Abstract
Objectives
Late survival is similar after EVAR and open AAA repair despite a perioperative benefit with EVAR. AAA-related reinterventions are more common after EVAR while laparotomy related reinterventions are more common after open repair. The impact of reinterventions on survival, however, is unknown. We therefore evaluate the rate of reinterventions and readmission after initial AAA repair along with 30-day mortality and the effect upon long term survival.
Methods
We identified AAA and laparotomy-related reinterventions for propensity score matched cohorts of Medicare beneficiaries (n=45,652) undergoing EVAR and open repair from 2001-2004. Follow-up was up to 6 years. Hospitalizations for ruptured AAA without repair and for bowel obstruction or ventral hernia without abdominal surgery were also recorded. Event rates were calculated per year and are also presented through 6 years of follow-up as events per 100 person years. Thirty day mortality was calculated for each reintervention or readmission.
Results
Through 6 years, overall reinterventions or readmissions were similar between repair methods but slightly more common after EVAR (7.6 vs. 7.0 per 100 person years, RR 1.1, P < .001). Overall 30 day mortality with any reintervention or readmission was 9.1%. EVAR patients had more ruptures (0.50 vs. 0.09, RR 5.7, P < .001) with a mortality of 28%, but these were uncommon. EVAR patients also had more AAA-related reinterventions through 6 years (3.7 vs. 0.9, RR 4.0, P < .001) (mortality 5.6%), the majority of which were minor endovascular reinterventions (2.4 vs. 0.2, RR 11.4, P < .001) with a 30 day mortality of 3.0%. However, minor open (0.8 vs. 0.5, RR 1.4, P < .001) (mortality 6.9%) and major reinterventions (0.4 vs. 0.2, RR 2.4, P < .001) (mortality 12.1%) were also more common after EVAR than open repair. Conversely, EVAR patients had fewer laparotomy related reinterventions than open patients (1.4 vs. 3.0, RR 0.5, P < .001) (mortality 8.1%) and readmissions without surgery (2.0 vs. 2.7, RR 0.7, P < .001) (mortality 10.9%). Overall, reinterventions or readmission accounted for 9.6% of all EVAR deaths and 7.6% of all open repair deaths in the follow-up period (P < .001).
Conclusions
Reintervention and readmission are slightly higher after EVAR. Survival is negatively impacted by reintervention or readmission after both EVAR and open surgery, which likely contributes to the erosion of the survival benefit of EVAR over time.
Introduction
Randomized trials and population-based studies have shown similar late survival after endovascular abdominal aortic aneurysm repair (EVAR) and open aneurysm repair despite an early perioperative benefit with EVAR.1-5 Survival equilibrated by 18 months in randomized control trials and at approximately 3 years in Medicare beneficiaries.1-3 Many theories have been proposed to explain the loss of survival benefit after EVAR.6 Chance alone is unlikely given the consistent replication of these findings as well as the large size of the Medicare database. The “survival of the fittest” theory holds that some of those who survive EVAR might not have survived open surgery. These patients tend to be older and more frail and thus more likely to die during the follow-up period.3, 6 A competing theory holds that rupture and reintervention are higher after EVAR and that these events will lead to increased late mortality after EVAR relative to open repair. We previously found, however, that the increase in AAA-related reintervention after EVAR is offset by an increase in laparotomy-related complications after open repair such as bowel obstruction and abdominal wall hernia, and these complications also may have implications for late survival.1
To further explore this issue we evaluated the rate of rupture, reintervention, and readmission for AAA-related and laparotomy-related complications after elective EVAR and open AAA repair in a previously defined cohort of propensity score matched Medicare beneficiaries. We calculated the 30-day mortality associated with each type of event and plotted postoperative survival after EVAR and open repair with and without reintervention or readmission.
Methods
All traditional Medicare beneficiaries undergoing elective AAA repair from 2001 to 2004 were identified from Medicare administrative files. This primary dataset has been used in prior analyses.1 Patient demographic characteristics were identified from the Medicare denominator file. Comorbidities were identified from inpatient and outpatient claims up to 2 years prior to but not including the admission for repair. Reinterventions and readmissions were determined from inpatient and outpatient claims and mortality was determined from the Medicare denominator file.
To control for the non-random assignment of patients to open repair versus EVAR, we created matched cohorts of patients using a logistic regression model from demographics and preexisting comorbidities predicting the likelihood of endovascular repair (propensity score). Our propensity score methods are described in detail in a prior publication.1 For the current analysis, follow-up records were analyzed through 2007. Patient follow-up for reinterventions and readmissions ranged from a minimum of three years to a maximum of seven years based on the initial procedure year.
