Abstract
There is clear evidence regarding the health benefits of physical activity. These benefits follow a dose-response relationship with a particular respect to exercise intensity. Guidelines for exercise testing and prescription have been established to provide optimal standards for exercise training. A wide range of intensities is used to prescribe exercise, but this approach is limited. Usually percentages of maximal oxygen uptake (VO2) or heart rate (HR) are applied to set exercise training intensity but this approach yields substantially variable metabolic and cardiocirculatory responses. Heterogeneous acute responses and training effects are explained by the nonuniform heart rate performance curve during incremental exercise which significantly alters the calculations of %HRmax and %HRR target HR data. Similar limitations hold true for using %VO2max and %VO2R. The solution of these shortcomings is to strictly apply objective submaximal markers such as thresholds or turn points and to tailor exercise training within defined regions.
1. Introduction
Evidence regarding the health benefits of physical activity is overwhelming and there is no doubt about the impact of exercise training on health and fitness [1–3]. Exercise training improves exercise tolerance as well as symptoms of particular diseases and increases submaximal and maximal exercise capacity [2–5]. Furthermore, exercise training improves quality of life and reduces hospitalisation, morbidity, and mortality [6–10]. There is clear evidence that exercise training therapy positively affects chronic diseases in general [2, 5], and therefore exercise training is usually an integral part of secondary prevention and specifically of cardiac rehabilitation [11]. However, the applied exercise prescriptions in the underlying training interventions studies vary considerably. Corra et al. [11] suggested the usually applied exercise modalities to be safe, however, the question about the most effective training mode still remains to be answered.
As presented by the American College of Sports Medicine (ACSM) the essential components of a systematic individualized exercise prescription include the appropriate mode(s), intensity, duration, frequency, and progression of exercise training at which exercise intensity is considered as the most important of the primary variables [12]. With respect to exercise intensity, we may suggest that the optimal individually tailored exercise prescription for each single subject can only be determined from an objective evaluation of the individuals' response to exercise. This implies the standard use of cardiopulmonary exercise testing for the functional evaluation of healthy subjects and patients and the determination of individual reference points for every single subject [13–16]. It seems obvious that the relative but not the absolute intensity is the major impact for an exercise-induced increase in several mRNA [17] pointing to the importance of individual reference points for exercise prescription, independent of health and fitness status.
Health and fitness benefits associated with exercise training follow a dose-response relationship where the importance of optimal individual exercise intensity has been highlighted [5, 17]. That applies particularly to subjects with disease but also for apparently healthy subjects and athletes.
However, in the numerous studies available, various combinations of the above-mentioned components of exercise prescription were applied, and up to now there is no consistent model of exercise prescription fulfilling the optimal individual needs for training studies in healthy subjects and patients.
Guidelines for exercise testing and prescription have been established to provide optimal standards for exercise training in healthy subjects as well as for cardiac rehabilitation and secondary prevention programs [12, 14–16]. These standards give a broad spectrum of possibilities for the attending physician by defining safe and effective upper and lower limits in general terms. However, this wide range of intensities for the prescription of exercise recommended in these guidelines (Table 1) makes it rather difficult to make an appropriate choice of exercise intensity for a single individual. The application of various exercise intensities within this wide spectrum gives good reasons for differences in the training responses and the heterogeneity in outcome seen in all kinds of different exercise training intervention studies limiting the comparability of data [25, 26].
Table 1.
Overview of recommendations for physical activity and public health in healthy adults and patients.
| Recommendation | Intensity | Duration | Frequency |
|---|---|---|---|
| ACSM [18] resource manual for guidelines for exercise testing and prescription healthy individuals | moderate intensity 40%–59% HRR (VO2R) vigorous intensity ≥ 60% HRR (VO2R) | 20–60 min·day−1 continuous or intermittent in bouts of at least 10 min 20–60 min·day−1 continuous or intermittent in bouts of at least 10 min | min. of 5 d·wk−1min. 3 d·wk−1 |
| CAD + MI patients | 40%–85% HRR (VO2R) | ||
| HF patients | 40%–70% HRR (VO2R) | ||
| ACSM [19] guidelines for exercise testing and prescription | 40%–85% HRR (VO2R) | 20–60 min·day−1 | 3–5 d·wk−1 |
| ACSM/AHA [20] healthy adults 18–65 years of age | moderate intensity (between 3.0 and 6.0 METs) vigorous intensity (above 6.0 METs) | at least 30 min·day−1 continuous or intermittent in bouts of at least 10 min each at least 20 min·day−1 continuous activity | min. of 5 d·wk−1min. of 3 d·wk−1 |
| ACSM/AHA [21] older adults aged >65 years | moderate intensity (5-6 on a 10-point scale)vigorous intensity (7-8 on a 10-point scale) | at least 30 min·day−1 continuous or intermittent (in bouts of at least 10 min each) activity at least 20 min·day−1 continuous activity | min. of 5 d·wk−1min. of 3 d·wk−1 |
| AHA [22] coronary artery disease | moderate intensity (40%–60% of HRR) vigorous intensity as tolerated (60%–85 % of HRR) | at least 30 min·day−1 | min. of 3 d·wk−1 |
| ACSM [23] hypertension | moderate intensity (40%–60% of VO2R) vigorous intensity acceptable for selected adults | 30–60 min·day−1 continuous or intermittent (in bouts of at least 10 min each) activity | most, preferably all days per week |
| AHA [24] stroke | 50%–80% of HRmax | 20–60 min/session (or multiple 10 min sessions) | 3–7 d·wk−1 |
| American Diabetes Association [21] type 2 diabetes | moderate intensity (50%–70% of HRmax) vigorous intensity (>70% of HRmax) | at least 150 min·wk−1 moderate and/or at least 90 min·wk−1 vigorous activity | min. of 3 d·wk−1, no more than 2 consecutive days without activity |
HRR: heart rate reserve; VO2R: oxygen consumption reserve.
CAD: coronary artery disease; MI: myocardial infarction; HF: heart failure.
