Abstract
Background
Current training practices and teaching methods for critical care medicine education during internal medicine residency have not been well described. This study explored critical care medicine education practices and environments for internal medicine residents in the United States.
Methods
A web-based survey recruited Pulmonary and Critical Care Medicine fellowship program directors involved with internal medicine residency programs at academic institutions in the United States.
Results
Of 127 accredited Pulmonary and Critical Care Medicine programs in 2007, 63 (50%) responded. Demographics of the intensive care units varied widely in size (7–52 beds), monthly admissions (25–300 patients), and presence of a “night float” (22%) or an admissions “cap” (34%). All programs used bedside teaching, and the majority used informal sessions (91%) or didactic lectures (75%). More time was spent on resident teaching in larger (≥20 bed) medical intensive care units, on weekdays, in programs with a night-float system, and in programs that suspended residents' primary care clinic duties during their intensive care unit rotation.
Conclusions
Although similar teaching methods were used within a wide range of training environments, there is no standardized approach to critical care medicine education for internal medicine residents. Some survey responses indicated a correlation with additional teaching time.
Editor's Note: The online version (59.5KB, doc) of this article contains the survey instrument used in this study.
Background
The intensive care unit (ICU) is a complex and rapidly evolving environment with many challenges for its health care providers. Although ample evidence indicates that care offered by subspecialists trained in critical care medicine (CCM) improves patient outcomes at a lesser cost,1,2 most ICUs in the United States are staffed by non-CCM–board certified physicians. This situation is likely to persist or increase due to the projected shortage in the number of intensivists over the next 2 decades.3 Because many of these non–critical care trained providers are internists, CCM training is increasingly becoming a priority for many internal medicine residency programs.
Despite this growing need, the education of residents in CCM is challenging. The severity and unpredictability of patients' illnesses, constantly evolving and growing nature of this specialty, residents' duty hour restrictions, and focus on patient safety and quality of care are some factors that may compromise resident education in this environment. These stresses on the current graduate medical education curriculum may generate conflict between providing optimal patient care and resident education. Therefore, an efficient, effective, and standardized system of medical education must be designed and implemented that achieves the dual goals of providing high-quality patient care and excellent resident education. Although guidelines for CCM training have been published to promote excellence in CCM education,4 an “ideal” education curriculum or standardized approach has not been established.5,6
The first step in developing such an ideal curriculum for educating internal medicine residents in CCM is to describe the current teaching practices, resources, and environments. Many studies have reported suboptimal training of residents in some CCM practices and topics, such as mechanical ventilation and cardiopulmonary resuscitation,7–11 and variation in the amount of time devoted to education in acute illness.12,13 In addition, 1 study reported that methods for teaching residents in the ICU have changed little since the Accreditation Council for Graduate Medical Education (ACGME) instituted duty hour standards and the general competencies.14 These deficiencies and apparent lack of progress in CCM medical education may not only affect patient care but may discourage residents from pursuing a career in this field.15
There does not appear to be a general framework for CCM teaching practices and learning environments in internal medicine residency programs. It is also not clear which methods or practices are optimal for resident education in CCM. Prior surveys have evaluated CCM education practices at the undergraduate level or in international settings and have focused on specific topics or techniques.5,6 The objective of our study is to identify current practices and training environments of CCM education for internal medicine residents.
Methods
Study Design and Participants
This study entailed a cross-sectional survey of program directors at all academic Pulmonary and Critical Care Medicine programs (PCCM) in the United States. All PCCM fellowship program directors listed in the Pulmonary Disease and Critical Care section of the 2006–2007 Graduate Medical Education Directory were selected to participate (N = 127). Although residency directors are familiar with residents' education and activities, PCCM fellowship program directors were the target audience for data collection in this study because they are familiar with ICU residents' team composition, call schedule, teaching sessions and activities, education resources in the ICU, and interactions with the ICU staff. Program directors were faxed a letter explaining the study objectives and inviting them to participate. Two weeks later, a second invitation was sent via e-mail that included instructions for completing the anonymous online survey. Reminder e-mails were sent every 2 to 3 weeks to nonresponders to maximize the response rate. The protocol was deemed exempt from review by the University of Cincinnati Institutional Review Board.
