Abstract
Background
Prior studies of resident experience in gynecology looked only at the year before and after adoption of ACGME duty hour standards. This study sought to determine whether procedure volume differed after completion of a 4-year residency training program, before and after work hour reform.
Method
Inpatient and outpatient procedures performed by MetroHealth Medical Center/Cleveland Clinic program residents from 1998 to 2006 were obtained from Annual Reports of Institutional and Resident Experience. Four-year experience before and after duty hour restrictions were compared: hours worked were collected from resident schedules, ambulatory hours and procedures were compared directly, surgical procedures and deliveries were compared using a 2-tailed t test. Data were also obtained for institutional volume changes, and a corrected value, based on the rates of resident cases per available cases, was analyzed.
Results
Ambulatory hours worked per resident decreased after implementing work hour reform from 674 to 366 hours. The types of ambulatory and surgical procedures performed varied over time. Overall, basic surgical and obstetrical volume per resident did not change before and after work hour reform (mean before reform, 723 ± 117, mean after reform, 781 ± 200, P = .58 for gynecologic procedures; mean before reform, 611 ± 107, mean after reform, 535 ± 73, P = .18 for basic obstetrics and vaginal and cesarean deliveries). Institutional volume did not change significantly, although the percentage of the institutions' cases performed by residents did decrease for some procedures.
Conclusion
The ACGME duty hour restrictions do not limit the overall ambulatory or surgical procedural volume in an obstetrics and gynecology residency-training period.
Introduction
During the past 20 years, resident training has come under scrutiny, particularly by regulatory bodies. In efforts to improve resident education, enhance resident well-being, and improve the quality of patient care, the Accreditation Council for Graduate Medical Education (ACGME) implemented resident duty hour restrictions.1 According to these guidelines, residents must work less than 80 hours per week, averaged over 4-week periods. Additional guidelines require certain amounts of time off per week, and residency programs in all specialties were required to adhere to these guidelines by July 2003.
There are many concerns regarding the effects of these limitations on the education and training of residents and how this translates to the quality of patient care, the continuity of care, and the preparedness of residents for future practice.2–5 Of particular interest is the number of operative procedures performed by residents in surgical subspecialties.5–8 Prior studies have evaluated surgical and procedural volume in obstetrics and gynecology and in general surgery, both before and after the work hour restrictions.5,6,9 These studies however, were not longitudinal and did not evaluate experience over a complete residency training period. In addition, there is concern that ambulatory experience may be compromised in efforts to provide adequate resident experience in other areas.
Our objective was to compare surgical and ambulatory procedure volume on completion of residency training in obstetrics and gynecology among residents at an academic institution, before and after implementation of ACGME residency work hour restrictions.
Materials and Methods
We performed a retrospective cohort study to examine resident procedural volume and time spent in the ambulatory setting. We selected 2 cohorts of residents from the Case Western Reserve University–MetroHealth Medical Center/Cleveland Clinic (MHMC/CC) residency program in obstetrics and gynecology. Our cohorts consisted of the residency graduating class of 2002 and the graduating class of 2006. This study was reviewed by Institutional Review Boards at MetroHealth Medical Center and Cleveland Clinic and received exempt status.
The MHMC/CC residency program is an integrated obstetrics and gynecology training program with residents rotating at 2 tertiary-care institutions. Before 2002, the MHMC/CC program consisted of 5 residents per class. Residents spent most of their time at MHMC with a 110-week rotation at CC during their second, third, and fourth years of residency. In July 2002, the MHMC/CC residency program expanded to 7 residents per class to further integrate the 2 institutions. After July 2002, residents from all 4 postgraduate years (PGYs) were at MHMC for 4 rotations of 7 weeks and were at CC for 3 rotations of 7 weeks. Original MHMC and CC rotations were maintained, and additional rotations were added in gynecologic subspecialties, general obstetrics, and ambulatory clinics. The MHMC/CC residency program adopted the ACGME duty hour regulations in July 2002. Therefore, our first cohort consisted of 5 residents who underwent training from July 1998 to June 2002, before duty hour regulations. The second cohort consisted of 7 residents who trained from July 2002 to June 2006, after duty hour regulations were adopted.