The questions to be answered are which optimal choice of intensity for an individual is safe (upper limit) and effective (lower limit) and, even much more important, which is the optimal definition of exercise intensity for scientific investigations to evaluate training effects in healthy subjects and patients suffering from various chronic diseases [13, 27, 28].
As exercise intensity is suggested to be the leading component of exercise prescription we draw our attention especially to this specific component, although one should be aware of the fact that all components of exercise training and their combination are also substantial parts of the action of exercise training.
2. Exercise Intensity
It is suggested that physiological benefits gained from exercise training are primarily dependent on the intensity of the training stimulus [32]. The intensity should be above a minimal level required to induce a training effect which was shown to be at 40%–49% heart rate reserve (HRR) or 64%–70% maximal heart rate (HRmax) or even lower at 30% oxygen uptake reserve (VO2R) in unfit subjects [19]. However, clearly defined standards for the lower limit of prescriptible aerobic training intensity have not been established yet, neither in healthy individuals nor in cardiac patients [27]. As it is well known in work physiology that staying below 33%–50% maximal oxygen uptake (VO2max) is necessary to sustain eight-hour work shifts [33], we may assume this threshold to be a limit which has to be exceeded to gain training effects.
The upper limit of prescriptible aerobic training intensity is crucial for safety and control of exercise-related risks [27]. Therefore, exercise prescription should include individually prescribed upper limits for exercise intensities. Several studies showed that in general training using higher intensities gains significantly greater improvements than moderate or low intensity exercise training with the same volume of exercise [34–36] or similar energy expenditure [37]. These findings led to a revival of intense interval-type exercise training [38–42]. However, approaching the limits of tolerance requires more precise and sophisticated diagnostics and exercise intensity prescriptions particularly for patients.
3. Exercise Intensity Prescription by Means of HRmax and HRR
Standard variables used to prescribe exercise intensity are percentages of maximal heart rate (HRmax) and maximal oxygen uptake (VO2max) as well as calculated subfractions of these variables such as HR reserve (HRR) and VO2 reserve (VO2R).
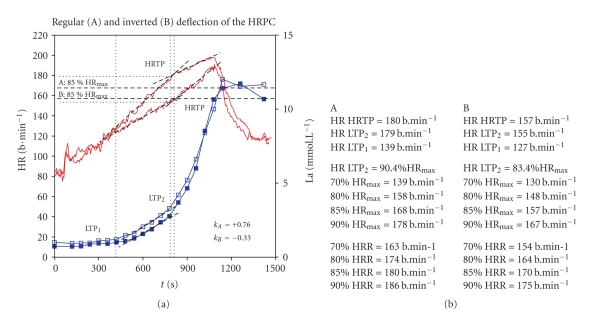
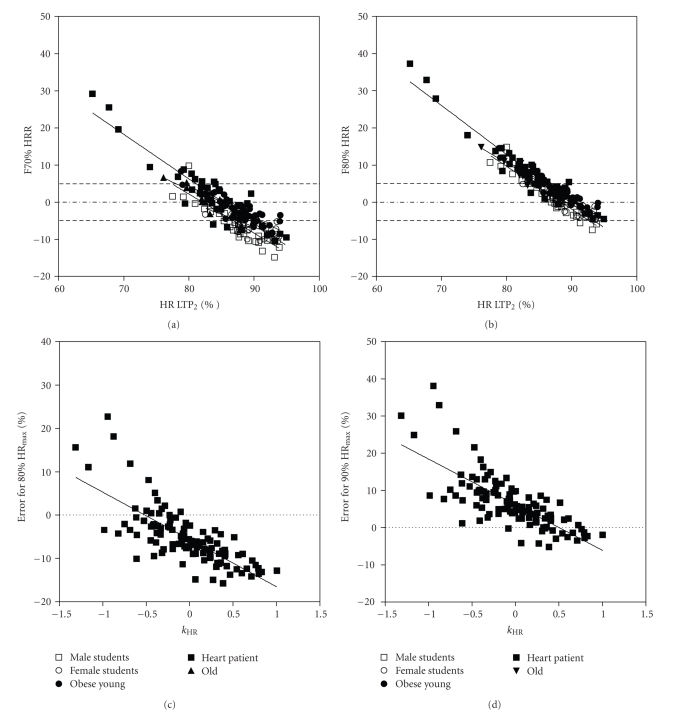
Heart rate is the most common parameter to determine target exercise training intensity. The usual recommendations are in a range between 64% and 70% to 94% of HRmax or between 40% and 50% to 85% of HRR (and VO2R) [19] (Table 1). However, the HR response to incremental exercise was shown to be neither linear nor uniform [29, 30, 43] (Figure 2). Consequently, this heterogeneous character of the heart rate performance curve (HRPC) significantly alters the calculations of %HRmax and %HRR target training HR as shown previously [29, 44–47]. It is demonstrated in Figure 2 that two healthy young subjects with more or less identical maximal power output (Pmax) and submaximal power output at the first lactate turn point (P LTP1) and at the second lactate turn point (P LTP2) vary considerably in their HR response, more precisely in their %HRmax at P LTP2. So calculating the same target training upper limits by means of %HRmax or %HRR gives a completely different training load with respect to the reference turn points [13, 25, 29, 46, 47]. More importantly most patients with cardiovascular disease present an upward deflection of the heart rate performance curve [48] stressing the importance of this problem in this kind of population (Figure 2). Using %HRmax methods such as the common 85% HRmax model will lead to an overestimation of the individual training heart rate by at least 5%–10% and up to 40% in single cases [44]. Figure 3 shows the error of estimate caused by different % HRmax at P LTP2 if fixed percentages of HRmax or HRR [29, 44] are applied. Similar results were also shown by Tabet et al. [46] and Wonisch et al. [47].
Figure 2.
Accuracy of target training heart rate dependent on the time course of the Heart Rate Performance Curve. The same relative intensity of 85% HRmax (usual upper limit) gives different work load related to the anaerobic threshold (LTP2) [29]. Subject (A) 85% HRmax is well below HR LTP2; subject (B) 85% HRmax is already above HR LTP2.