Survey
The survey questions focused on residents' activities during the ICU rotation, including their duties, workloads, educational resources, and rotation structure. Survey questions were developed based on validated educational surveys in the medical literature, educational requirements and core competencies by educational programs and examination boards, and recommendations by local educators. The first draft of the survey was pretested by local faculty at the University of Cincinnati for readability as well as face and content validity. Suggested changes were made and the final survey (supplemental online Appendix I) was uploaded into the commercially available online SurveyMonkey (Survey Monkey, Palo Alto, CA) program, www.surveymonkey.com. The electronic survey was pretested before study initiation.
Data Analysis
Survey responses were downloaded into a 2006 Excel spreadsheet data set (Microsoft Corporation, Seattle, WA). We used descriptive statistics to summarize categorical and/or binary variables using frequency (in percent) and numerical variables using means and standard deviations, respectively. Associations between categorical variables were assessed using chi square tests. All statistical analyses were performed using the SAS 9.2 software (SAS, Cary, NC) program. P values <.05 were considered statistically significant.
Results
ICU Teaching Environment
Of 127 listed accredited PCCM programs in the United States, 63 (50%) completed the online survey. Programs that responded and nonrespondents were similar in size (number of fellowship positions offered). Respondents included programs from all geographic regions (42% of programs in the West, 61% of those in the Midwest, 42% of those in the South, and 52% of those in the Northeast).
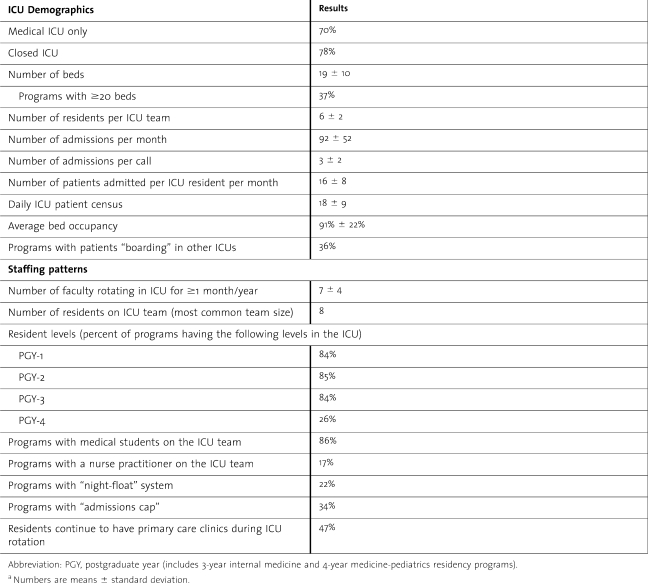
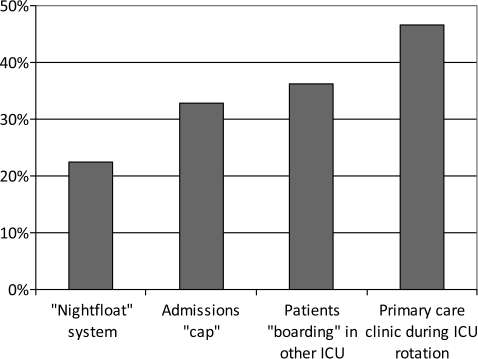
There was a wide distribution in ICU demographics and staffing patterns among programs (table 1). The mean ICU size was 19 beds (range 7–52), and 78% were “closed” medical ICUs (ICU team is the primary provider). Monthly admissions ranged from 25 to 300 patients. ICU teams were composed of 6 ± 2 residents from all postgraduate year levels. Some programs had a resident “night-float” system and/or a “cap” on resident admissions (mean 6 ± 2 patients per on-call period; figure 1). Although almost half (47%) of residents continued to have their outpatient primary care clinic during the ICU rotation, 36% of this group had it less often than during their non-ICU rotations.