Resident schedules from all 8 years were reviewed for hours of assigned ambulatory time. Residents were assumed to average 4 hours of ambulatory time for half-day clinics and 8 hours of ambulatory time for full-day clinics. Average ambulatory time per week was calculated for each rotation and multiplied by the total number of weeks spent on the given rotation. For the graduating class of 2006, a traditional 1∶4 in-house, overnight call schedule was used for PGY-1 rotations and PGY-2 to PGY-3 rotations at CC. Based on duty hour regulations, residents went home after 24 hours during on-call shifts, and these hours were deducted from the ambulatory hours for the corresponding rotations. Assigned ambulatory time was calculated for each 4-year resident class and was compared directly.
Ambulatory procedure data were based on ambulatory procedures performed in the resident clinic based at MetroHealth Medical Center. These included resident gynecology clinic, colposcopy clinic, and continuity clinic patients. Ambulatory procedure data were obtained per resident, based on current procedural terminology codes.
Obstetric and gynecologic procedures for the 12 residents in question were estimated using deidentified data obtained from annual reports of institutional and resident experience. These reports are submitted to the ACGME Residency Review Committee and consist of summaries of operative procedural volume based on individual resident case logs. Before 2003, residents completed a paper procedural log using a standard template on a weekly basis. These weekly logs were compiled by the residency program and submitted to the Residency Review Committee on an annual basis. After 2003, residents entered data regarding operative procedures directly on the ACGME website (https://www.acgme.org/residentdatacollection/).1 On this website, procedures were entered using current procedural terminology codes. For both paper logs and web-based entry, residents designated their role (primary surgeon versus assistant) and the location where the procedure was performed (MHMC or CC). We extracted procedure codes for total abdominal hysterectomy (TAH), total vaginal hysterectomy (TVH), surgery for stress urinary incontinence or pelvic organ prolapse, laparotomy, laparoscopy, sterilization, ectopic case, hysteroscopy, oncology case, and reproductive endocrinology case. Experience in these procedures was compared between the 2 cohorts. Because the collected data was deidentified, comparisons of specific rotations and breakdown of procedures specific to each rotation could not be obtained. Finally, MHMC and CC annual statistics were reviewed to assess total institutional procedure volume for each procedure from 1998 to 2006.
Institutional volume was totaled per procedure for each time period (1998–2002 and 2002–2006). To control for changes in institutional volume, we calculated a per-resident procedure rate for each category of operative procedure. To calculate the procedure rate, yearly volumes of cases per institution were obtained and combined. Yearly numbers of cases logged by residents were also obtained, and percentages were calculated from the cumulative annual volumes from both institutions and cumulative number of cases logged by each cohort. We divided the number of procedures each resident performed during 4 years by the total number of “available procedures” (ie, procedures from both institutions) from the same time period. A per-resident mean was then calculated. Continuous variables were analyzed using the 2-tailed Student t test, with P < .05 considered statistically significant. Mean percentages and differences in procedure rates (using a P value of <.05 as significant) were calculated. Analyses were performed using StatView from SAS Institute Inc. (Cary, NC).
Results
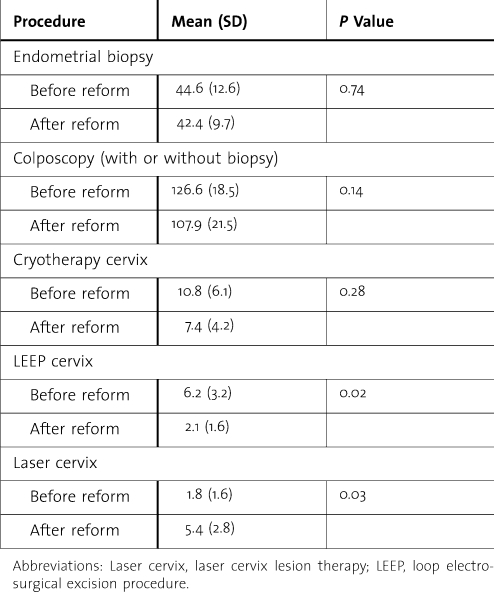
table 1 refers to number of ambulatory procedures performed by the 2 cohorts. The overall number of ambulatory hours (3372 versus 2560) and number of hours assigned per resident (674 versus 366) were greater before work hours restrictions. There were no significant differences between the 2 cohorts with respect to endometrial biopsy, colposcopy, or cryotherapy of the cervix. Residents performed more cervical loop electrosurgical excision procedures in the years before duty hour restrictions (6.2 before versus 2.1 after, P = .02), whereas after duty hour restrictions, residents performed more cervical laser procedures (1.8 before versus 5.4 after, P = .03).
