Abstract
Background
The Accreditation Council for Graduate Medical Education requires residency programs to teach 6 core competencies and to provide evidence of effective standardized training through objective measures. George Washington University's Department of Anesthesiology and Critical Care Medicine implemented a pilot program to address the interpersonal and communication skill competency. In this program, we aimed to pilot the Relationship Express model, a series of exercises in experiential learning to teach anesthesiology residents to build effective relationships with patients in time-limited circumstances. The purpose of this paper is to describe the application of this model for anesthesiology training.
Methods
A total of 7 first-year clinical anesthesiology residents participated in this pilot study, and 4 residents completed the entire program for analysis purposes. Relationship Express was presented in three 1.5-hour sessions: (1) introduction followed by 2-case, standardized patient pretest with feedback to residents from faculty observers; (2) interpersonal and communication skills didactic workshop with video behavior modeling; and (3) review discussion followed by 2-case, standardized patient posttest and evaluation.
Results
Modified Brookfield comments revealed the following themes: (1) time constraints were realistic compared with clinical practice; (2) admitting errors with patients was difficult; (3) patients were more aware of body language than anticipated; (4) residents liked the group discussions and the video interview; (5) standardized patients were convincing; and (6) residents found the feedback from faculty and standardized patients helpful.
Conclusions
Resident retrospective self-assessment and learning comments confirm the potential value of the Relationship Express model. This program will require further assessment and refinement with a larger number of residents.
Editor's Note: The online version of this article includes the case instructions for the SP and the resident (25KB, doc) , the C2UBE2 checklist (33.5KB, doc) , the communication self-assessment (46.5KB, doc) , the resident self-evaluation, modified Brookfield Critical Incident Questionnaire (26KB, doc) , and videos depicting a “poor” and “good” bad result case scenarios.
Background
The Accreditation Council for Graduate Medical Education requires residency programs to teach the 6 core competencies, including interpersonal skills and communication.1 Anesthesiologist-patient interactions are often confounded by time constraints, production pressure, patient anxiety and stress, medication or condition-induced delirium or amnesia, and absence of a historical relationship. Faculty instruction and assessment of interpersonal and communication skills also may be limited as residents attempt to learn proper strategies to describe procedures, obtain consents, and discuss complications. Formal teaching often does not address communication skills, potentially because of the challenge of assessing this competency.2 Yet poor communication accounts for many of the complaints registered by patients and may contribute, more than any other cause, to malpractice claims.2 This makes it important for anesthesiologists to address interpersonal and communication skills as an integral part of the residency training process and as an element of patient safety.
A recent assessment of communication patterns during the preoperative period found that anesthesiology residents failed to adequately involve patients in determining the goals of anesthesia and recovery.3 Other studies have focused on indirect measurements, such as patient satisfaction or patient anxiety levels, to assess communication skills.4,5 Although research suggests that the communication skills of anesthesiology residents are not always optimal, no methods have been suggested to date for teaching these skills in the time-constrained nature of anesthesiology practice. Our program, “Relationship Express,” is a new method of assessing and learning time-sensitive communication skills. We describe the application of this model to anesthesiology training.
Intervention
“Relationship Express” is a 3-session, 4.5-hour communication skills curriculum for anesthesiology residents that is brief enough to fit into a busy clinical program. In session 1 (1.5 hours), residents demonstrate their communications skills in 2 encounters with standardized patients (SPs), actors trained to convey a patient scenario in a reliable and consistent manner,6 and receive checklist feedback from the SPs and oral feedback from observing faculty. Session 2 consists of a 1.5-hour communication skills workshop. In session 3 (1.5 hours), residents reencounter the same SP cases as in session 1 and receive checklist feedback, allowing them to compare preworkshop and postworkshop performances.
