Abstract
Background
Although an increased risk for death after hip fracture is well established, whether this excess mortality persists over time is unclear.
Purpose
To determine the magnitude and duration of excess mortality after hip fracture in older men and women.
Data Sources
Electronic search of MEDLINE and EMBASE for English and non-English articles from 1957 to May 2009 and manual search of article references.
Study Selection
Prospective cohort studies were selected by 2 independent reviewers. The studies had to assess mortality in women (22 cohorts) or men (17 cohorts) aged 50 years or older with hip fracture, carry out a life-table analysis, and display the survival curves of the hip fracture group and age- and sex-matched control groups.
Data Extraction
Survival curve data and items relevant to study validity and generalizability were independently extracted by 2 reviewers.
Data Synthesis
Time-to-event meta-analyses showed that the relative hazard for all-cause mortality in the first 3 months after hip fracture was 5.75 (95% CI, 4.94 to 6.67) in women and 7.95 (CI, 6.13 to 10.30) in men. Relative hazards decreased substantially over time but did not return to rates seen in age- and sex-matched control groups. Through use of life-table methods, investigators estimated that white women having a hip fracture at age 80 years have excess annual mortality compared with white women of the same age without a fracture of 8%, 11%, 18%, and 22% at 1, 2, 5, and 10 years after injury, respectively. Men with a hip fracture at age 80 years have excess annual mortality of 18%, 22%, 26%, and 20% at 1, 2, 5, and 10 years after injury, respectively.
Limitations
Cohort studies varied, sometimes markedly, in size, duration of observation, selection of control populations, ascertainment of death, and adjustment for comorbid conditions. Only published data that displayed findings with survival curves were examined. Publication bias was possible.
Conclusion
Older adults have a 5- to 8-fold increased risk for all-cause mortality during the first 3 months after hip fracture. Excess annual mortality persists over time for both women and men, but at any given age, excess annual mortality after hip fracture is higher in men than in women.
Primary Funding Source
Fund for Scientific Research and Willy Gepts Foundation, Universitair Ziekenhuis Brussel.
Interest is increasing in quantifying the magnitude and duration of excess mortality after hip fractures for use in cost-effectiveness analyses of strategies for hip fracture prevention (1-3). Although an increased risk for death after hip fracture is well established in both women and men, it is unclear whether this excess mortality persists over time (4).
Although almost all studies have reported an increased risk for death in the first 3 to 6 months after injury, results from long-term (5- to 10-year) follow-up have been conflicting, with some studies finding persistent excess mortality and others finding none (5-8). These conflicting results have several potential causes, including differences in control populations, difficulties in comparing crude and adjusted mortality statistics, and differences in model covariates (4-6, 9-16). At longer follow-up, the number of patients at risk and therefore the number of events (deaths) provide limited statistical power (17). An additional source of variability occurs in time-to-event (survival) analyses when the mortality risk is not constant over time and follow-up varies across the cohorts (17, 18). Because of these factors, reported hazard estimates are varied and have wide CIs, limiting any inferences physicians or public health policymakers can make. Further drawbacks include limited sample size, low frequency of observations, lack of stratification by sex, and reporting relative rather than absolute risks (17, 19, 20).
We summarize longitudinal evidence about the magnitude and duration of excess mortality after hip fracture in older men and women.
Methods
Design Overview
We followed a standardized protocol and conducted a meta-analysis of cohort studies to estimate the pooled relative risk for death after hip fracture by time since fracture (time-to-event meta-analysis). We then used these estimates of relative risk to perform absolute risk calculations (life-table methods applied to a U.S. reference population).
Data Sources and Searches
We searched for English and non-English articles by using MEDLINE (Ovid and PubMed, 1957 to May 2009) and EMBASE; the last computerized search was done on 4 May 2009. The Medical Subject Heading terms included hip fracture and mortality. We supplemented the archived computerized search with a manual search of the references of all retrieved articles.
Study Selection
Two independent reviewers scanned titles and available abstracts to identify potentially relevant articles. We selected published studies that used a prospective cohort design and assessed mortality from the time of the hip fracture onward in women and men older than 50 years, performed a life-table analysis (actuarial approach or Kaplan–Meier approach), and constructed survival curves of the group with hip fracture and (at minimum) an age- and sex-matched control group. We excluded reviews, research letters, case–control studies, uncontrolled studies, studies with less than 1-year follow-up, and studies not reporting separate all-cause mortality according to sex. Because included studies encompassed many years and countries, we could not contact authors for unpublished mortality data according to sex.
Data Extraction and Quality Assessment
Two authors independently extracted data and assessed elements of study quality and validity, including completeness of mortality ascertainment, loss to follow-up, and appropriateness of control population. Disagreements were resolved by consensus. Because of feasibility constraints, we did not contact authors for unpublished mortality data according to sex.
Data Synthesis and Analysis
We critiqued multiple characteristics of studies related to validity and generalizability and examined relationships between these characteristics with findings regarding risk for death after hip fracture. We defined the relative hazard (RH) as the relative risk for death after hip fracture compared with control participants over the total follow-up or during a specific interval after injury. We calculated the RH and 95% CI from the survival curves of individual studies by using a graphical approach that showed time trends (18, 21-23). We limited the analysis to studies with graphical displays of mortality over time because the risk for death is particularly high during the initial months after the injury and because we wished to establish uniform periods for comparing trends across studies.
To track potential changes in the risk for death over time, we partitioned the time axis of each survival curve into 3-month intervals for the first year after injury and into yearly intervals thereafter. The time axis was initially divided into smaller intervals and subsequently into larger intervals, because a substantial proportion of events (deaths) occurs in the first months after injury. This procedure allowed us to calculate the relative risk for death during a specific period from the time, zero, of injury to a postfracture time, t, since injury (time-specific RH, cumulative RH, or RHt), as well as a relative risk for death during a given interval, x, provided that the person is alive at the start of that interval (conditional RH, interval RH, or RHx). We performed the first method to assess the relative differences in survival during the cumulative period from injury to a specific time after injury, such as the relative risk for survival (death) during the 5 years after injury. We performed the other method to reflect a person’s prognosis if he or she had already survived the injury for several months or years. The RHx represents the relative risk for death among patients with hip fracture relative to control participants during a given interval (for example, from year 2 to year 3 after injury), provided that the person is alive at the start of this interval (that is, at 2 years after injury).
Context
What is the magnitude and duration of excess mortality risk after hip fracture?
Contribution
This review and modeling study found a 5- to 8-fold increased risk for mortality in the first 3 months after a hip fracture. Excess mortality risk decreased during the first 2 years after fracture but did not return to the rate of age-matched control participants even after 10 years of follow-up. The excess risk increased with age and, at any given age, was higher for men than for women.
Caution
Results were modeled for a white U.S. population, and the reasons for persistent excess risk were not clarified.
—The Editors
We determined the pooled estimates of the mean effect of hip fracture on mortality (pooled RH) and the corresponding 95% CIs by using the inverse variance fixed-effects model and the DerSimonian and Laird random-effects model for time-specific and conditional RHs (22, 24). Point estimates were similar with both models; we present the random-effects analyses with the more conservative RH estimates.
We visually examined forest plots for heterogeneity, assessed between-study heterogeneity with the Cochran Q test (22, 24), and quantified heterogeneity with the I2 statistic (25, 26). We plotted the RH of each study against several potential sources of heterogeneity that we identified a priori, including country of origin (latitude), mean age at entry (years), cohort size, publication year, starting year of study, and total duration of study (years). We also used random-effects categorical and meta-regression analyses (27) to examine whether findings were affected by the following subgroup characteristics: geographic region, defined according to the categories of the Global Burden of Disease 2000 World Health Organization member states project (28); register-based versus hospital-based fracture cohort; studies including only community-dwelling participants versus studies including nursing-home residents; choice of control group; and death ascertained by interview of relatives, death certificates, or civic registries. We explored potential publication bias by funnel plot (22, 24), the Begg and Mazumdar test (29), and the Egger test (30, 31).
In our second step, we translated the estimates of relative risk for death (RHs) derived from the meta-analysis into estimates of the absolute survival differences between patients with hip fracture and control participants. We calculated absolute survival difference for each year up to 10 years after hip fracture by using standard life-table methods applied to U.S. population– based data on age- and sex-specific mortality (19, 32). Appendix Table 1 (available at www.annals.org) lists details of the mathematical calculations, their derivations, and a description of the underlying assumptions of the model.
The annual mean age- and sex-specific probability of all-cause mortality was based on 2004 U.S. life-tables published by the National Center for Health Statistics (32). These tables show the age-specific annual probability of dying from all causes for men and women starting at birth and ending at age 100 years. The U.S. annual probability of death was adjusted for the relative risk for death associated with hip fracture RHx, as estimated by the meta-analysis. We used this adjusted annual probability of death to compute the number of deaths that would occur annually and the cumulative number of deaths in 100 000 U.S. women and men with hip fracture and 100 000 U.S. control women and men (Table 1 and Appendix Table 1). We calculated estimates of annual and cumulative deaths for women and men at the ages of 70, 75, 80 (mean age of a first hip fracture in white U.S. women), 85, and 90 years.
Table 1.
RH of All-Cause Mortality for Women and Men With Hip Fracture Compared With Control Participants During a Given Interval*
| Age Interval | Women | Men | ||
|---|---|---|---|---|
| RH (95% CI) | P Value | RH (95% CI) | P Value | |
| 0–3 mo | 5.75 (4.94–6.69) | <0.001 | 7.95 (6.13–10.30) | <0.001 |
| 3–6 mo | 3.32 (2.18–5.07) | <0.001 | 3.56 (2.64–4.80) | <0.001 |
| 6–9 mo | 1.92 (1.59–2.32) | <0.001 | 2.33 (1.91–2.85) | <0.001 |
| 9–12 mo | 1.59 (1.26–2.00) | <0.001 | 2.30 (1.81–2.93) | <0.001 |
| 0–1 y | 2.87 (2.52–3.27) | <0.001 | 3.70 (3.31–4.14) | <0.001 |
| 1–2 y | 1.86 (1.60–2.16) | <0.001 | 1.90 (1.58–2.30) | <0.001 |
| 2–3 y | 1.58 (1.09–2.29) | 0.016 | 1.69 (1.36–2.10) | <0.001 |
| 3–4 y | 1.71 (1.35–2.16) | <0.001 | 1.76 (1.44–2.14) | <0.001 |
| 4–5 y | 1.91 (1.53–2.38) | <0.001 | 1.71 (1.37–2.13) | <0.001 |
| 5–6 y | 1.81 (1.30–2.53) | <0.001 | 1.51 (1.33–1.71) | <0.001 |
| 6–7 y | 1.50 (1.23–1.83) | <0.001 | 1.29 (0.98–1.72) | 0.073 |
| 7–8 y | 1.69 (1.16–2.45) | 0.006 | 1.66 (0.96–2.87) | 0.069 |
| 8–9 y | 1.99 (1.42–2.78) | <0.001 | 1.91 (1.32–2.78) | <0.001 |
| 9–10 y | 1.96 (1.30–2.95) | 0.001 | 1.79 (1.14–2.81) | 0.012 |
RH = relative hazard.
Conditional on the person being alive at the start of the interval.
Role of the Funding Source
The study was funded by the Fund for Scientific Research and the Willy Gepts Foundation. The funding sources had no role in defining research questions, abstracting data, synthesizing results, or preparing the manuscript or in the decision to submit the manuscript for publication.
