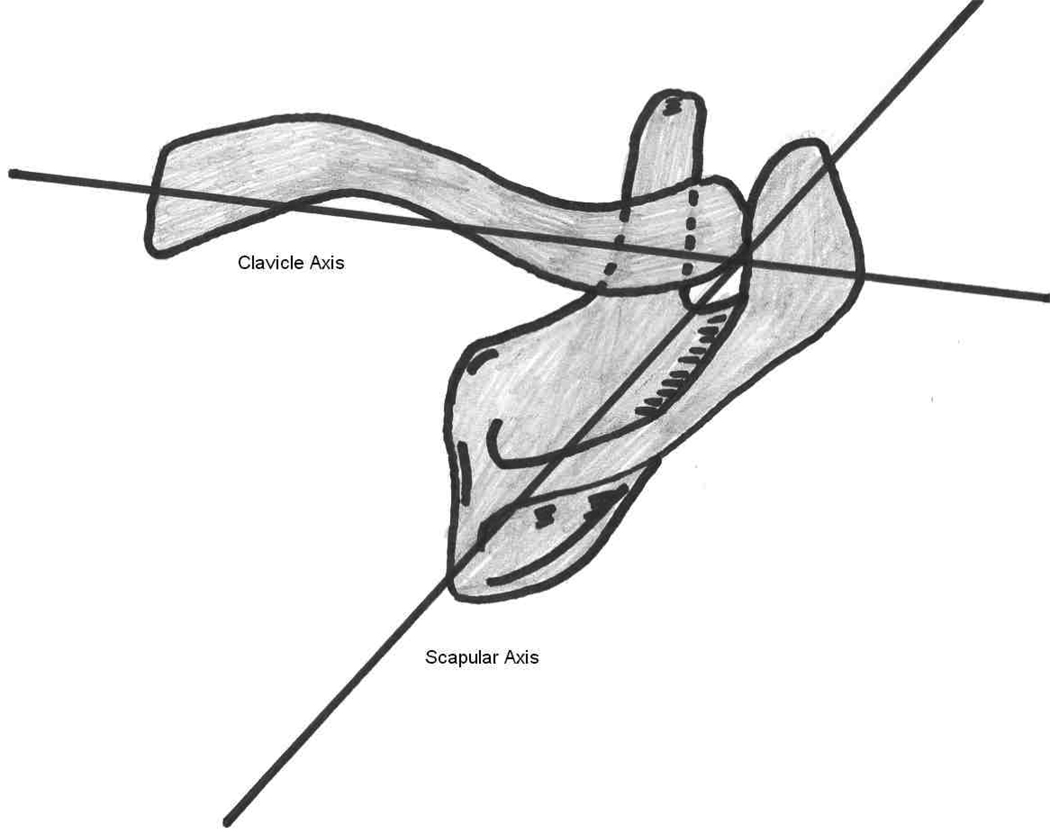
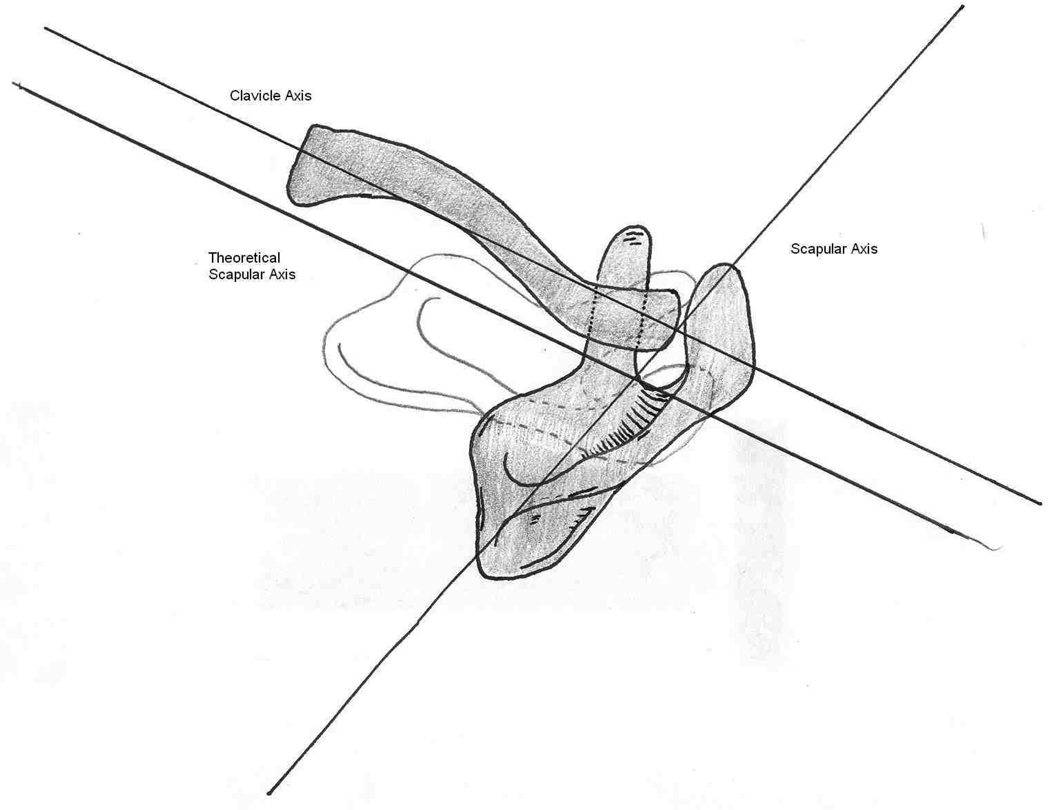
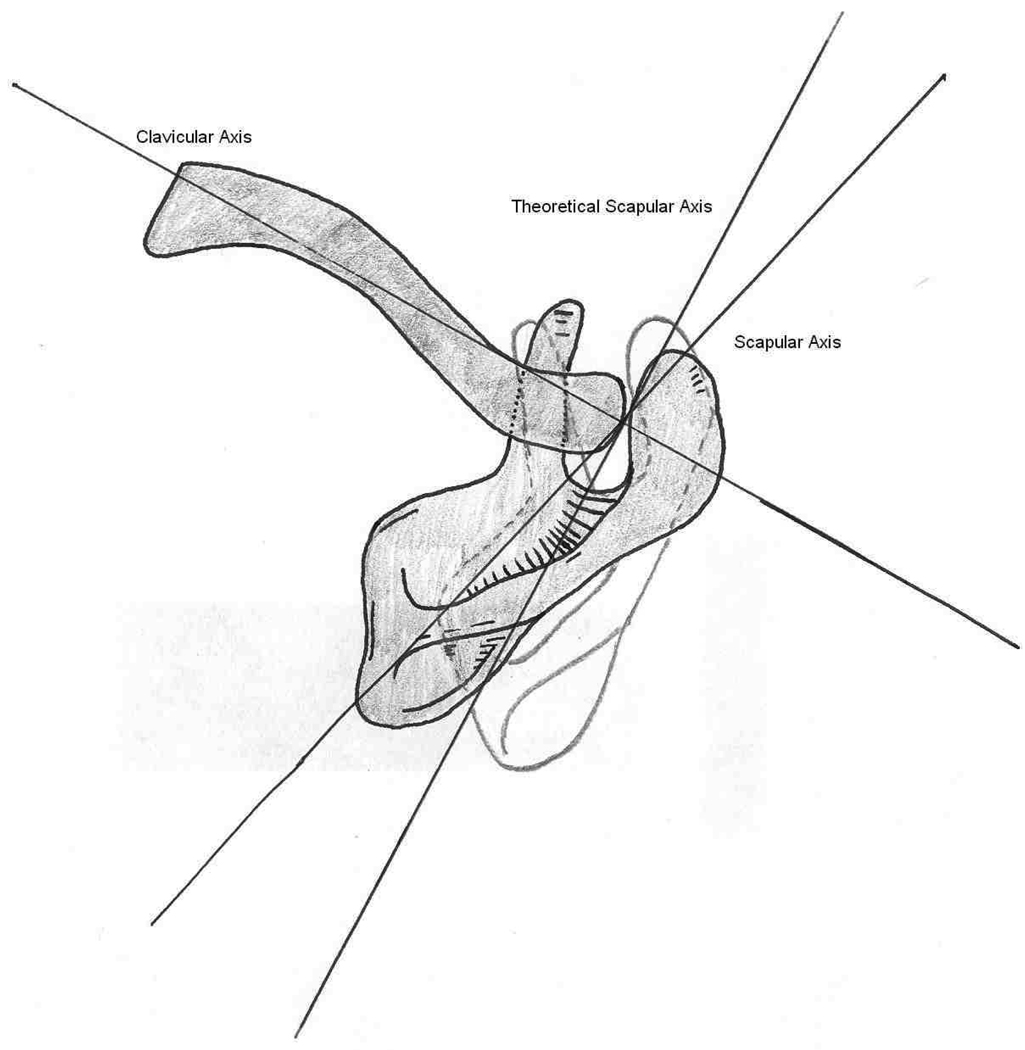
Overall ST motion occurs either through motion of the clavicle relative to the thorax, motion of the scapula relative to the clavicle, or some combination of both. During normal arm elevation in any plane, both clavicular (SC) and scapular (AC) motions described above are contributing to the final position of the scapula on the thorax. However, the non-parallel alignment of the axes of rotation of the SC and AC joints makes their contributions to ST motion challenging to visualize (Teece et al. 2008; Figure 3). The AC joint axes are aligned consistently with how the axes are described for the scapula on the thorax, such that if the scapula upwardly rotates, posteriorly tilts or internally rotates relative to the clavicle, there is a 1:1 “coupling” with ST motion. In other words 5° of scapular upward rotation relative to the clavicle would contribute to 5° of ST upward rotation. In order to understand the coupling of clavicular motion to ST motion, it is helpful to visualize an axis of rotation embedded along the long axis of the clavicle, and another embedded in the scapula from the root of the scapular spine to the AC joint (Figure 3). In a superior transverse plane view, first imagine a hypothetical situation where the clavicle and scapular axes are parallel (Figure 3B). In such a hypothetical alignment, if the clavicle were elevated about its anteriorly directed axis 9° relative to the thorax, the scapula would upwardly rotate 9° on the thorax, assuming no motion of the scapula relative to the clavicle at the AC joint. If the clavicle rotated posteriorly about its long axis 30° relative to the thorax, the scapula would posteriorly tilt 30° relative to the thorax, and if the clavicle retracted 9° relative to the thorax, the scapula would externally rotate 9° relative to the thorax (Teece et al. 2008). Now consider an alternative hypothetical situation where the scapula is internally rotated 90° relative to the clavicle, such that the described