Abstract
Overproduction of free radicals can damage cellular components resulting in progressive physiological dysfunction, which has been implicated in many human diseases. Oxidative damage to RNA received little attention until the past decade. Recent studies indicate that RNA, such as messenger RNA and ribosomal RNA, is very vulnerable to oxidative damage. RNA oxidation is not a consequence of dying cells but an early event involved in pathogenesis. Oxidative modification to RNA results in disturbance of the translational process and impairment of protein synthesis, which can cause cell deterioration or even cell death. In this review, we discuss the mechanisms of oxidative damage to RNA and the possible biological consequences of damaged RNA. Furthermore, we review recent evidence suggesting that oxidative damage to RNA may contribute to progression of many human diseases.
Keywords: RNA oxidation, Oxidative damage, Oxidative stress, Free radical, Neurodegeneration, Alzheimer’s disease, ALS
Introduction
Free radicals
Free radicals are chemical species which contain one or more unpaired electrons in their outer orbit. These unpaired electrons are usually highly reactive, so free radicals are likely to take part in chemical reactions. An unpaired electron is conventionally denoted by a superscript dot: X·. There are three biologically important free radicals in our body: the oxygen species, superoxide O·−2, the hydroxyl radical OH·, and the reactive nitrogen species NO·. Each plays a significant physiological role in the body; for example, they are involved in killing invading microorganisms [1] and in cell signaling processes [2]. However, because of their reactivity, these free radicals can participate in unwanted side reactions resulting in cell damage. Many forms of cancer are thought to be the result of reactions between free radicals and DNA that result in mutations that can adversely affect the cell cycle and potentially lead to malignancy. Some of the symptoms of aging such as atherosclerosis have also been attributed to free radical-induced oxidation of many of the chemicals making up the body [3, 4]. In addition, free radicals contribute to alcohol-induced liver damage, perhaps more than alcohol itself [5]. Free radicals also play a critical role in the pathogenesis of many neurological disorders, including among others Alzheimer’s disease (AD), Parkinson’s disease (PD), amyotrophic lateral sclerosis (ALS), spinal cord injury (SCI), and epilepsy.
Superoxide O·−2 is biologically quite toxic and is deployed by the immune system to kill invading microorganisms. In phagocytes, superoxide is produced in large quantities by the enzyme NADPH oxidase for use in oxygen-dependent killing of invading pathogens [6]. Superoxide is also deleteriously produced as a byproduct of mitochondrial respiration together with several other enzymes, for example xanthine oxidase. Because superoxide is toxic, nearly all organisms living in the presence of oxygen contain isoforms of the superoxide scavenging enzyme, superoxide dismutase (SOD), which catalyzes the dismutation of superoxide into oxygen and hydrogen peroxide H2O2 (2O·−2 + 2H+ → H2O2 + O2) [7]. However, hydrogen peroxide is dangerous in the cell because it can easily be converted into hydroxyl radical OH·, one of the most destructive free radicals, by interacting with Fe2+. This process is known as the Fenton reaction (Fe2+ + H2O2 → Fe3+ + OH· + OH−). To prevent damage, hydrogen peroxide must be quickly converted into other, less dangerous substances. To this end, catalase, which is concentrated in peroxisomes located next to mitochondria, is frequently used by cells to rapidly catalyze the decomposition of hydrogen peroxide into water and oxygen (2H2O2 → 2H2O + O2) [8]. In addition, glutathione peroxidase can also reduce hydrogen peroxide by transferring the energy of the reactive peroxides to a very small sulfur-containing tripeptide called glutathione (GSH). In the process, GSH is converted to its oxidized form GSH disulfide (2GSH + H2O2 → GS–SG + 2H2O) [9]. Superoxide as well as hydrogen peroxide is not only an injurious byproduct of cellular metabolism but also an essential participant in cell signaling and regulation.
The hydroxyl radical (OH·) has a very short in vivo half-life of approximately 10−9 s and a high reactivity [10]. This makes it a very dangerous compound to the organism. Unlike superoxide, which can be detoxified by SOD, the hydroxyl radical cannot be eliminated by an enzymatic reaction. As diffusion is slower than the half-life of the molecule, it reacts with any oxidizable compound in its vicinity. It can damage virtually all types of macromolecules: carbohydrates, nucleic acids, lipids, and amino acids.
Nitric oxide (NO) is an important signaling molecule in the body, participating in diverse biological processes, including vasodilation, bronchodilation, neurotransmission, and antimicrobial activity [11]. It is biosynthesized endogenously from arginine and oxygen by various NO synthase (NOS) enzymes. The NO molecule is a free radical. NO is generated by phagocytes as part of the human immune response. Phagocytes are armed with inducible NO synthase which can be activated by cytokines or microbial products [12]. NO is a relatively long-lived free radical species, with high diffusibility and selective reactivity. Most biological actions of NO appear to be mediated by interactions with paramagnetic centers in effector proteins, such as heme– or iron–sulfur centers. It is also known to react rapidly with other targets that carry unpaired electrons. NO can react with superoxide to produce the damaging oxidant peroxynitrite ONOO− (NO· + O·−2 → ONOO−) [2]. Peroxynitrite itself is a highly reactive species which can directly react with various components of the cell.
Oxidative damage
Overproduction of the above free radicals can damage all components of the cell, leading to a progressive decline in physiological function. For example, reactive oxygen species (ROS) can attack proteins causing their carbonylation, which is an irreversible oxidative damage, often leading to a loss of protein function and protein aggregation [13]. Peroxynitrite is able to nitrate tyrosine residues in proteins (protein nitration), leading to alterations in protein activity [14]. Free radicals can “steal” electrons from the lipids, often affecting polyunsaturated fatty acids, in the cell membranes (lipid peroxidation), resulting in degradation of lipids and cell damage. In addition, some end-products of lipid peroxidation, such as malondialdehyde, are mutagenic and carcinogenic [15]. Furthermore, ROS can damage DNA, most readily at guanine residues, which causes mutations resulting in inheritable disease, cancer and aging [16]. In the past decades, these processes of oxidative damage have been well characterized in a large variety of diseases and disorders of physiological dysfunction.
However, until the past decade, oxidative damage to RNA drew little attention, even though RNA is more vulnerable than other cellular components. Here, we discuss the mechanisms of oxidative damage to RNA and the possible biological consequences of damaged RNA. Furthermore, we review the recent evidence suggesting that oxidative modification to RNA may contribute to cell deterioration in many neurological disorders and also other human diseases associated with oxidative stress/damage.
Mechanisms of oxidative damage to RNA
Structural changes in oxidized RNA
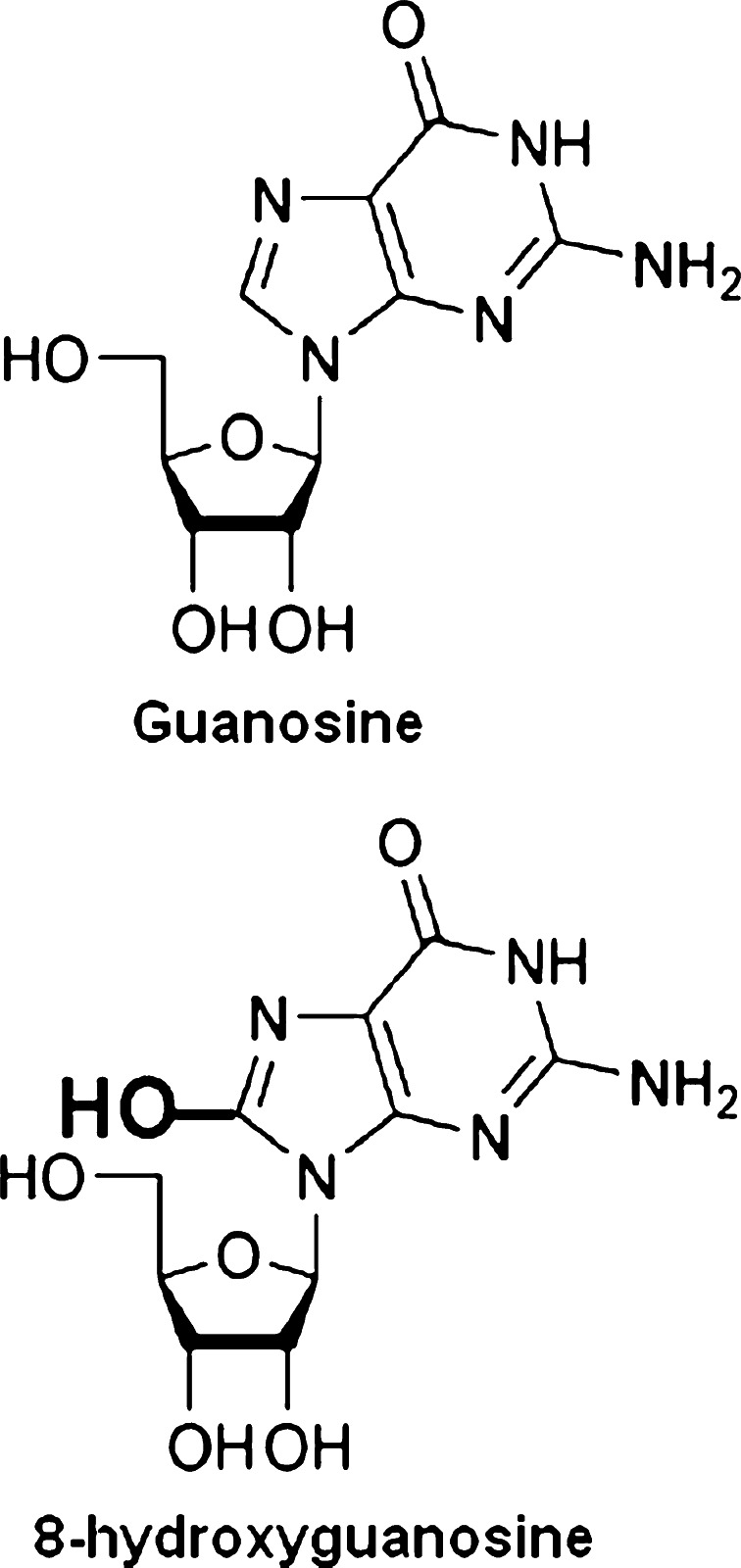
Out of a wide variety of free radicals generated in living cells during normal metabolism and by exogenous sources, the hydroxyl radical (OH·) is highly reactive and could well be directly responsible for most of the oxidative damage in biological macromolecules, including RNA. Hydroxyl radicals, produced in the vicinity of RNA, can easily modify RNA because they are highly reactive and cannot diffuse from their sites of formation. Therefore, hydroxyl radical-induced modifications constitute the most varied class of RNA damage. More than 20 different types of base damage by hydroxyl radicals have been identified [17]. The most prevalent oxidized base in RNA is 8-hydroxyguanosine (8-OHG) (Fig. 1). The highly reactive hydroxyl radical first reacts with guanine to form a C8-OH adduct radical. Then the loss of an electron (e−) and proton (H+) generates 8-OHG.