Results
Appendix Figure 1 (available at www.annals.org) shows our search and selection process (33). Of the 196 full-text articles that we examined, 153 did not display survival curves, 16 did not report separate survival curves according to sex (34-49), and 3 were duplicate reports (50-52). Twenty-four articles met all inclusion criteria (5, 6, 9-16, 53-66) and provided survival curves for 22 unique cohorts of women with hip fracture and 17 unique cohorts of men with hip fracture, as well as age- and sex-matched control groups.
Considered together, the cohorts included 578 436 women and 154 276 men with hip fracture. Reference mortality data reported in the 24 articles were taken from the general population in 17 studies, Medicare enrollees in 3 studies, hospital control participants without hip fracture in 2 studies, and community-dwelling participants without hip fracture in 2 studies. Survival was documented during observation periods of 1 to 15 years after injury. Six studies had observation periods of 2 years or less, were hospital-based, started between 1984 and 1995 (calendar year 1989 on average), and included 547 009 women and 144 214 and men with hip fracture (55, 57, 58, 61-63).
The overall quality of most studies was good, although they varied in size, duration of observation, selection of control populations, ascertainment of death, and adjustment for comorbid conditions (Table 2 and Appendix Table 2, available at www.annals.org). In particular, some studies differed substantially from others. Jacobsen and colleagues (58), for example, contributed information on 543 768 and 144 049 U.S. women and men, respectively, with hip fracture (most patients in the overall sample) over a 2-year observation period. Investigators of the Dubbo Osteoporosis Epidemiology Study, an Australian study with a 15-year observation period, acknowledged that selection bias was likely, because participants were healthier than nonparticipants (66, 67). Three studies with observation periods of 2 years or less (55, 61, 63) interviewed relatives to ascertain death.
Table 2.
Specific Design and Data Analyses of the Cohort Studies Included in the Current Time-to-Event Meta-analyses
| Study, Year (Reference) | Designed to Evaluate the Course of Patients After Hip Fracture | Data Stratified by Important Risk Factors* | Types of Stratified Analyses* Provided in the Original Article | Multivariable Analyses Provided | Adjustments for Any Factors* |
|---|---|---|---|---|---|
| Jensen and Tøndevold, 1979 (53) | Yes | Yes | Type of hip fracture, somatic complications | No | Not reported |
| Dahl, 1980 (54) | Yes | Yes | Severity of associated diseases | No | Not reported |
| Holmberg et al, 1986 (9) | Yes | Yes | Type of hip fracture surgery, type of residency before injury | No | Not reported |
| Elmerson et al, 1988 (10) | Yes | Yes | Type of hip fracture; type of residency before injury; discharge to nursing home, convalescent home, or own home | Yes | Age, sex, somatic complications, type of residency before injury, discharge to institution or own home, type of hip fracture, type of operation, concomitant diseases and medication, marital status |
| Magaziner et al, 1989 (55) | Yes | No | Not reported | Yes | Age, sex, race, type of fracture, orientation on admission, concomitant disease, noted dementia, delirium |
| Fisher et al, 1991 (56) | Yes | Yes | Degree of comorbid conditions, type of residency before injury | Yes | Age, sex, race, comorbid conditions, nursing home residence |
| Eiskjaer et al, 1992 (57) | Yes | No | Not reported | No | Not reported |
| Jacobsen et al, 1992 (58) | Yes | Yes | Race, number of comorbid conditions | No | Not reported |
| Schrøder and Erlandsen, 1993 (11) | Yes | No | Not reported | No | Not reported |
| Lu-Yao et al, 1994 (59) | Yes | Yes | Type of hip fracture surgery | Yes | Age, sex, race, number of comorbid conditions (few and many), prefracture residence, site of fracture, type of hip fracture surgery |
| Poór et al, 1995 (12) | Yes | Yes | Degree of comorbid conditions | Yes | Age, number of comorbid conditions, level of comorbidity, activity status at the time of fracture, discharge to a nursing home, mental deterioration during hospitalization |
| Browner et al, 1996 (60) | Yes | No | Not reported | Yes | Enrollment site, age, general heath status, previous hip fracture, diabetes, cigarette smoking, use of corticosteroids, exercise, body weight, functional status, bone density at the calcaneus |
| Magaziner et al, 1997 (5) | No | Yes | Number of impairments in ADLs, comorbid conditions | Yes | Age, education, number of impairments in ADLs, comorbid conditions |
| Forsén et al, 1999 (6) | Yes | No | Not reported | No | Not reported |
| Jitapunkul and Yuktanandana, 2000 (61) | Yes | No | Not reported | No | Not reported |
| Fitzpatrick et al, 2001 (62) | Yes | No | Not reported | Yes | Age, hysterectomy, mental test score, perception of health, dissatisfied with life, ADLs score, walking ability, GP visits in past year, sleep tablet use, hypnotic use, number of current medications, alcohol consumption |
| Haentjens et al, 2001 (63) | Yes | No | Not reported | No | Not reported |
| Trombetti et al, 2002 (13) | Yes | No | Not reported | Yes | Age, sex, fracture site, housing conditions before fracture, mental impairment, history of fracture, general health status, stroke, the extrapyramidal syndrome, diabetes, alcoholism, tobacco use |
| Farahmand et al, 2005 (64) | Yes | Yes | Previous hospitalization | Yes | Age, previous hospitalizations, diabetes mellitus, dementia or psychosis, alcohol or drug abuse, CVD, pneumonia, COPD, liver cirrhosis, renal failure |
| Pande et al, 2006 (65) | Yes | Yes | Initial physical component score of the SF-36 | Yes | Age, BMI, baseline functional capacity, baseline SF-36 physical component and mental component scores |
| Petersen et al, 2006 (14) | Yes | No | Not reported | Yes | Age, perioperative cardiac arrest, dementia, postoperative heart failure, decubitus, sex, stress ulcer, pneumonia, length of orthopedic hospital stay, cardiac arrhythmia (perioperatively), waiting time to operation |
| Robbins et al, 2006 (15) | No | No | Not reported | Yes | Age, race, frailty, MMSE score, Digit Symbol Substitution score, BMI, CHF |
| Giversen et al, 2007 (16) | Yes | Yes | Type of hip fracture | Yes | Age, sex, year |
| Bliuc et al, 2009 (66) | Yes | No | Not reported | Yes | Age, sex, femoral neck BMD, cigarette smoking, physical activity, quadriceps strength, sway, falls |
ADL = activity of daily living; BMD = bone mineral density; BMI = body mass index; CHF = congestive heart failure; COPD = chronic obstructive pulmonary disease; CVD = cardiovascular disease; GP = general practitioner; MMSE = Mini-Mental State Examination; SF-36 = Short Form-36.
Other than age and sex.
Long-term studies, with an observation period of 10 years or more, were started between 1975 and 1989 (calendar year 1980 on average) in Europe (4 studies [10, 11, 14, 16]), the United States (12), or Australia (66). In total, they included 6186 women and 3415 men with hip fractures, but only 859 women and 237 men with hip fractures were still alive (at risk) at the beginning of the 9- to 10-year follow-up for these studies. The long-term study from the United States (12) included only men. All of the long-term studies included all patients with hip fracture (without excluding nonambulatory or institutionalized patients), used mortality data from the general population as reference, and recorded deaths by using a civic registry.
Relative Likelihood of Death
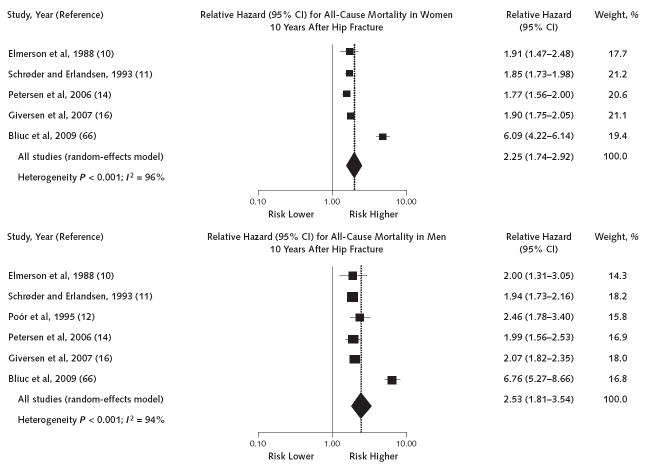
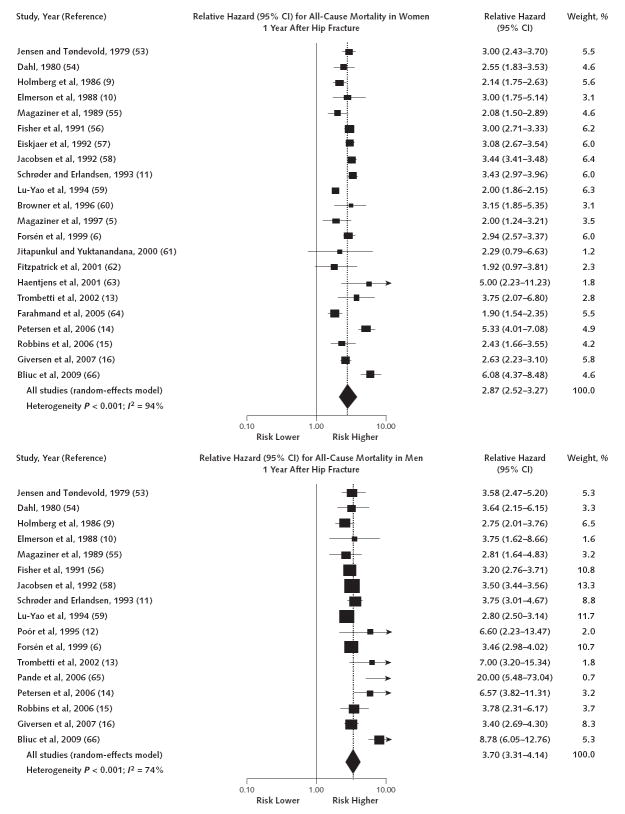
Figure 1 shows individual-study and pooled summary estimates of the cumulative RHs for long-term (10-year) all-cause mortality, and Figure 2 shows the estimates for short-term (1-year) all-cause mortality. The individual study estimates consistently showed increased mortality after hip fracture, but heterogeneity among the studies was statistically significant, with I2 values of up to 96%. Appendix Tables 3 to 5 and Appendix Figures 2 and 3 (available at www.annals.org) detail our exploration of potential sources of heterogeneity. Results for pooled summary estimates did not depend on any single outlying study, and excluding studies that seemed to be outliers (for example, Bliuc and colleagues [66]) did not eliminate statistical heterogeneity. The observed probability of death after 1 year in the control participants (for both women and men) ranged from about 2% to 12% across studies. Stratified analyses suggested that some of the observed heterogeneity in female and male cohorts (P < 0.001 for heterogeneity) might be explained by geographic region. The only factor statistically significantly and positively associated with the cumulative RHs for short-term all-cause mortality in the meta-regression analysis was the duration of observation in cohorts of both female and male patients (R2 = 22% and 24%, P = 0.047 and 0.008, respectively). However, this relationship disappeared when we omitted the study by Bliuc and colleagues (66) (P > 0.15 for all). We observed no differences between the groups when post hoc categorical meta-analyses were limited to the group of 6 studies with a 2-year observation period versus the group of the 6 other studies with an observation period of at least 10 years. The pooled RHs for short-term and long-term studies were 2.89 (95% CI, 2.27 to 3.68) and 3.83 (CI, 3.04 to 4.82), respectively, in women, and 3.23 (CI, 1.95 to 5.36) and 4.99 (CI, 3.62 to 6.89), respectively, in men. P values for between-group heterogeneity in women and men were 0.10 and 0.16, respectively.