The Relationship Express model teaches residents how to build effective relationships in a limited time using the C2UBE2 tool. C2UBE2 was developed by one of the authors (B.B.) after extrapolating key elements from The Kalamazoo Consensus Statement for Essential Elements of Communication in Medical Encounters.7 The tool was developed to respond to the time constraints of a busy anesthesiology practice. Accordingly, residents are expected to develop skills to establish effective relationships in a limited period of time, simulating the clinical anesthesiologist's experience in the perioperative setting. C2UBE2 presents a highly focused, simple method to rapidly build relationships by presenting 6 objectives the clinician can reasonably be expected to attain within a 10-minute visit: Concerns—identify concerns; Concerns—validate concerns; Understanding—ensure understanding; Buy-in—assure patient agreement with diagnosis and plans; Environment—create a warm relationship environment; and Environment—create a collaborative environment (box). C2UBE2 served as both a learning tool in the workshop and a feedback tool in the SP encounters. It formed the basis of the checklist the SPs used to provide feedback to the residents on their communication skills both before and after the workshop.
box Elements of C2UBE2 Checklist
Category
Concerns—identify concerns
Concerns—validate concerns
Understanding—ensure understanding
Buy-in—assure patient agreement with diagnosis and plans
Environment—create a warm relationship environment
Environment—create a collaborative environment
Procedure
All 7 anesthesiology residents from the first year of clinical anesthesiology training consented to participate in this pilot program in 2008. Two anesthesiology faculty members and 2 educators from the Clinical Learning and Simulation Skills (CLASS) center conducted the program. Faculty instructors participated in a 1.5-hour development session with CLASS educators to standardize the faculty in assessing residents and giving feedback. The SPs were recruited from a pool used by George Washington University and received 4 hours of training using standard protocols. Uniformity of assessment and feedback was tested with sample cases via video to confirm that faculty and SPs were providing similar scoring.
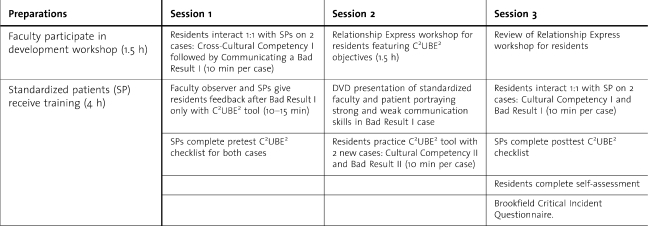
The three 1.5-hour sessions of the program were presented on consecutive Monday afternoons during protected educational time (table). In the first session, the residents encountered 2 cases: communicating a Bad Result I and Cultural Competency I, selected from the George Washington CREATE (Cross Residency Exercises for ACGME Training and Examination) communications workshops. Anesthesiology faculty adapted these cases for anesthesiology residents. The online appendixes 1 and 2 outline the Bad Results I case instructions for the SP and the resident, respectively.
Table.
Process of Relationship Express Workshop
Residents were given 10 minutes to conduct each interview. All residents performed the Cultural Competency I case first, then the Bad Result I case. The SPs used a checklist based on the C2UBE2 tool to conduct a formative assessment of the resident after each case (online appendix 3). The instrument used a 5-point Likert scale ranging from “strongly disagree” (1) to “strongly agree” (5). Faculty observers using real-time video monitors watched residents perform the Bad Results I case and completed the same checklist as the SPs.
In the second session, the residents were given a workshop presenting the C2UBE2 approach. Faculty summarized the C2UBE2 objectives, demonstrated sample skills to achieve the objectives, and challenged residents to personalize the skills to suit their communication styles. Residents practiced the C2UBE2 method by critiquing a video of a George Washington University anesthesiology faculty member's mock interview of an SP portraying the original Bad Result I case. The video demonstrated the case twice: first with weak communication skills, and second with strong communication skills based on C2UBE2 objectives. Residents then practiced the method at a higher level by interviewing 2 SPs portraying a Bad Result II and a Cultural Competency II case. In the third session, the pretest Bad Result I case and the Cultural Competency I case were reintroduced to the residents as a posttest in the form of an objective structured clinical evaluation. This program was internally funded by the CLASS center and approved by The university's Institutional Review Board.
Assessment
Data for this pilot project were collected from 2 instruments. The first was a communications self-assessment questionnaire based on the C2UBE2 checklist, which the residents completed retrospectively. It consisted of 7 items rated on a 5-point Likert scale, with 5 being the best score (online appendix 4). During the third session, residents were asked to self-assess their communication skills prior to the program versus their current perceptions (retrospective premethod/postmethod). Residents assessed the program using an adaptation of the Brookfield Critical Incident Questionnaire (online appendix 5).8 We identified themes from their narrative comments, focusing on comments made by 2 or more residents. The C2UBE2 checklist was completed by SPs and used to provide feedback to residents on their performance on the pretest and posttest SP exercises. Only 4 residents completed the entire program, because of call obligations and scheduled vacations, and no quantitative analyses were conducted.
