Abstract
Objective
To examine weight changes in obese patients with binge eating disorder (BED) during the year prior to seeking treatment and to explore correlates of weight changes.
Method
Seventy-eight consecutive, treatment-seeking, obese BED patients were assessed with structured interviews and self-report questionnaires.
Results
Overall, participants reported a mean weight gain of 15.1 pounds during the 12 months prior to treatment. This overall weight gain comprised remarkable heterogeneity, ranging from a 30-pound loss to a 53-pound gain. The subgroup of participants who reported gaining weight (76% of sample) reported gaining an average of 22.2 pounds during the 12 months prior to treatment. Weight change was associated with significantly more frequent binge eating and overeating during breakfasts.
Discussion
Treatment-seeking obese patients with BED reported having gained substantial amounts of weight during the previous year. These findings provide an important context for interpreting the modest weight losses typically reported by treatment studies of BED.
Binge Eating Disorder (BED) is characterized by recurrent binge eating (i.e., the consumption of an unusually large amount of food in a discrete period of time while experiencing a subjective sense of loss of control) in the absence of compensatory behaviors. Binge eating disorder currently affects approximately 3.5% of adult women and is strongly associated with obesity and increased morbidity.1 Although some treatments have efficacy for reducing binge eating, most are largely ineffective in producing significant weight losses.2,3 There is a clear need for understanding why weight losses tend to be so limited in light of substantial reductions or even remission of binge eating in treatment studies. One clinical hypothesis is that treatments for BED may stabilize or prevent further weight gain.4 On average, American adults gain approximately two pounds per year. In a sample of 48 women with BED, Fairburn and colleagues5 found an average weight gain of 9.2 lbs (SD=21.6) with an increase in obesity rates from 22% to 39% over the course of 5 years. However, this sample was much younger and thinner than patients with BED in most treatment studies.2 The present investigation aimed to examine weight changes in obese patients with BED during the year prior to seeking treatment and to explore correlates of weight changes with a focus on historical obesity/dieting variables and recent disordered eating behaviors.
Method
Participants
Participants were 78 consecutively evaluated, treatment-seeking obese individuals who met full research diagnostic criteria for BED. Participants were recruited via newspaper advertisements seeking obese men and women who eat “out of control” and “want to lose weight” for treatment studies at a medical school-based specialty clinic. Participants were aged 29 to 64 years (M = 47.3, SD = 8.0), 69.2% (n = 54) were female, 79.5% (n = 62) were Caucasian, 15.4% (n = 12) were Black/African-American, 3.8% (n = 3) were Hispanic, and 1.3% (n = 1) self-described as “Other.” Mean BMI was 40.1 (SD = 6.5) and ranged from 29.5 to 54.7. Educationally, 85.7% (n = 66) reported at least some college.
Assessment and Measures
The study received full review and approval by the Yale Human Investigation Committee and all participants provided informed-written consents. Assessment procedures were performed by trained doctoral-level research-clinicians. BED diagnosis was based on the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I/P)6 and confirmed with the Eating Disorder Examination interview (EDE).7 Participants also completed the self-report questionnaires described below. Participants' height and weight were measured at the initial assessment appointment using a medical balance beam scale.
Eating Disorder Examination (EDE).7
The EDE is a well-established investigator-based interview method for assessing eating disorder psychopathology8,9 with established reliability.10 Except for diagnostic items which are rated according to the appropriate duration stipulations, the EDE focuses on the previous 28 days. The EDE assesses the frequency of different forms of overeating, including objective bulimic episodes (OBEs; i.e., binge eating defined as unusually large quantities of food with a subjective sense of loss of control), objective overeating episodes (OOEs; i.e., unusually large quantities of food without a subjective sense of loss of control) and subjective bulimic episodes (SBEs; i.e., subjective sense of loss of control but a normal or small amount of food). The EDE also assesses participants' meal patterning by asking how many times in the past 28 days they have eaten specific meals and snacks. In addition, we expanded the EDE interview to assess participants' perception of overeating at meals and snacks by asking them to rate, in their opinion, how many of the meals or snacks comprised too much food or too many calories. This assessment was added in light of our clinical observations that overeating may occur but not be reported as OOEs (described above) because of the EDE interview threshold requiring “unusually large” quantities.
