Abstract
This longitudinal study identified common summer care arrangements for adolescents and examined whether those arrangements predicted risk for obesity (Body Mass Index (BMI) ≥ 85th percentile for age and gender) the following school year. Participants were a nationally representative sample of 1,766 adolescents ages 10–18 from the Panel Study of Income Dynamics-Child Development Supplement. Results showed that, beyond measures of BMI taken before the summer and several demographic aspects known to predict obesity, youth whose summer arrangements involved regular participation in organized activities (e.g., sports) showed significantly lower risk for obesity than other youth. This was most evident during early adolescence. Youth whose regular summer arrangement was predominated by parent care without organized activity participation showed the greatest risk for obesity.
Keywords: Summer, Obesity, BMI, Adolescence, Out-of-school, Organized Activities, Sports, Development
How adolescents spend their out-of-school time has important implications for their well-being (e.g., Mahoney, Vandell, Simpkins, & Zarrett, 2009). A variety of out-of-school care arrangements (e.g., parent care, self care, organized activities) have been studied and are associated with academic performance, social behaviors, and physical health. However, nearly all of the research on adolescence has focused on the school year, and this is problematic. For the typical American adolescent, summer represents about 23% of the calendar year and is the largest consecutive period of out-of-school time. Although the numbers of waking hours that youth spend during summertime rivals the amount of time they spend in the school context over an entire school year, there is a paucity of knowledge concerning what adolescents do during the summertime. For example, a literature search of PsychINFO for titles and abstracts published over the past 50 years in more than a dozen top journals concerned with adolescence and development yields a total of 14 articles that include the terms “summer” or “summertime.” Thus, while nearly one quarter of youth development occurs during the summer, it appears that fewer than 1 in 10,000 published studies on adolescence were concerned with summer in the last half century. As a result of the limited research, the extent to which summer care arrangements may affect adolescent health and development remains largely unknown.
This study begins filling the knowledge gap on some important aspects of adolescence and summertime. Using a nationally representative sample, the investigation examines what the regular summer care arrangements for adolescents are and to what extent those arrangements relate a risk for becoming obese. The topic is important insofar obesity is now a global epidemic and represents one of the most significant health problems confronting adolescents today (Anderson & Butcher, 2006). The research is also timely because the American Recovery and Reinvestment Act of 2009 provided a $10 billion increase in Title I funds that included the development of new summer activities (U.S. Department of Education, 2009). The literature review begins with an overview of the adolescent obesity problem. Research on the role of organized out-of-school activities and summer care arrangements in the development of obesity is then discussed.
Prevalence of and Contributors to Risk for Obesity during Adolescence
Obesity has been deemed a global epidemic by the World Health Organization (e.g., Anderson & Butcher, 2006). The condition is linked to a variety of short- and long-term health problems including sleep apnea, Type II diabetes, cardiovascular disease, stroke, liver and gallbladder disease, depression, social rejection, and mortality (Centers for Disease Control (CDC), 2009b). The rate of obesity for children and adolescents has increased markedly in recent decades. Between 1963–1965 and 2003–2006 the obesity rates for children ages 6–11 quadrupled from 4% to 17% and more than tripled for adolescents ages 12–19 going from 5% to 17.6% (Hedley et al., 2004; Ogden, Carroll, & Flegel, 2008; Ogden, Flegal, Carroll, & Johnson, 2002). Stability estimates of obesity from adolescence to adulthood are high (Campbell, Katzmarzyk, Malina, Rao-Louis Pérusse, Bouchard, 2001; Crimmins et al., 2007). This is of concern because the health risks identified above are most common when obesity is chronic. This fact underscores the importance of prevention and treatment efforts in childhood and adolescence.
Calorie intake that regularly exceeds energy expenditure is the primary cause of obesity, but a variety of factors affect the extent to which this occurs. An expanding toxic food environment that has made high fat and sugar laden products cheap and abundant coupled with an increasing sedentary lifestyle driven by changes in technology, work, and leisure are common explanations for the historic rise in obesity (e.g., Krishnamoorthy, Hart, & Jelalian, 2006; Wang & Brownell, 2005).
However, rates of obesity do vary according to individual and demographic aspects. With respect to individual aspects, prior obesity status matters. Youth who are obese during childhood are significantly more likely to be obese adolescents (e.g., Campbell et al., 2001). In addition, adolescent obesity has also been found to differ by gender, with recent studies showing males ages 12–19 are somewhat more likely to be overweight or obese than females (Ogden et al., 2008). Although related to socioeconomic status in complex ways (Anderson & Butcher, 2006; Kumanyika & Grier, 2006), research has shown that African-American and Hispanic children have higher rates of obesity than their White counterparts (e.g., Ogden et al., 2008). Lastly, there is some evidence that adolescence represents a distinct period of risk for the development of obesity (e.g., Mustillo, Worthman, Erkanli, Keeler, Angold, & Costello, 2003) and that some youth, particularly females, show a marked increase in obesity during early-to-middle adolescence (e.g., Dietz, 1994).
With respect to the adolescent’s ecology, the tendency for higher rates of obesity to be evident among low-income Americans may be due to the fact that less nutritious food is often cheaper and more accessible (Wang & Brownell, 2005). Moreover, beyond race/ethnicity, parental education positively predicts both healthy dietary behaviors (e.g., Lowry, Kann, Collins, & Kolbe, 1996; Videon & Manning, 2003) and physical activity levels (Kimm & Obarzanek, 2002). Variation in neighborhood safety can also contribute to obesity by encouraging or discouraging physical activity (e.g., Lopez, 2007; Molnar, Gortmaker, Bull, & Buka, 2004; Mota, Ribeiro, & Santos, 2009) and influencing availability of supervised recreational activities (e.g., Lord & Mahoney, 2007; Nelson, Gordon-Larsen, Song, & Popkin, 2006).
Organized Activity Arrangements during the Summer and Risk for Obesity
On average, care arrangements that offer a healthy diet and reduce sedentary behavior should be the least likely to encourage obesity. Perhaps for this reason, youth participation in organized out-of-school activities such as sports, after-school programs, and extracurricular activities have received attention from researchers interested in obesity. These activities tend to limit eating, offer opportunities for physical recreation, and may encourage healthy lifestyles (Mahoney, Lord, & Carryl, 2005a; Vandell et al., 2005).
Participation in organized activities has been linked to lower rates of obesity. For example, Mahoney and colleagues (2005a) tracked a sample of disadvantaged school-aged children over several years and found that, after controlling for earlier measures of BMI and demographic factors, those who became involved in after-school programs (ASPs) showed less marked increases in BMI and significantly lower rates of obesity at the end of the study than similar children who did not participate in ASPs. The differences in obesity were particularly apparent for children who showed regular and durable participation in ASPs over time. Similarly, Elkins and colleagues (2004) conducted a cross-sectional study of 5,484 low-income adolescents. Controlling for age, grade, and gender, the number of athletic activities that youth participated in was associated with a significant reduction in the likelihood of being overweight or obese. An exception was male football players who tended to have relatively high BMIs.
Despite popular notions of summer as a highly active time for youth, the risk for obesity is actually higher during the summer than the school year. For example, beyond individual and demographic predictors, von Hippel, Powell, Downey, and Rowland’s (2007) analysis of data from the Early Childhood Longitudinal Study found that the rate of children’s BMI increase during summer was more than double the rate during the school year. Results also showed that the gaps in obesity between African-American or Hispanic children and their White counterparts are driven largely by BMI increases during the summer rather than the school year. Given that summer appears to be a risky season for obesity and that organized activity participation is associated with relatively low BMI and obesity, the primary expectation of this study is that youth summer care arrangements featuring regular participation in organized activities should, on average, predict a subsequently lower BMI and risk for obesity compared to summer arrangements that do not feature such participation.
Moderating Factors
Several factors could moderate the likelihood that adolescent summer care arrangements featuring regular participation in organized activities may reduce the risk for obesity. In this study, we consider age, duration of participation, and gender as potential moderators.