Figure 1. Forest plots of long-term (10-year) all-cause mortality in older women and men.
Squares represent the long-term (10-year) cumulative relative hazard for all-cause mortality according to sex. Horizontal lines indicate 95% CIs. The dotted vertical line is the pooled relative hazard; the solid vertical line is the null effect. The size of the squares is proportional to the weight of the studies.
Figure 2. Forest plots of short-term (1-year) all-cause mortality in older women and men.
Squares represent the short-term (1-year) cumulative relative hazard for all-cause mortality according to sex. Horizontal lines indicate 95% CIs. The dotted vertical line is the pooled relative hazard; the solid vertical line is the null effect. The size of the squares is proportional to the weight of the studies.
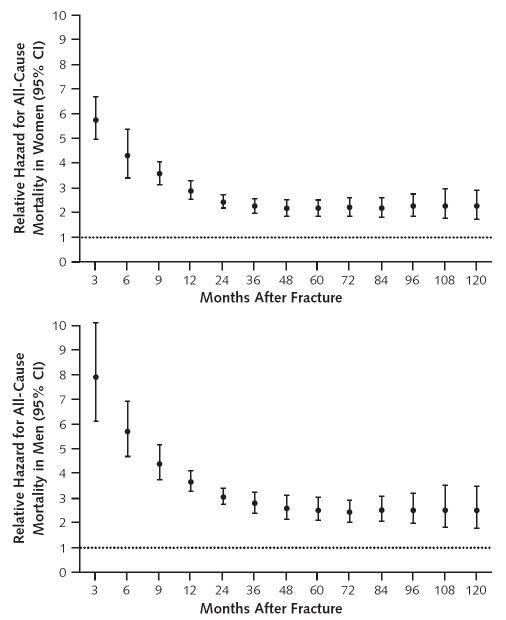
Figure 3 plots the pooled estimates of the cumulative RHs for all-cause mortality after hip fracture, according to sex and time since injury. Women with a hip fracture had a 5-fold (RH, 5.75 [CI, 4.94 to 6.67]) increase and men had an almost 8-fold (RH, 7.95 [CI, 6.13 to 10.30]) increase in the relative likelihood of death from all causes adjusted for age compared with control participants during the first 3 months after hip fracture. The RHs decreased substantially during the first 2 years after fracture but did not return to the mortality rates seen in age- and sex-matched control participants, even at the longest follow-up. Fifteen years after injury, the pooled cumulative RHs for women and men were 3.00 (CI, 1.10 to 8.18; 2 studies) and 3.52 (CI, 0.99 to 12.5; 2 studies), respectively.
Figure 3. Relative hazard of all-cause mortality for women and men with hip fracture versus control groups during a given follow-up period starting at the time of injury.
Solid circles represent the pooled relative hazard. Vertical bars represent the corresponding 95% CIs. The dotted horizontal line is the null effect.
Table 1 shows the pooled estimates of the conditional RH for all-cause mortality in women and men, reflecting the prognosis if the patient had already survived the injury. We observed the highest hazard estimates during the intervals immediately after injury, especially in men, with a subsequent decrease in both sexes. Beginning at the second year, the RH of mortality became relatively constant but remained substantially increased compared with control participants. We observed similar findings in men, even though the excess hazard of mortality did not reach statistical significance during all intervals, presumably because of the smaller number of men at risk and the smaller number of events (deaths) during certain intervals. Merging the estimates beyond the second year after fracture, the annual RH for all-cause mortality was 1.73 (CI, 1.56 to 1.90) in women and 1.61 (CI, 1.48 to 1.74) in men.
Funnel plots and formal statistical tests, including the rank correlation test of Begg and Mazumdar and the test of Egger and colleagues (29-31), suggested the possibility of publication bias (data not shown).
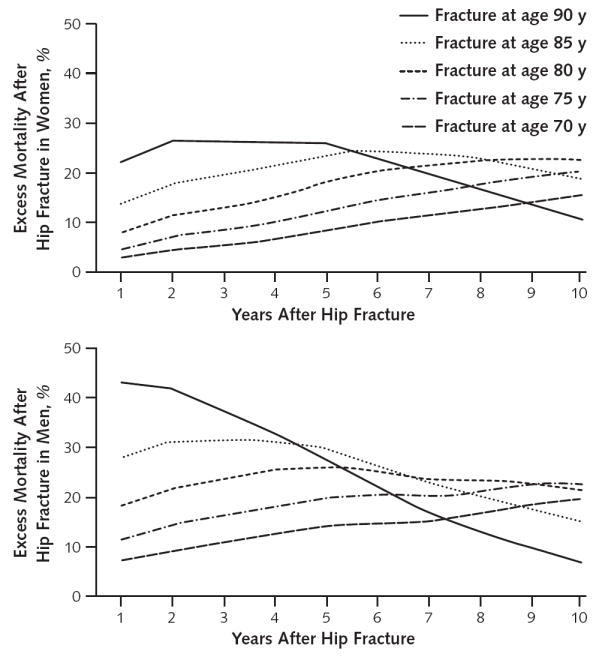
Absolute Risk for Death
Appendix Table 6 (available at www.annals.org) and Figure 4 show differences in absolute risk for death after hip fracture in the various age and sex groups. Appendix Table 1 gives life-tables for imaginary cohorts of 100 000 older women and 100 000 older men with and without hip fracture. These estimates show, for example, that a white woman in the United States who has a hip fracture at age 80 years has an excess annual mortality of 8%, 11%, 18%, and 22% at 1, 2, 5, and 10 years after injury, respectively. The corresponding figures for a white man in the United States who has a hip fracture at age 80 years are 18%, 22%, 26%, and 20%. Overall, these findings indicate that, in both sexes, excess mortality after hip fracture depends largely on age. At any given age, excess mortality after hip fracture is higher in men than in women. Beyond 5 years after hip fracture, and especially in persons older than 80 years, sex-related differences in excess risk for mortality start to decrease. In the older age categories, age-specific mortality from other causes increases very rapidly. The effect of this competing mortality reduces the absolute excess mortality after hip fracture in the oldest group of patients. Regardless, statistically significant excess mortality persists for 10 years after hip fracture.
Figure 4. Differences in absolute risk for death (excess mortality) from all causes for women and men with hip fracture compared with control participants during a given follow-up period starting at the time of injury.
Discussion
Our analysis of data from multiple cohort studies showed that older adults have a 5- to 8-fold increased risk for all-cause mortality during the first 3 months after hip fracture. Relative hazards for mortality decreased thereafter but did not return to rates seen in age- and sex-matched control groups without fracture. Moreover, an excess annual mortality for adults with hip fracture persisted over time in both women and men. At any given age, the excess annual mortality after hip fracture was higher in men than in women.
Several factors may contribute to the marked increase in short-term relative mortality risk after hip fracture. These include postoperative events associated with hip surgery, such as pulmonary embolism (68), infectious complications (69, 70), heart failure (69, 70), or cardiovascular or pulmonary complications (64). Multiple comorbid conditions predisposing to fracture, such as dementia, chronic obstructive pulmonary disease, psychiatric conditions, cardiovascular disease, kidney disease, and neurologic diseases could also increase short-term mortality risks (5, 12, 47). Whether some of these factors could help explain why excess mortality after hip fracture is consistently higher in men than in women merits further study. For example, 1 study suggested that the higher excess mortality in men might be related to an increased risk for postoperative complications, including infections (70). Another study showed that men with fracture have a greater burden of comorbid diseases at the time of fracture than women (71), although comorbid conditions do not fully explain the mortality difference between the sexes (58, 70).
We do not know whether the long-term excess mortality in patients with hip fracture is driven by differences in frailty that existed before hip fracture, were precipitated by hip fracture, or both. Patients with hip fracture are, on average, more functionally impaired and have more comorbid conditions than similar-aged patients without hip fracture. Prospective studies of functional outcomes after fracture also indicate that older adults who have a hip fracture have substantial new functional impairments and loss in quality of life that frequently persist at 1 year (71-73). Many of the components of the frailty syndrome that commonly occur after hip fracture are known risk factors for mortality, including poor mobility, balance, reduced muscle strength, impaired cognition, poor nutritional status, low levels of physical activity, and increased risk for falls (37, 74-77). However, 1 study comparing survival in women older than age 70 who had hip fracture with control participants matched by age, sex, comorbid conditions, and functional status found that although short-term mortality (up to 2 years) was more pronounced in women with comorbid disease and functional limitations at the time of fracture, excess mortality more than 2 years after the fracture was restricted to those who had fewer baseline comorbid conditions and functional limitations. This intriguing preliminary finding suggests that hip fracture, perhaps through an inflammatory or immunologic effect, may trigger or accelerate frailty in patients with few comorbid conditions at baseline, leading to longer-term effects on survival (78).
Several limitations affect the certainty and interpretation of our findings. First, some data derived from individual studies could have been biased. Most studies that we analyzed either pooled nursing home residents with community-dwelling participants or did not specify and differentiate nursing home residents from community-dwelling participants. Data from studies that pooled patients with varying underlying risks could potentially over-estimate the survival of nursing home residents with hip fracture and underestimate the survival of community-dwelling participants with hip fracture. Most studies assembled cohorts from hospital admissions or lists. These studies missed persons with hip fracture who were never admitted and probably had very high early mortality rates.
Second, we included only studies that displayed results with survival curves, and statistical testing suggested the possibility of publication bias. Third, studies varied, sometimes markedly, in size, duration of observation, selection of control populations, ascertainment of death, and adjustment for comorbid conditions. We had limited ability to explore how the accuracy or precision of RH estimates for short- and long-term mortality were affected by between-study heterogeneity.
Fourth, our analyses do not quantify how much of the observed excess mortality is directly attributable to hip fracture and its sequelae. We could not assess or take into account the potentially confounding effects of comorbid conditions and treatments received. Fifth, mortality rates in the hip fracture and control populations may vary over time and could bias the RH estimates. Life-table method–based analyses, as used in our study, assume no secular trends in relative risk for death, which may be unrealistic. Indeed, some evidence suggests that mortality risk after hip fracture has increased over time, even with adjustment for demographic shifts in the hip fracture population (47).
Sixth, although we pooled data from studies conducted in several geographic regions, the generalizability of our estimates of age-specific excess mortality is limited, because we modeled excess mortality only for a white U.S. population. Finally, our modeling of excess mortality was hypothetical and not an actual prospective study.
Regardless of limitations, we believe ours is the first systematic review to provide quantitative estimates of both relative and absolute survival in patients with hip fracture. Meta-analyses of survival data require specific techniques because of data censoring; ignoring censoring may bias the overall estimates. Potentially useful information about timing of events (deaths) and the shape of the published survival curves was not discarded in the current analysis, because we computed an RH and its standard error for each contributing cohort study and then increased the power of our analyses by pooling data. An advantage of this method is that we could estimate the RH of death at several intervals after the injury. The cohorts used in this analysis varied in size, and the designs of the studies were heterogeneous in many respects, but no single study was so large that it dominated the overall results regarding RH for all-cause mortality. From a public health perspective, calculations of absolute risk and estimates of excess mortality, such as those presented here, not only allow estimates of the consequences of various diseases and complications but may ultimately contribute to a more appropriate allocation of resources for competing causes of mortality.