axes in the transverse plane are at a 90° angle (Figure 3C). In such a hypothetical alignment, if the clavicle were elevated about its anteriorly directed axis 9° relative to the thorax, the scapula would anteriorly tilt 9° on the thorax. If the clavicle rotated posteriorly about its long axis 30° relative to the thorax, the scapula would upwardly rotate 30° on the thorax, and if the clavicle retracted 9° relative to the thorax, the scapula would externally rotate 9° on the thorax (Teece et al. 2008). The two scenarios completely change with regard to SC joint contributions to ST upward rotation and tilting, but remain the same for contributions to ST external rotation.
Figure 3.
Coupling of sternoclavicluar joint rotations with scapular motion on the thorax. Average position of acromioclavicular joint internal rotation angle (A), scapular and clavicular axes marked; theoretical 0° angle as compared to average angle (B); and theoretical 90° angle as compared to average angle (C) (reproduced from Teece et al.).
These scenarios illustrate the changes in coupling of SC to ST motion that can occur with changing the scapula to clavicle (AC joint) internal rotation angle. Neither of these extreme alignments occurs during normal motion. On average in healthy subjects, the scapula is internally rotated 60° relative to the clavicle (Ludewig et al. 2009). Such an alignment is 2/3 of the way from the initial parallel alignment to the 90° alignment(Figure 3A). Subsequently, the coupling that occurs during normal arm elevation in any plane is about 2/3 of what was described in the second scenario, and 1/3 of what was described in the first scenario (Teece et al. 2008). In such an alignment, if the clavicle were elevated about its anteriorly directed axis 9° relative to the thorax, the scapula would anteriorly tilt 6° and upwardly rotate 3° on the thorax. If the clavicle rotated posteriorly about its long axis 30° relative to the thorax, the scapula would upwardly rotate 20° and posteriorly tilt 10° on the thorax. Table 1 summarizes these relative coupling relationships.