Results
The following themes emerged from residents' assessment of the program: (1) the time constraints of the SP exercise appeared realistic compared with clinical practice; (2) admitting errors with patients was difficult; (3) patients were more aware of residents' body language than anticipated; (4) SPs were thought to be convincing in their portrayal of patients; (5) residents liked the group discussions and the video interview; (6) residents found the feedback from faculty and SPs helpful; and (7) overall, residents liked the Relationship Express model.
Discussion
Relationship Express is a novel approach to resident learning and assessment of communication skills that takes into account the limited time these clinicians have to interact with their patients. It provided residents with experiential, hands-on learning and immediate feedback through the use of SPs, case scenarios, and faculty with standardized training. By taking advantage of George Washington University's CLASS center, complete with SPs, examination rooms, and digital video with remote viewing capabilities, residents were able to learn in an interactive, dynamic learning environment that was psychologically safe.
Two theoretical constructs formed the basis of the C2UBE2 approach. The first was that a guide to communications for clinicians should be constituted as a series of objectives to be attained during every encounter. Our objectives-based checklist clarified the necessary tasks and allowed for easy learner comprehension and memory during the clinical encounter. The C2UBE2 tool encouraged learners to use skills compatible with their own individual styles by presenting a menu of sample skills that could be used to achieve the 6 C2UBE2 objectives. For example, when teaching the C—concern objective, suggested approaches included: (1) ask “Do you have any special concerns about this problem? Is there anything else?”; (2) probe explanatory model: “What do you think might be causing this?”; (3) respond to emotion: “You look upset…”; (4) summarize patient perspective: “So, if I understood you correctly…” The second theoretical construct, suggested by the workshop title, was that essential communications objectives could be achieved in a short period of time.
Residents perceived their communication skills to be improved as a result of the objective-based C2UBE2 tool. The modified Brookfield Critical Incident Questionnaire also captured interesting self-reflective learning: residents commented that they found it surprising to hear that SPs paid attention to a resident's body positioning as a cue for warmth and empathy. Other residents were intrigued by how difficult it was to take personal responsibility for an error. Although previous authors of SP studies have concluded that residents maintain a low level of self-awareness during SP experiences,9 the comments we solicited reflected a high degree of self-awareness. Overall, residents found the SPs convincing and valued the feedback from the program.
Our pilot study has several limitations. Past studies have suggested that communication skills are case specific6; consequently, a range of cases may be necessary to teach this competency to residents. The Accreditation Council for Graduate Medical Education posits that 16 to 18 scenarios may be required for adequate performance evaluation,1 yet our pilot only used 4 scenarios to assess resident improvement, potentially reducing generalizability. Also, although the C2UBE2 tool offers a useful framework for feedback to residents, it needs to be validated with a larger cohort before it can be used for assessment.
Implementation
Challenges in implementing the Relationship Express model included determining the proper resident cohort, coordinating scheduling of sessions, and establishing the optimal time required for the workshop. We chose first-year clinical anesthesiology residents because Social Skills Inventory studies have concluded that verbal communication improves as residents gain experience, so early exposure to Relationship Express may prove valuable to communication-naïve residents. A “rolling” approach to training based on availability, as was done in other studies, might alternatively have been considered to improve participation at the expense of efficiency. We made our program 4.5 hours in length. A review of studies evaluating teaching and assessment of communication skills concluded that observation of behavioral changes was detectable to a greater extent when interventions lasted longer than 4.5 hours.2
“Learning-in-action” with SPs has been promoted as one of the most effective means of teaching skills to adult learners and was therefore a potential advantage of the Relationship Express model.1 The SP-learner interactions improve upon traditional, observational learning by providing a safe climate to explore suboptimal communication strategies with immediate, personalized feedback,6,7 and video modeling of behavior has been shown to be useful in teaching communication skills.10 Group discussions and redundant exposure to common scenarios further solidified key concepts for resident learners.