Age
Scholars have suggested the importance of age in understanding developmental outcomes associated with organized activity participation (e.g., Riggs & Greenberg, 2004b). However, little empirical research has examined age a moderator. Instead, age (or grade) is usually treated as a control variable. Nonetheless, age does predict the types of activities in which young people participate (e.g., Grossman et al., 2002; Laird, Pettit, Dodge, & Bates, 1998; Vandell, Pierce, & Dadmisman, 2005) and activity types, in turn, differentially predict developmental outcomes (e.g., Barber et al., 2001; Hofferth & Sandberg, 2001; Larson, 2006; Mahoney et al., 2009). Moreover, Riggs and Greenberg (2004a) found that an ASP for Latino children was linked to larger reading gains for younger vs. older children, suggesting that age can moderate activity-related outcomes.
With respect to the current study, early adolescence represents a point when many aspects of the developmental system undergo rapid change (Lerner, 2006). Systemic reorganization occurs as a result of simultaneous developments in pubertal maturation, changing social ecologies (e.g., schools, peer groups), and cognitive advancements. This can be a stressful period in development (e.g., Eccles & Midgley, 1989) and one response the body has to stress is to become more efficient at storing energy which may increase the risk for obesity (e.g., Lohman, Stewart, Gundersen, Garasky, Eisenmann, 2009). As noted previously, this may help to explain why early adolescence may be a particularly risky period for the development of obesity.
However, with reference to organized activity participation, when in this state of reorganization, the developing system may be relatively more open to modifications involving the healthy behavior patterns encouraged by such activities. Although changes in the developmental system continue throughout the lifespan, to the extent that the system moves toward a state of equilibrium in later adolescence, correlated constraints on that system may make rapid, profound changes in health-related behaviors less likely (Cairns & Cairns, 1994). Furthermore, research suggests that opportunities to begin participating in organized activities may be greater during early vs. later adolescence (e.g., McNeal, 1998). This is so because as adolescence proceeds, activity-related competition and skill requirements in certain activities (e.g., sports) increase and bar entry for some youth. These restrictions could make it more difficult for obese children to become participants in activities that could promote health as they move across adolescence. Collectively, this supports a theoretical prediction that having organized activities as a care arrangement might protect youth from becoming obese and this associated benefit may be more apparent in early adolescence compared to later adolescence.
Duration of participation
Studies have found that psychosocial and educational benefits associated with organized activity participation accumulate over time such that positive outcomes are more likely when involvement is durable (e.g., Darling, Caldwell, & Smith, 2005; Fredricks & Eccles, 2006; Welsh, Russell, Williams, Reisner, & White, 2002; Zaff, Moore, Papillo, & Williams, 2003). It seems reasonable to expect that duration of participation will matter for adolescent obesity as well and some evidence supports this notion (Mahoney et al., 2005a). Accordingly, the associated benefits of organized activity participation should be greater for youth who show a history of durable participation over time, including regular participation during summertime, than those with transient participation.
Gender
As noted earlier, the risk for adolescent obesity differs by gender. Some research shows that the types of activities in which youth participate vary along these lines as well. For example, boys tend to participate in sports more often than do girls (e.g., Denault & Poulin, 1999; Eccles, Barber, Hunt, & Stone, 2003; Gibbons, Lynn, & Stiles, 1997; Marsh & Kleitman, 2003) and organized activity participation appears to affect boys and girls differently (e.g., Eitle, 2005; Pettit, Laird, Bates, & Dodge, 1997; Pierce, Hamm, & Vandell, 1999; Pierce, Vandell, & Bolt, 2010). Accordingly, it is of interest to explore the potential moderating role of gender in the association between participation in organized summer activities and subsequent risk for obesity.
Comparison of Summer Care Arrangements and Risk for Obesity
From a bioecological perspective to development (Bronfenbrenner & Morris, 2006), adolescent care arrangement involve unique person-context interactions. As such, different summer arrangements may confer different levels of risk for obesity. In addition, youth sometimes experience more than one common arrangement. Comparing potential differences across specific, alternative out-of-school ecologies (e.g., Mahoney et al., 2005b; Pettit et al., 2007) and summer experiences (e.g., Lumeng, Gannon, Appulgliese, Cabral, & Zuckerman, 2005) has been shown to be important.
During adolescence, common summer arrangements include parent care, self care, care from other adults (e.g., relatives), and organized activities (e.g., U.S. Census Bureau, 2009). It is presently unknown which of these arrangements may be more, or less, likely to encourage adolescent obesity. However, we anticipate that summer arrangements which often restrict youth to the home, permit extended passive leisure (e.g., TV, video games), and offer chances for unhealthy snacking will place youth at-risk for obesity. Parent care is a summer arrangement likely to feature these conditions. For example, evidence suggests that time with peers and friends may increase activity levels for young people more than time with parents (e.g., Salvy et al., 2008; Salvy et al., 2009). If parent care is the adolescent’s primary summer arrangement, then peer-related avenues for energy expenditure could be relatively diminished while convenient opportunities for snacking could be high. In contrast, organized activity arrangements are unlikely to be characterized by these conditions and should be negatively associated with the risk for obesity. By extension, an arrangement that combines regular parent care with regular organized activity care should be less predictive of obesity that one featuring parent care only.
Expected Findings
Based on the literature review, three main findings are expected. (1) Youth whose regular summer care arrangements involve organized activity participation will show a lower BMI percentile and risk for obesity the following school year compared to other youth. (2) The association between regular summer care arrangements involving organized activity participation with BMI percentile and risk for obesity will be moderated according duration of participation and participant age. Specifically, durable participation in organized activities across two waves of data will predict a lower BMI percentile and risk for obesity compared to organized activity participation at only one assessment. In addition, the associations between involvement in summer organized activity arrangements and risk for obesity will be most apparent during early adolescence compared to later adolescence. Moderation involving gender is explored, but no specific expectations are put forth. (3) In a comparison of specific alternative summer care arrangements, youth who regularly experience parent care as a sole, regular arrangement are expected to show the greatest risk for obesity the following school year. Because regular involvement in organized summer activities is anticipated to predict relatively low risk for obesity, the associated benefit of organized activity participation will be most apparent when comparing youth regularly involved in summer parent care who do, and who do not, also experience regular participation in organized summer activities.
All expected findings should hold after modeling earlier measures of youth BMI and control variables that consist of demographic factors (i.e., age, gender, race/ethnicity, head of household education level, family income) known to predict obesity as described earlier. In addition, the primary caregiver’s employment status, whether she/he works non-standard hours, single parent status, and perceptions of neighborhood safety are included as controls because these factors have been shown to predict the types of out-of-school experiences that youth have (e.g., Mahoney et al., 2009; Shann, 2001; U.S. Census Bureau, 2009) and are closely tied to other known predictors of child obesity (e.g., household income).
Method
Dataset and Participants
Data were drawn from the Child Development Supplement (CDS) to the Panel Study for Income Dynamics (PSID). The PSID began in 1968 as a nationally representative sample of 5,000 American families who were interviewed annually until 1997, after which data collection occurred on a biennial basis. In 1997, the PSID added the CDS to address the lack of information on children. Thus, the objective of the CDS was to provide a nationally representative longitudinal database of children and their families to support studies on the dynamic process of human development (Mainieri, 2006).
The first two waves of this longitudinal database are included in this study. CDS-I collected information from 2,394 families (3,563 children ages 0–12) who represent 88% of all families from PSID assessment in 1997. The follow-up wave (CDS-II) collected information from 2,019 families (2,907 children and adolescents ages 5–18) whose families remained active in the PSID panel. Overall, 91% of families who took part in CDS-I (1997) continued to participate in CDS-II (2002–2003). The reduction in sample size from CDS-I to CDS-II results either from attrition due to non-participation (N = 364) or because some families had left the PSID study before 2001 or were not part of the core PSID sample in 1968 (N = 292).
A weighting system was devised for the PSID-CDS to adjust for unequal probabilities of being sampled, attrition over time due to not being interviewed and non-response, and incorporates a post-stratification factor to ensure that the data are nationally representative (Gouskova, 2001). All subsequent descriptive statistics reported and analyses performed were computed using this sample weight.