Table 1.
Ambulatory Clinic Procedure Volume Before and After Duty Hour Restrictions
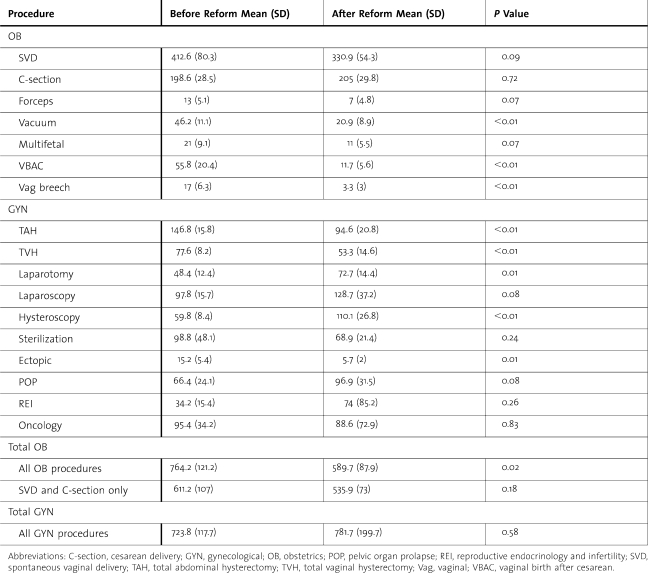
table 2 represents actual resident procedural volume per resident, as presented to the ACGME for accreditation purposes. Total obstetrics and gynecology volume per resident is adjusted for the number of residents in each cohort. Vaginal breech deliveries decreased significantly, (17 versus 3 per resident, P = .005) as did vacuum-assisted deliveries (46 versus 21, P = .003) and vaginal birth after cesarean (56 versus 12, P = .007). Further analysis of obstetrical procedures was performed to specifically examine basic obstetric procedures of spontaneous vaginal delivery and cesarean delivery (both primary and repeat) between the 2 cohorts. By eliminating operative, breech, and multifetal vaginal delivery from the analysis, there was no significant difference in mean obstetric procedures between the 2 cohorts (611 versus 536, P = .18).
Table 2.
Obstetric and Gynecologic Procedure Volumes per Resident Before and After Duty Hour Restrictions
Before duty hour restrictions, residents reported performing more TAHs, TVHs, and treatment of ectopic pregnancies. In contrast, after duty hour restrictions, residents reported performing more laparotomies and more hysteroscopies. Reported numbers of laparoscopies, surgical sterilizations, and procedures for pelvic organ prolapse, reproductive endocrinology and infertility, or oncology were not significantly different between the 2 cohorts. Overall, there were no significant differences between the 2 cohorts with respect to total gynecologic surgery volume.
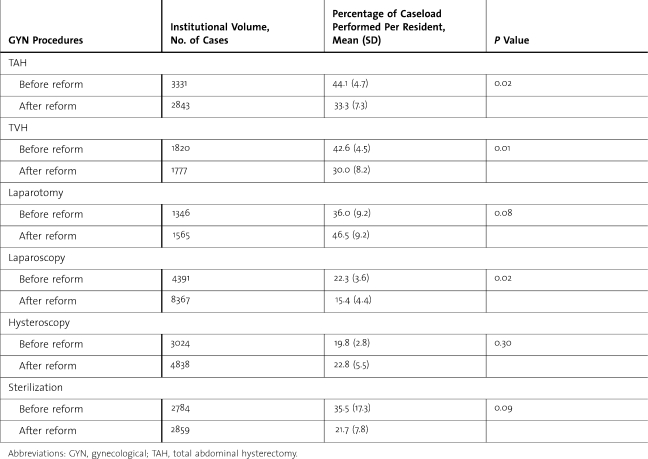
Institutional volumes of gynecologic procedures from both institutions were combined over our study period. There were no significant differences when comparing institutional volumes between 1998–2002 and 2002–2006. However, there were significant differences in the rates of resident participation in the institutional case volume. When corrected for institutional volume, the percentage of abdominal hysterectomies, vaginal hysterectomies, and laparoscopic cases performed by residents decreased (table 3).