Weight and Eating History Interview (WEH)
The WEH is a structured clinical interview, developed for this current study, which assesses current and historical obesity-related variables of interest. Dieting frequency was assessed with the following question: “Approximately how many diets, which have lasted at least three consecutive days, have you been on, whether or not you have succeeded?” Age of binge eating onset was assessed with the following question: “At what age do you remember first binge eating on a regular basis—at least one time per week?” Participants were asked to report their weight at three time points: 12 months ago, 6 months ago, and 3 months ago.
Questionnaire for Eating and Weight Patterns-Revised (QEWP-R).11
The QEWP is a self-report measure that assessed participants' current height and weight, age at which first overweight, weight cycling (number of times lost and regained 20+ pounds), and highest weight.
Statistical Analyses
To examine participants' pre-treatment weight gain trajectories, Weight Change was calculated by subtracting participants' weight 12 months ago from their current weight: [current weight - weight 12 months ago]. Weight Change frequencies were examined and participants were categorized into two groups: Weight Gainers and Weight Non-Gainers. Weight Gainers (75.6% of sample; n = 59) were those who gained 5 or more pounds in the past 12 months. Weight Non-Gainers (24.4% of sample; n = 19) were those who lost weight or stayed the same weight (gained no more than 4 pounds) in the past 12 months. Pearson's bivariate correlations, with Kendall's tau-b correction for nonparametric variables, assessed associations between Weight Change and historical obesity/dieting variables and recent disordered eating behaviors. Since the study group consisted of men and women, a parallel series of analyses were performed using BMI.
Results
Accuracy of Self-Report Weight
Participants' self-reported and actual measured current weight at baseline assessment were highly and significantly correlated (r = 0.98, p ≤ 0.0001). A paired-samples t-test revealed that the mean difference between self-reported and actual measured weight was significant (t (77) = -2.30, p = 0.02). The mean weight discrepancy (measured weight minus self-reported weight), however, was modest (3.0 pounds, SD = 7.6); on average, participants reported a lower current weight (M = 243.7, SD = 47.3) than their actual measured weight (M = 246.5, SD = 48.9). These findings suggest that this participant group was quite accurate in their self-reporting of weight. Moreover, participants' weight discrepancy scores were not significantly correlated with their self-reported weight changes (Kendall's tau-b = -0.08, p = 0.34).
Participants' self-reported and measured BMI at baseline assessment were significantly correlated (r = 0.96, p ≤ 0.0001). A paired-samples t-test revealed that the mean difference between self-reported and measured BMI was significant (t (77) = 2.34, p = 0.02). The mean BMI discrepancy (measured BMI minus self-reported BMI), however, was modest (0.46, SD = 1.73). On average, participants reported a lower current BMI (M = 39.7, SD = 6.3) than their measured BMI (M = 40.1, SD = 6.5). These findings suggest that this participant group was quite accurate in their self-reporting. Moreover, participants' BMI discrepancy scores were not significantly correlated with their self-reported BMI changes (Kendall's tau-b = -0.06, p = 0.45).
Weight Trajectories during the Year Prior to Seeking Treatment
Figure 1 summarizes the distribution of different amounts of weight changes (i.e., gains and losses) reported by participants during the 12 months prior to seeking treatment. Weight changes ranged from a 30 pound weight loss to a 53.4 pound weight gain. On average, participants reported a 15.1 pound (SD = 17.4) weight gain. BMI changes ranged from a 4.57 loss to a 9.85 gain. On average, participants reported a 2.51 (SD = 2.89) BMI gain. Seventy-six percent (n = 59) of the 78 participants were Weight Gainers and 24% (n = 19) were Weight Non-Gainers.
Figure 1.
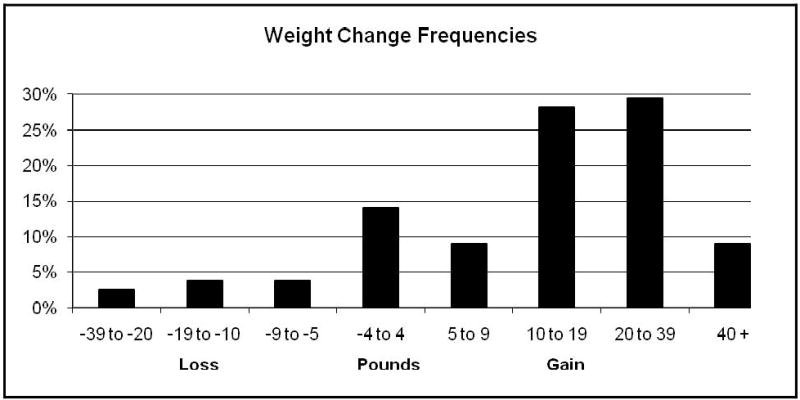
Categorization of participants based on weight trajectories (in pounds) during the year prior to initiating treatment.
