Abstract
Background
Residency programs accredited by the ACGME are required to teach core competencies, including systems-based practice (SBP). Projects are important for satisfying this competency, but the level of knowledge and problem-solving skills required presupposes a basic understanding of the field. The responsibilities of anesthesiologists include the coordination of patient flow in the surgical suite. Familiarity with this topic is crucial for many improvement projects.
Intervention
A course in operations research for surgical services was originally developed for hospital administration students. It satisfies 2 of the Institute of Medicine's core competencies for health professionals: evidence-based practice and work in interdisciplinary teams. The course lasts 3.5 days (eg, 2 weekends) and consists of 45 cognitive objectives taught using 7 published articles, 10 lectures, and 156 computer-assisted problem-solving exercises based on 17 case studies. We tested the hypothesis that the cognitive objectives of the curriculum provide the knowledge and problem-solving skills necessary to perform projects that satisfy the SBP competency. Standardized terminology was used to define each component of the SBP competency for the minimum level of knowledge needed. The 8 components of the competency were examined independently.
Findings
Most cognitive objectives contributed to at least 4 of the 8 core components of the SBP competency. Each component of SBP is addressed at the minimum requirement level of exemplify by at least 6 objectives. There is at least 1 cognitive objective at the level of summarize for each SBP component.
Conclusions
A curriculum in operating room management can provide the knowledge and problem-solving skills anesthesiologists need for participation in projects that satisfy the SBP competency.
Editor's Note: The online version of this article contains 3 supplemental tables providing additional details about the course material, as well as an appendix of the 156 exercises in 17 cases that the students perform.
Background
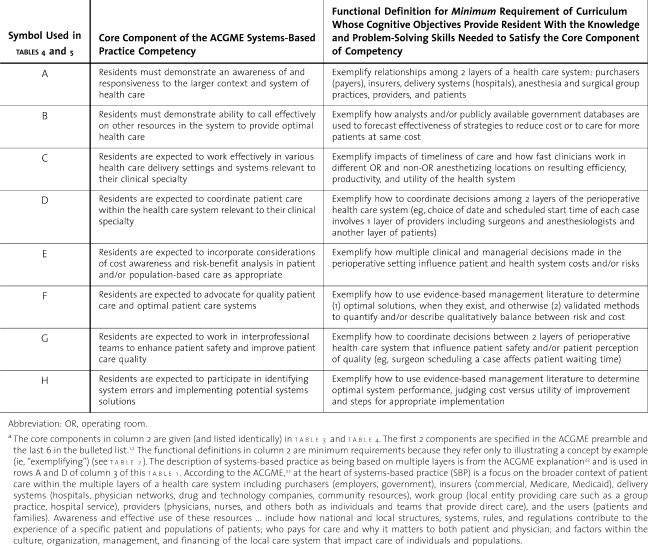
The Accreditation Council for Graduate Medical Education (ACGME) mandates that residency programs in all specialties teach and assess 6 general competencies, including systems-based practice (SBP).1,2 The components of the SBP competency (table 1) and functional definitions encompass content related to “cost effective practice,” including “tools and techniques for controlling costs and allocating resources, understanding of financing and insurance structures, mock practice experiences/mock financials, and evaluating risk and benefit of costly prescribing.”3 Anesthesiologists engage in operating room (OR) management, essentially directing the surgical suite and ensuring smooth patient flow. Practitioners must be able to understand coordination of surgical suites and explain the principles to OR nurses, nursing directors, surgeons, surgical technologists, anesthesia technicians, postanesthesia care unit nurses, intensive care unit nurses, and administrators.4,5 Among the 61 English language articles identified by searching “operating room management” in Web of Science, 74% were published in anesthesiology journals.
Table 1.