Figure 3.
Error of estimate for percent heart rate reserve (HRR) compared to %HR at the second lactate turn point (LTP2) as well as the error of estimate for percent HRmax related to the deflection of the heart rate performance curve (kHR) [29, 30] in healthy young male and female sports students, young obese subjects, older healthy subjects, and patients after myocardial infarction [31].
Additional concerns may be raised if true maximal HR or oxygen uptake values can be obtained in untrained subject and especially in patients [49, 50]. Because of local leg fatigue, tests may end prematurely before cardiopulmonary endpoints have been achieved [19].
4. Exercise Intensity Prescription by Means of VO2max and VO2R
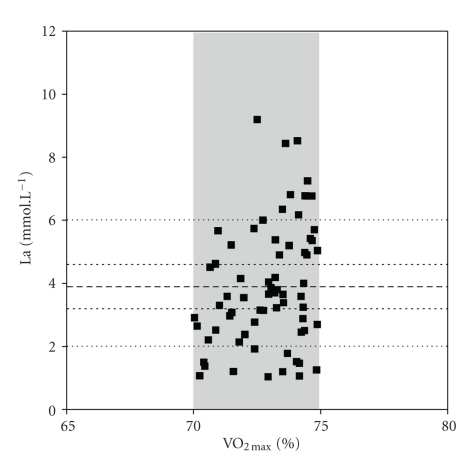
Oxygen uptake-based prescriptions are frequently used for individual training but more often for exercise training studies since VO2max is accepted as the criterion measure of cardiorespiratory fitness. Several studies [32, 51] indicated that among healthy adults, %VO2R is more closely related to %HRR than it is to %VO2max, although there is a disparity of 10% between the two first methods mentioned above. It has also been shown that the disparity increases with age [32]. These findings, in addition to the disparity between %HRR and %VO2max which is greater at low intensities and among low fit individuals, provoked the ACSM to adopt the use of %VO2R in place of %VO2max when prescribing exercise intensity among healthy adults and patients [51]. It is a common assumption that not only absolute oxygen uptake at the anaerobic threshold but also %VO2max at this threshold is higher in trained subjects [52]. Similarly as shown for HR, exercise prescription based on fixed percentages of VO2max will lead to an overestimation of target training intensity in patients with limited exercise tolerance and with a first lactate turn point appearing already at a very low power output [53]. In accordance with that, Scharhag-Rosenberger et al. [26] emphasized that applying the same fixed percentage of maximal oxygen uptake yields substantially variable acute metabolic responses across subjects (Figure 4) and that different training stimuli with respect to individual submaximal reference turn points (P LTP1, P LTP2) may be expected.
Figure 4.
Mean blood lactate concentration (La) during constant load exercise in trained subjects applying controlled 70%–75% of VO2max (unpublished results).
In addition, several studies have shown marked individual differences in responsiveness to exercise training interventions. For example, impacts of standardized training programs on VO2max have ranged from almost no gain up to 100% increase in large groups of sedentary individuals [54–56]. Similar results have been reported by Hansen et al. [57] in cardiac patients. Data from the HERITAGE family study [56] showed that subjects who exercised at an HR associated with the same relative %VO2max intensity vary substantially in their training response, in their rate of increase in power output over a 20-wk training program, and in their improvement of VO2max. However, age, sex, race, and initial fitness had little impact on these individual differences [54, 56], and a genetic component to explain these differences was suggested [58, 59]. However, one may suggest also the mode of exercise prescription to be a possible factor of influence [25, 26, 28]. Furthermore, similar as discussed for HRmax we may critically argue if a true VO2max can be obtained in untrained obese subjects [60] and patients [61].
Most of the prescription models used for exercise training interventions refer to maximal variables measured from incremental ergometer exercise giving a wide range of intensities (Table 1); however, given the aforementioned limitations of these models, the recommendations to use turn point models are increasing [13, 26, 62].
5. Exercise Intensity Prescription by Means of Submaximal Markers—The Turn Point Model
Scharhag-Rosenberger et al. [26] criticized the “traditional” concept to prescribe exercise intensity by means of maximal values, and they suggested that it might be more appropriate to consider the metabolic demand of exercise applying a threshold concept. Several authors [25, 46] have pointed out the shortcomings of training prescriptions without defining a threshold but applying fixed percentages of HRmax or HRR leading to differing levels of metabolic stress across subjects (see Figures 2 and 3). Recently Salvadego et al. [63] suggested that exercise prescription and evaluation should be made at workloads chosen with respect to submaximal markers from incremental exercise and not as percentages of VO2max. Binder et al. [13] showed the advantage of applying a three phase model, using the first- and the second- turn point approach presented earlier by Davis et al. [64] and later on by our own working group [29, 30, 43, 65–67] and other authors [68]. This method, however, is surprisingly only marginally described in the current guidelines.
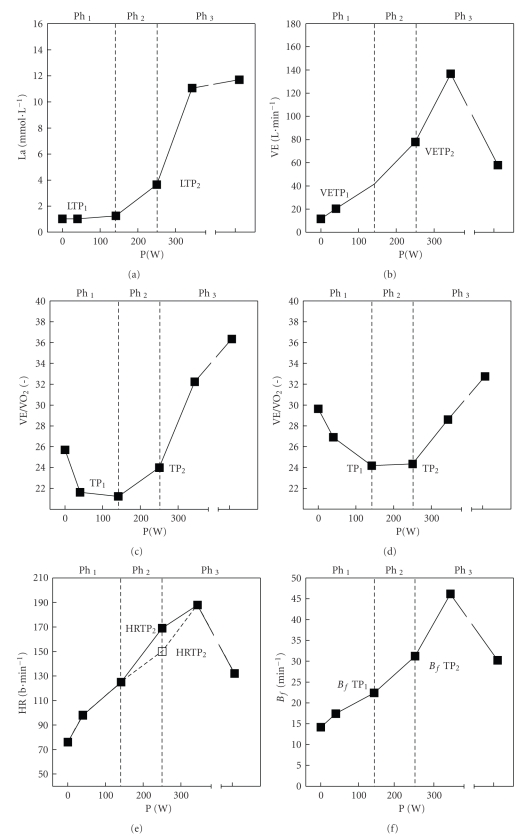
Figure 1.