Patients with hip fracture have a 5- to almost 8-fold increased hazard of all-cause mortality during the first 3 months after the fracture. This excess mortality decreases substantially during the first 2 years after fracture, but does not return to the mortality rate seen in age- and sex-matched control participants even after 10 years of follow-up. Over time, this excess mortality RH translates into statistically significant differences in the absolute risk for death. The absolute risk for death and the excess all-cause mortality in patients with hip fracture are largely dependent on age. At any given age, excess mortality after hip fracture is higher in men than in women. These findings may be helpful when performing cost-effectiveness analyses of hip fracture prevention strategies or designing treatment strategies in patients with hip fracture.
Acknowledgments
The authors thank Dr. Geert Verbeke, head of the Interuniversity Institute for Biostatistics and Statistical Bioinformatics, Katholieke Universiteit Leuven and Universiteit Hasselt for his support during the final revision process of our manuscript.
Grant Support: By the Fund for Scientific Research (G.0488.08); Leuven University; National Institutes of Health (R01 AG06322, R01 HD0073, R37 AG09901, and P60 AG12583); the Paul B. Beeson Award (K23 AG024787); and the Willy Gepts Foundation, Universitair Ziekenhuis Brussel.
Appendix
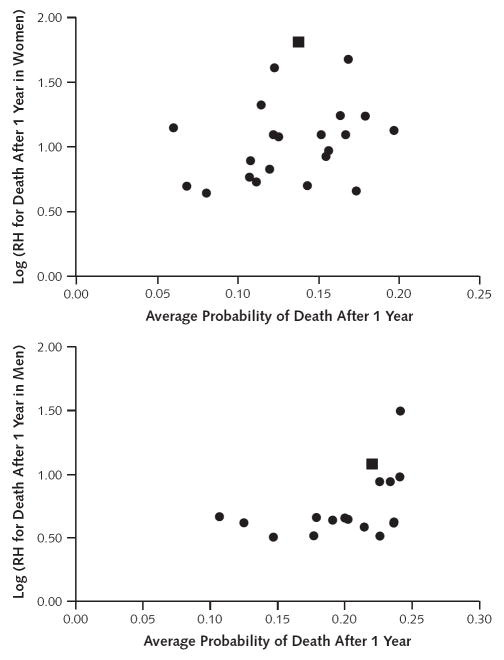
The additional post hoc meta-regression analyses indicated that the cumulative RHs for short-term (1-year) all-cause mortality might be positively associated with the underlying risk at 1 year in female cohorts (R2 = 15%, P = 0.043) but not in male cohorts (R2 = 7%, P = 0.18). These findings were similar when the Australian outlier study was excluded (R2 = 22%, P = 0.030, and R2 = 3%, P = 0.45, respectively) (Appendix Table 3 and Appendix Figure 3) (66).
Because of this information, we also formally explored heterogeneity in baseline mortality rates.
To examine heterogeneity (differences across control groups) and to calculate pooled summary proportions across all samples and for each control group, we used the logit method. In this method, the observed proportions are converted to logits, all analyses (fixed-effects and random-effects models) are performed on the logit, and the final results are converted back into proportions for ease of interpretation (27). According to the data in the individual studies, the observed probability of death after 1 year ranges from 2.9% to 11.8% and from 2.3% to 11.9% in the female and male control groups, respectively. Our analyses using the logit method confirm that mortality probability values after 1 year are highly heterogeneous in both sexes. In women, the I2 statistic is 90%, with a P value for the Q statistic less than 0.001 (chi-square = 202.44). In men, the I2 statistic is 91%, with a P value for the Q statistic less than 0.001 (chi-square = 174.32).
We conducted further post hoc categorical and meta-regression analyses to identify potential factors that might influence the underlying mortality risk in the reference populations. Lower baseline risks for all-cause mortality in female cohorts were associated with geographic location (P = 0.031 for the Australian study), control participants taken from community-dwelling populations (P = 0.012), and the study being started in a recent calendar year (P = 0.037) and in male cohorts were associated with geographic location (P = 0.001 for the Australian study) and the study being started in a recent calendar year (P < 0.001). After we excluded the Australian outlier study, only control participants taken from community-dwelling populations significantly (P = 0.004) affected the baseline risks for all-cause mortality in female cohorts (all other P values > 0.15). In male cohorts, baseline risk was lower in Europe than in the United States (P = 0.006) (Appendix Table 5).
Appendix Figure 1. Literature search and selection.
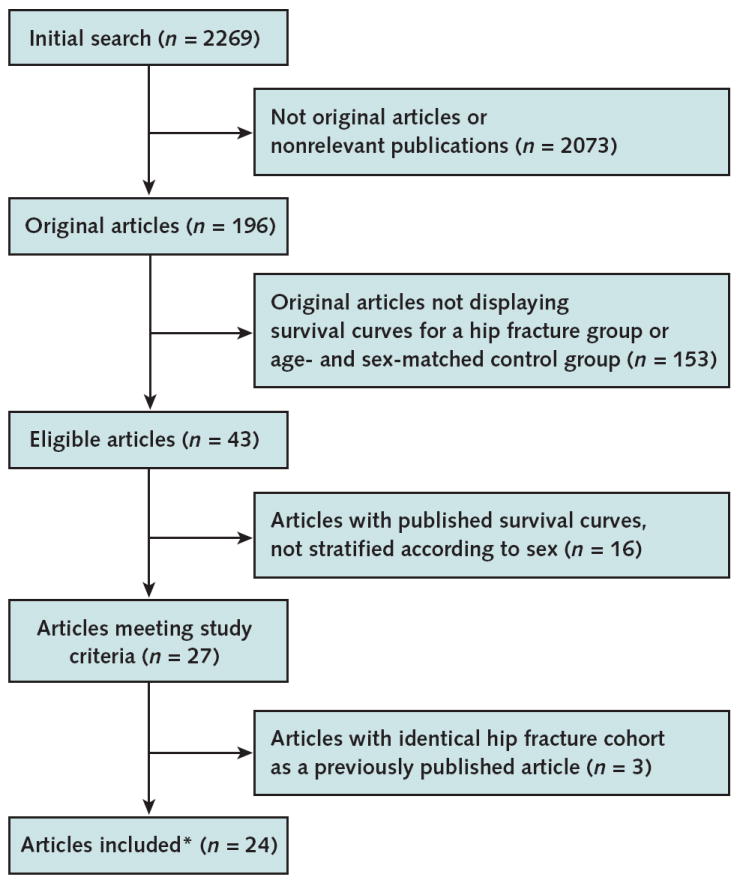
Adapted from MOOSE Statement flow diagram (33).
* These 24 articles present survival curves for 22 and 17 unique cohorts of women and men with hip fracture, respectively, as well as age- and sex-matched control groups.
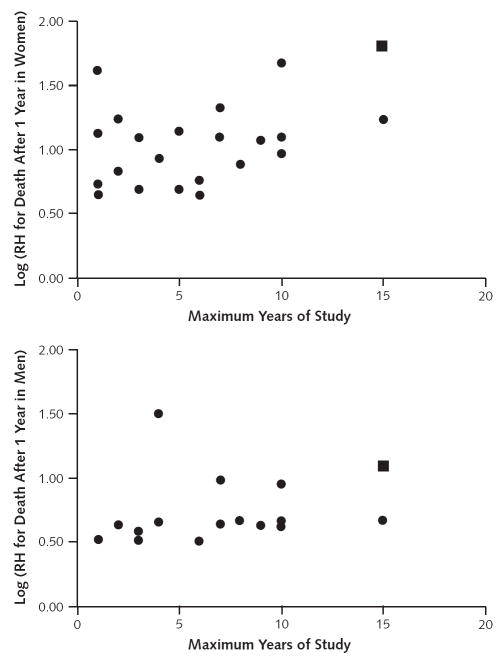
Appendix Figure 2. Meta-regression analyses exploring heterogeneity of the cumulative RHs for short-term (1-year) all-cause mortality in older women and men, according to maximum duration of study.
The square represents the Dubbo Osteoporosis Epidemiology Study, which was done in Australia and had a 15-year observation period (66). The authors acknowledge that there was probably selection bias in their study because participants were healthier than nonparticipants (67).
RH = relative hazard.
Appendix Figure 3. Meta-regression analyses exploring heterogeneity of the cumulative RHs for short-term (1-year) all-cause mortality in older women and men, according to average probability of death after 1 year.
The square represents the Dubbo Osteoporosis Epidemiology Study, which was done in Australia and had a 15-year observation period (66). The authors acknowledge that there was probably selection bias in their study because participants were healthier than nonparticipants (67).
RH = relative hazard.
Appendix Table 1.
