Summary
Introduction
In 2005 a visceral leishmaniasis (VL) elimination initiative was launched on the Indian subcontinent, with early diagnosis based on a rapid diagnostic test and treatment with the oral drug miltefosine as its main strategy. Several recent studies have signaled underreporting of VL cases in the region. Information on treatment outcomes is scanty. We conducted a study to document VL case management by the primary health care services in India.
Methods
We took a random sample of all VL patients registered in rural PHC facilities of Muzaffarpur district, Bihar, India during 2008. Patients were traced at home for an interview and their records were reviewed. We recorded patient and doctor delay, treatment regimens, treatment outcomes and costs incurred by patients.
Results
We could review records of all 150 patients sampled and interview 139 patients or their guardian. Most patients (81%) had first presented to unqualified practitioners; median delay before reaching the appropriate primary healthcare facility was 40 days (IQR 31-59 days). Existing networks of village health workers were under utilized. Forty eight percent of VL patients were treated with antimonials; 40% of those needed a second treatment course. Median direct expenditure by patients was 4000 rupees per episode (IQR 2695 – 5563 rupees), equivalent to almost two months of household income.
Conclusion
In 2008 there were still critical flaws in VL case management in the primary health care services in Bihar: obsolete use of antimonials with high failure rates and long patient delay. To meet the target of the VL elimination, more active case detection strategies are needed, and the existing village health worker networks could be more involved. Costs to patients remain an obstacle to early case finding.
Introduction
Visceral leishmaniasis (VL) is a vector-borne parasitic disease which is nearly always fatal if left untreated (Barnett et al. 2005; Bern et al. 2005). The clinical syndrome is characterized by fever, weight loss, splenomegaly, hepatomegaly and anemia. Though the disease is endemic in over 60 countries, 90% of all reported cases occur in just 5 countries: Bangladesh, Brazil, India, Nepal and Sudan. The estimated population at risk on the Indian subcontinent is around 200 million, the estimated annual incidence about 420,000. The disease affects mainly poor rural communities; of all cases reported in the region, almost 50% are from the state of Bihar in India (Joshi et al. 2008).
In 2005 the VL endemic countries of the South-East Asia region, Bangladesh, India and Nepal, agreed upon a regional strategic framework for elimination of VL from the Indian subcontinent (WHO, 2005). The target set for India is to reduce the annual incidence of VL at block level (an administrative division covering 100 000 to 300 000 inhabitants, see below) to less than one new case per 10,000 population by 2015. The main strategy to achieve this is entrusted to the public sector primary health care (PHC) services that should ensure early diagnosis and treatment. Any patient residing in a VL endemic area and presenting with a history of fever of more than two weeks duration with no response to antibiotics and antimalarials is to be tested for VL with an rK-39 dipstick test. Those testing positive are to be treated in first intention with oral miltefosine; amphotericin B is used in second intention for those not responding to miltefosine. VL drugs and diagnostics should be free to the patient in the public sector.
Recently, there have been various accounts of underreporting of VL in the PHC sector in Bihar with an estimated 76-88% of cases not being reported (Singh SP et al. 2006; Singh VP et al. 2010). Moreover during visits to health centres in two districts of Bihar State in April 2009, we observed that rK39 dipstick tests were often not available and that in case of VL suspicion, patients were referred to private-for-profit facilities for diagnosis. Most patients were treated with sodium stibogluconate (SSG) notwithstanding the program recommendation to use miltefosine. SSG has to be administered by intra muscular injection but no specific arrangements were being made for this. Vials of SSG were provided one at a time by the health centre to the patient or a relative. For the average adult patient this meant 10 visits to the centre over a 30-day period. Experience with other chronic diseases such as tuberculosis has shown that unless special measures are taken, compliance with treatment is the exception rather than the rule (Sbarbaro, 2004). Yet in the facilities visited, out of over 900 patients treated during 2008, not one single patient was reported to have defaulted. Though Sundar et al. (2001) documented high levels of resistance against SSG in Bihar State as early as 2001, among over 800 VL cases treated with SSG in 2008, according to the records there had been no more than 10 treatment failures. A patient was assumed to have been successfully treated if all vials prescribed had been collected. The reporting format used did not distinguish between ‘new cases’, ‘relapses’ and ‘treatment after failure’ and as treatment outcome only ‘death’ or ‘successful treatment’ were routinely reported.