Schematic representation of first- and second- turn points of selected variables (La blood lactate concentration; VE: ventilation; VE/VO2: equivalent for oxygen uptake; VE/VCO2: equivalent for carbon dioxide output; HR: heart rate; Bf: breathing frequency) and distinct phases (Ph 1–3) of energy supply determined from young healthy male subjects. Ph 1: no increase of blood lactate concentration above baseline during constant load exercise. Ph 2: increased but steady state blood lactate concentration during constant load exercise. Ph 3: continuous increase of blood lactate concentration during constant load exercise leading to early termination of exercise.
This concept is known as the three-phase-model presented already by Skinner and McLellan [69]. As there are numerous concepts to determine thresholds, this topic has been discussed extensively during the past decades. From all these concepts two different main approaches can be deduced:
-
(1)
thresholds indicating the first increase in blood lactate concentration originally defined as the “anaerobic threshold” (AT) by Wasserman and McIlroy [70] and mostly described as the “aerobic threshold” equivalent to the first-turn point for lactate (La), ventilation (VE), and the oxygen equivalent (VE/VO2), and breathing frequency (Bf) [13, 62],
-
(2)
thresholds indicating the maximal lactate steady state which is significantly higher than the first-turn point and mostly described as the “anaerobic threshold” equivalent to the second-turn point for La, VE, Bf, VE/VO2, and VE/VCO2 [13, 29, 62, 65–67, 71] as well as to the heart rate turn point (HRTP) as earlier shown by our own working group [29, 30, 65].
Numerous definitions and descriptions of these thresholds have been presented in the last decades [13].
To avoid any confusion, we therefore recommend to apply a nomenclature defining a first- (TP1) and a second-turn point (TP2) and denominate the turn points by the variable used to detect the turn point such as the first and the second turn points for lactate (LTP1, LTP2), heart rate (HRTP1, HRTP2) ventilation (VETP1, VETP2) or the oxygen equivalent (VE/VO2TP1, VE/VO2TP2) and the carbon dioxide equivalent (VE/VCO2TP1, VE/VCO2TP2). Figure 1 shows a schematic representation of the first and second turn points for these selected variables based on measures of 25 trained male subjects [31].
Using these objective individual turn points to prescribe exercise intensity allows for homogenous acute metabolic responses and uniform training stimuli across subjects yielding a reduction of health risk and enabling the comparison of results revealed by different training intervention studies.
The complex of problems associated with heterogeneous metabolic responses was pointed up by Hashimoto and Brooks [72] who argued that lactate is not only an oxidizable substrate and glucogenic precursor, but may also act as a pseudohormone called “lactormone” with a distinct signaling role. They nicely showed that lactate incubation up-regulated hundreds of ROS-sensitive genes, suggesting the presence of a vast lactate-activated transcription network, a lactate transcriptome. This gives a good reason to postulate the use of exercise training regimes that induce similar metabolic responses across subjects. To ensure this demand, however, one has to respect the lactate shuttle theory [73] which implies a three-phase framework of the lactate performance curve with two distinct turn points [29–31] and three distinct phases of energy supply. Up to date there are no studies available applying such specifically tailored exercise protocols; however, some studies strongly support this assumption. Lamprecht et al. [74] showed that oxidative protein damage, as indicated by carbonyl protein oxidation, was significantly increased at intensities slightly above LTP2 (VT2) but was not at intensities below this turn point. Additionally, Jürimäe et al. [75] applied two constant workloads, one just below and one just above HRTP2 (VT2) in trained rowers. These authors showed that despite minimal heart rate differences of only 5 b·min−1 between two rowing exercise bouts just below or above VT2, growth hormone response was almost doubled in exercise above the VT2. Given these findings, the second turn point for La, HR, or VE [29, 30, 65, 71, 76], consistent with the maximal lactate steady state [67, 76], seems to be a criterion for the upper level of exercise prescription in healthy subjects and patients.
In addition, the prescription of exercise intensity by means of the turn point concept is successfully applicable not only for constant load exercise, but also for interval-type exercise as recently shown by Tschakert et al. [77].
However, there are still some controversies about the “correct” concept of AT-determination to apply. Standards have been set for ventilatory threshold [62]; however, standard lactate-derived thresholds are still missing.
6. Conclusions
Exercise intensity plays a pivotal role to gain a sufficient training response without harmful side effects in healthy subjects and patients. Higher exercise intensities seem to be more beneficial; however, approaching the upper limits of exercise tolerance demands a more precise determination of these limits. Fixed percentages of HRmax or VO2max are not sufficient when approaching the upper limits and include some serious errors. For safety reasons, it may be concluded that the upper limit of target heart rate for exercise prescription should therefore not be assessed by means of a particular percentage of HRmax, HRR, VO2max, or VO2R, but by using intensities related to a certain threshold or turn point. The lactate turn point (LTP) concept gives a valid approach as it has a theoretical foundation and is consistent with other threshold determinations. As turn point concepts for lactate, heart rate, or ventilatory variables define these upper limits more precisely, this somewhat sophisticated approach is expected to be superior to the usual “art” of exercise prescription using fixed percentages and is therefore recommended by our working group especially for training studies. In addition, we ascertain that this definition of target training zones by means of turn points is necessary for trainings studies to obtain similar relative intensities and therefore comparable results for all study participants independent of their fitness level.
However, evidence regarding the most efficient training mode and intensity is still lacking. Further research is encouraged applying the turn point model describing distinct phases of energy supply to set exercise intensity standards for training intervention studies in patients.