Fig. 1.
The most prevalent oxidized base in RNA is 8-hydroxyguanosine (8-OHG). Guanosine (a RNA nucleoside) can be oxidized by highly reactive hydroxyl radicals to form a C8-OH adduct radical, which then loses an electron (e−) and a proton (H+) to form 8-OHG (an oxidized RNA nucleoside)
Detection and isolation of oxidatively damaged RNA
High-performance liquid chromatography-electrochemical detection (HPLC-ECD) is a common method used to detect/quantify oxidation products, such as 8-OHG, in tissues, cerebrospinal fluid (CSF), serum, and urine. Abe et al. applied HPLC-ECD to measure the 8-OHG levels in the CSF and the serum of patients with AD. They reported a significant increase in the concentration of 8-OHG in the CSF, but not in the serum, of AD patients [18]. This group, using the same approach, also found an increase in 8-OHG levels in the CSF of patients with PD [19]. Furthermore, Hofer et al. developed a method for the simultaneous analysis of oxidized RNA and DNA guanine products in tissues using HPLC-ECD [20]. They reported a greater RNA than DNA oxidation in rat liver after administration of doxorubicin, an antitumor antibiotic used to treat many human neoplasms.
Another way to detect oxidation products is the use of antibodies. The monoclonal antibodies 15A3 and 1F7 are the most commonly used antibodies for detection of 8-OHG in RNA and 8-OHdG in DNA. These antibodies have high specificity and affinity for 8-OHdG and 8-OHG [21, 22]. Both antibodies have been used in studying RNA oxidation in various human diseases by immunocytochemical and biochemical approaches. A series of elegant studies by the group of Smith and Perry, examining post-mortem brains by immunocytochemistry, demonstrated that RNA oxidation is involved in a wide variety of neurological diseases, including AD [23, 24], PD [25, 26], Down syndrome [27], dementia with Lewy bodies [28], and prion diseases [29]. Other researchers have also reported that RNA oxidation is involved in other neurological conditions, including mild cognitive impairment (MCI) [30], subacute sclerosing panencephalitis [31], and xeroderma pigmentosum [32].
Immunoblot analysis is one way to detect RNA containing 8-OHG. Our group applied Northwestern analysis to examine poly(A)+ mRNAs isolated from the brains of patients with AD and showed an increase in poly(A)+ mRNAs oxidation in the brains [33]. Ding et al. [34] applied slot blot analysis to demonstrate elevation in RNA oxidation within ribosome complex of the brains of patients with AD and MCI. This group, also using same approach, found an increase in RNA oxidation following proteasome inhibition in astrocyte and neuron cultures [35]. Gorg et al. [36] applied both Northwestern and slot blot analysis to demonstrate increased RNA oxidation in rats treated with ammonia, a model of hepatic encephalopathy.
However, the above methods cannot further analyze oxidized RNA species. We previously developed an immunoprecipitation procedure using 15A3 antibodies to separate oxidized RNAs from non-oxidized RNAs, which allowed us to quantify oxidized RNA levels and identify oxidized RNA species [33]. We applied this procedure to analyze oxidized RNA species in AD and ALS post-mortem tissues [33, 37, 38].
Types of oxidized RNA
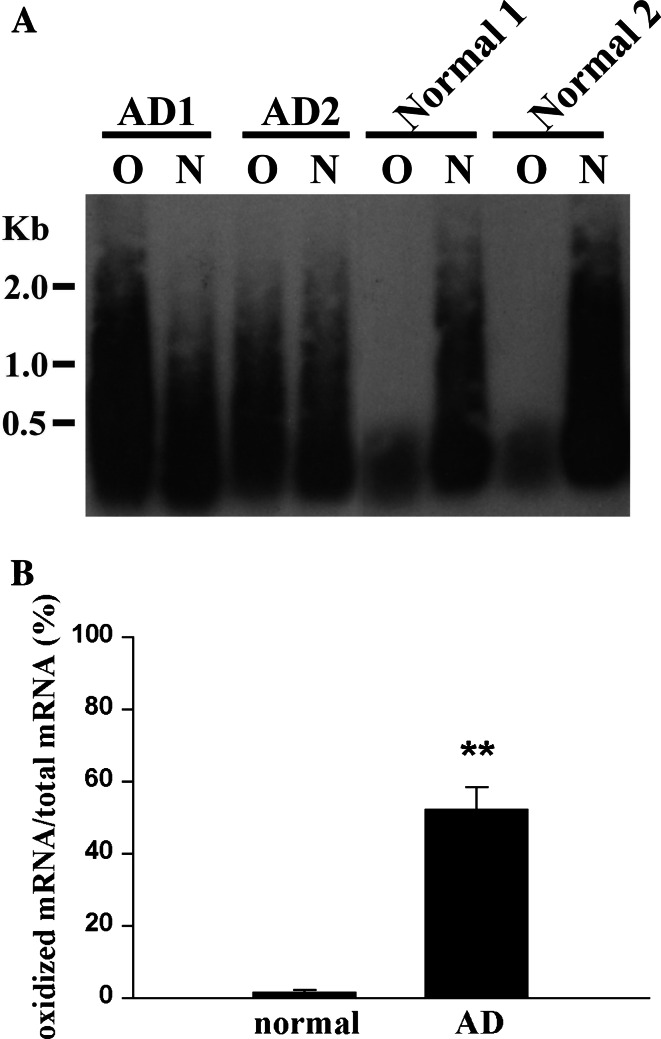
As has been known for decades, poly(A)+ mRNAs make up a very small percentage of total cellular RNA (about 1–2%) [39]. The majority of cellular RNA is composed of ribosomal RNAs (rRNAs) and transfer RNAs (tRNAs). In addition, there are a great many more types of different noncoding RNAs, including microRNAs (miRNAs), small nucleolar RNAs (snoRNAs) and small nuclear RNAs (snRNAs). These noncoding RNAs play critical roles in, for example, pre-mRNA splicing, nonsplicing RNA modifications and mRNA translational regulation [40]. Our group has demonstrated that significant amounts of poly(A)+ mRNAs are oxidized in areas affected by AD (Fig. 2) and ALS affected areas [33, 37, 38]. Honda et al. [24] reported that rRNAs in areas affected by AD are oxidized by bound redox-active iron. Ding et al. [41] also reported increased rRNA oxidation in the brains of patients with AD and MCI. Whether other types of cytoplasmic RNAs, such as tRNA and miRNA, are oxidatively damaged in diseased tissues requires further investigation.
Fig. 2.
Significant amounts of mRNAs are oxidized in the frontal cortices of AD patients. a Southern blot analysis of oxidized (O) and non-oxidized (N) mRNA pools prepared from the frontal cortices from AD patients or normal controls (n = 6 per group). Oxidized mRNAs were separated from non-oxidized mRNAs by immunoprecipitation with 15A3 antibodies. Both oxidized and non-oxidized mRNA pools were then reverse transcribed to cDNAs. DIG-labeled dUTPs were incorporated into cDNAs to facilitate analysis by Southern blotting. b Densitometric analysis of the Southern blot results reveals that 52.3 ± 6.15% of total mRNA is oxidized in the brains of AD patients while only 1.78 ± 0.56% of total mRNA is oxidized in those of normal controls. Values are means ± SEM; **P < 0.001. Details are provided in reference [37]
More vulnerable than other cellular components
Several lines of evidence suggest that RNA is more vulnerable to oxidative damage than other cellular components. Nunomura et al. [23] used the in situ immunohistochemistry approach to identify oxidized nucleosides in tissue from AD patients and found that most of the oxidized nucleosides are associated with cytoplasmic RNA, not nuclear DNA or mitochondrial DNA. This phenomenon was also observed in post-mortem tissues from those with many other neurodegenerative diseases [28, 38], in a transgenic mouse model of ALS expressing SOD1G93A mutation (SOD1G93A mice) [38], in cell culture models of oxidative stress [37], in a mouse model of SCI (F. Sun and C. Lin, unpublished observation), and in a mouse model of epilepsy (Q. Kong and C. Lin, unpublished observation). These studies indicate that RNA is more vulnerable to oxidative damage than DNA. Furthermore, in the study of RNA oxidation in SOD1G93A mice [38], there was no increase (or only slight increases) in protein carbonylation or lipid peroxidation, while a significant increase in RNA oxidation was detected in the spinal cords of the SOD1G93A mice at the presymptomatic stage. This suggests that RNA is probably more vulnerable to oxidative damage than proteins and lipids.
An early event in the process of neurodegeneration
There are many studies that indicate that RNA oxidation is an early event in the pathological cascade of neurodegeneration. Increased RNA oxidation has been observed in post-mortem brains of subjects with MCI [30, 41], which is a transitional condition between normal aging and dementia. It has also been observed in a presymptomatic subject with a familiar AD mutation [42]. Studies on the relationship between oxidative damage and pathological changes in AD have revealed that neuronal RNA oxidation precedes the formation of amyloid β (Aβ) or tau pathology [43].