Our observations raised several questions. The fact that a substantial proportion of patients were referred to private-for-profit laboratories for diagnosis could be a reason for underreporting of VL. Since VL patients are known to be among the poorest of the poor, having to pay for diagnostic tests could be a major obstacle (Boelaert et al. 2009). Moreover treatment outcomes reported seemed at odds with earlier reports on SSG resistance by Sundar et al. albeit from a specialised treatment centre. We therefore initiated a study to investigate healthcare seeking behaviour of VL patients treated in PHC facilities and document their treatment outcomes as well as direct costs incurred.
Methods
Background
Administratively, India is made up of 28 states; each state is divided into districts and districts are divided into blocks of approximately 100,000 to 300,000 inhabitants. Each district capital has a district hospital that functions as referral level for the block primary health care system. In rural areas, primary health care services at block level have been organized as a 3-tier system, made up of community health centers, primary health centers and health sub-centers. The highest level within the block is the community health center, which according to the norms should cater for a population of 120,000 and support 4 primary health centers and 24 sub-centers. The primary health center is the first level at which a physician is available. Sub-centers are the most peripheral unit and are staffed by midlevel health workers, one female and one male; these health workers are referred to as auxiliary nurse/midwife or ANM. At village level there is a network of volunteers, also known as ‘accredited social health activists’ or ASHA's, who constitute the link between the PHC system and the community (WHO1; WHO2). The community health center is the level at which VL diagnostics and drugs should be freely available and to which lower echelons in the PHC system should refer suspect cases. Our study was conducted in Muzaffarpur district of Bihar state, a district with an estimated 4,503,397 inhabitants. The district which has 14 rural blocks with a total population of 3,994,175, each served by one community health center, was among the pilot districts to be supplied with miltefosine at the time of our study. The average population per community health center is thus 285,000, more than twice the target of 120,000; in all 14 rural blocks of Muzaffapur district there are altogether only 4 functioning primary health centers.
Study design
We conducted a random cross-sectional survey of all VL patients registered in the public sector PHC services of all rural blocks of Muzaffarpur district during 2008; these blocks are known to be highly endemic for VL. We compiled a list of all cases reported by the community health centres in each of these blocks and took a random sample of 150. Study subjects had their medical records reviewed and were visited at home for an interview. In case a patient was a minor we interviewed a guardian; for patients who had died we tried to interview relatives.
Two sets of questionnaires were developed and pretested, one questionnaire for the review of patient records, another questionnaire for patient interviews. Reviews of patient records were done by a physician with experience in treatment of VL; patient interviews were conducted by a team of trained field workers who had also been involved in earlier studies in the area.
Case definitions
As case definition for VL we adopted the standard definition used by the PHC system, i.e. a patient with a history of fever of more than two weeks duration with no response to antibiotics and antimalarials, and a positive result of the rK-39 dipstick test and/or positive on parasitological examination.