Research sample demographics
The research sample for this study consists of 1,766 adolescents (M age = 14.33, SE age = .08, Range age = 10–18) from 956 families who participated in both CDS-I and CDS-II. Median family household income was $48,020 (M = $74,699, SE = $2,634); educational status of the CDS-II family head of household was: less than high school (18%), high school completion (31%), some college (23%), four-year college degree (18%), post-graduate education (10%); and gender and racial/ethnic status were: male (49%), White (62%), Black or African-American (17%), Hispanic or Latino (15%), Asian or Pacific Islander (1%), American Indian or Alaskan Native (0.6%), and Multi-Racial (3%).
Procedure
Interviews and assessments with a primary caregiver (usually the biological mother) and target adolescent provided the information for this study. Depending on the measure considered, primary caregiver information was collected in person and/or by telephone; information from adolescents was always obtained in person. Trained staff conducted the interviewers. Primary caregivers received $75 and adolescents received $20 for their participation.
Parent interviews occurred at different times during the school year. Accordingly, the amount of time that passed between CDS-II summer and parents’ retrospective reports (see below) of their adolescent’s summer arrangements during the following school year varied. To account for this recall lag, the number of days between an arbitrarily chosen mid-point in the summer (July 15, 2002) and the parent’s interview date the following school year was computed for each participant and included as a covariate in all analyses.
Assessment schedule
The participants were assessed at two points in time during the school year (i.e., CDS-I school year in 1997–1998 and CDS-II school year in 2002–2003). During CDS-II school year, parents were asked to retrospectively report information about their child’s regular care arrangements the past summer (i.e., CDS-II summer in 2002). Taken together, three time points are referenced in the present study and occur in the following sequence: CDS-I school year, CDS-II summer (reported retrospectively), and CDS-II school year.
Measures
Organized activities and other adolescent care arrangements
During CDS-I school year, primary caregivers reported whether their child was currently participating in organized activities including extracurricular activities (e.g., gymnastics, scouts, music lessons, sports teams, Boys & Girls Clubs) and after-school programs. Participation was coded dichotomously (0 = no, 1 = yes) reflecting whether the child was involved in any of the organized activities during the CDS-I school year. This variable was included in all analyses.
During CDS-II school year, primary caregivers were asked to recall whether each of the following care arrangements were used (yes/no) by their child on a regular basis during the previous summer: care from a parent, self care (i.e., not supervised by a parent or adult), care from a relative (and whether under/over age 13), care from a non-related adult, summer programs, extracurricular activities, and organized sports. Primary caregivers could identify multiple regular summer care arrangements for their child. Responses were categorized into four types of summer arrangements and coded dichotomously (0 = no, 1 = yes): 1) parent care, 2) self/sibling care (sibling under age 13), 3) care from other adults (e.g., relative over age 13, sitter), and 4) organized activity care (sports, extracurricular activities, and/or summer programs).
Parents provided an important account of their child’s summer care arrangements, but reports by others (e.g., the child himself or herself) may differ. If comparable information is gathered from these independent reports, then the validity of parent-reported data is strengthened. Although child reports of summer care arrangements were not available in the PSID-CDS, it was possible to compare parent- and child-reports of participation in organized sports taken during the CDS-II school year assessment. Cross-tabulation analyses show that when parents reported their child participated in organized sports, the child agreed in 85% of cases (χ2 (1, 1737) = 367.61, p < .001). Similarly, the correlation between parent-reported participation in organized sports and child-reported frequency of sports participation was r (1737) = .54, p < .001. Thus, parent report about their child’s organized sports participation showed a moderate and statistically significant level of correspondence with parallel information provided by the child.
Body mass index (BMI) and risk for obesity status
BMI was determined through individual measurements of height and weight taken during CDS-I school year (serving as a control variable) and the CDS-II school year (serving as the outcome). To assess height, trained interviewers asked the participants to remove their shoes and stand against a wall or door. Then, a Post-it note was attached to the wall directly above the participant’s head and a mark was placed on the note at the child’s height. A tape measure was used to measure the distance from the floor to the mark on the Post-it. To assess weight, the participant was asked to remove their shoes and empty their pockets. A Strain-Gauge Lithium Bath Scale "THINNER MS-7" model was then activated and set to zero. The participant was asked to step onto the scale and stand in the center of the unit for 5–10 seconds.
At both time points, BMI was computed according to the Centers for Disease Control (CDC, 2009a) formula (BMI = (weight in pounds/(height in inches) x (height in inches)) x 703). The BMI for each participant was then transformed in a BMI percentile according to standard CDC charts for age and gender and a dichotomous coding of risk for obesity was created from the percentile (BMI ≥ 85th percentile). Distributional estimates of BMI obtained from the PSID-CDS are comparable to those obtained from the National Health Interview Survey (Andreski, Gouskova, McConagle, & Shoeni, 2005).
Demographic variables
Variables involving individual and demographic aspects collected during the CDS-II school year were included in all analyses and, unless noted otherwise, Cronbach’s α ≥ .78 for all scales reported. Individual aspects included child age (years and months), gender (0 = female, 1 = male), and a dummy coded variable indicating race/ethnicity in four categories as follows: White (reference group), Black or African American, Hispanic or Latino, or Other Race/Ethnicity. Demographic aspects included primary caregiver reports of total family household income in 2000 including taxable and transfer income of head of household, wife/husband, and other family members, and total social security income. To ease the interpretation of results, income was rescaled into units of $10,000. Educational level of the head of household was coded to represent the actual grade of school completed (e.g., 8 = completion of eighth grade; 17 = completion of some postgraduate work). Single parent status of the primary caregiver was coded dichotomously (0 = no, 1 = yes). Whether the primary caregiver was employed and, if so, whether she/he worked a non-standard schedule (i.e., other than a regular daytime schedule) were coded dichotomously (0 = no, 1 = yes). Finally, primary caregiver perceptions of neighborhood safety were determined through a two-item scale. Scale items included “How would you rate your neighborhood as a safe place to raise children?” (1 = excellent, 5 = poor) and “How safe is it to walk around in your neighborhood alone after dark?” (1 = completely safe, 4 = extremely dangerous). Items were standardized and averaged (α = .65).
Data Analysis
Data were analyzed using Stata 11 software. Missing data was handled using the Stata ICE program for multiple imputation and 20 imputations were conducted. In addition to the sample weighting described earlier, the Stata cluster option was used to account for the dependence of observations caused by the fact that PSID-CDS assessments sometimes included siblings from the same family.
Results
Organized Activity Arrangements during the Summer and Risk for Obesity
Overall, 32.6% of adolescents participated in organized activities as part of a regular summer care arrangement. Considering the three types of summertime organized activities that were assessed, 30.3%, 3.0%, and 1.3% of regular summer arrangements involved sports, extracurricular activities, and summer programs, respectively. Accordingly, results are driven largely by youth participation in summer sports. 1
Regression analyses were performed to evaluate the first two study expectations: 1. Whether summer care arrangements that involve regular participation in organized activities predict a relatively low BMI percentile and risk for obesity the following school year. 2. Whether age, duration of participation, or gender moderate the association anticipated by the first expectation. To begin, linear regressions were conducted to examine whether, net of controls, summer arrangements involving organized activity participation were predictive of BMI percentile during the subsequent school year. Two regression models were compared. In Model 1, BMI percentile during the CDS-II school year was regressed on CDS-I school year BMI and nine individual and demographic factors (i.e., age, gender, race/ethnicity, head of household education level, single parent status, family income, primary caregiver employment status, primary caregiver working non-standard hours, and interview lag time). In Model 2, arrangements involving organized activities at CDS-I and CDS-II summer were added (i.e., Expectation 1) along with interactions to test the presumed moderator variables (Expectation 2). Table 1 shows the results.
Table 1.