Life-Tables Estimating Probability of All-Cause Mortality for Imaginary Cohorts of 100 000 Women and 100 000 Men, With and Without Hip Fracture, in the United States
| Age Interval, y | Proportion Dying During Age Interval (U.S. Population)* | Relative Risk for Death After Hip Fracture† | Adjusted Proportion of Deaths During Age Interval‡ | Persons Alive at Beginning of Age Interval, n | Persons Dying During Age Interval, n | Cumulative Deaths at End of Interval, n | Deaths From Initial Age to End of Interval, % | Years Between Initial Age and End of Interval |
|---|---|---|---|---|---|---|---|---|
| Women with hip fracture | ||||||||
| 80–81 | 0.046299 | 2.87 | 0.133019 | 100 000 | 13 302 | 13 302 | 13 | 1 |
| 81–82 | 0.051190 | 1.86 | 0.095340 | 86 698 | 8266 | 21 568 | 22 | 2 |
| 82–83 | 0.056564 | 1.58 | 0.089292 | 78 432 | 7003 | 28 571 | 29 | 3 |
| 83–84 | 0.062668 | 1.71 | 0.107115 | 71 429 | 7651 | 36 222 | 36 | 4 |
| 84–85 | 0.069752 | 1.91 | 0.133196 | 63 778 | 8495 | 44 717 | 45 | 5 |
| 85–86 | 0.077062 | 1.81 | 0.139801 | 55 283 | 7729 | 52 446 | 52 | 6 |
| 86–87 | 0.085061 | 1.50 | 0.127657 | 47 554 | 6071 | 58 516 | 59 | 7 |
| 87–88 | 0.093796 | 1.69 | 0.158130 | 41 484 | 6560 | 65 076 | 65 | 8 |
| 88–89 | 0.103316 | 1.99 | 0.205802 | 34 924 | 7187 | 72 264 | 72 | 9 |
| 89–90 | 0.113667 | 1.96 | 0.223088 | 27 736 | 6188 | 78 451 | 78 | 10 |
| Control women | ||||||||
| 80–81 | 0.046299 | 1.00 | 0.046299 | 100 000 | 4630 | 4630 | 5 | 1 |
| 81–82 | 0.051190 | 1.00 | 0.051190 | 95 370 | 4882 | 9512 | 10 | 2 |
| 82–83 | 0.056564 | 1.00 | 0.056564 | 90 488 | 5118 | 14 630 | 15 | 3 |
| 83–84 | 0.062668 | 1.00 | 0.062668 | 85 370 | 5350 | 19 980 | 20 | 4 |
| 84–85 | 0.069752 | 1.00 | 0.069752 | 80 020 | 5582 | 25 562 | 26 | 5 |
| 85–86 | 0.077062 | 1.00 | 0.077062 | 74 438 | 5736 | 31 298 | 31 | 6 |
| 86–87 | 0.085061 | 1.00 | 0.085061 | 68 702 | 5844 | 37 142 | 37 | 7 |
| 87–88 | 0.093796 | 1.00 | 0.093796 | 62 858 | 5896 | 43 038 | 43 | 8 |
| 88–89 | 0.103316 | 1.00 | 0.103316 | 56 962 | 5885 | 48 923 | 49 | 9 |
| 89–90 | 0.113667 | 1.00 | 0.113667 | 51 077 | 5806 | 54 729 | 55 | 10 |
| Men with hip fracture | ||||||||
| 80–81 | 0.066477 | 3.70 | 0.246262 | 100 000 | 24 626 | 24 626 | 25 | 1 |
| 81–82 | 0.073126 | 1.90 | 0.139189 | 75 374 | 10 491 | 35 117 | 35 | 2 |
| 82–83 | 0.080046 | 1.69 | 0.135151 | 64 883 | 8769 | 43 886 | 44 | 3 |
| 83–84 | 0.087161 | 1.76 | 0.153125 | 56 114 | 8592 | 52 479 | 52 | 4 |
| 84–85 | 0.094768 | 1.71 | 0.162044 | 47 521 | 7701 | 60 179 | 60 | 5 |
| 85–86 | 0.103554 | 1.51 | 0.156461 | 39 821 | 6230 | 66 410 | 66 | 6 |
| 86–87 | 0.113038 | 1.29 | 0.146376 | 33 590 | 4917 | 71 326 | 71 | 7 |
| 87–88 | 0.123254 | 1.66 | 0.204825 | 28 674 | 5873 | 77 200 | 77 | 8 |
| 88–89 | 0.134235 | 1.91 | 0.256772 | 22 800 | 5855 | 83 054 | 83 | 9 |
| 89–90 | 0.146007 | 1.79 | 0.261145 | 16 946 | 4425 | 87 479 | 87 | 10 |
| Control men | ||||||||
| 80–81 | 0.066477 | 1.00 | 0.066477 | 100 000 | 6648 | 6648 | 7 | 1 |
| 81–82 | 0.073126 | 1.00 | 0.073126 | 93 352 | 6826 | 13 474 | 13 | 2 |
| 82–83 | 0.080046 | 1.00 | 0.080046 | 86 526 | 6926 | 20 400 | 20 | 3 |
| 83–84 | 0.087161 | 1.00 | 0.087161 | 79 600 | 6938 | 27 338 | 27 | 4 |
| 84–85 | 0.094768 | 1.00 | 0.094768 | 72 662 | 6886 | 34 224 | 34 | 5 |
| 85–86 | 0.103554 | 1.00 | 0.103554 | 65 776 | 6811 | 41 036 | 41 | 6 |
| 86–87 | 0.113038 | 1.00 | 0.113038 | 58 964 | 6665 | 47 701 | 48 | 7 |
| 87–88 | 0.123254 | 1.00 | 0.123254 | 52 299 | 6446 | 54 147 | 54 | 8 |
| 88–89 | 0.134235 | 1.00 | 0.134235 | 45 853 | 6155 | 60 302 | 60 | 9 |
| 89–90 | 0.146007 | 1.00 | 0.146007 | 39 698 | 5796 | 66 098 | 66 | 10 |
Age-specific probability of all-cause mortality for the general white female and male population, taken from U.S. vital statistics for 2004 (32).
Relative risk for death after hip fracture, estimated from time-to-event meta-analyses based on prospective studies of the relationship between hip fracture and subsequent risk for death in patients with hip fracture versus the general population.
All-cause mortality for women or men aged 50 years with hip fracture.
Appendix Table 2.
Qualitative Characteristics of the Cohort Studies Included in the Current Time-to-Event Meta-analyses
| Study, Year (Reference) | Country | Latitude, degrees | Region* | Source of Hip Fracture Population† | Patients With Hip Fracture Considered for Inclusion‡ | Source of Control Population | |
|---|---|---|---|---|---|---|---|
| Jensen and Tøndevold, 1979 (53) | Denmark | 56 | Europe | Hospital | All comers | General population | |
| Dahl, 1980 (54) | Norway | 60 | Europe | Hospital | All comers | General population | |
| Holmberg et al, 1986 (9) | Sweden | 59 | Europe | Hospital | All comers | General population | |
| Elmerson et al, 1988 (10) | Sweden | 59 | Europe | Hospital | All comers | General population | |
| Magaziner et al, 1989 (55) | United States | 39 | Americas | Hospital | Community dwellers | General population | |
| Fisher et al, 1991 (56) | United States | 39 | Americas | Register | All comers | Medicare | |
| Eiskjaer et al, 1992 (57) | Denmark | 56 | Europe | Hospital | All comers | General population | |
| Jacobsen et al, 1992 (58) | United States | 39 | Americas | Hospital | All comers | General population | |
| Schrøder and Erlandsen, 1993 (11) | Denmark | 56 | Europe | Hospital | All comers | General population | |
| Lu-Yao et al, 1994 (59) | United States | 39 | Americas | Register | All comers | Medicare | |
| Poór et al, 1995 (12) | United States | 39 | Americas | Register | All comers | General population | |
| Browner et al, 1996 (60) | United States | 39 | Americas | Hospital | Community dwellers | Community dwellers | |
| Magaziner et al, 1997 (5) | United States | 39 | Americas | Register | Community dwellers | Community dwellers | |
| Forsén et al, 1999 (6) | Norway | 60 | Europe | Register | All comers | General population | |
| Jitapunkul and Yuktanandana, 2000 (61) | Thailand | – | Southeast Asia | Hospital | All comers | Hospital | |
| Fitzpatrick et al, 2001 (62) | Ireland | 52 | Europe | Hospital | All comers | Hospital | |
| Haentjens et al, 2001 (63) | Belgium | 51 | Europe | Hospital | All comers | General population | |
| Trombetti et al, 2002 (13) | Switzerland | 47 | Europe | Hospital | All comers | General population | |
| Farahmand et al, 2005 (64) | Sweden | 59 | Europe | Register | All comers | General population | |
| Pande et al, 2006 (65) | United Kingdom | 52 | Europe | Hospital | All comers | General population | |
| Petersen et al, 2006 (14) | Denmark | 56 | Europe | Hospital | All comers | General population | |
| Robbins et al, 2006 (15) | United States | 39 | Americas | Register | All comers | Medicare | |
| Giversen et al, 2007 (16) | Denmark | 56 | Europe | Register | All comers | General population | |
| Bliuc et al, 2009 (66) | Australia | 34 | Western Pacific | Register | All comers | General population | |
| Starting Year of Study | Duration of Study, y§ | Women With Hip Fracture, n | Men With Hip Fracture, n | Average Age at Hip Fracture, y | Procedure to Ascertain Death | ||
| Jensen and Tøndevold, 1979 (53) | 1971 | 7 | 1224 | 368 | 77 | Civic registry | |
| Dahl, 1980 (54) | 1961 | 4 | 500 | 175 | 72 | Civic registry | |
| Holmberg et al, 1986 (9) | 1975 | 6 | 1770 | 608 | 76 | Death certificate | |
| Elmerson et al, 1988 (10) | 1975 | 10 | 207 | 81 | 76 | Civic registry | |
| Magaziner et al, 1989 (55) | 1984 | 1 | 649 | 165 | 80 | Interview of relatives | |
| Fisher et al, 1991 (56) | 1984 | 3 | 7175 | 1916 | 80 | Civic registry | |
| Eiskjaer et al, 1992 (57) | 1987 | 1 | 2273 | – | 80 | Death certificate | |
| Jacobsen et al, 1992 (58) | 1984 | 2 | 543 768 | 144 049 | 83 | Civic registry | |
| Schrøder and Erlandsen, 1993 (11) | 1970 | 15 | 2846 | 1049 | 78 | Civic registry | |
| Lu-Yao et al, 1994 (59) | 1986 | 3 | 10 395 | 2761 | 81 | Civic registry | |
| Poór et al, 1995 (12) | 1978 | 10 | – | 1312 | 79 | Civic registry | |
| Browner et al, 1996 (60) | 1988 | 5 | 361 | – | – | Death certificate | |
| Magaziner et al, 1997 (5) | 1984 | 5 | 529 | – | 82 | Civic registry | |
| Forsén et al, 1999 (6) | 1984 | 9 | 1338 | 487 | – | Civic registry | |
| Jitapunkul and Yuktanandana, 2000 (61) | 1995 | 2 | 60 | – | 72 | Interview of relatives | |
| Fitzpatrick et al, 2001 (62) | 1989 | 1 | 89 | – | 79 | Death certificate | |
| Haentjens et al, 2001 (63) | 1995 | 1 | 170 | – | 80 | Interview of relatives | |
| Trombetti et al, 2002 (13) | 1992 | 7 | 264 | 106 | 81 | Civic registry | |
| Farahmand et al, 2005 (64) | 1993 | 6 | 1327 | – | 72 | Death certificate | |
| Pande et al, 2006 (65) | 1995 | 4 | – | 100 | 80 | Death certificate | |
| Petersen et al, 2006 (14) | 1985 | 10 | 970 | 216 | 81 | Civic registry | |
| Robbins et al, 2006 (15) | 1989 | 8 | 282 | 99 | – | Civic registry | |
| Giversen et al, 2007 (16) | 1987 | 10 | 1980 | 694 | 81 | Civic registry | |
| Bliuc et al, 2009 (66) | 1989 | 15 | 183 | 63 | 79 | Civic registry | |
| Age Limit Used as Inclusion Criterion | Presence of Substantive Comorbid Conditions | Inclusion of Institutionalized Patients | Hip Fracture Type Specified | Hip Fracture Surgery Specified | Length of Hospitalization Specified | Missing Mortality Data Specified | |
| Jensen and Tøndevold, 1979 (53) | > 50 y | – | Yes | Yes | Yes | 24 d | No |
| Dahl, 1980 (54) | None reported | Yes | Yes | Yes | Yes | No | No |
| Holmberg et al, 1986 (9) | None reported | – | Yes | Yes | Yes | No | No |
| Elmerson et al, 1988 (10) | None reported | – | Yes | Yes | Yes | No | No |
| Magaziner et al, 1989 (55) | ≥65 y | Yes | No | Yes | No | No | No |
| Fisher et al, 1991 (56) | None reported | Yes | Yes | No | No | No | 2.5% |
| Eiskjaer et al, 1992 (57) | ≥50 y | – | Yes | Yes | Yes | No | No |
| Jacobsen et al, 1992 (58) | ≥65 y | Yes | Yes | No | No | No | No |
| Schrøder and Erlandsen, 1993 (11) | ≥40 y | – | Yes | No | No | No | No |