We categorized treatment outcomes using definitions adapted from those used in tuberculosis control (WHO, 2003). As treatment outcome categories we used ‘treatment success’, ‘treatment failure’, ‘relapse’, ‘defaulted’, ‘transferred out’, referred to higher level', ‘died’ and ‘other’. Patients who had taken all the prescribed treatment, had been discharged in good clinical condition and were not known to have relapsed at the time of the study were classified as ‘treatment success’. Treatment failure was defined as no clinical improvement noted during or at the end of the treatment; relapse was defined as the return of signs and symptoms of VL after initially having been considered successfully treated, with or without parasitological confirmation. ‘Defaulted’ was defined as a patient who did not come to pick up the remainder of his treatment before completion, resulting in a treatment “break” of more than one week. ‘Transferred out’ was defined as the patient being transferred to another facility for non-medical reasons, those referred to higher levels for medical reasons were classified as ‘referred to higher level’. Any patient reported to have died from whatever cause was classified as ‘died’; patients not fitting any of the above categories were classified as ‘other’. We made a distinction between patients never treated before and patients with a history of previous treatment. Treatment results from the records were triangulated with results from interviews; patients were asked whether (first) treatment had been effective, how they would describe their state of health at the end of treatment and whether they had needed a second treatment for VL.
In the public sector, diagnosis and treatment for VL are only available at community health center level. Mindful of the fact that a wide array of formal and informal health care services exists in rural areas of India (Kumar et al. 2007) and that even after having consulted lower echelons of the PHC system patients may still delay presenting to a community health center, we defined patient's delay as the time between onset of symptoms and first presentation to a community health center. Health system's delay was defined as the time between first presentation at a community health center and start of treatment for VL. For those first presenting to an ANM or ASHA, we also calculated the time between presenting to ANM or ASHA and presenting at a community health center.
Direct costs to patients were estimated by asking each patient how much had been spent in Indian rupees on consultation fees, diagnostic tests, drugs, other treatment services, admission fees, travel and other charges for each provider visited in the course of diagnosis and treatment.
Sample size
Sample size was calculated to estimate treatment defaulter rates with adequate precision, and based on the assumption that at least 10% of patients do not complete VL treatment. To estimate a factor present in 10% of cases with a precision of ±5% and an α-error of 0.05 requires a sample size of 138. To account for the fact that some patients may be absent or may not agree to cooperate, we set the sample size at 150.
Ethical aspects
Ethical clearance was obtained from the ethics committee of Banaras Hindu University in Varanasi, India, as well as from the ethics committee of the University of Antwerp, Belgium. Any person identified with (suspected) VL in the process of the study, whether due to treatment failure/relapse or a first episode, was eligible for free diagnosis and treatment at the Kala-azar Medical Research Centre (KAMRC) in Muzaffarpur.
Data management
Data was double entered in a Microsoft Access database independently by 2 data entry clerks. Upon completion of the 2nd entry, the two files were compared. In case of discrepancies corrections were made after reviewing the original questionnaire forms.
Data analysis
For data analysis we used Stata/ IC V10.1 (Stata Corp., College Station Tx, USA). We calculated proportions and confidence intervals and medians with interquartile ranges as required.
Results
During the year 2008 the 14 rural blocks of Muzaffarpur district reported a total of 1878 VL cases, with a median by block of 106 cases (IQR 71-182) and a range from 8 cases to 409 cases. Of 150 cases sampled, all had their medical records reviewed and 138 could be personally interviewed; for one patient who had died we were able to interview the relatives. There were 11 patients who could not be interviewed, out of those one was known to have died. In all 11 cases the addresses recorded at the community health centers were inaccurate, making it impossible to locate the homes of the patients.
Seventy seven patients (51.3%) were male; the median age was 18 years (IQR 10- 35 years). Fever, loss of appetite, weight loss and swelling of the abdomen were the initial symptoms reported by the vast majority of patients interviewed (100%, 97.8%, 94.2% and 74.8% respectively). One hundred thirty two patients (88.0%, 95% CI 82.7-93.3%) had been diagnosed on the basis of clinical symptoms plus a positive rK39 dipstick test, the remaining 18 patients (12.0% 95% CI 6.7-17.3%) had been parasitologically confirmed.