Another potential educational advantage to this program was the objective nature of the assessment. Our Relationship Express model trained all faculty and SP evaluators to achieve a uniform rating of residents. The Likert scale rating sheet was formulated directly from the C2UBE2 tool, and consequently mirrored resident expectations precisely.
Conclusions
The Relationship Express model, featuring the C2UBE2 tool, offers a novel approach to teaching interpersonal and communication skills. We are optimistic that the ease of use and practical value of the Relationship Express model may stimulate interest in a collaborative effort among anesthesiology residency programs and other specialties that require focused, time-limited patient interactions to validate the model and the C2UBE2 instrument. Validation with a larger number of residents and cases is warranted prior to widespread adoption.
Footnotes
All authors are at George Washington University Medical Center. Jeffrey S. Berger, MD, MBA, is Assistant Professor of Anesthesiology, Department of Anesthesiology and Critical Care Medicine; Benjamin Blatt, MD, is Associate Professor of Medicine, Clinical Learning and Simulation Skills Center; Brian McGrath, MD, MPH, is Professor of Anesthesiology, Department of Anesthesiology and Critical Care Medicine; Larrie Greenberg, MD, is Professor of Pediatrics, Clinical Learning and Simulation Skills Center; and Michael J. Berrigan, MD, PhD, is Seymour Alpert Professor of Anesthesiology, Department of Anesthesiology and Critical Care Medicine.
No grants, external sponsors, or funding were required for this research.
References
- 1.Accreditation Council for Graduate Medical Education. 2005 Outcome Project. Available at: http://www.acgme.org/Outcome. Accessed September 5, 2010. [DOI] [PubMed]
- 2.Hulsman R. L., Ros W. J. G., Winnubst J. A. M., Bensing J. M. Teaching clinically experienced physicians communication skills: a review of evaluation studies. Med Educ. 1999;33((9)):655–668. doi: 10.1046/j.1365-2923.1999.00519.x. [DOI] [PubMed] [Google Scholar]
- 3.Zollo R. A., Lurie S. J., Epstein R., Ward D. S. Patterns of communication during the preanesthesia visit. Anesthesiology. 2009;111((5)):971–978. doi: 10.1097/ALN.0b013e3181b8f7e3. [DOI] [PubMed] [Google Scholar]
- 4.Harms C., Young J. R., Amsler F., Zettler C., Scheidegger D., Kindler C. H. Improving anesthetists' communication skills. Anaesthesia. 2004;59((2)):166–172. doi: 10.1111/j.1365-2044.2004.03528.x. [DOI] [PubMed] [Google Scholar]
- 5.Becker K. L., Rose L. E., Berg J. B., Park H., Shatzer J. H. The teaching effectiveness of standardized patients. J Nurs Educ. 2006;45((4)):103–111. doi: 10.3928/01484834-20060401-03. [DOI] [PubMed] [Google Scholar]
- 6.Yudkowsky R., Downing S., Sandlow L. Developing an institution-based assessment of resident communication and interpersonal skills. Acad Med. 2006;81((12)):1115–1122. doi: 10.1097/01.ACM.0000246752.00689.bf. [DOI] [PubMed] [Google Scholar]
- 7.Makoul G. essential elements of communication in medical encounters: the Kalamazoo consensus statement. Acad Med. 2001;76((4)):390–393. doi: 10.1097/00001888-200104000-00021. [DOI] [PubMed] [Google Scholar]
- 8.Brookfield S. Critically reflective practice. J Contin Educ Health Prof. 1998;18((4)):197–205. [Google Scholar]
- 9.Hassett J. M., Zinnerstrom K., Nawotniak R. H., Schimpfhauser F., Dayton M. T. Utilization of standardized patients to evaluate clinical and interpersonal skills of surgical residents. Surgery. 2006;140((4)):633–638. doi: 10.1016/j.surg.2006.07.014. discussion 638-9. Epub 2006 Sep 6. [DOI] [PubMed] [Google Scholar]
- 10.Fertleman C., Gibbs J., Eisen S. Video improved role play for teaching communication skills. Med Educ. 2006;39((11)):1155–1156. doi: 10.1111/j.1365-2929.2005.02283.x. [DOI] [PubMed] [Google Scholar]