Abstract
Compared to bone marrow (BM) derived mesenchymal stem cells (MSCs) from human origin or from other species, the in vitro expansion and purification of murine MSCs (mMSCs) is much more difficult because of the low MSC yield and the unwanted growth of non-MSCs in the in vitro expansion cultures. We describe a modified protocol to isolate and expand murine BM derived MSCs based on the combination of mechanical crushing and collagenase digestion at the moment of harvest, followed by an immunodepletion step using microbeads coated with CD11b, CD45 and CD34 antibodies. The number of isolated mMSCs as estimated by colony forming unit-fibroblast (CFU-F) assay showed that this modified isolation method could yield 70.0% more primary colonies. After immunodepletion, a homogenous mMSC population could already be obtained after two passages. Immunodepleted mMSCs (ID-mMSCs) are uniformly positive for stem cell antigen-1 (Sca-1), CD90, CD105 and CD73 cell surface markers, but negative for the hematopoietic surface markers CD14, CD34 and CD45. Moreover the immunodepleted cell population exhibits more differentiation potential into adipogenic, osteogenic and chondrogenic lineages. Our data illustrate the development of an efficient and reliable expansion protocol increasing the yield and purity of mMSCs and reducing the overall expansion time.
1. Introduction
Mesenchymal stem cells are self-renewing and multipotent progenitors that can differentiate into a variety of cell types, including adipocytes, osteoblasts, chondrocytes, myocytes, hepatocytes, cardiomyocytes, neurons, and beta-pancreatic islets cells [1–4].BM is the most common source of MSCs. However, MSCs have also been isolated from various other sources, namely, placenta, amniotic fluid, cord blood, fetal liver, and adipose tissue [5–9]. MSCs have been referred by other terminology such as colony-forming fibroblastic cells, marrow stromal stem cells, and mesenchymal progenitor cells [10–12]. At present, MSCs are reported to possess, besides their multipotent differentiation capacity, also other properties such as low immunogenicity and tissue-homing ability making them an attractive tool for cell-mediated therapy in several diseases processes, including tissue injury and tissue degeneration as well as graft-versus-host disease [13–16].
MSCs have been successfully isolated and characterized from BM samples of many species including human, rabbit, rat, sheep, goat, rhesus monkeys, dog, and pig through their preferential attachment to tissue culture plastic [17–25]. In contrast, the isolation and purification of mMSCs from BM has been more difficult than that from human and other species whose marrow adherent cells are relatively homogenous and contain a high percentage of MSCs. The future use of MSCs for human disease therapies depends on the establishment of representative and efficient preclinical animal models. In many respects, a murine model is an ideal model to study the cell biology and the therapeutic potential of MSCs. The standard method of plastic adherence has, however, proven ineffective to yield relatively pure mMSCs populations since various hematopoietic cell lineages survive and/or proliferate on stromal layers, even in the absence of exogenous cytokines [26]. The majority of the contaminated hematopoietic cells can be removed after a prolonged expansion time by frequent subculturing. The MSCs differentiation potentials might, however, decrease during long-term in vitro culture. In addition, several reports suggest that mMSCs can undergo spontaneous transformation following long term in vitro culture [27–29]. So far, several techniques have been described to reduce or eliminate non-MSCs from plastic adherent murine BM cultures, including the use of low-density culture, frequent medium change, and positive and negative selection [30–37]. However, none of these techniques has gained widespread acceptance so far. It is, therefore, still necessary to develop a standardized, reliable, and easy-to-perform method to obtain high amounts of purified mMSCs, but with reduced expansion time to avoid possible transformation and to retain the differentiation potential of the expanded stem cells. Our present study aimed to develop an improved method to increase the yield and purity of culture-expanded mMSCs.
2. Materials and Methods
2.1. mMSCs Modified Harvest and Primary Culture
C57BL/KaLwRij mice (Harlan CPB, The Netherlands), 6–8 weeks old, were sacrificed by cervical dislocation. The hind legs and vertebrae were dissected and carefully cleaned from adherent tissues. The standard accepted isolation for BM-derived MSCs was to flush BM cells from hind legs [38]. Here, we modified the harvest protocol. After the tips of each bone were removed and the BM was collected by flushing out the content of femurs and tibias with RPMI 1640 (Lonza, Verviers, Belgium), we further chopped the femurs, tibias and vertebrae into fine pieces (1-2 mm) with a scalpel and crushed gently with the back side of a 5-ml syringe in RPMI 1640. Next, the bone fragments were transferred into a 50 ml polypropylene tube with 10 ml 0.25% Collagenase A solution (Roche Diagnostics GmbH, Mannheim, Germany). The tube with bone fragments and Collagenase A solution was placed in 37°C water bath for 30 minutes. Next phosphate buffered saline (PBS) was added to a final volume of 30 ml. When the fragments were settled, supernatant was collected, mixed with the previously harvested cells, and filtered through 70-μm nylon mesh filter. Cells were then washed twice with PBS, and subsequently nucleated and viable cells were counted in a hemocytometer using 3% Acetic acid with Crystal Violet and Trypan Blue, respectively. Cells were plated at 1 × 106 cells/cm2 in McCoy's 5A media (Lonza, Verviers, Belgium) containing 20% mesenchymal stem cell stimulatory supplements for mouse (Stem Cell Technologies, Vancouver, BC, Canada), 1% L-glutamine(Lonza, Verviers, Belgium), and 1% penicillin/streptomycin (Lonza, Verviers, Belgium). The culture was kept in a humidified 5% CO2 incubator at 37°C for 24–48 hours, followed by removal of nonadherent cells with PBS and replacement with fresh complete medium. All of the procedures involving mice were approved by the Ethical Committee for Animal Experiments, VUB (license no. LA1230281).