Choice of provider
Out of 139 patients interviewed, 113 (81.3%, 95% CI 74.7- 87.9%) had first reported to an unqualified local practitioner; 12 (8.6%, 95% CI 3.9-13.4%) had reported to a qualified private practitioner and 14 (10.1%, 95% CI 5.0- 15.1%) had reported directly to the PHC system. Of those reporting directly to the PHC system, 12 (8.6%, 95% CI 3.9-13.4% of all patients) had first reported to an ANM or ASHA, 2 (1.4%, 95% CI 0-3.4% of all cases) had reported directly to a community health center.
Delay
Median patient delay between onset of symptoms and reporting to the community health centre was 40 days (IQR 31-59 days). Once the patient had reported to the community health center, system's delay was minimal with a median of 2 days till start of treatment (IQR 1-4 days). Those first reporting to an ANM or ASHA (n=12) had a median delay of a further 36 days (IQR 28-56 days) before reporting to a community health center. Out of 139 patients interviewed, 79 (56.8%, 95% CI 48.5-65.2%) had completed the full diagnostic process at the community health center, 58 (41.7%, 95% CI 33.4 – 50.0%) had been referred by the doctor of the community health centre to a private-for-profit laboratory for a VL diagnostic test, the remaining 2 patients (1.4%, 95% CI 0-3.4%)) had been diagnosed at an NGO facility.
Treatment regimens and treatment outcomes
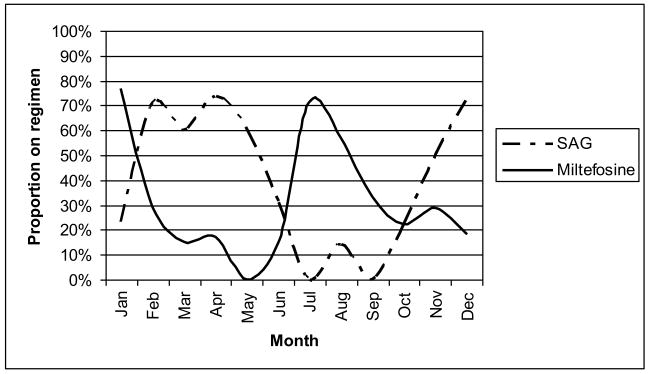
Out of 150 patients assessed, eight had a history of previous treatment for VL. Excluding those eight patients, 68 (47.9%, 95% CI 39.6-56.2%) were prescribed SSG as initial treatment regimen, 43 (30.3%, 95%CI 22.6 – 38.0%) were prescribed miltefosine and the remaining 31 (21.8%, 95% CI 15.0-28.7%) were prescribed amphotericin B. Excluding three blocks from which five or less patients were assessed, the percentage of patients on SSG by block ranged from 36 to 90%. We hypothesized that possibly in the course of the year SSG had gradually been replaced by miltefosine as a first line treatment but this was not the case as shown in figure 1. The cyclical patterns observed suggest that during some periods of the year Miltefosine was not available and that SSG was used instead.
Figure 1.
Proportions of patients prescribed SSG and miltefosine by month during the year 2008
Compliance was excellent according to the records. Excluding those who defaulted, died or were transferred, 94.0% of patients (95% CI 90.0-98.1%) had collected at least 90% of prescribed treatment dosages. This was confirmed by the patients; 91.9% (95% CI 87.0-96.8%) of those that did not die or default and were not transferred said that they had taken all medicines as prescribed.
First treatment outcomes varied by treatment regimen. Out of 68 patients without a history of previous treatment treated on SSG, 51 (75.0%, 95% CI 64.4-85.6%) were classified as treatment success according to the patient records. Thirty seven out of 43 patients (86.0%, 95% CI 75.3-96.8%) were successfully treated with miltefosine; for amphotericin B the figures were 29 out of 31 (93.5%, 95% CI 84.4-100%). First treatment results assessed from patient interviews were worse with very consistent replies to the 3 related questions asked. Twenty seven out of 67 patients treated with SSG interviewed (40.3%, 95% CI 28.2 – 52.4%) had needed a second treatment course for VL. Six out of 40 patients treated with miltefosine (15.0%, 95% CI 4.4 – 26.6%) and three out of 24 patients treated with amphotericin B (12.5%, 95% CI 0 – 26.8%) had needed a second VL treatment. Details on first treatment outcomes are presented in table 1 and 2.
