Abstract
Background
Lifelong learning is an integral component of practice-based learning and improvement. Physicians need to be lifelong learners to provide timely, efficient, and state-of-the-art patient care in an environment where knowledge, technology, and social requirements are rapidly changing.
Objectives
To assess graduates' self-reported perception of the usefulness of a residency program requirement to submit a narrative report describing their planned educational modalities for their future continued medical learning (“Education for Life” requirement), and to compare the modalities residents intended to use with their reported educational activities.
Materials and Methods
Data was compiled from the Education for Life reports submitted by internal medicine residents at the University of Tennessee College of Medicine Chattanooga from 1998 to 2000, and from a survey sent to the same 27 graduates 2 to 4 years later from 2000 to 2004.
Results
Twenty-four surveys (89%) were returned. Of the responding graduates, 58% (14/24) found the Education for Life requirement useful for their future continued medical learning. Graduates intended to keep up with a mean of 3.4 educational modalities, and they reported keeping up with 4.2. In a multivariable analysis, the number of modalities graduates used was significantly associated with the number they had planned to use before graduation (P = .04) but not with their career choice of subspecialization.
Conclusion
The majority of residents found the Education for Life requirement useful for their future continued medical learning. Graduates, regardless of specialty, reported using more modalities for continuing their medical education than they thought they would as residents. Considering lifelong learning early in training and then requiring residents to identify ways to practice lifelong learning as a requirement for graduation may be dispositive.
Introduction
Lifelong learning in one's profession is an integral component of professionalism and practice-based learning and improvement.1 Educational literature2 suggests that lifelong learning skills should be included in every degree curriculum and should be student-centered with room for independent learning during and after graduation. The need for physicians to have highly developed learning skills is even more crucial because the rate of advances in the medical field requires timely and ongoing acquisition of new knowledge and skills.3
The Accreditation Council for Graduate Medical Education4 describes internal medicine as a discipline requiring evidence-based decision making and commitment to lifelong learning. The practice of evidence-based medicine requires continuous updating of one's knowledge to incorporate new medical evidence.5 To date, there appears to be little information in the literature regarding residents' intentions or reported practices of continued medical learning.
Since 1998, the Internal Medicine Department at the University of Tennessee College of Medicine Chattanooga has required that (prior to graduation) all third-year residents submit a reflective information summary about how they intend to keep up with their continuing medical learning. This report is a description of residents' intentions; students are also asked to complete a postgraduation questionnaire that assesses the self-reported utility of the requirement and their current continued medical learning practices.
We hypothesized that most graduates would find the requirement useful, and that those who sought specialization would use more modalities to keep up with continued medical learning and medical advances than other graduates.
Methods
Since 1998, all internal medicine residents have been required submit a narrative report describing their plan for keeping up with continued medical learning (the “Education for Life” requirement) in April of their third year. The information submitted by graduates in 1998, 1999, and 2000 was compiled and tabulated into the following 6 categories: journals, Internet sites, regular readings, continuing medical education, (grand rounds, review courses, etc), affiliation with teaching programs, and involvement in clinical research. We then conducted a survey of the first 3 graduating classes that completed this requirement. The survey was faxed to 27 physicians 2 to 4 years after graduation. For those who failed to return the survey, 2 follow-up calls were made. The project was approved by the university's Institutional Review Board.
The initial survey questions dealt with demographics (name, age, sex, year of graduation, current specialty) and then asked the graduates whether they remembered the Education for Life requirement (yes or no), what modalities they had actually used since graduation (options are listed in the table), whether they were affiliated with teaching programs (yes or no), whether they were involved in clinical research (yes or no), and whether they thought that the requirement was useful for their continued medical learning (yes or no).
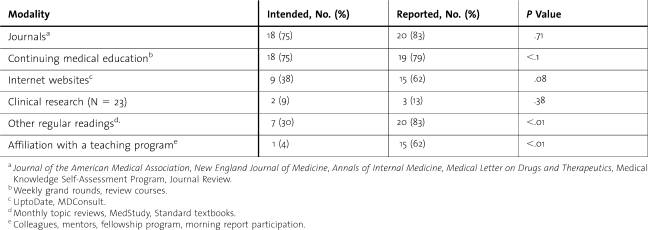
Table.
Educational Modalities Intended to Be Used and Those Actually Used by Graduates to Keep Up With Their Continued Medical Learning (N = 24)
Data from the Education for Life reports and surveys were tabulated, and P values were calculated using the McNemar test. Ordinary least squares regression analysis was done using S-Plus version 6.1 (Insightful Corporation, Seattle, WA) to determine whether the number of education modalities they reported using was associated with specialization after adjusting for the number of modalities they had intended to use. Two-sided P values of less than .05 were considered statistically significant.