TABLE 1.
Hypothetical listing of Sternoclavicular (SC) Joint Couplings with Scapulothoracic (ST) Motion on the Thorax at Varying Angles of Acromioclavicular (AC) Joint Internal Rotation.
| AC Internal Rotation Angle | 0° | 90° | 60° |
|---|---|---|---|
| SC Retraction | 100% ST External Rotation | 100% ST External Rotation | 100% ST External Rotation |
| SC Elevation | 100% ST Upward Rotation; 0% ST Anterior Tilting | 100% ST Anterior Tilting; 0% ST Upward Rotation | 75% ST Anterior Tilting; 25% ST Upward Rotation |
| SC Posterior Rotation | 100% ST Posterior Tilting; 0% ST Upward Rotation | 100% ST Upward Rotation; 0% ST Posterior Tilting | 75% ST Upward Rotation; 25% ST Posterior Tilting |
(reproduced from Teece et al. 2008)
In addition to the coupling of clavicle motion to ST motion, during arm elevation in any plane, the scapula relative to the clavicle is also moving at the AC joint. These AC joint motions may increase or decrease the overall ST joint motion depending on whether they complement or offset the SC joint coupled scapular motions. So in the example above for scapular plane abduction to 120° relative to the thorax, the 20° ST upward rotation coupled with clavicle posterior rotation on the thorax, and 3° ST upward rotation coupled with clavicle elevation on the thorax would be complemented by an average of 11° of scapular upward rotation relative to the clavicle across the same increment of scapular plane abduction (Ludewig et al. 2009). The end result would be 34° of ST upward rotation. For ST tilting, the 10° posterior tilting coupled with clavicle posterior rotation on the thorax would be reduced by 6° anterior tilting coupled with clavicle elevation on the thorax as described above. Subsequently, the clavicle overall contribution to ST posterior tilting would only be 4°. However, the scapula relative to the clavicle is tilting posteriorly during that scapular plane abduction motion on average 16°, to result in overall ST motion of 20° (Ludewig et al. 2009). Finally the 9° of ST external rotation coupled with clavicle retraction on the thorax is offset by an average of 6° scapula internal rotation relative to the clavicle, resulting in 3° of ST external rotation. Note that final resulting scapular upward rotation motion and position on the thorax is produced by complementary motion of the clavicle relative to the thorax and scapula relative to the clavicle. ST tilting is produced almost exclusively by scapular motion relative to the clavicle as the clavicle elevation and posterior rotation motions at the SC joint are offsetting. ST external rotation is minimal due to offsetting motions of clavicle retraction relative to the thorax and scapular internal rotation relative to the clavicle.
EFFECTS OF TRAPEZIUS AND SERRATUS ANTERIOR MUSCLE FUNCTION
Although somewhat complex to understand, these interrelationships between how SC and AC joints contribute to overall motion of the scapula on the thorax are also important with regard to how they influence muscle function. Based on common clinical presumptions, the upper trapezius is often described as an ST upward rotator. However, as identified by Johnson et al. (1994), its distal attachments are to the clavicle. The line of action of the upper trapezius muscle attached to the distal clavicle results in it having the capability to produce elevation and retraction of the clavicle relative to the thorax (Fey et al. 2007, Johnson et al. 1994). We know from the coupling discussion above, that for every degree of clavicular elevation relative to the thorax, only 1/3 of that motion results in ST upward rotation, and 2/3 will result in ST anterior tilting. So in healthy people, the upper trapezius is only contributing about 3° (1/3 of 9° average clavicle elevation relative to the thorax; Ludewig et al. 2009) to overall ST upward rotation, while ST upward rotation can average 50° or more (McClure et al. 2001, Ludewig et al. 2009). As such, based on unpublished modeling work (Fey et al. 2007,) the upper trapezius muscle does not appear to have a line of action to be a substantive upward rotator in healthy persons, but rather likely generates the necessary clavicle retraction relative to the thorax to prevent excessive ST internal rotation (Johnson et al. 1994, Fey et al. 2007). Thus, if attempting to increase ST upward rotation in a clinical patient, targeting upper trapezius strengthening would not seem an optimal strategy. The lower trapezius, however, with its direct attachment to the scapula, has a line of action that appears to assist in producing ST upward rotation at the AC joint (Fey et al. 2007).
We also know from the coupling discussion, that over 50% of the overall ST upward rotation is occurring through clavicle posterior rotation on the thorax. It does not appear that any of the clavicular musculature has a line of action contributing to posterior rotation torque capability (Fey et al. 2007, Johnson et al. 1994). Because of this, it is likely that clavicular posterior rotation on the thorax is produced secondarily by tension in the coracoclavicular and acromioclavicular ligaments when the serratus anterior and lower trapezius are pulling on the scapula with upward rotation torque (Ludewig et al. 2009) . The serratus anterior has the largest moment arm for the production of scapular upward rotation torque (Dvir & Berme 1978, Johnson et al. 1994, Phadke et al. 2009). The serratus anterior line of action is also such that it can contribute substantively to scapular posterior titling. The upper, middle, or lower trapezius do not appear to contribute substantively to scapular posterior tilting torque, based on their line of action (Fey et al. 2007). In fact excess activation of the upper trapezius, if occurring (Ludewig and Cook 2000), could result in excess clavicular elevation on the thorax and subsequently excess ST anterior tilting though its coupled motion. The primary role of the upper trapezius appears to be in generating retraction of the clavicle at the SC joint and the middle and lower trapezius in generating external rotation of the scapula at the AC joint (Fey et al. 2007, Johnson et al 1994).