References
- 1.Church TS, Blair SN. When will we treat physical activity as a legitimate medical therapy…even though it does not come in a pill? British Journal of Sports Medicine. 2009;43(2):80–81. doi: 10.1136/bjsm.2008.053850. [DOI] [PubMed] [Google Scholar]
- 2.Kujala UM. Evidence on the effects of exercise therapy in the treatment of chronic disease. British Journal of Sports Medicine. 2009;43(8):550–555. doi: 10.1136/bjsm.2009.059808. [DOI] [PubMed] [Google Scholar]
- 3.Warburton DER, Nicol CW, Bredin SSD. Health benefits of physical activity: the evidence. Canadian Medical Association Journal. 2006;174(6):801–809. doi: 10.1503/cmaj.051351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jolliffe JA, Rees K, Taylor RS, Thompson D, Oldridge N, Ebrahim S. Exercise-based rehabilitation for coronary heart disease. Cochrane Database of Systematic Reviews. 2001;(1) doi: 10.1002/14651858.CD001800. Article ID CD001800. [DOI] [PubMed] [Google Scholar]
- 5.Pedersen BK, Saltin B. Evidence for prescribing exercise as therapy in chronic disease. Scandinavian Journal of Medicine and Science in Sports. 2006;16(1):3–63. doi: 10.1111/j.1600-0838.2006.00520.x. [DOI] [PubMed] [Google Scholar]
- 6.Blair SN, Kohl HW, Barlow CE, Paffenbarger RS, Gibbons LW, Macera CA. Changes in physical fitness and all-cause mortality: a prospective study of healthy and unhealthy men. Journal of the American Medical Association. 1995;273(14):1093–1098. [PubMed] [Google Scholar]
- 7.Sakamoto S, Yokoyama N, Tamori Y, Akutsu K, Hashimoto H, Takeshita S. Patients with peripheral artery disease who complete 12-week supervised exercise training program show reduced cardiovascular mortality and morbidity. Circulation Journal. 2009;73(1):167–173. doi: 10.1253/circj.cj-08-0141. [DOI] [PubMed] [Google Scholar]
- 8.Sandvik L, Erikssen J, Thaulow E, Erikssen G, Mundal R, Rodahl K. Physical fitness as a predictor of mortality among healthy, middle-aged Norwegian men. New England Journal of Medicine. 1993;328(8):533–537. doi: 10.1056/NEJM199302253280803. [DOI] [PubMed] [Google Scholar]
- 9.Smart N, Marwick TH. Exercise training for patients with heart failure: a systematic review of factors that improve mortality and morbidity. American Journal of Medicine. 2004;116(10):693–706. doi: 10.1016/j.amjmed.2003.11.033. [DOI] [PubMed] [Google Scholar]
- 10.Wei M, Gibbons LW, Kampert JB, Nichaman MZ, Blair SN. Low cardiorespiratory fitness and physical inactivity as predictors of mortality in men with type 2 diabetes. Annals of Internal Medicine. 2000;132(8):605–611. doi: 10.7326/0003-4819-132-8-200004180-00002. [DOI] [PubMed] [Google Scholar]
- 11.Corr U, Carré F, Heuschmann P, et al. Secondary prevention through cardiac rehabilitation: physical activity counselling and exercise training. European Heart Journal. 2010;31(16):1967–1974b. doi: 10.1093/eurheartj/ehq236. [DOI] [PubMed] [Google Scholar]
- 12.ACSM’s Guidelines for Exercise Testing and Prescription. 8th edition. Baltimore, Md, USA: Lippincott Williams & Wilkins; 2010. [Google Scholar]
- 13.Binder RK, Wonisch M, Corra U, et al. Methodological approach to the first and second lactate threshold in incremental cardiopulmonary exercise testing. European Journal of Cardiovascular Prevention and Rehabilitation. 2008;15(6):726–734. doi: 10.1097/HJR.0b013e328304fed4. [DOI] [PubMed] [Google Scholar]
- 14.Giada F, Biffi A, Agostoni P, et al. Exercise prescription for the prevention and treatment of cardiovascular diseases: part I. Journal of Cardiovascular Medicine. 2008;9(5):529–544. doi: 10.2459/JCM.0b013e3282f7ca77. [DOI] [PubMed] [Google Scholar]
- 15.Giada F, Biffi A, Agostoni P, et al. Exercise prescription for the prevention and treatment of cardiovascular diseases: part II. Journal of Cardiovascular Medicine. 2008;9(6):641–652. doi: 10.2459/JCM.0b013e3282f7ca96. [DOI] [PubMed] [Google Scholar]
- 16.Mezzani A, Agostoni P, Cohen-Solal A, et al. Standards for the use of cardiopulmonary exercise testing for the functional evaluation of cardiac patients: a report from the exercise physiology section of the European association for cardiovascular prevention and rehabilitation. European Journal of Cardiovascular Prevention and Rehabilitation. 2009;16(3):249–267. doi: 10.1097/HJR.0b013e32832914c8. [DOI] [PubMed] [Google Scholar]
- 17.Nordsborg NB, Lundby C, Leick L, Pilegaard H. Relative workload determines exercise-induced increases in PGC-1α mRNA. Medicine and Science in Sports and Exercise. 2010;42(8):1477–1484. doi: 10.1249/MSS.0b013e3181d2d21c. [DOI] [PubMed] [Google Scholar]
- 18.ACSM’s Resource Manual for Guidelines for Exercise Testing and Prescription. 6th edition. Baltimore, Md, USA: Lippincott Williams & Wilkins; 2010. [Google Scholar]
- 19.ACSM’s Guidelines for Exercise Testing and Prescription. 7th edition. Baltimore, Md, USA: Lippincott Williams & Wilkins; 2006. [Google Scholar]
- 20.Haskell WL, Lee IM, Pate RR, et al. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Circulation. 2007;116(9):1081–1093. doi: 10.1161/CIRCULATIONAHA.107.185649. [DOI] [PubMed] [Google Scholar]