Results
Of 27 surveys, 24 were returned, for a response rate of 89%. The respondents had graduated a mean of 3 years prior. The current ages of the graduates ranged from 29 to 42 years with a median of 33 years. Sixty-seven percent (16/24) were men; 29% (7/24) pursued fellowship training, while the others practiced as generalists (primary care and hospitalists).
All the respondents except one remembered the Education for Life requirement, and 58% (14/24) thought it was useful for their future continued medical learning. Journals were the most frequently reported educational modality: 75% (18/24) had intended to use journals, while 83% (20/24) reported using them (P = .68). Continuing medical education was frequently intended and actually used by 75% (18/24) and 79% (19/24), respectively (P ≤ 1). While 38% (9/24) had intended to use Internet sites, 62% (15/24) reported using them (P = .07). Though 8% (2/24) had intended to be involved in clinical research, 13% (3/24) reported involvement (P ≤ 1).
For 2 modalities, graduates reported significantly more use than intended at graduation. Twenty-nine percent (7/24) had intended to use regular readings, while 83% (20/24) reported using this modality (P < .001). Only 4% (1/24) had intended to use affiliation with a teaching program (teaching faculty, morning report, colleagues/mentors, and fellowship program), but 62% (15/24) reported actually using participation in a teaching program (P < .001; see the table).
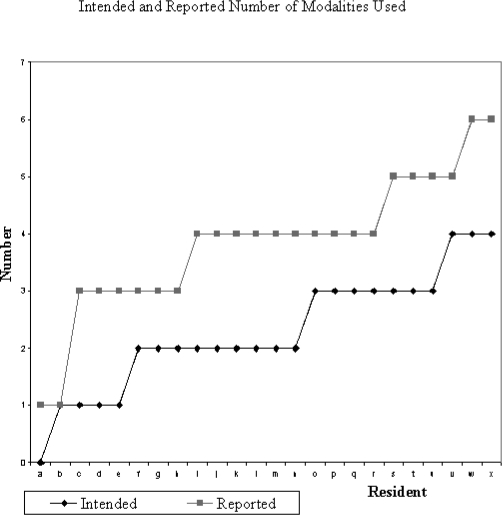
Overall, graduates reported keeping up with a larger number of different modalities than initially intended (a mean of 4.2 methods currently used versus a mean of 3.4 reported at graduation). Graduates usually kept up with one or two more modalities than they originally estimated (figure). In the multivariable analysis we found that the total number of modalities graduates reported using was significantly associated with the number they had planned to use before graduation (P = .04) but was not associated with their career choice.
Figure.
Number of Educational Modalities Physicians Intended to Use and Reported Using to Keep Up With Their Continuing Medical Learning. Each Letter on the X-axis Refers to an Individual Physician, and the Y-axis Denotes the Number of Educational Modalities
Discussion
Our study demonstrated that graduates remembered the Education for Life requirement and the majority perceived it to be useful for their future continued medical learning. Having this requirement helps create an awareness about lifelong learning throughout the residents' training period.
Our graduates reported utilizing journal reading as the most frequent modality for continued learning. In our program, residents conduct a monthly journal review with faculty participation. Repeated exposure to this modality starting from their intern year might explain their continued high utilization of this method. Use of journals is also consistent with the report by Cole6 indicating that medical journal reading is a standard and time-tested method of continuing education among physicians at all stages of the learning process.7
Similarly, residents have consistent exposure to weekly grand rounds organized by the department. They are also allocated one week per year of paid continuing medical education of their selection and are encouraged to attend any medical conferences held locally. This may be why we saw a high and almost equal intent and reported use of weekly grand rounds and review courses.
Literature8,9 suggests an increased use of electronic educational options and that Internet-based continuing medical education programs are just as effective in imparting knowledge as are traditional formats. The significantly greater use of the Internet than was intended by the physicians in our study likely reflects the growing use of this technology as a gateway to learning. This finding is congruent with the results of a randomized controlled trial done by Cook et al10 that found that residents preferred web-based learning.
We were surprised to find that the graduates reported using some modalities more than they had originally intended, particularly for the reported use of regular readings and involvement in teaching programs. It is possible that the flexibility in modes of learning and the easy availability of these opportunities during residency make residents underestimate their desirability. It may also be that residents tend to have a sense of security due to the availability of constant consultation and supervision in a structured environment. Contact with the “real world” may have made the difference between their medical knowledge and the demands of practice starker and precipitated the use of more modalities than they had intended.