We identified all reinterventions and readmissions occurring in patients surviving beyond the perioperative period (90 days). These were identified using CPT (Current Procedural Terminology, American Medical Association) and ICD-9 (International Classification of Diseases, 9th Revision, Clinical Modification) coding. In addition, we used a hierarchical schema within a single hospitalization with major reinterventions superseding minor reinterventions. Admissions for ruptured AAA (with and without subsequent repair), AAA-related (major and minor), and laparotomy-related (major and minor) reinterventions and readmissions were recorded.
Major AAA-related reinterventions included conversion to open repair from EVAR, revision open repair, repair of an infected graft or a graft-enteric fistula, or an axillo-bifemoral or unifemoral bypass. Minor AAA-related reinterventions were divided into open and endovascular categories. Minor open reinterventions included iliac aneurysm repair, fem-fem bypass, femoral-popliteal aneurysm repair, thrombectomy, and embolectomy. Minor endovascular procedures included repeat EVAR, extension cuffs, iliac aneurysm repair, aortic or iliac angioplasty, and embolization procedures.
Major laparotomy-related reinterventions included small bowel resection, large bowel resection, and lysis of adhesions without bowel resection. Minor-laparotomy related reinterventions included ventral hernia repair. Hospitalizations for bowel obstruction or ventral hernia without a subsequent operation were also recorded. We defined age categories as 67-69 years, 70-74 years, 75-79 years, and ≥80 years. All readmissions with reinterventions for each patient were counted, not only first reinterventions, in order to determine the proportion of patients having 0, 1, 2, or 3 or more reinterventions during follow-up.
Statistical Analysis
We calculated the total number of reinterventions within each category as the total number per 100 patient years based on a lifetable analysis of patients surviving to each follow-up year. 30-day mortality rates for each category of reintervention as well as mortality within 30 days of admission with a diagnosis of AAA rupture without subsequent repair or a laparotomy-related readmission without reintervention were calculated. Additionally, Kaplan-Meier survival curves for long-term survival with and without subsequent reinterventions or readmissions were created for each repair method. Finally, the number of deaths secondary to a reintervention or readmission (occurring within 30 days of any reintervention or laparotomy-related readmission) as a proportion of total deaths during follow-up are reported.
Analyses were performed using SAS statistical software (Version 9.1, SAS Institute Inc., Cary, NC). Reinterventions and readmissions are reported as raw numbers and as events per 100 person years. Mortality rates are 30-day mortality from date of reintervention. Reinterventions and readmissions were compared with paired-sample T-tests. Kaplan-Meier survival was compared by chi-square analysis. Statistical significance was defined as P < .05.
Results
There were 61,598 patients who underwent elective AAA repair from 2001 to 2004. After propensity score matching we included 22,826 open repairs and 22,826 EVARs in our study sample.
Demographics for each repair method of patients with and without a reintervention or readmission during follow-up are presented in Table I. There were few significant clinical predictors of reintervention in either group. There was a statistical but not clinically significant age and gender difference. EVAR patients with a reintervention or readmission were less likely to have chronic renal disease but more likely to have CAD without a recent revascularization, peripheral vascular disease, and hypertension. Open repair patients with an eventual reintervention or readmission were more likely to have coronary artery disease (CAD), peripheral arterial disease, chronic obstructive pulmonary disease (COPD), or end stage renal disease.
Table I.
Baseline demographics and comorbid conditions of Medicare beneficiaries with and without reinterventions or readmissions after endovascular and open aortic aneurysm repair 2001-2004.