Table 1.
Treatment outcomes by regimen for patients without a history of previous VL treatment (based on data retrieved from patient records at community health centers)
| Outcome/ Regimen | SSG (95% CI) |
miltefosine (95% CI) |
amphotericin B (95% CI) |
All (95% CI) |
|---|---|---|---|---|
| Treatment success | 51 (75%) (64-86%) |
37 (86%) (75-97%) |
29 (94%) (84-100%) |
117 (82.4%) (76.1-88.7%) |
| Failure | 2 (3%) (0-7%) |
0 | 0 | 2 (1.4%) (0-3.4%) |
| Defaulted | 4 (6%) (0-12%) |
3 (7%) (0-15%) |
1 (3%) (0-10%) |
8 (5.6%) (1.8-9.5%) |
| Died | 1 (1%) (0-4%) |
1 (2%) (0-7%) |
0 | 2 (1.4%) (0-3.4%) |
| Referred | 8 (12%) (4-20%) |
2 (5%) (0-11%) |
1 (3%) (0-10%) |
11 (7.7%) (3.3 -12.2%) |
| Transferred out | 2 (3%) (0-7%) |
0 | 0 | 2 (1.4%) (0-3.4%) |
| Total | 68 | 43 | 31 | 142 |
Table 2.
Treatment results by regimen for patients without a history of previous VL treatment (based on data from interviews with patients)
| Result/ Regimen | SSG (95% CI) |
miltefosine (95% CI) |
amphotericin B (95% CI) |
All (95% CI) |
|---|---|---|---|---|
| Was treatment effective? | ||||
| - Yes | 41 (61%) (49-73%) |
34 (85%) (73-97%) |
22 (92%) (80-100%) |
97 (74.0%) (66.4-81.7%) |
| - Moderately | 8 (12%) (4-20%) |
2 (5%) (0-12%) |
1 (4%) (0-13%) |
11(8.4%) (3.6 -13.2%) |
| - No | 18 (27%) (16-38%) |
4 (10%) (0-20%) |
1(4%) (0-13%) |
23 (17.6%) (11.0-24.2%) |
| State of health at end of first treatment? | ||||
| - Good | 41 (61%) (49-73%) |
34 (85%) (73-97%) |
22 (92%) (80-100%) |
97 (74.0%) (66.4-81.7% |
| - Better, not good | 8 (12%) (4-20%) |
1 (3%) (0-8%) |
1 (4%) (0-13%) |
10 (7.6%) (3.0 -12.2%) |
| - Unchanged or worse | 18 (27%) (16-38%) |
5 (13%) (2-20%) |
1 (4%) (0-13%) |
24 (18.3%) (11.6 -25.0%) |
| Needed 2nd treatment? | ||||
| - Yes | 27 (40%) (28-52%) |
6 (15%) (3-27%) |
3 (13%) (0-27%) |
36 (27.5%) (19.7-35.2%) |
| - No | 40 (60%) (48-72%) |
34 (85%) (73-97%) |
21 (88%) (73-100%) |
95 (72.5%) (64.8-80.3%) |
Of those who had required a second VL treatment, 7 had been retreated at PHC level, 11 at a district hospital, 5 by private practitioners and 13 at an NGO facility. When asked about their current state of health, all 36 indicated that they had fully recovered from their VL episode.