Table 1.
Intensive Care Unit (ICU) Demographics and Staffing Patterns Among Academic Institutionsa
Figure 1.
Structure of Intensive Care Unit Rotations for Residents
A minority of programs had admissions “cap” and “night-float” systems that limit resident workload or duty hours. The night-float system and the absence of the outpatient clinic during the ICU rotation correlated significantly with more time for teaching. Abbreviations: CCM, critical care medicine; ICU, intensive care unit.
Educational Methods
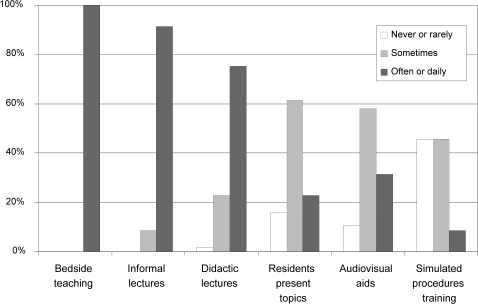
Resident education was provided using several formats (figure 2). Bedside teaching was the most common (used “often or daily”) and was offered by all programs. Informal sessions such as case or topic discussions away from the bedside (91%) and didactic lectures (75%) were also used “often or daily” and were more common in larger ICUs (≥20 beds; P < .01). The use of these modalities was also associated with a larger number of faculty rotating through the ICU each year (≥5 faculty; P < .05). The combined use of different modalities of teaching (bedside teaching, didactic lectures, and informal sessions) was less likely to occur in programs with patients “boarding” in other ICUs than in those where all patients were in one ICU (30% vs 60% of programs used all 3 modalities regularly, P < .05).
Figure 2.
Type of Teaching Methods Used in the Intensive Care Unit
Almost all programs routinely used bedside teaching and informal (group discussion) or didactic (standardized format) lectures, while a minority used other technologies.
Technological tools for education, such as audiovisual aids or simulated procedures training, were used “sometimes” by many programs (58% and 46%, respectively), but the number of programs using these tools was too small to conduct any statistical comparisons.
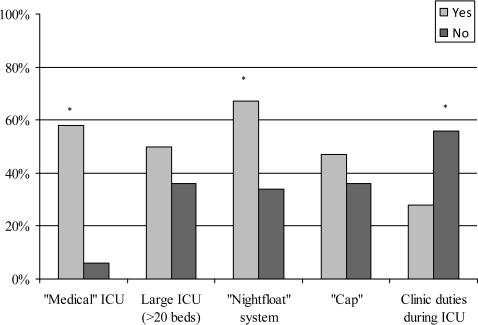
The presence of an admission cap or a night-float system was associated with a higher frequency of residents using self-teaching methods (40% in programs with cap vs 8% without; 42% of programs with night float vs 13% without, P < .01). The time spent on teaching ranged from 10% to 80% of ICU rounds, with less teaching time on the weekends (3.0 ± 1.2 hours per day on weekdays vs 1.9 ± 1.3 hours per day on weekends; P < .001). In addition, teaching time varied considerably among programs with different ICU and rotation characteristics: Medical ICUs, larger programs (>20 beds), and programs with a night-float system and cap offered more teaching time; ICUs in which residents continued their outpatient clinics during the CCM rotation offered less teaching time (figure 3).
Figure 3.
The Proportion of Programs Offering Teaching Time ≥4 Hours a Day Based on Different Intensive Care Unit (ICU) and Rotation Characteristics
Programs with large, medical ICUs and “night-float” systems were more likely to offer ≥4 hours a day of teaching time to residents. * P < .05.