| Endovascular Repair | Open Repair | |||||
|---|---|---|---|---|---|---|
| Any Reintervention (15.3%) |
No Reintervention (84.7%) |
P value | Any Reintervention (14.4%) |
No Reintervention (85.6%) |
P value | |
| Male Gender | 79.0% | 80.5% | < .05 | 81.3% | 80.5% | .25 |
| Age, mean +/- SD | 76.6 +/- 5.3 | 76.2 +/- 5.4 | < .001 | 75.9 +/- 5.2 | 76.3 +/- 5.4 | < .001 |
| Comorbid Conditions | ||||||
| Prior Myocardial Infarction within 6 mo | 2.0% | 1.9% | .72 | 1.4% | 1.8% | .10 |
| Myocardial Infarction within 6-24 mo | 8.1% | 8.0% | .81 | 8.6% | 7.9% | .13 |
| Cardiovascular Disease with CABG within 24 mo | 4.6% | 4.4% | .74 | 7.5% | 6.6% | < .05 |
| Cardiovascular Disease with PTCA within 24 mo | 4.6% | 5.1% | .20 | 4.4% | 4.9% | .17 |
| Cardiovascular Disease without recent intervention | 22.1% | 19.6% | < .001 | 19.4% | 17.5% | < .01 |
| Valvular Heart Disease | 11.0% | 10.9% | .89 | 11.0% | 10.4% | .23 |
| Congestive Heart Failure | 14.0% | 13.2% | .16 | 13.2% | 13.1% | .86 |
| Peripheral Vascular Disease | 23.3% | 20.9% | < .01 | 23.7% | 20.3% | < .001 |
| Cerebrovascular Disease | 15.6% | 16.5% | .17 | 17.0% | 16.2% | .23 |
| Hypertension | 67.9% | 65.9% | < .05 | 66.2% | 65.7% | .59 |
| Diabetes Mellitus | 15.3% | 15.8% | .47 | 15.2% | 15.8% | .35 |
| Chronic Obstructive Pulmonary Disease | 30.0% | 29.7% | .68 | 33.4% | 29.1% | < .001 |
| Renal Disease | 3.1% | 4.1% | < .01 | 3.8% | 4.0% | .55 |
| End Stage Renal Disease | 0.8% | 0.8% | .91 | 0.8% | 0.5% | < .05 |
Reinterventions: EVAR versus open repair
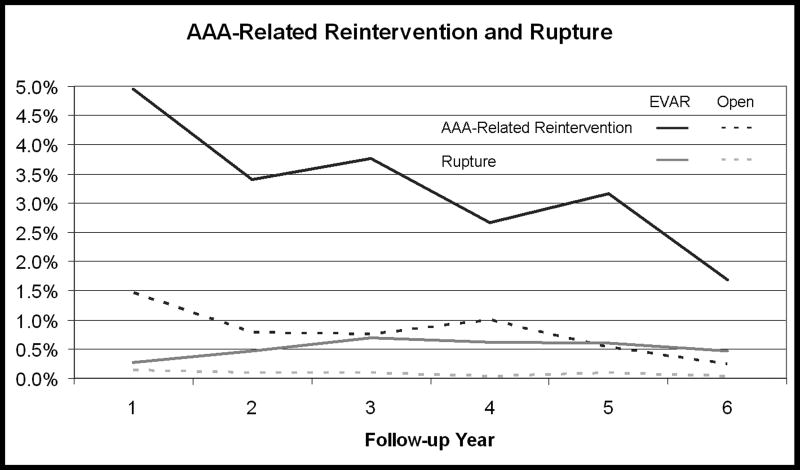
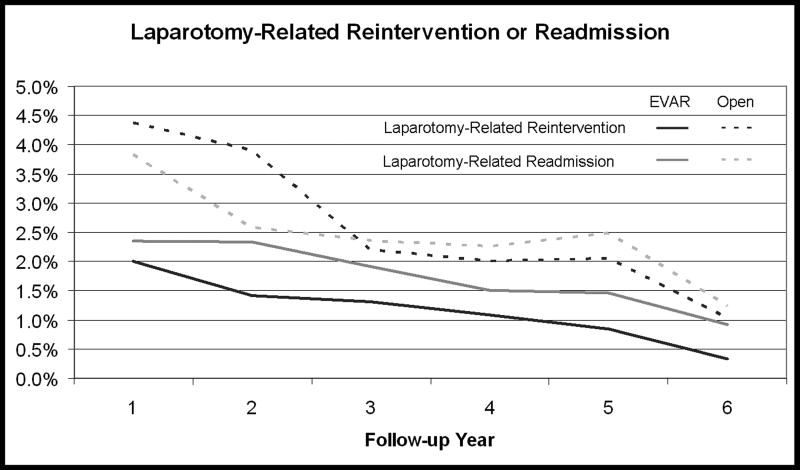
Reinterventions and readmissions were slightly more frequent after EVAR than open repair (7.56 vs. 6.96 per 100 person years, P < .001, Table II). Rupture (with or without subsequent repair) was five times more common after EVAR (0.50 vs. 0.09 events per 100 person years, P < .001), but with a relatively low rate overall. AAA-related reinterventions including rupture repair were over 3 times more common after EVAR (3.67 vs. 0.93, P < .001). Rupture repair was performed in 110 patients after EVAR as compared with just 6 after open repair (0.13 vs. 0.01 events per 100 person years, P < .001). Other major AAA-related reinterventions were also rare but were 2 times more common after EVAR (0.41 vs. 0.17 events per 100 person years, P < .001). Minor endovascular and open AAA-related reinterventions also were more common after EVAR (2.38 vs. 0.21, P < .001 and 0.75 vs. 0.54, P< .001 respectively). Laparotomy-related reinterventions were more than twice as likely after open repair (3.04 per 100 person years vs. 1.39) (Table II). Both major laparotomy-related reinterventions (1.51 vs. 1.10 events per 100 person years, P< .001) and minor laparotomy-related reinterventions (1.53 vs. 0.28 events per 100 person years, P< .001) were higher after open repair as were laparotomy-related hospitalizations for bowel obstruction or ileus without surgery (2.72 vs. 1.98, P < .001). AAA-related, laparotomy-related reinterventions or readmissions, and rupture after open repair were highest within the first year of follow-up and decreased over time. Ruptures after EVAR were greatest in the second year of follow-up only slightly declining in subsequent years (Figure 1A & 1B).