| Lu-Yao et al, 1994 (59) | ≥65 y | Yes | Yes | Yes | Yes | No | No |
| Poór et al, 1995 (12) | None reported | – | Yes | Yes | Yes | No | No |
| Browner et al, 1996 (60) | ≥65 y | No | No | No | No | No | No |
| Magaziner et al, 1997 (5) | ≥70 y | No | No | No | No | No | No |
| Forsén et al, 1999 (6) | ≥50 y | Yes | Yes | No | No | No | 0.1% |
| Jitapunkul and Yuktanandana, 2000 (61) | ≥50 y | Yes | Yes | No | No | No | No |
| Fitzpatrick et al, 2001 (62) | ≥50 y | Yes | Yes | No | No | No | No |
| Haentjens et al, 2001 (63) | ≥50 y | Yes | Yes | No | No | 29 d | 0% |
| Trombetti et al, 2002 (13) | ≥55 y | Yes | Yes | Yes | No | 20 d | No |
| Farahmand et al, 2005 (64) | 50–81 y | Yes | Yes | No | No | No | 0% |
| Pande et al, 2006 (65) | ≥50 y | Yes | Yes | No | No | No | 0% |
| Petersen et al, 2006 (14) | ≥75 y | Yes | Yes | Yes | Yes | 18 d | No |
| Robbins et al, 2006 (15) | ≥65 y | Yes | Yes | No | No | No | No |
| Giversen et al, 2007 (16) | ≥50 | – | Yes | Yes | No | No | No |
| Bliuc et al, 2009 (66) | ≥60 | Yes | Yes | No | No | No | No |
| Control Matching∥ | |||||||
| Jensen and Tøndevold, 1979 (53) | A comparable number of participants with similar age and sex, obtained from the Danish Central Bureau of Statistics | ||||||
| Dahl, 1980 (54) | Persons from the population with comparable age and sex, given by the Central Bureau of Statistics, Norway | ||||||
| Holmberg et al, 1986 (9) | Age- and sex-matched persons from the general population, based on data from the National Central Bureau of Statistics, Sweden | ||||||
| Elmerson et al, 1988 (10) | Life-tables for all of Sweden, adjusted for age and sex of the patient with fracture | ||||||
| Magaziner et al, 1989 (55) | Age-, sex-, and race-specific death rates published by the National Center for Health Statistics for the U.S. population | ||||||
| Fisher et al, 1991 (56) | Expected survival of the population for each sex by applying survival probabilities for Medicare enrollees to a population demographically matched (age/race) to the patients with hip fracture | ||||||
| Eiskjaer et al, 1992 (57) | Life-tables for the standard population in Aarhus County, Denmark, adjusted for age of the women with fracture | ||||||
| Jacobsen et al, 1992 (58) | Expected mortality rates within sex- and race-specific stratum, calculated by using the 1-year age-specific 1980 decennial life-table estimates | ||||||
| Schrøder and Erlandsen, 1993 (11) | Expected survival curves of an age- and sex-matched Danish background population, calculated by using the national life-tables published by the Danish Central Bureau of Statistics | ||||||
| Lu-Yao et al, 1994 (59) | Medicare reference group with the same sex, race, and age structure | ||||||
| Poór et al, 1995 (12) | Each survival curve compared with the curve that would have been expected if the study participants had survived according to the mortality rates of Minnesota men of similar age | ||||||
| Browner et al, 1996 (60) | Mortality in a control group by selecting 2 age-matched control participants who were alive on the date of the fracture but who had not had that type of fracture during the study | ||||||
| Magaziner et al, 1997 (5) | White male respondents aged ≥70 y interviewed for the LSOA | ||||||
| Forsén et al, 1999 (6) | Sex- and age-matched control residents of the Norwegian county of Nord-Trøndelag who had no hip fracture and who were alive at the date of the injury of the matched patient with hip fracture | ||||||
| Jitapunkul and Yuktanandana, 2000 (61) | Sex- and age-matched control women randomly selected from patients who had been admitted to the hospital during the same period and had been discharged | ||||||
| Fitzpatrick et al, 2001 (62) | Age-matched control women recruited from patients attending the accident and emergency department, from the inpatient department of the hospital, and from community residences for elderly persons | ||||||
| Haentjens et al, 2001 (63) | Control participants chosen from the same municipality and matched for residence and age (within 5 years) by using the “nearest neighborhood” method | ||||||
| Trombetti et al, 2002 (13) | Sex- and age-matched control participants randomly selected from patients who had been treated at the same hospital during the same period | ||||||
| Farahmand et al, 2005 (64) | Age-matched, native-born control women randomly selected from the national, continuously updated population registry in the study area | ||||||
| Pande et al, 2006 (65) | Control men aged ≥50 y with no history of hip fracture recruited from a local general practitioner register | ||||||
| Petersen et al, 2006 (14) | Age- and sex-matched reference population from Statistics Denmark | ||||||
| Robbins et al, 2006 (15) | 3 participants from the CHS, individually matched to each patient with hip fracture on time since enrollment, recruitment wave, age at enrollment, sex, and race | ||||||
| Giversen et al, 2007 (16) | Mortality tables for the Danish population matched by sex, age, and year | ||||||
| Bliuc et al, 2009 (66) | Age- and sex-specific mortality rates for each fracture group were compared with expected mortality from age- and sex-specific population mortality rates in Dubbo, Australia | ||||||
CHS = Cardiovascular Health Study; LSOA = Longitudinal Study on Aging.
Defined according to the categories for the Global Burden of Disease 2000 World Health Organization member states project (28).
Register = register-based cohort of patients with hip fracture; hospital = hospital-based cohort of patients with hip fracture.
Community dwellers = only community dwellers considered for inclusion; all comers = community dwellers and nursing home residents.
Maximum duration of follow-up.
Test of heterogeneity for 1-year probability of death between control groups: P < 0.001, I2 = 90% for women (chi-square = 202.44); P < 0.001, I2 = 91% for men (chi-square = 174.32). See Appendix for further details.
Appendix Table 3.
Potential Predictors of the Cumulative Relative Hazards for Short-Term (1-Year) All-Cause Mortality, Exploring Heterogeneity by Using Categorical and Meta-regression Analyses*
| Variable | Women | Men | ||||||
|---|---|---|---|---|---|---|---|---|
| All Studies | Outlying Study Omitted† | All Studies | Outlying Study Omitted† | |||||
| R2, % | P Value | R2, % | P Value | R2, % | P Value | R2, % | P Value | |
| Categorical meta-analyses | ||||||||
| Region‡ | <0.001 | 0.64 | <0.001 | 0.19 | ||||
| Hip fracture population source | 0.23 | 0.134 | 0.96 | 0.27 | ||||
| Patients with hip fracture considered for inclusion | 0.24 | 0.32 | 0.38 | 0.48 | ||||
| Control population source | 0.28 | 0.44 | 0.083 | 0.072 | ||||
| Procedure to ascertain death | 0.27 | 0.43 | 0.58 | 0.71 | ||||
| Meta-regression analyses | ||||||||
| Latitude | 0.2 | 0.84 | 2.4 | 0.57 | 1.7 | 0.48 | 2.4 | 0.48 |
| Starting year of study | 0.2 | 0.85 | 0.3 | 0.83 | 5.0 | 0.21 | 0.1 | 0.88 |
| Duration of study, y§ | 21.6 | 0.047 | 8.7 | 0.28 | 23.9 | 0.008 | 10.1 | 0.154 |
| Included participants with hip fracture, n | 2.2 | 0.49 | 4.9 | 0.35 | 0.9 | 0.65 | 0.1 | 0.93 |
| Average age at hip fracture, y | 9.3 | 0.18 | 12.1 | 0.177 | 0.2 | 0.82 | 0.2 | 0.84 |
| Underlying risk∥ | 15.4 | 0.043 | 22.2 | 0.030 | 6.5 | 0.174 | 2.7 | 0.45 |
Between-group heterogeneity P value for categorical meta-analyses and model P value for meta-regression analyses. P values are presented without adjustment for multiple testing.
The outlying study is the Dubbo Osteoporosis Epidemiology Study, which was done in Australia and had a 15-year observation period (66). The authors acknowledge that there was probably selection bias in their study because participants were healthier than nonparticipants (67).
See Appendix Table 4.
See Appendix Figure 2.
See Appendix Figure 3.
Appendix Table 4.
Categorical Meta-analyses Exploring Heterogeneity of the Cumulative RHs for Short-Term (1-Year) All-Cause Mortality
| Region | Women | Men | ||||
|---|---|---|---|---|---|---|
| Studies, n | RH (95% CI) for All-Cause Mortality 1 Year After Hip Fracture | P Value* | Studies, n | RH (95% CI) for All-Cause Mortality 1 Year After Hip Fracture | P Value* | |
| All studies included* | <0.001 | <0.001 | ||||
| Americas | 7 | 2.55 (1.96–3.30) | 6 | 3.27 (2.85–3.75) | ||
| Europe | 13 | 2.90 (2.52–3.34) | 10 | 3.76 (3.20–4.42) | ||
| Southeast Asia | 1 | 2.29 (0.79–6.63) | – | – | ||
| Western Pacific (Australia)† | 1 | 6.09 (4.37–8.48) | 1 | 8.78 (6.05–12.76) | ||
| Outlying study omitted† | 0.64 | 0.19 | ||||
| Americas | 7 | 2.55 (1.96–3.30) | 6 | 3.27 (2.85–3.75) | ||
| Europe | 13 | 2.90 (2.52–3.34) | 10 | 3.76 (3.20–4.42) | ||
| Southeast Asia | 1 | 2.29 (0.79–6.63) | ||||
RH = relative hazard.
Between-group heterogeneity.
Appendix Table 5.
Potential Predictors of Underlying Risk (Percentage of All-Cause Mortality After 1 Year in Reference Population), Exploring Heterogeneity by Using Categorical and Meta-regression Analyses*
| Explanatory Variable | Women | Men | ||||||
|---|---|---|---|---|---|---|---|---|
| All Studies | Outlying Study Omitted† | All Studies | Outlying Study Omitted† | |||||
| R2, % | P Value | R2, % | P Value | R2, % | P Value | R2, % | P Value | |
| Categorical meta-analyses | ||||||||
| Region | 0.031 | 0.62 | <0.001 | 0.006 | ||||
| Control population source | 0.012 | 0.004 | 0.141 | 0.149 | ||||
| Procedure to ascertain death | 0.91 | 0.66 | 0.64 | 0.48 | ||||
| Meta-regression analyses | ||||||||
| Latitude | 9.7 | 0.073 | 2.9 | 0.34 | 0.1 | 0.89 | 0.3 | 0.84 |
| Starting year of study | 11.4 | 0.037 | 7.8 | 0.152 | 2.7 | 0.53 | 4.2 | 0.71 |
| Duration of study, y | 10.9 | 0.041 | 2.3 | 0.39 | 41.2 | <0.001 | 22.8 | 0.063 |
| Included participants with hip fracture, n | 2.5 | 0.44 | 2.1 | 0.49 | 8.0 | 0.32 | 8.4 | 0.33 |
Between-group heterogeneity P value for categorical meta-analyses and model P value for meta-regression analyses. P values are presented without adjustment for multiple testing.
Appendix Table 6.