2.2. Increasing the Purity of in Vitro Expanded mMSCs by Immunodepletion and mMSCs Subculture
After about 7–10 days, when primary cultures (passage 0) became nearly confluent, the cells were detached with 0.25% trypsin/0.02% EDTA for 5 minutes at 37°C. The residual cells which were not detached within 5 minutes were collected by gentle scraping using a cell scraper. The cells were resuspended in 1 ml 0.1%BSA/PBS, followed by an immunodepletion using anti-CD11b, CD34, CD45-conjugated Dynabeads M-280 Streptavidin superparamagnetic polystyrene beads (In vitrogen Dynal AS, Oslo, Norway) according to the manufacturer's instruction. In brief, Dynabeads were washed with 0.1%BSA/PBS for 5 times and then precoated with the following biotinylated antibodies, respectively, at appropriate concentration (5–10 μg antibodies per mg Dynabeads M-280 streptavidin) by incubation for 30 minutes at room temperature using gentle rotation: Biotin antimouse CD11b, CD34 and CD45 (eBioscience, San Diego, USA). Three consecutive rounds of immunodepletion using antibodies against CD11b, CD34 and CD45, respectively, were performed for depleting contaminated non-MSCs. In each case, cells and antibody conjugated Dynabeads were thoroughly mixed at a ratio of 1 cell: 5 beads and incubated on the rotator for 30 minutes at 4°C. Then, cells were washed using a Dynal MPC to remove unbound cells. The immunodepleted cells were suspended in complete medium, plated in one T-25 flask at 1000 cells/cm2 (Nunc, VWR International, Leuven, Belgium) followed by incubation in a 37°C with 5% CO2 humidified incubator. Culture medium was changed every 3-4 days until cell culture reached 80%–90% confluence. At that point cells were trypsinized (passage 1) and plated in one T-75 flask at 1000 cells/cm2. Subsequent passages were performed similarly, but split ratios were 1 : 2 (T-75 flask).
2.3. CFU-F Assay
The CFU-F assay was performed as described previously [39]. In brief, 1 × 106 nucleated cells obtained from fresh BM were plated into each well of a six-well plate and incubated for 10 days in humidified atmosphere (37°C, 5% CO2). Culture medium was changed on days 3 and 8 of culture. Subsequently, cultures were fixed and stained with Giemsa. The number of colonies displaying five or more cells with spindled mMSCs morphology was scored under an inverted microscope. Colonies whose morphology clearly differed from the mMSC morphology were excluded from the results. This assay was performed using BM samples from 10 mice (for 5 mice, cells were isolated using Collagenase, while for 5 other mice cells were isolated without Collagenase). Each sample was analyzed in triplicate.
2.4. Growth Curve and Doubling Time
Passage 1 mMSCs were plated in 6-well culture plates at 2000 cells/well in medium with 20% mesenchymal stem cell stimulatory supplements or 10% fetal bovine serum (FBS). The cells from each well were trypsinized and counted in duplicate with a hemocytometer every two days until day 12. The doubling time was calculated according to the equation: TD = t × lg2/lg(Nt/N0), where N0 is the initial cell number, Nt is the end point cell number, and t is time interval.
2.5. Flow Cytometry Analysis
mMSCs were detached from the culture dish using 0.25% trypsin/0.02% EDTA, and 1 × 105 mMSCs were washed by 4%HuAlb/PBS and pelleted by centrifugation for 3 minutes at 400 g. The cells were stained with rat anti-mouse CD14, CD34, CD105, Sca-1, CD45, CD90 (all purchased from eBioscience, San Diego, USA), and CD73 (PharMingen, San Diego, USA), at a concentration of 2 μg/ml at 4°C. The cells stained with corresponding rat anti-mouse IgG served as negative controls. After 30 minutes, unbound antibody was washed with 2 ml 1%HuAlb/PBS. Next, the cells were incubated with 10 μL mouse antirat fluorescein isothiocyanate (FITC) antibody at 4°C for 30 minutes followed by a wash with 2 ml 1%HuAlb/PBS. The cell pellets were resuspended in 600 μl PBS and examined by flow cytometry (Coulter Epics XL-MCL, Brussels, Belgium) with 5,000 events being recorded for each condition. The results were analyzed by cell quest software and WinMDI 2.8 software was used to create the histograms.
2.6. Differentiation Assays
2.6.1. Adipogenic Differentiation
For adipogenic differentiation, 2 × 105 P3 mMSCs were seeded into a well of a 6-well plate (Nunc, VWR International, Leuven, Belgium) and fed every 2-3 days by replacing the complete medium until a confluent cell layer was formed. Then cells, were stimulated to differentiate into the adipogenic lineage by submitting them to three cycles of alternating culture in adipogenic induction medium (LONZA, Walkersville, USA) and adipogenic maintenance medium (LONZA, Walkersville, USA) according to the manufacturer's instructions. The adipogenic induction medium contains according to the manufacture Insulin (recombinant), L-glutamine, MCGS, dexamethasone, indomethacin, IBMX (3-isobuty-l-methyl-xanthine), and Pen/Strep, while the the Adipogenic Maintenance Medium includes insulin (recombinant), L-Glutamine, MCGS, and pen/strep. At the end of these cycles, cells were grown for another 7 days in adipogenic maintenance medium. As a control MSC were grown in Adipogenic Maintenance Medium only to exclude spontaneous adipogenic differentiation. To visualize adipocytes, cells were stained with Oil Red O (Sigma, Bornem, Belgium) [40].