Table II.
Total number of reinterventions and readmissions and rate per 100 person years for Medicare beneficiaries undergoing initial open and endovascular AAA repair 2001-2004.
| Through 6 Years | ||||
|---|---|---|---|---|
| EVAR | Open | |||
| N | Rate | N | Rate | |
| All Reinterventions | 6,640 | 7.56 | 5,991 | 6.96 |
| Rupture | 441 | 0.50 | 76 | 0.09 |
| AAA-related Reintervention | 3,222 | 3.67 | 798 | 0.93 |
| Rupture Repair | 110 | 0.13 | 6 | 0.01 |
| Major Reintervention | 362 | 0.41 | 149 | 0.17 |
| Minor Reintervention | 2,750 | 3.13 | 643 | 0.75 |
| Minor Open | 655 | 0.75 | 463 | 0.54 |
| Minor Endovascular | 2,095 | 2.38 | 180 | 0.21 |
| Laparotomy-Related Reinterventions | 1,218 | 1.39 | 2,616 | 3.04 |
| Major | 968 | 1.10 | 1,300 | 1.51 |
| Minor | 250 | 0.28 | 1,316 | 1.53 |
| Hospitalization for Bowel Obstruction or Ileus without surgery | 1,736 | 1.98 | 2,340 | 2.72 |
Figure 1.
Reintervention and readmission rates through 6 years of follow-up for Medicare beneficiaries undergoing initial open and endovascular AAA repair. A) AAA-related reinterventions and AAA rupture. B) Laparotomy-related reinterventions and readmissions.
For patients originally undergoing EVAR, 84.7% of patients had no reinterventions or readmissions during the follow-up period compared to 85.6% of open repair patients (P< .01). Among patients with reinterventions or readmissions, 54% of EVAR patients vs. 57% of open repair patients had only a single reintervention or readmission (P = .21) while 26% vs. 25% had 2 (P = .34) and 20% vs. 18% had 3 or more (P = .18).
After stratifying by age, those < 70 years old were less likely to have a reintervention or readmission after EVAR compared to open repair (EVAR vs. Open RR 0.87, P < .05) (Table III). Patients 70-74 years old had a similar risk regardless of initial repair method (RR 0.99, P = .74), and those 75-79 and ≥80 years were more likely to have a reintervention or readmission if they initially underwent EVAR (RR 1.14 and 1.21, P < .001 and < .001). Rupture and rupture repair were more frequent after EVAR for all ages. AAA-related reinterventions were more common after EVAR and laparotomy-related reinterventions and readmissions were significantly more likely after open repair across all age groups.
Table III.
Rate per 100 person years and relative risk of reintervention or readmission after endovascular versus open AAA repair in Medicare beneficiaries. 30-day mortality after reintervention or readmission.