Figure 2 presents the mean self-reported weight for the overall sample (N = 78), Weight Gainers (n = 59), and Weight Non-Gainers (n = 19) at 12 months, 6 months, and 3 months prior to seeking treatment as well as at their baseline evaluation prior to initiating treatment. Overall, participants gained weight during the year prior to treatment. On average, participants weighed an average of 228.6 pounds (SD = 52.3; BMI M = 37.2, SD = 7.1) at 12 months prior, 234.4 pounds (SD = 49.2; BMI M = 38.1, SD = 6.5) at 6 months prior, 238.4 pounds (SD = 48.1; BMI M = 38.8, SD = 6.3) at 3 months prior, and 243.7 pounds (SD = 47.3; BMI M = 39.7, SD = 6.3) at intake. However, these averages comprised remarkable heterogeneity which is described below.
Figure 2.
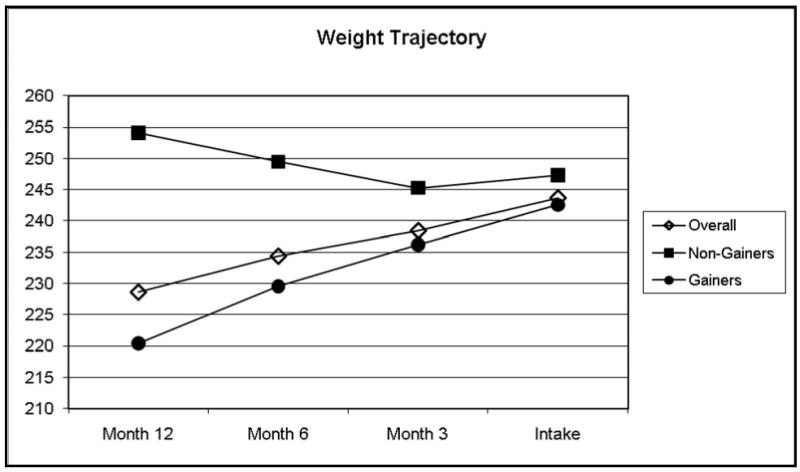
Participants' weight change trajectories during the year prior to initiating treatment are shown for the overall sample (N = 78) and separately for Weight Non-Gainers (n = 19) and Weight-Gainers (n = 59).
Weight Gainers gained an average of 22.2 pounds (SD = 12.7; BMI M = 3.7, SD = 2.2) in the year prior to seeking treatment. On average, Weight Gainers weighed 220.4 pounds (SD = 46.2; BMI M = 35.9, SD = 6.6) at 12 months prior, 229.5 pounds (SD = 46.0; BMI M = 37.4, SD = 6.6) at 6 months prior, 236.2 pounds (SD = 45.2; BMI M = 38.5, SD = 6.4) at 3 months prior, and 242.6 pounds (SD = 44.0; BMI M = 39.6, SD = 6.2) at intake. Weight Non-Gainers lost an average of 6.8 pounds (SD = 10.2; BMI M = 1.1, SD = 1.5) in the year prior to seeking treatment. On average, Weight Non-Gainers weighed 254.1 pounds (SD = 62.4; BMI M = 41.0, SD = 7.4) at 12 months prior, 249.5 pounds (SD = 57.0; BMI M = 40.2, SD = 6.1) at 6 months prior, 245.3 pounds (SD = 57.2; BMI M = 39.5, SD = 6.3) at 3 months prior, and 247.3 pounds (SD = 57.5; BMI M = 39.9, SD = 6.7) at intake. Although Weight Non-Gainers lost weight from 12 months prior to 3 months prior, they gained an average of 2.0 pounds (SD = 9.5; BMI M = 0.4, SD = 1.6) in the 3 months immediately preceding seeking treatment.
Historical and Recent Disordered Eating (EDE) Variables
Weight Change was not significantly correlated with current BMI or with historical obesity-related variables including highest weight, age at which first overweight, age at binge-eating onset, weight cycling, and number of times on a diet. In contrast, Weight Change was significantly positively correlated with the average number of OBE days in the past 6 months (r = 0.23, p = 0.05). Weight Change was not, however, significantly correlated with frequency of OBEs during the prior three months, nor with the frequency of OOEs or SBEs during the prior three months. In terms of meal and eating patterns, Weight Change was significantly positively correlated with overeating at breakfast meals (r = 0.28, p = 0.01). Similarly, BMI Change was not significantly correlated with historical obesity-related variables. However, BMI Change was significantly and positively correlated with the average number of OBE days in the past 6 months (r = 0.20, p = 0.02), overeating at breakfast meals (r = 0.27, p = 0.02), and overeating at double meals (Kendall's tau-b = 0.16, p = 0.05).