2.6.2. Osteogenic Differentiation
Osteogenic differentiation was induced by exposing 3 × 104 P3 mMSCs to osteogenic induction medium (LONZA, Walkersville, USA) into a well of a 6-well plate. The medium was changed every 3 to 4 days. As a negative control, cells were cultured in complete medium and medium was changed at the same frequency as that for the differentiating MSC. The osteogenic induction medium contains according to the manufacturer dexamethasone, L-Glutamine, ascorbate, Pen/Strep, MCGS, and glycerophosphate. To verify osteogenic differentiation, von Kossa's method was used to stain calcium deposits [41].
2.6.3. Chondrogenic Differentiation
In order to induce chondrogenic differentiation 2.5 × 105 P3 mMSCs were washed twice in incomplete chondrogenesis induction medium (LONZA, Walkersville, USA). Cells were then sedimented by centrifugation at 150 g for 5 minutes and 0.5 mL complete chondrogenesis induction medium (LONZA, Walkersville, USA) was added to the cell pellet. Incomplete chondrogenesis induction medium contains according to the manufacturer dexamethasone, ascorbate, ITS + supplement, pen/strep, sodium pyruvate, Proline and L-Glutamine. Complete medium was made by adding 5 μL TGFβ3 (LONZA, Walkersville, USA) to 1 mL incomplete medium. The medium was changed every 3 to 4 days. After 21 days of culture, the pellets were embedded in paraffin, cut into 4 μm sections and immunohistochemically stained by A rabbit polyclonal anticollagen II antibody (NCL-COLL-IIp, NovoCastra, Prosan, Merelbeke, Belgium).
2.7. Statistical Analysis
Statistical significance was assessed by comparing mean values (±SD) using Mann Whitney test. P < .05 were considered statistically significant.
3. Results
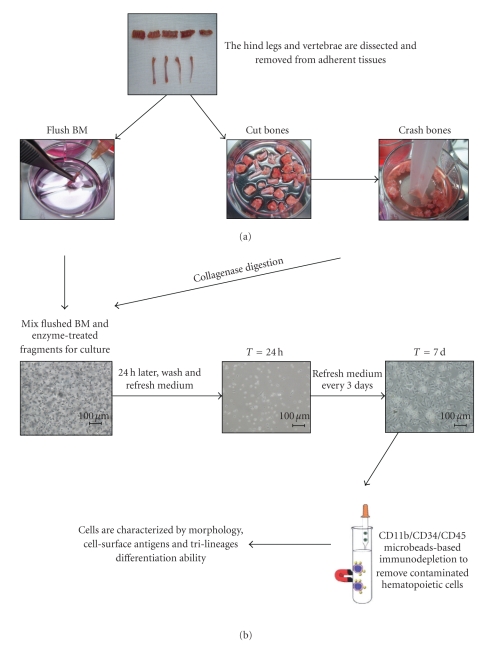
As shown in the flow chart (Figure 1), the isolation and expansion method of BM-derived mMSCs includes a combination of mechanical bone crushing, enzymatic treatment of bone fragments, and flushing out BM cells at the harvest step with immunodepletion of CD11b+, CD34+, and CD45+ cells in the following culture step.
Figure 1.
Flow chart for our modified harvest and expansion protocol. (a) Mice were sacrificed by cervical dislocation. The hind legs and vertebrae were dissected and carefully removed from adherent tissues. The BM was collected by flushing out the content of femurs and tibias with RPMI 1640. Next, the femurs, tibias, and vertebrae were cutted into small pieces and crushed gently. Next, the bone fragments were incubated with 0.25% Collagenase A solution in 37°C water bath for 30 minutes. (b) Collagenase-treated bone fragments were mixed with the previously flushed BM cells, filtered through 70-μm nylon mesh filter and cultured at 1 × 106 cells/cm2. At 24 h after initial culture, the nonadherent cells were washed away. After about 7–10 days, when primary cultures became nearly confluent, the cells were trypsinized, followed by a CD11b/CD34/CD45 negative immunodepletion in order to remove contaminated hematopoietic cells. The immunodepleted cells were cultivated and characterized at the level of their morphology, immunophenotype, and differentiation potentials. Scale bar = 100 μm.
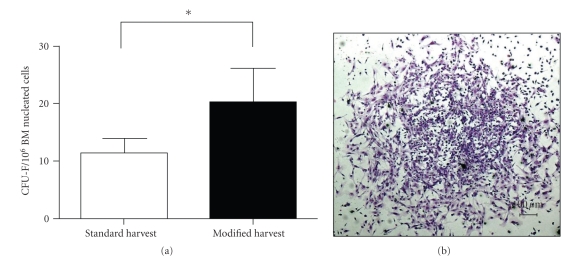
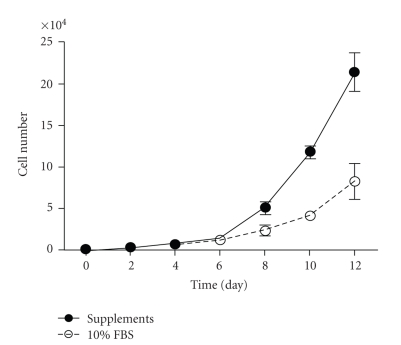
The number of BM-nucleated cells harvested with the modified method was 19.4% higher than the number of BM nucleated cells obtained by the standard method although this difference was not significant (data not shown). However, with the modified harvest method, the mean number of colonies was 70.0% more than the mean number of colonies obtained by the standard method (P < .05) (Figure 2(a)). The number of colonies displaying five or more cells was scored under an inverted microscope (Figure 2(c)). Colonies with four cells were counted when one of them presented two nuclei. Colonies whose morphology clearly differed from the mMSC morphology were excluded from the results. We compared medium with fetal bovine serum (FBS) to medium with mesenchymal stem cell stimulatory supplements (mouse) from Stem cell technologies and found that cells cultured with Mesenchymal Stem Cell Stimulatory Supplements showed a higher proliferation rate (Figure 3).