Functional Definitions of the Accreditation Council for Graduate Medical Education (ACGME) Competencies in Systems-Based Practicea
Three characteristics of hospital surgical suites cause coordination of surgical care to differ from SBP in other specialties. First, surgery is non-preemptive, meaning that once a surgical procedure is started, it must be completed. The patient cannot be moved out of the OR and replaced by another patient, with the surgery to be finished at a later time. All decisions concerning the scheduling of a case are therefore made before the case is started. Second, surgical cases with anesthesia have a large mean absolute error in predicted duration.6 Third, variability in the daily numbers of scheduled cases affects the efficiency of use of OR time. Coordination of cases is therefore an important issue.
The mathematics of forecasting case durations is nonintuitive. For example, the time remaining in a case that is running late is the time until the end of surgery, plus a relative constant for irrigation, inspection, incision closure, awakening from anesthesia, and transport to recovery. If a case scheduled for 3 hours is still ongoing after 2.5 hours, the median expected time remaining is not 0.5 hour but longer, for example, 1.0 hour.7 If still ongoing at 3.5 hours, the best estimate of the time remaining, and when the next case can begin, is still 1.0 hour.7 These nonintuitive aspects of OR scheduling should be understood by anesthesiologists coordinating the perioperative team, as well as by anesthesiology residents embarking on an SPB project in OR management. The knowledge and problem-solving skills needed for OR management are generally not readily learned on the job but through formal study.8 Innate psychological biases9 and misconceptions10 must be overcome.
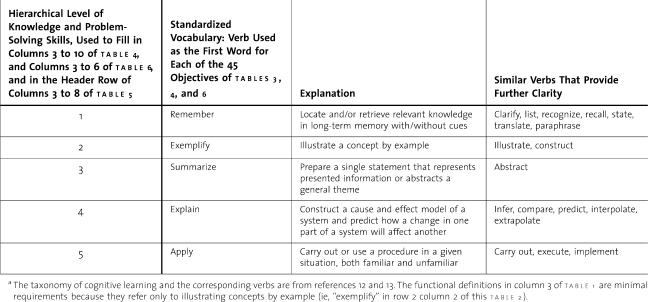
In a previous study of teaching related to the SBP competency in anesthesiology, Delphin and Davidson11 showed that resident team projects are effective. Although indispensable to satisfying the competency, the level of knowledge and problem-solving skills needed to select and conduct projects presupposes a basic level of understanding, such as exemplifying and summarizing principles according to higher levels of Bloom's taxonomy (table 2).12,13 Residents may not yet possess this knowledge. Delphin and Davidson's team-oriented approach is best applied once residents have acquired these basic skills.
Table 2.
Definitions of Standardized Vocabulary for the Knowledge and Skill Levels Attained for Each Competency and Cognitive Objectivea
Curriculum Design
To offer residents a basic understanding of the scientific principles of OR management as they relate to SBP, we developed a course in OR management originally designed for master's-level hospital administration students in the University of Iowa Department of Health Management & Policy. The 35-hour course is given over 3.5 days during 1 weekend or 2 successive weekends. The course teaches residents when statistical forecasting is necessary, ways to apply literature searches to choose among forecasting methods, and how to explain to analysts the needs of an anesthesia group.
Although the curriculum was designed for hospital administration students, participants to date have been anesthesiologists and a few perioperative analysts and OR nursing directors. Other hospitals send representatives to the course to learn principles of OR management for application at their own institutions. One hospital sent a contingent of anesthesiologists, OR nursing directors, and financial analysts to the course to lay a common foundation on which they could base their decisions. Thus, the course has been attended by a wide variety of personnel with varying backgrounds. As part of our needs assessment to apply for continuing medical education credit, we observed that the curriculum's cognitive objectives provide the knowledge and problem-solving skills necessary to satisfy the ACGME recommendations for teaching “an awareness of and responsiveness to the larger context and system of health care” and teaching cost-effective practice (supplemental online tables 4 (48.5KB, doc) through 6 (98KB, doc) ).