| Rate of Reintervention | Relative Risk | P-Value | 30-Day Mortality | ||
|---|---|---|---|---|---|
| EVAR | Open | EVAR vs Open | |||
| All Reinterventions | 7.56 | 6.96 | 1.09 | < .001 | 9.1% |
| Age 67-69 | 4.90 | 5.60 | 0.87 | < .05 | 6.3% |
| 70-74 | 6.86 | 6.93 | 0.99 | .74 | 7.9% |
| 75-79 | 6.90 | 6.03 | 1.14 | < .001 | 10.1% |
| ≥80 | 12.00 | 9.96 | 1.21 | < .001 | 13.6% |
| Rupture | 0.50 | 0.09 | 5.69 | < .001 | 27.7% |
| AAA-related Reintervention | 3.67 | 0.93 | 3.96 | < .001 | 6.2% |
| Rupture Repair | 0.13 | 0.01 | 17.97 | < .001 | 30.2% |
| Major Reintervention | 0.41 | 0.17 | 2.38 | < .001 | 13.7% |
| Minor Reintervention | 3.13 | 0.75 | 4.19 | < .001 | 4.2% |
| Minor Open | 0.75 | 0.54 | 1.39 | < .001 | 7.2% |
| Minor Endovascular | 2.38 | 0.21 | 11.41 | < .001 | 2.8% |
| Laparotomy-Related Reinterventions | 1.39 | 3.04 | 0.46 | < .001 | 8.5% |
| Major | 1.10 | 1.51 | 0.73 | < .001 | 12.2% |
| Minor | 0.28 | 1.53 | 0.19 | < .001 | 3.1% |
| Hospitalization for Bowel Obstruction or Ileus without surgery | 1.98 | 2.72 | 0.73 | < .001 | 10.9% |
It was more likely that patients requiring a reintervention or readmission were older (≥ 75 vx < 75 years) after both EVAR and open repair (EVAR RR 1.38, P < .001; Open RR 1.13, P < .001). Relative risks of all subsets of reintervention or readmission for patients ≥ 75 years compared to those < 75 years for both EVAR and open repair are presented in Table IV.
Table IV.
Relative risk of reintervention or readmission for patients ≥75 years versus those <75 years old after endovascular and open repair.
| Relative Risk ≥ 75 vs. < 75 | P-Value | |||
|---|---|---|---|---|
| EVAR | Open | EVAR | Open | |
| All Reinterventions | 1.38 | 1.13 | < .001 | < .001 |
| Rupture | 2.41 | 2.05 | < .001 | < .01 |
| AAA-related Reintervention | 1.53 | 0.75 | < .001 | < .001 |
| Rupture Repair | 3.06 | 1.67 | < .001 | .55 |
| Major Reintervention | 0.96 | 0.94 | .66 | .71 |
| Minor Reintervention | 1.59 | 0.71 | < .001 | < .001 |
| Minor Open | 1.10 | 0.66 | .21 | < .001 |
| Minor Endovascular | 1.79 | 0.87 | < .001 | .36 |
| Laparotomy-Related Reinterventions | 1.18 | 1.03 | < .01 | .38 |
| Major | 1.27 | 1.32 | < .001 | < .001 |
| Minor | 0.89 | 0.82 | .36 | < .001 |
| Hospitalization for Bowel Obstruction or Ileus without surgery | 1.24 | 1.41 | < .001 | < .001 |
30 Day Mortality after Reinterventions
Deaths within 30 days of reinterventions or readmissions accounted for 9.6% of all EVAR deaths and 7.6% of all open repair deaths in the follow-up period (P < .001). Thirty-day mortality for any reintervention or readmission was 9.1% (Table III). The highest 30 day mortality was for a diagnosis of rupture (27.7% 30-day mortality and rupture with repair had a 30.2% mortality). Other major AAA-related reinterventions had a 13.7% mortality whereas minor AAA-related reinterventions had a mortality of 4.2%. Minor open reinterventions had a mortality of 7.2% whereas minor endovascular reinterventions had a lower 30-day mortality of 2.8%. Laparotomy related reinterventions had a mortality of 8.5%. Split into major and minor categories the major laparotomy related reinterventions had mortality of 12.2% and the minor laparotomy related reinterventions had only a 3.1% mortality. Hospitalizations for bowel obstruction or ileus without reintervention had a mortality of 10.9%. Mortality increased with age for all reintervention/readmission categories with the exception of rupture and rupture repair where patients aged 71-75 had the lowest mortality.
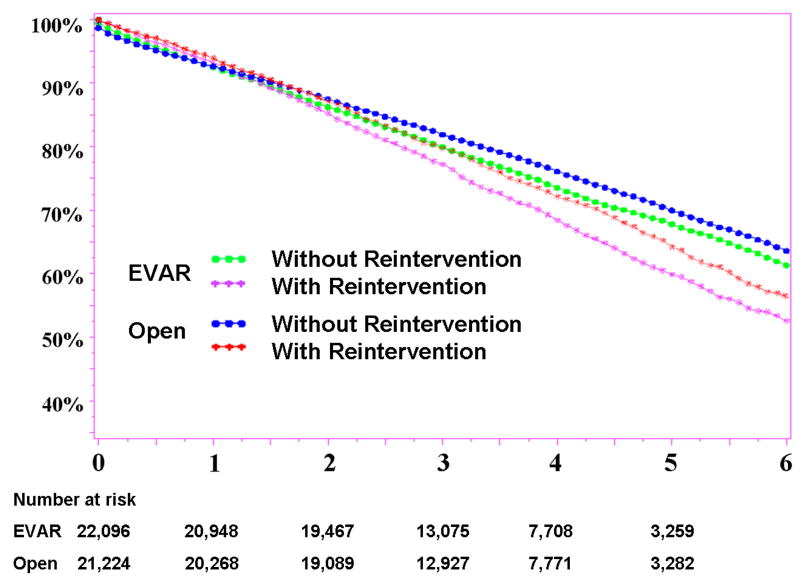
After exclusion of deaths within 90 days of the original AAA intervention, patients with a reintervention or readmission after originally receiving EVAR had a decreased survival compared to those without. Similarly, after open AAA repair, patients needing a reintervention or readmission had a lower long-term survival (Figure 2).