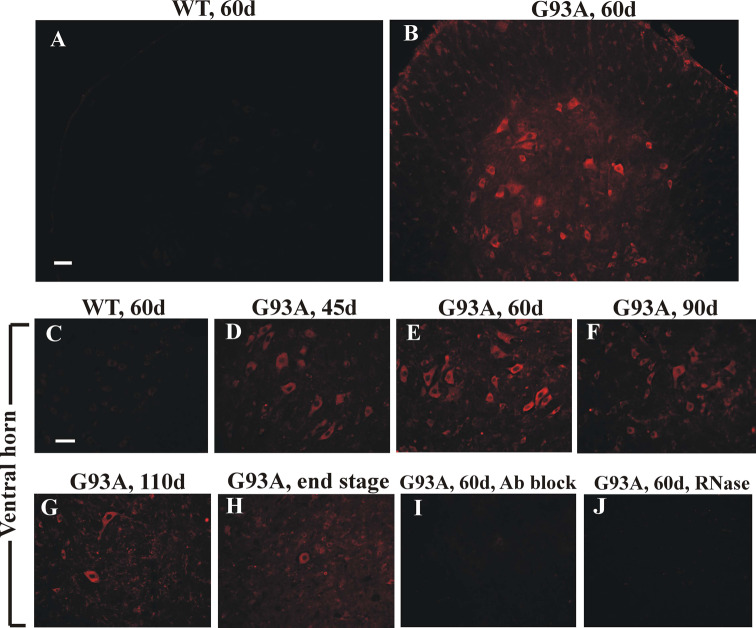
These observations in post-mortem tissues are supported by studies in mice and cultured neurons. SOD1G93A mice develop clinical and pathological phenotypes similar to those in ALS patients. These mice develop hind-limb weakness around 3 months of age that progresses to hyperreflexia, paralysis and death around 4 months of age. In these mice, increased RNA oxidation, primarily in the motor neurons and oligodendrocytes of the spinal cord, occurs as early as 1 month of age, progressively increases with age until it peaks at 2½ months of age and then diminishes when the motor neurons begin to degenerate (Fig. 3). Similarly, increased RNA oxidation also occurs in the presymptomatic stage in transgenic mice expressing other ALS-linked mutant SOD1, suggesting that RNA oxidation may be a common early event preceding motor neuron degeneration in ALS [38]. We have also observed a similar phenomenon in a mouse model of SCI (F. Sun and C. Lin, unpublished observation) and in a mouse model of epilepsy (Q. Kong and C. Lin, unpublished observation). Furthermore, our group used primary cortical cultures to investigate the relationship between RNA oxidation and neuron degeneration induced by insults that mediate the production of ROS, including hydrogen peroxide, glutamate and Aβ peptide [44]. We have also observed that RNA oxidation occurs at an early stage primarily in a distinct group of neurons that later die. These studies clearly indicate that RNA oxidation is an early event far preceding neuron degeneration, and is therefore not a consequence of cells dying.
Fig. 3.
RNA oxidation is an early event in the process of motor neuron degeneration in SOD1G93A mice. Oxidative RNA damage was examined by immunohistochemistry with 15A3 antibodies in lumbar spinal cord sections of SOD1G93A mice at the indicated ages (G93A; b, d–j) and nontransgenic littermates (WT; a, c). Increased 15A3 immunofluorescence is apparent in the motor neurons of SOD1G93A lumbar spinal cord of mice as young as 45 days (d), is further enhanced at 60 days of age (b, e), and then starts to diminish during the symptomatic stage (f–h). The immunoreactivity was diminished greatly by RNase treatment (j) and when the antibody was preincubated with 8-OHG (i). Scale bars 50 μm. Details are provided in reference [38]
Selective mRNA oxidation
We have observed an interesting phenomenon while analyzing oxidized mRNA species by filter array and DNA microarray. We found that mRNA oxidation is not random but highly selective. Some mRNA species are more susceptible to oxidative damage. This phenomenon was observed in AD and ALS post-mortem tissues [33, 38], SOD1G93A mice [38], and primary cortical cultures treated with oxidative insults described above [44]. Selective mRNA oxidation is not due to the abundance of mRNA species. For instance, β-actin and MAP-2 mRNAs are abundant mRNA species, but only very small amounts of β-actin and MAP-2 mRNAs are oxidized. We have examined RNA sequences and RNA structures for those identified mRNA species, but found no common motifs or structures. The mechanisms underlying the selective mRNA oxidation remain unknown.
Consequences of oxidatively damaged RNA
Defective protein synthesis
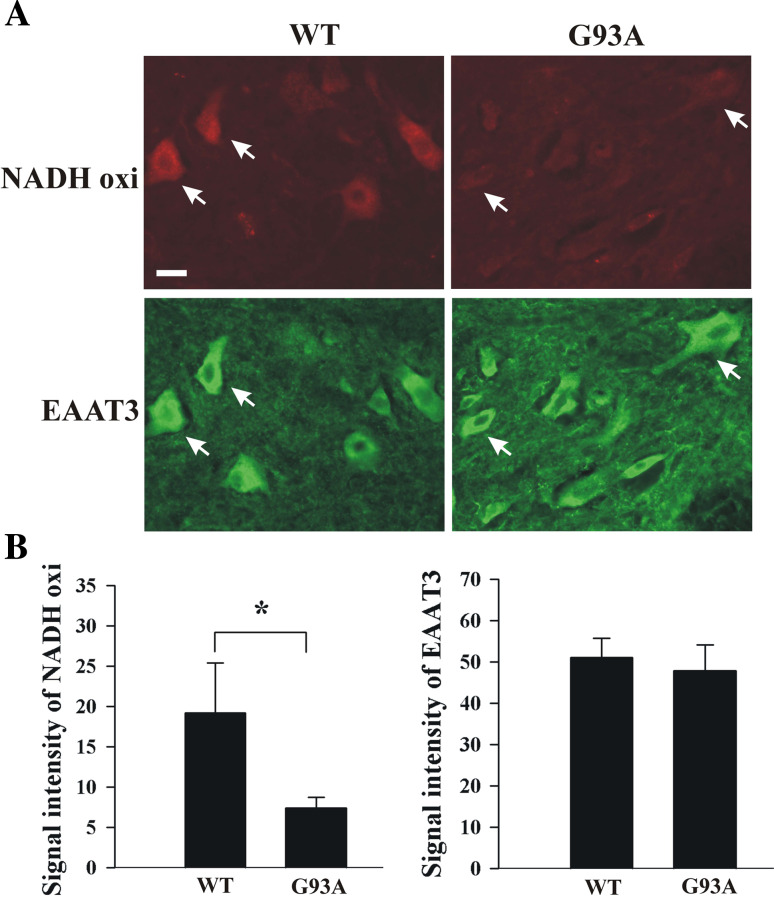
Our group has investigated how oxidative modification of mRNA affects the downstream translational process by translating oxidized mRNAs in rabbit reticulocyte lysates and by expressing oxidized mRNAs in cell lines [33, 44]. We observed that oxidative modification of mRNA causes reduced protein production. Polyribosome analysis of the oxidized mRNAs translated in rabbit reticulocyte lysates showed that oxidative modification of mRNA causes an abnormal increase in the association of mRNAs with polyribosomes during translation [44]. The results suggest that oxidized bases on mRNA may cause ribosome stalling on the mRNA or slow the translational process, leading to a decrease in protein expression. Importantly, in the study of SOD1G93A mice, we also revealed that proteins corresponding to oxidized mRNA species are significantly decreased (Fig. 4) [38]. These studies indicate that oxidative modification of mRNA affects the translational process. The detailed mechanism of how oxidized bases on mRNA affect the translational process needs to be further explored.
Fig. 4.
Proteins corresponding to oxidized mRNA species are decreased in SOD1G93A mice. a Immunofluorescent staining of lumbar spinal cord sections prepared from 60-day-old SOD1G93A mice (G93A) and nontransgenic littermates (WT) (n = 3). Mouse anti-NADH-ubiquinol oxidoreductase antibodies and rabbit anti-EAAT3 antibodies were used. A decrease in protein levels in SOD1G93A mice was found in NADH-ubiquinol oxidoreductase subunit 39 kDa (NADH oxi), whose mRNAs were highly oxidized, but not in EAAT3 protein, whose mRNAs were not oxidized. Scale bar 25 μm. b Statistical analysis of immunoreactivity within motor neurons (n = 20). Values are means ± SEM; *P < 0.0001. Details are provided in reference [38]
Furthermore, Ding et al. [41] reported a significant impairment in ribosome function in the affected areas of AD and MCI subjects. This impairment is associated with a decreased rate of and capacity for protein synthesis, decreased rRNA and tRNA levels, and increased RNA oxidation. In addition, impaired protein synthesis and decreased RNA levels were also observed in cultured neurons treated with an oxidative stressor (hydrogen peroxide) [45]. Taken together these results indicate that oxidative modification of RNA can affect the translational process and consequently less protein and/or defective protein is produced, which may have detrimental effects on cellular function.
Removal and/or repair
The detailed mechanisms of how cells handle oxidatively damaged RNA under normal physiological conditions remain largely unexplored. For the mRNAs, there are four possible scenarios which can occur when the translational machinery encounters an oxidized base on mRNA. First, translational processes may terminate at the oxidized site and produce truncated proteins. Tanaka et al. [46] reported that oxidized mRNA induces translation errors, producing short polypeptides because of premature termination or translation error-induced degradation. However, we did not detect truncated proteins produced from oxidatively damaged mRNAs in our studies [33, 44]. Second, oxidized bases on mRNAs may alter the base-pairing capacity with tRNA and consequently produce mutated proteins. Currently, there are no reports supporting this possibility. We have performed mass spectrometry of products translated from oxidized mRNAs but found no mutated proteins. Third, oxidized RNA may be recognized and subject to degradation. Quality control of gene expression operates post-transcriptionally at various levels in eukaryotes. For example, nonsense-mediated mRNA decay (NMD) is an RNA surveillance mechanism that rapidly degrades mRNAs harboring premature termination codons [47]. Mutant mRNAs that have an in-frame stop codon upstream of the normal stop codon are recognized by the NMD machinery, leading to mRNA destabilization. There is a possibility that similar RNA surveillance mechanisms are present in cells for removing oxidatively damaged mRNAs. It is possible that the translational process may terminate when translational machinery encounters the oxidatively modified bases on mRNA. This aberrant termination may trigger the NMD-like machinery, which directs the oxidized mRNAs to degradation. It has been shown that Y box-binding protein (YB-1) has the ability to bind specifically to 8OHG-containing RNA, which may discriminate the oxidized RNA from normal RNA, thereby sequestrating the damaged RNA from the translation and directing the oxidized RNA to degradation [48, 49]. Finally, oxidized bases may be repaired. Alkylation damage in RNA can be repaired by the E. coli enzyme AlkB and its human homologue hABH3 by hydroxylation of the methyl group on damaged RNA bases, thereby directly reversing alkylation damage [50]. Although no repair enzyme for oxidized mRNA has yet been found, there is a possibility that such an enzyme is present in cells, as mRNA oxidation occurs no less frequently than methylation.