Costs
Out of 139 patients interviewed, 136 were able to provide information about expenditures made while visiting different healthcare providers. Median total expenditure was 4000 Rupees (IQR 2695-5563 Rupees) per patient, equivalent to 86 US Dollar. Most money was spent on drugs (median 1500 Rupees, IQR 1000-2200 Rupees). When breaking down expenditure by type of provider, equal amounts were spent on private practitioners and in the PHC system, with median expenditures of 1455 Rupees (IQR 545-2715) and 1480 Rupees (IQR 1025-2045 Rupees) respectively. Village health workers were usually not paid, the median expenditure to unqualified practitioners was 500 Rupees (IQR 300-1000 Rupees). All 139 patients interviewed had experienced financial difficulties as a result of their illness, 47 (34%, 95% CI 26-42%) had experienced minor financial problems whereas 92 (66%, 95% CI 58-74%) had experienced major financial problems. Details on costs incurred are provided in table 3.
Table 3.
Reported median direct expenditures in Indian Rupees, overall and by type of practitioner:
| Overall median (IQR) |
Health workers median (IQR) |
Unqualified practitioner (IQR) |
PHC median (IQR) |
Private doctor (IQR) |
NGO (IQR) |
|
|---|---|---|---|---|---|---|
| Consultation fees | 120 (50-200) |
0 (0-0) |
0 (0-0) |
0 (0-0) |
150 (100-200) |
0 (0-20) |
| Diagnostic tests | 425 (259-650) |
0 (0-0) |
0 (0-0) |
0 (0-50) |
500 (300-700) |
0 (0-0) |
| Drugs | 1500 (1000-2200) |
0 (0-0) |
600 (400-1000) |
0 (0-200) |
1000 (500-1700) |
150 (0-200) |
| Other treatment services | 200 (0-450) |
0 (0-0) |
0 (0-0) |
180 (0-400) |
0 (0-0) |
0 (0-0) |
| Admission costs (fees and feeding) | 0 (0-0) |
0 (0-0) |
0 (0-0) |
0 (0-0) |
0 (0-0) |
600 (0-1000) |
| Travel costs | 600 (335-900) |
0 (0-0) |
0 (0-0) |
300 (200-500) |
300 (150-400) |
300 (300-400) |
| Other* | 800 (500-1500) |
0 (0-0) |
0 (0-0) |
700 (400-1000) |
0 (0-0) |
300 (0-500) |
| Total | 4000 (2695-5563) |
0 (0-0) |
500 (300-1000) |
1480 (1065-2045) |
1455 (545-2715) |
0 (0-0) |
Mostly costs of additional feeding prescribed by treating physicians
Discussion
Our study subjects were all VL cases treated within the PHC system, yet 81% had first presented to an unqualified practitioner. VL case management in rural Bihar is entrusted to the community health centre, yet patients reported to this facility with a delay of one to two months after onset of symptoms. Those who first presented to a village health worker (ANM or ASHA) still had median delays of a further 36 days before reporting to the community health center. Despite guidelines to use miltefosine as first line treatment and amphotericin B as second line, 70% of new patients were prescribed either SSG or amphotericin B in first intention. Though not apparent from the official reports, 27.5% of all patients treated in the PHC system (95% CI 19.7-35.2%) required a second VL treatment; 15% (95% CI 3-27%) of those treated on miltefosine and 40% (95% CI 28-52%) of those treated on SSG. VL diagnosis and treatment are in principle free but patients still spent a median of 4000 rupees per disease episode on various fees for medical services and transport costs at all levels of the system.
The long and winding road a VL patient has to travel before the disease is adequately taken care of could be due to village health workers not being sufficiently aware of the disease, the referral system within the PHC system being dysfunctional, and/or access to care not being sufficiently close to the patient. These problems can all be addressed by making better use of the existing network of village health workers. The dipstick test used for diagnosis (rK39) is easy to perform and can be stored at ambient temperatures (Lockwood & Sundar, 2006); making this test available at the level of ANM and ASHA can reduce diagnostic delays. Since the first line treatment is an oral drug, treatment for uncomplicated cases could be initiated at ANM level. As is done for tuberculosis, ASHAs could be involved in monitoring treatment intake. At the same time they could actively search for cases in the hamlet of the patient, since VL is known to have a very focal distribution (Boelaert et al. 2000; Elnaiem et al. 2003).