Difference in Absolute Annual Risk for Death (Excess Mortality) From All Causes in U.S. Patients With Hip Fracture, by Age, Sex, and Time Since Injury*
| Age at the Time of Hip Fracture, y | Differences in Absolute Annual Risk for Death, by Years After Hip Fracture, % | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 Year | 2 Years (95% CI) | 3 Years | 4 Years | 5 Years (95% CI) | 6 Years | 7 Years | 8 Years | 9 Years | 10 Years (95% CI) | |
| Women | ||||||||||
| 70 | 3 | 5 (4–6) | 5 | 7 | 8 (6–13) | 10 | 11 | 13 | 14 | 16 (8–27) |
| 75 | 5 | 7 (6–9) | 8 | 10 | 13 (8–19) | 15 | 16 | 18 | 19 | 20 (11–33) |
| 80 | 8 | 11 (9–15) | 13 | 15 | 18 (12–27) | 20 | 21 | 22 | 23 | 22 (13–34) |
| 85 | 4 | 18 (15–23) | 19 | 21 | 24 (16–33) | 25 | 24 | 23 | 21 | 19 (12–25) |
| 90 | 22 | 26 (22–34) | 26 | 26 | 26 (19–34) | 24 | 20 | 17 | 14 | 10 (8–12) |
| Men | ||||||||||
| 70 | 7 | 9 (7–11) | 11 | 13 | 14 (10–19) | 15 | 15 | 17 | 18 | 19 (10–32) |
| 75 | 11 | 14 (12–17) | 16 | 18 | 20 (14–26) | 21 | 20 | 21 | 22 | 22 (12–34) |
| 80 | 18 | 22 (18–26) | 23 | 25 | 26 (19–33) | 25 | 24 | 23 | 22 | 20 (12–28) |
| 85 | 28 | 31 (26–37) | 31 | 31 | 30 (23–36) | 27 | 23 | 20 | 17 | 14 (10–18) |
| 90 | 43 | 42 (35–49) | 38 | 33 | 28 (23–32) | 22 | 17 | 13 | 10 | 7 (5–8) |
Estimates based on results from time-to-event meta-analyses of fracture cohort studies and life-table analyses applied to age- and sex-specific U.S. vital statistics for 2004 (32). The upper and lower 95% CIs of the pooled relative hazards were used to compute the corresponding upper and lower 95% CIs of excess mortality.
Footnotes
Author Contributions: Conception and design: P. Haentjens, S. Boonen.
Analysis of the data: P. Haentjens.
Interpretation of the data: P. Haentjens, S. Boonen, J. Magaziner, C.S. Colón-Emeric.
Drafting of the article: P. Haentjens, B. Velkeniers, S. Boonen.
Critical revision of the article for important intellectual content: P. Haentjens, J. Magaziner, C.S. Colón-Emeric, D. Vanderschueren, K. Milisen, B. Velkeniers, S. Boonen.
Final approval of the article: P. Haentjens, J. Magaziner, C.S. Colón-Emeric, D. Vanderschueren, K. Milisen, B. Velkeniers, S. Boonen.
Reproducible Research Statement: Study protocol and data set: Not available. Statistical code: Available from Dr. Haentjens (patrick.haentjens@uzbrussel.be).
Potential Conflicts of Interest: Disclosures can be viewed at www.acponline.org/authors/icmje/ConflictOfInterestForms.do?msNum=M09-0450.
References
- 1.Kanis JA, Borgstrom F, Zethraeus N, Johnell O, Oden A, Jönsson B. Intervention thresholds for osteoporosis in the UK. Bone. 2005;36:22–32. doi: 10.1016/j.bone.2004.08.018. [DOI] [PubMed] [Google Scholar]
- 2.Kanis JA, Johnell O, Oden A, Borgstrom F, Johansson H, De Laet C, et al. Intervention thresholds for osteoporosis in men and women: a study based on data from Sweden. Osteoporos Int. 2005;16:6–14. doi: 10.1007/s00198-004-1623-4. [DOI] [PubMed] [Google Scholar]
- 3.Tosteson AN, Jo¨nsson B, Grima DT, O’Brien BJ, Black DM, Adachi JD. Challenges for model-based economic evaluations of postmenopausal osteoporosis interventions. Osteoporos Int. 2001;12:849–57. doi: 10.1007/s001980170036. [DOI] [PubMed] [Google Scholar]
- 4.Tosteson AN, Gottlieb DJ, Radley DC, Fisher ES, Melton LJ., 3rd Excess mortality following hip fracture: the role of underlying health status. Osteoporos Int. 2007;18:1463–72. doi: 10.1007/s00198-007-0429-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Magaziner J, Lydick E, Hawkes W, Fox KM, Zimmerman SI, Epstein RS, et al. Excess mortality attributable to hip fracture in white women aged 70 years and older. Am J Public Health. 1997;87:1630–6. doi: 10.2105/ajph.87.10.1630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Forsén L, Sogaard AJ, Meyer HE, Edna T, Kopjar B. Survival after hip fracture: short- and long-term excess mortality according to age and gender. Osteoporos Int. 1999;10:73–8. doi: 10.1007/s001980050197. [DOI] [PubMed] [Google Scholar]
- 7.Cauley JA, Thompson DE, Ensrud KC, Scott JC, Black D. Risk of mortality following clinical fractures. Osteoporos Int. 2000;11:556–61. doi: 10.1007/s001980070075. [DOI] [PubMed] [Google Scholar]
- 8.Empana JP, Dargent-Molina P, Bréart G EPIDOS Group. Effect of hip fracture on mortality in elderly women: the EPIDOS prospective study. J Am Geriatr Soc. 2004;52:685–90. doi: 10.1111/j.1532-5415.2004.52203.x. [DOI] [PubMed] [Google Scholar]
- 9.Holmberg S, Conradi P, Kalén R, Thorngren KG. Mortality after cervical hip fracture. 3002 patients followed for 6 years. Acta Orthop Scand. 1986;57:8–11. doi: 10.3109/17453678608993205. [DOI] [PubMed] [Google Scholar]
- 10.Elmerson S, Zetterberg C, Andersson GB. Ten-year survival after fractures of the proximal end of the femur. Gerontology. 1988;34:186–91. doi: 10.1159/000212951. [DOI] [PubMed] [Google Scholar]
- 11.Schrøder HM, Erlandsen M. Age and sex as determinants of mortality after hip fracture: 3,895 patients followed for 2.5-18.5 years. J Orthop Trauma. 1993;7:525–31. doi: 10.1097/00005131-199312000-00007. [DOI] [PubMed] [Google Scholar]
- 12.Poór G, Atkinson EJ, O’Fallon WM, Melton LJ., 3rd Determinants of reduced survival following hip fractures in men. Clin Orthop Relat Res. 1995:260–5. [PubMed] [Google Scholar]
- 13.Trombetti A, Herrmann F, Hoffmeyer P, Schurch MA, Bonjour JP, Rizzoli R. Survival and potential years of life lost after hip fracture in men and age-matched women. Osteoporos Int. 2002;13:731–7. doi: 10.1007/s001980200100. [DOI] [PubMed] [Google Scholar]
- 14.Petersen MB, Jørgensen HL, Hansen K, Duus BR. Factors affecting post-operative mortality of patients with displaced femoral neck fracture. Injury. 2006;37:705–11. doi: 10.1016/j.injury.2006.02.046. [DOI] [PubMed] [Google Scholar]
- 15.Robbins JA, Biggs ML, Cauley J. Adjusted mortality after hip fracture: From the cardiovascular health study. J Am Geriatr Soc. 2006;54:1885–91. doi: 10.1111/j.1532-5415.2006.00985.x. [DOI] [PubMed] [Google Scholar]
- 16.Giversen IM. Time trends of mortality after first hip fractures. Osteoporos Int. 2007;18:721–32. doi: 10.1007/s00198-006-0300-1. [DOI] [PubMed] [Google Scholar]
- 17.Katz MH. Multivariable analysis: a primer for readers of medical research. Ann Intern Med. 2003;138:644–50. doi: 10.7326/0003-4819-138-8-200304150-00012. [DOI] [PubMed] [Google Scholar]
- 18.Tierney JF, Stewart LA, Ghersi D, Burdett S, Sydes MR. Practical methods for incorporating summary time-to-event data into meta-analysis. Trials. 2007;8:16. doi: 10.1186/1745-6215-8-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schlesselman JJ. Risk of endometrial cancer in relation to use of combined oral contraceptives. A practitioner’s guide to meta-analysis. Hum Reprod. 1997;12:1851–63. doi: 10.1093/humrep/12.9.1851. [DOI] [PubMed] [Google Scholar]
- 20.Kanis JA, Johnell O, Oden A, Jonsson B, Dawson A, Dere W. Risk of hip fracture derived from relative risks: an analysis applied to the population of Sweden. Osteoporos Int. 2000;11:120–7. doi: 10.1007/PL00004173. [DOI] [PubMed] [Google Scholar]
- 21.Parmar MK, Torri V, Stewart L. Extracting summary statistics to perform meta-analyses of the published literature for survival endpoints. Stat Med. 1998;17:2815–34. doi: 10.1002/(sici)1097-0258(19981230)17:24<2815::aid-sim110>3.0.co;2-8. [DOI] [PubMed] [Google Scholar]
- 22.Sutton A, Abrams K, Jones D, et al. Wiley Series in Probability and Statistics. Chichester, UK: J Wiley; 2000. Methods for Meta-Analysis in Medical Research. [Google Scholar]
- 23.Williamson PR, Clough HE, Hutton JL, Marson AG, Chadwick DW. Statistical issues in the assessment of the evidence for an interaction between factors in epilepsy trials. Stat Med. 2002;21:2613–22. doi: 10.1002/sim.1044. [DOI] [PubMed] [Google Scholar]
- 24.Deeks JJ, Altman DG, Bradburn MJ. Statistical methods for examining heterogeneity and combining results from several studies in meta-analysis. In: Egger M, Smith GD, Altman DG, editors. Systematic Reviews in Healthcare: Meta-analysis in Context. 2. London: BMJ; 2001. pp. 285–312. [Google Scholar]
- 25.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–58. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 27.Lipsey MW, Wilson DB. Applied Societal Research Methods Series. Vol. 49. Newbury Park, CA: Sage; 2001. Practical Meta-analysis. [Google Scholar]
- 28.Johnell O, Kanis JA. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int. 2006;17:1726–33. doi: 10.1007/s00198-006-0172-4. [DOI] [PubMed] [Google Scholar]
- 29.Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50:1088–101. [PubMed] [Google Scholar]
- 30.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–34. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Borenstein M, Hedges L, Higgins J, Rothstein H. Introduction to Meta analysis. Hoboken, NJ: J Wiley; 2009. [Google Scholar]
- 32.Arias E. National vital statistics reports. 9. Vol. 56. Hyattsville, MD: National Center for Health Statistics; 2007. United States life tables, 2004. [PubMed] [Google Scholar]
- 33.Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283:2008–12. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 34.Miller CW. Survival and ambulation following hip fracture. J Bone Joint Surg Am. 1978;60:930–4. [PubMed] [Google Scholar]
- 35.Clayer MT, Bauze RJ. Morbidity and mortality following fractures of the femoral neck and trochanteric region: analysis of risk factors. J Trauma. 1989;29:1673–8. doi: 10.1097/00005373-198912000-00016. [DOI] [PubMed] [Google Scholar]
- 36.de Palma L, Rizzi L, Lorini G, Greco F. Survival after trochanteric fracture. Biological factors analyzed in 270 patients. Acta Orthop Scand. 1992;63:645–7. doi: 10.1080/17453679209169727. [DOI] [PubMed] [Google Scholar]
- 37.Cooper C, Atkinson EJ, Jacobsen SJ, O’Fallon WM, Melton LJ., 3rd Population-based study of survival after osteoporotic fractures. Am J Epidemiol. 1993;137:1001–5. doi: 10.1093/oxfordjournals.aje.a116756. [DOI] [PubMed] [Google Scholar]