Role of RNA oxidation in the pathogenesis of various diseases
Alzheimer’s disease
An estimated 35 million-plus people worldwide had AD in 2009. AD is the most common neurodegenerative disease, and is characterized by progressive loss of neurons, particularly in the cortex and hippocampus [51]. The clinical hallmarks are progressive impairment in memory, judgment, language, and orientation to physical surroundings. The pathological hallmarks are loss of neurons and synapses, extracellular senile plaques containing the Aβ peptide, and neurofibrillary tangles (aggregates of the microtubule-associated protein tau).
Oxidative damage has been implicated as an important mediator in the onset, progression and pathogenesis of AD. Redox-active metals, such as iron, are important causes of oxidative damage in AD because they accumulate in the brain of AD patients and are sources of redox-generated hydroxyl radicals. In the brain of AD patients, excessive amounts of iron have been found to accumulate within the senile plaques and neurofibrillary tangles in the affected areas [52–56]. In addition, the vulnerable neurons in the earliest stages of the disease show elevated iron deposition [57]. Furthermore, iron can promote the cleavage and synthesis of Aβ precursor protein in an oxidative stress-mediated pathway [58–60]. Moreover, Aβ can be oxidatively modified by metal-catalyzed hydroxyl radicals and become more water-insoluble and resistant to the protease [61].
In 1999, Nunomura et al. [23] examined oxidized nucleosides in the brains of AD patients and found that oxidative damage to nucleic acids occurs predominantly in cytoplasmic RNA and is restricted to vulnerable neurons. Honda et al. [24] later showed that RNA-bound iron plays a pivotal role in RNA oxidation. They observed that the cytoplasm of hippocampal neurons showed significantly higher redox activity and iron staining in the brains of AD patients than that in the brains of age-matched controls. Importantly, both iron staining and redox activity were susceptible to RNase treatment, suggesting a possible physical association between iron and RNA. Consistently, ribosomes purified from hippocampi of the brains of AD patients contained significantly higher levels of RNase-sensitive iron and redox activity than those of the controls. The results of this study suggest that rRNA in AD is oxidized by bound redox-active iron.
Our group has investigated mRNA oxidation in the brains of AD patients. We determined the magnitude of mRNA oxidation by an immunoprecipitation procedure (described above). The results showed that up to 50% of mRNAs are oxidatively damaged in the frontal cortices of AD patients diagnosed as the mild or moderate stage, while less than 2% of the mRNAs were oxidized in age-matched controls (Fig. 2) [37]. Furthermore, we previously cloned oxidized mRNAs [33] and also recently performed DNA microarray analysis to identify oxidized mRNA species. The results showed that many oxidized mRNA species are related to AD—either the mRNAs have been characterized in AD or their protein functions have been implicated in the pathogenesis. RNA oxidation may be an important factor that causes neuron deterioration in AD.
Parkinson’s disease
There are likely to be more than 6 million people worldwide with PD. PD is the second most common neurodegenerative disease after AD. It is characterized clinically by muscular rigidity, resting tremor, bradykinesia, and postural instability [62]. The pathological hallmarks are loss of dopaminergic neurons in the substantia nigra in association with the presence of the intracytoplasmic neuronal inclusions (Lewy bodies) of α-synuclein [63].
Oxidative stress has been identified as one of the pathogenic factors. In PD patients, ROS, such as hydrogen peroxide, can be generated by dopamine redox chemistry through the Fenton reaction, as dopamine is a good metal chelator and electron donor that reacts with iron and manganese [64, 65]. An increase of metal iron(III) and total iron concentration has been found in the post-mortem substantia nigra of PD patients [66]. Furthermore, studies have indicated that mutation in α-synuclein could promote the accumulation and interaction of dopamine with iron and thus enhance ROS production [67]. Manganese can also cause oxidative damage to DNA, induce dopaminergic neuronal loss through apoptotic pathways, and reduce antioxidants such as GSH, catalase and thiols [68–72]. Beside the oxidative damage to lipid, protein and DNA [25, 73–75], elevated RNA oxidation has also been observed in both post-mortem substantia nigra tissue and CSF from living PD patients [19, 25, 26]. Investigations of the relationship between the levels of 8-OHG in the CSF and the duration of disease suggest that RNA oxidation may occur in the early stage of PD. Further studies are needed to determine if RNA oxidation contributes to the pathogenesis of PD.
Amyotrophic lateral sclerosis
ALS is a fatal neurodegenerative disorder characterized by progressive degeneration of motor neurons in the spinal cord, motor cortex and brainstem [76]. Approximately 5–10% of patients with ALS show familial inheritance (familial ALS, FALS). In the majority of patients, there is no inherited link, i.e. sporadic ALS (SALS). Both FALS and SALS produce similar pathological changes and symptoms. Our group has investigated RNA oxidation in ALS (both SALS and FALS) post-mortem tissues and found that poly(A)+ mRNAs are oxidatively damaged in the affected areas of ALS patients [38].
In about 20% of FALS patients, there is mutation in the gene encoding the antioxidant enzyme Cu2+/Zn2+ SOD (SOD1). In transgenic mice overexpression of some of FALS-linked mutant SOD1 proteins results in the development of a neurological disorder that resembles ALS [77]. Mutant SOD1 causes motor neuron degeneration by the acquisition of a toxic gain of function rather than by the loss of enzymatic activity [76]. Moreover, mutant SOD1 toxicity to motor neurons is non-cell autonomous, i.e. mutant damage is required within both motor neurons and non-neuronal cells [78]. One of the proposed mechanisms is that mutations promote oxidative stress by weakening catalytic copper binding and buffering [79]. Treatment of various antioxidants has been tested in mutant SOD1 transgenic models. Such treatments have resulted in delayed disease onset and in some cases, have slowed disease progression (for review see reference [80]).
We have investigated the role of mRNA oxidation in the pathogenesis of mutant SOD1-mediated motor neuron degeneration using SOD1G93A mice, the most commonly used transgenic mouse in ALS basic research [38]. This was the first study using an animal model of the disease to demonstrate the role RNA oxidation in the process of neuron degeneration. There are several important findings of this study. First, RNA oxidation in motor neurons occurs at an early presymptomatic stage far preceding motor neuron degeneration, and is therefore not a consequence of motor neurons dying, as described above (Fig. 3). Second, many mRNA species that have been found to be highly oxidized in SOD1G93A mice are related to ALS, including mRNAs encoded for SOD1, dynactin 1, vesicle-associated membrane protein 1 (VAMP), and neurofilament subunits. Third, the protein expression levels for the oxidized mRNA species are significantly decreased (Fig. 4). This indicates that oxidative modification of mRNA does cause reduced protein expression and/or induces translation errors in vivo. Finally, we observed that vitamin E treatment reduces oxidized mRNA levels, restores protein expression levels and partially protects vulnerable motor neurons. The results of this study suggest that RNA oxidation promotes motor neuron deterioration during the disease process.
Spinal cord injury
In the United States, a new SCI is sustained on average every 40–50 min, which represents about 10,000 new cases each year. Most SCIs result from a contusion-type injury in which the vertebral bodies and/or intervertebral discs are rapidly displaced into the spinal canal causing crushing and bruising of the delicate spinal tissue [81, 82]. The initial impact leads to immediate hemorrhage and rapid cell death at the impact site. After the initial mechanical destruction, SCI progresses over time with the induction of a delayed cell death cascade which results in lesion enlargement. This secondary injury is the current research focus and a treatment target for SCI. Free radical formation is believed to be a critical component of secondary injury evolution.
During the development of secondary injury, several free radical pathways are activated by increased intracellular calcium, which is mediated by glutamate and cytokine release after the initial injury. The quickly increasing reactive free radicals in turn closely cooperate with glutamate and cytokines to enhance the oxidative stress propagation and contribute to the spreading of secondary cell death [83]. There is substantial evidence that oxidative damage is a critical component during the development of secondary injury [84–94].
We have investigated RNA oxidation after spinal cord contusion injury in rats. We observed a significant increase in RNA oxidation in the lesion center immediately after the injury and the level remained high over 3 h (unpublished data), while in the cord segment rostral to the lesion center (10 mm), RNA oxidation did not increase significantly until 3 h after the injury. Increased RNA oxidation primarily occurred in the neurons around the lesion center at an early stage and in the oligodendrocytes during secondary injury progression, and these cells died later. These results indicate a spreading pattern of the RNA oxidation from the lesion site to distal areas, and this coincides with the developmental pattern of the secondary injury. These results suggest that RNA oxidation may play an important role in the development of secondary injury.
Epilepsy
As a common chronic neurological disorder, epilepsy is characterized by recurrent unprovoked seizures. It afflicts more than 50 million people worldwide. Previous studies have demonstrated that seizure-induced mitochondrial dysfunction and excess free radical production cause oxidative damage to cellular components and initiate the mitochondrial apoptotic pathway [95, 96]. Oxidative stress is also considered an important consequence of excitotoxicity [97–100], one of the proposed mechanisms for seizure-induced brain damage [101]. Seizure-induced pathology can be partially prevented by treatment with antioxidants including SOD mimetics, melatonin, spin traps, vitamin C, and coenzyme Q10 ([102–105]; unpublished data). Oxidative damage has been reported in proteins, lipids and mitochondrial DNA after seizure activity [106–108].
Our group has recently investigated whether RNA oxidation plays a role in epileptogenesis, a series of events that occur between the event that causes epilepsy and the first spontaneous seizure. The pilocarpine-induced status epilepticus model was used in this study. We observed a significant increase in RNA oxidation in vulnerable neurons of mouse brain shortly after pilocarpine-induced status epilepticus and these neurons died later (unpublished data). Furthermore, daily supplementation with antioxidant, i.e. coenzyme Q10, significantly reduced RNA oxidation and importantly also protected the mice from pilocarpine-induced seizure activity and neuronal loss. These results suggest that RNA oxidation may be an important contributing factor in the process of seizure-induced neuron degeneration and epileptogenesis.