- 21.Nelson ME, Rejeski WJ, Blair SN, et al. Physical activity and public health in older adults: recommendation from the American College of Sports Medicine and the American Heart Association. Circulation. 2007;116(9):1094–1105. doi: 10.1161/CIRCULATIONAHA.107.185650. [DOI] [PubMed] [Google Scholar]
- 22.Fletcher GF, Balady GJ, Amsterdam EA, et al. Exercise standards for testing and training: a statement for healthcare professionals from the American Heart Association. Circulation. 2001;104(14):1694–1740. doi: 10.1161/hc3901.095960. [DOI] [PubMed] [Google Scholar]
- 23.Pescatello LS, Franklin BA, Fagard R, Farquhar WB, Kelley GA, Ray CA. American College of Sports Medicine position stand. Exercise and hypertension. Medicine and science in sports and exercise. 2004;36(3):533–553. doi: 10.1249/01.mss.0000115224.88514.3a. [DOI] [PubMed] [Google Scholar]
- 24.Gordon NF, Gulanick M, Costa F, Fletcher G, Franklin BA, Roth EJ. Physical Activity and Exercise Recommendations for Stroke Survivors: an American Heart Association Scientific Statement from the Council on Clinical Cardiology, Subcommittee on Exercise, Cardiac Rehabilitation, and Prevention; the Council on Cardiovascular Nursing; the Council on Nutrition, Physical Activity, and Metabolism; and the Stroke Council. Circulation. 2004;109(16):2031–2041. doi: 10.1161/01.CIR.0000126280.65777.A4. [DOI] [PubMed] [Google Scholar]
- 25.Meyer T, Gabriel HHW, Kindermann W. Is determination of exercise intensities as percentages of VO2max or HRmax adequate? Medicine and Science in Sports and Exercise. 1999;31(9):1342–1345. doi: 10.1097/00005768-199909000-00017. [DOI] [PubMed] [Google Scholar]
- 26.Scharhag-Rosenberger F, Meyer T, Gäßler N, Faude O, Kindermann W. Exercise at given percentages of VO2max: heterogeneous metabolic responses between individuals. Journal of Science and Medicine in Sport. 2010;13(1):74–79. doi: 10.1016/j.jsams.2008.12.626. [DOI] [PubMed] [Google Scholar]
- 27.Carvalho VO, Mezzani A. Aerobic exercise training intensity in patients with chronic heart failure: principles of assessment and prescription. doi: 10.1097/HJR.0b013e32833a9c63. European Journal of Cardiovascular Prevention & Rehabilitation. In press. [DOI] [PubMed] [Google Scholar]
- 28.Meyer T, Kindermann M, Kindermann W. Exercise programmes for patients with chronic heart failure. Sports Medicine. 2004;34(14):939–954. doi: 10.2165/00007256-200434140-00001. [DOI] [PubMed] [Google Scholar]
- 29.Hofmann P, Von Duvillard SP, Seibert FJ, et al. %HR target heart rate is dependent on heart rate performance curve deflection. Medicine and Science in Sports and Exercise. 2001;33(10):1726–1731. doi: 10.1097/00005768-200110000-00017. [DOI] [PubMed] [Google Scholar]
- 30.Hofmann P, Pokan R, Von Duvillard SP, Seibert FJ, Zweiker R, Schmid P. Heart rate performance curve during incremental cycle ergometer exercise in healthy young male subjects. Medicine and Science in Sports and Exercise. 1997;29(6):762–768. doi: 10.1097/00005768-199706000-00005. [DOI] [PubMed] [Google Scholar]
- 31.Hofmann P, Tschakert G, Pokan R, VonDuvillard SP. Three-phase time course of physiological variables during incremental cycling in young male and female subjects. Medicine and Science in Sports and Exercise. 2010;42(5):p. 238. Abstract. [Google Scholar]
- 32.Patterson JA, Selig SE, Toia D, Geerling RH, Bamroongsuk V, Hare DL. Comparing methods for prescribing exercise for individuals with chronic heart failure. Journal of Exercise Physiology Online. 2005;8(4):9–19. [Google Scholar]
- 33.Ilmarinen J, Tuomi K, Eskelinen L, Nygard CH, Huuhtanen P, Klockars M. Background and objectives of the Finnish research project on aging workers in municipal occupations. Scandinavian Journal of Work, Environment and Health. 1991;17(1):7–11. [PubMed] [Google Scholar]
- 34.Duncan GE, Anton SD, Sydeman SJ, et al. Prescribing exercise at varied levels of intensity and frequency: a randomized trial. Archives of Internal Medicine. 2005;165(20):2362–2369. doi: 10.1001/archinte.165.20.2362. [DOI] [PubMed] [Google Scholar]
- 35.Jensen BE, Fletcher BJ, Rupp JC, Fletcher GF, Lee JY, Oberman A. Training level comparison study: effect of high and low intensity exercise on ventilatory threshold in men with coronary artery disease. Journal of Cardiopulmonary Rehabilitation. 1996;16(4):227–232. doi: 10.1097/00008483-199607000-00003. [DOI] [PubMed] [Google Scholar]
- 36.Lee IM, Paffenbarger RS. Associations of light, moderate, and vigorous intensity physical activity with longevity: the Harvard Alumni Health Study. American Journal of Epidemiology. 2000;151(3):293–299. doi: 10.1093/oxfordjournals.aje.a010205. [DOI] [PubMed] [Google Scholar]
- 37.Swain DP, Franklin BA. Comparison of cardioprotective benefits of vigorous versus moderate intensity aerobic exercise. American Journal of Cardiology. 2006;97(1):141–147. doi: 10.1016/j.amjcard.2005.07.130. [DOI] [PubMed] [Google Scholar]
- 38.Rognmo Ø, Hetland E, Helgerud J, Hoff J, Slørdahl SA. High intensity aerobic interval exercise is superior to moderate intensity exercise for increasing aerobic capacity in patients with coronary artery disease. European Journal of Cardiovascular Prevention and Rehabilitation. 2004;11(3):216–222. doi: 10.1097/01.hjr.0000131677.96762.0c. [DOI] [PubMed] [Google Scholar]