The high proportion treated on SSG (48%) confirms the findings from our site visit. The treatment results observed with SSG are very much in agreement with those reported by Sundar et al. (2001) but, contrastingly, our patients were recruited directly from the PHC system. With 40 percent of all those treated on SSG requiring a second treatment course for VL, patients are put at risk, transmission is prolonged and the reputation of the PHC system is being damaged. Erratic supply of miltefosine appears to be a key factor precluding its consistent use. Since the drug has a shelf life of more than 2 years under tropical conditions (Nwaka & Hudson, 2006), the problem can be solved by maintaining a 1 year buffer stock at district level and a 6 months buffer stock at block level; the former being replenished twice yearly, the latter quarterly.
Although with the exception of 2 patients who died, all patients were eventually cured, drug resistance and/or lack of compliance do seem to be serious problems. In this, VL control could learn from the experience of the tuberculosis control system that has developed a strong tradition in monitoring treatment outcomes. The tuberculosis system, which is also in place in Bihar State, requires program managers to account for the treatment outcome of each and every patient started on treatment in their district. Contrary to tuberculosis, VL does require a follow up till 6 months after initial cure but with the network of village health workers available this could easily be realized. An important first step would be the introduction of appropriate recording and reporting formats that do not just report just the caseload but also the treatment results.
Our findings on costs were comparable to those of Meheus et al. in 2006, who estimated the median direct cost of an episode of VL in Muzaffarpur, Bihar, at 3920 rupees. The same authors estimated the median monetary household income among VL patients in Muzaffarpur at 2200 rupees. Obviously the 4000 rupees observed in our study is a large amount when compared to monthly household income and this may be an important contributor to the patient delay observed.
Our study has several limitations. First and foremost, it is restricted to those patients registered by the public sector health services, and does not give the full picture of VL case management in Bihar, as many patients are taken care of by the private sector or remain undetected. Secondly, the patients interviewed were all started on treatment in 2008; improvement has been reported since then. Furthermore we did not follow-up patients in a prospective manner, which would have allowed for proper documentation of the reasons for not responding to treatment. The same is true for the estimated direct costs, as a certain recall bias cannot be ruled out. However, the retrospective design was more efficient and allowed us to arrive at conclusions more rapidly, in order to provide relevant and timely information to the health authorities and the elimination initiative.
Conclusion
To achieve the objective of ensuring early diagnosis and complete case management, the rural PHC system in India should involve its networks of village health workers in case finding, monitoring of treatment and follow-up after completion of treatment. The erratic supply of miltefosine in the public sector needs to be addressed urgently as SSG can no longer be relied upon for VL treatment. Even among those treated on miltefosine, there were patients who required a second treatment; the recording and reporting system currently used is unable to generate such vital information on treatment results. The VL control program needs to adopt a system of cohort reporting, similar to that practiced by the tuberculosis control program. Every patient started on treatment for VL needs to be assessed six months after completion of treatment; the outcomes need to be reported in a systematic way.