Atherosclerosis
Atherosclerosis is a chronic vasculoocclusive disease characterized by intimal thickening, atheromatous plaques in the intima of the medium, and macrophage infiltration with endothelial dysfunction [109]. Atherosclerosis develops from low-density lipoprotein (LDL) molecules becoming oxidized by free radicals (the LDL molecule carries cholesterol throughout the body). Blood in arteries contains plenty of oxygen and is the site of atherosclerosis development. When oxidized LDL comes into contact with an artery wall, a series of reactions occur to repair the resulting damage. The body’s immune system responds to such damage by sending specialized white blood cells (macrophages and T lymphocytes) which absorb the oxidized LDL by forming specialized “foam cells”. However, these white blood cells are not able to process the oxidized LDL, and ultimately grow and then rupture, depositing a greater amount of oxidized cholesterol on the artery walls. Eventually, the artery becomes inflamed. The cholesterol plaque causes the muscle cells to enlarge and form a hard cover over the affected area. This hard cover causes narrowing of the artery, reducing blood flow and increasing blood pressure.
Oxidative stress plays a key role in the progression of atherosclerosis. Elevated oxidative damage to DNA has been reported in both human and experimental atherosclerosis [110, 111]. Substantial RNA oxidation has also been detected in smooth muscle cells and endothelial cells of human atherosclerotic plaques [112, 113]. The implications of RNA oxidation in atherosclerosis still remain unknown.
Other diseases
Increased RNA oxidation has also been detected in brain samples from patients with Down syndrome, dementia of Lewy bodies, prion diseases, subacute sclerosing panencephalitis and xeroderma pigmentosum [27–29, 31, 32, 114], in urine samples from patients with hereditary hemochromatosis [115], in rat skeletal muscle with aging and disuse atrophy [116], in muscle cells of patients with rimmed vacuole myopathy [117], and in human emphysematous lungs [118]. However, currently, studies on RNA oxidation are still limited to neurodegenerative diseases, while oxidative stress has been well characterized in a large spectrum of diseases and disorders of physiological dysfunction, e.g. ischemia, cancers, obesity, diabetes, inflammatory diseases, viral infections, chronic fatigue syndrome, kidney diseases, depression and AIDS. The role of RNA oxidation in these oxidative stress-associated diseases remains to be explored.
Conclusions and perspectives
In the past decade, we have learned that RNA is very vulnerable to oxidative damage. RNA oxidation is involved in a wide variety of diseases and is not a consequence of cells dying but an early event in pathogenesis. Oxidative damage to RNA results in disruption of the translational process and impairment of protein synthesis. From the study of SOD1G93A mice, we have learned that RNA oxidation is an important contributing factor and not simply an epiphenomenon in the process of cell death. However, we are still in the early stages of understanding the role of RNA oxidation in the process of cell deterioration and cell death.
In our opinion, the following questions need to be answered in this field. How do cells handle oxidatively damaged RNA under normal physiological conditions? Is oxidized RNA degraded, repaired, or both? What are the repair/degradation processes and what proteins are involved in the processes? These are very challenging questions that require further research in order to move forward. One could isolate the repair/degradation complexes and apply protein microarray or proteomic analysis to identify proteins involved in the processes. Once such proteins have been identified, one could modify the handling processes by the knockdown approach, in cells or in animals, and study the consequences. When more information about how cells handle oxidatively damaged RNA is known, one could further ask “is the capacity to handle oxidatively damaged RNA altered in the diseased condition?”. One could characterize the handling processes in animal models of disease, such as SOD1G93A mice. One could analyze the proteins that are involved in handling oxidized RNA in post-mortem tissues from patients. Furthermore, one could enhance the handling processes or prevent oxidative damage to RNA from by a transgenic or pharmacological approach. Further investigation of the above-described mechanisms is necessary to better understand the functional role of RNA oxidation in the pathogenesis of various diseases. Finally, RNA oxidation is an early event preceding cell death, and might be a diagnostic target. Early diagnosis allowing treatment at the prodromal stage may prevent or slow disease progression.
Acknowledgments
This work was supported by the NIH (grant AG027797), the ALS Association, the Alzheimer’s Association, and the Neuroscience Education and Research Foundation.
References
- 1.Miller RA, Britigan BE. Role of oxidants in microbial pathophysiology. Clin Microbiol Rev. 1997;10:1–18. doi: 10.1128/cmr.10.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pacher P, Beckman JS, Liaudet L. Nitric oxide and peroxynitrite in health and disease. Physiol Rev. 2007;87:315–424. doi: 10.1152/physrev.00029.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Muller FL, Lustgarten MS, Jang Y, Richardson A, Van Remmen H. Trends in oxidative aging theories. Free Radic Biol Med. 2007;43:477–503. doi: 10.1016/j.freeradbiomed.2007.03.034. [DOI] [PubMed] [Google Scholar]
- 4.Fearon IM, Faux SP. Oxidative stress and cardiovascular disease: novel tools give (free) radical insight. J Mol Cell Cardiol. 2009;47:372–381. doi: 10.1016/j.yjmcc.2009.05.013. [DOI] [PubMed] [Google Scholar]
- 5.Cederbaum AI, Lu Y, Wu D. Role of oxidative stress in alcohol-induced liver injury. Arch Toxicol. 2009;83:519–548. doi: 10.1007/s00204-009-0432-0. [DOI] [PubMed] [Google Scholar]
- 6.Shatwell KP, Segal AW. NADPH oxidase. Int J Biochem Cell Biol. 1996;28:1191–1195. doi: 10.1016/s1357-2725(96)00084-2. [DOI] [PubMed] [Google Scholar]
- 7.Zelko IN, Mariani TJ, Folz RJ. Superoxide dismutase multigene family: a comparison of the CuZn-SOD (SOD1), Mn-SOD (SOD2), and EC-SOD (SOD3) gene structures, evolution, and expression. Free Radic Biol Med. 2002;33:337–349. doi: 10.1016/s0891-5849(02)00905-x. [DOI] [PubMed] [Google Scholar]
- 8.Chelikani P, Fita I, Loewen PC. Diversity of structures and properties among catalases. Cell Mol Life Sci. 2004;61:192–208. doi: 10.1007/s00018-003-3206-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mills GC. Hemoglobin catabolism. I. Glutathione peroxidase, an erythrocyte enzyme which protects hemoglobin from oxidative breakdown. J Biol Chem. 1957;229:189–197. [PubMed] [Google Scholar]
- 10.Sies H. Strategies of antioxidant defense. Eur J Biochem. 1993;215:213–219. doi: 10.1111/j.1432-1033.1993.tb18025.x. [DOI] [PubMed] [Google Scholar]
- 11.Culotta E, Koshland DE., Jr NO news is good news. Science. 1992;258:1862–1865. doi: 10.1126/science.1361684. [DOI] [PubMed] [Google Scholar]
- 12.Hibbs JB, Jr, Taintor RR, Vavrin Z, Rachlin EM. Nitric oxide: a cytotoxic activated macrophage effector molecule. Biochem Biophys Res Commun. 1988;157:87–94. doi: 10.1016/s0006-291x(88)80015-9. [DOI] [PubMed] [Google Scholar]
- 13.Dalle-Donne I, Aldini G, Carini M, Colombo R, Rossi R, Milzani A. Protein carbonylation, cellular dysfunction, and disease progression. J Cell Mol Med. 2006;10:389–406. doi: 10.1111/j.1582-4934.2006.tb00407.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ischiropoulos H. Protein tyrosine nitration—an update. Arch Biochem Biophys. 2009;484:117–121. doi: 10.1016/j.abb.2008.10.034. [DOI] [PubMed] [Google Scholar]
- 15.Nair U, Bartsch H, Nair J. Lipid peroxidation-induced DNA damage in cancer-prone inflammatory diseases: a review of published adduct types and levels in humans. Free Radic Biol Med. 2007;43:1109–1120. doi: 10.1016/j.freeradbiomed.2007.07.012. [DOI] [PubMed] [Google Scholar]
- 16.Cadet J, Douki T, Gasparutto D, Ravanat JL. Oxidative damage to DNA: formation, measurement and biochemical features. Mutat Res. 2003;531:5–23. doi: 10.1016/j.mrfmmm.2003.09.001. [DOI] [PubMed] [Google Scholar]
- 17.Barciszewski J, Barciszewska MZ, Siboska G, Rattan SI, Clark BF. Some unusual nucleic acid bases are products of hydroxyl radical oxidation of DNA and RNA. Mol Biol Rep. 1999;26:231–238. doi: 10.1023/a:1007058602594. [DOI] [PubMed] [Google Scholar]
- 18.Abe T, Tohgi H, Isobe C, Murata T, Sato C. Remarkable increase in the concentration of 8-hydroxyguanosine in cerebrospinal fluid from patients with Alzheimer’s disease. J Neurosci Res. 2002;70:447–450. doi: 10.1002/jnr.10349. [DOI] [PubMed] [Google Scholar]