Overall, our graduates actually reported using more modalities to keep up with their continued medical learning after graduation than they intended. We had hypothesized that physicians who pursued specialization would report using significantly more educational modalities by virtue of their longer training period and exposure to the academic environment. On the contrary, we found that specialization was not an important factor but that the number of educational modalities they reported for their lifelong learning was influenced by their intended plans before graduation, suggesting that intentions are associated with later reports.
Though there is information on designing curricula that addresses lifelong learning in the educational and nursing literature,12 we were unable to find any in the medicine literature using Entrez PubMed and the search phrase “life-long learning and residency programs.” Having physicians plan a strategy during residency for keeping up with the rapidly advancing field of medicine may thus be a vital initial step to helping promote lifelong learning habits.
Study limitations include the small number of respondents from a single internal medicine residency program, providing a convenience sample without a comparison group, and the fact that the survey tool we used has not been validated. However, to our knowledge this study provides a novel report about efforts to instill the concept of lifelong learning within a residency program.
We now require this narrative report to be a component of a student's educational portfolio, which is reviewed at least biannually with the program director and more frequently with a student's mentors.
In conclusion, the majority of residents found the Education for Life requirement beneficial for their future continued medical learning. They also used more learning modalities than they had initially intended, especially nonjournal readings, affiliation with teaching programs, and the use of the Internet. Having them consider lifelong learning early in residency training and then requiring them to actually identify ways to practice lifelong learning as a requirement for graduation may be dispositive. We suggest that instilling the concept of lifelong learning early in training with longitudinal coaching that identifies the residents' learning methods encourages the resident to reflect on methods of learning and can promote self-directed lifelong learning skills.
Footnotes
Mukta Panda, MD, is Professor, Department of Internal Medicine at University of Tennessee College of Medicine Chattanooga; and Norman A. Desbiens, MD, is Chair, Department of Internal Medicine, University of Tennessee, College of Medicine, Chattanooga, TN.
References
- 1.Brookfield S. D. Understanding and Facilitating Adult Learning. San Francisco, CA: Jossey-Bass Inc; 1986. [Google Scholar]
- 2.Candy P. C. Developing lifelong learners through undergraduate education. In: Summers L., editor. A Focus on Learning. Proceedings of the 4th Annual Teaching Learning Forum. Perth, Australia: Edith Cowan University; 1995. pp. ii–viii. [Google Scholar]
- 3.Lewis M. Lifelong learning: why professionals must have the desire for and the capacity to continue learning throughout life. Health Inf Manag. 1998;28:62–66. [PubMed] [Google Scholar]
- 4.Accreditation Council for Graduate Medical Education. Internal medicine program requirements. Available at: http://www.acgme.org/acwebsite/rrc_140/140_prindex.asp. Accessed March 31, 2009.
- 5.Gupta M. A critical appraisal of evidence-based medicine: some ethical considerations. J Eval Clin Pract. 2003;9:111–121. doi: 10.1046/j.1365-2753.2003.00382.x. [DOI] [PubMed] [Google Scholar]
- 6.Cole T. B. Journal-based continuing medical education. J Med Pract Manage. 1998;14:123–126. [PubMed] [Google Scholar]
- 7.Neill R. A., Bowman M. A., Wilson J. P. Journal article content as a predictor of commitment to change among continuing medical education respondents. J Contin Educ Health Prof. 2001;21:40–45. doi: 10.1002/chp.1340210107. [DOI] [PubMed] [Google Scholar]
- 8.Bennett N. L., Casebeer L. L., Kristofco R. E., et al. Physicians' Internet information-seeking behaviors. J Contin Educ Health Prof. 2004;24:31–38. doi: 10.1002/chp.1340240106. [DOI] [PubMed] [Google Scholar]
- 9.Wutoh R., Boren S. A., Balas E. A. eLearning: a review of Internet-based continuing medical education. J Contin Educ Health Prof. 2004;24:20–30. doi: 10.1002/chp.1340240105. [DOI] [PubMed] [Google Scholar]
- 10.Cook D. A., Dupras D. M., Thompson W. G., Pankratz V. S. Web-based learning in residents' continuity clinics: a randomized, controlled trial. Acad Med. 2005;80:90–97. doi: 10.1097/00001888-200501000-00022. [DOI] [PubMed] [Google Scholar]
- 11.Cook D. A., Dupras D. M. Teaching on the Web: automated online instruction and assessment of residents in an acute care clinic. Med Teach. 2004;26:599–603. doi: 10.1080/01421590400004932. [DOI] [PubMed] [Google Scholar]
- 12.Howatson-Jones I. L. Difficulties in clinical supervision and lifelong learning. Nurs Stand. 2003;17:37–41. doi: 10.7748/ns2003.05.17.37.37.c3398. [DOI] [PubMed] [Google Scholar]