Figure 2.
Optimized isolation of murine BM derived MSCs. (a) In the CFU-F assay, 70.0% more colonies are observed with the modified isolation method, n = 6/group. *P < .05 (b) One representative colony in CFU-F assay (Giemsa staning, ×40), scale bar = 100 μm.
Figure 3.
Comparison proliferation rate in medium with fetal bovine serum versus mesenchymal stem cell stimulatory supplements. Passage 1 cells show a higher growth rate in medium with mesenchymal stem cell stimulatory supplements as compared to the proliferation rate observed in medium with the 10% FBS. The values are expressed as means ± SD of 3 independent measurements.
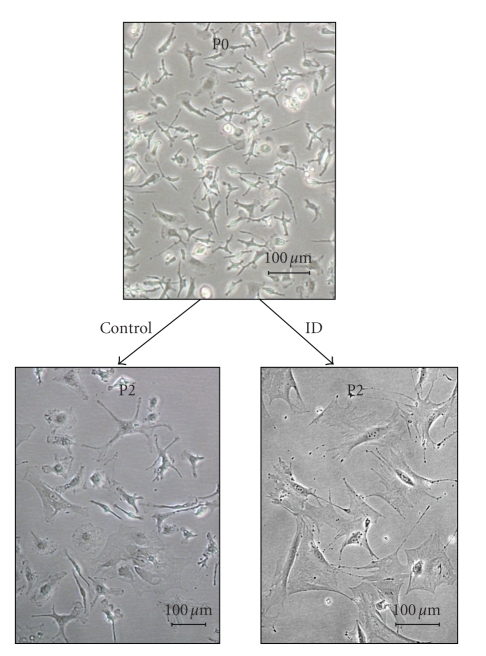
Using the standard expansion conditions, cultures usually remained morphologically heterogeneous at passage 2, presenting round, polygonal, spindle-shaped, and flattened cells (Figure 4). Some degree of morphological heterogeneity could still be observed up to passage 6–8 (data not shown). However, using the immunodepletion step, much less heterogeneity could be observed, and at passage 2, a homogeneous population of spindle-shaped cells could be observed. The doubling time of ID-mMSCs was found to be 46.9 ± 1.78 h.
Figure 4.
Morphology of cultured mouse BM cells. Seven days post harvest CD11b/CD34/CD45 immunodepletion was performed. Cultured cells already appeared homogeneous already at passage 2 while controls remain heterogeneous (×100). Representative pictures are shown, n = 6/group, scale bar = 100 μm.
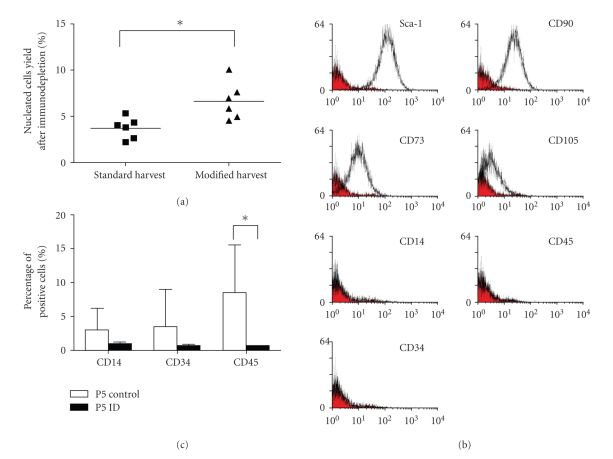
We further investigated whether the two different harvest methods had an effect on the yields of ID-mMSCs. The result showed that using the same immunodepletion procedure, the ID-mMSC yield with the standard isolation method was 3.7%, while the yield with the modified isolation method could reach up to 6.6% (Figure 5(a)), confirming that our modified isolation method results in a higher mMSC harvest.
Figure 5.
Cell-surface antigens on mMSCs. (a) The yield of ID-mMSCs with modified isolation method is 78.3% higher as compared to the standard isolation methold, n = 6/group, *P < .05. (b) A representative phenotype of ID-mMSCs from 6 donors at passage 3. Plots show isotype control IgG staining profile (red) versus specific Ab staining profile (white). (c) Contaminated heamatopoietic cells still can be detected in the nonimmunodepleted MSC fraction showing CD14, CD34, and CD45 expression at passage 5, n = 6/group, *P < .05.
The cells (cultured with and without immunodepletion) were further analyzed for cell surface antigens at passage 3. Results showed that ID-mMSCs were strongly positive for CD90, CD73 and Sca-1, but totally negative for CD14, CD34, and CD45 (Figure 5(b)). The cell population cultured without immunodepletion showed significantly less expression of CD90, CD73, and Sca-1 but more expression of CD45 compared with ID-mMSCs (Figure 5(c)). Without immunodepletion mMSCs still seemed to be contaminated with hematopoietic cells after 5-6 passages, which was consistent with the morphological observations.