- 19.Abe T, Isobe C, Murata T, Sato C, Tohgi H. Alteration of 8-hydroxyguanosine concentrations in the cerebrospinal fluid and serum from patients with Parkinson’s disease. Neurosci Lett. 2003;336:105–108. doi: 10.1016/s0304-3940(02)01259-4. [DOI] [PubMed] [Google Scholar]
- 20.Hofer T, Seo AY, Prudencio M, Leeuwenburgh C. A method to determine RNA and DNA oxidation simultaneously by HPLC-ECD: greater RNA than DNA oxidation in rat liver after doxorubicin administration. Biol Chem. 2006;387:103–111. doi: 10.1515/BC.2006.014. [DOI] [PubMed] [Google Scholar]
- 21.Park EM, Shigenaga MK, Degan P, Korn TS, Kitzler JW, Wehr CM, Kolachana P, Ames BN. Assay of excised oxidative DNA lesions: isolation of 8-oxoguanine and its nucleoside derivatives from biological fluids with a monoclonal antibody column. Proc Natl Acad Sci USA. 1992;89:3375–3379. doi: 10.1073/pnas.89.8.3375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yin B, Whyatt RM, Perera FP, Randall MC, Cooper TB, Santella RM. Determination of 8-hydroxydeoxyguanosine by an immunoaffinity chromatography-monoclonal antibody-based ELISA. Free Radic Biol Med. 1995;18:1023–1032. doi: 10.1016/0891-5849(95)00003-g. [DOI] [PubMed] [Google Scholar]
- 23.Nunomura A, Perry G, Pappolla MA, Wade R, Hirai K, Chiba S, Smith MA. RNA oxidation is a prominent feature of vulnerable neurons in Alzheimer’s disease. J Neurosci. 1999;19:1959–1964. doi: 10.1523/JNEUROSCI.19-06-01959.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Honda K, Smith MA, Zhu X, Baus D, Merrick WC, Tartakoff AM, Hattier T, Harris PL, Siedlak SL, Fujioka H, Liu Q, Moreira PI, Miller FP, Nunomura A, Shimohama S, Perry G. Ribosomal RNA in Alzheimer disease is oxidized by bound redox-active iron. J Biol Chem. 2005;280:20978–20986. doi: 10.1074/jbc.M500526200. [DOI] [PubMed] [Google Scholar]
- 25.Zhang J, Perry G, Smith MA, Robertson D, Olson SJ, Graham DG, Montine TJ. Parkinson’s disease is associated with oxidative damage to cytoplasmic DNA and RNA in substantia nigra neurons. Am J Pathol. 1999;154:1423–1429. doi: 10.1016/S0002-9440(10)65396-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kikuchi A, Takeda A, Onodera H, Kimpara T, Hisanaga K, Sato N, Nunomura A, Castellani RJ, Perry G, Smith MA, Itoyama Y. Systemic increase of oxidative nucleic acid damage in Parkinson’s disease and multiple system atrophy. Neurobiol Dis. 2002;9:244–248. doi: 10.1006/nbdi.2002.0466. [DOI] [PubMed] [Google Scholar]
- 27.Nunomura A, Perry G, Hirai K, Aliev G, Takeda A, Chiba S, Smith MA. Neuronal RNA oxidation in Alzheimer’s disease and Down’s syndrome. Ann N Y Acad Sci. 1999;893:362–364. doi: 10.1111/j.1749-6632.1999.tb07855.x. [DOI] [PubMed] [Google Scholar]
- 28.Nunomura A, Chiba S, Kosaka K, Takeda A, Castellani RJ, Smith MA, Perry G. Neuronal RNA oxidation is a prominent feature of dementia with Lewy bodies. Neuroreport. 2002;13:2035–2039. doi: 10.1097/00001756-200211150-00009. [DOI] [PubMed] [Google Scholar]
- 29.Guentchev M, Siedlak SL, Jarius C, Tagliavini F, Castellani RJ, Perry G, Smith MA, Budka H. Oxidative damage to nucleic acids in human prion disease. Neurobiol Dis. 2002;9:275–281. doi: 10.1006/nbdi.2002.0477. [DOI] [PubMed] [Google Scholar]
- 30.Lovell MA, Markesbery WR. Oxidatively modified RNA in mild cognitive impairment. Neurobiol Dis. 2008;29:169–175. doi: 10.1016/j.nbd.2007.07.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hayashi M, Arai N, Satoh J, Suzuki H, Katayama K, Tamagawa K, Morimatsu Y. Neurodegenerative mechanisms in subacute sclerosing panencephalitis. J Child Neurol. 2002;17:725–730. doi: 10.1177/08830738020170101101. [DOI] [PubMed] [Google Scholar]
- 32.Hayashi M, Araki S, Kohyama J, Shioda K, Fukatsu R. Oxidative nucleotide damage and superoxide dismutase expression in the brains of xeroderma pigmentosum group A and Cockayne syndrome. Brain Dev. 2005;27:34–38. doi: 10.1016/j.braindev.2004.04.001. [DOI] [PubMed] [Google Scholar]
- 33.Shan X, Tashiro H, Lin CL. The identification and characterization of oxidized RNAs in Alzheimer’s disease. J Neurosci. 2003;23:4913–4921. doi: 10.1523/JNEUROSCI.23-12-04913.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ding Q, Markesbery WR, Cecarini V, Keller JN. Decreased RNA, and increased RNA oxidation, in ribosomes from early Alzheimer’s disease. Neurochem Res. 2006;31:705–710. doi: 10.1007/s11064-006-9071-5. [DOI] [PubMed] [Google Scholar]
- 35.Ding Q, Dimayuga E, Markesbery WR, Keller JN. Proteasome inhibition increases DNA and RNA oxidation in astrocyte and neuron cultures. J Neurochem. 2004;91:1211–1218. doi: 10.1111/j.1471-4159.2004.02802.x. [DOI] [PubMed] [Google Scholar]
- 36.Gorg B, Qvartskhava N, Keitel V, Bidmon HJ, Selbach O, Schliess F, Haussinger D. Ammonia induces RNA oxidation in cultured astrocytes and brain in vivo. Hepatology. 2008;48:567–579. doi: 10.1002/hep.22345. [DOI] [PubMed] [Google Scholar]
- 37.Shan X, Lin CL. Quantification of oxidized RNAs in Alzheimer’s disease. Neurobiol Aging. 2006;27:657–662. doi: 10.1016/j.neurobiolaging.2005.03.022. [DOI] [PubMed] [Google Scholar]
- 38.Chang Y, Kong Q, Shan X, Tian G, Ilieva H, Cleveland DW, Rothstein JD, Borchelt DR, Wong PC, Lin CL. Messenger RNA oxidation occurs early in disease pathogenesis and promotes motor neuron degeneration in ALS. PLoS One. 2008;3:e2849. doi: 10.1371/journal.pone.0002849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nelson PT, Keller JN. RNA in brain disease: no longer just “the messenger in the middle”. J Neuropathol Exp Neurol. 2007;66:461–468. doi: 10.1097/01.jnen.0000240474.27791.f3. [DOI] [PubMed] [Google Scholar]
- 40.Cao X, Yeo G, Muotri AR, Kuwabara T, Gage FH. Noncoding RNAs in the mammalian central nervous system. Annu Rev Neurosci. 2006;29:77–103. doi: 10.1146/annurev.neuro.29.051605.112839. [DOI] [PubMed] [Google Scholar]
- 41.Ding Q, Markesbery WR, Chen Q, Li F, Keller JN. Ribosome dysfunction is an early event in Alzheimer’s disease. J Neurosci. 2005;25:9171–9175. doi: 10.1523/JNEUROSCI.3040-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nunomura A, Chiba S, Lippa CF, Cras P, Kalaria RN, Takeda A, Honda K, Smith MA, Perry G. Neuronal RNA oxidation is a prominent feature of familial Alzheimer’s disease. Neurobiol Dis. 2004;17:108–113. doi: 10.1016/j.nbd.2004.06.003. [DOI] [PubMed] [Google Scholar]
- 43.Nunomura A, Perry G, Aliev G, Hirai K, Takeda A, Balraj EK, Jones PK, Ghanbari H, Wataya T, Shimohama S, Chiba S, Atwood CS, Petersen RB, Smith MA. Oxidative damage is the earliest event in Alzheimer disease. J Neuropathol Exp Neurol. 2001;60:759–767. doi: 10.1093/jnen/60.8.759. [DOI] [PubMed] [Google Scholar]
- 44.Shan X, Chang Y, Lin CL. Messenger RNA oxidation is an early event preceding cell death and causes reduced protein expression. FASEB J. 2007;21:2753–2764. doi: 10.1096/fj.07-8200com. [DOI] [PubMed] [Google Scholar]
- 45.Ding Q, Dimayuga E, Keller JN. Oxidative stress alters neuronal RNA- and protein-synthesis: implications for neural viability. Free Radic Res. 2007;41:903–910. doi: 10.1080/10715760701416996. [DOI] [PubMed] [Google Scholar]
- 46.Tanaka M, Chock PB, Stadtman ER. Oxidized messenger RNA induces translation errors. Proc Natl Acad Sci USA. 2007;104:66–71. doi: 10.1073/pnas.0609737104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Shyu AB, Wilkinson MF, van Hoof A. Messenger RNA regulation: to translate or to degrade. EMBO J. 2008;27:471–481. doi: 10.1038/sj.emboj.7601977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hayakawa H, Kuwano M, Sekiguchi M. Specific binding of 8-oxoguanine-containing RNA to polynucleotide phosphorylase protein. Biochemistry. 2001;40:9977–9982. doi: 10.1021/bi010595q. [DOI] [PubMed] [Google Scholar]
- 49.Hayakawa H, Uchiumi T, Fukuda T, Ashizuka M, Kohno K, Kuwano M, Sekiguchi M. Binding capacity of human YB-1 protein for RNA containing 8-oxoguanine. Biochemistry. 2002;41:12739–12744. doi: 10.1021/bi0201872. [DOI] [PubMed] [Google Scholar]
- 50.Aas PA, Otterlei M, Falnes PO, Vagbo CB, Skorpen F, Akbari M, Sundheim O, Bjoras M, Slupphaug G, Seeberg E, Krokan HE. Human and bacterial oxidative demethylases repair alkylation damage in both RNA and DNA. Nature. 2003;421:859–863. doi: 10.1038/nature01363. [DOI] [PubMed] [Google Scholar]
- 51.McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM. Clinical diagnosis of Alzheimer’s disease: report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer’s Disease. Neurology. 1984;34:939–944. doi: 10.1212/wnl.34.7.939. [DOI] [PubMed] [Google Scholar]
- 52.Smith MA, Harris PL, Sayre LM, Perry G. Iron accumulation in Alzheimer disease is a source of redox-generated free radicals. Proc Natl Acad Sci USA. 1997;94:9866–9868. doi: 10.1073/pnas.94.18.9866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lovell MA, Robertson JD, Teesdale WJ, Campbell JL, Markesbery WR. Copper, iron and zinc in Alzheimer’s disease senile plaques. J Neurol Sci. 1998;158:47–52. doi: 10.1016/s0022-510x(98)00092-6. [DOI] [PubMed] [Google Scholar]