ABNORMAL SHOULDER MOTION IN IMPINGEMENT
A recent review article identified scapular motion abnormalities in subjects with impingement or rotator cuff disease (Ludewig and Reynolds 2009). Briefly, nine of 11 studies reviewed demonstrated a statistically significant scapular movement deviation in at least 1 variable, as compared to healthy control groups (Warner et al. 1992, Lukasiewicz et al. 1999, Ludewig & Cook 2000, Graichen et al. 2001, Endo et al. 2001, Hebert et al. 2002, Su et al. 2004, Mell et al. 2005, McClure et al. 2006, Lin et al. 2005, Laudner et al. 2006). The most frequent findings have been reduced ST posterior tilting, reduced ST upward rotation, increased ST internal rotation, or increased clavicular elevation relative to the thorax (Ludewig and Reynolds 2009). These movement alterations are believed to increase proximity of the rotator cuff tendons to the coracoacromial arch or glenoid rim. However, there is little direct evidence of how movement deviations contribute to reduced subacromial space or increased internal impingement (Solem-Bertoft et al. 1993, Karduna et al. 2005). Additionally, there are inconsistencies and contradictions in movement alterations identified across studies (Ludewig and Reynolds 2009). Small subject samples, lack of distinction between categories of impingement, frequent lack of distinction between rotator cuff tendinopathy and cuff tearing in patient samples, a wide variety of measurement approaches, and skin surface measurement methods with limited precision have prevented a full understanding of the role of scapular movement patterns in the development or progression of shoulder dysfunction (Ludewig and Reynolds 2009).
Additionally, increased humeral head superior or anterior translation has been found in subjects with impingement (Deutsch et al. 1996, Ludewig & Cook 2002). These directions of humeral head motion are believed to reduce the subacromial space and increase impingement risk. Biomechanical evidence also supports the idea of glenohumeral internal rotation contributing to subacromial impingement beneath the anterior structures (Flatow et al. 1994, Werner et al. 2006, Yanai et al. 2006).
Recent work also demonstrates how angles of humeral elevation which minimize the subacromial space may differ from angles of humeral elevation where the rotator cuff soft tissues are at greatest risk. The subacromial space is typically described as minimized at 90° of humeral elevation in all planes (Bey et al. 2007). However, the portion of the humerus in closest contact at that point in the range of motion of abduction is actually the lateral aspect of the greater tuberosity, which has no rotator cuff soft tissue (Bey et al. 2007). The rotator cuff tendons are actually in closest proximity to the undersurface of the acromion near 45° of humeral abduction relative to the thorax (Bey et al. 2007). By angles past 60° humeral abduction, the attachment sites or footprints of the cuff tendons on the greater tuberosity have rotated past the lateral acromial undersurface (Bey et al. 2007). Patients may still have a painful arc of motion near 90° of humeral elevation in any plane, since this is where rotator cuff muscle forces are highest. However, pain at or above 90° of humeral elevation relative to the thorax is unlikely a direct result of a compressive subacromial impingement of the rotator cuff tendons. Alternatively, proximity of the undersurface of the cuff tendons to the superior glenoid rim increases at higher angles of humeral elevation in any plane, suggesting increased risk of internal impingement with humeral elevation above 90° relative to the thorax (Petersen et al. 2010).
Influencing Factors in Movement Abnormalities
The previous review manuscript also described potential mechanisms by which abnormal scapular or clavicular motions might occur (Ludewig and Reynolds 2009). These included pain, soft tissue tightness, muscle strength or activation imbalances, muscle fatigue, and thoracic posture (Borich et al. 2006; Borstad and Ludewig 2005; Cools et al. 2003; Cools et al. 2004; Cools et al. 2007; Culham and Peat 1993; Ebaugh et al. 2006a; Ebaugh et al. 2006b; Endo et al. 2004; Falla et al. 2007; Kebaetse et al. 1999; Lin et al. 2005; Ludewig and Cook 2000; McQuade et al. 1998; Tsai et al. 2003; Wadsworth and Bullock-Saxton 1997). These same factors can influence humeral motions (Harryman et al. 1990). Influences of these factors on shoulder motion are summarized in Table 2 (adapted from Ludewig and Reynolds 2009). In summary, there is some evidence of increased upper trapezius activation and reduced serratus anterior activation in the same subjects who have demonstrated reduced ST posterior tilting, increased internal rotation, and reduced upward rotation (Lin et al. 2005; Ludewig and Cook 2000). There is also evidence of increased ST anterior tilting and internal rotation in subjects with a relatively short resting length of the pectoralis minor (Borstad and Ludewig 2005). Glenohumeral internal rotation deficit and experimentally induced posterior capsule tightness have also been shown to increase ST anterior tilting and humeral anterior translations relative to the glenoid, respectively (Borich et al. 2006; Harryman et al. 1990). Slouched sitting, thoracic kyphosis, and increased age have also been related to increased ST anterior tilting and internal rotation and reduced ST upward rotation (Culham and Peat 1993; Endo et al 2004; Kebaetse et al. 1999). Although not experimentally demonstrated, other factors including reduced rotator cuff activation and pectoralis major tightness can be biomechanically theorized to impact ST or glenohumeral kinematics in ways that are believed to increase impingement risk. Each of these factors provides additional insight in planning treatment intervention approaches targeted to specific movement deviations.
TABLE 2.
Proposed Biomechanical Mechanisms of Clavicular, Scapular or Humeral Kinematic Deviations (adapted from Ludewig and Reynolds 2009).
| Mechanism | Associated Effects |
|---|---|
| Inadequate serratus anterior activation | Lesser scapular upward rotation and posterior tilt |
| Excess upper trapezius activation | Greater clavicular elevation, reduced scapular posterior tilt |
| Pectoralis minor tightness | Greater scapular internal rotation and anterior tilt |
| Posterior capsule tightness | Greater scapular anterior tilt, glenohumeral internal rotation deficit, greater humeral superior or anterior translation |
| Inadequate rotator cuff activation or partial tearing | Greater humeral superior translation, lesser humeral external rotation |
| Pectoralis major tightness | Lesser clavicular retraction, greater humeral internal rotation |
| Thoracic kyphosis or flexed posture | Greater scapular internal rotation and anterior tilt, lesser scapular upward rotation |
MOVEMENT BASED INTERVENTION CASE EXAMPLES
Clinical trials demonstrate that therapeutic exercise can reduce pain and improve function in patients with shoulder impingement and rotator cuff disease (Bang and Deyle 2000; Haahr et al. 2006; Ludewig and Borstad 2003; McClure et al. 2004; Michener et al. 2004; Senbursa et al. 2007). However, this evidence also suggests that not all patients improve, and that most do not return to healthy levels of function (Ludewig & Borstad 2003). Exercise protocols vary widely across these clinical trials. We believe it is important to consider the current biomechanical evidence when rehabilitating patients presenting with shoulder pain and abnormal movement patterns. Targeting stretching or strengthening exercises to the particular movement deviations they can contribute to or alleviate may have the potential to improve overall treatment effectiveness. Consider the application of these biomechanical factors through the following two case examples.