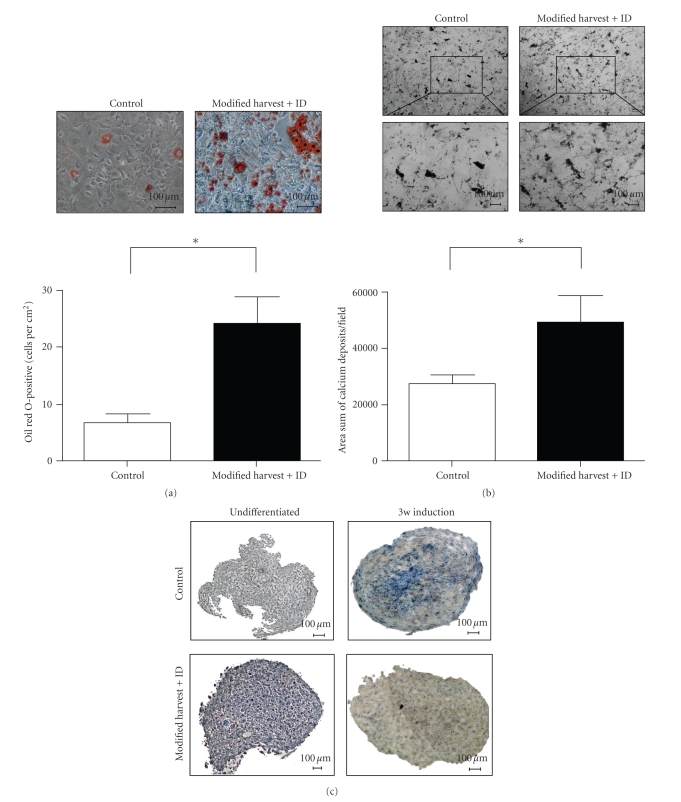
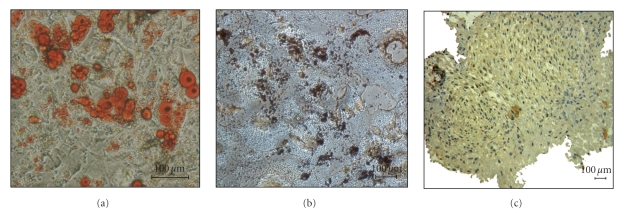
Tri-lineage differentiation abilities of cells cultured with and without immunodepletion were tested at passage 3. When cultured in adipogenic, osteogenic, and chondrogenic media, cells were able to differentiate exclusively into adipocytes, osteoblasts, and chondrocytes as determined by Oil Red O, von Kossa and type II collagen staining, respectively. However, the differentiation abilities were significantly different. The extent of adipogenic differentiation was quantified by counting Oil red O-positive cells per cm2. As shown in Figure 6(a), the amount of Oil red O-positive cells in the immunodepleted group was significantly higher than that of the control group. When osteogenic differentiation was examined using a bone nodule formation assay, von Kossa staining revealed that cells cultured after immunodepletion produced significantly more calcium nodules than cells cultured without immunodepletion (Figure 6(b)). In accordance, chondrogenic differentiation of ID-cells was more pronounced compared to control cells (Figure 6(c)). These data indicate that a higher purity of multipotent mouse MSCs can be achieved after immunodepletion of CD11b, CD34, and CD45 positive cells. Moreover, we observed that late passage ID-mMSCs (at passage 8) retained their robust capacity to differentiate into adipocytes, osteoblasts, and chondrocytes (Figure 7).
Figure 6.
In vitro differentiation of mMSCs. The same amount of nonimmunodepleted mMSCs and ID-mMSCs were plated and adipogenic, osteogenic, and chondrogenic differentiation was evaluated at passage 3. Oil Red O staining ((a), ×200), von Kossa staining ((b), ×40 or ×100) and collagen type II staining ((c), ×100) show that ID-mMSCs exhibit much more differentiated cells, indicating a higher purity of multipotent MSCs with modified harvest method and immunodepletion. Representative pictures are shown from three independent experiments. *P < .05, scale bar = 100 μm.
Figure 7.
Late passage ID-mMSCs retain tri-lineage differentiation potential. When exposed in induction medium, passage 8 ID-mMSCs can still exhibit differentiation potential into adipocytes, osteoblasts, and chondrocytes, as shown by Oil Red O staining ((a) ×200), von Kossa staining ((b) ×100) and collagen type II staining ((c) ×100). Representative pictures are shown from three independent experiments, scale bar = 100 μm.
4. Discussion
Mesenchymal stem cells (MSCs) have generated a great deal of interest and promise as a potential source of cells for cell-based therapeutic strategies for tissue repair and regenerative diseases, primarily owing to their intrinsic ability to self renew and differentiate into functional cell types that constitute the tissue in which they exist. At present, there is also a great interest for genetically modified MSCs in cell-based therapy for cancers based on the rationale of tumor-homing properties of MSCs. However, most of MSC therapeutic applications are still in preclinical studies.
Friedenstein and his colleagues firstly established MSCs culture from guinea pig by virtue of MSCs preferential attachment to plastic flasks [38], and the original method has been further used for the culture BM MSCs from human and other experimental animals [17–22]. This method has, however, proven inefficient for mMSCs due to low mMSCs number and contamination of hematopoietic cells in the cultures. To solve this problem, many groups have developed various modified mMSCs culture conditions to obtain sufficient numbers of cells in the shortest time and with the highest homogeneity. Kopen et al. firstly developed a method to eliminate myelopoietic cells using an anti-CD11b antibody, but this protocol could not deplete all the hematopoietic cells [33]. Baddoo et al. presented a modified purification approach based on immunodepletion of CD11b/CD34/CD45 positive cells from cultured BM cells [34]. In one study, positive selection was performed in an attempt to obtain a more homogeneous mMSCs population [32]. But since there is no specific marker for MSCs, other non-MSCs were unavoidable introduced into the cultures. Moreover, several other techniques, including optimization of culture density and frequent medium change, have also been proposed but these protocols are not standardized [30, 31]. Therefore, it remains necessary to develop a reliable and easy method to isolate and expand a homogeneous population of mMSCs from mouse BM.