Discussion
This is the first study, to our knowledge, to examine recent weight trajectories in obese men and women with BED seeking treatment at medical-school-based specialty clinic. Our study revealed several important findings. First, overall, participants reported gaining on average 15.1 pounds during the 12 months prior to seeking treatment. Second, this overall average weight gain comprised remarkable heterogeneity in patterns of weight changes. The majority of participants (76%) could be categorized as Weight Gainers, and those who gained weight appeared to be on a steep weight gain trajectory (i.e., an average of 22.2 pounds during the 12 months prior to seeking treatment). Third, despite the absence of significant associations between weight change and historical obesity/dieting variables, greater weight gain during the year prior to seeking treatment was significantly associated with higher frequency of binge eating during the previous six months and with overeating at breakfast and double meals.
Our research findings should be interpreted in light of the study's strengths and limitations. Strengths include a thorough assessment of BED with the administration of structured interviews by specialist doctoral-level research-clinicians as well as the consecutive assessment of men and women who were seeking treatment specifically for binge eating and weight concerns. In terms of limitations, we note our relatively small sample size and limited power; however, there was significant range in the variables of interest, which reduces the likelihood that small sample sizes obscured otherwise significant relationships. It is possible that the use of the phrase “want to lose weight” in the recruitment ads may have increased the likelihood of obtaining participants who had recently gained weight. Thus, it is possible that we obtained a higher proportion of participants who were gaining weight than if different ads had been used. These ads, however, are similar to those used in other treatment studies12 as well as studies of treatment preferences and goals13 of obese persons with BED. Nonetheless, it is unknown whether recent weight gain (versus binge eating) is what motivated participants to seek treatment at this specific time. Since we did not include a comparison group of treatment-seeking obese patients who do not binge eat, it is not possible to directly compare weight trajectories of different obese groups prior to starting treatments.
This investigation also relied on self-report data for weight trajectories in the 12 months prior to seeking treatment. Such self-reports may be inaccurate. However, we emphasize that, in this study, there was a high degree of accuracy between participants' self-reported and measured weights at the time of evaluation and that previous research with this specific patient group found that these patients tend to be accurate reporters of their weight.14 Nonetheless, prospective studies would be necessary to determine the accuracy of these retrospective self-reported weights. Furthermore, since the data were collected retrospectively and interviewers did not calculate the total calories consumed at meals, such as breakfast, it is not entirely clear that participants' reports of “overeating” at breakfast accurately reflects excessive calories consumed. It is possible that participants could perceive “overeating” at breakfast to mean any eating at breakfast, given that a majority of participants with BED report frequently skipping breakfast15 perhaps to prevent weight gain.
With these strengths and weaknesses in mind, we offer several conclusions. The reported overall mean weight gain for this sample (15.1 pounds) and the mean weight gain reported by those on a pre-treatment weight gain trajectory (22.2 pounds) during the year prior to seeking treatment provide a potential new context for interpreting both treatment-seeking and weight-loss outcomes reported in treatment studies for BED. Our findings suggest the possibility of two different pathways that lead to seeking treatment in this patient group. Although Weight Gainers and Weight Non-Gainers had very similar weights at intake, these two subgroups arrived at this point with different weight trajectories during the past year. Weight Non-Gainers appeared to be close to their highest lifetime weight before seeking treatment whereas a majority of Weight Gainers were currently at their highest lifetime weight when they sought treatment. This sample's pre-treatment weight gain trajectory in conjunction with previous research demonstrating a small amount of weight loss with successful binge remission16,17 suggests that BED treatments achieving binge remission may be important by reducing future weight gains.4 Future research should continue to explore the predictive significance of pre-treatment weight gain trajectory on weight loss treatment outcomes. Our findings suggest the potential importance of prevention and early treatment interventions for BED to prevent excess weight gain.
Acknowledgments
This research was supported by grants from the National Institutes of Health (R01 DK49587, K24 DK070052, and K23 DK071646).