In the first case, the patient presents with anterior shoulder pain, positive clinical impingement tests, and a visually observed movement pattern during lower angles of arm elevation including excess clavicle elevation relative to the thorax, reduced ST upward rotation, and reduced ST posterior tilting. In such a case, we believe their movement pattern may be contributing to subacromial shoulder impingement. Our goal is to focus on normalizing their movement, allowing for symptomatic improvement. Given the ability of the serratus anterior as the most mechanically effective ST upward rotator and posterior tilter, we target this as a primary muscle for increasing activation or strengthening. Over-activation of the upper trapezius (Ludewig & Cook 2000) can contribute to the excess clavicle elevation on the thorax. Through elevation of the clavicle coupling with ST anterior tilt, the excess upper trapezius activation may reduce the ability of the serratus to posteriorly tilt the scapula relative to the clavicle at the AC joint. Subsequently, we train the patient to reduce upper trapezius activation. Secondarily, we may also include lower trapezius exercise for this patient. Exercises maximizing serratus anterior and lower trapezius activation while minimizing upper trapezius activation are of primary focus. Because of the reduced ST posterior tilt, we would also stretch the pectoralis minor and posterior capsule if tightness were identified in these structures. Focus on stretching and strengthening exercises for these targeted muscle groups has shown positive outcomes in subjects with shoulder pain (Ludewig and Borstad 2003).
In the second case, an overhead thrower presents with posterior shoulder pain with humeral elevation at and above 90° relative to the thorax. He also presents with a positive posterior internal impingement sign, and glenohumeral internal rotation deficit. The glenohumeral internal rotation deficit presents as soft tissue tightness rather than bony retroversion. The subject’s movement pattern during arm elevation in any plane includes reduced ST upward rotation, reduced clavicular retraction relative to the thorax, and increased ST internal rotation or “winging”. In this case we also target serratus anterior strengthening due to the ST upward rotation deficit. However, we simultaneously strengthen all components of the trapezius: upper trapezius to improve clavicular retraction, and middle and lower trapezius to improve scapular external rotation relative to the clavicle at the AC joint. Accordingly, exercises capable of more global strengthening of the scapulothoracic muscles are of primary focus. In addition to stretching the posterior capsule, we would also stretch the pectoralis major (clavicular protractor) and pectoralis minor (scapular internal rotator) if tightness were identified in these structures.
Clearly these are not comprehensive case studies, and illustrating all possible contributing factors to the patients’ pain presentation is beyond the scope of this manuscript. However, these cases briefly illustrate the application of biomechanical principles and evidence in targeted treatment approaches for subgroups of patients with shoulder pain. Although there is increasing evidence of ability to effectively reduce shoulder symptoms in patients with shoulder pain, there is minimal evidence of exercise programs changing movement patterns (McClure et al. 2004; Wang et al. 1999). This may be due to inadequate exercise intensity or “dose”, lack of targeting exercises to specific movement abnormalities and associated biomechanical factors, or limitations in clinical diagnosis. Linking effective exercise programs to improvements in movement patterns is an area in great need of further investigation.
SUMMARY
Shoulder impingement is a common condition presumed to contribute to rotator cuff disease. Impingement can occur externally with the coracoacromial arch or internally with the glenoid rim. Normal ST motions that occur during arm elevation in any plane include upward rotation, posterior tilting, and either internal or external rotation. These motions and positions are the result of coupled interactions between SC and AC joints. Based on consideration of these coupled interactions and modeling, the primary role of the upper trapezius appears to be in generating retraction of the clavicle at the SC joint and the middle and lower trapezius in generating external rotation of the scapula at the AC joint. The lower trapezius can also assist in producing scapular upward rotation relative to the clavicle. The serratus anterior has the largest moment arm to produce ST upward rotation, and based on its line of action, also contributes to ST posterior tilting. Understanding these SC and AC joint interactions, muscle function, and potential mechanisms of movement abnormalities in impingement patients can assist the therapist in targeting treatment interventions to specific movement problems.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Paula M. Ludewig, Department of Physical Medicine & Rehabilitation, Programs in Physical Therapy & Rehabilitation Sciences, The University of Minnesota, Minneapolis, MN, USA.
Jonathan P Braman, Department of Orthopaedic Surgery, The University of Minnesota, Minneapolis, MN, USA.