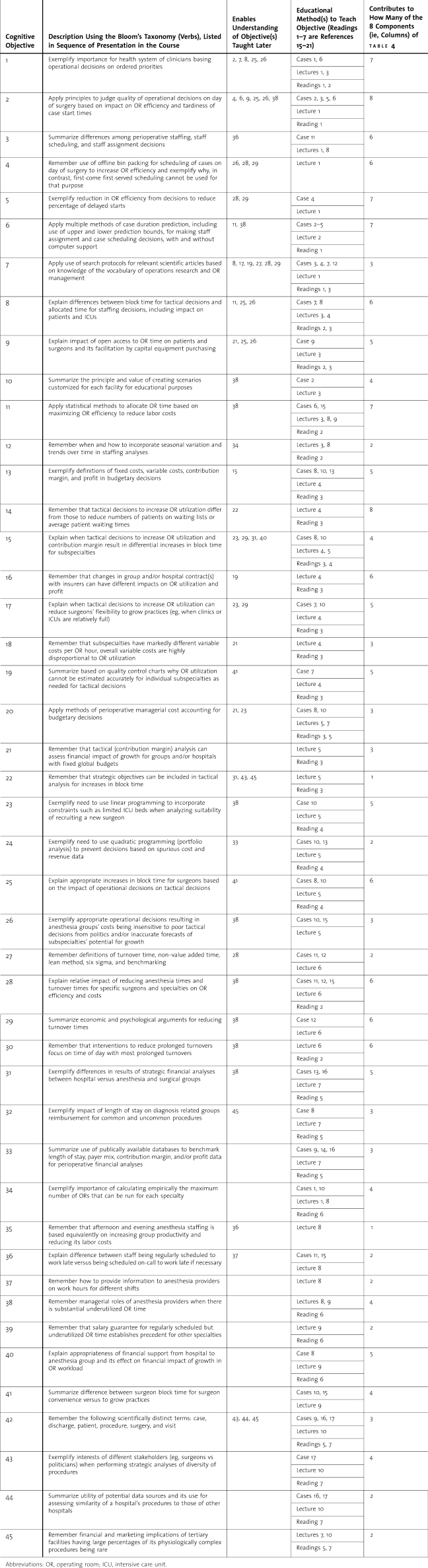
The curriculum includes 3 educational methods (table 3 and supplemental online table 5 (95KB, doc) ): 10 lectures and 156 exercises using 17 case studies (online appendix (134KB, doc) ). Our website (www.FranklinDexter.net/education.htm) contains all slides used in the lectures, 7 targeted articles relevant to SBP for anesthesiology residents,14–21 and a link to “statistics for anesthesia,” which is a review of required background material involving basic statistics up to the level of Student t test.22 The lectures, slides, and review of statistics are all publicly available. Learners complete the 156 exercises using an Excel workbook tool that provides immediate, adaptive, elaborated feedback to numeric and short answer questions. The adaptive feedback is programmed without macros by the use of more than 4250 Excel spreadsheet formulae containing more than 8300 Excel functions. Variations of the curriculum have been given to groups of 7 to 50 students on 14 occasions.
Table 3.
The Teaching of Cognitive Objectives and the Contribution of Each Objective to Accreditation Council for Graduate Medical Education Components
table 2 lists 5 hierarchical levels of knowledge from the review by Anderson and colleagues13 of the revision of Bloom's taxonomy. table 1 shows the ACGME's definitions of the components of SPB. Remembering a new concept is the minimum level of knowledge, followed by an ability to exemplify, summarize, explain, and apply that concept. We used this standardized vocabulary to formulate the 45 objectives of the curriculum and evaluate the extent to which each objective satisfies the core components of the SBP competency.
Using the ACGME language in table 1, we created functional definitions that would provide anesthesia residents with the knowledge and problem-solving skills needed to satisfy the component. Each definition is based only on exemplifying the material (ie, illustrating by example).
Implementation of the Curriculum
We assigned ratings (levels of knowledge using standardized verbs) to calculate the level at which each of the 45 objectives satisfied each of the core components of the competency (supplemental online table 4) and the ACGME recommendations for implementation (supplemental online table 6). Ratings were based on the depth of the lecture material presented to the students and the nature of the 156 exercises in the Excel workbook. The exercises are included as supplemental online appendix. We use Objective 6 as an example to show how the educational materials and exercises were used to determine without ambiguity the appropriate verb from the standardized vocabulary. The number of core components satisfied by each objective is summed in table 3 column 5. The number of cognitive objectives that satisfy each core component at each hierarchical level of knowledge is summed in table 3. The number of cases, readings, and lectures associated with each component is also summed in table 3.