The standard method that is used for isolation of murine BM-derived MSCs is to flush BM cells from hind legs of mice. However, with this method, the frequency of collected MSCs is rather low [42]. Our harvest method involves not only flushing out BM cells, but also crushing the bones of hind legs and vertebrae as well as enzymatical treatment of the bones with Collagenase (Figure 1(a)). Stromal cells are present in the endosteum whereas mature hematopoietic cells exist in the center of the BM [43, 44]. Because of this deep location, it is difficult to obtain enough MSCs even after strong flushing during marrow cell harvest. In this study, using the modified isolation method, we could isolate 19.4% more BM-nucleated cells than the standard method. CFU-F assay, which was used to detect and evaluate the frequency of the MSCs in fresh BM, has furthermore been used to validate the effectiveness of this modified method (Figures 2(b) and 2(c)).
After harvesting BM with our modified protocol, we performed magnetic cell sorting after the first passage using negative selection with CD11b/CD34/CD45 antibodies-coupled microbeads as proposed by Baddoo et al. [34] (Figure 1(b)). Two consecutive rounds of immunodepletion, removing respectively CD11b-positive monocytic cells and CD34-positive hematopoietic stem cells can deplete the major part of contaminated cells, and the third round of CD45-positive cells depletion could further eliminate all residual contaminated hematopoietic cells. We found that after immunodepletion the MSCs population appeared much more homogeneous showing mostly spindle-shaped, cells (Figure 4), while under the standard expansion conditions, cultures usually remained morphologically highly heterogeneous until passage 5-6, presenting round, polygonal, spindle-shaped and flattened cells. Some degree of morphological heterogeneity could still be observed up to passage 6–8 or more. Although the CD11b/CD34/CD45 immunodepletion protocol did remove almost all the contaminated hematopoietic cells from the BM cultures, we have to notice that the nucleated cell yield in our mouse strain was low after the immunodepletion step in combination with the standard harvest method (3.7% on average). However, we observed that after CD11b/CD34/CD45 immunodepletion in combination with our modified BM harvest method, the yield of nucleated cells was nearly twice higher (Figure 5(a)). The immunodepleted cells cultured up to passage 3 were positive for CD90, CD73, and Sca-1 but totally negative for CD14, CD34, and CD45 (Figure 5(b)), while control cells were still significantly contaminated with CD45+ cells and slightly contaminated with CD14+ and CD34+ cells (Figure 5(c)). In addition to morphology and phenotype, the biological property that uniquely identifies MSCs is their capacity for tri-lineage mesenchymal differentiation. So, we further tested the tri-lineage differentiation ability of ID-mMSCs and control cells at passage 3. ID-mMSCs and control cells were both able to differentiate into adipocytes, osteoblasts, and chondrocytes determined by Oil Red O, von Kossa and type II collagen staining when exposed to respectively adipogenic, osteogenic, and chondrogenic media. However, with the same initial cell numbers and induction conditions, ID-mMSCs exhibited a more vigorous tri-lineage differentiation potential as compared to the control cells (Figure 6) and can retain their robust differentiation potential at least until passage 8 (Figure 7). Based on the morphology, phenotype, and differentiation potential in vitro, we can conclude that immunodepleted mMSCs are more purified in the early passages.
5. Conclusion
Taken together, the current study presents an effective, quick and easy-to-perform method for enrichment and purification of murine BM derived mesenchymal stem cells in vitro by combining mechanical crushing and Collagenase treatment at the moment of harvest and a negative immunodepletion step during the in vitro expansion culture. This protocol can facilitate the in vitro and in vivo study of mMSCs, both for examining their biological properties as well as their therapeutic potential in various murine disease models.
Acknowlegments
The authors would like to thank Nicole Arras, Angelo Willems, Veerle De Greef, and Wim Renmans for their expert technical assistance. Their research work is supported by grants from the Foundation for Scientific Research (FWO), the Vrije Universiteit Brussel (HOA), the “Vlaamse Liga tegen Kanker” Belgium. S. Xu is supported by a CSC-VUB scholarship.
Conflicts of Interests
No conflicting financial interests exist.
References
- 1.Pittenger MF, Mackay AM, Beck SC, et al. Multilineage potential of adult human mesenchymal stem cells. Science. 1999;284(5411):143–147. doi: 10.1126/science.284.5411.143. [DOI] [PubMed] [Google Scholar]
- 2.Kang X-Q, Zang W-J, Song T-S, et al. Rat bone marrow mesenchymal stem cells differentiate into hepatocytes in vitro. World Journal of Gastroenterology. 2005;11(22):3479–3484. doi: 10.3748/wjg.v11.i22.3479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sanchez-Ramos JR. Neural cells derived from adult bone marrow and umbilical cord blood. Journal of Neuroscience Research. 2002;69(6):880–893. doi: 10.1002/jnr.10337. [DOI] [PubMed] [Google Scholar]