- 54.Sayre LM, Perry G, Harris PL, Liu Y, Schubert KA, Smith MA. In situ oxidative catalysis by neurofibrillary tangles and senile plaques in Alzheimer’s disease: a central role for bound transition metals. J Neurochem. 2000;74:270–279. doi: 10.1046/j.1471-4159.2000.0740270.x. [DOI] [PubMed] [Google Scholar]
- 55.Connor JR, Milward EA, Moalem S, Sampietro M, Boyer P, Percy ME, Vergani C, Scott RJ, Chorney M. Is hemochromatosis a risk factor for Alzheimer’s disease? J Alzheimers Dis. 2001;3:471–477. doi: 10.3233/jad-2001-3506. [DOI] [PubMed] [Google Scholar]
- 56.Casadesus G, Smith MA, Zhu X, Aliev G, Cash AD, Honda K, Petersen RB, Perry G. Alzheimer disease: evidence for a central pathogenic role of iron-mediated reactive oxygen species. J Alzheimers Dis. 2004;6:165–169. doi: 10.3233/jad-2004-6208. [DOI] [PubMed] [Google Scholar]
- 57.Honda K, Casadesus G, Petersen RB, Perry G, Smith MA. Oxidative stress and redox-active iron in Alzheimer’s disease. Ann N Y Acad Sci. 2004;1012:179–182. doi: 10.1196/annals.1306.015. [DOI] [PubMed] [Google Scholar]
- 58.Yan SD, Yan SF, Chen X, Fu J, Chen M, Kuppusamy P, Smith MA, Perry G, Godman GC, Nawroth P, Zweier JL, Stern D. Non-enzymatically glycated tau in Alzheimer’s disease induces neuronal oxidant stress resulting in cytokine gene expression and release of amyloid beta-peptide. Nat Med. 1995;1:693–699. doi: 10.1038/nm0795-693. [DOI] [PubMed] [Google Scholar]
- 59.Rogers JT, Randall JD, Cahill CM, Eder PS, Huang X, Gunshin H, Leiter L, McPhee J, Sarang SS, Utsuki T, Greig NH, Lahiri DK, Tanzi RE, Bush AI, Giordano T, Gullans SR. An iron-responsive element type II in the 5′-untranslated region of the Alzheimer’s amyloid precursor protein transcript. J Biol Chem. 2002;277:45518–45528. doi: 10.1074/jbc.M207435200. [DOI] [PubMed] [Google Scholar]
- 60.Tamagno E, Parola M, Bardini P, Piccini A, Borghi R, Guglielmotto M, Santoro G, Davit A, Danni O, Smith MA, Perry G, Tabaton M. Beta-site APP cleaving enzyme up-regulation induced by 4-hydroxynonenal is mediated by stress-activated protein kinases pathways. J Neurochem. 2005;92:628–636. doi: 10.1111/j.1471-4159.2004.02895.x. [DOI] [PubMed] [Google Scholar]
- 61.Atwood CS, Perry G, Zeng H, Kato Y, Jones WD, Ling KQ, Huang X, Moir RD, Wang D, Sayre LM, Smith MA, Chen SG, Bush AI. Copper mediates dityrosine cross-linking of Alzheimer’s amyloid-beta. Biochemistry. 2004;43:560–568. doi: 10.1021/bi0358824. [DOI] [PubMed] [Google Scholar]
- 62.Hoehn MM, Yahr MD. Parkinsonism: onset, progression and mortality. Neurology. 1967;17:427–442. doi: 10.1212/wnl.17.5.427. [DOI] [PubMed] [Google Scholar]
- 63.Pollanen MS, Dickson DW, Bergeron C. Pathology and biology of the Lewy body. J Neuropathol Exp Neurol. 1993;52:183–191. doi: 10.1097/00005072-199305000-00001. [DOI] [PubMed] [Google Scholar]
- 64.Parenti M, Rusconi L, Cappabianca V, Parati EA, Groppetti A. Role of dopamine in manganese neurotoxicity. Brain Res. 1988;473:236–240. doi: 10.1016/0006-8993(88)90852-9. [DOI] [PubMed] [Google Scholar]
- 65.Kienzl E, Puchinger L, Jellinger K, Linert W, Stachelberger H, Jameson RF. The role of transition metals in the pathogenesis of Parkinson’s disease. J Neurol Sci. 1995;134(Suppl):69–78. doi: 10.1016/0022-510x(95)00210-s. [DOI] [PubMed] [Google Scholar]
- 66.Sofic E, Riederer P, Heinsen H, Beckmann H, Reynolds GP, Hebenstreit G, Youdim MB. Increased iron (III) and total iron content in post mortem substantia nigra of parkinsonian brain. J Neural Transm. 1988;74:199–205. doi: 10.1007/BF01244786. [DOI] [PubMed] [Google Scholar]
- 67.Lotharius J, Brundin P. Impaired dopamine storage resulting from alpha-synuclein mutations may contribute to the pathogenesis of Parkinson’s disease. Hum Mol Genet. 2002;11:2395–2407. doi: 10.1093/hmg/11.20.2395. [DOI] [PubMed] [Google Scholar]
- 68.Liccione JJ, Maines MD. Selective vulnerability of glutathione metabolism and cellular defense mechanisms in rat striatum to manganese. J Pharmacol Exp Ther. 1988;247:156–161. [PubMed] [Google Scholar]
- 69.Desole MS, Sciola L, Delogu MR, Sircana S, Migheli R, Miele E. Role of oxidative stress in the manganese and 1-methyl-4-(2'-ethylphenyl)-1,2,3,6-tetrahydropyridine-induced apoptosis in PC12 cells. Neurochem Int. 1997;31:169–176. doi: 10.1016/s0197-0186(96)00146-5. [DOI] [PubMed] [Google Scholar]
- 70.Desole MS, Esposito G, Migheli R, Sircana S, Delogu MR, Fresu L, Miele M, de Natale G, Miele E. Glutathione deficiency potentiates manganese toxicity in rat striatum and brainstem and in PC12 cells. Pharmacol Res. 1997;36:285–292. doi: 10.1006/phrs.1997.0197. [DOI] [PubMed] [Google Scholar]
- 71.Shen XM, Dryhurst G. Iron- and manganese-catalyzed autoxidation of dopamine in the presence of l-cysteine: possible insights into iron- and manganese-mediated dopaminergic neurotoxicity. Chem Res Toxicol. 1998;11:824–837. doi: 10.1021/tx980036t. [DOI] [PubMed] [Google Scholar]
- 72.Oikawa S, Hirosawa I, Tada-Oikawa S, Furukawa A, Nishiura K, Kawanishi S. Mechanism for manganese enhancement of dopamine-induced oxidative DNA damage and neuronal cell death. Free Radic Biol Med. 2006;41:748–756. doi: 10.1016/j.freeradbiomed.2006.05.018. [DOI] [PubMed] [Google Scholar]
- 73.Yoritaka A, Hattori N, Uchida K, Tanaka M, Stadtman ER, Mizuno Y. Immunohistochemical detection of 4-hydroxynonenal protein adducts in Parkinson disease. Proc Natl Acad Sci USA. 1996;93:2696–2701. doi: 10.1073/pnas.93.7.2696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Alam ZI, Jenner A, Daniel SE, Lees AJ, Cairns N, Marsden CD, Jenner P, Halliwell B. Oxidative DNA damage in the parkinsonian brain: an apparent selective increase in 8-hydroxyguanine levels in substantia nigra. J Neurochem. 1997;69:1196–1203. doi: 10.1046/j.1471-4159.1997.69031196.x. [DOI] [PubMed] [Google Scholar]
- 75.Alam ZI, Daniel SE, Lees AJ, Marsden DC, Jenner P, Halliwell B. A generalised increase in protein carbonyls in the brain in Parkinson’s but not incidental Lewy body disease. J Neurochem. 1997;69:1326–1329. doi: 10.1046/j.1471-4159.1997.69031326.x. [DOI] [PubMed] [Google Scholar]
- 76.Boillee S, Vande Velde C, Cleveland DW. ALS: a disease of motor neurons and their nonneuronal neighbors. Neuron. 2006;52:39–59. doi: 10.1016/j.neuron.2006.09.018. [DOI] [PubMed] [Google Scholar]
- 77.Julien JP, Kriz J. Transgenic mouse models of amyotrophic lateral sclerosis. Biochim Biophys Acta. 2006;1762:1013–1024. doi: 10.1016/j.bbadis.2006.03.006. [DOI] [PubMed] [Google Scholar]
- 78.Lobsiger CS, Cleveland DW. Glial cells as intrinsic components of non-cell-autonomous neurodegenerative disease. Nat Neurosci. 2007;10:1355–1360. doi: 10.1038/nn1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Carri MT, Battistoni A, Polizio F, Desideri A, Rotilio G. Impaired copper binding by the H46R mutant of human Cu,Zn superoxide dismutase, involved in amyotrophic lateral sclerosis. FEBS Lett. 1994;356:314–316. doi: 10.1016/0014-5793(94)01295-4. [DOI] [PubMed] [Google Scholar]
- 80.Turner BJ, Talbot K. Transgenics, toxicity and therapeutics in rodent models of mutant SOD1-mediated familial ALS. Prog Neurobiol. 2008;85:94–134. doi: 10.1016/j.pneurobio.2008.01.001. [DOI] [PubMed] [Google Scholar]
- 81.Bunge RP, Puckett WR, Becerra JL, Marcillo A, Quencer RM. Observations on the pathology of human spinal cord injury. A review and classification of 22 new cases with details from a case of chronic cord compression with extensive focal demyelination. Adv Neurol. 1993;59:75–89. [PubMed] [Google Scholar]
- 82.Kakulas BA. A review of the neuropathology of human spinal cord injury with emphasis on special features. J Spinal Cord Med. 1999;22:119–124. doi: 10.1080/10790268.1999.11719557. [DOI] [PubMed] [Google Scholar]
- 83.Springer JE, Azbill RD, Mark RJ, Begley JG, Waeg G, Mattson MP. 4-hydroxynonenal, a lipid peroxidation product, rapidly accumulates following traumatic spinal cord injury and inhibits glutamate uptake. J Neurochem. 1997;68:2469–2476. doi: 10.1046/j.1471-4159.1997.68062469.x. [DOI] [PubMed] [Google Scholar]
- 84.Hall ED, Braughler JM. Role of lipid peroxidation in post-traumatic spinal cord degeneration: a review. Cent Nerv Syst Trauma. 1986;3:281–294. doi: 10.1089/cns.1986.3.281. [DOI] [PubMed] [Google Scholar]
- 85.Amar AP, Levy ML. Pathogenesis and pharmacological strategies for mitigating secondary damage in acute spinal cord injury. Neurosurgery. 1999;44:1027–1039. doi: 10.1097/00006123-199905000-00052. [DOI] [PubMed] [Google Scholar]