REFERENCES
- 1.Bang MD, Deyle GD. Comparison of supervised exercise with and without manual physical therapy for patients with shoulder impingement syndrome. Journal of Orthopaedic and Sports Physical Therapy. 2000;30:126–137. doi: 10.2519/jospt.2000.30.3.126. [DOI] [PubMed] [Google Scholar]
- 2.Bey MJ, Brock SK, Beierwaltes WN, Zauel R, Kolowich PA, Lock TR. In vivo measurement of subacromial space width during shoulder elevation: technique and preliminary results in patients following unilateral rotator cuff repair. Clinical Biomechanics. 2007;22(7):767–773. doi: 10.1016/j.clinbiomech.2007.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Borich MR, Bright JM, Lorello DJ, Cieminski CJ, Buisman T, Ludewig PM. Scapular angular positioning at end range internal rotation in cases of glenohumeral internal rotation deficit. Journal of Orthopaedic and Sports Physical Therapy. 2006;36:926–934. doi: 10.2519/jospt.2006.2241. [DOI] [PubMed] [Google Scholar]
- 4.Borstad JD, Ludewig PM. The effect of long versus short pectoralis minor resting length on scapular kinematics in healthy individuals. Journal of Orthopaedic and Sports Physical Therapy. 2005;35:227–238. doi: 10.2519/jospt.2005.35.4.227. [DOI] [PubMed] [Google Scholar]
- 5.Braman JP, Engel SC, LaPrade RF, Ludewig PM. In vivo assessment of scapulohumeral rhythm during unconstrained over head reaching in asymptomatic subjects. Journal of Shoulder and Elbow Surgery. 2009;18(6):960–967. doi: 10.1016/j.jse.2009.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Budoff JE, Nirschl RP, Ilahi OA, Rodin DM. Internal impingement in the etiology of rotator cuff tendinosis revisited. Arthroscopy. 2003;19(8):810–814. doi: 10.1016/s0749-8063(03)00732-1. [DOI] [PubMed] [Google Scholar]
- 7.Cools AM, Declercq GA, Cambier DC, Mahieu NN, Witvrouw EE. Trapezius activity and intramuscular balance during isokinetic exercise in overhead athletes with impingement symptoms. Scandinavian Journal of Medicine and Science in Sports. 2007;17:25–33. doi: 10.1111/j.1600-0838.2006.00570.x. [DOI] [PubMed] [Google Scholar]
- 8.Cools AM, Witvrouw EE, Declercq GA, Danneels LA, Cambier DC. Scapular muscle recruitment patterns: Trapezius muscle latency with and without impingement symptoms. American Journal of Sports Medicine. 2003;31:542–549. doi: 10.1177/03635465030310041101. [DOI] [PubMed] [Google Scholar]
- 9.Cools AM, Witvrouw EE, Declercq GA, Vanderstraeten GG, Cambier DC. Evaluation of isokinetic force production and associated muscle activity in the scapular rotators during a protraction-retraction movement in overhead athletes with impingement symptoms. British Journal of Sports Medicine. 2004;38:64–68. doi: 10.1136/bjsm.2003.004952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Culham E, Peat M. Functional anatomy of the shoulder complex. Journal of Orthopaedic and Sports Physical Therapy. 1993;18:342–350. doi: 10.2519/jospt.1993.18.1.342. [DOI] [PubMed] [Google Scholar]
- 11.Deutsch A, Altchek D, Schwartz E, Otis JC, Warren RF. Radiologic measurement of superior displacement of the humeral head in impingement syndrome. Journal of Shoulder and Elbow Surgery. 1996;5(3):186–193. doi: 10.1016/s1058-2746(05)80004-7. [DOI] [PubMed] [Google Scholar]
- 12.Dvir Z, Berme N. The shoulder complex in elevation of the arm: A mechanism approach. Journal of Biomechanics. 1978;11:219–225. doi: 10.1016/0021-9290(78)90047-7. [DOI] [PubMed] [Google Scholar]
- 13.Ebaugh DD, McClure PW, Karduna AR. Effects of shoulder muscle fatigue caused by repetitive overhead activities on scapulothoracic and glenohumeral kinematics. Journal of Electromyography and Kinesiology. 2006a;16:224–235. doi: 10.1016/j.jelekin.2005.06.015. [DOI] [PubMed] [Google Scholar]
- 14.Ebaugh DD, McClure PW, Karduna AR. Scapulothoracic and glenohumeral kinematics following an external rotation fatigue protocol. Journal of Orthopaedic and Sports Physical Therapy. 2006b;36:557–571. doi: 10.2519/jospt.2006.2189. [DOI] [PubMed] [Google Scholar]
- 15.Endo K, Yukata K, Yasui N. Influence of age on scapulo-thoracic orientation. Clinical Biomechanics. 2004;19:1009–1013. doi: 10.1016/j.clinbiomech.2004.07.011. [DOI] [PubMed] [Google Scholar]
- 16.Edelson Gm Teitz C. Internal impingement in the shoulder. Journal of Shoulder and Elbow Surgery. 2000;9(4):308–315. doi: 10.1067/mse.2000.105449. [DOI] [PubMed] [Google Scholar]
- 17.Endo K, Ikata T, Katoh S, Takeda Y. Radiographic assessment of scapular rotational tilt in chronic shoulder impingement syndrome. Journal of Orthopedic Science. 2001;6(1):3–10. doi: 10.1007/s007760170017. [DOI] [PubMed] [Google Scholar]
- 18.Falla D, Farina D, Graven-Nielsen T. Experimental muscle pain results in reorganization of coordination among trapezius muscle subdivisions during repetitive shoulder flexion. Experimental Brain Research. 2007;178:385–393. doi: 10.1007/s00221-006-0746-6. [DOI] [PubMed] [Google Scholar]
- 19.Fey AJ, Dorn CS, Busch BP, Laux LA, Hassett DR, Ludewig PM. Potential torque capabilities of the trapezius [abstract] Journal of Orthopaedic and Sports Physical Therapy. 2007;37(1):A44–A45. [Google Scholar]
- 20.Flatow EL, Soslowsky LJ, Ticker JB, et al. Excursion of the rotator cuff under the acromion: Patterns of subacromial contact. American Journal of Sports Medicine. 1994;22(6):779–788. doi: 10.1177/036354659402200609. [DOI] [PubMed] [Google Scholar]
- 21.Graichen H, Stammberger T, Bonel H, et al. Three-dimensional analysis of shoulder girdle and supraspinatus motion patterns in patients with impingement syndrome. Journal of Orthopaedic Research. 2001;19(6):1192–1198. doi: 10.1016/S0736-0266(01)00035-3. [DOI] [PubMed] [Google Scholar]