Perceptions of Resident Education
Program directors were asked about their perceptions of resident education in the ICU. When asked about the effect of the ACGME duty hour limits on resident education, 58% stated it had a negative effect, 16% said it had a positive effect, and 26% said it did not have any effect or they did not know. Perceptions of a negative effect were more likely reported from programs that limited resident workloads, such as an admissions cap. In these programs, 80% of the program directors felt the duty hour limits had a negative effect, compared with 49% in programs without a cap (P < .05). Programs that spent more time teaching (≥4 hours per day) were also more likely to perceive a negative effect (77% vs 46% in programs spending <4 hours per day on teaching, P < .05). Most respondents (63%) reported that the duty hour limits “somewhat or very likely” changed their approach to teaching in the ICU. When asked to rank their perception of residents' satisfaction with their CCM education, 77% of respondents believed they would rank it as “excellent” and 23% said they would rank it as “good.” “Excellent” responses were more likely to come from programs with a medical ICU (88% vs 53%, P < .01), ≥5 faculty per year on service (84% vs 50%, P < .05), daily didactic lectures (100% vs 71%, P < .05), and daily bedside teaching (82% vs 43%, P < .05).
Our survey also revealed that almost all programs (91%) indicated that their residents were “extremely or very likely” to have received “formal training” in invasive procedures. Whether this training involves direct supervision by senior colleagues during actual procedures or the use of simulation technology is unclear and was not determined in our study. We suspect direct supervision is more likely because only a minority of programs reported using simulation-based training routinely.
Discussion
Our study produced several important findings regarding the current state of CCM education for internal medicine residents. First and foremost, there is no standardized approach to CCM education, potentially reflecting the highly variable ICU environment and practice patterns. Our survey demonstrated significant variability in ICU types (ie, medical, surgical, cardiac) and sizes, resident workloads, ICU team structure, and the presence of night-float systems, caps on admissions, and continuation of residents' primary care clinics during their ICU service. Such differences may affect the quality and perception of residents' CCM education through varied exposure to different patient cases, opportunities to perform procedures, experience with different attending practice styles, and total teaching time. Programs that limit residents' work duties by implementing night-float systems or suspending their primary care clinic during the ICU rotation reported dedicating roughly twice the proportion of time to teaching, confirming other reports that suggest excess workload may be a factor in limited teaching in some critical care settings.6 Although we did not evaluate the extent of residents learning from these rotations, correlating differences in their learning outcomes with various ICU and program characteristics would offer further insight into the effects of different teaching environments.
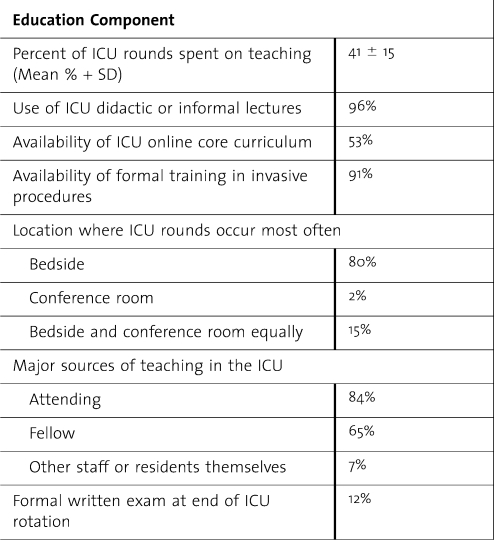
Despite this lack of a standardized structure, most programs used similar traditional clinical teaching methods (table 2). All programs indicated that bedside teaching was the most common format of resident education, and many also offered informal sessions and didactic lectures, including access to an online “core curriculum” of ICU topics. These findings confirm prior national and international surveys that reported 91% to 94% of programs used bedside teaching and 68% to 79% offered didactic lectures.6,14
Table 2.