Ordinary least squares regression models (N = 1631) predicting adolescent BMI percentile during CDS-II school year.
| Variables | Model 1 | Model 2 | ||
|---|---|---|---|---|
| β | RSE | β | RSE | |
| BMI CDS-I | 2.63*** | .22 | 2.62*** | .21 |
| Child Age CDS-II | −1.03*** | .38 | −1.91*** | .49 |
| Child Gender (Male) CDS-II |
1.81 | 1.85 | 1.83 | 2.24 |
| Child Race 1 CDS-II | ||||
| Black | 6.41* | 2.33 | 5.69* | 2.31 |
| Hispanic | −2.12 | 3.57 | −2.21 | 3.49 |
| Other | 4.39 | 4.22 | 3.36 | 4.33 |
| Family Income CDS-II ($10k) | −.09 | .09 | −.07 | .09 |
| Education of Head CDS-II | −1.08** | .35 | −.99** | .35 |
| Single Parent | −3.28 | 2.19 | −3.02 | 2.20 |
| PC Employed | .30 | 2.12 | .61 | 2.08 |
| PC Non-Standard Work Hours |
.63 | 2.49 | .66 | 2.48 |
| Neighborhood Safety | −.01 | .97 | −.28 | .95 |
| Interview Lag | .18 | 8.00 | .21 | 8.00 |
| Organized Activity Arrangement | ||||
| CDS-I | −2.31 | 2.55 | ||
| CDS-II Summer | − 2.70 | 5.25 | ||
| CDS-II Summer x Age | 2.85*** | .79 | ||
| CDS-I x | 2.80 | 5.47 | ||
| CDS-II Summer | ||||
| CDS-II Summer x Gender | .92 | 3.82 | ||
| RVI | .180 | .196 | ||
Reference category is White.
Note: RSE = Robust Standard Error, BMI = Body Mass Index, CDS-I = Child Development Supplement Wave I, CDS-II = Child Development Supplement Wave II, PC = Primary Caregiver, Head = Head of Household, RVI = Relative Variance Increase
p < .05,
p < .01,
p < .001
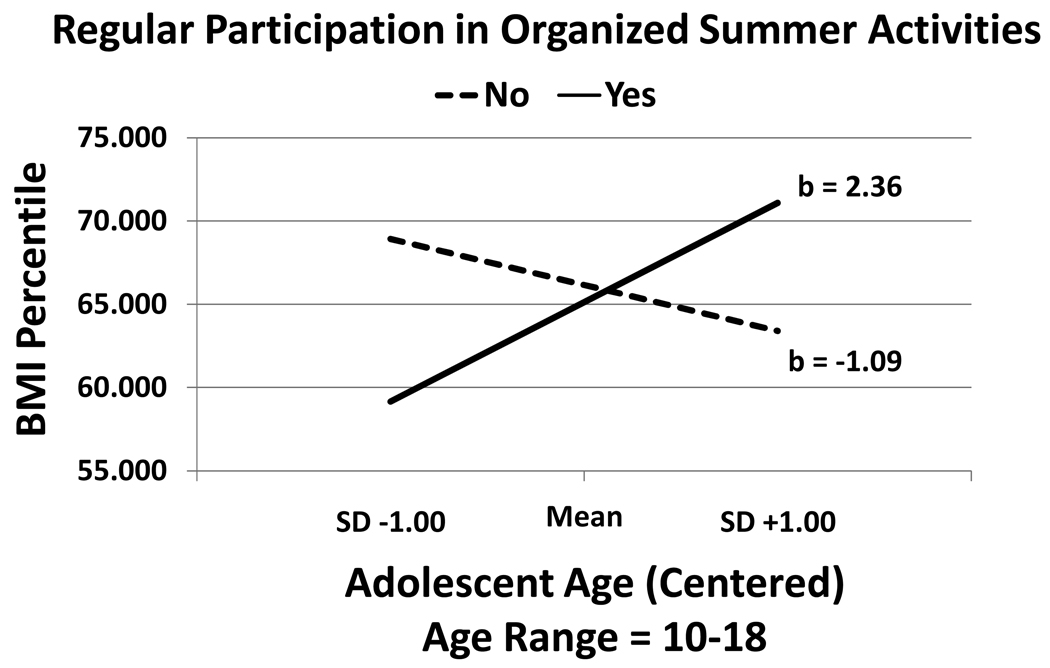
For model 1, BMI percentile during the CDS-II school year was significantly higher for youth with a higher BMI at CDS-I, for younger adolescents, for Black (vs. White) youth, and when the household head had a lower level education. In Model 2, adding information on arrangements that involved regular participation in organized activities and related interactions modestly increased the relative variance accounted for in the model. No significant main effects of regular participation in organized activities during CDS-I or CDS-II summer were found. However, there was a significant age x CDS-II summer activity interaction. Following procedures described in Holmbeck (2002), the interaction is depicted in Figure 1. Youth whose summer arrangements did involve regular participation in organized summer activities tended to have a relatively low BMI percentile in early adolescence, but a relatively high BMI percentile during later adolescence, compared to youth whose summer arrangements did not involve regular participation in organized summer activities. Interactions involving duration (i.e., the CDS-I x CDS-II summer term) of organized activity participation or gender were not significant.
Figure 1.
Regression lines for adolescent age (+/−1 SD) and BMI percentile during the school year plotted according to whether participation in organized activities was a regular care arrangement the previous summer.
A parallel set of logistic regressions were conducted to examine risk for obesity. Results are shown in Table 2. For model 1, risk for obesity during the CDS-II school year was significantly higher for youth with a higher BMI at CDS-I, for younger adolescents, males, and when the household head had a lower level education. Adding information on arrangements that involved regular participation in organized activities and related interactions increased the relative variance accounted for in the model. Main effects involving regular participation in organized activities at CDS-I and CDS-II summer were significant. First, the proportion of youth at-risk for obesity who participated in organized activities during the CDS-I school year was significantly lower during the CDS-II school year (M = .32, SE = .03) than youth who did not participate in such activities at CDS-I (M = .43, SE = .02). Second, the proportion of youth whose care arrangement during CDS-II summer included regular participation in organized activities was significantly lower during the CDS-II school year (M = .26, SE= .04) compared to youth who did not have such an arrangement (M = .43, SE = .03). Interactions involving age, duration of organized activity participation, or gender were not significant.
Table 2.
Logistic regression models (N = 1631) predicting risk for obesity (BMI ≥ 85th percentile) during CDS-II school year.
| Variables | Model 1 | Model 2 | ||
|---|---|---|---|---|
| β | RSE | β | RSE | |
| BMI CDS-I | .23*** | .03 | 23*** | .03 |
| Child Age CDS-II | − .17*** | .03 | − .18*** | .04 |
| Child Gender (Male) CDS-II |
.37* | .14 | .28 | .18 |
| Child Race 1 CDS-II | ||||
| Black | .21 | .21 | .18 | .21 |
| Hispanic | −.28 | .32 | −.33 | .31 |
| Other | .29 | .33 | .15 | .32 |
| Family Income CDS-II ($10k) | − .02 | .07 | − .04 | .07 |
| Education of Head CDS-II | − .10** | .03 | − .08* | .03 |
| Single Parent | − .32 | .19 | − .35 | .19 |
| PC Employed | .04 | .18 | .06 | .18 |
| PC Non-Standard Work Hours |
−. 14 | .21 | − .15 | .22 |
| Neighborhood Safety | .02 | .08 | −.02 | .08 |
| Interview Lag | .06 | .66 | .04 | .07 |
| Organized Activity Arrangement | ||||
| CDS-I | − .51* | .22 | ||
| CDS-II Summer | − .92* | .44 | ||
| CDS-II Summer x Age | .04 | .07 | ||
| CDS-I x | .67 | .46 | ||
| CDS-II Summer | ||||
| CDS-II Summer x Gender | .30 | .34 | ||
| RVI | .142 | .154 | ||
Reference category is White.
Note: RSE = Robust Standard Error, BMI = Body Mass Index, CDS-I = Child Development Supplement Wave I, CDS-II = Child Development Supplement Wave II, PC = Primary Caregiver, Head = Head of Household, RVI = Relative Variance Increase
p < .05,
p < .01,
p < .001
Comparison of Summer Care Arrangements and Risk for Obesity
The third expected finding was that parent care as a sole, regular summer arrangement would be linked to the greatest risk for adolescent obesity the following school year. It was further anticipated that the associated benefit of organized activity participation would be most apparent when contrasting youth in parent care who did, and who did not, also regularly participate in organized activities during the summer. To assess this expectation, all combinations of regular summer care arrangements that involved at least 5% of the sample were identified (cf., Bergman, Magnusson, & El-Khouri, 2003). Seven arrangements met this criterion as follows: Parent Care (29%) (479/1631), Parent Care and Organized Activity Care (12%) (n = 199/1631), Self Care (28%) (n = 455/1631), Self Care and Organized Activity Care (8%) (n = 129/1631), Other Adult Care (10%) (n = 166/1631), Other Adult Care with Organized Activity Care (6%) (n = 104/1631), and Organized Activity Care (6%) (n = 99/1631).