- 22.Haahr JP, Andersen JH. Exercises may be as efficient as subacromial decompression in patients with subacromial stage II impingement: 4–8-years' follow-up in a prospective, randomized study. Scandinavian Journal of Rheumatology. 2006;35:224–228. doi: 10.1080/03009740600556167. [DOI] [PubMed] [Google Scholar]
- 23.Harryman DT, Sidles JA, Clark JM, McQuade KJ, Gibb TD, Matsen FA. Translation of the humeral head on the glenoid with passive glenohumeral motion. Journal of Bone and Joint Surgery. 1990;72-A:1334–1343. [PubMed] [Google Scholar]
- 24.Hebert LJ, Moffet H, McFadyen BJ, Dionne CE. Scapular behavior in shoulder impingement syndrome. Archives of Physical Medicine and Rehabilitation. 2002;83(1):60–69. doi: 10.1053/apmr.2002.27471. [DOI] [PubMed] [Google Scholar]
- 25.Heyworth BE, Williams RJ. Internal impingement of the shoulder. American Journal of Sports Medicine. 2009;37(5):1024–1037. doi: 10.1177/0363546508324966. [DOI] [PubMed] [Google Scholar]
- 26.Johnson G, Bogduk N, Nowitzke A, House D. Anatomy and actions of the trapezius muscle. Clinical Biomechanics. 1994;9(1):44–50. doi: 10.1016/0268-0033(94)90057-4. [DOI] [PubMed] [Google Scholar]
- 27.Karduna AR, Kerner PJ, Lazarus MD. Contact forces in the subacromial space: Effects of scapular orientation. Journal of Shoulder and Elbow Surgery. 2005;14(4):393–399. doi: 10.1016/j.jse.2004.09.001. [DOI] [PubMed] [Google Scholar]
- 28.Kebaetse M, McClure P, Pratt N. Thoracic position effect on shoulder range of motion, strength and three-dimensional scapular kinematics. Archives of Physical Medicine and Rehabilitation. 1999;80:945. doi: 10.1016/s0003-9993(99)90088-6. [DOI] [PubMed] [Google Scholar]
- 29.Laudner KG, Myers JB, Pasquale MR, Bradley JP, Lephart SM. Scapular dysfunction in throwers with pathologic internal impingement. Journal of Orthopaedic and Sports Physical Therapy. 2006;36(7):485–494. doi: 10.2519/jospt.2006.2146. [DOI] [PubMed] [Google Scholar]
- 30.Lin JJ, Hanten WP, Olson SL, et al. Functional activity characteristics of individuals with shoulder dysfunctions. Journal of Electromyography and Kinesiology. 2005;15(6):576–586. doi: 10.1016/j.jelekin.2005.01.006. [DOI] [PubMed] [Google Scholar]
- 31.Ludewig PM, Behrens SA, Meyer SM, Spoden SM, Wilson LA. Three-dimensional clavicular motion during arm elevation: Reliability and descriptive data. Journal of Orthopaedic and Sports Physical Therapy. 2004;34(3):140–149. doi: 10.2519/jospt.2004.34.3.140. [DOI] [PubMed] [Google Scholar]
- 32.Ludewig PM, Borstad JD. Effects of a home exercise programme on shoulder pain and functional status in construction workers. Occupational & Environmental Medicine. 2003;60(11):841–849. doi: 10.1136/oem.60.11.841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ludewig PM, Cook TM. Alterations in shoulder kinematics and associated muscle activity in people with symptoms of shoulder impingement. Physical Therapy. 2000;80(3):276–291. [PubMed] [Google Scholar]
- 34.Ludewig PM, Phadke V, Braman JP, Hassett DR, Cieminski CJ, LaPrade RF. Motion of the shoulder complex during multiplanar humeral elevation. Journal of Bone and Joint Surgery. 2009;91(2):378–389. doi: 10.2106/JBJS.G.01483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ludewig PM, Reynolds JR. The association of scapular kinematics and glenohumeral joint pathologies. Journal of Orthopaedic and Sports Physical Therapy. 2009;39(2):90–104. doi: 10.2519/jospt.2009.2808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lukaseiwicz AC, McClure P, Michener L, Pratt N, Sennett B. Comparison of 3-dimensional scapular position and orientation between subjects with and without shoulder impingement. Journal of Orthopaedic and Sports Physical Therapy. 1999;29(10):574–583. doi: 10.2519/jospt.1999.29.10.574. [DOI] [PubMed] [Google Scholar]
- 37.McClure PW, Bialker J, Neff N, Williams G, Karduna A. Shoulder function and 3-dimensional kinematics in people with shoulder impingement syndrome before and after a 6-week exercise program. Physical Therapy. 2004;84:832–848. [PubMed] [Google Scholar]
- 38.McClure PW, Michener LA, Karduna AR. Shoulder function and 3-dimensional scapular kinematics in people with and without shoulder impingement syndrome. Physical Therapy. 2006;86(8):1075–1090. [PubMed] [Google Scholar]
- 39.McClure PW, Michener LA, Sennett BJ, Karduna AR. Direct 3-dimensional measurement of scapular kinematics during dynamic movements in vivo. Journal of Shoulder and Elbow Surgery. 2001;10(3):269–277. doi: 10.1067/mse.2001.112954. [DOI] [PubMed] [Google Scholar]
- 40.McQuade KJ, Dawson J, Smidt JL. Scapulothoracic muscle fatigue associated with alterations in scapulohumeral rhythm kinematics during maximum resistive shoulder elevation. Journal of Orthopaedic and Sports Physical Therapy. 1998;28:74–80. doi: 10.2519/jospt.1998.28.2.74. [DOI] [PubMed] [Google Scholar]
- 41.Mell AG, LaScalza S, Guffey P, et al. Effect of rotator cuff pathology on shoulder rhythm. Journal of Shoulder and Elbow Surgery. 2005;14(1 supplement):58S–64S. doi: 10.1016/j.jse.2004.09.018. [DOI] [PubMed] [Google Scholar]
- 42.Michener LA, McClure PW, Karduna AR. Anatomical and biomechanical mechanisms of subacromial impingement syndrome. Clinical Biomechanics. 2003;18(5):369–379. doi: 10.1016/s0268-0033(03)00047-0. [DOI] [PubMed] [Google Scholar]
- 43.Michener LA, Walsworth MK, Burnet EN. Effectiveness of rehabilitation for patients with subacromial impingement syndrome: A systematic review. Journal of Hand Therapy. 2004;17(2):152–164. doi: 10.1197/j.jht.2004.02.004. [DOI] [PubMed] [Google Scholar]