- 86.Leski ML, Bao F, Wu L, Qian H, Sun D, Liu D. Protein and DNA oxidation in spinal injury: neurofilaments—an oxidation target. Free Radic Biol Med. 2001;30:613–624. doi: 10.1016/s0891-5849(00)00500-1. [DOI] [PubMed] [Google Scholar]
- 87.Aksenova M, Butterfield DA, Zhang SX, Underwood M, Geddes JW. Increased protein oxidation and decreased creatine kinase BB expression and activity after spinal cord contusion injury. J Neurotrauma. 2002;19:491–502. doi: 10.1089/08977150252932433. [DOI] [PubMed] [Google Scholar]
- 88.Bao F, Chen Y, Dekaban GA, Weaver LC. Early anti-inflammatory treatment reduces lipid peroxidation and protein nitration after spinal cord injury in rats. J Neurochem. 2004;88:1335–1344. doi: 10.1046/j.1471-4159.2003.02240.x. [DOI] [PubMed] [Google Scholar]
- 89.Bao F, Chen Y, Dekaban GA, Weaver LC. An anti-CD11d integrin antibody reduces cyclooxygenase-2 expression and protein and DNA oxidation after spinal cord injury in rats. J Neurochem. 2004;90:1194–1204. doi: 10.1111/j.1471-4159.2004.02580.x. [DOI] [PubMed] [Google Scholar]
- 90.Xu M, Yip GW, Gan LT, Ng YK. Distinct roles of oxidative stress and antioxidants in the nucleus dorsalis and red nucleus following spinal cord hemisection. Brain Res. 2005;1055:137–142. doi: 10.1016/j.brainres.2005.07.003. [DOI] [PubMed] [Google Scholar]
- 91.Sharma HS, Sjoquist PO, Mohanty S, Wiklund L. Post-injury treatment with a new antioxidant compound H-290/51 attenuates spinal cord trauma-induced c-fos expression, motor dysfunction, edema formation, and cell injury in the rat. Acta Neurochir Suppl. 2006;96:322–328. doi: 10.1007/3-211-30714-1_68. [DOI] [PubMed] [Google Scholar]
- 92.King VR, Huang WL, Dyall SC, Curran OE, Priestley JV, Michael-Titus AT. Omega-3 fatty acids improve recovery, whereas omega-6 fatty acids worsen outcome, after spinal cord injury in the adult rat. J Neurosci. 2006;26:4672–4680. doi: 10.1523/JNEUROSCI.5539-05.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Huang WL, King VR, Curran OE, Dyall SC, Ward RE, Lal N, Priestley JV, Michael-Titus AT. A combination of intravenous and dietary docosahexaenoic acid significantly improves outcome after spinal cord injury. Brain. 2007;130:3004–3019. doi: 10.1093/brain/awm223. [DOI] [PubMed] [Google Scholar]
- 94.Huang WL, George KJ, Ibba V, Liu MC, Averill S, Quartu M, Hamlyn PJ, Priestley JV. The characteristics of neuronal injury in a static compression model of spinal cord injury in adult rats. Eur J Neurosci. 2007;25:362–372. doi: 10.1111/j.1460-9568.2006.05284.x. [DOI] [PubMed] [Google Scholar]
- 95.Henshall DC, Bonislawski DP, Skradski SL, Lan JQ, Meller R, Simon RP. Cleavage of bid may amplify caspase-8-induced neuronal death following focally evoked limbic seizures. Neurobiol Dis. 2001;8:568–580. doi: 10.1006/nbdi.2001.0415. [DOI] [PubMed] [Google Scholar]
- 96.Henshall DC, Araki T, Schindler CK, Lan JQ, Tiekoter KL, Taki W, Simon RP. Activation of Bcl-2-associated death protein and counter-response of Akt within cell populations during seizure-induced neuronal death. J Neurosci. 2002;22:8458–8465. doi: 10.1523/JNEUROSCI.22-19-08458.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Dugan LL, Sensi SL, Canzoniero LM, Handran SD, Rothman SM, Lin TS, Goldberg MP, Choi DW. Mitochondrial production of reactive oxygen species in cortical neurons following exposure to N-methyl-D-aspartate. J Neurosci. 1995;15:6377–6388. doi: 10.1523/JNEUROSCI.15-10-06377.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Reynolds IJ, Hastings TG. Glutamate induces the production of reactive oxygen species in cultured forebrain neurons following NMDA receptor activation. J Neurosci. 1995;15:3318–3327. doi: 10.1523/JNEUROSCI.15-05-03318.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Bindokas VP, Jordan J, Lee CC, Miller RJ. Superoxide production in rat hippocampal neurons: selective imaging with hydroethidine. J Neurosci. 1996;16:1324–1336. doi: 10.1523/JNEUROSCI.16-04-01324.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Patel M, Day BJ, Crapo JD, Fridovich I, McNamara JO. Requirement for superoxide in excitotoxic cell death. Neuron. 1996;16:345–355. doi: 10.1016/s0896-6273(00)80052-5. [DOI] [PubMed] [Google Scholar]
- 101.Olney JW, Collins RC, Sloviter RS. Excitotoxic mechanisms of epileptic brain damage. Adv Neurol. 1986;44:857–877. [PubMed] [Google Scholar]
- 102.MacGregor DG, Higgins MJ, Jones PA, Maxwell WL, Watson MW, Graham DI, Stone TW. Ascorbate attenuates the systemic kainate-induced neurotoxicity in the rat hippocampus. Brain Res. 1996;727:133–144. doi: 10.1016/0006-8993(96)00362-9. [DOI] [PubMed] [Google Scholar]
- 103.Tan DX, Manchester LC, Reiter RJ, Qi W, Kim SJ, El-Sokkary GH. Melatonin protects hippocampal neurons in vivo against kainic acid-induced damage in mice. J Neurosci Res. 1998;54:382–389. doi: 10.1002/(SICI)1097-4547(19981101)54:3<382::AID-JNR9>3.0.CO;2-Y. [DOI] [PubMed] [Google Scholar]
- 104.Rong Y, Doctrow SR, Tocco G, Baudry M. EUK-134, a synthetic superoxide dismutase and catalase mimetic, prevents oxidative stress and attenuates kainate-induced neuropathology. Proc Natl Acad Sci USA. 1999;96:9897–9902. doi: 10.1073/pnas.96.17.9897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Gupta RC, Milatovic D, Zivin M, Dettbarn WD. Seizure-induced changes in energy metabolites and effects of N-tert-butyl-alpha-phenylnitrone (PNB) and vitamin E in rats. Pflugers Arch. 2000;440:R160–R162. [PubMed] [Google Scholar]
- 106.Bruce AJ, Baudry M. Oxygen free radicals in rat limbic structures after kainate-induced seizures. Free Radic Biol Med. 1995;18:993–1002. doi: 10.1016/0891-5849(94)00218-9. [DOI] [PubMed] [Google Scholar]
- 107.Lan J, Henshall DC, Simon RP, Chen J. Formation of the base modification 8-hydroxyl-2’-deoxyguanosine and DNA fragmentation following seizures induced by systemic kainic acid in the rat. J Neurochem. 2000;74:302–309. doi: 10.1046/j.1471-4159.2000.0740302.x. [DOI] [PubMed] [Google Scholar]
- 108.Roberts LJ, Morrow JD. Measurement of F(2)-isoprostanes as an index of oxidative stress in vivo. Free Radic Biol Med. 2000;28:505–513. doi: 10.1016/s0891-5849(99)00264-6. [DOI] [PubMed] [Google Scholar]
- 109.Lusis AJ. Atherosclerosis. Nature. 2000;407:233–241. doi: 10.1038/35025203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Martinet W, Knaapen MW, De Meyer GR, Herman AG, Kockx MM. Oxidative DNA damage and repair in experimental atherosclerosis are reversed by dietary lipid lowering. Circ Res. 2001;88:733–739. doi: 10.1161/hh0701.088684. [DOI] [PubMed] [Google Scholar]
- 111.Martinet W, Knaapen MW, De Meyer GR, Herman AG, Kockx MM. Elevated levels of oxidative DNA damage and DNA repair enzymes in human atherosclerotic plaques. Circulation. 2002;106:927–932. doi: 10.1161/01.cir.0000026393.47805.21. [DOI] [PubMed] [Google Scholar]
- 112.Martinet W, de Meyer GR, Herman AG, Kockx MM. Reactive oxygen species induce RNA damage in human atherosclerosis. Eur J Clin Invest. 2004;34:323–327. doi: 10.1111/j.1365-2362.2004.01343.x. [DOI] [PubMed] [Google Scholar]
- 113.Martinet W, De Meyer GR, Herman AG, Kockx MM. Amino acid deprivation induces both apoptosis and autophagy in murine C2C12 muscle cells. Biotechnol Lett. 2005;27:1157–1163. doi: 10.1007/s10529-005-0007-y. [DOI] [PubMed] [Google Scholar]
- 114.Petersen RB, Siedlak SL, Lee HG, Kim YS, Nunomura A, Tagliavini F, Ghetti B, Cras P, Moreira PI, Castellani RJ, Guentchev M, Budka H, Ironside JW, Gambetti P, Smith MA, Perry G. Redox metals and oxidative abnormalities in human prion diseases. Acta Neuropathol (Berl) 2005;110:232–238. doi: 10.1007/s00401-005-1034-4. [DOI] [PubMed] [Google Scholar]
- 115.Broedbaek K, Poulsen HE, Weimann A, Kom GD, Schwedhelm E, Nielsen P, Boger RH. Urinary excretion of biomarkers of oxidatively damaged DNA and RNA in hereditary hemochromatosis. Free Radic Biol Med. 2009;47:1230–1233. doi: 10.1016/j.freeradbiomed.2009.08.004. [DOI] [PubMed] [Google Scholar]
- 116.Hofer T, Marzetti E, Xu J, Seo AY, Gulec S, Knutson MD, Leeuwenburgh C, Dupont-Versteegden EE. Increased iron content and RNA oxidative damage in skeletal muscle with aging and disuse atrophy. Exp Gerontol. 2008;43:563–570. doi: 10.1016/j.exger.2008.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Tateyama M, Takeda A, Onodera Y, Matsuzaki M, Hasegawa T, Nunomura A, Hirai K, Perry G, Smith MA, Itoyama Y. Oxidative stress and predominant Abeta42(43) deposition in myopathies with rimmed vacuoles. Acta Neuropathol. 2003;105:581–585. doi: 10.1007/s00401-003-0685-2. [DOI] [PubMed] [Google Scholar]
- 118.Deslee G, Woods JC, Moore C, Conradi SH, Gierada DS, Atkinson JJ, Battaile JT, Liu L, Patterson GA, Adair-Kirk TL, Holtzman MJ, Pierce RA. Oxidative damage to nucleic acids in severe emphysema. Chest. 2009;135(4):965–974. doi: 10.1378/chest.08-2257. [DOI] [PMC free article] [PubMed] [Google Scholar]