Figure 2.
Long-term survival in Medicare beneficiaries with and without reinterventions after initial open or endovascular repair. SE < 10% throughout.
Discussion
Although AAA-related reinterventions were more frequent after EVAR, the majority of these were minor endovascular reinterventions with relatively low 30-day mortality. Major AAA-related reinterventions and rupture, both with a high mortality, were uncommon for either repair method but comparatively more frequent after EVAR. In contrast to AAA-related reinterventions, laparotomy-related reinterventions and readmissions were more common with open repair and also had relatively high mortality. The overall cumulative and long-term effect of these reinterventions and the higher rate of subsequent rupture after EVAR likely contribute to, but don't fully explain the equalization of overall survival during the follow-up period after AAA repair, since 2% more deaths during follow-up were attributable to reinterventions / readmissions in the EVAR group compared to open repair. Given that the perioperative mortality predictors for all AAA repair include age, congestive heart failure, and renal failure, it is also true that these characteristics are more common in the EVAR cohort beyond the perioperative period and likely also contribute to a loss of survival benefit with EVAR.7
Two European randomized controlled trials included reinterventions in their follow-up outcomes analysis. However, the total numbers of patients treated were only 351 within the Dutch Randomized Endovascular Aneurysm Management (DREAM) trial and 1,082 within EVAR I and thus had insufficient numbers of reinterventions for comparison to our findings. The DREAM trial defined reinterventions as “any surgical or endovascular procedure performed after the primary aneurysm repair procedure and related to the aneurysm or the primary procedure, including incisional hernia repairs but exclusive of procedures involving superficial wound complications” and found that reinterventions by 9 months of follow-up were nearly 3-fold higher after EVAR than open repair but became similar thereafter. The rate of aneurysm related death still remained lower after EVAR up to 2 years.3 Similarly, the EVAR I trial found a reintervention rate of 6.9 per 100 person years in the EVAR group and 2.4 per 100 person years in the open repair group. These reinterventions after EVAR included those for type 1 (17) and type 2 endoleaks (17), “other surgery required” (13), graft thromboses (10), type 3 and unspecified endoleaks (8), graft migrations (7), graft rupture (3), and graft infection (1). Reinterventions after open repair were predominately “re-exploration of open repair” (16) and “other surgery required” (16).2 Recently, the Open Versus Endovascular Repair (OVER) Veterans Affairs Cooperative Study Group reported 2 year outcomes of 881 patients randomized to open or endovascular AAA repair. They reported reinterventions including any unplanned surgery within 30 days of AAA repair or any aorto-iliac procedures at any time during follow-up. They found no differences between the two treatment groups with 55 secondary procedures after open repair and 61 after EVAR. The most common secondary procedure after open repair (24 of 55) was incisional hernia repair while the most common procedure after EVAR (42 of 61) was an endovascular procedure.8
The overall rate of reinterventions we found after EVAR is similar to that shown in EVAR I. Our current study, however, includes a broader range of laparotomy related complications and thus is able to identify more procedure-related reinterventions and readmissions after open repair. Given the high mortality associated with major laparotomy-related complications, this is an important consideration. It should be noted however, that when patients were stratified by age, only patients ≥ 75 years had a higher rate of reintervention after EVAR whereas patients < 70 years actually had a higher rate of reintervention after open repair. We have previously shown that older patients had an increased perioperative survival advantage with EVAR compared to younger patients.1 A higher reintervention rate may be considered acceptable for the elderly with EVAR given high risks with open repair. As shown in Table IV, patients requiring a reintervention or readmission during followup were more likely older than 75 years indicating that older patients are also more likely to require multiple reinterventions or readmissions.