References
- 1.Hudson JI, Hiripi E, Pope HG, Kessler RC. The prevalence and correlates of eating disorders in the NCS Replication. Biol Psychiatry. 2007;61:348–358. doi: 10.1016/j.biopsych.2006.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Reas DL, Grilo CM. Review and meta-analysis of pharmacotherapy for binge-eating disorder. Obesity. 2008;16:2024–2038. doi: 10.1038/oby.2008.333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wilson GT, Grilo CM, Vitousek KM. Psychological treatment of eating disorders. Am Psychol. 2007;62:199–216. doi: 10.1037/0003-066X.62.3.199. [DOI] [PubMed] [Google Scholar]
- 4.Yanovski SZ. Binge eating disorder and obesity in 2003: Could treating an eating disorder have a positive effect on the obesity epidemic? Int J Eat Disord. 2003;34S:117–120. doi: 10.1002/eat.10211. [DOI] [PubMed] [Google Scholar]
- 5.Fairburn CG, Cooper Z, Doll HA, Norman P, O'Connor M. The natural course of bulimia nervosa and binge eating disorder in young women. Arch Gen Psychiatry. 2000;57:659–665. doi: 10.1001/archpsyc.57.7.659. [DOI] [PubMed] [Google Scholar]
- 6.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical interview for DSM-IV Axis I disorders - Patient Edition (SCID-I/P, Version 2.0) New York State Psychiatric Institute, Biometrics Research Department; New York: 1996. [Google Scholar]
- 7.Fairburn CG, Cooper Z. The eating disorders examination. In: Fairburn CG, Wilson GT, editors. Binge eating: nature, assessment, and treatment. 12th. New York: The Guilford Press; 1993. pp. 317–331. [Google Scholar]
- 8.Grilo CM, Masheb RM, Wilson GT. A comparison of different methods for assessing the features of eating disorders in patients with binge eating disorder. J Consult Clin Psychol. 2001;69:317–322. doi: 10.1037//0022-006x.69.2.317. [DOI] [PubMed] [Google Scholar]
- 9.Grilo CM, Masheb RM, Wilson GT. Different methods for assessing the features of eating disorders in patients with binge eating disorder: A replication. Obes Res. 2001;9:418–422. doi: 10.1038/oby.2001.55. [DOI] [PubMed] [Google Scholar]
- 10.Grilo CM, Masheb RM, Lozano-Blanco C, Barry DT. Reliability of the Eating Disorder Examination in patients with binge eating disorder. Int J Eating Disord. 2004;35:80–85. doi: 10.1002/eat.10238. [DOI] [PubMed] [Google Scholar]
- 11.Spitzer RL, Yanovski SZ, Marcus MD. The questionnaire on eating and weight patterns-revised (QEWP-R) New York: New York State Psychiatric Institute; 1993. [Google Scholar]
- 12.Grilo CM, Masheb RM. A randomized controlled comparison of guided self-help cognitive behavioral therapy and behavioral weight loss for binge eating disorder. Beh Res Therapy. 2005;43:1509–1525. doi: 10.1016/j.brat.2004.11.010. [DOI] [PubMed] [Google Scholar]
- 13.Brody ML, Masheb RM, Grilo CM. Treatment preferences of patients with binge eating disorder. Int J Eating Disord. 2005;37:352–356. doi: 10.1002/eat.20137. [DOI] [PubMed] [Google Scholar]
- 14.White MA, Masheb RM, Grilo CM. Accuracy of self-reported weight and height in binge eating disorder: misreport is not related to psychological factors. Int J Eating Disord. doi: 10.1038/oby.2009.347. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Masheb RM, Grilo CM. Eating patterns and breakfast consumption in obese patients with binge eating disorder. Beh Res Therapy. 2006;44:1545–1553. doi: 10.1016/j.brat.2005.10.013. [DOI] [PubMed] [Google Scholar]
- 16.Grilo CM, Masheb RM, Wilson GT. Efficacy of cognitive behavioral therapy and fluoxetine for the treatment of binge eating disorder: A randomized double-blind placebo-controlled comparison. Biol Psychiatry. 2005;57:301–309. doi: 10.1016/j.biopsych.2004.11.002. [DOI] [PubMed] [Google Scholar]
- 17.Wilfley DE, Welch RR, Stein RI, Spurrell EB, Cohen LR, Saelens BE, et al. A randomized comparison of group cognitive-behavioral therapy and group interpersonal psychotherapy for the treatment of overweight individuals with binge-eating disorder. Arch Gen Psychiatry. 2002;59:713–721. doi: 10.1001/archpsyc.59.8.713. [DOI] [PubMed] [Google Scholar]