Regression analyses were performed to examine potential differences for both BMI percentile and risk for obesity across the seven arrangements. As above, individual, demographic, and interaction terms were modeled. Descriptive statistics for these subgroup comparisons are shown in Table 3. With respect to BMI percentile, youth who regularly experienced both self care and organized summer activities as a regular arrangement had significantly higher BMI percentiles than youth who experienced only self care as a regular summer care arrangement. In addition, there was a significant age x summer care arrangement interaction (β = .51, SE = .22, t = 2.36, p < .05). Follow-up pairwise comparisons of age and arrangement showed that youth who regularly experience self care as a summer arrangement were significantly older (p < .001) than youth in all alternative care arrangements (M age range difference = 2.5 to 3.2 years older). Accordingly, adolescents who were older experienced self care as a regular summer care arrangement more often than their younger counterparts. Among this relatively older group of youth experiencing self care, BMI percentiles were higher for those who also were regular participants in organized summer activities. No other pairwise comparisons or interactions involving duration of organized activity participation or gender were significant.
Table 3.
Youth BMI percentile and proportion at-risk for obesity (BMI ≥ 85th percentile) the following school year according to regular summer care arrangements.
| Summer Care Arrangements |
BMI Percentile | Proportion At-Risk for Obesity |
||
|---|---|---|---|---|
| M | SE | M | SE | |
| Parent Care | 66.40 a, b | 2.43 | .44 a | .04 |
| Parent Care with Organized Activity Care |
64.04 a | 2.52 | . 35 b, c | .04 |
| Self Care | 63.37 b | 1.78 | . 33 b, c | .03 |
| Self Care with Organized Activity Care |
69.11 a, b | 2.51 | .31 a, b, c | .05 |
| Other Adult Care | 69.19 a, b | 3.18 | .37 a, b | .05 |
| Other Adult Care with Organized Activity Care |
67.01 a, b | 4.58 | .36 a, b | .07 |
| Organized Activity Care | 58.17 a, b | 6.76 | .19 c | .07 |
Notes: BMI = Body Mass Index. Adjusted marginal means are reported. Means in each column that do not share the same subscript are significantly different from one another (p < .05).
Turning to risk for obesity as the outcome, a comparison of the seven arrangements (Table 3) showed that the risk was highest for youth who regularly experienced parent care as a sole summer arrangement. Indeed, 44% of these youth were at-risk for obesity the following school year. This rate was significantly higher compared to youth whose regular summer arrangement was parent care with organized activity participation (35%) and to youth whose sole, regular arrangement was either self care (33%) or organized activity care (19%). Risk for obesity among the latter group (i.e., only organized activity care) was also significantly lower than adolescents experiencing regular summer care from other adults. No other pairwise comparisons or interactions involving age, duration of participation, or gender were significant.
Discussion
This study appears to be the first investigation to examine whether adolescent summer care arrangements relate to the development of risk for obesity. The main result is that the summer arrangements adolescents experience do predict their subsequent risk for obesity. This is new information. Given that the investigation involves a nationally representative, longitudinal sample of youth ranging in age from early to late adolescence (10–18 years of age) the findings have the potential to generalize broadly. Moreover, because the results hold after modeling multiple known contributors to obesity and the selection of care arrangements, the findings should encourage further study in this area.
There were three main expectations in this study and the findings related to each will be discussed in turn according to results for BMI percentile and risk for obesity, respectively. First, both BMI percentile and risk for obesity were expected to be relatively low for youth whose summer care arrangements involved regular participation in organized activities. This result was anticipated to be more apparent for early adolescents and those who showed durable participation in activities across the two assessments. Consistent with this expectation, the BMI percentile of early adolescents whose regular summer care arrangements included participation in organized activities was significantly lower than similar youth that did not experience such an arrangement. In this study, as in other work (e.g., Deitz, 1994), BMI percentile and risk for obesity were somewhat higher in early vs. later adolescence. As such, the finding may indicate that participation in organized summer activities has a larger associated impact on BMI during an age period when young people are at heightened risk for becoming obese. This resonates with research showing greater associated benefits of organized activity participation among youth at high vs. low risk for developing other types of adjustment problems (e.g., Cosden, Morrison, Albanese, & Macias, 2001; Knutson, 2005; Mahoney & Cairns, 1997). However, the age-related difference may also involve changing patterns of care arrangements across adolescence and we return to this issue below.
In contrast, the reverse finding was also observed (i.e., later adolescents whose regular summer care arrangements included participation in organized activities showed relatively high BMI percentiles) and this was not expected. The result could be explained by the fact that the types of organized summer activities in which adolescents participated were primarily sport-related. Later adolescents that participate in summer sports during high school often do so to prepare for the upcoming athletic season. Indeed, during the summer, many high schools offer training programs where athletes exercise and practice to gain strength. As these youth gain muscle mass through such training, their BMIs may also increase because muscle is denser than adipose/fat tissue. Accordingly, because BMI correlates with, but does not actually measure body fat, the measure has been criticized as an index of body fat among athletes (e.g., Ode, Pivarnik, Reeves, & Knous, 2007). As noted below, this would be consistent with the finding that while BMI percentile was moderated by age, actual risk for obesity was not. That is, irrespective of age, those adolescents whose regular summer care arrangements included participation in organized activities were significantly less likely to be at-risk for obesity than youth without such arrangements.
The finding that youth whose regular summer care arrangement(s) involved organized activities had a relatively a lower risk for obesity compared to other youth builds on prior research concerning organized activity participation during the school year (e.g., Elkins et al., 2004; Mahoney et al., 2005a). The implication is that efforts to combat adolescent obesity needs to take seriously the contributions of out-of-school time, including care arrangements during the summer. In doing so, providing convenient and affordable opportunities for youth to participate in organized activities during the summer months seems important. However, it should be noted that the proportion of youth at-risk for obesity was still high among those whose regular summer arrangements included organized activity participation. Accordingly, if the association is causal, then organized activities would constitute only one important part of a broader approach to obesity reduction.
The other two presumed moderators – duration of activity participation and gender – were not significant. With respect to duration, it should be noted that organized activity participation was measured dichotomously with a lapse of five years between the two assessments. As such, the study design could not disentangle duration (i.e., longevity of participation) from stability (i.e., consistency of participation). Indeed, it is unknown what regular care arrangements youth experienced between the two assessments. Available research shows the importance of examining cumulative involvement in organized activities from one school year to the next (e.g., Darling, 2005). Additional research that examines participation over consecutive summers and school years seems warranted.
Gender was explored as a potential moderator because prior research shows that boys and girls participate in different types of organized activities that, in turn, may affect different aspects of their development. However, of the three types of organized summer activities assessed in this study (i.e., sports, extracurricular activities, and summer programs), sports was the only one to involve a sizable proportion of the sample. Accordingly, variability according to activity type could not be assessed. Additional research involving larger samples of youth should be able to compare the associated health-related properties of different organized summer activities for boys and girls. Nonetheless, it is noteworthy that gender did not moderate the findings because this implies that the link between regular participation in organized summer sports and the lowered risk for obesity are apparent for both boys and girls.
Third, following a bioecological perspective to adolescent development, BMI percentile and risk for obesity were compared for youth in specific, alternative summer care arrangements. The BMI percentile for youth who regularly experienced self care with organized activity participation was significantly higher than youth who only regularly experienced self care. However, for BMI percentile, there was also an interaction between age and summer care arrangement. Together, the results help to clarify the finding that later adolescents who regularly participated in organized summer activities had higher BMI percentiles than later adolescents who did not. Specifically, later adolescents were most likely to experience self care on a regular basis over the summer. Consistent with the earlier proposal that high school students participating in summer sports may increase their BMI through an augmentation of muscle (vs. fat), those later adolescents who are apt to regularly experience self care during the summer would be expected to have a relatively high BMI percentile if they were also regular participants in organized summer sports.