Organization of Resident Education in the Intensive Care Unit (ICU)
When asked about their faculty's perceptions of the 80-hour workweek on resident education, most respondents indicated that faculty perceived it to have a negative influence and this opinion was more prevalent among programs that limited residents' workloads, such as those implementing a cap on admissions. These data confirm a previous study that reported perceptions of a worsening effect of the duty hour limits on CCM education.14 In addition, 63% of respondents felt their faculty had changed their approach to teaching in the ICU as a consequence of the duty hour restrictions. Duty hour limits also may dampen faculty's enthusiasm for teaching, which in turn may affect resident education as well as recruitment into CCM.15
Our findings suggest some areas for improving resident education in CCM, particularly the use of night-float systems and limiting resident outpatient duties during the ICU rotation; these appear to have a positive effect on teaching time. We acknowledge that these suggestions reflect program directors' perceptions and may thus include bias. Our study did not attempt to determine how best to teach/learn specific CCM topics or skills; we suggest further research to study the optimal approaches to teaching topics such as mechanical ventilation and end of life care, which clearly cannot be effectively taught using didactic formats. Other skills, such as teamwork, communication, quality improvement, critical review of the literature, and the practical application of evidence-based principles, need to be evaluated and appropriately incorporated into the CCM education curriculum.16,17
Our study has several limitations. First, self-reporting of the PCCM fellowship program directors may not accurately reflect the perceptions of faculty members who interact with residents in the ICU or the program directors who oversee the residents' education. Second, we did not collect data on the type of hospitals, the background of physicians who provided the teaching, the patient population, and the specialty or the affiliation of supervising physicians. Finally, although our response rate is considered quite high for a national survey, it is possible that nonresponding programs may offer other novel educational approaches or resources not captured by our data.
Conclusions
Our data provide a national assessment of current CCM practice and learning environments that may be used as a first step to improving CCM education programs for internal medicine residents. Our national survey of PCCM programs indicated that despite significant variability in the ICU environment, workload, and team structure, most programs use similar teaching methods and resources for CCM education of internal medicine residents. Some program characteristics such as the presence of night-float systems or limitation of resident outpatient duties during the ICU rotation appear to have a positive effect on teaching time. The findings also suggest that program changes to ensure compliance with duty hour limits are not well perceived by faculty, and their effects on education in the ICU need to be assessed. Our data provide a national assessment of current CCM practice and learning environments that may be used as a first step to improving CCM education programs for internal medicine residents.
Footnotes
Khalid F. Almoosa, MD, MSc, is Assistant Professor of Medicine at University of Texas Health Science Center at Houston; Linda M. Goldenhar, PhD, is Professor of Family Medicine at University of Cincinnati; Jonathan Puchalski, MD, is Assistant Professor of Medicine at Yale University School of Medicine; Jun Ying, PhD, is Assistant Professor and Biostatistician at University of Cincinnati; and Ralph J. Panos, MD, is Professor of Medicine at University of Cincinnati.
This multicenter project was designed and coordinated at the University of Cincinnati and was partially supported by funds from the Division of Pulmonary, Critical Care, and Sleep Medicine and the Department of Internal Medicine, University of Cincinnati.
For this study, all authors report no conflict of interest or any personal or financial support or any involvement with any organization with financial interests in the subject matter of this study.
References