- 4.Chen L-B, Jiang X-B, Yang L. Differentiation of rat marrow mesenchymal stem cells into pancreatic islet beta-cells. World Journal of Gastroenterology. 2004;10(20):3016–3020. doi: 10.3748/wjg.v10.i20.3016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.In’t Anker PS, Scherjon SA, Kleijburg-Van Der Keur C, et al. Isolation of mesenchymal stem cells of fetal or maternal origin from human placenta. Stem Cells. 2004;22(7):1338–1345. doi: 10.1634/stemcells.2004-0058. [DOI] [PubMed] [Google Scholar]
- 6.In ’t Anker PS, Scherjon SA, Kleijburg-van der Keur C, et al. Amniotic fluid as a novel source of mesenchymal stem cells for therapeutic transplantation. Blood. 2003;102(4):1548–1549. doi: 10.1182/blood-2003-04-1291. [DOI] [PubMed] [Google Scholar]
- 7.Erices A, Conget P, Minguell JJ. Mesenchymal progenitor cells in human umbilical cord blood. British Journal of Haematology. 2000;109(1):235–242. doi: 10.1046/j.1365-2141.2000.01986.x. [DOI] [PubMed] [Google Scholar]
- 8.Zuk PA, Zhu M, Ashjian P, et al. Human adipose tissue is a source of multipotent stem cells. Molecular Biology of the Cell. 2002;13(12):4279–4295. doi: 10.1091/mbc.E02-02-0105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Campagnoli C, Roberts IAG, Kumar S, Bennett PR, Bellantuono I, Fisk NM. Identification of mesenchymal stem/progenitor cells in human first-trimester fetal blood, liver, and bone marrow. Blood. 2001;98(8):2396–2402. doi: 10.1182/blood.v98.8.2396. [DOI] [PubMed] [Google Scholar]
- 10.Friedenstein AJ, Gorskaja UF, Kulagina NN. Fibroblast precursors in normal and irradiated mouse hematopoietic organs. Experimental Hematology. 1976;4(5):267–274. [PubMed] [Google Scholar]
- 11.Bianco P, Riminucci M, Gronthos S, Robey PG. Bone marrow stromal stem cells: nature, biology, and potential applications. Stem Cells. 2001;19(3):180–192. doi: 10.1634/stemcells.19-3-180. [DOI] [PubMed] [Google Scholar]
- 12.Sun S, Guo Z, Xiao X, et al. Isolation of mouse marrow mesenchymal progenitors by a novel and reliable method. Stem Cells. 2003;21(5):527–535. doi: 10.1634/stemcells.21-5-527. [DOI] [PubMed] [Google Scholar]
- 13.Tang YL. Autologous mesenchymal stem cells for post-ischemic myocardial repair. Methods in molecular medicine. 2005;112:183–192. doi: 10.1385/1-59259-879-x:183. [DOI] [PubMed] [Google Scholar]
- 14.Le Blanc K, Rasmusson I, Sundberg B, et al. Treatment of severe acute graft-versus-host disease with third party haploidentical mesenchymal stem cells. Lancet. 2004;363(9419):1439–1441. doi: 10.1016/S0140-6736(04)16104-7. [DOI] [PubMed] [Google Scholar]
- 15.Kassem M, Abdallah BM. Human bone-marrow-derived mesenchymal stem cells: biological characteristics and potential role in therapy of degenerative diseases. Cell and Tissue Research. 2008;331(1):157–163. doi: 10.1007/s00441-007-0509-0. [DOI] [PubMed] [Google Scholar]
- 16.Nakamizo A, Marini F, Amano T, et al. Human bone marrow-derived mesenchymal stem cells in the treatment of gliomas. Cancer Research. 2005;65(8):3307–3318. doi: 10.1158/0008-5472.CAN-04-1874. [DOI] [PubMed] [Google Scholar]
- 17.Caterson EJ, Nesti LJ, Danielson KG, Tuan RS. Human marrow-derived mesenchymal progenitor cells: isolation, culture expansion, and analysis of differentiation. Molecular Biotechnology. 2002;20(3):245–256. doi: 10.1385/MB:20:3:245. [DOI] [PubMed] [Google Scholar]
- 18.Martin DR, Cox NR, Hathcock TL, Niemeyer GP, Baker HJ. Isolation and characterization of multipotential mesenchymal stem cells from feline bone marrow. Experimental Hematology. 2002;30(8):879–886. doi: 10.1016/s0301-472x(02)00864-0. [DOI] [PubMed] [Google Scholar]
- 19.Kadiyala S, Young RG, Thiede MA, Bruder SP. Culture expanded canine mesenchymal stem cells possess osteochondrogenic potential in vivo and in vitro. Cell Transplantation. 1997;6(2):125–134. doi: 10.1177/096368979700600206. [DOI] [PubMed] [Google Scholar]
- 20.Lennon DP, Caplan AI. Isolation of rat marrow-derived mesenchymal stem cells. Experimental Hematology. 2006;34(11):1606–1607. doi: 10.1016/j.exphem.2006.07.015. [DOI] [PubMed] [Google Scholar]
- 21.Jessop HL, Noble BS, Cryer A. The differentiation of a potential mesenchymal stem cell population within ovine bone marrow. Biochemical Society Transactions. 1994;22(3):p. 248S. doi: 10.1042/bst022248s. [DOI] [PubMed] [Google Scholar]
- 22.Izadpanah R, Joswig T, Tsien F, Dufour J, Kirijan JC, Bunnell BA. Characterization of multipotent mesenchymal stem cells from the bone marrow of rhesus macaques. Stem Cells and Development. 2005;14(4):440–451. doi: 10.1089/scd.2005.14.440. [DOI] [PubMed] [Google Scholar]
- 23.Ringe J, Kaps C, Schmitt B, et al. Porcine mesenchymal stem cells: induction of distinct mesenchymal cell lineages. Cell and Tissue Research. 2002;307(3):321–327. doi: 10.1007/s00441-002-0525-z. [DOI] [PubMed] [Google Scholar]
- 24.Wakitani S, Goto T, Pineda SJ, et al. Mesenchymal cell-based repair of large, full-thickness defects of articular cartilage. Journal of Bone and Joint Surgery A. 1994;76(4):579–592. doi: 10.2106/00004623-199404000-00013. [DOI] [PubMed] [Google Scholar]