- 39.Schjerve IE, Tyldum GA, Tjønna AE, et al. Both aerobic endurance and strength training programmes improve cardiovascular health in obese adults. Clinical Science. 2008;115(9):283–293. doi: 10.1042/CS20070332. [DOI] [PubMed] [Google Scholar]
- 40.Tjønna AE, Stølen TO, Bye A, et al. Aerobic interval training reduces cardiovascular risk factors more than a multitreatment approach in overweight adolescents. Clinical Science. 2009;116(4):317–326. doi: 10.1042/CS20080249. [DOI] [PubMed] [Google Scholar]
- 41.Wisløff U, Støylen A, Loennechen JP, et al. Superior cardiovascular effect of aerobic interval training versus moderate continuous training in heart failure patients: a randomized study. Circulation. 2007;115(24):3086–3094. doi: 10.1161/CIRCULATIONAHA.106.675041. [DOI] [PubMed] [Google Scholar]
- 42.Wisløff U, Ellingsen Ø, Kemi OJ. High-intensity interval training to maximize cardiac benefits of exercise training? Exercise and sport sciences reviews. 2009;37(3):139–146. doi: 10.1097/JES.0b013e3181aa65fc. [DOI] [PubMed] [Google Scholar]
- 43.Hofmann P, Wonisch M, Pokan R, Schwaberger G, Smekal G, Von Duvillard SP. β1-adrenoceptor mediated origin of the heart rate performance curve deflection. Medicine and Science in Sports and Exercise. 2005;37(10):1704–1709. doi: 10.1249/01.mss.0000176308.70316.cc. [DOI] [PubMed] [Google Scholar]
- 44.Hofmann P, Tschakert G, Stark M, et al. Estimation error when using the %HRR method compared to the lactate turn point. Medicine and Science in Sports and Exercise. 2009;41(supplement 5):221–222. [Google Scholar]
- 45.Omiya K, Itoh H, Osada N, et al. Impaired heart rate response during incremental exercise in patients with acute myocardial infarction and after coronary artery bypass grafting evaluation of coefficients with Karvonen's formula. Japanese Circulation Journal. 2000;64(11):851–855. doi: 10.1253/jcj.64.851. [DOI] [PubMed] [Google Scholar]
- 46.Tabet J-Y, Meurin P, Driss AB, et al. Determination of exercise training heart rate in patients on β-blockers after myocardial infarction. European Journal of Cardiovascular Prevention and Rehabilitation. 2006;13(4):538–543. doi: 10.1097/01.hjr.0000209813.05573.4d. [DOI] [PubMed] [Google Scholar]
- 47.Wonisch M, Hofmann P, Fruhwald FM, et al. Influence of beta-blocker use on percentage of target heart rate exercise prescription. European Journal of Cardiovascular Prevention and Rehabilitation. 2003;10(4):296–301. doi: 10.1097/00149831-200308000-00013. [DOI] [PubMed] [Google Scholar]
- 48.Pokan R, Hofmann P, Von Duvillard SP, et al. The heart rate performance curve and left ventricular function during exercise in patients after myocardial infarction. Medicine and Science in Sports and Exercise. 1998;30(10):1475–1480. doi: 10.1097/00005768-199810000-00002. [DOI] [PubMed] [Google Scholar]
- 49.Kjelkenes I, Thorsen E. Anticipating maximal or submaximal exercise: no differences in cardiopulmonary responses. Clinical Physiology and Functional Imaging. 2010;30(5):333–337. doi: 10.1111/j.1475-097X.2010.00948.x. [DOI] [PubMed] [Google Scholar]
- 50.Midgley AW, McNaughton LR, Polman R, Marchant D. Criteria for determination of maximal oxygen uptake: a brief critique and recommendations for future research. Sports Medicine. 2007;37(12):1019–1028. doi: 10.2165/00007256-200737120-00002. [DOI] [PubMed] [Google Scholar]
- 51.Brawner CA, Keteyian SJ, Ehrman JK. The relationship of heart rate reserve to VO2 reserve in patients with heart disease. Medicine and Science in Sports and Exercise. 2002;34(3):418–422. doi: 10.1097/00005768-200203000-00006. [DOI] [PubMed] [Google Scholar]
- 52.Åstrand PO, Rodahl K, Dahl H, Strømme S. Textbook of Work Physiology: Physiological Bases of Exercise. 4th edition. Human Kinetics; 2003. [Google Scholar]
- 53.Zoladz JA, Korzeniewski B. Physiological background of the change point in VO2 and the slow component of oxygen uptake kinetics. Journal of Physiology and Pharmacology. 2001;52(2):167–184. [PubMed] [Google Scholar]
- 54.Kohrt WM, Malley MT, Coggan AR, et al. Effects of gender, age, and fitness level on response of VO2max to training in 60–71 yr olds. Journal of Applied Physiology. 1991;71(5):2004–2011. doi: 10.1152/jappl.1991.71.5.2004. [DOI] [PubMed] [Google Scholar]
- 55.Lortie G, Simoneau JA, Hamel P, Boulay MR, Landry F, Bouchard C. Responses of maximal aerobic power and capacity to aerobic training. International Journal of Sports Medicine. 1984;5(5):232–236. doi: 10.1055/s-2008-1025911. [DOI] [PubMed] [Google Scholar]
- 56.Skinner JS, Jaskólski A, Jaskólska A, et al. Age, sex, race, initial fitness, and response to training: the HERITAGE Family Study. Journal of Applied Physiology. 2001;90(5):1770–1776. doi: 10.1152/jappl.2001.90.5.1770. [DOI] [PubMed] [Google Scholar]
- 57.Hansen D, Dendale P, Berger J, Meeusen R. Rehabilitation in cardiac patients: what do we know about training modalities? Sports Medicine. 2005;35(12):1063–1084. doi: 10.2165/00007256-200535120-00005. [DOI] [PubMed] [Google Scholar]