Table 3.
Institutional Volumes and Proportion of Resident-Performed Cases Before and After Duty Hour Restrictions
Discussion
After duty hour limitations were instituted, residents reported fewer overall obstetric procedures, with no significant differences in spontaneous vaginal deliveries or cesarean deliveries. Total gynecologic procedural volume was similar: Before duty hour restrictions residents reported more TAHs, TVHs, and surgeries for ectopic pregnancy, whereas after duty hour restrictions, residents reported more laparotomies and hysteroscopies. When adjusting gynecologic procedures for institutional volume after duty hour restrictions went into effect, residents performed a smaller percentage of the TAHs, TVHs, and laparoscopies, although resident involvement in laparotomies, hysteroscopies, and surgical sterilizations remained unchanged. Ambulatory procedural volume was maintained after duty hour restrictions, but total assigned ambulatory time decreased.
We evaluated resident experience over entire 4-year training periods to better understand how duty hour limitations may have affected obstetrics and gynecology resident education. This is the first longitudinal study, to our knowledge, looking at cases performed over a complete residency program, and it is also the first study to evaluate the ambulatory component of residency training. The decrease in ambulatory hours did not affect the numbers of procedures performed, but the decrease in longitudinal patient contact may have lasting effects on the performance of physicians in practice and also on the perception of the physician's education upon completion of the residency.
Although ambulatory procedural volume was obtained from billing records, surgical data were obtained from resident case logs, which are subject to recall and recording biases. In our training program, residents were required to update either their paper-based or computerized logs on a weekly or semimonthly basis, which may minimize some of this bias. In addition, the standard deviations of our calculated mean values are similar in both cohorts. This suggests that if reporting errors occurred, they were equally distributed across both 4-year intervals. If, for example, there were large standard deviations in 1 cohort and very small standard deviations in the other cohort, we would be more likely to suspect a systematic bias related to reporting. Finally, because these are the same numbers that are reported to the Residency Review Committee for maintenance of accreditation, we believe that these data are the best proxy for true resident procedural volume, which is otherwise difficult to ascertain.
Our study has several limitations. A major limitation is that this was a single-site study, with limited numbers of residents and possibly limited reproducibility at other institutions and limited generalizability. A benefit of single-site studies is the ability to have consistency across the samples. In our study, this benefit was lost because of multiple changes that took place at our institution and within our training program. Concurrent with the implementation of the ACGME duty hour limits, there was an increase in the number of residents per class. To adjust for this, we analyzed data using mean values for each cohort to determine significance. With the expansion of the residency program, resident rotations were further distributed across 2 institutions. In addition, surgical trends may have changed during the 8-year study period. We attempted to account for these factors by calculating proportions of resident involvement using combined institutional volume and by comparing the mean percentages of cases performed by each resident in each cohort. However, it is unclear whether the adjusted rates truly reflect changes related to work hour reform.
Finally, before 2003, residents submitted weekly case logs via standardized paper-based reporting templates. After 2003, residents used the ACGME web-based reporting system, which requires logging of procedures using current procedural terminology codes. This may explain some of the variation in the types of procedures between the 2 cohorts. After the duty hour limits went into effect, residents reported fewer surgical procedures for treatment of ectopic pregnancy. This could indeed be due to residents logging these procedures using current procedural terminology codes for laparoscopy instead of surgery for ectopic pregnancy. The data collected are the most accurate available in a retrospective review, and they are the material submitted to the Residency Review Committee for maintenance of accreditation.