- 44.Neer CS. Impingement lesions. Clinical Orthopaedics and Related Research. 1983;173:70–77. [PubMed] [Google Scholar]
- 45.Okroro T, Reddy VR, Pimpelnarkar A. Coracoid impingement syndrome: A literature review. Current Reviews in Musculoskeletal Medicine. 2009;2(1):51–55. doi: 10.1007/s12178-009-9044-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Paley KJ, Jobe FW, Pink MM, Kvitne RS, ElAttrache NS. Arthroscopic findings in the overhand throwing athlete: Evidence for posterior internal impingement of the rotator cuff. Arthroscopy. 2000;16(1):35–40. doi: 10.1016/s0749-8063(00)90125-7. [DOI] [PubMed] [Google Scholar]
- 47.Pappas GP, Blemker SS, Beaulieu CF, McAdams TR, Whalen ST, Gold GE. In vivo anatomy of the Neer and Hawkins sign positions for shoulder impingement. Journal of Shoulder and Elbow Surgery. 2006;15(1):40–49. doi: 10.1016/j.jse.2005.04.007. [DOI] [PubMed] [Google Scholar]
- 48.Petersen BW, Nystrom CS, Pham TD, et al. Effects of elevation angle and plane of motion on subacromial and internal impingement [abstract] 2010;40(1):A68. [Google Scholar]
- 49.Phadke V, Camargo PR, Ludewig PM. Scapular and rotator cuff function during arm elevation: A review of normal function and alterations with shoulder impingement. Revista Brasileira de Fisioterapia. 2009;13(1):1–9. doi: 10.1590/S1413-35552009005000012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Sahara W, Sugamoto K, Murai M, Tanaka H, Yoshikawa H. 3D kinematic analysis of the acromioclavicular joint during arm abduction using vertically open MRI. Journal of Orthopaedic Research. 2006;24(9):1823–1831. doi: 10.1002/jor.20208. [DOI] [PubMed] [Google Scholar]
- 51.Sahara W, Sugamoto K, Murai M, Yoshikawa H. Three-dimensional clavicular and acromioclavicular rotations during arm abduction using vertically open MRI. Journal of Orthopaedic Research. 2007;25(9):1243–1249. doi: 10.1002/jor.20407. [DOI] [PubMed] [Google Scholar]
- 52.Senbursa G, Baltaci G, Atay A. Comparison of conservative treatment with and without manual physical therapy for patients with shoulder impingement syndrome: A prospective, randomized clinical trial. Knee Surgery, Sports, Traumatology Arthroscopy. 2007;15:915–921. doi: 10.1007/s00167-007-0288-x. [DOI] [PubMed] [Google Scholar]
- 53.Solem-Bertoft E, Thuomas KA, Westerberg CE. The influence of scapular retraction and protraction on the width of the subacromial space. An MRI study. Clinical Orthopaedics and Related Research. 1993;(296):99–103. [PubMed] [Google Scholar]
- 54.Soslowsky LJ, Thomopoulos S, Esmail A, et al. Rotator cuff tendinosis in an animal model: Role of extrinsic and overuse factors. Annals of Biomedical Engineering. 2002;30(8):1057–1063. doi: 10.1114/1.1509765. [DOI] [PubMed] [Google Scholar]
- 55.Su KP, Johnson MP, Gracely EJ, Karduna AR. Scapular rotation in swimmers with and without impingement syndrome: Practice effects. Medicine and Science in Sports and Exercise. 2004;36(7):1117–1123. doi: 10.1249/01.mss.0000131955.55786.1a. [DOI] [PubMed] [Google Scholar]
- 56.Teece RM, Lunden JB, Lloyd AS, Kaiser AP, Cieminski CJ, Ludewig PM. Three-dimensional acromioclavicular joint motion during elevation of the arm. Journal of Orthopaedic and Sports Physical Therapy. 2008;38(4):181–190. doi: 10.2519/jospt.2008.2386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Tsai NT, McClure PW, Karduna AR. Effects of muscle fatigue on 3-dimensional scapular kinematics. Archives of Physical Medicine and Rehabilitation. 2003;84:1000–1005. doi: 10.1016/s0003-9993(03)00127-8. [DOI] [PubMed] [Google Scholar]
- 58.van der Windt DA, Koes BW, de Jong BA, Bouter LM. Shoulder disorders in general practice: Incidence, patient characteristics, and management. Annals of the Rheumatic Diseases. 1995;54:959–964. doi: 10.1136/ard.54.12.959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wadsworth DJ, Bullock-Saxton JE. Recruitment patterns of the scapular rotator muscles in freestyle swimmers with subacromial impingement. International Journal of Sports Medicine. 1997;18:618–624. doi: 10.1055/s-2007-972692. [DOI] [PubMed] [Google Scholar]
- 60.Wang CH, McClure P, Pratt NE, Nobilini R. Stretching and strengthening exercises: Their effect on three-dimensional scapular kinematics. Archives of Physical Medicine and Rehabilitation. 1999;80:923–929. doi: 10.1016/s0003-9993(99)90084-9. [DOI] [PubMed] [Google Scholar]
- 61.Warner JJ, Micheli LJ, Arslanian LE, Kennedy J, Kennedy R. Scapulothoracic motion in normal shoulders and shoulders with glenohumeral instability and impingement syndrome: A study using moiré topographic analysis. Clinical Orthopaedics and Related Research. 1992;285:191–199. [PubMed] [Google Scholar]
- 62.Werner CM, Blumenthal S, Curt A, Gerber C. Subacromial pressures in vivo and effects of selective experimental suprascapular nerve block. Journal of Shoulder and Elbow Surgery. 2006;15(3):319–323. doi: 10.1016/j.jse.2005.08.017. [DOI] [PubMed] [Google Scholar]
- 63.Yanai T, Fuss FK, Fukunaga T. In vivo measurements of subacromial impingement: substantial compression develops in abduction with large internal rotation. Clinical Biomechanics. 2006;21(7):692–700. [Google Scholar]
- 64.Zuckerman JD, Kummer FJ, Cuomo F, Simon J, Rosenblum S, Katz N. The influence of coracoacromial arch anatomy on rotator cuff tears. Journal of Shoulder and Elbow Surgery. 1992;1(1):4–14. doi: 10.1016/S1058-2746(09)80010-4. [DOI] [PubMed] [Google Scholar]