The greatest number of reinterventions after EVAR fell into the “minor endovascular AAA-related” category. As Brewster et al. showed, most reinterventions following EVAR are catheter-based interventions.9 These carry a lower mortality in this population with a 4% 30-day mortality compared to major AAA-related reinterventions with a mortality of 13.7%. Thus the overall effect on long-term outcome is not as substantial.
Rupture and rupture repair were more frequent after EVAR at 0.5 compared to 0.09 per 100 patient years. The EUROSTAR group in their early studies found an annual rate of rupture after EVAR of 1% with more occurring in their first year of follow-up (1.4%) than the second year (0.6%).10 Updated data from the EUROSTAR registry has shown a lower rate of rupture of 0.5% annually. Grafts subsequently removed from the market (and not available in the US) had the highest rates of rupture and reintervention.11,12 In the current study, the first year of follow-up was found to have the lowest rate of rupture (0.27) compared to later years (range 0.46-0.69). EVAR I had an overall rupture rate of 1.7% after EVAR and no ruptures after open repair with up to four years of followup.2 In the current dataset, given the trends of rupture rate during followup (Figure 1A), it is possible that with longer followup the differences between repair methods would be more substantial.
Laparotomy-related reinterventions and readmissions, with greater than 10% 30-day mortality, make up the majority of reinterventions and readmissions following open repair. Admissions for laparotomy related reinterventions after EVAR are unlikely to be related to the AAA repair and instead reflects the baseline rate in this elderly population. The relative increase in laparotomy-related reinterventions after open repair therefore represents the effect of laparotomy for AAA repair. This is probably underestimated as well as we did not adjust for prior laparotomy in our propensity score matching. This likely introduced bias against EVAR since prior laparotomy probably pushes repair selection toward EVAR.
Our analyses are subject to several limitations. The strengths of the 100% Medicare sample are its large size, longitudinal design, and broad representation of US patients. The limitations are those inherent to administrative data such as coding error and lack of clinical detail. An example of this is that the mortality with rupture repair is higher than that for rupture without repair implying that patients diagnosed with ruptured AAA during followup may not have true ruptures. We have attempted to minimize coding discrepancies by utilizing both hospital and physician claims as well as both inpatient and outpatient data, which provides verification and also allows for greater procedural detail and specificity of comorbid diagnoses. Patients with a diagnosis of peripheral arterial disease were more likely to have a reintervention or readmission but we also did not identify prior surgical procedures for lower extremity peripheral arterial disease, which may further predispose patients to some of the AAA-related reinterventions we used as outcomes. This likely would affect both repair groups equally however. Finally, we are unable to assess anatomic differences among patients and unfortunately cannot evaluate these criteria for risk of reintervention or readmission within this study. Larger aneurysm diameter has been shown to be a risk factor for reintervention as has severe neck angulation.13,14 Patients who are not candidates for open repair but have large aneurysms deemed to be at high risk for rupture may have been offered EVAR even with less than ideal anatomy with the acknowledgement that mortality and reintervention rates may be higher but still within an acceptable margin given the risk without surgery. Given the age related increase in reintervention rates, this seems likely.
Conclusion
Late survival is worse in those undergoing reintervention or readmission after both EVAR and open repair. Among initial AAA repair survivors, reintervention and readmission are slightly more common after EVAR than open and likely contributes somewhat to the loss of early survival advantage seen with EVAR. However, reinterventions do not fully account for the survival curves coming together after three years. AAA-related reinterventions are more common after EVAR, but typically are minor endovascular reinterventions while laparotomy-related reinterventions are more common after open repair. Future work should attempt to identify predictors of reintervention or readmission in order to factor this into clinical decision algorithms.
Acknowledgments
This work was supported by the NIH T32 Harvard-Longwood Research Training in Vascular Surgery grant HL007734.
Footnotes
The opinions expressed do not necessarily represent the views or policy positions of the Centers for Medicare and Medicaid Services.