A prior study at our institution, comparing PGY4 classes in the year before and after the implementation of ACGME restrictions, suggested a decline in procedural volume due to limited duty hours.6 Since that time, other surgical subspecialties have reported no change in total surgical volume after work hour limitations were instituted.7,10–13 In some cases, although total volume had been maintained, there was a shift in the types of cases in which residents participated.14 Our results are consistent with these data. Other studies have suggested that the use of physician extenders may improve resident education.15 In our study, the percentage of institutional caseload performed by residents trended downward for all procedures, with significant decreases noted, especially for TAHs and TVHs. Although the number of laparoscopies increased, the resident caseload percentage did not reflect that increase. One possible explanation is that cases previously logged as treatment of ectopic pregnancy could have been coded under laparoscopy or laparotomy, and prior TVH cases could have been listed under prolapse procedures. It is also unclear whether these changes are due to the use of physician extenders or to the shifting of the caseload toward fellows or other attending physicians. It is likely that ambulatory procedures were able to remain constant because of increased nurse-practitioner numbers and their ability to see low-risk obstetric patients, thus allowing residents to see gynecology-procedure appointments more often. We did not look at the volume of surgical cases that included no qualified resident modifiers or the volume of procedures performed solely by attending physicians.
National trends have shown a decline in procedures such as operative vaginal delivery and breech vaginal delivery.16 Vaginal birth after cesarean deliveries have also declined since the 1990s.17,18 Our data reflect these national trends. Therefore, we feel our secondary analysis of basic obstetric procedures limited to spontaneous vaginal delivery and cesarean delivery is more indicative of the educational implications that decreased work hours may have had on the specialty.
Prior studies at our institution suggested no differences in exam scores or job satisfaction but have suggested an improved quality of life since duty hour restrictions.3 This is corroborated by recent evidence from other specialties showing improvements in exam scores and job satisfaction.10,12 However, our data suggest that the preservation in procedural volume may come at the expense of time spent in the ambulatory clinic and in decreasing numbers of “major” cases. This may have a significant effect on obstetric-gynecology physicians because those entering practice spend a significant portion of their time in the ambulatory setting and do limited major surgeries. Future research is warranted to see how duty hour limitations may affect educational satisfaction and the quality of physicians within the first few years of practice.
Conclusions
We found that ACGME duty hour restrictions do not limit the overall ambulatory or surgical procedural volume in an obstetrics and gynecology residency training period.
Footnotes
Sarah M. Kane, MD, is a Urogynecology Fellow, Female Pelvic Medicine and Reconstructive Surgery, Case Western Reserve University School of Medicine, MetroHealth Campus; Nazema Y. Siddiqui, MD, is Assistant Professor of Female Pelvic Medicine and Reconstructive Surgery at Duke University Medical Center; Jennifer Bailit, MD, MPH, is Associate Professor of Maternal-Fetal Medicine and Infant Health, Case Western Reserve University School of Medicine, MetroHealth Campus; and May Hsieh Blanchard, MD, is Assistant Professor, Department of Obstetrics, Gynecology, and Reproductive Sciences, University of Maryland.
References
- 1.Accreditation Council for Graduate Medical Education. ACGME duty hours standards now in effect for all residency programs. Available at: http://www.acgme.org. Accessed July 1, 2007.