- 58.Bouchard C, Rankinen T. Individual differences in response to regular physical activity. Medicine and Science in Sports and Exercise. 2001;33(6):S446–S451. doi: 10.1097/00005768-200106001-00013. [DOI] [PubMed] [Google Scholar]
- 59.Skinner JS, Gaskill SE, Rankinen T, et al. Heart rate versus %VO2max: age, sex, race, initial fitness, and training response—HERITAGE. Medicine and Science in Sports and Exercise. 2003;35(11):1908–1913. doi: 10.1249/01.MSS.0000093607.57995.E3. [DOI] [PubMed] [Google Scholar]
- 60.Jakicic JM, Donnelly JE, Pronk NP, Jawad AF, Jacobsen DJ. Prescription of exercise intensity for the obese patient: the relationship between heart rate, VO2 and perceived exertion. International Journal of Obesity. 1995;19(6):382–387. [PubMed] [Google Scholar]
- 61.Okita K, Yonezawa K, Nishijima H, et al. Skeletal muscle metabolism limits exercise capacity in patients with chronic heart failure. Circulation. 1998;98(18):1886–1891. doi: 10.1161/01.cir.98.18.1886. [DOI] [PubMed] [Google Scholar]
- 62.Meyer T, Lucía A, Earnest CP, Kindermann W. A conceptual framework for performance diagnosis and training prescription from submaximal gas exchange parameters—theory and application. International Journal of Sports Medicine. 2005;26(1):S38–S48. doi: 10.1055/s-2004-830514. [DOI] [PubMed] [Google Scholar]
- 63.Salvadego D, Lazzer S, Busti C, et al. Gas exchange kinetics in obese adolescents. Inferences on exercise tolerance and prescription. American Journal of Physiology. 2010;299(5):R1298–R1305. doi: 10.1152/ajpregu.00038.2010. [DOI] [PubMed] [Google Scholar]
- 64.Davis HA, Bassett J, Hughes P, Gass GC. Anaerobic threshold and lactate turnpoint. European Journal of Applied Physiology and Occupational Physiology. 1983;50(3):383–392. doi: 10.1007/BF00423244. [DOI] [PubMed] [Google Scholar]
- 65.Hofmann P, Leitner H, Gaisl G. Heart rate threshold, lactate turn point andanaerobic threshold determination by electromyography. Hungarian Review of Sports Medicine. 1992;33(1):13–20. [Google Scholar]
- 66.Hofmann P, Pokan R, Preidler K, et al. Relationship between heart rate threshold, lactate turn point and myocardial function. International Journal of Sports Medicine. 1994;15(5):232–237. doi: 10.1055/s-2007-1021052. [DOI] [PubMed] [Google Scholar]
- 67.Hofmann P, Bunc V, Leitner H, Pokan R, Gaisl G. Heart rate threshold related to lactate turn point and steady-state exercise on a cycle ergometer. European Journal of Applied Physiology and Occupational Physiology. 1994;69(2):132–139. doi: 10.1007/BF00609405. [DOI] [PubMed] [Google Scholar]
- 68.Aunola S, Rusko H. Does anaerobic threshold correlate with maximal lactate steady-state? Journal of Sports Sciences. 1992;10(4):309–323. doi: 10.1080/02640419208729931. [DOI] [PubMed] [Google Scholar]
- 69.Skinner JS, McLellan TH. The transition from aerobic to anaerobic metabolism. Research Quarterly for Exercise and Sport. 1980;51(1):234–248. doi: 10.1080/02701367.1980.10609285. [DOI] [PubMed] [Google Scholar]
- 70.Wasserman K, McIlroy MB. Detecting the threshold of anaerobic metabolism in cardiac patients during exercise. The American Journal of Cardiology. 1964;14(6):844–852. doi: 10.1016/0002-9149(64)90012-8. [DOI] [PubMed] [Google Scholar]
- 71.Hofmann P, Jürimäe T, Jürimäe J, et al. HRTP, prolonged ergometer exercise, and single sculling. International Journal of Sports Medicine. 2007;28(11):964–969. doi: 10.1055/s-2007-965074. [DOI] [PubMed] [Google Scholar]
- 72.Hashimoto T, Brooks GA. Mitochondrial lactate oxidation complex and an adaptive role for lactate production. Medicine and Science in Sports and Exercise. 2008;40(3):486–494. doi: 10.1249/MSS.0b013e31815fcb04. [DOI] [PubMed] [Google Scholar]
- 73.Brooks GA. Cell-cell and intracellular lactate shuttles. Journal of Physiology. 2009;587(23):5591–5600. doi: 10.1113/jphysiol.2009.178350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Lamprecht M, Greilberger JF, Schwaberger G, Hofmann P, Oettl K. Single bouts of exercise affect albumin redox state and carbonyl groups on plasma protein of trained men in a workload-dependent manner. Journal of Applied Physiology. 2008;104(6):1611–1617. doi: 10.1152/japplphysiol.01325.2007. [DOI] [PubMed] [Google Scholar]
- 75.Jürimäe J, Hofmann P, Jürimäe T, et al. Plasma ghrelin responses to acute sculling exercises in elite male rowers. European Journal of Applied Physiology. 2007;99(5):467–474. doi: 10.1007/s00421-006-0370-y. [DOI] [PubMed] [Google Scholar]
- 76.Wonisch M, Hofmann P, Fruhwald FM, et al. Effect of β-selective adrenergic blockade on maximal blood lactate steady state in healthy men. European Journal of Applied Physiology. 2002;87(1):66–71. doi: 10.1007/s00421-002-0595-3. [DOI] [PubMed] [Google Scholar]
- 77.Tschakert, G, Groeschl W, Schwaberger G, Von Duvillard SP, Hofmann P. Prescription for aerobic high-intensity interval training by means of incremental exercisetests markers. Medicine and Science in Sports and Exercise. 2009;41(supplement 5):p. 430. [Google Scholar]