For example, Objective 6 is to “Apply multiple methods of case duration prediction, including use of upper and lower prediction bounds, for making staff assignment and case scheduling decisions, with and without computer support.” This objective refers to the frequent decision whether or not to insert a pending add-on case into a gap in the schedule. Assume the first case of the day was scheduled to last until noon but ended at 9 am because the pathology was more extensive than anticipated. The next case was not scheduled to begin until 12:30 pm. Another surgeon had a 3-hour add-on case in a different OR and was hoping to start sooner than the scheduled noon start time. The OR manager should consider the 90% upper prediction bound for the duration of the add-on case when deciding whether it would fit into the schedule without disrupting later cases and extending the workday. In addition to using prediction bounds, the case requires students to calculate the economic savings by moving a case, revise case scheduling to reduce the probability of resource conflict over a surgical microscope, estimate the cost of time spent waiting for patients, determine optimal hours of staffing based on the standard deviation for the length of the workday, and examine the effects of nonsequential case scheduling on personnel needs. The case thus requires students to “apply” their knowledge.
The curriculum is taught using 17 cases, 10 lectures, and 7 readings (shown in supplemental online table 5 last 3 columns). Each objective contributes to at least 1 of the 8 ACGME SBP core components, and most contribute to at least 4 of them (table 3 last 3 columns). The objectives contributing to just 1 component enable understanding of objectives taught later and thus cannot be deleted.
Each component of SBP is addressed at the minimum requirement level of exemplify by at least 6 of the 45 specific objectives (table 5 column 8). There is at least 1 cognitive objective at the level of summarize (level 3) for each component (table 5 column 5).
Discussion and Conclusions
We designed a 35-hour curriculum to teach the basic principles of operations research for use in OR management. The curriculum consists of 10 lectures, 7 readings, and 17 case studies. We have shown that 45 cognitive objectives provide the knowledge and problem-solving skills needed for anesthesiology residents to perform projects that would satisfy the ACGME competency in SBP. The unique curriculum reflects anesthesiologists' responsibilities for coordinating OR care and the fundamental differences of hospital OR management from that of other medical specialties.
Our curriculum in operations research for surgical services provides the knowledge and problem-solving skills needed to satisfy all elements of the ACGME core competency in SBP. Examples illustrate the reliability and face validity of the objectives of the curriculum, the assignment of levels of knowledge using a standardized vocabulary, and the assessment of the extent to which each objective meets the 8 ACGME core components of SBP and the 4 elements for implementation.
Anesthesiologists differ from physicians in other specialties in that their professional work involves the smooth flow of patients through the surgical suite. The literature on SBP projects for other disciplines focuses on quality improvement or reducing medical error, while our curriculum addresses the coordination of patient flow. Our curriculum is therefore useful for practicing anesthesiologists, nursing directors, analysts, and other OR staff. In addition, the curriculum addresses 2 of the 5 Institute of Medicine core competencies for health professionals—evidence-based practice and work in interdisciplinary teams.21 Evidence-based practice is addressed by almost all of the cases and lectures. Participation of nursing directors, certified registered nurse anesthetists, operations managers, financial officers, and others enhances understanding on the part of anesthesia personnel of the viewpoint of others, satisfying the Institute of Medicine's competency of “work in interdisciplinary teams.”23
Anesthesiologists, OR nursing directors, industrial engineers, analysts, and administrators report that the curriculum is useful. All 17 students enrolled in the most recent course presentation submitted evaluation forms. They were asked to agree or disagree with various statements on a 5-point scale, with 4 being “agree” and 5 being “strongly agree.” All students scored the course a 4 or 5 with respect to “class increased my trust in applying evidence-based statistical methods and analytic reports in health care management decisions,” “class enhanced my ability to analyze managerial questions critically and solve the problems in a logical, evidence-based manner,” “course was well planned and content was organized logically,” and “cases and readings aided in learning the material.” However, we have no such formative assessments from anesthesiology residents. Future work is needed to evaluate the curriculum to determine the extent to which it aids anesthesiology residents in developing projects for SBP.