- 38.Pitto RP. The mortality and social prognosis of hip fractures. A prospective multifactorial study. Int Orthop. 1994;18:109–13. doi: 10.1007/BF02484420. [DOI] [PubMed] [Google Scholar]
- 39.Katelaris AG, Cumming RG. Health status before and mortality after hip fracture. Am J Public Health. 1996;86:557–60. doi: 10.2105/ajph.86.4.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cooper C. The crippling consequences of fractures and their impact on quality of life. Am J Med. 1997;103:12S–17S. doi: 10.1016/s0002-9343(97)90022-x. discussion 17S-19S. [DOI] [PubMed] [Google Scholar]
- 41.Meyer HE, Tverdal A, Falch JA, Pedersen JI. Factors associated with mortality after hip fracture. Osteoporos Int. 2000;11:228–32. doi: 10.1007/s001980050285. [DOI] [PubMed] [Google Scholar]
- 42.Willig R, Keinänen-Kiukaaniemi S, Jalovaara P. Mortality and quality of life after trochanteric hip fracture. Public Health. 2001;115:323–7. doi: 10.1038/sj.ph.1900773. [DOI] [PubMed] [Google Scholar]
- 43.Richmond J, Aharonoff GB, Zuckerman JD, Koval KJ. Mortality risk after hip fracture. J Orthop Trauma. 2003;17:53–6. doi: 10.1097/00005131-200301000-00008. [DOI] [PubMed] [Google Scholar]
- 44.Tjiang GC, Koppert CL, Hermans ET, Poelhekke LM, Dawson I. Replacement of the femoral head due to fracture of the hip: prognostic factors for the duration of hospitalisation, institutionalisation and mortality. Ned Tijdschr Geneeskd. 2003;147:2483–7. [PubMed] [Google Scholar]
- 45.Muraki S, Yamamoto S, Ishibashi H, Nakamura K. Factors associated with mortality following hip fracture in Japan. J Bone Miner Metab. 2006;24:100–4. doi: 10.1007/s00774-005-0654-z. [DOI] [PubMed] [Google Scholar]
- 46.Tsuboi M, Hasegawa Y, Suzuki S, Wingstrand H, Thorngren KG. Mortality and mobility after hip fracture in Japan: a ten-year follow-up. J Bone Joint Surg Br. 2007;89:461–6. doi: 10.1302/0301-620X.89B4.18552. [DOI] [PubMed] [Google Scholar]
- 47.Vestergaard P, Rejnmark L, Mosekilde L. Increased mortality in patients with a hip fracture-effect of pre-morbid conditions and post-fracture complications. Osteoporos Int. 2007;18:1583–93. doi: 10.1007/s00198-007-0403-3. [DOI] [PubMed] [Google Scholar]
- 48.de Luise C, Brimacombe M, Pedersen L, Sørensen HT. Chronic obstructive pulmonary disease and mortality following hip fracture: a population-based cohort study. Eur J Epidemiol. 2008;23:115–22. doi: 10.1007/s10654-007-9211-5. [DOI] [PubMed] [Google Scholar]
- 49.Ryg J, Rejnmark L, Overgaard S, Brixen K, Vestergaard P. Hip fracture patients at risk of second hip fracture: a nationwide population-based cohort study of 169,145 cases during 1977-2001. J Bone Miner Res. 2009;24:1299–307. doi: 10.1359/jbmr.090207. [DOI] [PubMed] [Google Scholar]
- 50.Poór G, Atkinson EJ, Lewallen DG, O’Fallon WM, Melton LJ., 3rd Age-related hip fractures in men: clinical spectrum and short-term outcomes. Osteoporos Int. 1995;5:419–26. doi: 10.1007/BF01626602. [DOI] [PubMed] [Google Scholar]
- 51.Poór G, Atkinson EJ, O’Fallon WM, Melton LJ., 3rd Predictors of hip fractures in elderly men. J Bone Miner Res. 1995;10:1900–7. doi: 10.1002/jbmr.5650101209. [DOI] [PubMed] [Google Scholar]
- 52.Center JR, Nguyen TV, Schneider D, Sambrook PN, Eisman JA. Mortality after all major types of osteoporotic fracture in men and women: an observational study. Lancet. 1999;353:878–82. doi: 10.1016/S0140-6736(98)09075-8. [DOI] [PubMed] [Google Scholar]
- 53.Jensen JS, Tøndevold E. Mortality after hip fractures. Acta Orthop Scand. 1979;50:161–7. doi: 10.3109/17453677908989751. [DOI] [PubMed] [Google Scholar]
- 54.Dahl E. Mortality and life expectancy after hip fractures. Acta Orthop Scand. 1980;51:163–70. doi: 10.3109/17453678008990781. [DOI] [PubMed] [Google Scholar]
- 55.Magaziner J, Simonsick EM, Kashner TM, Hebel JR, Kenzora JE. Survival experience of aged hip fracture patients. Am J Public Health. 1989;79:274–8. doi: 10.2105/ajph.79.3.274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Fisher ES, Baron JA, Malenka DJ, Barrett JA, Kniffin WD, Whaley FS, et al. Hip fracture incidence and mortality in New England. Epidemiology. 1991;2:116–22. doi: 10.1097/00001648-199103000-00005. [DOI] [PubMed] [Google Scholar]
- 57.Eiskjaer S, Ostgård SE, Jakobsen BW, Jensen J, Lucht U. Years of potential life lost after hip fracture among postmenopausal women. Acta Orthop Scand. 1992;63:293–6. doi: 10.3109/17453679209154785. [DOI] [PubMed] [Google Scholar]
- 58.Jacobsen SJ, Goldberg J, Miles TP, Brody JA, Stiers W, Rimm AA. Race and sex differences in mortality following fracture of the hip. Am J Public Health. 1992;82:1147–50. doi: 10.2105/ajph.82.8.1147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lu-Yao GL, Baron JA, Barrett JA, Fisher ES. Treatment and survival among elderly Americans with hip fractures: a population-based study. Am J Public Health. 1994;84:1287–91. doi: 10.2105/ajph.84.8.1287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Browner WS, Pressman AR, Nevitt MC, Cummings SR. Mortality following fractures in older women. The study of osteoporotic fractures. Arch Intern Med. 1996;156:1521–5. [PubMed] [Google Scholar]
- 61.Jitapunkul S, Yuktanandana P. Consequences of hip fracture among Thai women aged 50 years and over: a prospective study. J Med Assoc Thai. 2000;83:1447–51. [PubMed] [Google Scholar]
- 62.Fitzpatrick P, Kirke PN, Daly L, Van Rooij I, Dinn E, Burke H, et al. Predictors of first hip fracture and mortality post fracture in older women. Ir J Med Sci. 2001;170:49–53. doi: 10.1007/BF03167722. [DOI] [PubMed] [Google Scholar]
- 63.Haentjens P, Autier P, Barette M, Boonen S Belgian Hip Fracture Study Group. The economic cost of hip fractures among elderly women. A one-year, prospective, observational cohort study with matched-pair analysis. Belgian Hip Fracture Study Group. J Bone Joint Surg Am. 2001;83-A:493–500. [PubMed] [Google Scholar]
- 64.Farahmand BY, Michaëlsson K, Ahlbom A, Ljunghall S, Baron JA Swedish Hip Fracture Study Group. Survival after hip fracture. Osteoporos Int. 2005;16:1583–90. doi: 10.1007/s00198-005-2024-z. [DOI] [PubMed] [Google Scholar]
- 65.Pande I, Scott DL, O’Neill TW, Pritchard C, Woolf AD, Davis MJ. Quality of life, morbidity, and mortality after low trauma hip fracture in men. Ann Rheum Dis. 2006;65:87–92. doi: 10.1136/ard.2004.034611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Bliuc D, Nguyen ND, Milch VE, Nguyen TV, Eisman JA, Center JR. Mortality risk associated with low-trauma osteoporotic fracture and subsequent fracture in men and women. JAMA. 2009;301:513–21. doi: 10.1001/jama.2009.50. [DOI] [PubMed] [Google Scholar]
- 67.Nguyen ND, Ahlborg HG, Center JR, Eisman JA, Nguyen TV. Residual lifetime risk of fractures in women and men. J Bone Miner Res. 2007;22:781–8. doi: 10.1359/jbmr.070315. [DOI] [PubMed] [Google Scholar]
- 68.Handoll HH, Farrar MJ, McBirnie J, Tytherleigh-Strong G, Milne AA, Gillespie WJ. Heparin, low molecular weight heparin and physical methods for preventing deep vein thrombosis and pulmonary embolism following surgery for hip fractures. Cochrane Database Syst Rev. 2002:CD000305. doi: 10.1002/14651858.CD000305. [DOI] [PubMed] [Google Scholar]
- 69.Roche JJ, Wenn RT, Sahota O, Moran CG. Effect of comorbidities and postoperative complications on mortality after hip fracture in elderly people: prospective observational cohort study. BMJ. 2005;331:1374. doi: 10.1136/bmj.38643.663843.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Wehren LE, Hawkes WG, Orwig DL, Hebel JR, Zimmerman SI, Magaziner J. Gender differences in mortality after hip fracture: the role of infection. J Bone Miner Res. 2003;18:2231–7. doi: 10.1359/jbmr.2003.18.12.2231. [DOI] [PubMed] [Google Scholar]
- 71.Hawkes WG, Wehren L, Orwig D, Hebel JR, Magaziner J. Gender differences in functioning after hip fracture. J Gerontol Med Sci. 2006;61A:495–9. doi: 10.1093/gerona/61.5.495. [DOI] [PubMed] [Google Scholar]
- 72.Boonen S, Autier P, Barette M, Vanderschueren D, Lips P, Haentjens P. Functional outcome and quality of life following hip fracture in elderly women: a prospective controlled study. Osteoporos Int. 2004;15:87–94. doi: 10.1007/s00198-003-1515-z. [DOI] [PubMed] [Google Scholar]
- 73.Magaziner J, Hawkes W, Hebel JR, Zimmerman SI, Fox KM, Dolan M, et al. Recovery from hip fracture in eight areas of function. J Gerontol A Biol Sci Med Sci. 2000;55A:M498–507. doi: 10.1093/gerona/55.9.m498. [DOI] [PubMed] [Google Scholar]
- 74.Cree M, Soskolne CL, Belseck E, Hornig J, McElhaney JE, Brant R, et al. Mortality and institutionalization following hip fracture. J Am Geriatr Soc. 2000;48:283–8. doi: 10.1111/j.1532-5415.2000.tb02647.x. [DOI] [PubMed] [Google Scholar]
- 75.Ensrud KE, Ewing SK, Taylor BC, Fink HA, Stone KL, Cauley JA, et al. for the Study of Osteoporotic Fractures Research Group Frailty and risk of falls, fracture, and mortality in older women: the study of osteoporotic fractures. J Gerontol A Biol Sci Med Sci. 2007;62:744–51. doi: 10.1093/gerona/62.7.744. [DOI] [PubMed] [Google Scholar]
- 76.Hamerman D. Toward an understanding of frailty. Ann Intern Med. 1999;130:945–50. doi: 10.7326/0003-4819-130-11-199906010-00022. [DOI] [PubMed] [Google Scholar]
- 77.Ferrucci L, Guralnik JM, Studenski S, Fried LP, Cutler GB, Jr, Walston JD Interventions on Frailty Working Group. Designing randomized, controlled trials aimed at preventing or delaying functional decline and disability in frail, older persons: a consensus report. J Am Geriatr Soc. 2004;52:625–34. doi: 10.1111/j.1532-5415.2004.52174.x. [DOI] [PubMed] [Google Scholar]
- 78.Miller RR, Cappola AR, Shardell MD, Hawkes WG, Yu-Yahiro JA, Hebel JR, et al. Persistent changes in interleukin-6 and lower extremity function following hip fracture. J Gerontol Med Sci. 2006;61A:1053–8. doi: 10.1093/gerona/61.10.1053. [DOI] [PubMed] [Google Scholar]