Acknowledgments
This work was supported by NIAID, NIH TMRC Grant No. 1P50AI074321 and the European Commission, grant HEALTH-F3-2008-222895 KALADRUG
References
- Barnett PG, Singh SP, Bern C, Hightower AW, Sundar S. Virgin soil: the spread of visceral leishmaniasis into Uttar Pradesh, India. Am J Trop Med Hyg. 2005;73:720–725. [PubMed] [Google Scholar]
- Bern C, Hightower AW, Chowdhury R, et al. Risk factors for kala-azar in Bangladesh. Emerg Infect Dis. 2005;11:655–662. doi: 10.3201/eid1105.040718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boelaert M, Criel B, Leeuwenburg J, et al. Visceral leishmaniasis control: a public health perspective. Trans R Soc Trop Med Hyg. 2000;94:465–471. doi: 10.1016/s0035-9203(00)90055-5. [DOI] [PubMed] [Google Scholar]
- Boelaert M, Meheus F, Sanchez A, et al. The poorest of the poor: a poverty appraisal of households affected by visceral leishmaniasis in Bihar, India. Trop Med Int Health. 2009;14:639–644. doi: 10.1111/j.1365-3156.2009.02279.x. [DOI] [PubMed] [Google Scholar]
- Elnaiem DE, Schorscher J, Bendall A, et al. Risk mapping of visceral leishmaniasis: the role of local variation in rainfall and altitude on the presence and incidence of kala-azar in eastern Sudan. Am J Trop Med Hyg. 2003;68:10–17. [PubMed] [Google Scholar]
- Joshi A, Narain JP, Prasittisuk C, et al. Can visceral leishmaniasis be eliminated from Asia? J Vector Borne Dis. 2008;45:105–111. [PubMed] [Google Scholar]
- Kumar R, Jaiswal V, Tripathi S, Kumar A, Idris MZ. Inequity in health care delivery in India: the problem of rural medical practitioners. Health Care Anal. 2007;15:223–233. doi: 10.1007/s10728-007-0060-x. [DOI] [PubMed] [Google Scholar]
- Lockwood DN, Sundar S. Serological tests for visceral leishmaniasis. BMJ. 2006;333:711–712. doi: 10.1136/bmj.38989.567083.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meheus F, Boelaert M, Baltussen R, Sundar S. Costs of patient management of visceral leishmaniasis in Muzaffarpur, Bihar, India. Trop Med Int Health. 2006;11:1715–1724. doi: 10.1111/j.1365-3156.2006.01732.x. [DOI] [PubMed] [Google Scholar]
- Nwaka S, Hudson A. Innovative lead discovery strategies for tropical diseases. Nat Rev Drug Discov. 2006;5:941–955. doi: 10.1038/nrd2144. [DOI] [PubMed] [Google Scholar]
- Sbarbaro J. Toman's Tuberculosis, Case detection, treatment, and monitoring –questions and answers. Geneva: WHO; 2004. How frequently do patients stop taking treatment prematurely? pp. 181–182. [Google Scholar]
- Singh SP, Reddy DC, Rai M, Sundar S. Serious underreporting of visceral leishmaniasis through passive case reporting in Bihar, India. Trop Med Int Health. 2006;11:899–905. doi: 10.1111/j.1365-3156.2006.01647.x. [DOI] [PubMed] [Google Scholar]
- Singh VP, Ranjan A, Topno RK, et al. Estimation of under-reporting of visceral leishmaniasis cases in Bihar, India. Am J Trop Med Hyg. 2010;82:9–11. doi: 10.4269/ajtmh.2010.09-0235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sundar S, Pai K, Kumar R, et al. Resistance to treatment in Kala-azar: speciation of isolates from northeast India. Am J Trop Med Hyg. 2001;65:193–196. doi: 10.4269/ajtmh.2001.65.193. [DOI] [PubMed] [Google Scholar]
- World Health Organization. WHO/CDS/TB/2003.1313. Geneva, Switzerland: WHO; 2003. Treatment of tuberculosis: guidelines for national programmes. [Google Scholar]
- World Health Organization, Regional office for South-East Asia. Regional Strategic Framework for Elimination of Kala-azar from the South-East Asia Region (2005-2015) [March 2010];2005a Available from: http://www.searo.who.int/LinkFiles/Kala_azar_VBC-85_Rev_1.pdf.
- World Health Organization, Country office for India. Primary healthcare resources in India. [March 2010]; Available from: http://www.whoindia.org/LinkFiles/Health_Systems_Development_Primary_Health_Care_Primary_health_care_resources_.pdf.
- World Health Organization, Country office for India. Origin and evolution of primary health care in India. [March 2010]; Available from: http://www.whoindia.org/LinkFiles/Health_Systems_Development_Primary_Health_Care_Origin_and_Evolution_.pdf.