- 25.Mosca JD, Hendricks JK, Buyaner D, et al. Mesenchymal stem cells as vehicles for gene delivery. Clinical Orthopaedics and Related Research. 2000;379(supplement):S71–S90. doi: 10.1097/00003086-200010001-00011. [DOI] [PubMed] [Google Scholar]
- 26.Da Silva Meirelles L, Nardi NB. Murine marrow-derived mesenchymal stem cell: isolation, in vitro expansion, and characterization. British Journal of Haematology. 2003;123(4):702–711. doi: 10.1046/j.1365-2141.2003.04669.x. [DOI] [PubMed] [Google Scholar]
- 27.Tolar J, Nauta AJ, Osborn MJ, et al. Sarcoma derived from cultured mesenchymal stem cells. Stem Cells. 2007;25(2):371–379. doi: 10.1634/stemcells.2005-0620. [DOI] [PubMed] [Google Scholar]
- 28.Aguilar S, Nye E, Chan J, et al. Murine but not human mesenchymal stem cells generate osteosarcoma-like lesions in the lung. Stem Cells. 2007;25(6):1586–1594. doi: 10.1634/stemcells.2006-0762. [DOI] [PubMed] [Google Scholar]
- 29.Li H, Fan X, Kovi RC, et al. Spontaneous expression of embryonic factors and p53 point mutations in aged mesenchymal stem cells: a model of age-related tumorigenesis in mice. Cancer Research. 2007;67(22):10889–10898. doi: 10.1158/0008-5472.CAN-07-2665. [DOI] [PubMed] [Google Scholar]
- 30.Eslaminejad MB, Nikmahzar A, Taghiyar L, Nadri S, Massumi M. Murine mesenchymal stem cells isolated by low density primary culture system. Development Growth and Differentiation. 2006;48(6):361–370. doi: 10.1111/j.1440-169X.2006.00874.x. [DOI] [PubMed] [Google Scholar]
- 31.Soleimani M, Nadri S. A protocol for isolation and culture of mesenchymal stem cells from mouse bone marrow. Nature Protocols. 2009;4(1):102–106. doi: 10.1038/nprot.2008.221. [DOI] [PubMed] [Google Scholar]
- 32.Nadri S, Soleimani M. Isolation murine mesenchymal stem cells by positive selection. In Vitro Cellular and Developmental Biology—Animal. 2007;43(8-9):276–282. doi: 10.1007/s11626-007-9041-5. [DOI] [PubMed] [Google Scholar]
- 33.Kopen GC, Prockop DJ, Phinney DG. Marrow stromal cells migrate throughout forebrain and cerebellum, and they differentiate into astrocytes after injection into neonatal mouse brains. Proceedings of the National Academy of Sciences of the United States of America. 1999;96(19):10711–10716. doi: 10.1073/pnas.96.19.10711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Baddoo M, Hill K, Wilkinson R, et al. Characterization of mesenchymal stem cells isolated from murine bone marrow by negative selection. Journal of Cellular Biochemistry. 2003;89(6):1235–1249. doi: 10.1002/jcb.10594. [DOI] [PubMed] [Google Scholar]
- 35.Eslaminejad MB, Nadri S. Murine mesenchymal stem cell isolated and expanded in low and high density culture system: surface antigen expression and osteogenic culture mineralization. In Vitro Cellular and Developmental Biology—Animal. 2009;45(8):451–459. doi: 10.1007/s11626-009-9198-1. [DOI] [PubMed] [Google Scholar]
- 36.Morikawa S, Mabuchi Y, Kubota Y, et al. Prospective identification, isolation, and systemic transplantation of multipotent mesenchymal stem cells in murine bone marrow. The Journal of experimental medicine. 2009;206(11):2483–2496. doi: 10.1084/jem.20091046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Short BJ, Brouard N, Simmons PJ. Prospective isolation of mesenchymal stem cells from mouse compact bone. Methods in Molecular Biology. 2009;482:259–268. doi: 10.1007/978-1-59745-060-7_16. [DOI] [PubMed] [Google Scholar]
- 38.Friedenstein AJ, Chailakhjan RK, Lalykina KS. The development of fibroblast colonies in monolayer cultures of guinea-pig bone marrow and spleen cells. Cell and Tissue Kinetics. 1970;3(4):393–403. doi: 10.1111/j.1365-2184.1970.tb00347.x. [DOI] [PubMed] [Google Scholar]
- 39.Castro-Malaspina H, Gay RE, Resnick G. Characterization of human bone marrow fibroblast colony-forming cells (CFU-F) and their progeny. Blood. 1980;56(2):289–301. [PubMed] [Google Scholar]
- 40.Sekiya I, Larson BL, Vuoristo JT, Cui J-G, Prockop DJ. Adipogenic differentiation of human adult stem cells from bone marrow stroma (MSCs) Journal of Bone and Mineral Research. 2004;19(2):256–264. doi: 10.1359/JBMR.0301220. [DOI] [PubMed] [Google Scholar]
- 41.Sheehan DC, Hrapchak BB. Theory and Practice of Histotechnology. 2nd edition. St. Louis, Mo, USA: Mosby; 1980. [Google Scholar]
- 42.Phinney DG, Kopen G, Isaacson RL, Prockop DJ. Plastic adherent stromal cells from the bone marrow of commonly used strains of inbred mice: variations in yield, growth, and differentiation. Journal of Cellular Biochemistry. 1999;72(4):570–585. [PubMed] [Google Scholar]
- 43.Fouillard L, Bensidhoum M, Bories D, et al. Engraftment of allogeneic mesenchymal stem cells in the bone marrow of a patient with severe idiopathic aplastic anemia improves stroma. Leukemia. 2003;17(2):474–476. doi: 10.1038/sj.leu.2402786. [DOI] [PubMed] [Google Scholar]
- 44.Short B, Brouard N, Driessen R, Simmons PJ. Prospective isolation of stromal progenitor cells from mouse BM. Cytotherapy. 2001;3(5):407–408. doi: 10.1080/146532401753277265. [DOI] [PubMed] [Google Scholar]