Author Disclosures: KA Giles, None; BE Landon, Gore unrestricted educational grant; AJ O'Malley, None; P Cotterill, None; FB Pomposelli, None; ML Schermerhorn, Gore unrestricted educational grant, Endologix DSMB, Medtronic consultant.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Schermerhorn ML, O'Malley AJ, Jhaveri A, Cotterill P, Pomposelli F, Landon BE. Endovascular vs. Open Repair of Abdominal Aortic Aneurysms in the Medicare Population. N Engl J Med. 2008;358:464–74. doi: 10.1056/NEJMoa0707348. [DOI] [PubMed] [Google Scholar]
- 2.EVAR Trial Participants. Endovascular aneurysm repair versus open repair in patients with abdominal aortic aneurysm (EVAR trial 1): randomised controlled trial. The Lancet. 365:2179–86. doi: 10.1016/S0140-6736(05)66627-5. [DOI] [PubMed] [Google Scholar]
- 3.Blankensteijn JD, de Jong SECA, Prinssen M, van der Ham AC, Buth J, van Sterkenburg SM, et al. Two-Year Outcomes after Conventional or Endovascular Repair of Abdominal Aortic Aneurysms. N Engl J Med. 2005;352:2398–405. doi: 10.1056/NEJMoa051255. [DOI] [PubMed] [Google Scholar]
- 4.Greenhalgh RM, Brown LC, Kwong GP, Powell JT, Thompson SG, EVAR trial participants Comparison of endovascular aneurysm repair with open repair in patients with abdominal aortic aneurysm (EVAR trial 1), 30-day operative mortality results: randomised controlled trial. Lancet. 364:843–8. doi: 10.1016/S0140-6736(04)16979-1. [DOI] [PubMed] [Google Scholar]
- 5.Prinssen M, Verhoeven ELG, Buth J, Cuypers PW, van Sambeek MR, Balm R, et al. A randomized trial comparing conventional and endovascular repair of abdominal aortic aneurysms. N Engl J Med. 2004;351:1607–18. doi: 10.1056/NEJMoa042002. [DOI] [PubMed] [Google Scholar]
- 6.Lederle FA. Endovascular repair of abdominal aortic aneurysm -- round two. N Engl J Med. 2005;352:2443–5. doi: 10.1056/NEJMe058126. [DOI] [PubMed] [Google Scholar]
- 7.Giles KA, Schermerhorn ML, O'Malley AJ, Cotterill P, Jhaveri A, Pomposelli FB, et al. Risk prediction for perioperative mortality of endovascular vs open repair of abdominal aortic aneurysms using the Medicare population. J Vasc Surg. 2009;50:256–62. doi: 10.1016/j.jvs.2009.01.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lederle FA, Freischlag JA, Kyriakides TC, Padberg FT, Jr, Matsumura JS, Kohler TR, et al. Outcomes following endovascular vs open repair of abdominal aortic aneurysm: a randomized trial. JAMA. 2009;302:1535–42. doi: 10.1001/jama.2009.1426. [DOI] [PubMed] [Google Scholar]
- 9.Brewster DC, Jones JE, Chung TK, Lamuraglia GM, Kwolek CJ, Watkins MT, et al. Long-term outcomes after endovascular abdominal aortic aneurysm repair: the first decade. Ann Surg. 2006;244:426–38. doi: 10.1097/01.sla.0000234893.88045.dc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Harris PL, Vallabhaneni SR, Desgranges P, Becquemin JP, van Marrewijk C, Laheij RJ. Incidence and risk factors of late rupture, conversion, and death after endovascular repair of infrarenal aortic aneurysms: The EUROSTAR experience. J Vasc Surg. 2000;32:739–49. doi: 10.1067/mva.2000.109990. [DOI] [PubMed] [Google Scholar]
- 11.Peppelenbosch N, Buth J, Harris PL, van Marrewijk C, Fransen G, EUROSTAR Collaborators Diameter of abdominal aortic aneurysm and outcome of endovascular aneurysm repair: does size matter? A report from EUROSTAR. J Vasc Surg. 2004;39:288–97. doi: 10.1016/j.jvs.2003.09.047. [DOI] [PubMed] [Google Scholar]
- 12.van Marrewijk CJ, Leurs LJ, Vallabhaneni SR, Harris PL, Buth J, Laheij RJ, et al. Risk-adjusted outcome analysis of endovascular abdominal aortic aneurysm repair in a large population: how do stent-grafts compare? J Endovasc Ther. 2005;12:417–29. doi: 10.1583/05-1530R.1. [DOI] [PubMed] [Google Scholar]
- 13.Schermerhorn M. Should usual criteria for intervention in abdominal aortic aneurysms be “downsized,” considering reported risk reduction with endovascular repair? Annals of the New York Academy of Sciences. 2006;1085:47–58. doi: 10.1196/annals.1383.043. [DOI] [PubMed] [Google Scholar]
- 14.Hobo R, Kievit J, Leurs LJ, Buth J, EUROSTAR Collaborators Influence of severe infrarenal aortic neck angulation on complications at the proximal neck following endovascular AAA repair: a EUROSTAR study. J Endovasc Ther. 2008;14:1–11. doi: 10.1583/06-1914.1. [DOI] [PubMed] [Google Scholar]