In terms of risk for obesity and summer care arrangements, youth who regularly experienced parent care without organized activity participation showed the greatest risk for obesity the following school year. Importantly, youth who regularly experienced both parent care and organized activity participation were at significantly lower risk for obesity than those who experienced parent care alone. That parent care predicts a high risk for obesity could require some refinement in our understanding of how parents contribute to adolescent development. Parental supervision during adolescence can protect against poor developmental outcomes such as antisocial behavior (Mahoney & Parente, 2009). However, when youth primarily experience parent care over the summer, the arrangement might also invite passivity and/or unhealthy eating. If so, then there could be developmental trade-offs that result from care arrangements predominated by direct parental supervision (e.g., lowered risk for deviance, but heightened risk for obesity). Ideally, adolescent arrangements would provide an appropriate balance of adult supervision with a physically healthy environment. Organized activities appear to be a relatively healthy setting that could help to achieve this balance.
Another implication is that summer care arrangements may be partly responsible for age-related differences in the prevalence of risk for obesity across adolescence. Parent care was most common during early adolescence and this was also the age period where both BMI percentile and risk for obesity were highest. As adolescence proceeds, other care arrangements such as self care become increasingly common. The change in care arrangements probably coincides with parents’ views that more adult supervision is required during early vs. later adolescence. Indeed, the potential risks of self care during early adolescence are well-documented (Mahoney & Parente, 2009). But, the findings suggest that parents should also be mindful of the possible health risks that can accompany any care setting featuring regular opportunities for over-eating and passivity. For example, one trade-off of parent care could be less involvement with peers and friends that, in turn, could diminish physical activity (Salvy et al., 2008; 2009). Again, one implication this is possible is that adolescents of all ages need regular opportunities to be engaged in organized activities during the summer to help offset risks for obesity.
Limitations and Future Directions
At the beginning of any new area of study there are limitations and restrictions on the scope of what can be accomplished and the types of data available to address research questions. Such is the case with this investigation. To begin, the study was quasi-experimental and causal interpretations are not possible. This is true despite the longitudinal nature of the research design that allowed for several demographic control variables, as well as earlier measures of youth BMI and organized activity participation, to be accounted for in the analysis. Unmeasured person or context factors could influence the results reported. On that score, the study findings point to several avenues for further research.
First, although the use of the PSID-CDS offers the significant advantage of being a longitudinal study involving a nationally representative youth ages 10–18, the measures of summertime care arrangements are very basic. Unlike the rich data on school year time use available in the PSID-CDS, summer care arrangements were primarily measured dichotomously. Because intensity of involvement in care arrangements is clearly important, research designed to assess the summertime experience of adolescents, including detailed information on both time use that specifies the people and contexts that youth experience and broad indicators of their adjustment, is sorely needed.
Second, and related, information about the quality and content of the care arrangements that youth experienced in the summer was not measured in the PSID-CDS. Decades of research on child care and out-of-school time makes it clear that knowledge of quality can temper general conclusions made about the types of arrangements included in this investigation (e.g., Durlak & Weissberg, 2007; Vandell & Wolfe, 2000). Although certain arrangements may be positively or negatively related to indicators of adolescent health overall, the variability within arrangements also needs to be understood to offer recommendations about how best to structure summertime care for different types of adolescents.
Third, this investigation focused on providing descriptive information on summer care arrangements and evaluating whether an association between those arrangements and BMI percentile or risk for obesity exists at the population level. Much more research on moderating factors is needed in research out-of-school time and youth development. The need to study the health promoting and compromising features of the care arrangements was mentioned earlier. It would also be valuable to assess a more refined list of organized activities. For example, summer camp was not studied in this investigation because it was not a common care arrangement and was not defined in enough detail to determine whether it was an organized activity. However, it seems likely that summer camp could influence obesity rates. In addition, it remains an open question whether the care arrangements operate similarly for youth who differ in terms of childhood BMI percentiles and obesity status, peer involvement, socioeconomic status, and neighborhood conditions. Moreover, information on parents’ health habits concerning diet and exercise and measures of their own BMI/obesity status might clarify the conditions under which each arrangement is likely to predict adolescent obesity. In general, additional research on summer that is guided by a developmental-ecological perspective seems warranted (e.g., Durlak, Mahoney, Bohnert, & Parente, 2010).
Fourth, the use of BMI as a measure of obesity in this study has limitations. In terms of the measurement procedure itself, the assessment of height may have been more precise if a stadiometer was used. More generally, although BMI is a convenient measure of obesity, it appears insensitive to small, but significant differences in the distribution of lean and fat tissues (e.g., Ischander, Zaldivar, Eliakim et al., 2007) and has questionable validity for assessing obesity among athletes (Ode et al., 2007). For a more comprehensive assessment of obesity, it is recommended that additional correlates be studied to provide complementary information (e.g., body composition, waist circumference, glucose and insulin levels, and bone health) (e.g., Barlow & Expert Committee, 2009; Ischander et al., 2007; The HEALTHY Study Group, 2010).
Lastly, although CDS-I school year measures of BMI and a variety of demographics were included in the analyses, the lag time between the CDS-I and CDS-II summer involved several years. Experiences that could affect risk for obesity during this lag time could not be accounted for in this study. A more rigorous design would involve a fully prospective, longitudinal study with assessments spaced together more closely in time. Specifically, the measurement of BMI (and associated risk for obesity) would occur shortly before and immediately after the summer across several consecutive years. In addition, assessments of parents’ and adolescents’ preferences and the decision-making process concerning the choice of summer care arrangements should be obtained to determine how BMI might be involved in the selection process. Finally, selection bias can sometimes be eliminated in random assignment designs. Given the possibility that summer care arrangements might reduce the risk for obesity during adolescence it seems prudent to conduct experimental work in this area now.
Concluding Comments
Research in the field of out-of-school time and youth development has expanded markedly in recent years and considerable progress has made. However, investigations concentrating on summertime – the largest consecutive period of out-of-school time – or aspects of adolescent physical health have been given relatively little attention. The findings from this investigation suggest that it is important to begin understanding how summer experiences contribute to the healthy functioning of young people. In developing a future research agenda that can inform policy and practice, new investigations should be designed to study summertime in ways that will elucidate the particular person and ecological conditions most conducive to developing healthy behavior patterns from childhood through adolescence and beyond.
Acknowledgments
This study was supported by a grant from the National Institute of Child Health and Human Development (R03HD055318). The author thanks Greg Duncan and Elizabeth Vandewater for methodological advice pertaining to the PSID-CDS dataset. Thanks also to Amy Bohnert, Kelly Brownell, Daniel Cooper, Kristen Fay, Paul von Hippel, Richard Lerner, Adam Sheppard, Eric Stice, and Marlene Schwartz for feedback on findings from earlier versions of this manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Because of the small percentage of youth whose summer arrangement(s) involved regular participation in extracurricular activities and summer programs, it was not possible to compare activities types in this study. However, results were substantially similar when focusing only on arrangements that included regular participation in organized summer sports.
References
- Anderson PM, Butcher KF. Childhood obesity: Trends and potential causes. Future of Children. 2006;16:19–45. doi: 10.1353/foc.2006.0001. [DOI] [PubMed] [Google Scholar]
- Andreski P, Gouskova E, McConagle K, Shoeni B. An analysis of the quality of the health data in the Panel Study of Income Dynamics: 1999–2003. 2005 Retrieved April 5, 2006 from: http://psidonline.isr.umich.edu.