- 2.Bailit J. L., Blanchard M. H. The effect of house staff working hours on the quality of obstetric and gynecologic care. Obstet Gynecol. 2004;103((4)):613–616. doi: 10.1097/01.AOG.0000119225.57285.c1. [DOI] [PubMed] [Google Scholar]
- 3.Bailit J. L., Weisberger A., Knotek J. Resident job satisfaction and quality of life before and after work hour reform. J Reprod Med. 2005;50((9)):649–652. [PubMed] [Google Scholar]
- 4.Barden C. B., Specht M. C., McCarter M. D., Daly J. M., Fahey T. J. Effects of limited work hours on surgical training. J Am Coll Surg. 2002;195((4)):531. doi: 10.1016/s1072-7515(02)01242-5. [DOI] [PubMed] [Google Scholar]
- 5.Chandra R. K. M. The resident 80-hour work week: how has it affected surgical specialties? Laryngoscope. 2004;114((8)):1394. doi: 10.1097/00005537-200408000-00014. [DOI] [PubMed] [Google Scholar]
- 6.Blanchard M. H., Amini S. B., Frank T. M. Impact of work hour restrictions on resident case experience in an obstetrics and gynecology residency program. Am J Obstet Gynecol. 2004;191((5)):1746. doi: 10.1016/j.ajog.2004.07.060. [DOI] [PubMed] [Google Scholar]
- 7.Baskies M. A., Ruchelsman D. E., Capeci C. M., Zuckerman J. D., Egol K. A. Operative experience in an orthopaedic surgery residency program: the effect of work-hour restrictions. J Bone Joint Surg Am. 2008;90((4)):924–927. doi: 10.2106/JBJS.G.00918. [DOI] [PubMed] [Google Scholar]
- 8.Hassett J. M., Nawotniak R., Cummiskey D., Berger R., Posner A., Seibel R. Maintaining outcomes in a surgical residency while complying with resident working hour regulations. Surgery. 2002;132((4)):635–639. doi: 10.1067/msy.2002.127542. [DOI] [PubMed] [Google Scholar]
- 9.Ferguson C. M., Kellogg K. C., Hutter M. M., Warshaw A. L. Effect of work-hour reforms on operative case volume of surgical residents. Curr Surg. 2005;62((5)):535. doi: 10.1016/j.cursur.2005.04.001. [DOI] [PubMed] [Google Scholar]
- 10.Durkin E. T., McDonald R., Munoz A., Mahvi D. The impact of work hour restrictions on surgical resident education. J Surg Educ. 2008;65((1)):54–60. doi: 10.1016/j.jsurg.2007.08.008. [DOI] [PubMed] [Google Scholar]
- 11.Shin S., Britt R., Britt L. D. Effect of the 80-hour work week on resident case coverage: corrected article. J Am Coll Surg. 2008;207((1)):148–150. doi: 10.1016/j.jamcollsurg.2008.05.004. [DOI] [PubMed] [Google Scholar]
- 12.Shonka D. C., Jr, Ghanem T. A., Hubbard M. A., Barker D. A., Kesser B. W. Four years of accreditation council of graduate medical education duty hour regulations: have they made a difference? Laryngoscope. 2009;119((4)):635–639. doi: 10.1002/lary.20144. [DOI] [PubMed] [Google Scholar]
- 13.Connors R. C., Doty J. R., Bull D. A., May H. T., Fullerton D. A., Robbins R. C. Effect of work-hour restriction on operative experience in cardiothoracic surgical residency training. J Thorac Cardiovasc Surg. 2009;137((3)):710–713. doi: 10.1016/j.jtcvs.2008.11.038. [DOI] [PubMed] [Google Scholar]
- 14.Sarff M., Ellis M. C., Vetto J. T. Case log review produces translational change in surgical oncology education. J Cancer Educ. 2009;24((3)):176–179. doi: 10.1080/08858190902876213. [DOI] [PubMed] [Google Scholar]
- 15.Stahlfeld K. R., Robinson J. M., Burton E. C. What do physician extenders in a general surgery residency really do? J Surg Educ. 2008;65((5)):354–358. doi: 10.1016/j.jsurg.2008.06.002. [DOI] [PubMed] [Google Scholar]
- 16.Kozak L. J., Weeks J. D. U.S. trends in obstetric procedures, 1990–2000. Birth. 2002;29((3)):157–161. doi: 10.1046/j.1523-536x.2002.00182.x. [DOI] [PubMed] [Google Scholar]
- 17.Yang Y. T., Mello M. M., Subramanian S. V., Studdert D. M. Relationship between malpractice litigation pressure and rates of cesarean section and vaginal birth after cesarean section. Med Care. 2009;47((2)):234–242. doi: 10.1097/MLR.0b013e31818475de. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zweifler J., Garza A., Hughes S., Stanich M. A., Hierholzer A., Lau M. Vaginal birth after cesarean in California: before and after a change in guidelines. Ann Fam Med. 2006;4((3)):228–234. doi: 10.1370/afm.544. [DOI] [PMC free article] [PubMed] [Google Scholar]