Footnotes
All authors are at University of Iowa. Ruth E. Wachtel, PhD, MBA, is Associate Professor of Anesthesia; and Franklin Dexter, MD, PhD, is Professor of Anesthesia and Health Management & Policy.
Drs Wachtel and Dexter are professors at University of Iowa, and their teaching responsibilities include the course whose curriculum is described in this article. They receive no funds personally other than their salaries from the university, including no travel expenses or honoraria, and have tenure with no incentive programs (eg, linked to tuition). Dr Dexter also performs paid statistical consulting work for hospitals and health care facilities, for which all remuneration is paid to the university. Curriculum development was funded by departmental and institutional sources.
References
- 1.Accreditation Council for Graduate Medical Education (ACGME), 2006. Available at: http://www.ACGME.org/outcome/e-learn/FacManual_module2.pdf. Accessed June 1, 2010.
- 2.Accreditation Council for Graduate Medical Education (ACGME) Educational program, curriculum components, ACGME competencies, systems-based practice, common program requirement, 2008. Available at: www.ACGME.org/acWebsite/navPages/commonpr_documents/IVA5f_EducationalProgram_ACGMECompetencies_SBP_Explanation.pdf. Accessed June 1, 2010.
- 3.Joyce B. Practical implementation of the competencies. Accreditation Council for Graduate Medical Education (ACGME), 2006. Available at: http://www.ACGME.org/outcome/e-learn/redir_module2.asp. Accessed June 1, 2010.
- 4.Marjamaa R. A., Kirvela O. A. Who is responsible for operating room management and how do we measure how well we do it. Acta Anaesthesiol Scand. 2007;51:809–814. doi: 10.1111/j.1399-6576.2007.01368.x. [DOI] [PubMed] [Google Scholar]
- 5.Larsson J., Holmström I., Rosenqvist U. Professional artist, good Samaritan, servant and co-ordinator: four ways of understanding the anaesthetist's work. Acta Anaesthesiol Scand. 2003;47:787–793. doi: 10.1034/j.1399-6576.2003.00151.x. [DOI] [PubMed] [Google Scholar]
- 6.Stepaniak P. S., Heij C., Mannaerts G. H., de Quelerij M., de Vries G. Modeling procedure and surgical times for current procedural terminology-anesthesia-surgeon combinations and evaluation in terms of case-duration prediction and operating room efficiency: a multicenter study. Anesth Analg. 2009;109:1232–1245. doi: 10.1213/ANE.0b013e3181b5de07. [DOI] [PubMed] [Google Scholar]
- 7.Dexter F., Epstein R. H., Lee J. D., Ledolter J. Automatic updating of times remaining in surgical cases using Bayesian analysis of historical case duration data and instant messaging updates from anesthesia providers. Anesth Analg. 2009;108:929–940. doi: 10.1213/ane.0b013e3181921c37. [DOI] [PubMed] [Google Scholar]
- 8.Dexter E. U., Dexter F., Masursky D., Garver M. P., Nussmeier N. A. Both bias and lack of knowledge influence organizational focus on first case of the day starts. Anesth Analg. 2009;108:1257–1261. doi: 10.1213/ane.0b013e31819a6dd4. [DOI] [PubMed] [Google Scholar]
- 9.Dexter F., Lee J. D., Dow A. J., Lubarsky D. A. A psychological basis for anesthesiologists' operating room managerial decision-making on the day of surgery. Anesth Analg. 2007;105:430–434. doi: 10.1213/01.ane.0000268540.85521.84. [DOI] [PubMed] [Google Scholar]
- 10.Brown D. E. Using examples and analogies to remediate misconceptions in physics: factors influencing conceptual change. J Res Sci Teach. 1992;29:17–34. [Google Scholar]