- Barber BL, Eccles JS, Stone MR. Whatever happened to the jock, the brain, and the princess? Young adult pathways linked to adolescent activity involvement and social identity. Journal of Adolescent Research. 2001;16:429–455. [Google Scholar]
- Barlow SE the Expert Committee. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: Summary report. Pediatrics. 2007;120:S164–S192. doi: 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]
- Bergman LR, Magnusson D, El-Khouri BM. Studying individual development in an interindividual context: A person-oriented Approach. Mahwah, NJ: Erlbaum; 2003. [Google Scholar]
- Bronfenbrenner U, Morris P. The bioecological model of human development. In: Daman W, Lerner RM, Lerner RM, editors. Handbook of child psychology: Vol 1. Theoretical models of human development. Hoboken, NJ: John Wiley & Sons; 2006. pp. 793–828. [Google Scholar]
- Cairns RB, Cairns BD. Lifelines and risks: Pathways of youth in our time. New York, NY: Cambridge University Press; 1994. [Google Scholar]
- Campbell PT, Katzmarzyk PT, Malina RM, Rao-Louise Pérusse DC, Bouchard C. Stability of adiposity phenotypes from childhood and adolescence into young adulthood with contribution of parental measures. Obesity Research. 2001;9:394–400. doi: 10.1038/oby.2001.51. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control. How is BMI calculated and interpreted for children and teens? 2009a Retreived November 04, 2009 from: http://www.cdc.gov/healthyweight/assessing/bmi/childrens_bmi/about_childrens_bmi.html.
- Centers for Disease Control. Obesity: Halting the epidemic by making health easier. 2009b Retrieved April 28, 2009 from: www.cdc.gov/NCCDPHP/publications/AAG/pdf/obesity_aaa.pdf.
- Cosden M, Morrison G, Albanese AL, Macias S. When homework is not home work: After-school programs for homework assistance. Educational Psychologist. 2001;36:211–221. [Google Scholar]
- Crimmins NA, Dolan LM, Martin LJ, Bean JA, Daniels SR, Lawson ML, Goodman E, Woo JG. Stability of adolescent body mass index during three years of follow-up. Journal of Pediatrics. 2007;151:383–387. doi: 10.1016/j.jpeds.2007.04.005. [DOI] [PubMed] [Google Scholar]
- Darling N. Participation in extracurricular activities and adolescent adjustment: Cross-sectional and longitudinal findings. Journal of Youth and Adolescence. 2005;34:493–505. [Google Scholar]
- Darling N, Caldwell LL, Smith R. Participation in school-based extracurricular activities and adolescent adjustment. Journal of Leisure Research. 2005;37:51–76. [Google Scholar]
- Denault A-S, Poulin F. Predictor of adolescent participation in organized activities: A five-year longitudinal study. Journal of Research on Adolescence. 1999;19:287–311. [Google Scholar]
- Durlak JA, Weissberg RP. The impact of after-school programs that promote personal and social skills. Chicago, IL: Collaborative for Academic, Social, and Emotional Learning; 2007. [Google Scholar]
- Durlak J, Mahoney JL, Bohnert AM, Parente ME. Developing and improving after-school programs to enhance youth’s personal growth and adjustment: A special issue of AJCP. American Journal of Community Psychology. 2010;45:285–293. doi: 10.1007/s10464-010-9298-9. [DOI] [PubMed] [Google Scholar]
- Eccles JS, Barber BL, Stone M, Hunt J. Extracurricular activities and adolescent development. Journal of Social Issues. 2003;59:10–43. [Google Scholar]
- Eccles JS, Midgley C. Stage-environment fit: Developmentally appropriate classrooms for young adolescents. In: Ames C, Ames R, editors. Research on motivation in education: Goals and cognitions. Vol. 3. New York: Academic Press; 1989. pp. 139–186. [Google Scholar]
- Eitle TM. Do gender and race matter?: Explaining the relationship between sports participation and achievement. Sociological Spectrum. 2005;25:177–195. [Google Scholar]
- Eitle TM, Eitle DJ. Race, cultural capital, and the educational effects of participation in sports. Sociology of Education. 2002;75:123–146. [Google Scholar]
- Elkins WL, Cohen DA, Koralewicz LM, Taylor SN. After school activities, overweight, and obesity among inner city youth. Journal of Adolescence. 2004;27:181–189. doi: 10.1016/j.adolescence.2003.10.010. [DOI] [PubMed] [Google Scholar]
- Feldman DE, Barnett T, Shrier I, Rossignol M, Abenhaim L. Is physical activity differentially associated with different types of sedentary pursuits? Archives of Pediatric & Adolescent Medicine. 2003;157:797–802. doi: 10.1001/archpedi.157.8.797. [DOI] [PubMed] [Google Scholar]
- Fredricks JA, Eccles JS. Extracurricular involvement and adolescent adjustment: Impact of duration, number of activities, and breadth of participation. Applied Developmental Science. 2006;10:132–146. [Google Scholar]
- Gibbons JL, Lynn M, Stiles DA. Cross-national differences in adolescents’ preferences for free-time activities. Cross-Cultural Research: The Journal of Comparative Social Science. 1997;31:55–69. [Google Scholar]
- Hedley AA, Ogden CL, Johnson CL, Carroll MD, Curtin LR, Flegal KM. Overweight and obesity among US children, adolescents, and adults, 1999–2002. JAMA. 2004;291:2847–2850. doi: 10.1001/jama.291.23.2847. [DOI] [PubMed] [Google Scholar]
- Holmbeck GN. Post-hoc probing of significant moderational and meditational effects in studies of pediatric populations. Journal of Pediatric Psychology. 2002;27:87–96. doi: 10.1093/jpepsy/27.1.87. [DOI] [PubMed] [Google Scholar]
- Ischander M, Zaldivar F, Eliakim A, Nussbaum E, Dunton G, Leu S-Y, Cooper DM, Schneider M. Physical activity, growth, and inflammatory mediators of BMI-matched female adolescents. Medicine & Science in Sports & Exercise. 2007;39:1131–1138. doi: 10.1249/mss.0b013e318053e7a2. [DOI] [PubMed] [Google Scholar]
- Kimm SYS, Obarzanek E. Child obesity: A new pandemic of the new millennium. Pediatrics. 2002;110:1003–1007. doi: 10.1542/peds.110.5.1003. [DOI] [PubMed] [Google Scholar]
- Knutson KA. CHAMPS after-school program outcome evaluation year three: FY2005. Coral Springs, FL: Author; 2005. [Google Scholar]
- Krishnamoorthy JS, Hart C, Jelalian E. The epidemic of childhood obesity: Review of research implications for policy. Social Policy Report. 2006;20:1–20. [Google Scholar]
- Larson RW, Richards MH, Sims B, Dworkin J. How urban African American young adolescents spend their time: Time budgets for locations, activities, and companionship. American Journal of Community Psychology. 2001;29:565–597. doi: 10.1023/A:1010422017731. [DOI] [PubMed] [Google Scholar]
- Lerner RM. Developmental science, developmental systems, and contemporary theories of human development. In: Lerner RM, Damon W, Lerner RM, editors. Handbook of child psychology: Vol. 1 Theoretical models of human development. 6th ed. Hoboken, NJ: John Wiley; 2006. pp. 1–17. [Google Scholar]
- Lohman BJ, Stewart S, Gundersen C, Garasky S, Eisenmann J. Adolescent overweight and obesity: Links to food insecurity and individual, maternal, and family stressors. Journal of Adolescent Health. 2009;45:230–257. doi: 10.1016/j.jadohealth.2009.01.003. [DOI] [PubMed] [Google Scholar]
- Lord H, Mahoney JL. Neighborhood crime and Self Care: Risks for aggression and lower academic performance. Developmental Psychology. 2007;43:1321–1333. doi: 10.1037/0012-1649.43.6.1321. [DOI] [PubMed] [Google Scholar]
- Lopez RP. Neighborhood risk factors for obesity. Obesity. 2007;15:2111–2119. doi: 10.1038/oby.2007.251. [DOI] [PubMed] [Google Scholar]
- Lowry R, Kann L, Collins JL, Kolbe LJ. The effect of socioeconomic status on chronic disease risk behaviors among US adolescents. JAMA. 1996;276:792–797. [PubMed] [Google Scholar]
- Lumeng JC, Gannon K, Appulgliese D, Cabral HJ, Zuckerman B. Preschool child care and risk of overweight in 6- to 12-year-old children. International Journal of Obesity. 2005;29:60–66. doi: 10.1038/sj.ijo.0802848. [DOI] [PubMed] [Google Scholar]
- Mahoney JL, Cairns RB. Do extracurricular activities protect against early school dropout? Developmental Psychology. 1997;33:241–253. doi: 10.1037//0012-1649.33.2.241. [DOI] [PubMed] [Google Scholar]
- Mahoney JL, Lord H, Carryl E. Afterschool program participation and the development of child obesity and peer acceptance. Applied Developmental Science. 2005a;9:202–215. [Google Scholar]
- Mahoney JL, Lord H, Carryl E. An ecological analysis of after-school program participation and the development of academic performance and motivational attributes for disadvantaged children. Child Development. 2005b;76:811–825. doi: 10.1111/j.1467-8624.2005.00879.x. [DOI] [PubMed] [Google Scholar]
- Mahoney JL, Parente ME. Should we care about adolescents who care for themselves?: What we’ve learned and what we need to know about youth in self-care. Child Development Perspectives. 2009;3:189–195. doi: 10.1111/j.1750-8606.2009.00105.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahoney JL, Vandell DL, Simpkins SD, Zarrett NR. Adolescent out-of-school activities. In: Lerner RM, Steinberg L, editors. Handbook of Adolescent Psychology. 3rd ed. Vol. 2. Hoboken, NJ: Wiley & Sons; 2009. pp. 228–267. Contextual influences on adolescent development. [Google Scholar]
- Mainieri T. The Panel Study of Income Dynamics Child Development Supplement: User guide for CDS-II. 2006 Retrieved April 4, 2006 from: http://psidonline.isr.umich.edu/CDS/cdsii_userGD.pdf.