- 1.Pronovost P. J., Angus D. C., Dorman T., Robinson K. A., Dremsizov T. T., Young T. L. Physician staffing patterns and clinical outcomes in critically ill patients: a systematic review. JAMA. 2002;288((17)):2151–2162. doi: 10.1001/jama.288.17.2151. [DOI] [PubMed] [Google Scholar]
- 2.Pronovost P. J., Jenckes M. W., Dorman T., et al. Organizational characteristics of intensive care units related to outcomes of abdominal aortic surgery. JAMA. 1999;281((14)):1310–1317. doi: 10.1001/jama.281.14.1310. [DOI] [PubMed] [Google Scholar]
- 3.Angus D. C., Kelley M. A., Schmitz R. J., White A., Popovich J., Jr Caring for the critically ill patient: current and projected workforce requirements for care of the critically ill and patients with pulmonary disease: can we meet the requirements of an aging population? JAMA. 2000;284((21)):2762–2770. doi: 10.1001/jama.284.21.2762. [DOI] [PubMed] [Google Scholar]
- 4.Dorman T., Angood P. B., Angus D. C., et al. Guidelines for critical care medicine training and continuing medical education. Crit Care Med. 2004;32((1)):263–272. doi: 10.1097/01.CCM.0000104916.33769.9A. [DOI] [PubMed] [Google Scholar]
- 5.Barrett H., Bion J. F. An international survey of training in adult intensive care medicine. Intensive Care Med. 2005;31((4)):553–561. doi: 10.1007/s00134-005-2583-7. [DOI] [PubMed] [Google Scholar]
- 6.Shen J., Joynt G. M., Critchley L. A., Tan I. K., Lee A. Survey of current status of intensive care teaching in English-speaking medical schools. Crit Care Med. 2003;31((1)):293–298. doi: 10.1097/00003246-200301000-00047. [DOI] [PubMed] [Google Scholar]
- 7.Cox C. E., Carson S. S., Ely E. W., et al. Effectiveness of medical resident education in mechanical ventilation. Am J Respir Crit Care Med. 2003;167((1)):32–38. doi: 10.1164/rccm.200206-624OC. [DOI] [PubMed] [Google Scholar]
- 8.Hayes C. W., Rhee A., Detsky M. E., Leblanc V. R., Wax R. S. Residents feel unprepared and unsupervised as leaders of cardiac arrest teams in teaching hospitals: a survey of internal medicine residents. Crit Care Med. 2007;35((7)):1668–1672. doi: 10.1097/01.CCM.0000268059.42429.39. [DOI] [PubMed] [Google Scholar]
- 9.Morgan R., Westmoreland C. Survey of junior hospital doctors' attitudes to cardiopulmonary resuscitation. Postgrad Med J. 2002;78((921)):413–415. doi: 10.1136/pmj.78.921.413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nadel F. M., Lavelle J. M., Fein J. A., Giardino A. P., Decker J. M., Durbin D. R. Assessing pediatric senior residents' training in resuscitation: fund of knowledge, technical skills, and perception of confidence. Pediatr Emerg Care. 2000;16((2)):73–76. doi: 10.1097/00006565-200004000-00001. [DOI] [PubMed] [Google Scholar]
- 11.Scott G., Mulgrew E., Smith T. Cardiopulmonary resuscitation: attitudes and perceptions of junior doctors. Hosp Med. 2003;64((7)):425–428. doi: 10.12968/hosp.2003.64.7.2311. [DOI] [PubMed] [Google Scholar]
- 12.Hanson C. W., III, Durbin C. G., Jr, Maccioli G. A., et al. The anesthesiologist in critical care medicine: past, present, and future. Anesthesiology. 2001;95((3)):781–788. doi: 10.1097/00000542-200109000-00034. [DOI] [PubMed] [Google Scholar]
- 13.Trainor J. L., Krug S. E. The training of pediatric residents in the care of acutely ill and injured children. Arch Pediatr Adolesc Med. 2000;154((11)):1154–1159. doi: 10.1001/archpedi.154.11.1154. [DOI] [PubMed] [Google Scholar]
- 14.Chudgar S. M., Cox C. E., Que L. G., Andolsek K., Knudsen N. W., Clay A. S. Current teaching and evaluation methods in critical care medicine: has the Accreditation Council for Graduate Medical Education affected how we practice and teach in the intensive care unit? Crit Care Med. 2009;37((1)):49–60. doi: 10.1097/CCM.0b013e31819265c8. [DOI] [PubMed] [Google Scholar]
- 15.Lorin S., Heffner J., Carson S. Attitudes and perceptions of internal medicine residents regarding pulmonary and critical care subspecialty training. Chest. 2005;127((2)):630–636. doi: 10.1378/chest.127.2.630. [DOI] [PubMed] [Google Scholar]
- 16.Donchin Y., Gopher D., Olin M., et al. A look into the nature and causes of human errors in the intensive care unit. Crit Care Med. 1995;23((2)):294–300. doi: 10.1097/00003246-199502000-00015. [DOI] [PubMed] [Google Scholar]
- 17.Miller P. A. Nurse-physician collaboration in an intensive care unit. Am J Crit Care. 2001;10((5)):341–350. [PubMed] [Google Scholar]