- 11.Delphin E., Davidson M. Teaching and evaluating group competency in systems-based practice in anesthesiology. Anesth Analg. 2008;106:1837–1843. doi: 10.1213/ane.0b013e318173216e. [DOI] [PubMed] [Google Scholar]
- 12.Thomas P. A. Step 3, goals and objectives, focusing the curriculum. In: Kern D. E., Thomas P. A., Hughes M. T., editors. Curriculum Development for Medical Education, a Six-Step Approach. 2nd ed. Baltimore, MD: Johns Hopkins University Press; 2009. [Google Scholar]
- 13.Anderson L. W., Krathwohl D. R., Airasian P. W., et al. A Taxonomy for Learning, Teaching, and Assessing: A Revision of Bloom's Taxonomy of Educational Objectives. Abridged ed. Vol. 31. New York, NY: Longman; 2001. [Google Scholar]
- 14.Commission on Accreditation of Healthcare Management Education. Self study handbook appendix A–a glossary of curriculum content areas, section III.B.5 Operations assessment and improvement, 2008, pp. ii. Available at: http://www.cahme.org/Resources/Appendix%20A%20-%20Glossary%20of%20Curriculum%20Content%20Areas.pdf. Accessed June 1, 2010.
- 15.McIntosh C., Dexter F., Epstein R. H. Impact of service-specific staffing, case scheduling, turnovers, and first-case starts on anesthesia group and operating room productivity: tutorial using data from an Australian hospital. Anesth Analg. 2006;103:1499–1516. doi: 10.1213/01.ane.0000244535.54710.28. [DOI] [PubMed] [Google Scholar]
- 16.Dexter F., Epstein R. D., Traub R. D., Xiao Y. Making management decisions on the day of surgery based on operating room efficiency and patient waiting times. Anesthesiology. 2004;101:1444–1453. doi: 10.1097/00000542-200412000-00027. [DOI] [PubMed] [Google Scholar]
- 17.Wachtel R. E., Dexter F. Tactical increases in operating room block time for capacity planning should not be based on utilization. Anesth Analg. 2009;106:215–226. doi: 10.1213/01.ane.0000289641.92927.b9. [DOI] [PubMed] [Google Scholar]
- 18.Dexter F., Ledolter J., Wachtel R. E. Tactical decision making for selective expansion of operating room resources incorporating financial criteria and uncertainty in sub-specialties' future workloads. Anesth Analg. 2005;100:1425–1432. doi: 10.1213/01.ANE.0000149898.45044.3D. [DOI] [PubMed] [Google Scholar]
- 19.Wachtel R. E., Dexter F., Lubarsky D. A. Financial implications of a hospital's specialization in rare physiologically complex surgical procedures. Anesthesiology. 2005;103:161–167. doi: 10.1097/00000542-200507000-00024. [DOI] [PubMed] [Google Scholar]
- 20.Dexter F., Epstein R. H. Calculating institutional support that benefits both the anesthesia group and hospital. Anesth Analg. 2008;106:544–553. doi: 10.1213/ane.0b013e31815efb18. [DOI] [PubMed] [Google Scholar]
- 21.Wachtel R. E., Dexter F. Differentiating among hospitals performing physiologically complex operative procedures in the elderly. Anesthesiology. 2004;100:1552–1561. doi: 10.1097/00000542-200406000-00031. [DOI] [PubMed] [Google Scholar]
- 22.Dexter F., Masursky D., Wachtel R. E., Nussmeier N. A. Application of an online reference for reviewing basic statistical principles of operating room management. J Stat Educ. 2010;18((3)) [Google Scholar]
- 23.Greiner A. C., Knebel E. Committee on the Health Professions Education Summit. Health Professions Education: A Bridge to Quality. Washington, DC: Institute of Medicine, The National Academy; 54, 56, 57, 62, 63. Available at: http://www.nap.edu/openbook.php?record_id=10681. Accessed November 3, 2010. [Google Scholar]