- Marsh HW, Kleitman S. School athletic participation: Mostly gain with little pain. Journal of Sport & Exercise Psychology. 2003;25:205–228. [Google Scholar]
- Molnar BE, Gortmaker SL, Bull FC, Buka SL. Unsafe to play? Neighborhood disorder and lack of safety predict reduced physical activity among urban children and adolescents. American Journal of Health Promotion. 2004;18:378–386. doi: 10.4278/0890-1171-18.5.378. [DOI] [PubMed] [Google Scholar]
- Mota J, Rebeiro JC, Santos MP. Obese girls differences in neighbourhood perceptions, screen time and socioeconomic status according to level of physical activity. Health Education Research. 2009;24:98–104. doi: 10.1093/her/cyn001. [DOI] [PubMed] [Google Scholar]
- Mustillo S, Worthman C, Erkanli A, Keeler G, Angold A, Costello EJ. Obesity and psychiatric disorder: Developmental trajectories. Pediatrics. 2003;111:851–859. doi: 10.1542/peds.111.4.851. [DOI] [PubMed] [Google Scholar]
- Nelson MC, Gordon-Larsen P, Song Y, Popkin BM. Build and social environments: Associations with adolescent overweight and obesity. American Journal of Preventive Medicine. 2006;31:109–117. doi: 10.1016/j.amepre.2006.03.026. [DOI] [PubMed] [Google Scholar]
- Ode JJ, Pivarnik JM, Reeves MJ, Knous JL. Body mass index as a predictor of percent fat in college athletes and nonathletes. Medicine & Science in Sports & Exercise. 2007;39:403–409. doi: 10.1249/01.mss.0000247008.19127.3e. [DOI] [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Flegel KM. High body mass index for age among US children and adolescents, 2003–2006. JAMA. 2008;20:2401–2405. doi: 10.1001/jama.299.20.2401. [DOI] [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegel KM. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA. 2006;295:1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- Ogden CL, Flegal KM, Carroll MD, Johnson CL. Prevalence and trends in overweight among US children and adolescents, 1999–2000. JAMA. 2002;288:1728–1732. doi: 10.1001/jama.288.14.1728. [DOI] [PubMed] [Google Scholar]
- Phillip SF. Race and gender differences in adolescent peer group approval of leisure activities. Journal of Leisure Research. 1998;30:214–232. [Google Scholar]
- Pierce KM, Hamm JV, Vandell DL. Experiences in after-school programs and children’s adjustment in first-grade classrooms. Child Development. 1999;70:756–767. doi: 10.1111/1467-8624.00054. [DOI] [PubMed] [Google Scholar]
- Pierce KM, Bolt DM, Vandell DL. Specific features of after-school program quality: Associations with children’s functioning in middle childhood. American Journal of Community Psychology. 2010 doi: 10.1007/s10464-010-9304-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pettit GS, Laird RD, Bates JE, Dodge KA. Patterns of after-school care in middle childhood: Risk factors and developmental outcomes. Merrill-Palmer Quarterly. 1997;43:515–538. [Google Scholar]
- Riggs NR, Greenberg MT. After-school youth development programs: A developmental-ecological model of current research. Clinical Child and Family Psychology Review. 2004a;7:177–190. doi: 10.1023/b:ccfp.0000045126.83678.75. [DOI] [PubMed] [Google Scholar]
- Riggs NR, Greenberg MT. Moderators in the academic development of migrant Latino children attending after-school programs. Applied Developmental Psychology. 2004b;25:349–367. [Google Scholar]
- Salvy S-J, Bowker JW, Roemich JN, Romero N, Kieffer E, Paluch R, Epstein LH. Peer influences on children’s physical activity: An experience sampling study. Journal of Pediatric Psychology. 2008;33:39–49. doi: 10.1093/jpepsy/jsm039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salvy S-J, Roemmich JN, Bowker JC, Romero ND, Stadler PJ, Epstein LH. Effect of peers and friends on youth physical activity and motivation to be physically active. Journal of Pediatric Psychology. 2009;34:217–225. doi: 10.1093/jpepsy/jsn071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shann MH. Students’ use of time outside of school: A case for after school programs for urban middle school youth. Urban Review. 2001;33:339–356. [Google Scholar]
- The HEALTHY Study Group. A school-based intervention for diabetes risk reduction. The New England Journal of Medicine. 2010;363:443–453. doi: 10.1056/NEJMoa1001933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vandell DL, Posner JK. Conceptualization and measurement of children’s after-school environments. In: Friedman SL, Wachs T, editors. Measuring environments across the lifespan: Emerging methods and concepts. Washington, DC: American Psychological Association; 1999. pp. 167–196. [Google Scholar]
- Vandell DL, Shernoff DJ, Pierce KM, Bolt DM, Dadisman K, Brown BB. Activities, engagement, and emotion in after - school programs. In: Weiss HB, Little PMD, Bouffard SM, Noam GG, editors. New directions in youth development. vol. 105. San Francisco: Jossey - Bass; 2005. pp. 121–129. Participation in youth programs: Enrollment, attendance, and engagement. [DOI] [PubMed] [Google Scholar]
- Vandell DL, Wolfe B. Child care quality: Does it matter and does it need to be improved? 2000 Retrieved on May 3, 2009 from: http://www.aspe.hhs.gov/hsp/ccquality00/ccqual.htm.
- Videon TM, Manning CK. Influences on adolescent eating patterns: The importance of family meals. Journal of Adolescent Health. 2003;32:365–373. doi: 10.1016/s1054-139x(02)00711-5. [DOI] [PubMed] [Google Scholar]
- von Hippel PT, Powell B, Downey DB, Rowland NJ. The effect of school on overweight in childhood: Gain in Body Mass Index during the school year and during summer vacation. American Journal of Public Health. 2007;97:696–702. doi: 10.2105/AJPH.2005.080754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang SS, Brownell KD. Public policy and obesity: The need to marry science with advocacy. Psychiatric Clinics of North America. 2005;28:235–252. doi: 10.1016/j.psc.2004.09.001. [DOI] [PubMed] [Google Scholar]
- Welsh ME, Russell CA, Williams I, Reisner ER, White RN. Promoting learning and school attendance through after-school programs: Student-level changes in educational performance across TASC’s first three years. Washington, DC: Policy Studies Associates; 2002. [Google Scholar]
- U.S. Census Bureau. Who’s minding the kids? Child care arrangements: Summer 2006. 2009 Retrieved October 14, 2009 from: http://www.census.gov/population/www/socdemo/child/tables-2006.html.
- U.S. Department of Education. American Recovery and Reinvestment Act of 2009: Title I, Part A Funds for Grants to Local Education Agencies. 2009 Retrieved May 3, 2009 from: http://www.ed.gov/policy/gen/leg/recovery/factsheet/title-i.html.
- Zaff JS, Moore KA, Papillo AR, Williams S. Implications of extracurricular activity participation during adolescence on positive outcomes. Journal of Adolescent Research. 2003;18:599–630. [Google Scholar]